Leishmania spp Trypanosoma spp Haemoflagellates of medical importance

![Trypanosomiasis [1] African Trypanosomiasis [Sleeping sickness]: Trypanosomiasis [1] African Trypanosomiasis [Sleeping sickness]:](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-10.jpg)
![[1] African Trypanosomiasis [Sleeping Sickness Disease] Geographical distribution: corresponds to that of the vector [1] African Trypanosomiasis [Sleeping Sickness Disease] Geographical distribution: corresponds to that of the vector](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-12.jpg)
![Vector: Glossina spp. [tse fly], Transmission: Cyclopropagative transmission. Infective stage: Metacyclic trypomastigotes. Mode of Vector: Glossina spp. [tse fly], Transmission: Cyclopropagative transmission. Infective stage: Metacyclic trypomastigotes. Mode of](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-15.jpg)
![Morphology [Cont. ] 2. in the vector a- Epimastigote in the midgut. b- Metacyclic Morphology [Cont. ] 2. in the vector a- Epimastigote in the midgut. b- Metacyclic](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-17.jpg)
![2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system 2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-20.jpg)
![2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system 2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-21.jpg)
![3 - Meningoencephalitis stage [CNS] (Sleeping sickness stage) By end of 1 st year; 3 - Meningoencephalitis stage [CNS] (Sleeping sickness stage) By end of 1 st year;](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-22.jpg)
![Laboratory diagnosis == Card Agglutination Trypanosomiasis Test [CATT]: It is a simple & rapid Laboratory diagnosis == Card Agglutination Trypanosomiasis Test [CATT]: It is a simple & rapid](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-30.jpg)
- Slides: 33
Leishmania spp. Trypanosoma spp.
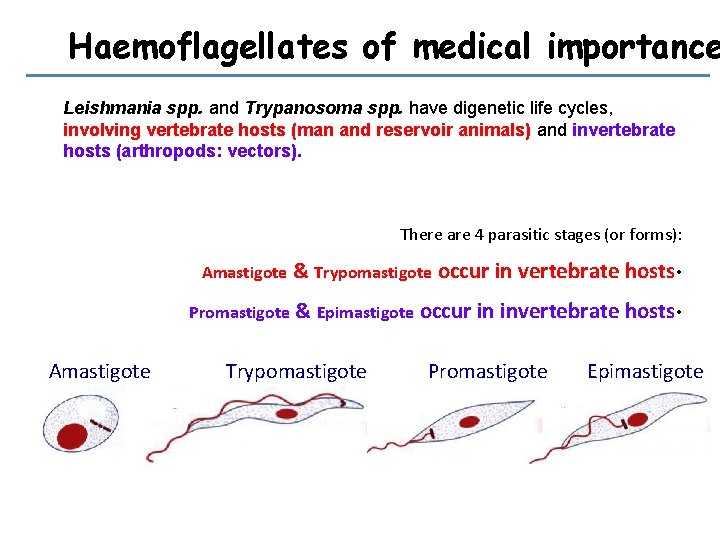
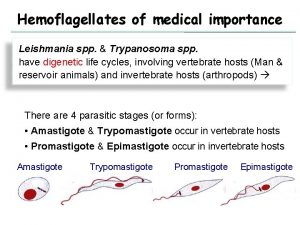
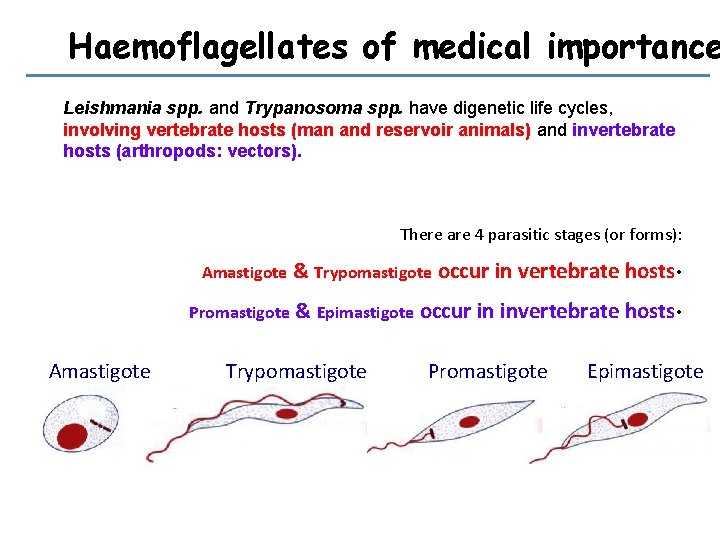
Haemoflagellates of medical importance Leishmania spp. and Trypanosoma spp. have digenetic life cycles, involving vertebrate hosts (man and reservoir animals) and invertebrate hosts (arthropods: vectors). There are 4 parasitic stages (or forms): Amastigote & Trypomastigote occur in vertebrate hosts • Promastigote & Epimastigote occur in invertebrate hosts • Amastigote Trypomastigote Promastigote Epimastigote
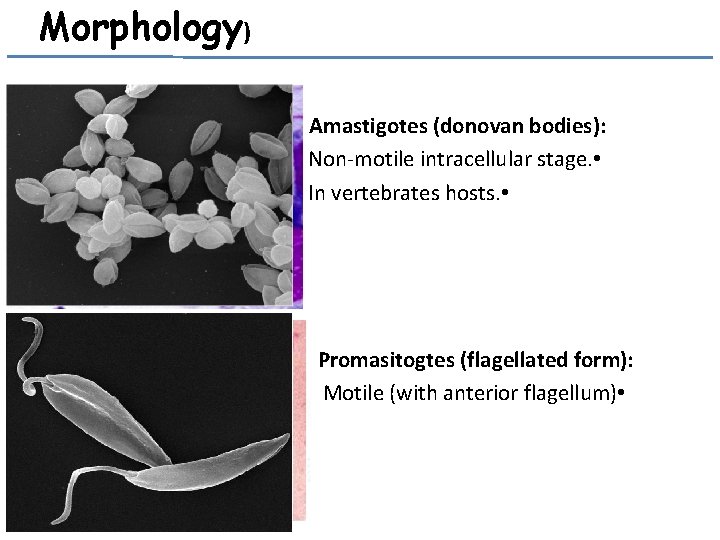
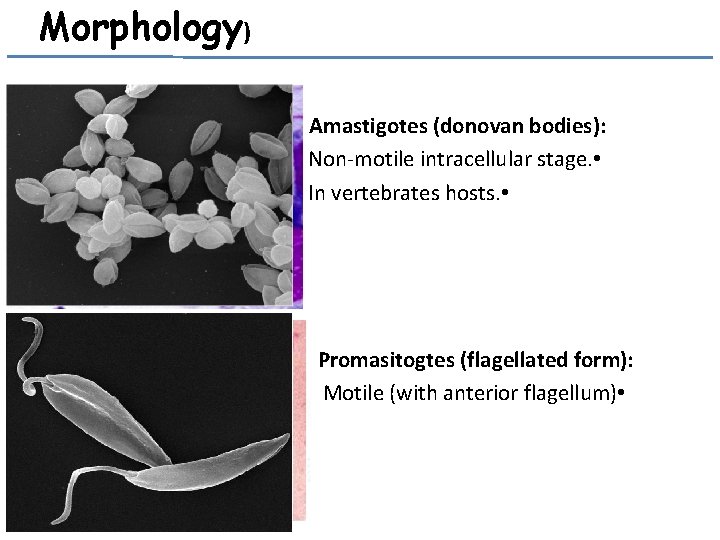
Morphology) Amastigotes (donovan bodies): Non-motile intracellular stage. • In vertebrates hosts. • Promasitogtes (flagellated form): Motile (with anterior flagellum) •
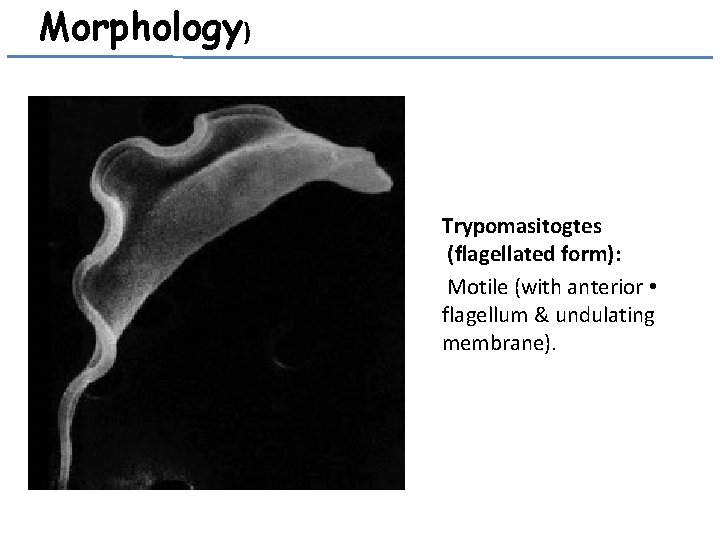
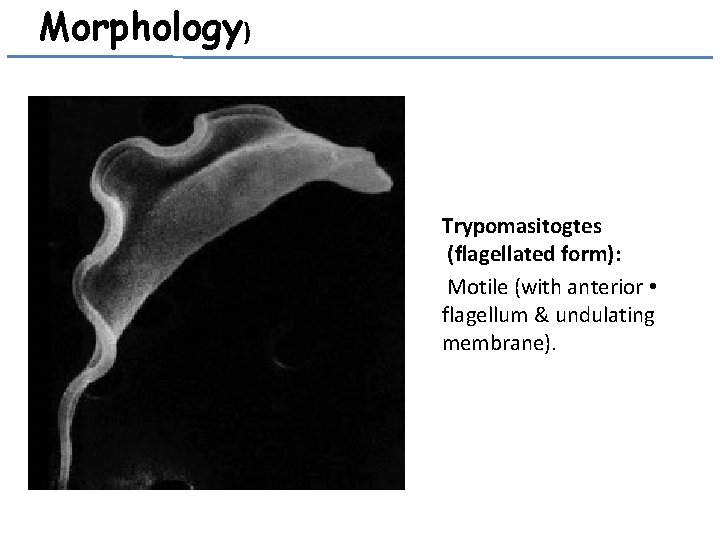
Morphology) Trypomasitogtes (flagellated form): Motile (with anterior • flagellum & undulating membrane).
