Male Circumcision Is it Worth The Pain Vijay













- Slides: 46
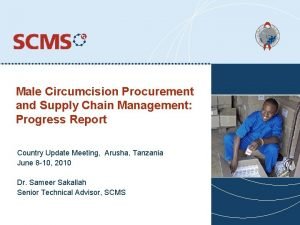
Male Circumcision: Is it Worth The Pain? Vijay Kandula, MD MPH AAHIVS Adjunct Assistant Professor Division of Public Health, Department of Family and Preventive Medicine University of Utah, Salt Lake City
Acknowledgements: Male Circumcision to Reduce Risk for HIV Infection: Current Knowledge and Future Challenges Stephen Moses MD, MPH University of Manitoba
Current Prevention Tools Against Heterosexual HIV Transmission · Behavior Change – Abstinence – Faithfulness – Condoms · STI Treatment · Voluntary Counseling and Testing · Pr. EP? · Anti-retroviral therapy? · Microbicides? · Diaphragm? · Vaccines?

Male circumcision is probably the oldest and most common surgery performed in humans
What is Male Circumcision? · Male circumcision is the surgical removal of some or all of the foreskin (or prepuce) from the penis 1. Alanis MC, Lucidi RS. Neonatal circumcision: a review of the world’s oldest and most controversial operation. Obstet Gynecol Surv. 2004 May; 59(5): 379 -95.

Biologic Plausibility Compared with the dry external skin surface, the inner mucosa of the foreskin has · less keratinization (deposition of fibrous protein), · a higher density of target cells for HIV infection (Langerhans cells), and is · more susceptible to HIV infection than other · penile tissue in laboratory studies [2]. · greater susceptibility to traumatic epithelial disruptions (tears) during intercourse, 2. Patterson BK, Landay A, Siegel JN, et al. Susceptibility to human immunodeficiency virus-1 infection of human foreskin and cervical tissue grown in explant culture. Am J Pathol. 2002 Sep; 161(3): 867 -73.
Biologic Plausibility. . contd · microenvironment in the preputial sac between the unretracted foreskin and the glans penis may be conducive to viral survival · higher STI rates – Genital ulcerative disease, e. g. : syphilis, may also increase susceptibility to HIV infection [4]. 3. Szabo R, Short RV. How does male circumcision protect against HIV infection? BMJ. 2000 Jun 10; 320(7249): 1592 -4. 4. Weiss HA, Thomas SL, Munabi SK, Hayes RJ. Male circumcision and risk of syphilis, chancroid, and genital herpes: a systematic review and meta-analysis. Sex Transm Infect. 2006 Apr; 82(2): 101 -9; discussion 10.
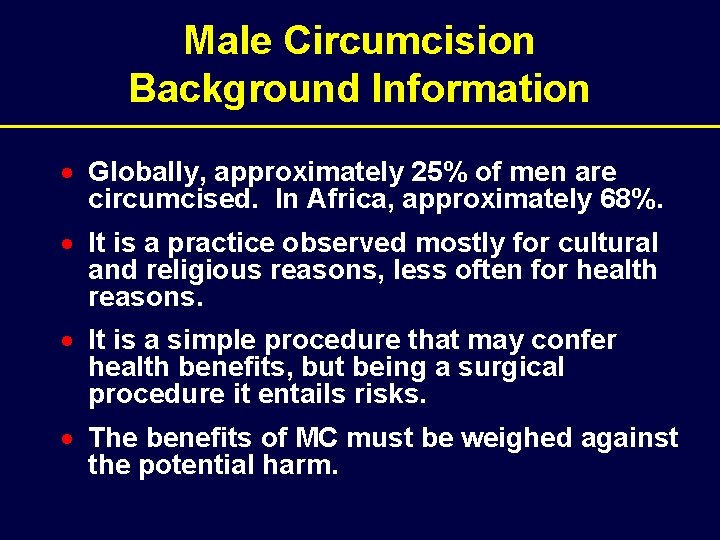
