Knee posterolateral corner structure damage Management Case report












- Slides: 56
Knee posterolateral corner structure damage. Management. Case report. K. Bliznikas, M. Šakalinis, A. Pocius, M. Liubauskas Klaipėda 2013. 09. 27
Epidemiology Injuries of the posterolateral (PLC) structures are relatively rare and often associated with cruciate ligament injuries. (1), (2), (3) In our literature review, out of 84 cases we found: Male 67, Female 17 Age 15 -55 y. o. (~25) Time from trauma until OP 1 -120 month (usualy 5 -6 month) (1) Johan von Heideken „Acute Injuries to the Posterolateral Corner of the Knee in Children“ (2) Shin Miyatake „Biomechanical Comparisons Between 4 -Strand Modified Larson 2 -Strand Procedures for Reconstruction of the Posterolateral Corner of the Knee“ (3) Kyoung Ho Yoon „Comparison of Clinical Results of Anatomic Posterolateral Corner Reconstruction for Posterolateral Rotatory Instability of the Knee With or Without Popliteal Tendon Reconstruction“
Causes High energy trauma: Car accidents Fall from height Sports trauma (contact sport, extreme sports, . . . ) Skiing or snowboarding etc.
Classification (grades) • I minimal tearing • II partial tearing • III complete tearing
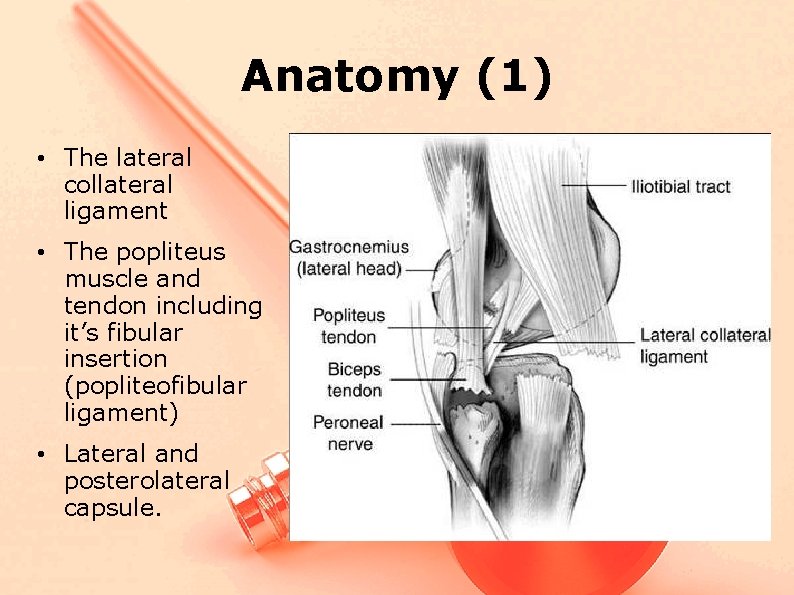
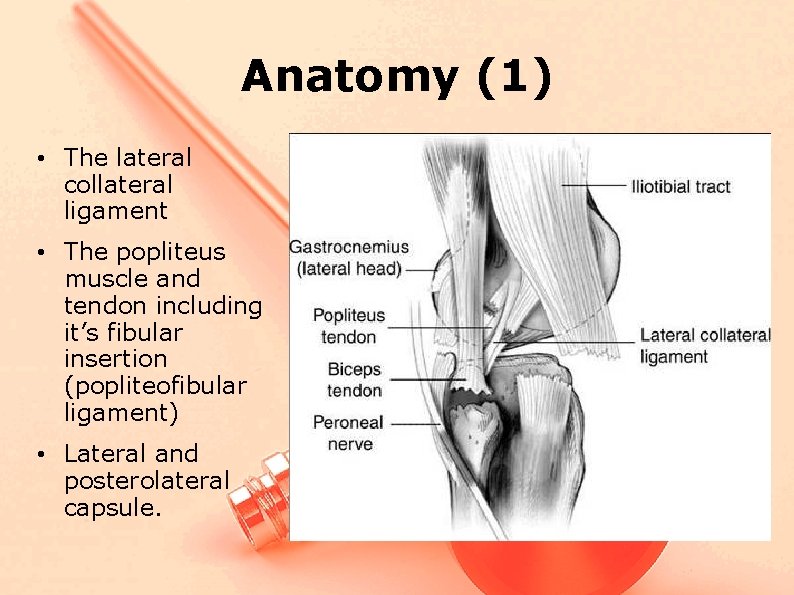
Anatomy (1) • The lateral collateral ligament • The popliteus muscle and tendon including it’s fibular insertion (popliteofibular ligament) • Lateral and posterolateral capsule.