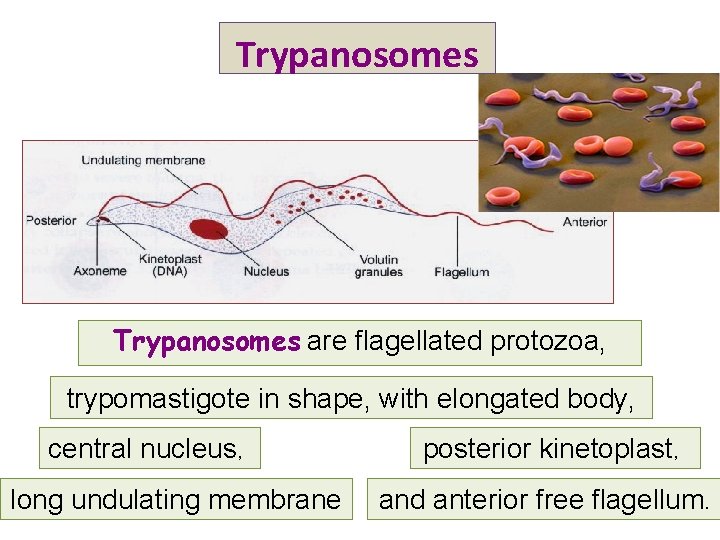
Trypanosomes are flagellated protozoa, trypomastigote in shape, with elongated body, central nucleus, long undulating membrane posterior kinetoplast, and anterior free flagellum.
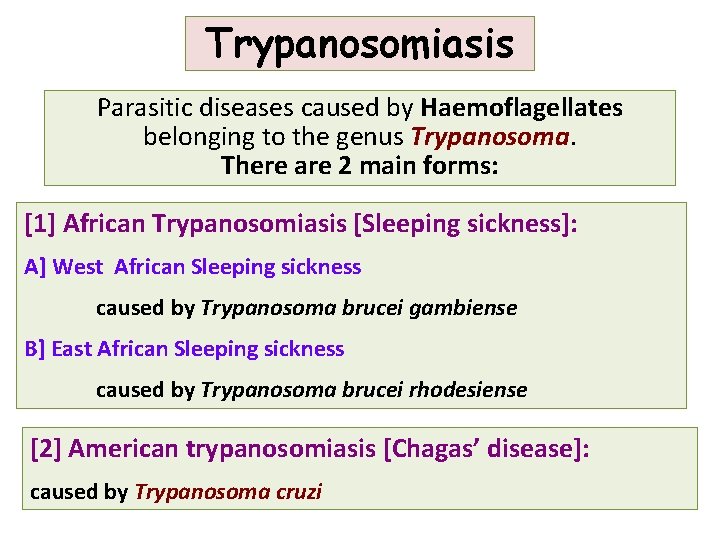
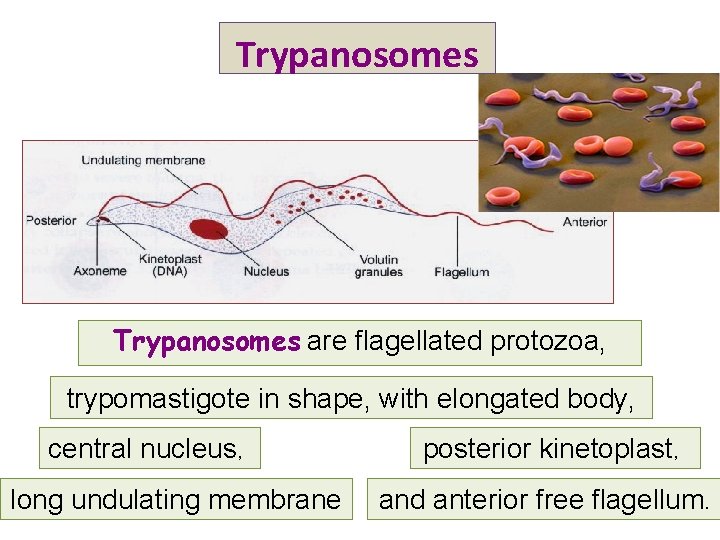
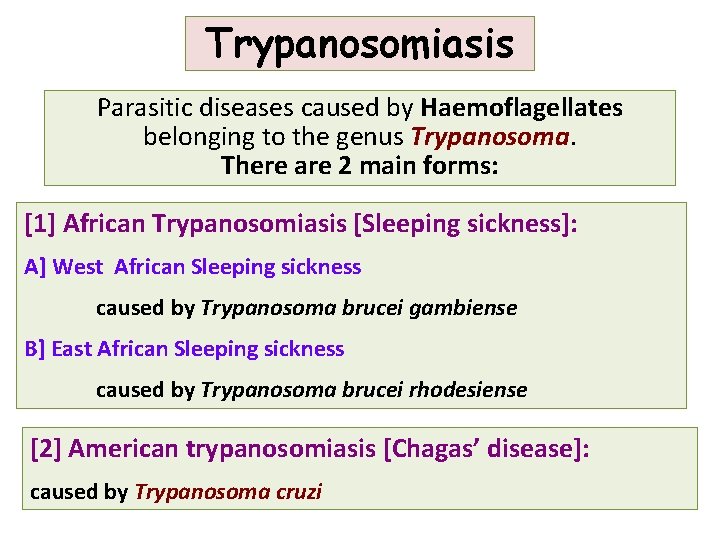
Trypanosomiasis Parasitic diseases caused by Haemoflagellates belonging to the genus Trypanosoma. There are 2 main forms: [1] African Trypanosomiasis [Sleeping sickness]: A] West African Sleeping sickness caused by Trypanosoma brucei gambiense B] East African Sleeping sickness caused by Trypanosoma brucei rhodesiense [2] American trypanosomiasis [Chagas’ disease]: caused by Trypanosoma cruzi
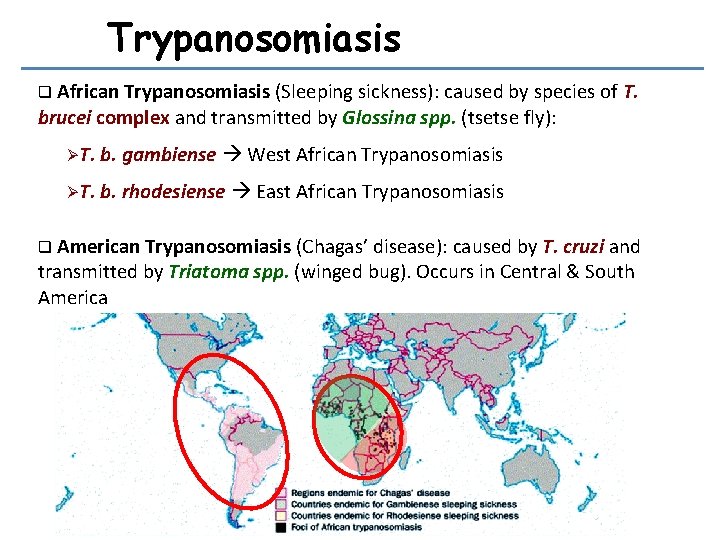
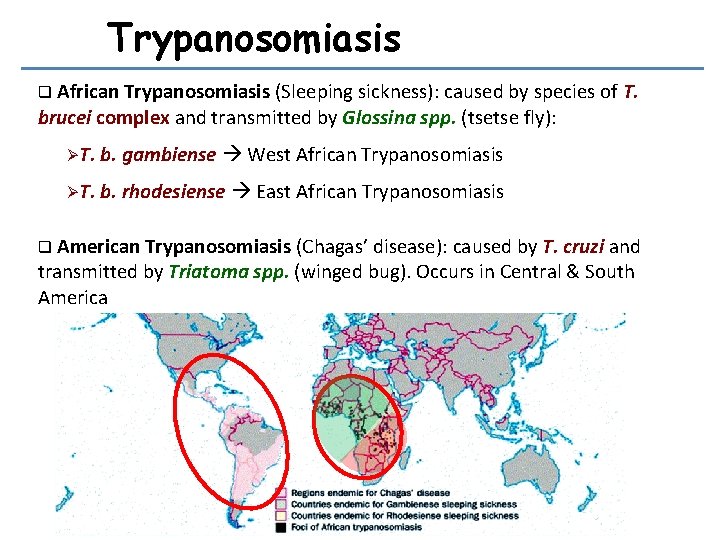
Trypanosomiasis q African Trypanosomiasis (Sleeping sickness): caused by species of T. brucei complex and transmitted by Glossina spp. (tsetse fly): ØT. b. gambiense West African Trypanosomiasis ØT. b. rhodesiense East African Trypanosomiasis q American Trypanosomiasis (Chagas’ disease): caused by T. cruzi and transmitted by Triatoma spp. (winged bug). Occurs in Central & South America
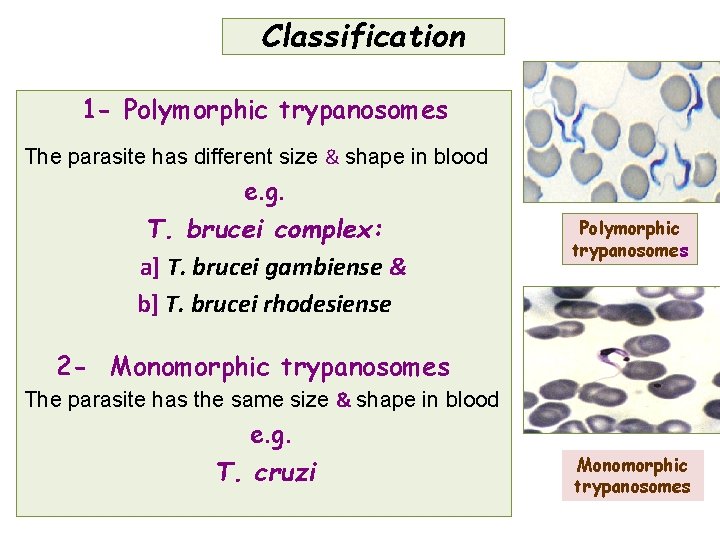
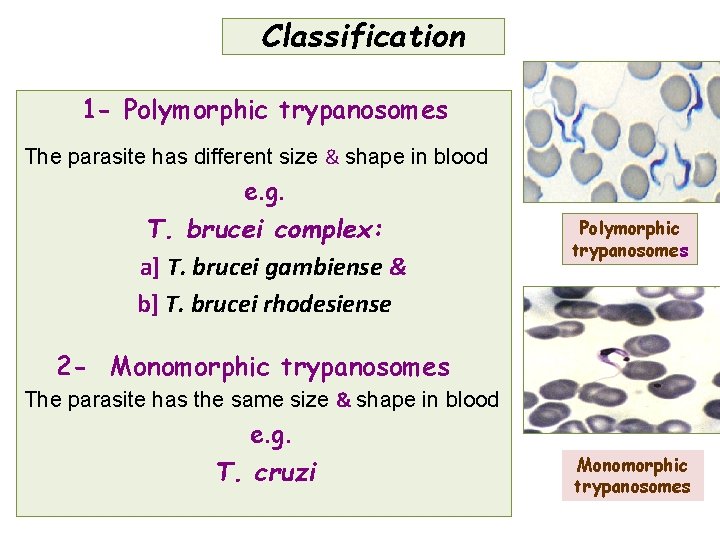
Classification 1 - Polymorphic trypanosomes The parasite has different size & shape in blood e. g. T. brucei complex: a] T. brucei gambiense & b] T. brucei rhodesiense Polymorphic trypanosomes 2 - Monomorphic trypanosomes The parasite has the same size & shape in blood e. g. T. cruzi Monomorphic trypanosomes

