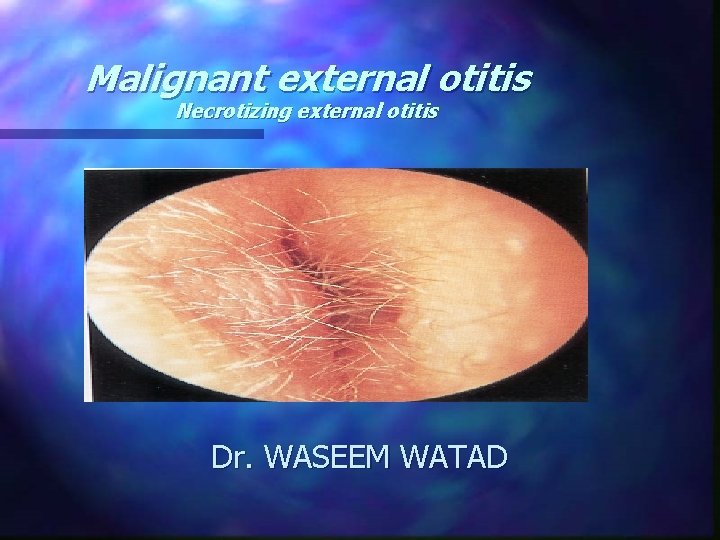
Malignant external otitis Necrotizing external otitis Dr WASEEM
- Slides: 20
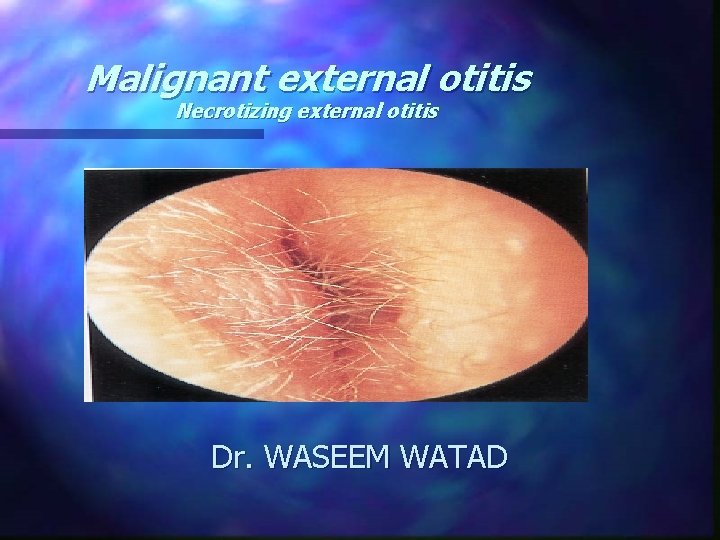
Malignant external otitis Necrotizing external otitis Dr. WASEEM WATAD
Case 1. ( SH. Y ) n n n 80 years old 3 VD , PTCA , DM-type 2 , HTN , BPH Ext. otitis with PO ABX and ear drops with improvement several months before admission severe Rt. otalgia , facial pain Rt. , and Rt. parotid mass at admission 19/09/04 Rt ear discharge Weight loss
Case 1. n n CT scan (20/09/04): Rt parotid mass , infiltration of parapharyngeal fat , EAC , infratemporal fossa , Rt. lat. pterygoid and masseter. no bony erosion and no lymphadenopathy MRI (19/10/04) : process infiltrating the Rt. ear, temporal bone , TMJ, sphenoid sinus , infratemporal fossa and skull base Biopsy of EAC polyp, parotid FNA (28/10/04) – mixed inflammation Positive culture for p. aeruginosa