Male Circumcision Background Information · Globally, approximately 25% of men are circumcised. In Africa, approximately 68%. · It is a practice observed mostly for cultural and religious reasons, less often for health reasons. · It is a simple procedure that may confer health benefits, but being a surgical procedure it entails risks. · The benefits of MC must be weighed against the potential harm.

Studies of the Association Between Circumcision and HIV Infection · · 4 ecological studies 35 cross-sectional studies 14 prospective studies The adjusted relative risk of HIV infection for circumcised men in the prospective studies is 0. 52 – 0. 18

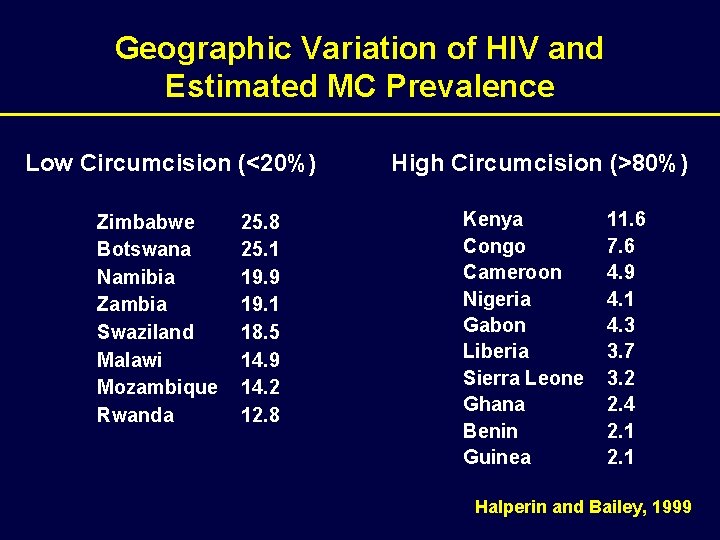
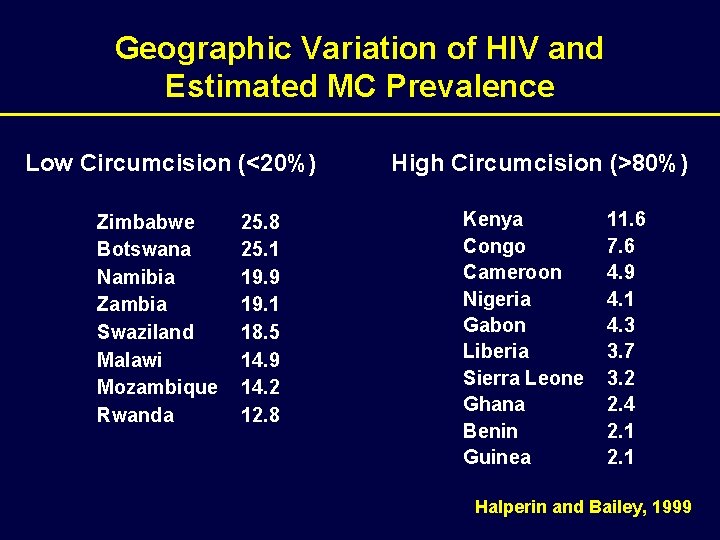
Geographic Variation of HIV and Estimated MC Prevalence Low Circumcision (<20%) Zimbabwe Botswana Namibia Zambia Swaziland Malawi Mozambique Rwanda 25. 8 25. 1 19. 9 19. 1 18. 5 14. 9 14. 2 12. 8 High Circumcision (>80%) Kenya Congo Cameroon Nigeria Gabon Liberia Sierra Leone Ghana Benin Guinea 11. 6 7. 6 4. 9 4. 1 4. 3 3. 7 3. 2 2. 4 2. 1 Halperin and Bailey, 1999
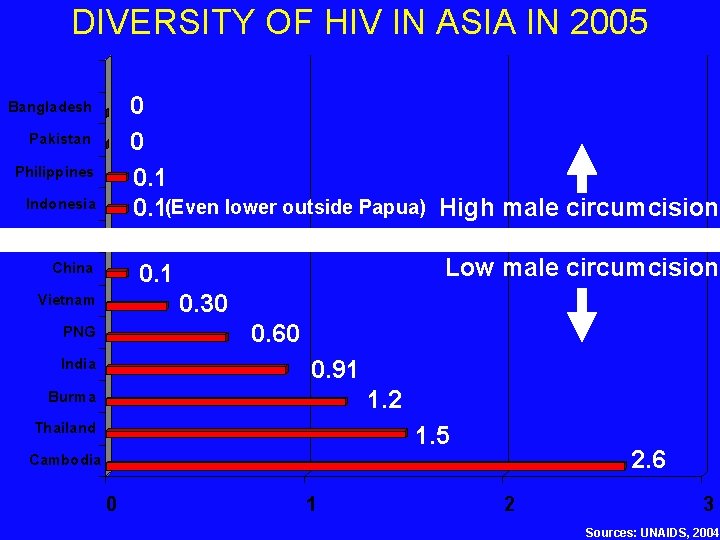
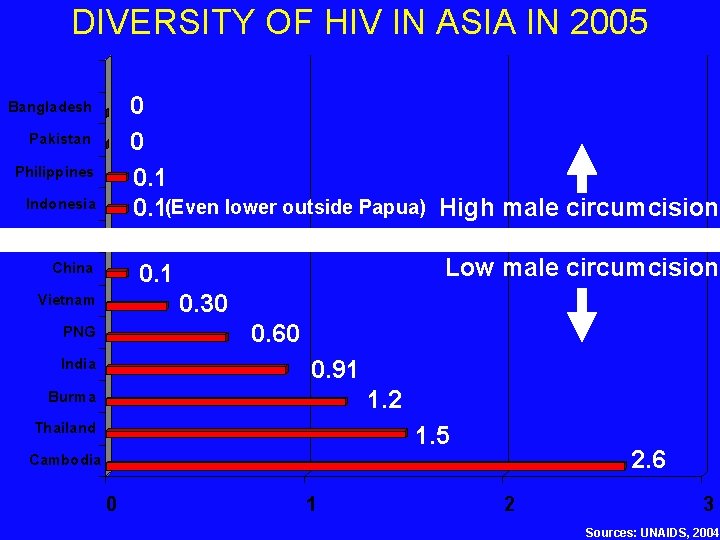
DIVERSITY OF HIV IN ASIA IN 2005 0 0 0. 1(Even lower outside Papua) High male circumcision Bangladesh Pakistan Philippines Indonesia Fiji China Low male circumcision 0. 1 0. 30 Vietnam 0. 60 PNG India 0. 91 1. 2 Burma Thailand 1. 5 2. 6 Cambodia 0 1 2 3 Sources: UNAIDS, 2004
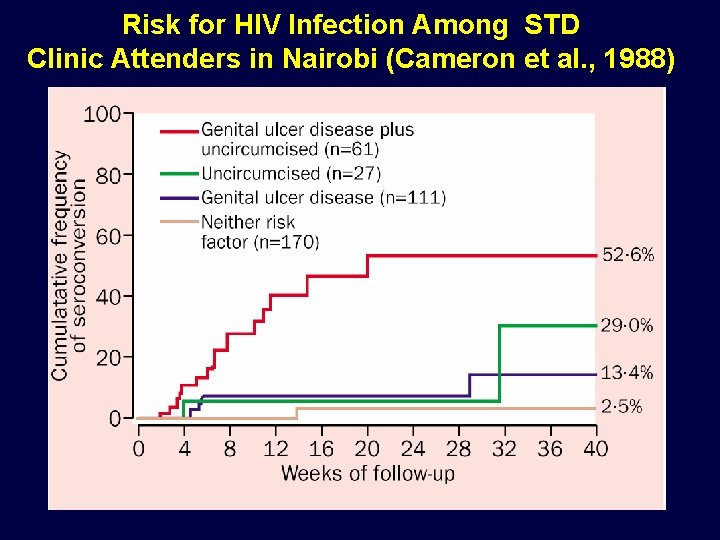
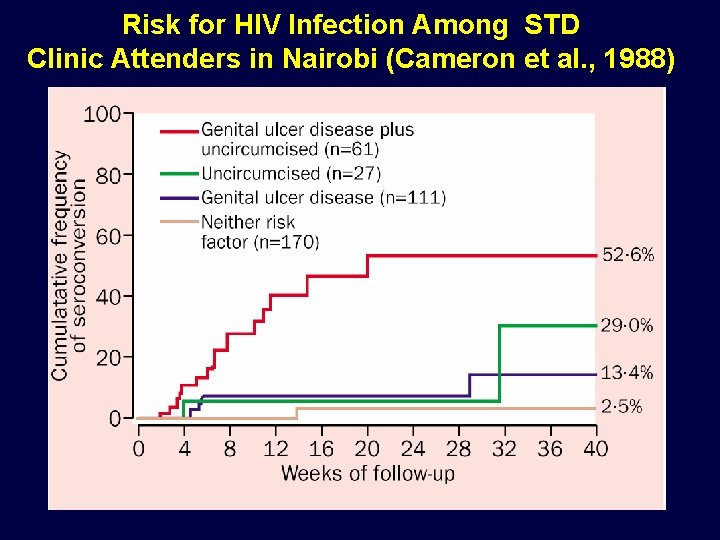
Risk for HIV Infection Among STD Clinic Attenders in Nairobi (Cameron et al. , 1988)

Meta-analysis (Weiss et al. , AIDS 2000; 14: 2261 -70)
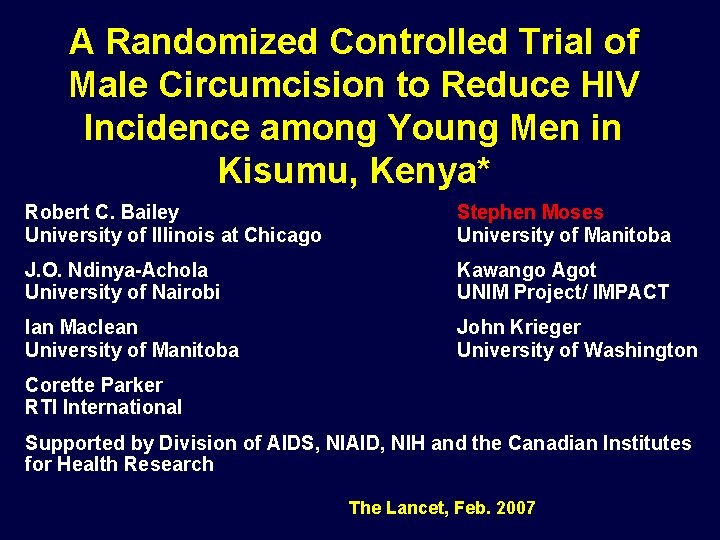
A Randomized Controlled Trial of Male Circumcision to Reduce HIV Incidence among Young Men in Kisumu, Kenya* Robert C. Bailey University of Illinois at Chicago Stephen Moses University of Manitoba J. O. Ndinya-Achola University of Nairobi Kawango Agot UNIM Project/ IMPACT Ian Maclean University of Manitoba John Krieger University of Washington Corette Parker RTI International Supported by Division of AIDS, NIAID, NIH and the Canadian Institutes for Health Research The Lancet, Feb. 2007
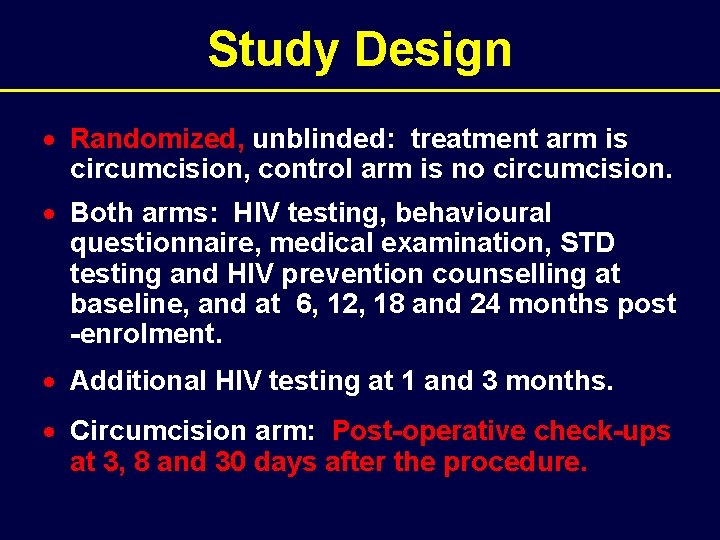
Study Design · Randomized, unblinded: treatment arm is circumcision, control arm is no circumcision. · Both arms: HIV testing, behavioural questionnaire, medical examination, STD testing and HIV prevention counselling at baseline, and at 6, 12, 18 and 24 months post -enrolment. · Additional HIV testing at 1 and 3 months. · Circumcision arm: Post-operative check-ups at 3, 8 and 30 days after the procedure.