![Trypanosomiasis 1 African Trypanosomiasis Sleeping sickness Trypanosomiasis [1] African Trypanosomiasis [Sleeping sickness]:](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-10.jpg)
Trypanosomiasis [1] African Trypanosomiasis [Sleeping sickness]:
Tributary of Lopori River near Bongan danga in Gambian trypanosomiasisendemic area of northwestern Democratic Republic of the Congo. Note forested Tsetse flies
![1 African Trypanosomiasis Sleeping Sickness Disease Geographical distribution corresponds to that of the vector [1] African Trypanosomiasis [Sleeping Sickness Disease] Geographical distribution: corresponds to that of the vector](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-12.jpg)
[1] African Trypanosomiasis [Sleeping Sickness Disease] Geographical distribution: corresponds to that of the vector which is approximately 20° N & 20° S of the equator G. palpalis G. morsitans In West & Central Africa In East Africa Annual cases estimated in 50. 000– 70. 000:
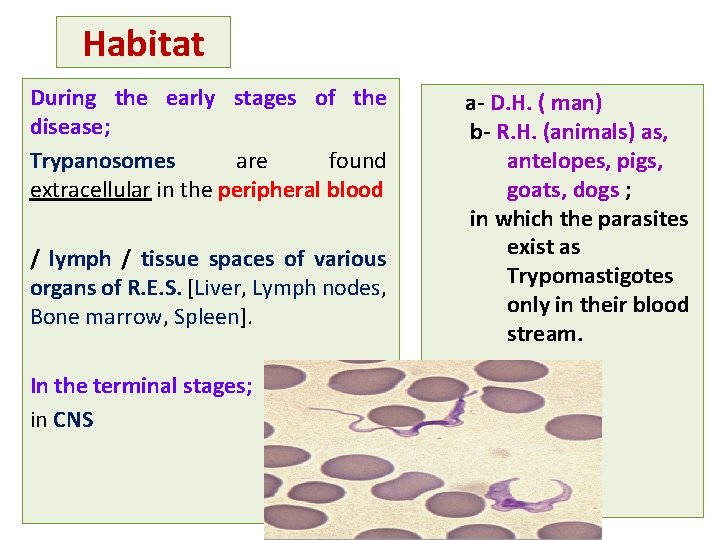
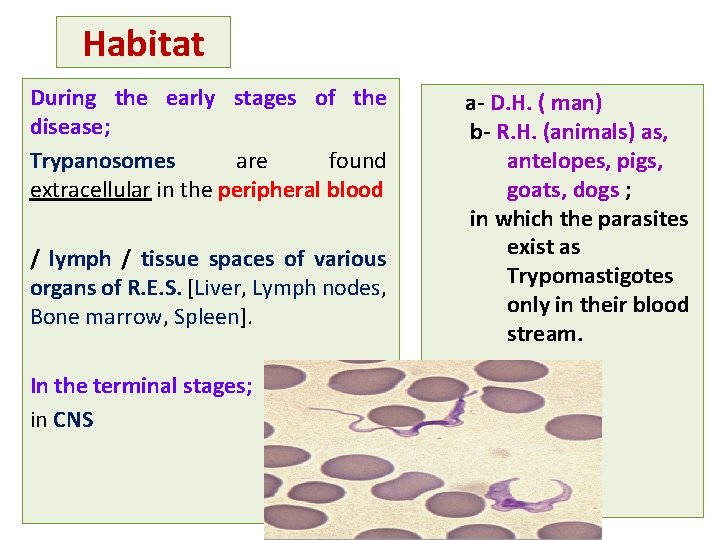
Habitat During the early stages of the disease; Trypanosomes are found extracellular in the peripheral blood / lymph / tissue spaces of various organs of R. E. S. [Liver, Lymph nodes, Bone marrow, Spleen]. In the terminal stages; in CNS a- D. H. ( man) b- R. H. (animals) as, antelopes, pigs, goats, dogs ; in which the parasites exist as Trypomastigotes only in their blood stream.