Anatomy (2) Main functions – LCL resist lateral joint opening, varus angulation – PLC & PFL resist posterior subluxation of the lateral tibial plateau with tibial external rotation – resist knee hyperextension (1), (2) (1) Shin Miyatake „Biomechanical Comparisons Between 4 -Strand Modified Larson 2 -Strand Procedures for Reconstruction of the Posterolateral Corner of the Knee“ (2) Gollehon“The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am. 1987; 69: 233 -242“
Mechanism of injury • A direct blow to the anteromedial proximal tibia. (1) • External rotation hyperextension injury. (2) (1) De. Lee JC, Riley MB, Rockwood CA. Acute posterolateral rotatory instability of the knee. Am J Sports Med 1983; 11: 199– 20 (2) Baker CL, Norwood LA, Hughston JC. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am 1983; 65: 614– 618
Physical examination ● Varus angulation laxity ● External rotation laxity ● The dial test, or posterolateral rotation test (1) Larsen MW, Toth A. Examination of posterolateral corner injuries. J Knee Surg 2005; 28: 146– 150
Why we need to talk about this? • Difficult diagnosis and complicate treatment • It can cause significant disability due to instability, cartilage degeneration • It contributes to ACL graft failure!!! (1), (2) (1) Kyoung Ho Yoon „Comparison of Clinical Results of Anatomic Posterolateral Corner Reconstruction for Posterolateral Rotatory Instability of the Knee With or Without Popliteal Tendon Reconstruction“ (2) La. Prade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force: a biomechanical analysis. Am J Sports Med 1999; 27: 469– 475
Treatment • Grade I and II injuries are often treated with rehabilitation and observation (1) • In patients with laxity, corresponding to grade III injuries, most authors advocate either repair or reconstruction of the posterolateral corner in the setting of acute or chronic posterolateral instability (2) (1) Fanelli GC. Surgical reconstruction for acute posterolateral injury of the knee. J Knee Surg 2005; 28: 157– 162 (2) Fanelli GC. Surgical reconstruction for acute posterolateral injury of the knee. J Knee Surg 2005; 28: 157– 162
Surgical treatment methods Operative treatment methods for posterolateral instability have not been standardized, with many reconstruction techniques reporting varying results (1) It has been reported, that the results of anatomical reconstruction is better than non-anatomical (2) (1) Kyoung Ho Yoon „Comparison of Clinical Results of Anatomic Posterolateral Corner Reconstruction for Posterolateral Rotatory Instability of the Knee With or Without Popliteal Tendon Reconstruction“ (2) Noyes FR, Barber-Westin SD. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996; 24: 415 -426

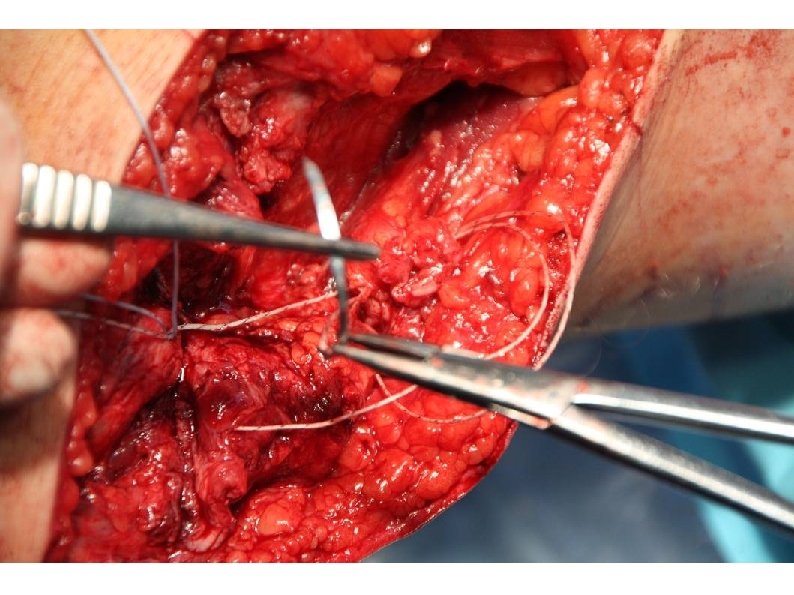
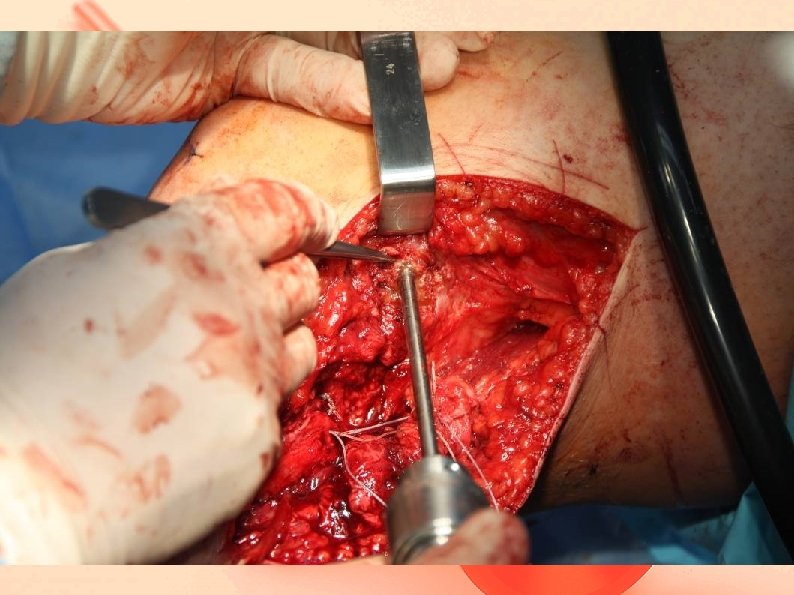
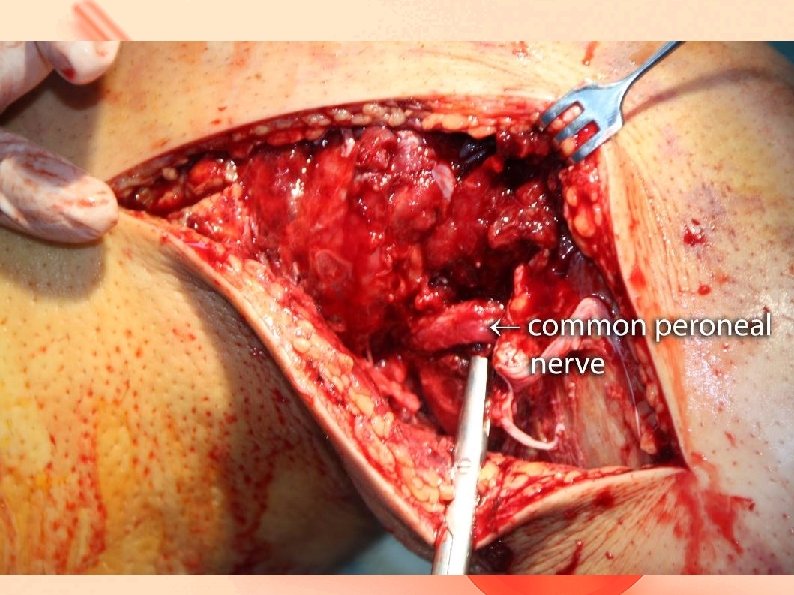
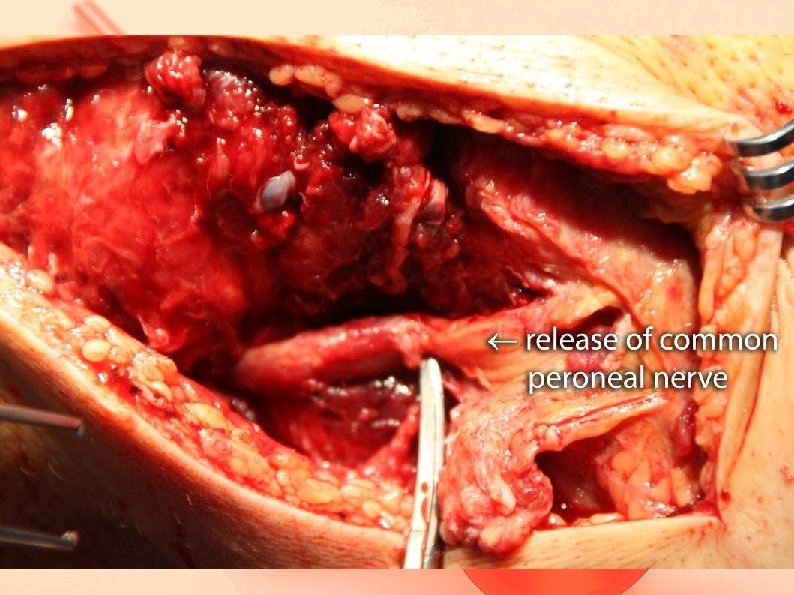
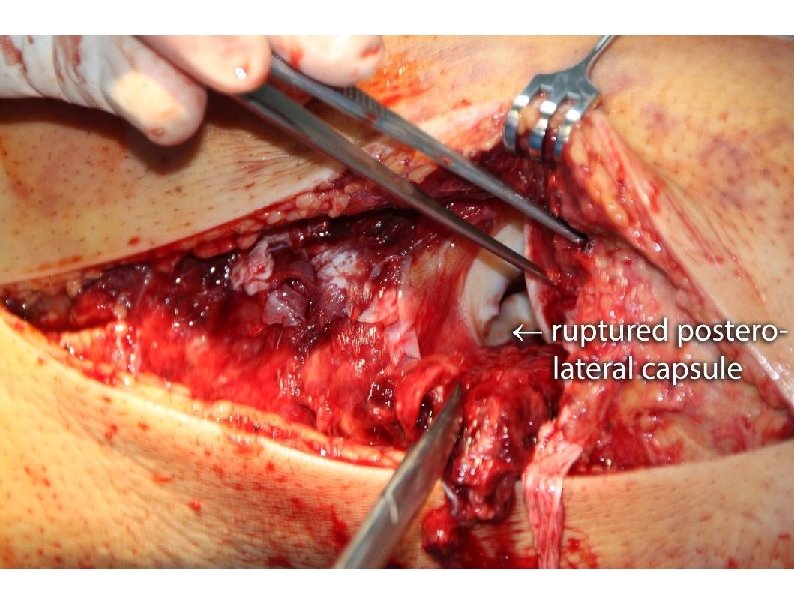
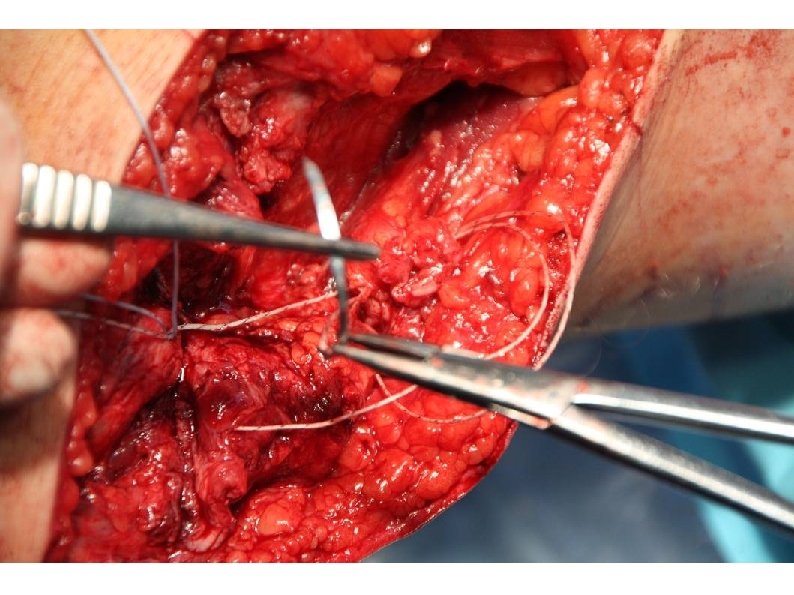
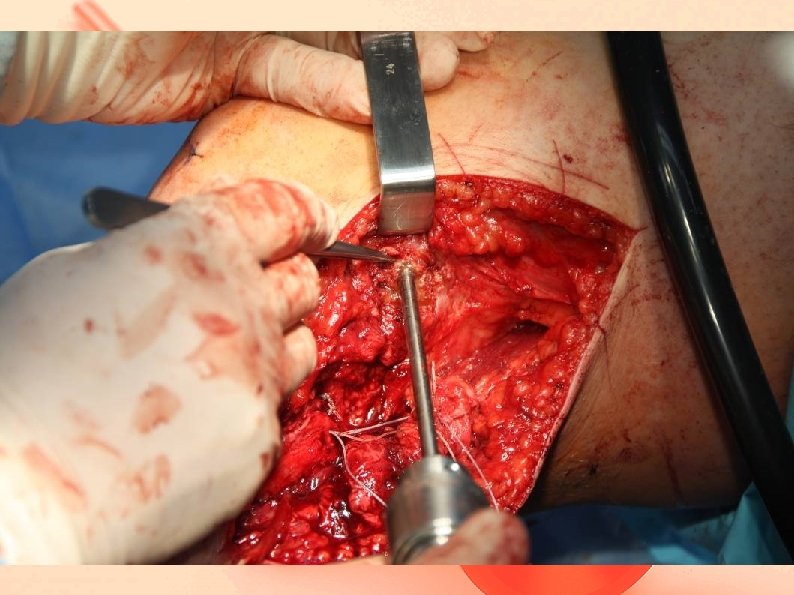
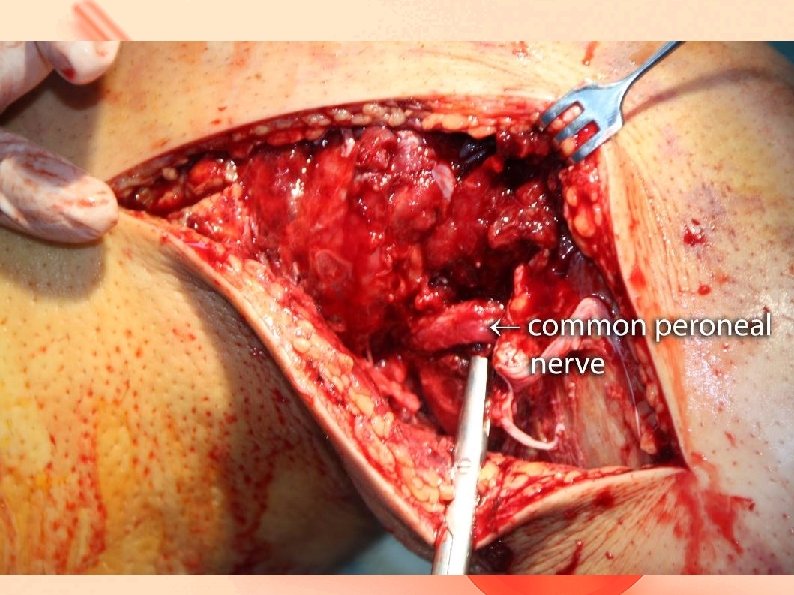
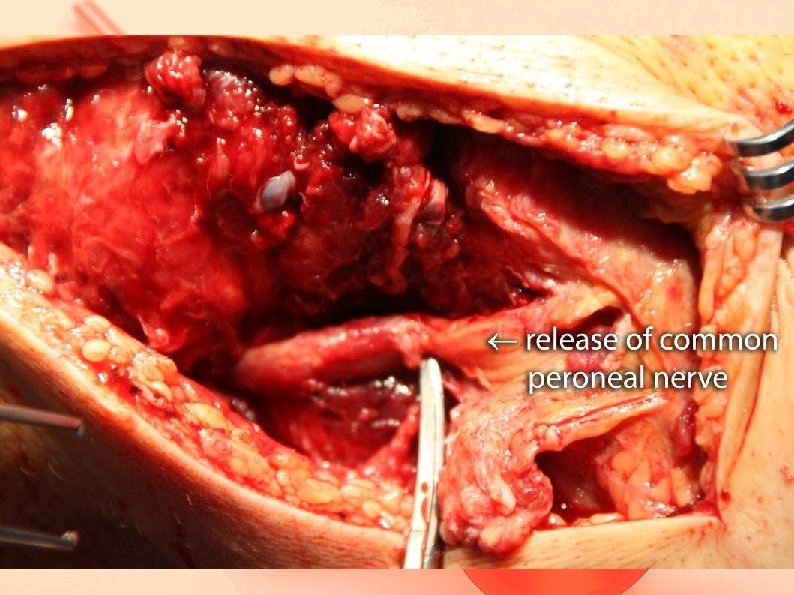
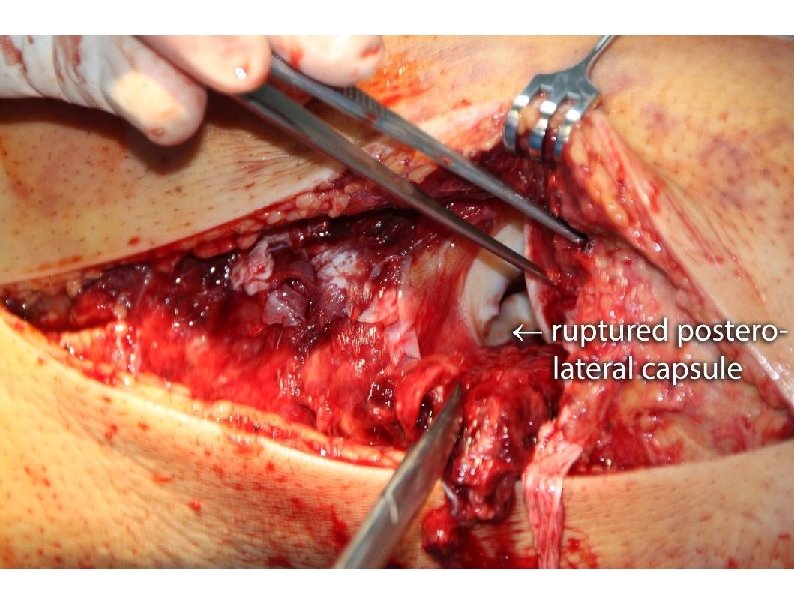
Goals of our operations - Complete anatomical structure reconstruction/ suture - CPN revision and decompression - Lesser operation trauma, single stage rec. - Adequate rehabilitation
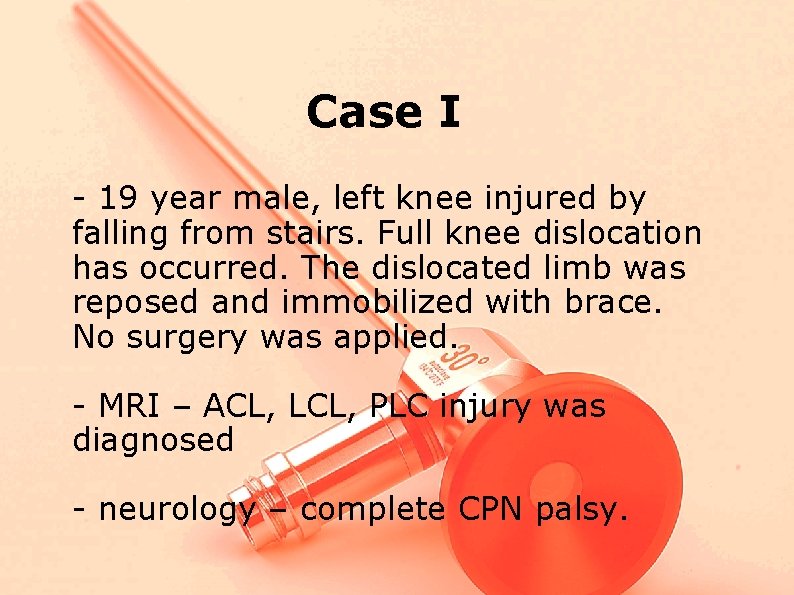
Case I - 19 year male, left knee injured by falling from stairs. Full knee dislocation has occurred. The dislocated limb was reposed and immobilized with brace. No surgery was applied. - MRI – ACL, LCL, PLC injury was diagnosed - neurology – complete CPN palsy.