Case 1. IV ABX treatment ( cephalosporine and quinolones ) with ear drops and toilette n Improvement in pain , ear discharge n There was no CN involvement n
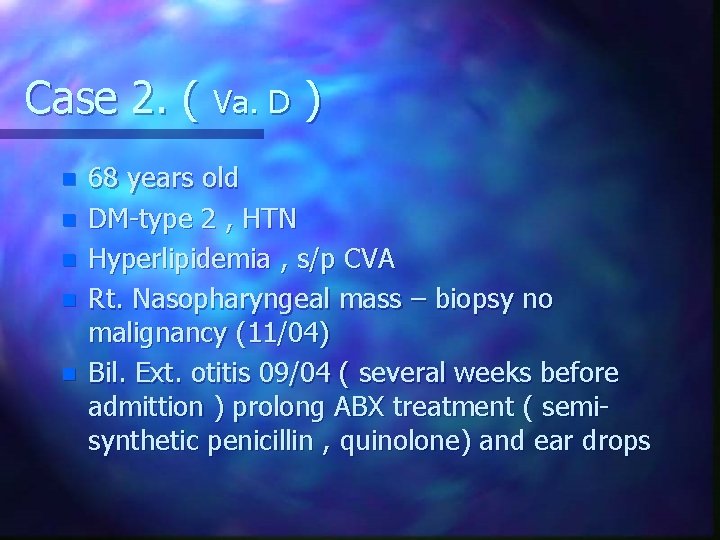
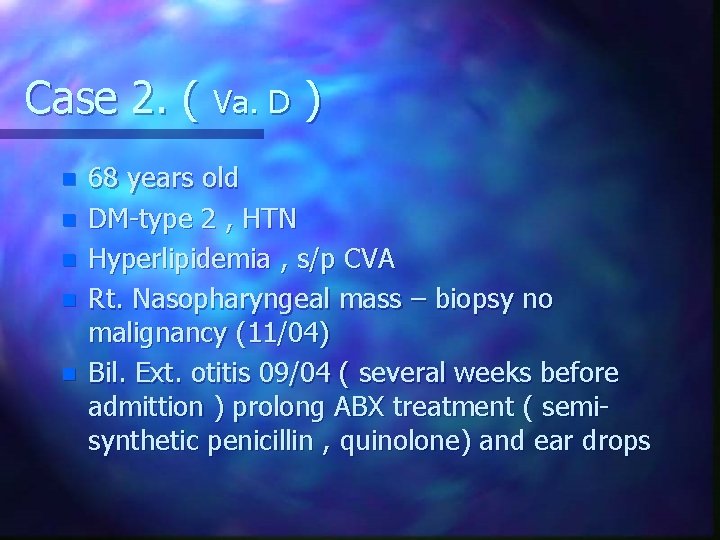
Case 2. ( Va. D ) n n n 68 years old DM-type 2 , HTN Hyperlipidemia , s/p CVA Rt. Nasopharyngeal mass – biopsy no malignancy (11/04) Bil. Ext. otitis 09/04 ( several weeks before admittion ) prolong ABX treatment ( semisynthetic penicillin , quinolone) and ear drops
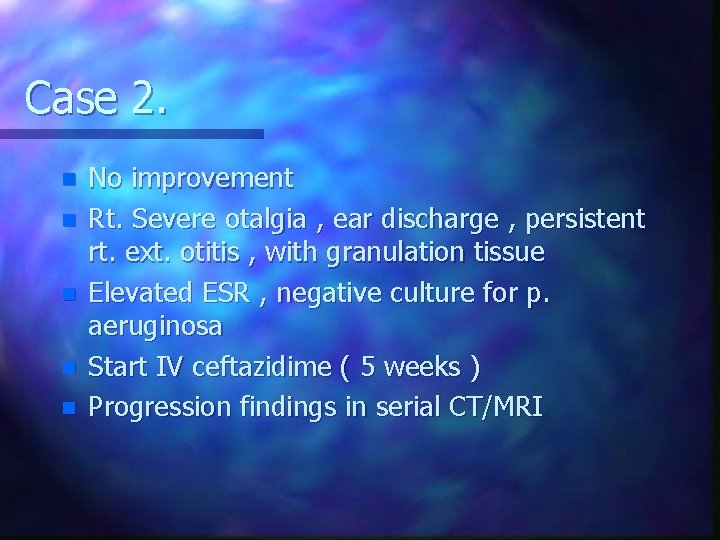
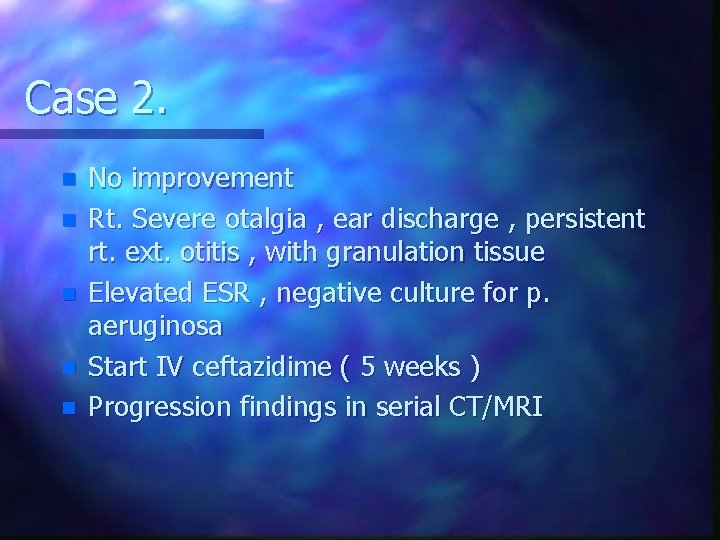
Case 2. n n n No improvement Rt. Severe otalgia , ear discharge , persistent rt. ext. otitis , with granulation tissue Elevated ESR , negative culture for p. aeruginosa Start IV ceftazidime ( 5 weeks ) Progression findings in serial CT/MRI