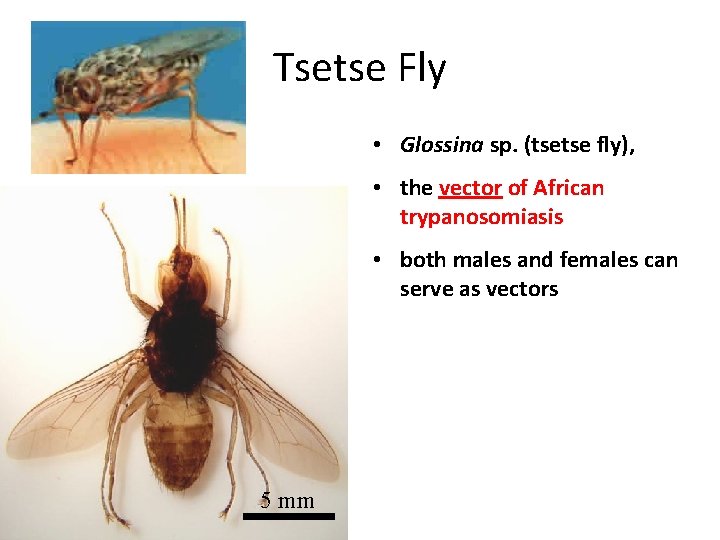
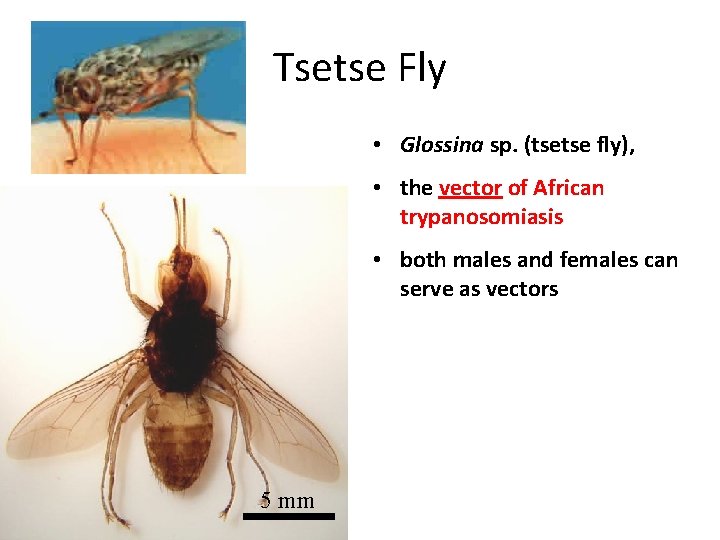
Tsetse Fly • Glossina sp. (tsetse fly), • the vector of African trypanosomiasis • both males and females can serve as vectors 5 mm
![Vector Glossina spp tse fly Transmission Cyclopropagative transmission Infective stage Metacyclic trypomastigotes Mode of Vector: Glossina spp. [tse fly], Transmission: Cyclopropagative transmission. Infective stage: Metacyclic trypomastigotes. Mode of](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-15.jpg)
Vector: Glossina spp. [tse fly], Transmission: Cyclopropagative transmission. Infective stage: Metacyclic trypomastigotes. Mode of transmission Bite of the fly : infective stages are introduced with the Saliva of infected vector; (Anterior station transmission, ) & may be transmitted by - mechanical transmission (e. g. stomoxys) - blood transfusion, - organ transplantation - congenital
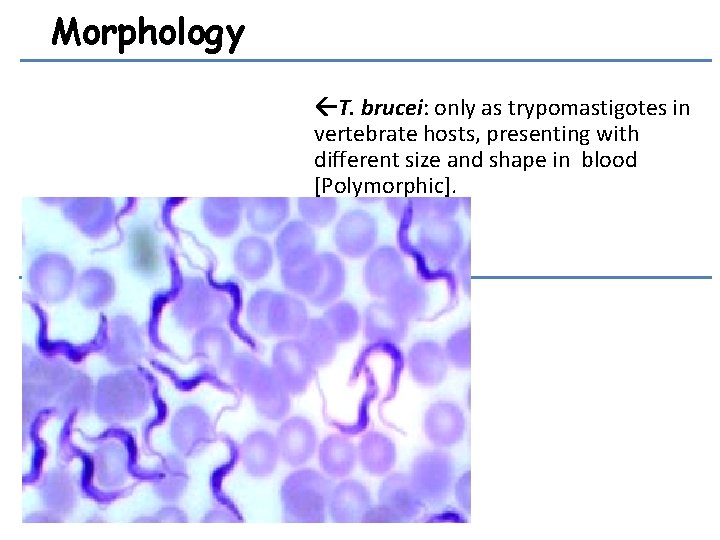
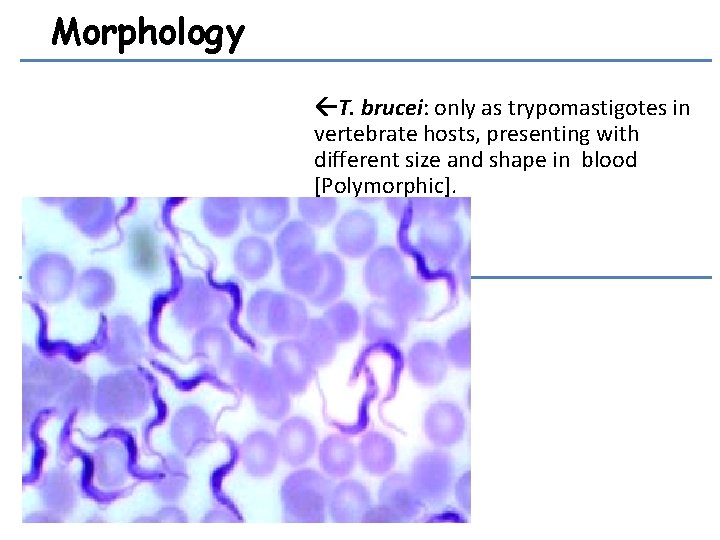
Morphology T. brucei: only as trypomastigotes in vertebrate hosts, presenting with different size and shape in blood [Polymorphic].
![Morphology Cont 2 in the vector a Epimastigote in the midgut b Metacyclic Morphology [Cont. ] 2. in the vector a- Epimastigote in the midgut. b- Metacyclic](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-17.jpg)
Morphology [Cont. ] 2. in the vector a- Epimastigote in the midgut. b- Metacyclic or short stumpy trypanosomes (infective stage) in salivary gland.