Clients of STD clinics Clients of VCT centres Organizations (boda, jua kali, car washers) Peer recruiters Fliers, radio, shows Beaches, discos, rural communities
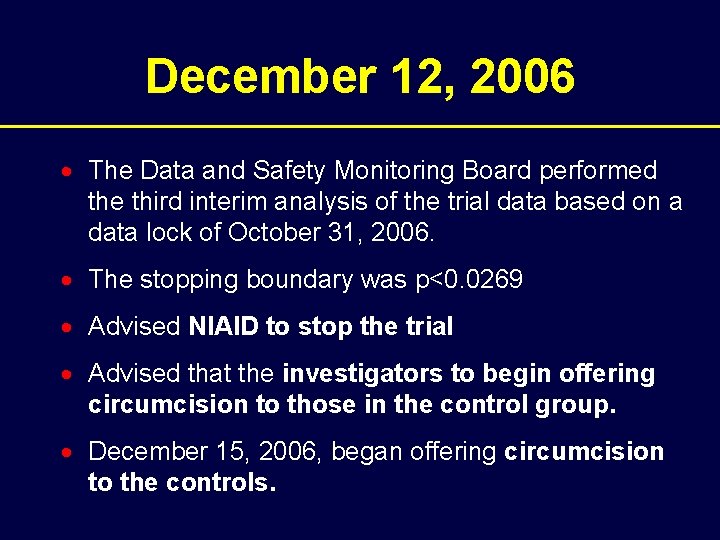
December 12, 2006 · The Data and Safety Monitoring Board performed the third interim analysis of the trial data based on a data lock of October 31, 2006. · The stopping boundary was p<0. 0269 · Advised NIAID to stop the trial · Advised that the investigators to begin offering circumcision to those in the control group. · December 15, 2006, began offering circumcision to the controls.
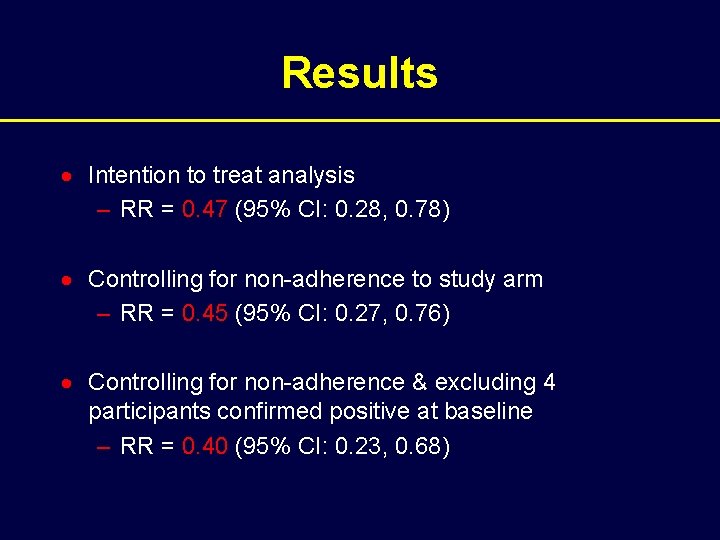
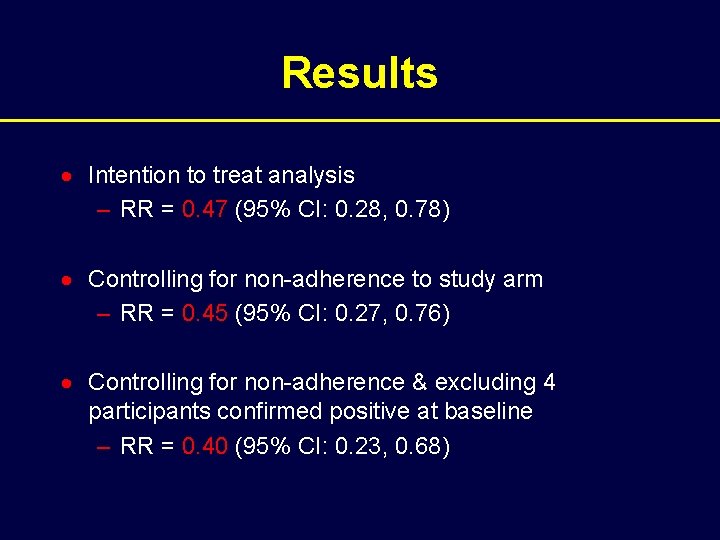
Results · Intention to treat analysis – RR = 0. 47 (95% CI: 0. 28, 0. 78) · Controlling for non-adherence to study arm – RR = 0. 45 (95% CI: 0. 27, 0. 76) · Controlling for non-adherence & excluding 4 participants confirmed positive at baseline – RR = 0. 40 (95% CI: 0. 23, 0. 68)

Summary of Behavioural Results · From baseline to M 6, both circumcised and uncircumcised participants reported safer sexual behaviours in absolute terms. · No significant with respect to changes in sexual behaviour measures from baseline to M 24. · Uncircumcised men reported less risky behaviour at M 24.