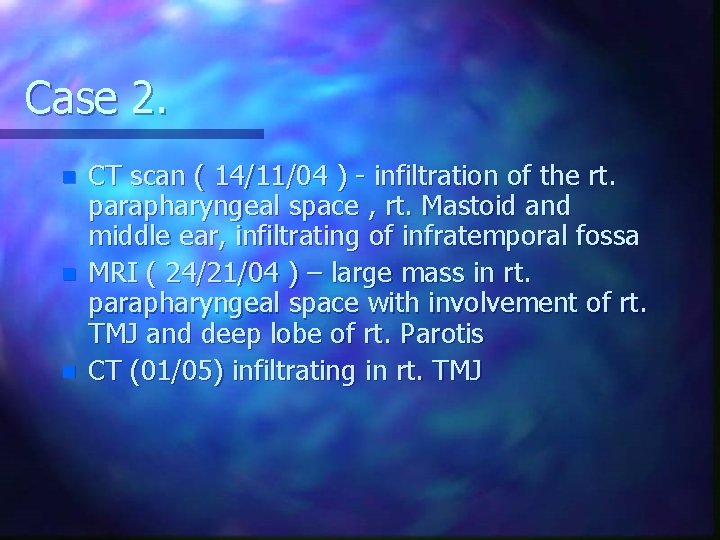
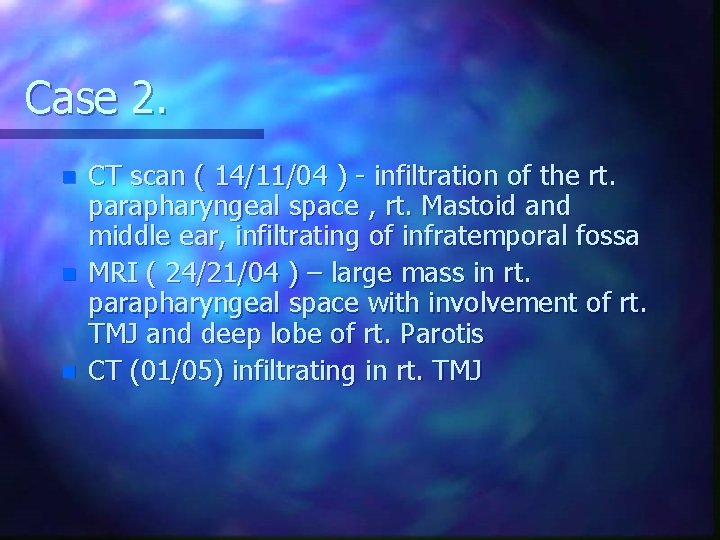
Case 2. n n n CT scan ( 14/11/04 ) - infiltration of the rt. parapharyngeal space , rt. Mastoid and middle ear, infiltrating of infratemporal fossa MRI ( 24/21/04 ) – large mass in rt. parapharyngeal space with involvement of rt. TMJ and deep lobe of rt. Parotis CT (01/05) infiltrating in rt. TMJ
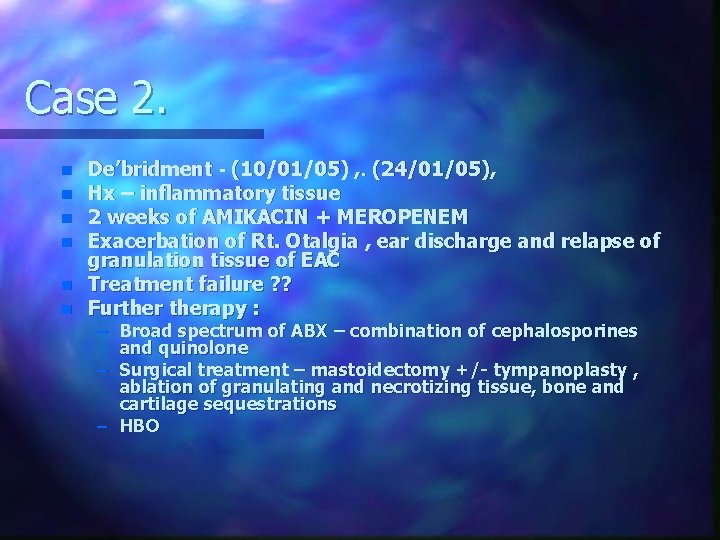
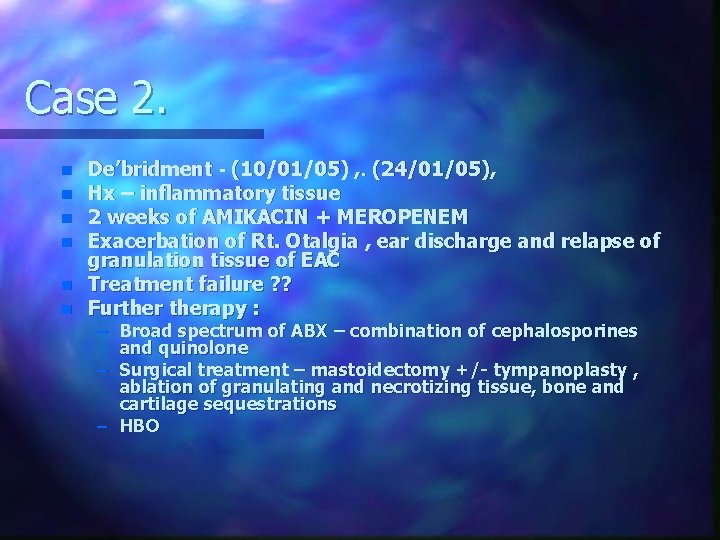
Case 2. n n n De’bridment - (10/01/05) , . (24/01/05), Hx – inflammatory tissue 2 weeks of AMIKACIN + MEROPENEM Exacerbation of Rt. Otalgia , ear discharge and relapse of granulation tissue of EAC Treatment failure ? ? Furtherapy : – Broad spectrum of ABX – combination of cephalosporines and quinolone – Surgical treatment – mastoidectomy +/- tympanoplasty , ablation of granulating and necrotizing tissue, bone and cartilage sequestrations – HBO