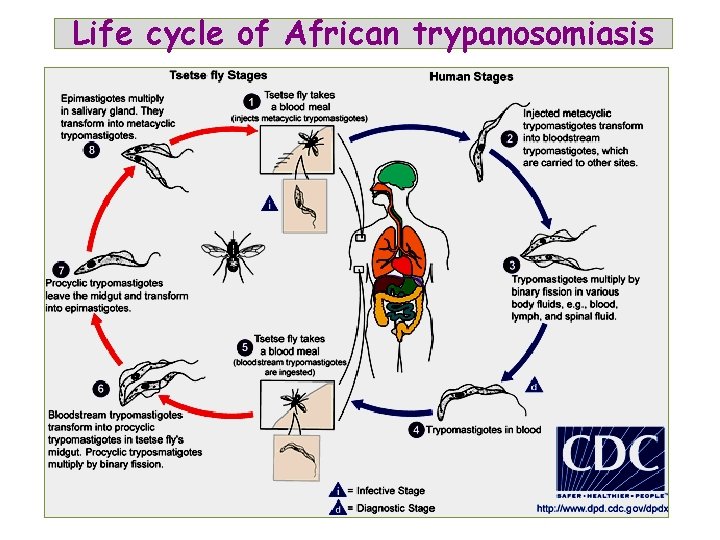
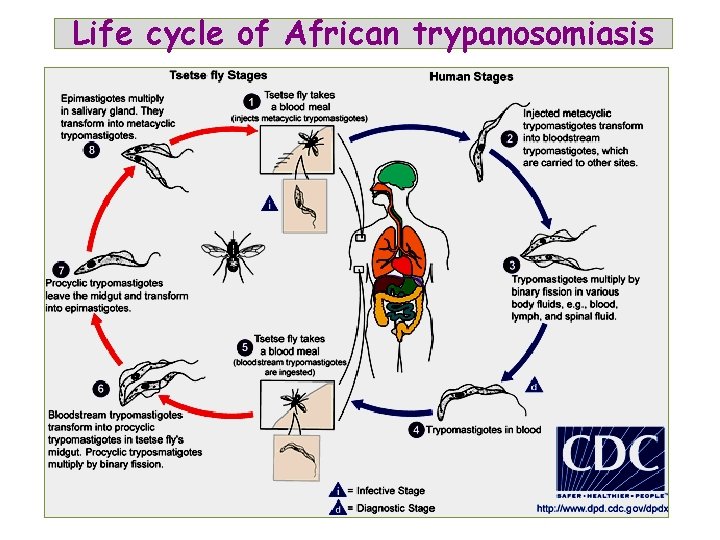
Life cycle of African trypanosomiasis
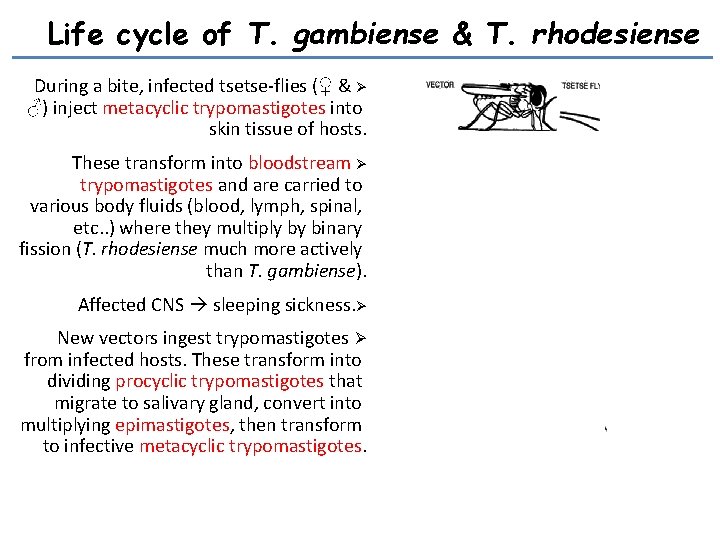
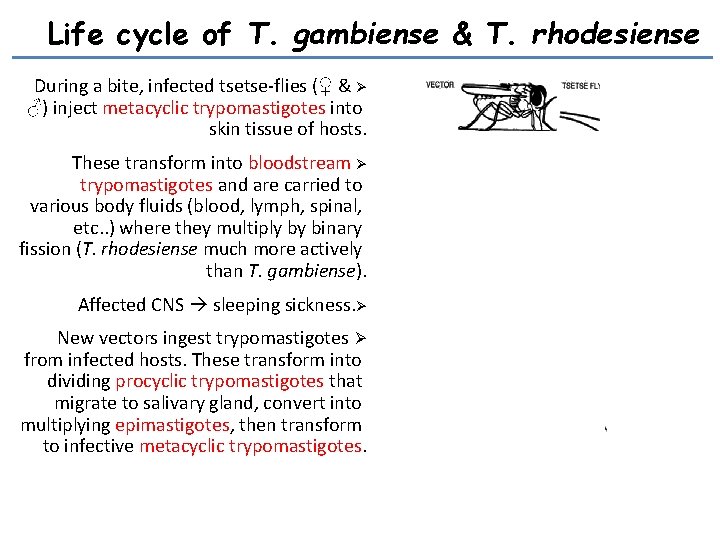
Life cycle of T. gambiense & T. rhodesiense During a bite, infected tsetse-flies (♀ & Ø ♂) inject metacyclic trypomastigotes into skin tissue of hosts. These transform into bloodstream Ø trypomastigotes and are carried to various body fluids (blood, lymph, spinal, etc. . ) where they multiply by binary fission (T. rhodesiense much more actively than T. gambiense). Affected CNS sleeping sickness. Ø New vectors ingest trypomastigotes Ø from infected hosts. These transform into dividing procyclic trypomastigotes that migrate to salivary gland, convert into multiplying epimastigotes, then transform to infective metacyclic trypomastigotes.
![2 Haemolymphatic stage Blood Lymph nodes Trypomastigotes invade blood lymphatic system 2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-20.jpg)
2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system and multiply producing >>> Toxic manifestations & Lymphocytic hyperplasia. Enlarged liver & spleen, lymphadenopathy especially triangle of neck >>> in “Winter bottom sign” posterior
![2 Haemolymphatic stage Blood Lymph nodes Trypomastigotes invade blood lymphatic system 2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-21.jpg)
2 - Haemolymphatic stage [Blood & Lymph nodes] Trypomastigotes invade blood & lymphatic system and multiply producing >>> Toxic manifestations: Patient gets irregular fever, headache, joint & muscle pain and rash. Bone Marrow affection: Anaemia [Hypoplastic anaemia], Leucopenia & Thrombocytopenia.
![3 Meningoencephalitis stage CNS Sleeping sickness stage By end of 1 st year 3 - Meningoencephalitis stage [CNS] (Sleeping sickness stage) By end of 1 st year;](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-22.jpg)
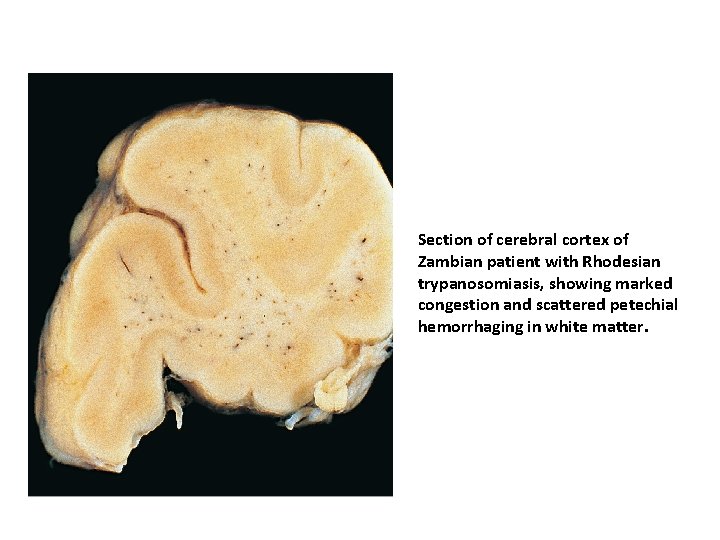
3 - Meningoencephalitis stage [CNS] (Sleeping sickness stage) By end of 1 st year; Trypomastigotes invade CNS >> perivascular infiltration of cerebral vessel with chronic inflammatory cells >> ischaemia & haemorrhage >> Meningoencephalitis & Meningomyelitis. Patient suffers of: Severe headache, mental apathy, slow speech, tremors, involuntary movements & convulsions. Sleeping stage develops >> Coma & death [from the disease or from intercurrent infections as pneumonia]. Coma before death
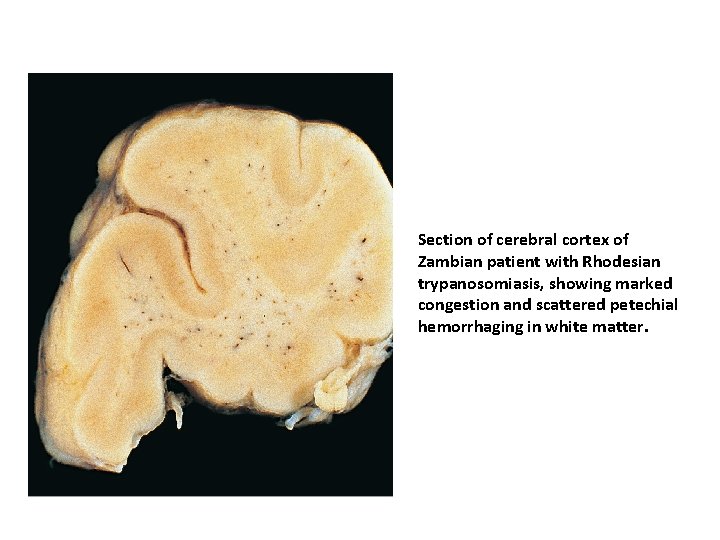
Section of cerebral cortex of Zambian patient with Rhodesian trypanosomiasis, showing marked congestion and scattered petechial hemorrhaging in white matter.