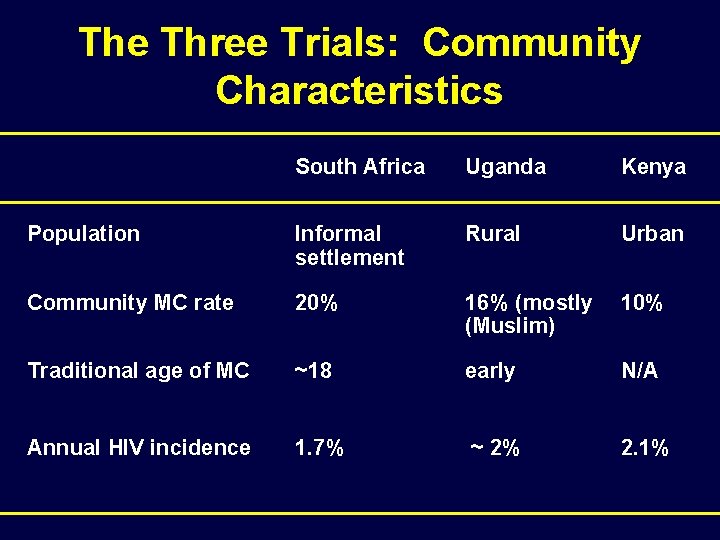
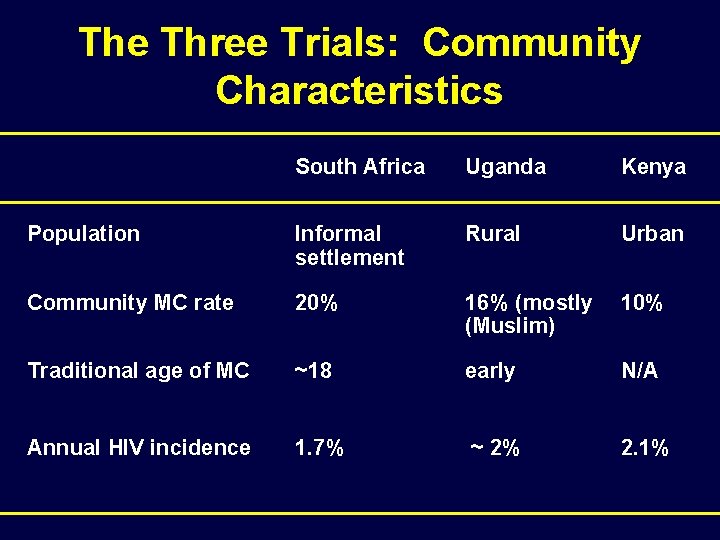
The Three Trials: Community Characteristics South Africa Uganda Kenya Population Informal settlement Rural Urban Community MC rate 20% 16% (mostly (Muslim) 10% Traditional age of MC ~18 early N/A Annual HIV incidence 1. 7% ~ 2% 2. 1%
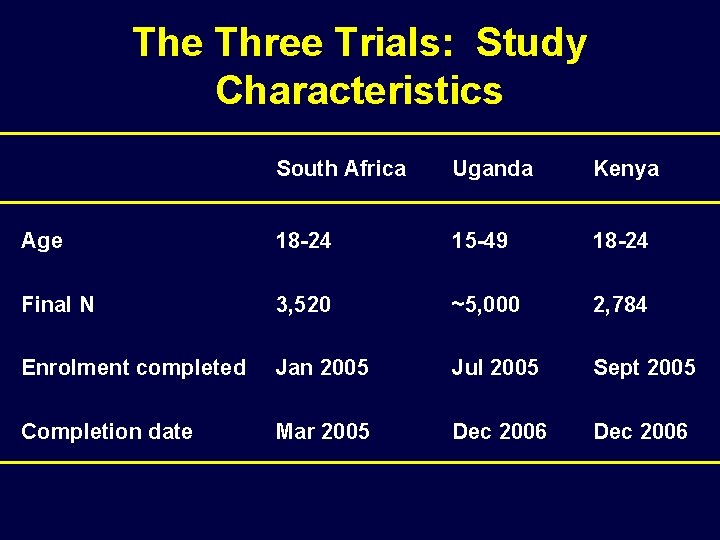
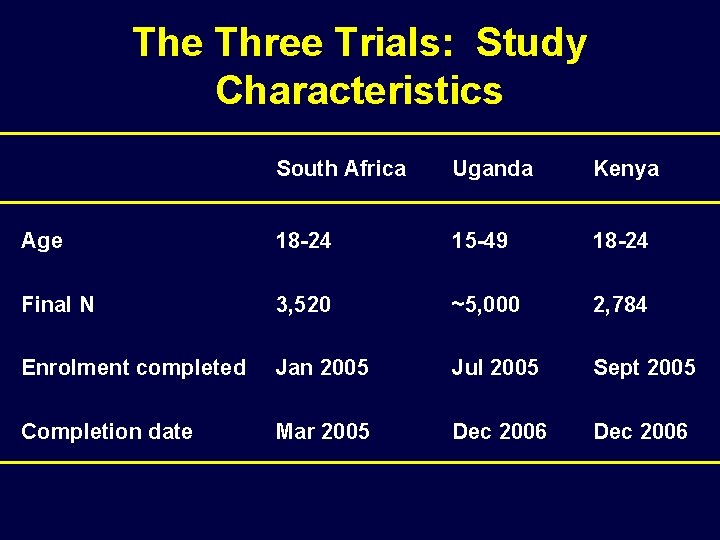
The Three Trials: Study Characteristics South Africa Uganda Kenya Age 18 -24 15 -49 18 -24 Final N 3, 520 ~5, 000 2, 784 Enrolment completed Jan 2005 Jul 2005 Sept 2005 Completion date Mar 2005 Dec 2006
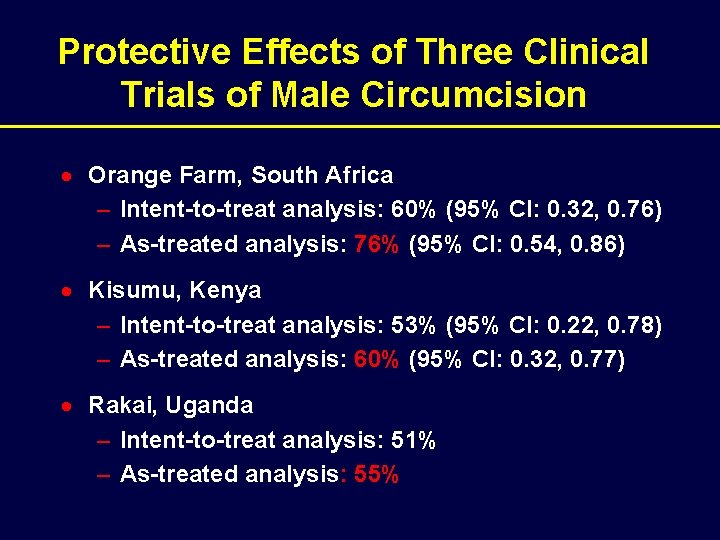
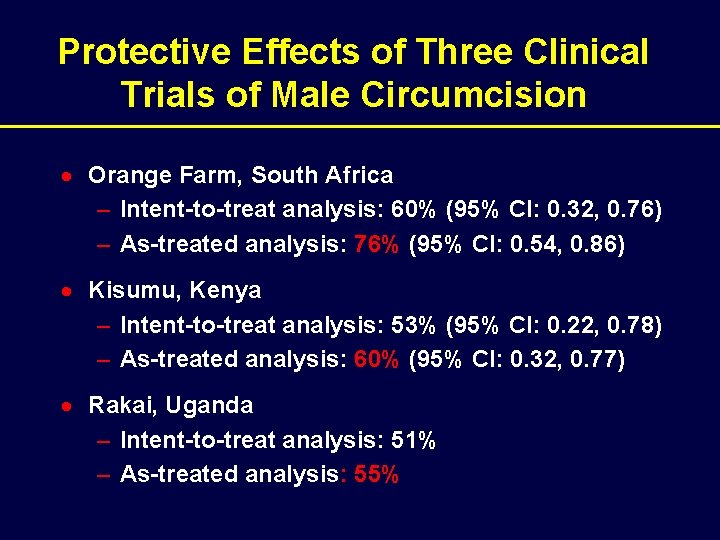
Protective Effects of Three Clinical Trials of Male Circumcision · Orange Farm, South Africa – Intent-to-treat analysis: 60% (95% CI: 0. 32, 0. 76) – As-treated analysis: 76% (95% CI: 0. 54, 0. 86) · Kisumu, Kenya – Intent-to-treat analysis: 53% (95% CI: 0. 22, 0. 78) – As-treated analysis: 60% (95% CI: 0. 32, 0. 77) · Rakai, Uganda – Intent-to-treat analysis: 51% – As-treated analysis: 55%
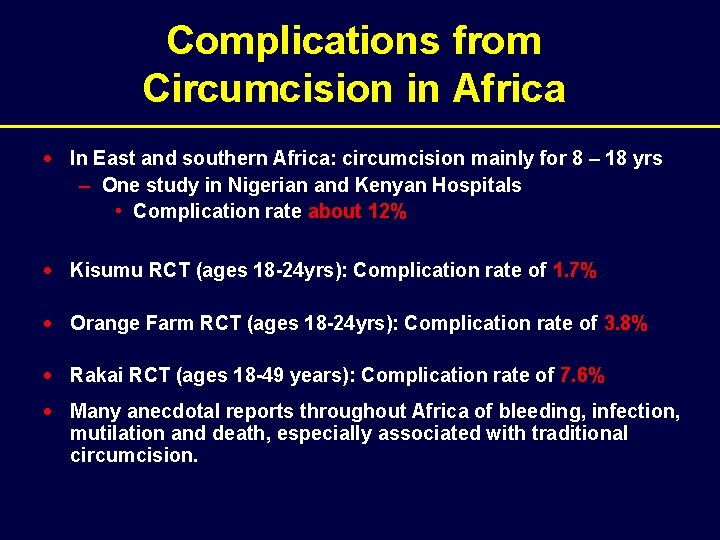
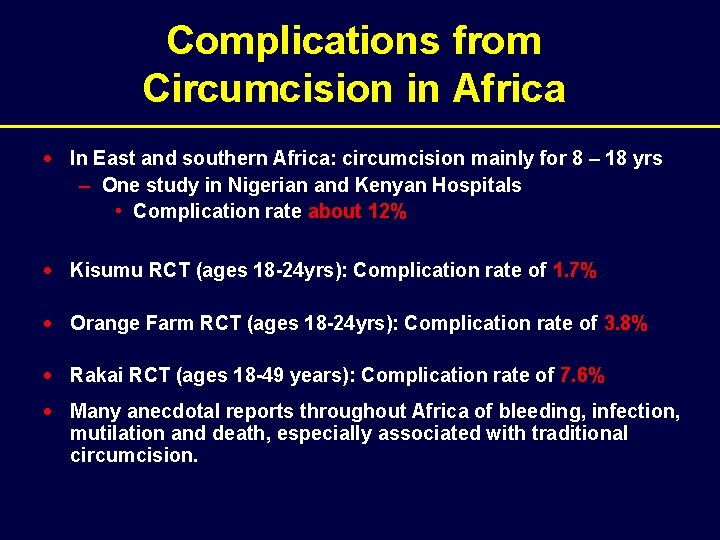