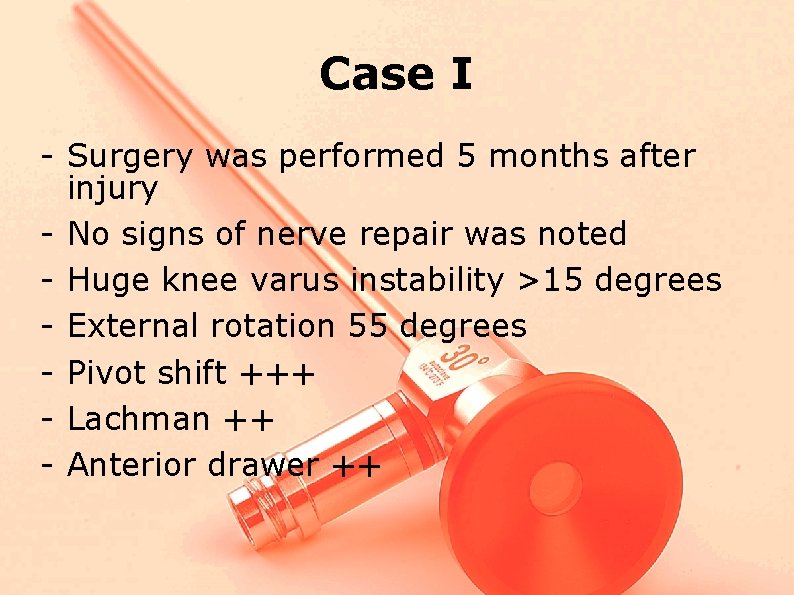
Case I - Surgery was performed 5 months after injury - No signs of nerve repair was noted - Huge knee varus instability >15 degrees - External rotation 55 degrees - Pivot shift +++ - Lachman ++ - Anterior drawer ++
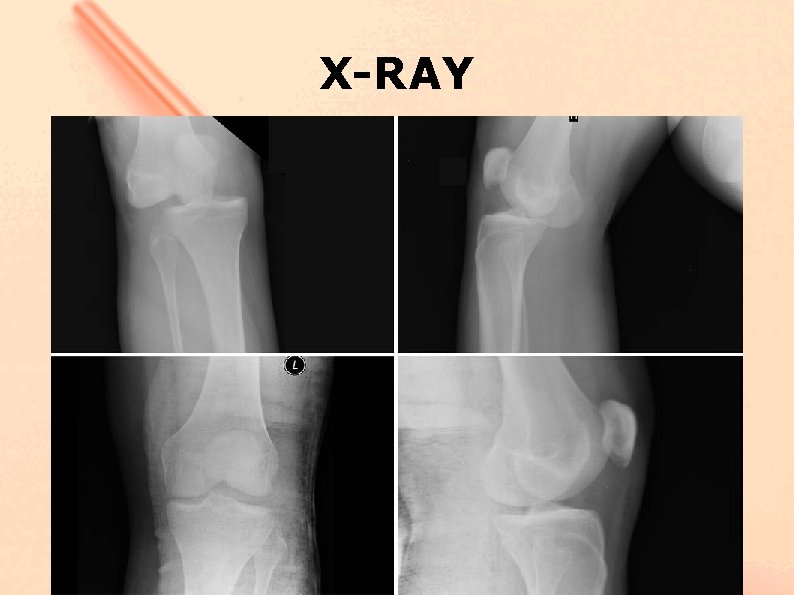
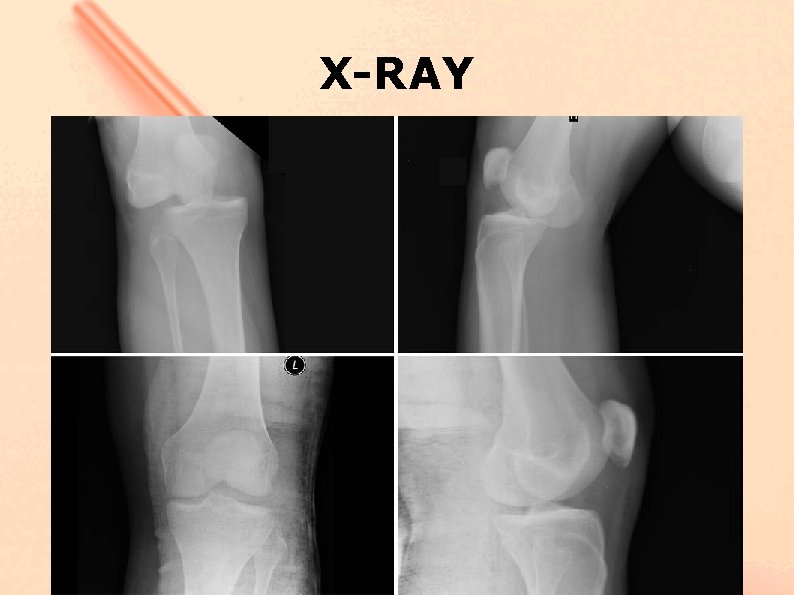
X-RAY
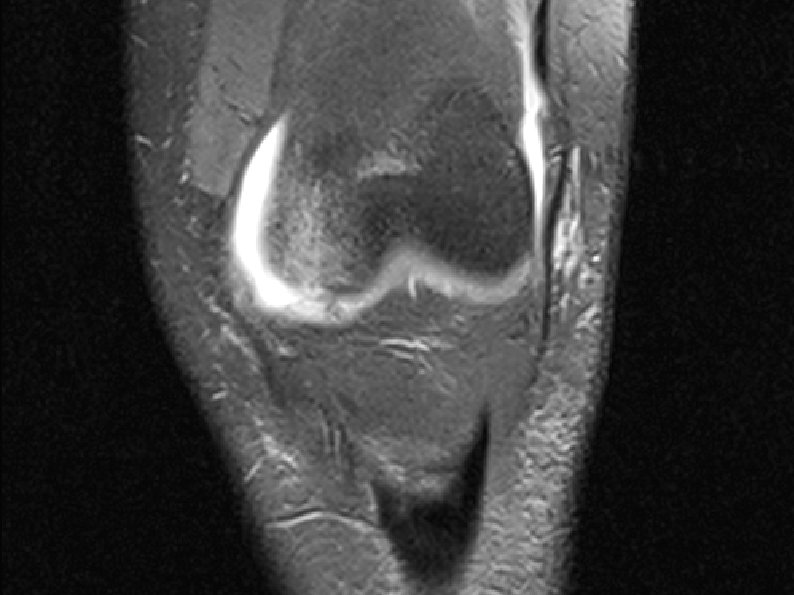