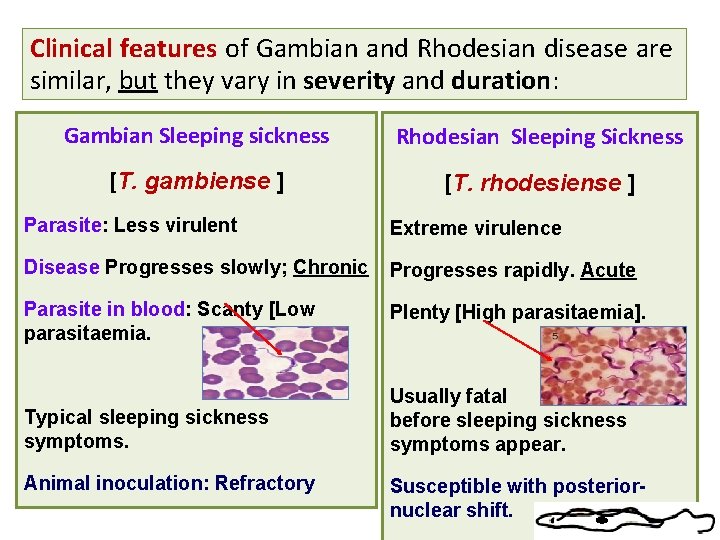
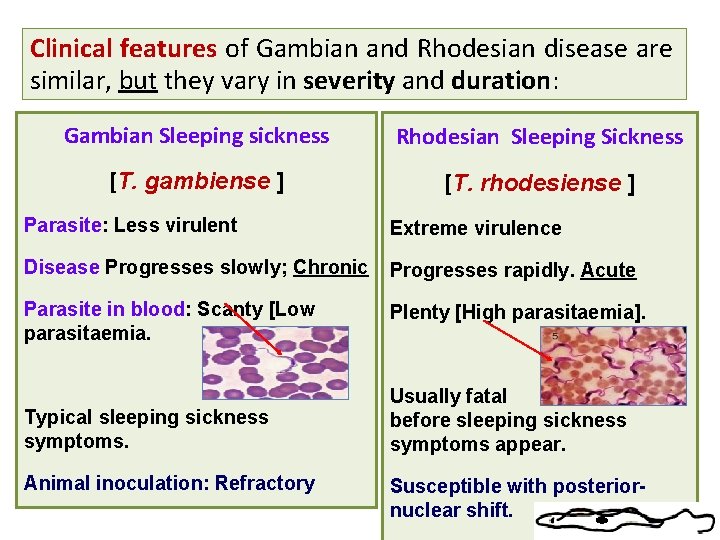
Clinical features of Gambian and Rhodesian disease are similar, but they vary in severity and duration: Gambian Sleeping sickness Rhodesian Sleeping Sickness [T. gambiense ] [T. rhodesiense ] Parasite: Less virulent Extreme virulence Disease Progresses slowly; Chronic Progresses rapidly. Acute Parasite in blood: Scanty [Low parasitaemia. Plenty [High parasitaemia]. Typical sleeping sickness symptoms. Usually fatal before sleeping sickness symptoms appear. Animal inoculation: Refractory Susceptible with posteriornuclear shift.
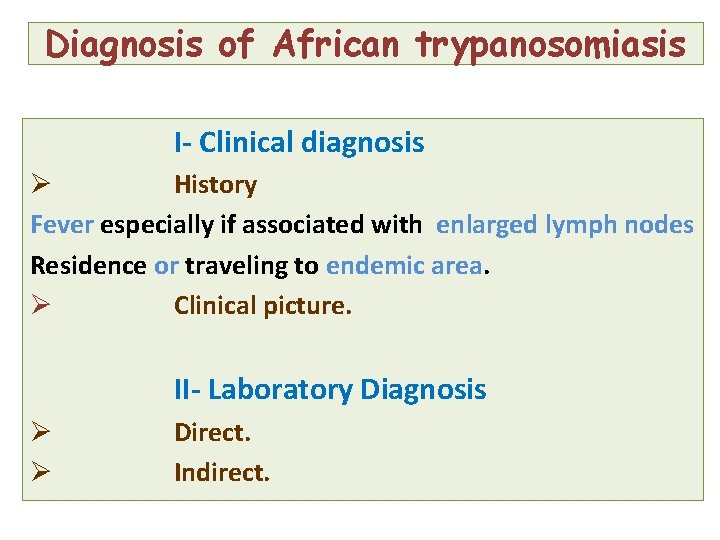
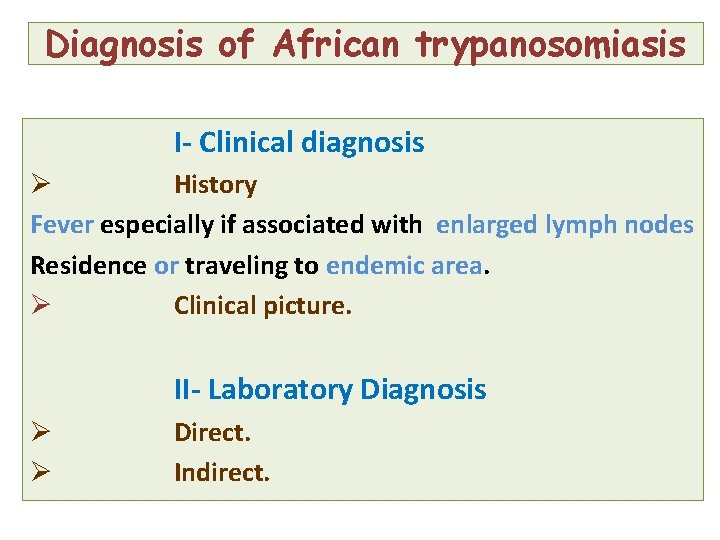
Diagnosis of African trypanosomiasis I- Clinical diagnosis Ø History Fever especially if associated with enlarged lymph nodes Residence or traveling to endemic area. Ø Clinical picture. II- Laboratory Diagnosis Ø Ø Direct. Indirect.