Complications from Circumcision in Africa · In East and southern Africa: circumcision mainly for 8 – 18 yrs – One study in Nigerian and Kenyan Hospitals • Complication rate about 12% · Kisumu RCT (ages 18 -24 yrs): Complication rate of 1. 7% · Orange Farm RCT (ages 18 -24 yrs): Complication rate of 3. 8% · Rakai RCT (ages 18 -49 years): Complication rate of 7. 6% · Many anecdotal reports throughout Africa of bleeding, infection, mutilation and death, especially associated with traditional circumcision.
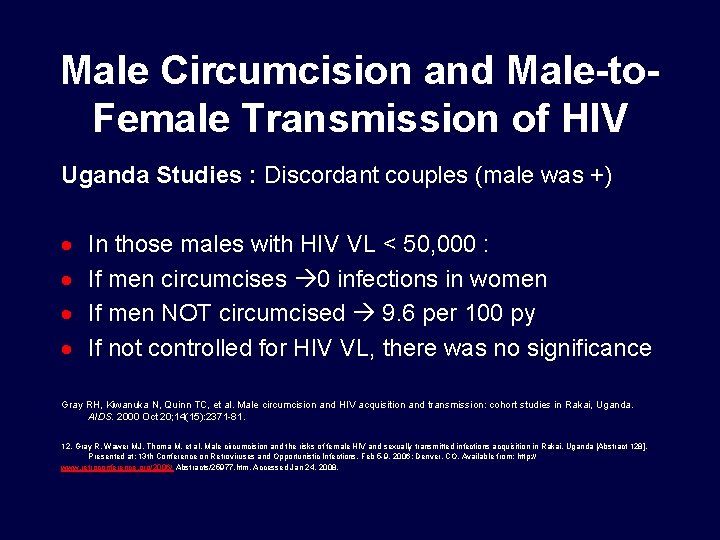
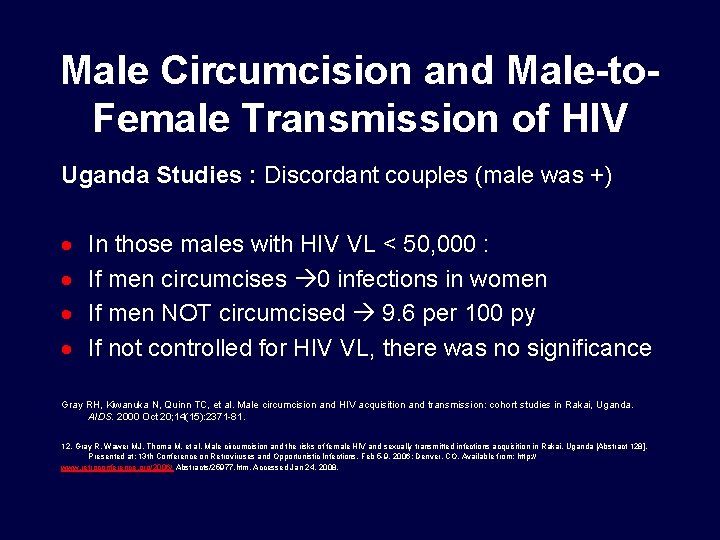
Male Circumcision and Male-to. Female Transmission of HIV Uganda Studies : Discordant couples (male was +) · · In those males with HIV VL < 50, 000 : If men circumcises 0 infections in women If men NOT circumcised 9. 6 per 100 py If not controlled for HIV VL, there was no significance Gray RH, Kiwanuka N, Quinn TC, et al. Male circumcision and HIV acquisition and transmission: cohort studies in Rakai, Uganda. AIDS. 2000 Oct 20; 14(15): 2371 -81. 12. Gray R, Wawer MJ, Thoma M, et al. Male circumcision and the risks of female HIV and sexually transmitted infections acquisition in Rakai, Uganda [Abstract 128]. Presented at: 13 th Conference on Retroviruses and Opportunistic Infections. Feb 5 -9, 2006; Denver, CO. Available from: http: // www. retroconference. org/2006/ Abstracts/25977. htm. Accessed Jan 24, 2008.