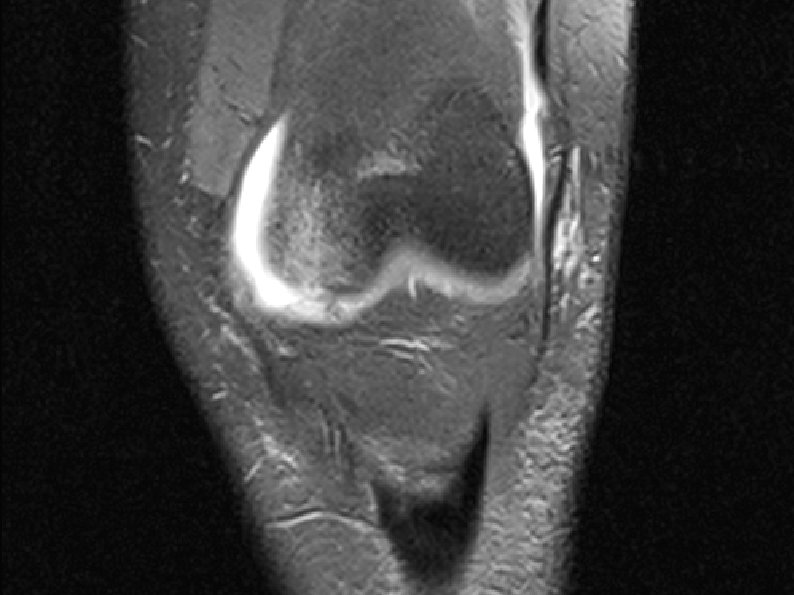
• Mrt / ro
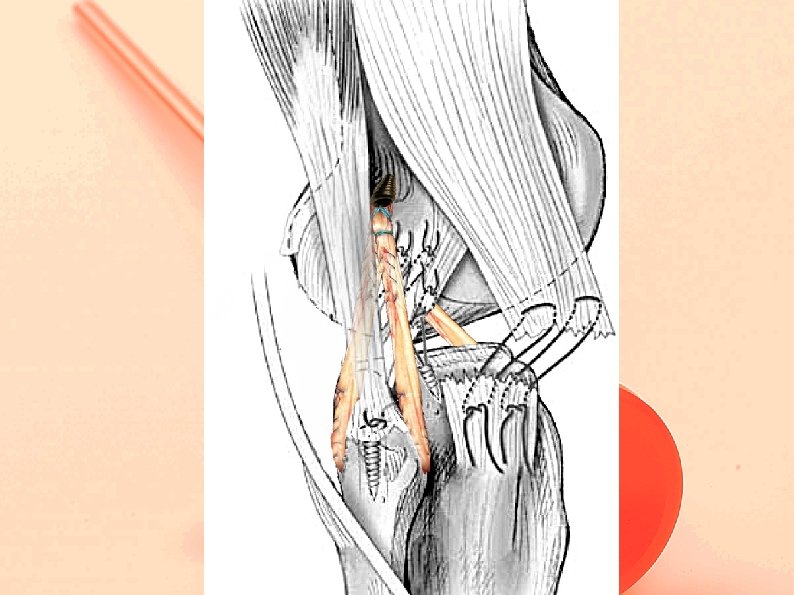
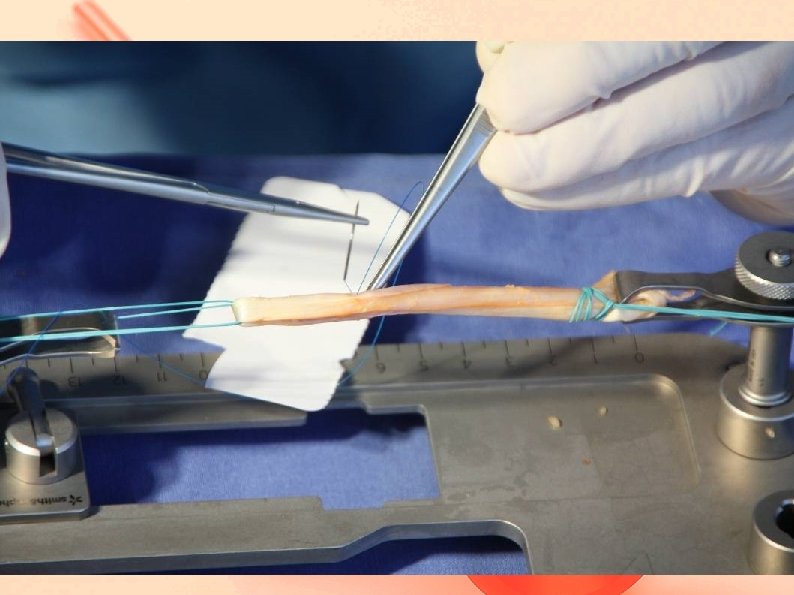
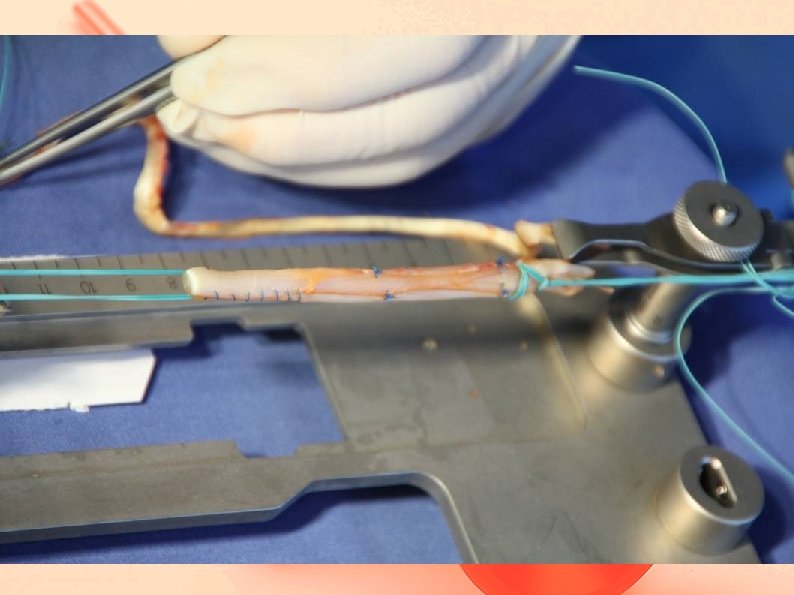
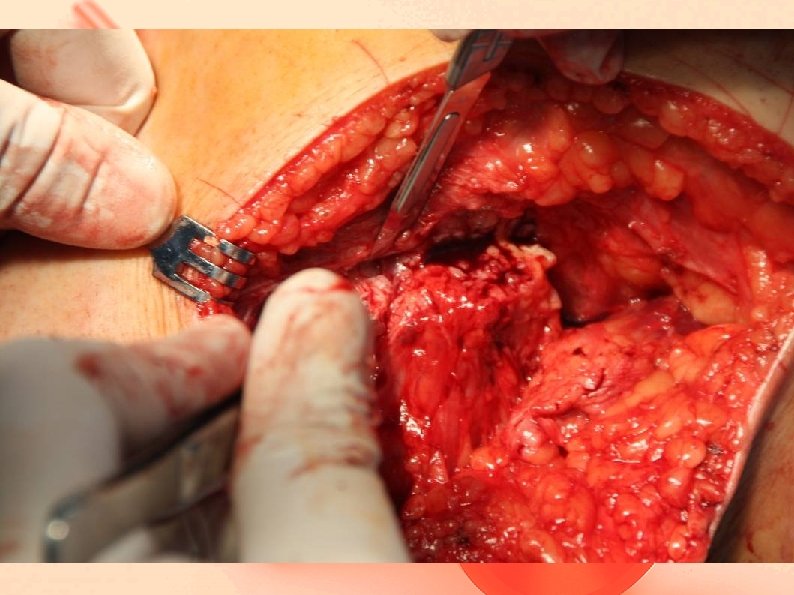