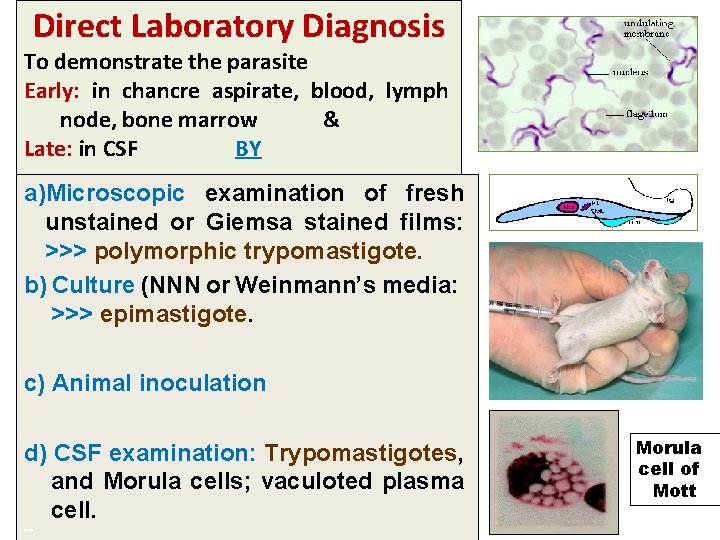
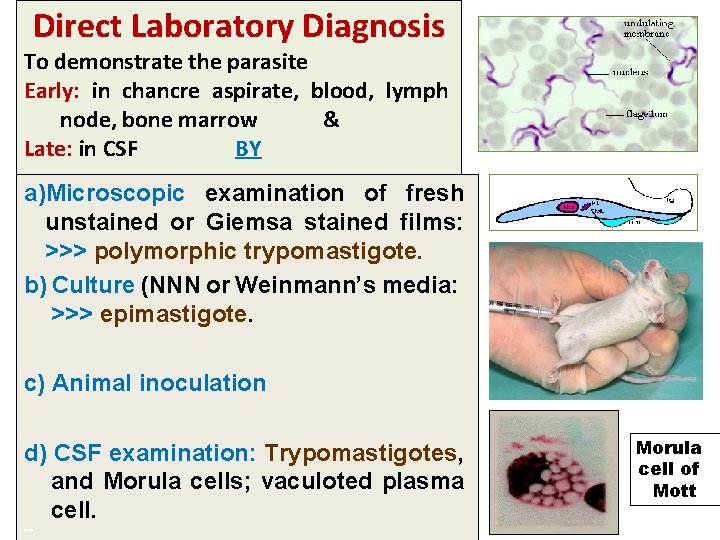
Direct Laboratory Diagnosis To demonstrate the parasite Early: in chancre aspirate, blood, lymph node, bone marrow & Late: in CSF BY a)Microscopic examination of fresh unstained or Giemsa stained films: >>> polymorphic trypomastigote. b) Culture (NNN or Weinmann’s media: >>> epimastigote. c) Animal inoculation d) CSF examination: Trypomastigotes, and Morula cells; vaculoted plasma cell. == Morula cell of Mott
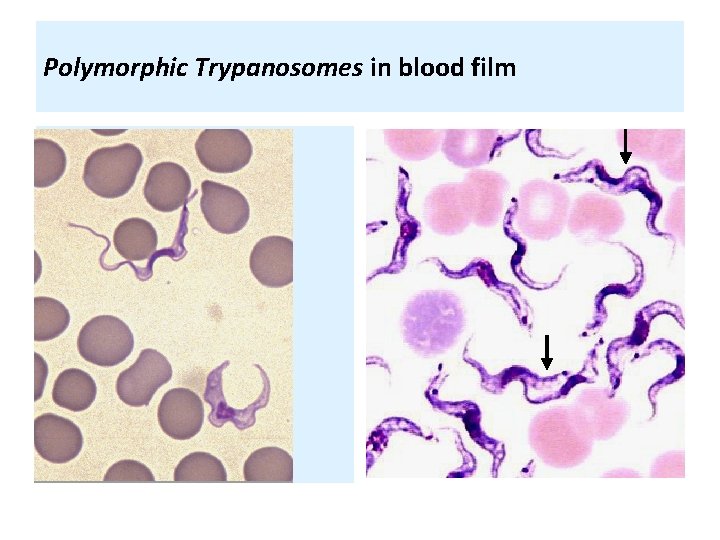
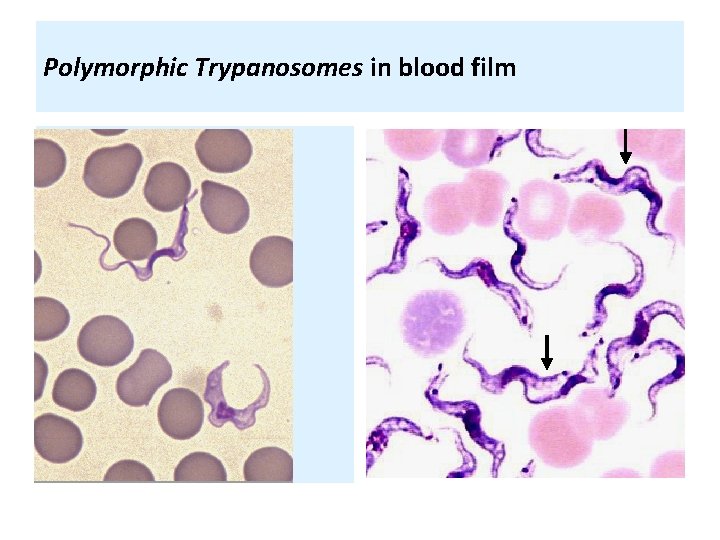
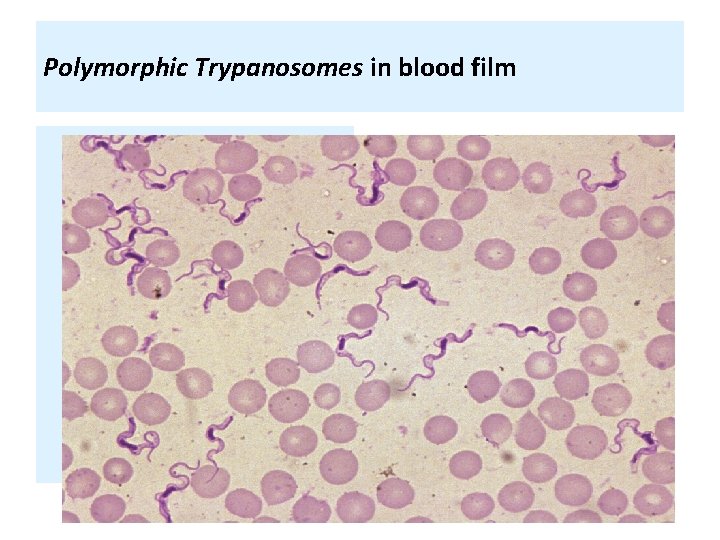
Polymorphic Trypanosomes in blood film
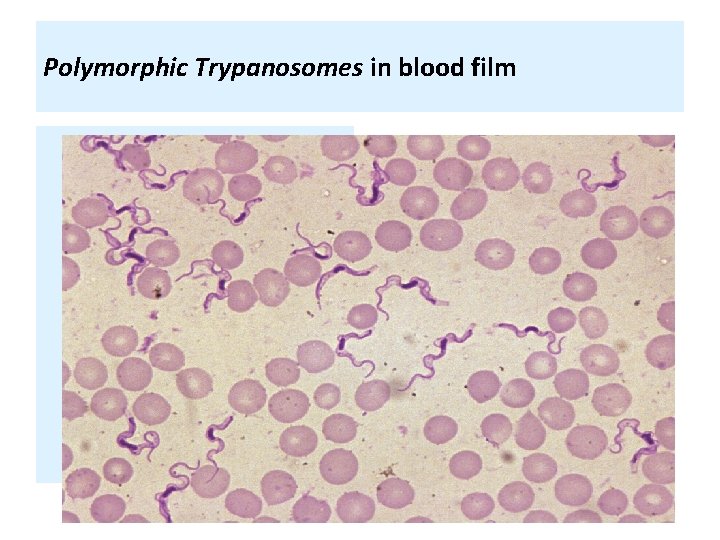
Polymorphic Trypanosomes in blood film
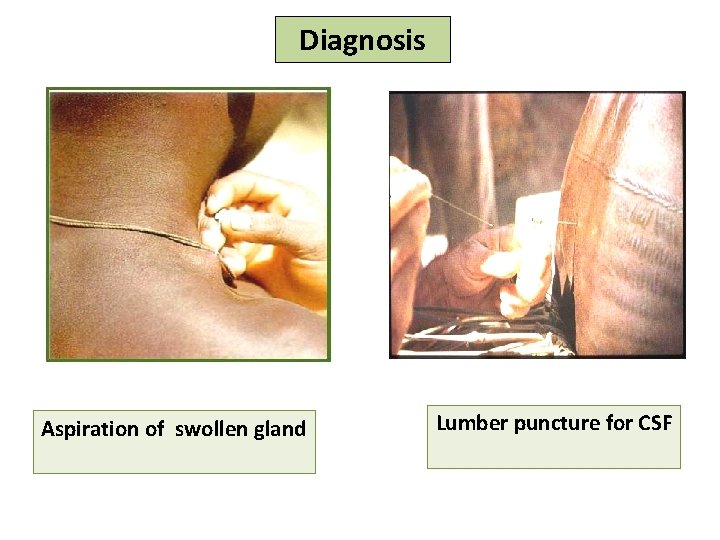
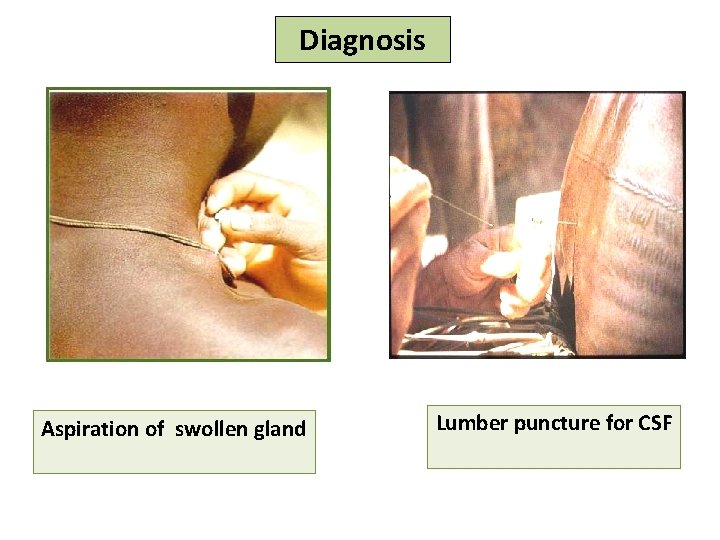
Diagnosis Aspiration of swollen gland Lumber puncture for CSF
![Laboratory diagnosis Card Agglutination Trypanosomiasis Test CATT It is a simple rapid Laboratory diagnosis == Card Agglutination Trypanosomiasis Test [CATT]: It is a simple & rapid](https://slidetodoc.com/presentation_image_h2/905c9206f4d09df984f11b98967ed5cf/image-30.jpg)
Laboratory diagnosis == Card Agglutination Trypanosomiasis Test [CATT]: It is a simple & rapid test for detection of circulating antigens in the blood of the patient. It is useful in surveys specially for T. b. gambiense. Other methods: Molecular techniques (e. g. PCR).