Male Circumcision and Male-to. Female Transmission of HIV Another Study in Uganda Discordant Couples · Higher HIV infection rates in women partners · Attributed resumption of sex prior to certified post surgical wound healing · no difference in HIV acquisition after wound healing was completed Wawer MJ. Trial of male circumcision: HIV, sexually transmitted disease (STD) and behavioral effects in men, women and the community. Available from: http: //www. clinicaltrials. gov/ct 2/show/NCT 00124 878? term=circumcision+AND+uganda&ran k=2. Accessed Jan 23, 2008.
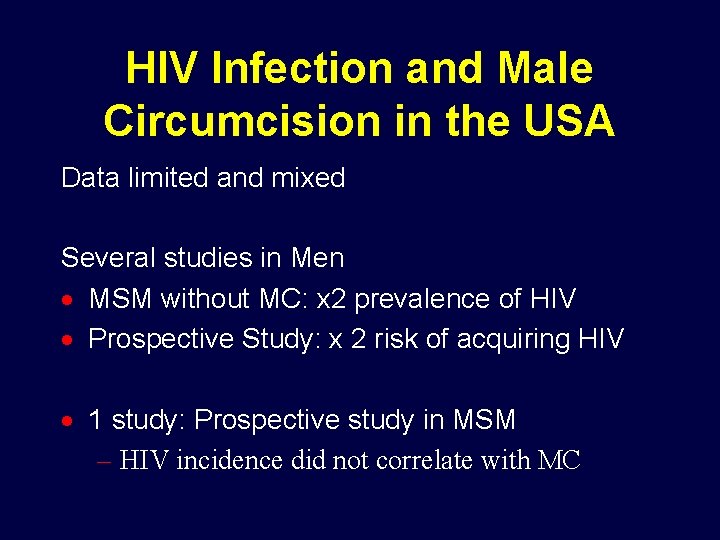
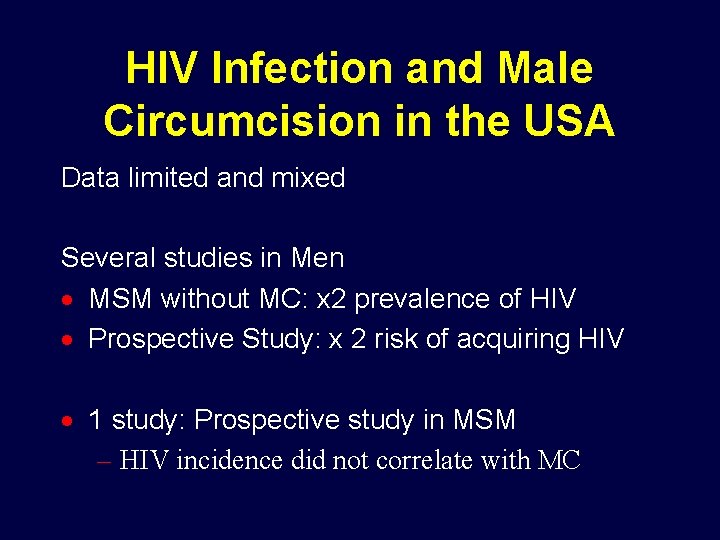
HIV Infection and Male Circumcision in the USA Data limited and mixed Several studies in Men · MSM without MC: x 2 prevalence of HIV · Prospective Study: x 2 risk of acquiring HIV · 1 study: Prospective study in MSM – HIV incidence did not correlate with MC

HIV Infection and Male Circumcision in the USA: Challenges · NHANES 1999– 04, Ault Men: 79% circumcised, – 88% white 73% black – 42% Mexican 50% other races · Caveat: be subject to misclassification. · Risser JM et al: study of adolescents: correctly identified their circumcision status as verified by physical exam • 69% of circumcised • 65% of uncircumcised · American Academy of Pediatrics (AAP) – Neutral Stance

Botswana – MC uptake 50% over 10 years, if relative risk = 0. 5 if relative risk = 0. 33
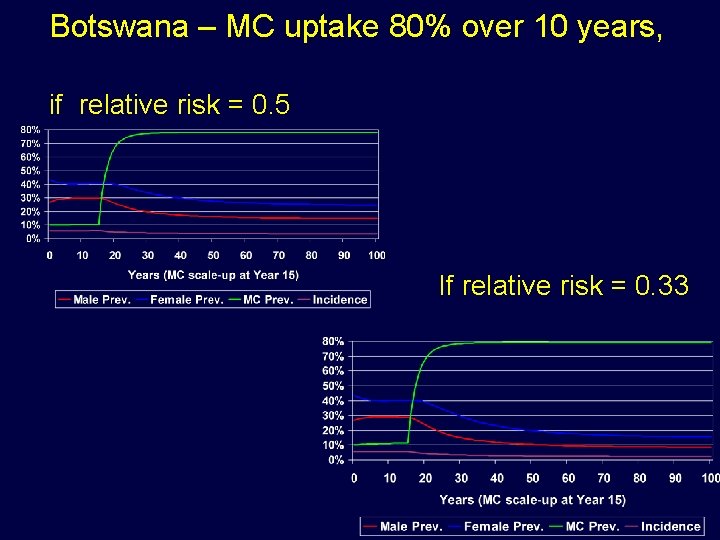
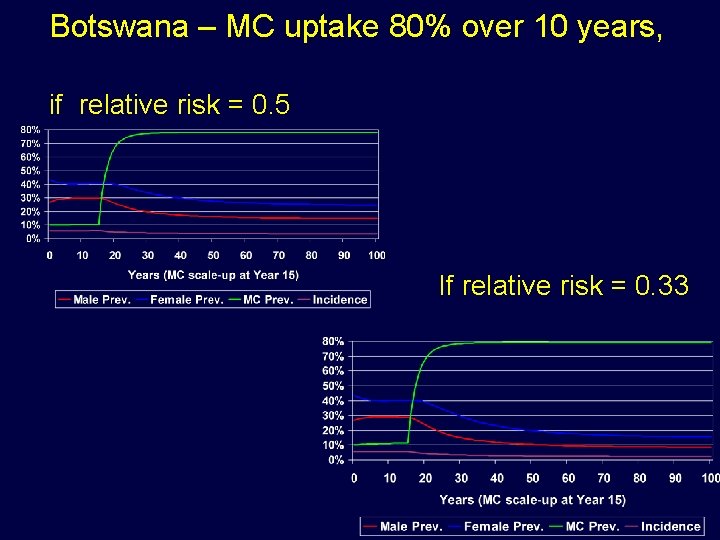
Botswana – MC uptake 80% over 10 years, if relative risk = 0. 5 If relative risk = 0. 33
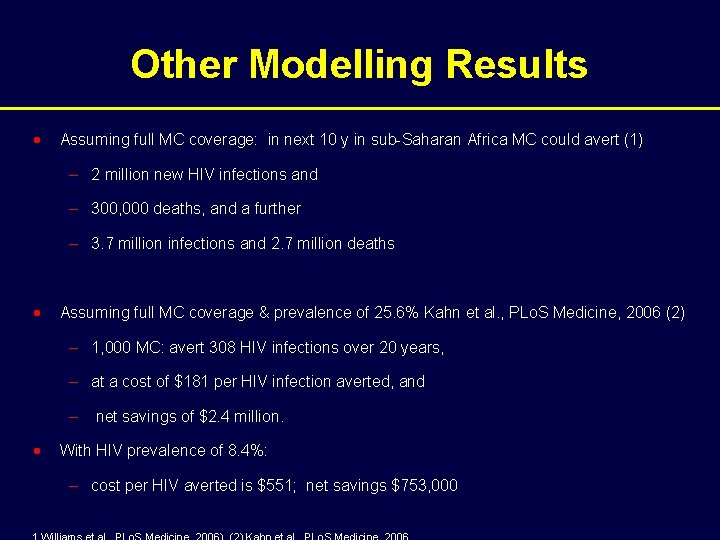
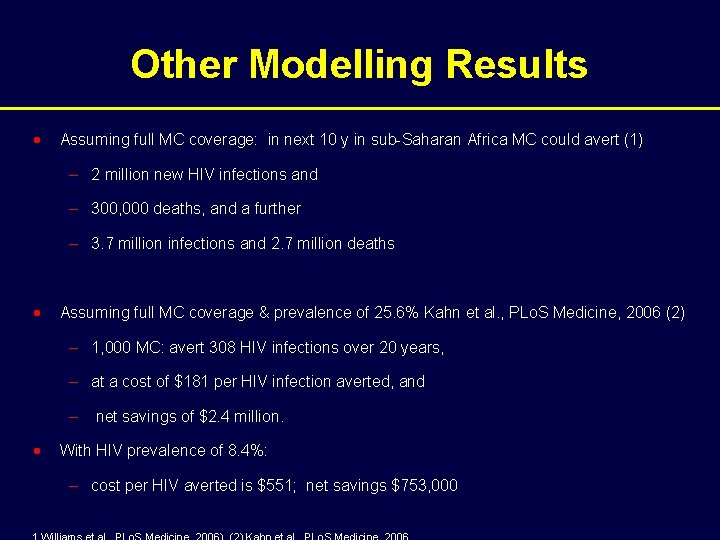
Other Modelling Results · Assuming full MC coverage: in next 10 y in sub-Saharan Africa MC could avert (1) – 2 million new HIV infections and – 300, 000 deaths, and a further – 3. 7 million infections and 2. 7 million deaths · Assuming full MC coverage & prevalence of 25. 6% Kahn et al. , PLo. S Medicine, 2006 (2) – 1, 000 MC: avert 308 HIV infections over 20 years, – at a cost of $181 per HIV infection averted, and – net savings of $2. 4 million. · With HIV prevalence of 8. 4%: – cost per HIV averted is $551; net savings $753, 000
Male circumcision to reduce risk for HIV infection: where do we go from here? · Public health strategies · Individual health responses
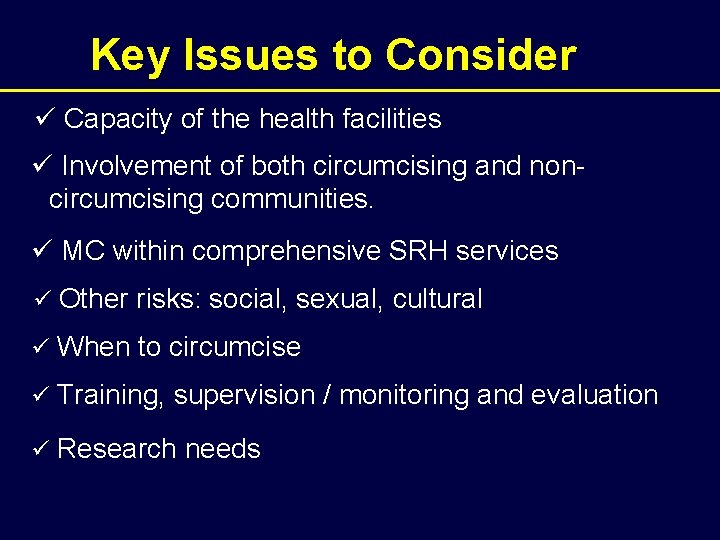
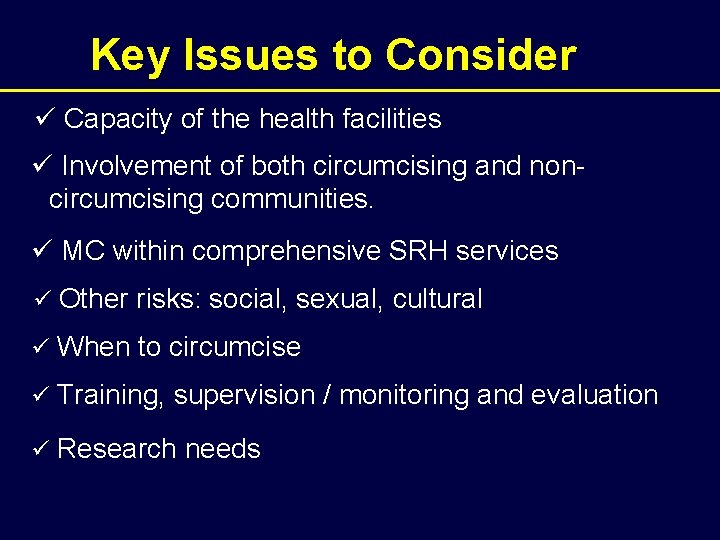
Key Issues to Consider ü Capacity of the health facilities ü Involvement of both circumcising and non- circumcising communities. ü MC within comprehensive SRH services ü Other risks: social, sexual, cultural ü When to circumcise ü Training, supervision / monitoring and evaluation ü Research needs
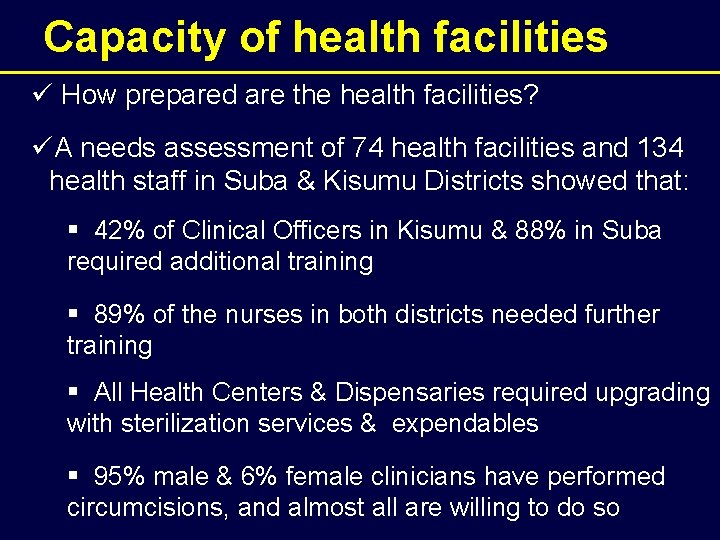
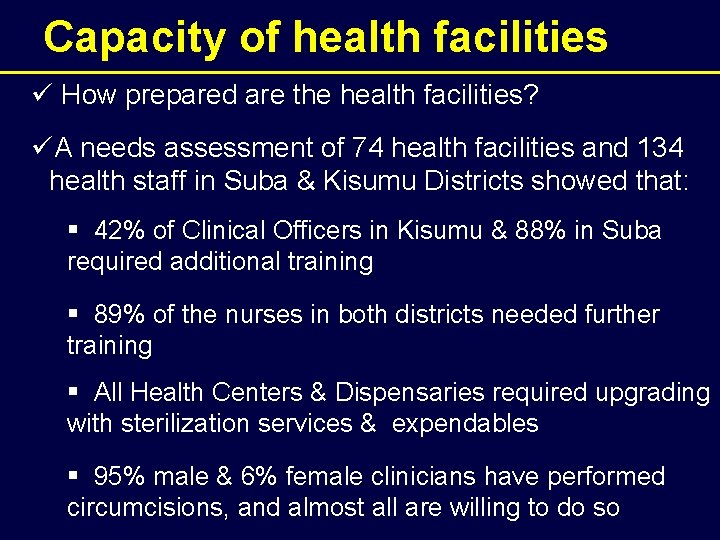