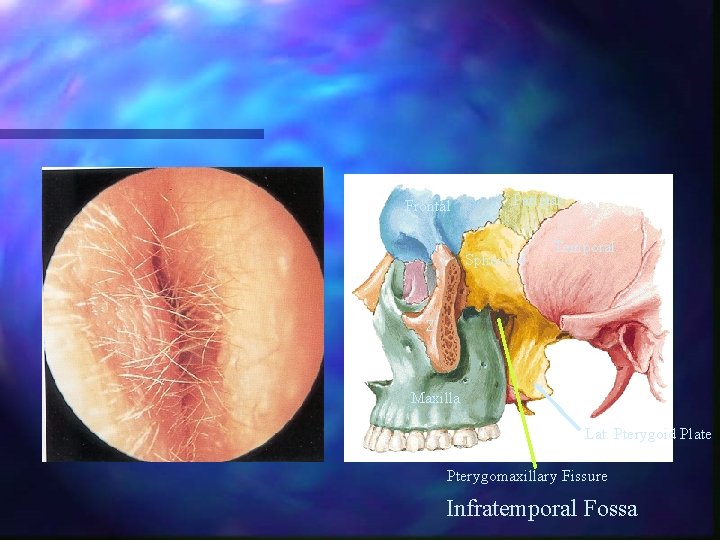
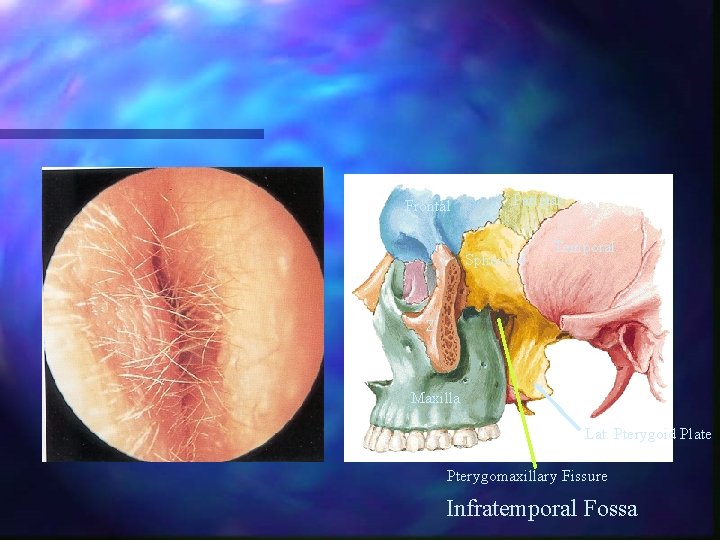
Frontal Parietal Sphenoid Temporal Z Maxilla Lat. Pterygoid Plate Pterygomaxillary Fissure Infratemporal Fossa
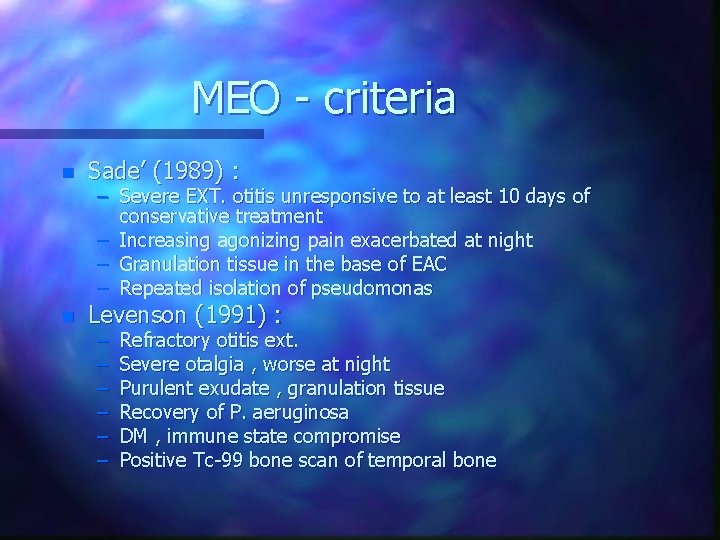
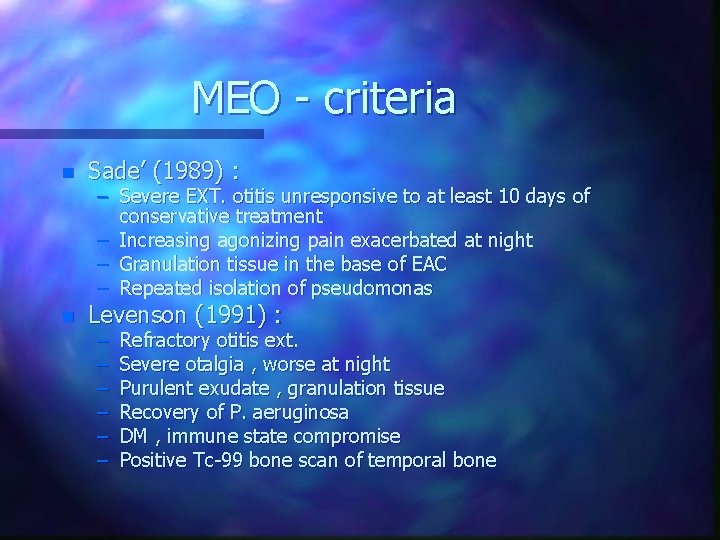
MEO - criteria n Sade’ (1989) : n Levenson (1991) : – Severe EXT. otitis unresponsive to at least 10 days of conservative treatment – Increasing agonizing pain exacerbated at night – Granulation tissue in the base of EAC – Repeated isolation of pseudomonas – – – Refractory otitis ext. Severe otalgia , worse at night Purulent exudate , granulation tissue Recovery of P. aeruginosa DM , immune state compromise Positive Tc-99 bone scan of temporal bone
etiopathogenesis