Indirect Laboratory diagnosis == Detecting anti-Trypanosoma Abs by serological methods (ELISA, IFA, IHA etc. . ), But can't distinguish between current and previous infections.
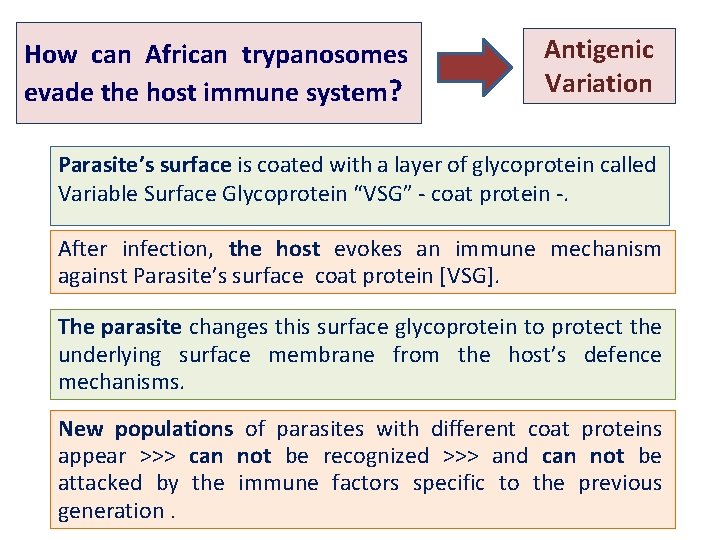
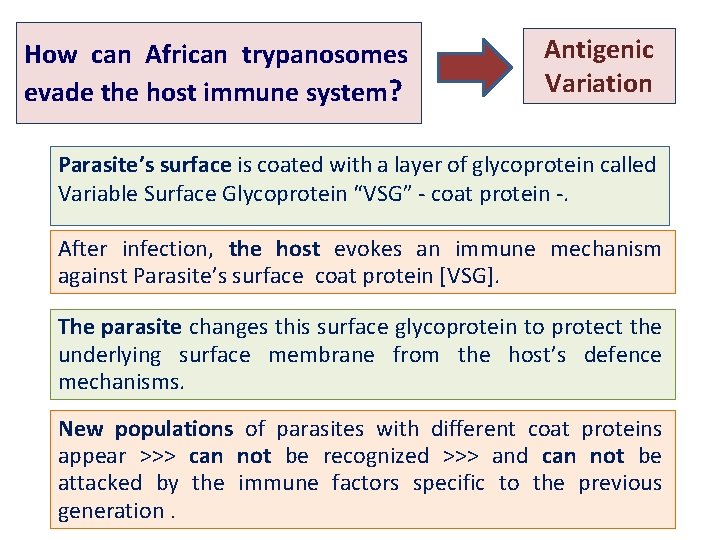
How can African trypanosomes evade the host immune system? Antigenic Variation Parasite’s surface is coated with a layer of glycoprotein called Variable Surface Glycoprotein “VSG” - coat protein -. After infection, the host evokes an immune mechanism against Parasite’s surface coat protein [VSG]. The parasite changes this surface glycoprotein to protect the underlying surface membrane from the host’s defence mechanisms. New populations of parasites with different coat proteins appear >>> can not be recognized >>> and can not be attacked by the immune factors specific to the previous generation.
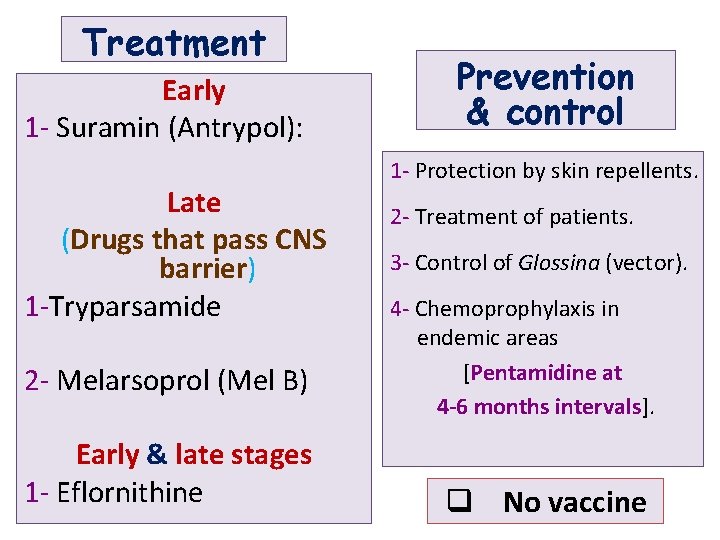
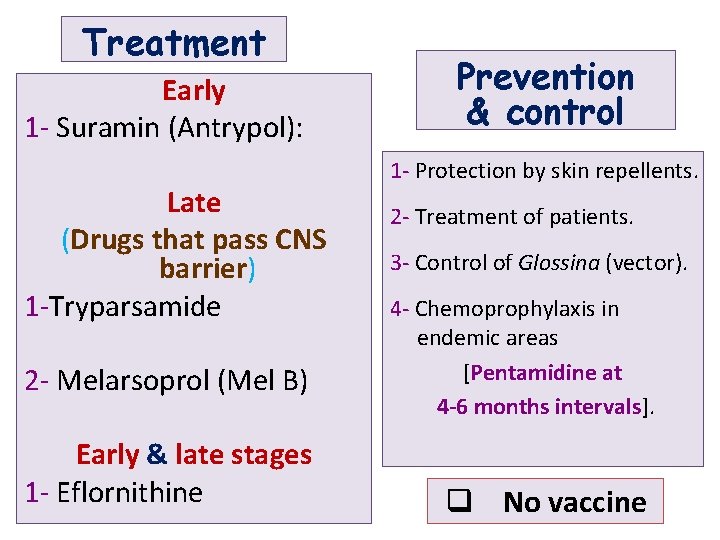
Treatment Early 1 - Suramin (Antrypol): Late (Drugs that pass CNS barrier) 1 -Tryparsamide 2 - Melarsoprol (Mel B) Early & late stages 1 - Eflornithine Prevention & control 1 - Protection by skin repellents. 2 - Treatment of patients. 3 - Control of Glossina (vector). 4 - Chemoprophylaxis in endemic areas [Pentamidine at 4 -6 months intervals]. q No vaccine
 цилиатура
цилиатура Trypanosomaiasis
Trypanosomaiasis Mosquito-palha
Mosquito-palha Salmolenose
Salmolenose Leishmania
Leishmania Leishmania
Leishmania Tricomonase vaginalis
Tricomonase vaginalis Parasita
Parasita Leishmania disease
Leishmania disease Leishmania disease
Leishmania disease Promastigote
Promastigote Morfologi leishmania donovani
Morfologi leishmania donovani Chagas
Chagas Trypanosoma cruzi filo
Trypanosoma cruzi filo Trypanosoma
Trypanosoma Thin and thick smear
Thin and thick smear Thick and thin malaria smear
Thick and thin malaria smear Trypanosoma cruzi
Trypanosoma cruzi Etimologia zoo
Etimologia zoo 5 characteristics of protozoa
5 characteristics of protozoa Trypanosoma cruzi genus
Trypanosoma cruzi genus Trypomastigote form
Trypomastigote form Medical
Medical Trypanosoma cruzi
Trypanosoma cruzi Peranan sporozoa
Peranan sporozoa P.ovale
P.ovale Chagoma
Chagoma Tripanosoma cruci
Tripanosoma cruci Prevanece
Prevanece Trypanosoma vivax ciclo de vida
Trypanosoma vivax ciclo de vida Hypermastigida
Hypermastigida Blepharoblast
Blepharoblast L
L Trypanosoma
Trypanosoma