Capacity of health facilities ü How prepared are the health facilities? üA needs assessment of 74 health facilities and 134 health staff in Suba & Kisumu Districts showed that: § 42% of Clinical Officers in Kisumu & 88% in Suba required additional training § 89% of the nurses in both districts needed further training § All Health Centers & Dispensaries required upgrading with sterilization services & expendables § 95% male & 6% female clinicians have performed circumcisions, and almost all are willing to do so
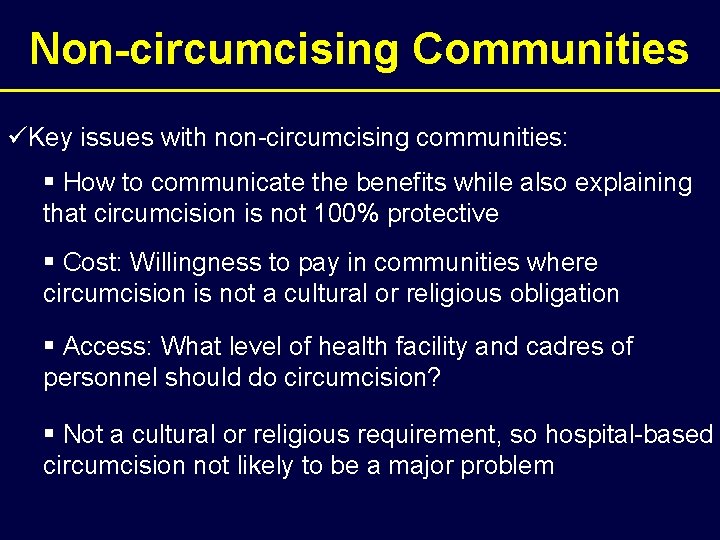
Non-circumcising Communities üKey issues with non-circumcising communities: § How to communicate the benefits while also explaining that circumcision is not 100% protective § Cost: Willingness to pay in communities where circumcision is not a cultural or religious obligation § Access: What level of health facility and cadres of personnel should do circumcision? § Not a cultural or religious requirement, so hospital-based circumcision not likely to be a major problem
Acceptability • 13 published studies from 9 countries (Botswana, Kenya, Malawi, South Africa, Swaziland, Tanzania Uganda, Zambia, Zimbabwe) – show reasonable acceptability, with acceptability among males interviewed ranging from 29 -87% (median 65%) • 69% of women favoured MC for partner • 71% of men and 81% of women were willing to circumcised their sons • Main barriers are cost, fear of pain and concern for safety
Is Cultural Change Possible? · Several of the most severely affected countries – Swaziland, Botswana, Lesotho, South Africa – have practised male circumcision in living memory · In such contexts, we are returning to traditional culture, not imposing alien culture
Is Cultural Change Possible? · What about countries without tradition of male circumcision? · In South Korea, where male circumcision was not traditionally practised, male circumcision became increasingly common after the 1950 s, reaching over 70% prevalence today.
Circumcising Communities ü Key issues with circumcising communities are: § Can traditional circumcisers be trained to provide safe circumcision? o Can they perform safe circumcision without suturing? o Should they do suturing outside a clinical setting? § How to encourage young men to go to health facilities § How to identify qualified circumcisers & educate parents & sons on how to find or identify them. § Train candidates and circumcisers on wound care
MC Within Comprehensive SRH ü Minimum package: § Behavioral counseling, including safe sex after MC § HIV counseling and testing § STI diagnosis, treatment and partner referral ü Additionally: § Gender sensitivity training § Family planning § Access to female partners

When to Circumcise üKisumu and SA trials: 18 -24 years; Rakai, 18 -49 yrs üQuestions: Infants? Pre-pubescent? Adolescent? Adult? üBenefit of Infants – less pain? heal fast? But: § Parents likely hesitant about subjecting babies to the procedure § Cultural meaning of rite of passage compromised § However, there are ethical concerns in circ’ng minors üPrepubescent and adolescent preferred in the Kisumu & Suba needs assessments üBest before initiation of sex