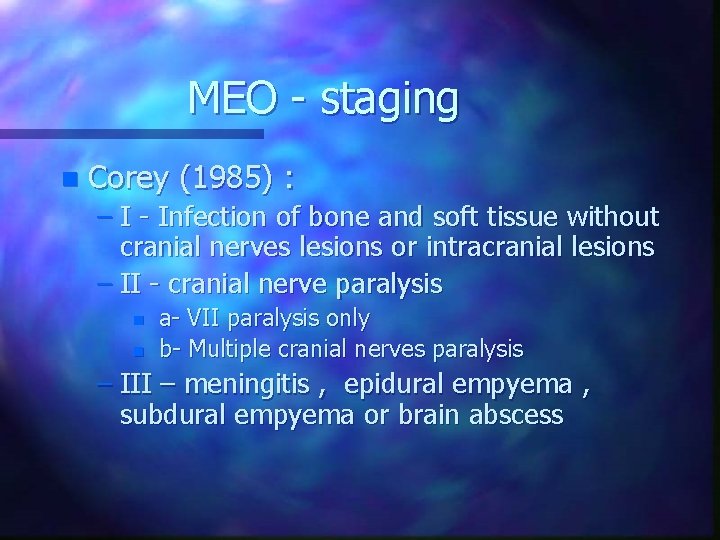
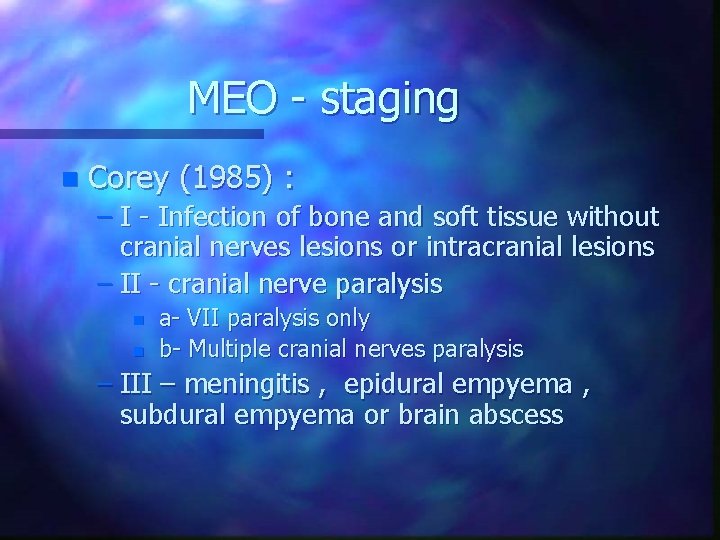
MEO - staging n Corey (1985) : – I - Infection of bone and soft tissue without cranial nerves lesions or intracranial lesions – II - cranial nerve paralysis n n a- VII paralysis only b- Multiple cranial nerves paralysis – III – meningitis , epidural empyema , subdural empyema or brain abscess
NEO - diagnosis Clinical findings n Laboratory tests n Culture n Ga-67, Tc-99 scans n HR-CT with contrast n Biopsy of granulation tissue n
mortality (46% (1968 n 10% recent articles n High mortality in facial n. paralysis n
Management – cont. n n n HR-CT contrast evaluation Ga-67 (every 4 weeks) follow up with treatment Management underlying process ( DM / immunosuppressive) Surgical de’bridment , drinage – intracranial ext. , brain abscess 6 weeks of ABX , repeat cultures , oral ABX after 2 weeks of cessation of symptoms
Management – cont. n Deep biopsy of granulation tissue – underlying carcinoma
Therapeutic problems n Main problem is : – Choice of the ABX – Duration of treatment
Therapeutic problems n Duration of treatment – Standard indication ( 6 -8 weeks ) – Identifying objective parameter of definitive recovery Healing of skin EAC n ESR n Ga-67 n
Therapeutic problems n Surgical treatment : – Complementary role – Mastoidectomy +/- tympanoplasty – Recommendation – biopsy , cleansing , ablation of necrotizing and granulation tissue and the bone , cartilage sequestrations
Therapeutic problems n Hyperbaric oxygen therapy – Daily , 2. 4 -3 atm, 90 minutea , 30 courses – Indications : advanced stages , recurrent cases, refractory to ABX – Hypoxia impaired oxygen dependent bacterial killing by phagocytosis