Training, Supervision, Monitoring and Evaluation ü Possible approaches to training/service provision § Centres of excellence (multiplicative) § Mobile/outreach services by experts (issue of f/u? ) § Circumcision blitzes (issue of f/u? ) § Replicate local best practices among circumcising populations ü Supervision and M&E: § Hierarchical (provincial => district => health center) § Localized (at least one staff trained for every facility) ü Certification for training, supervision & M&E personnel

Operations Research · Needs assessments – Training, equipment, supplies · Integration of MC services with VCT, STI treatment, behavioural counseling, and male reproductive services · Acceptability – Barriers and facilitators – Uptake by age, education, residence, gender · Acceptability outside Africa – India, China, Caribbean · Safety – evaluation of AEs in medical and traditional settings, including local models · Scaling up from demonstration to national programs · Trials of sutureless procedures for adults – Mogen, Gomco clamps, Plastibell, other


Acknowledgements · Kawango Agot, UNIM Project · Robert C. Bailey, University of Illinois at Chicago · David Wilson, World Bank
 Baptism vs circumcision
Baptism vs circumcision Male circumcision
Male circumcision Male circumcision
Male circumcision Male circumcision
Male circumcision Anything worth doing is not necessarily worth doing well
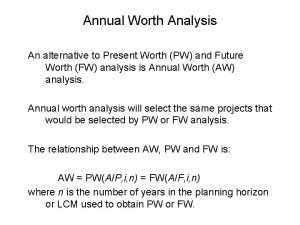
Anything worth doing is not necessarily worth doing well Annual worth analysis example
Annual worth analysis example Present worth vs annual worth
Present worth vs annual worth Martian pain
Martian pain Menstruation during pregnancy symptoms
Menstruation during pregnancy symptoms Period vs pregnancy
Period vs pregnancy Disadvantages of circumcision
Disadvantages of circumcision Prolapsring komplikationer
Prolapsring komplikationer Circumcision
Circumcision Circumcision
Circumcision Circumcision
Circumcision Circumcision
Circumcision Circumcision
Circumcision Smegma
Smegma Pure-hearted meaning
Pure-hearted meaning Circumcision ptsd
Circumcision ptsd Vijay
Vijay Vijay kharadi ias
Vijay kharadi ias Chatbot juridique
Chatbot juridique R. vijay krishna
R. vijay krishna Vijay samant
Vijay samant Vijay sathaye
Vijay sathaye Vijay kharadi ias
Vijay kharadi ias Vijay ramchandani
Vijay ramchandani Vijay kumar mit
Vijay kumar mit Vijay bhattiprolu
Vijay bhattiprolu Vijay nayar
Vijay nayar Dr. vijay kumar
Dr. vijay kumar Vijay aswani md obituary
Vijay aswani md obituary Ifcsi
Ifcsi Vijay saraswat
Vijay saraswat Pavan kumar vijay
Pavan kumar vijay Vijay tewari
Vijay tewari Vijay tallapragada
Vijay tallapragada Số nguyên tố là
Số nguyên tố là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Tư thế worms-breton
Tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Hệ hô hấp
Hệ hô hấp Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