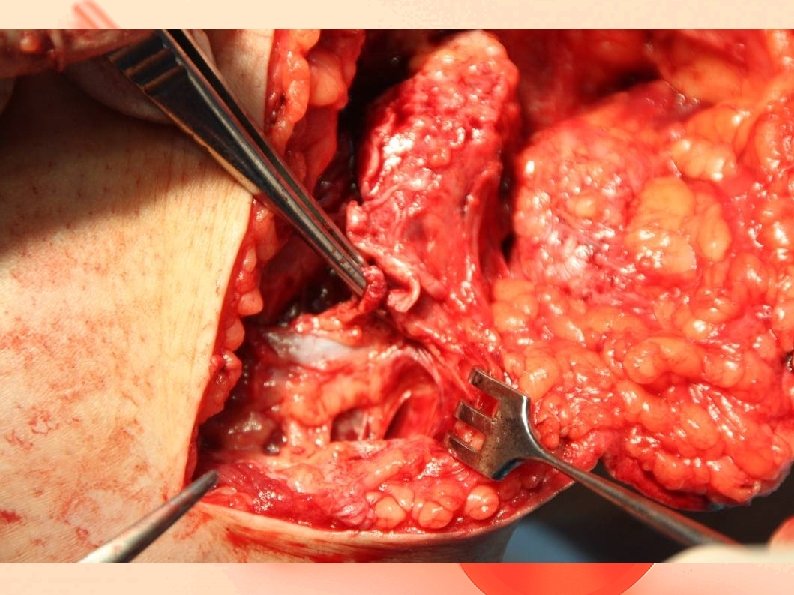
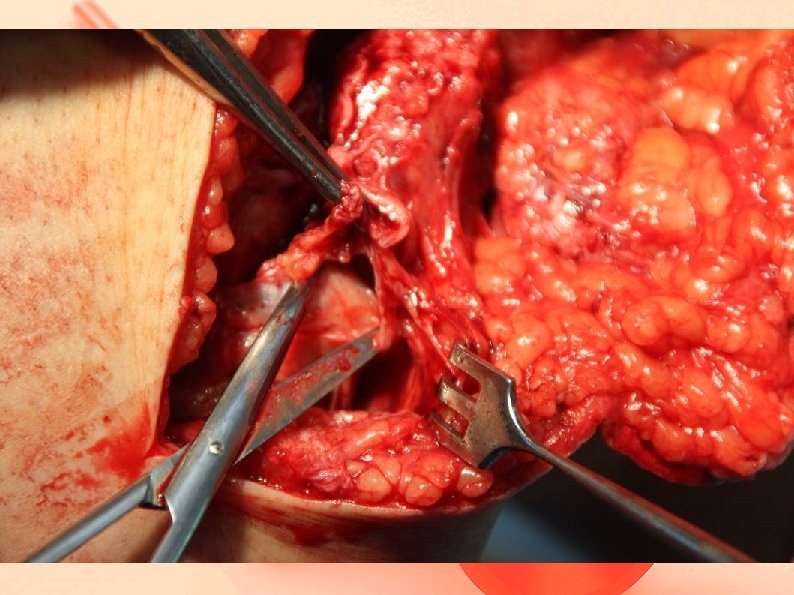
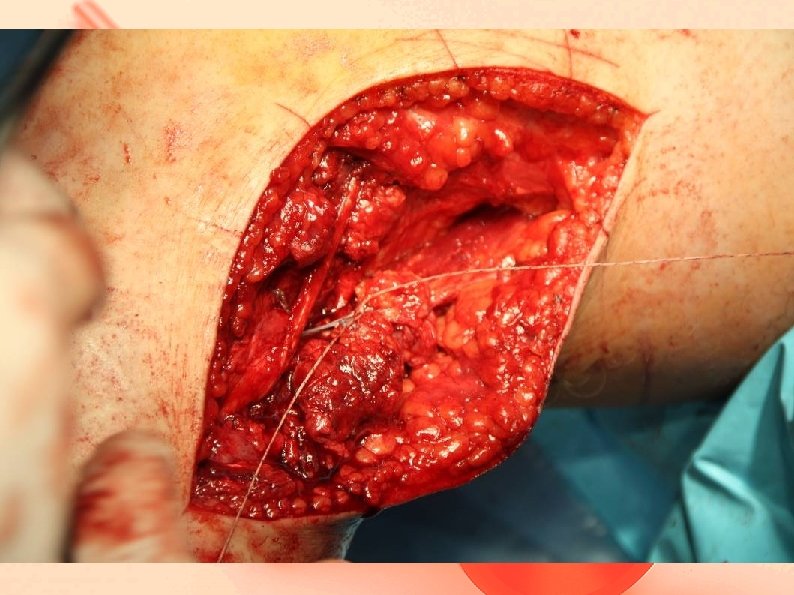
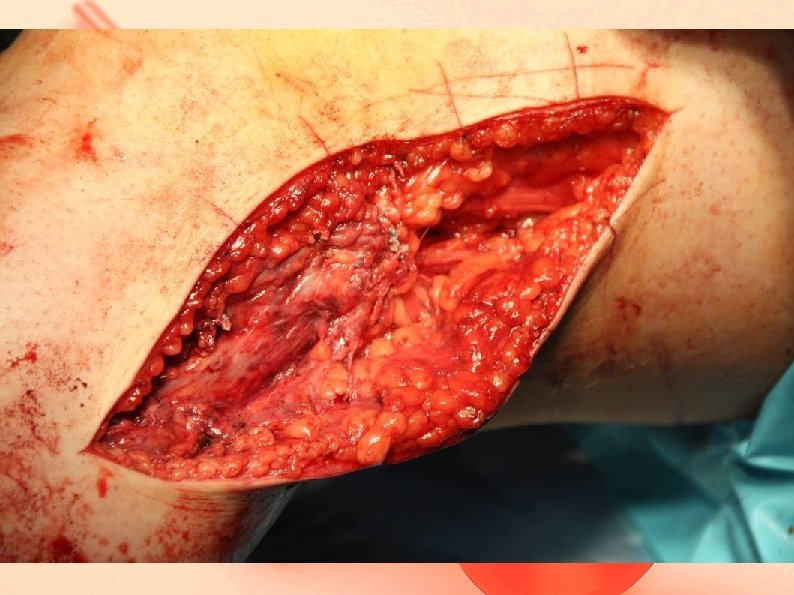
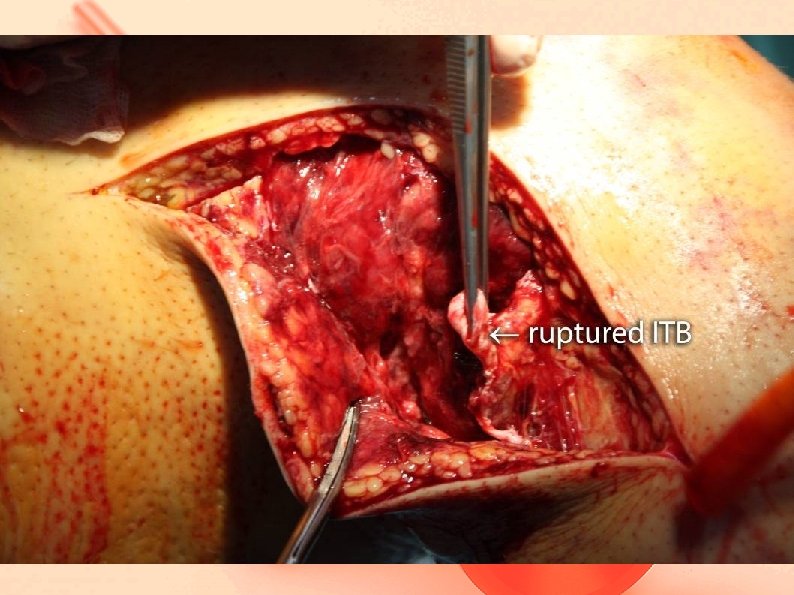
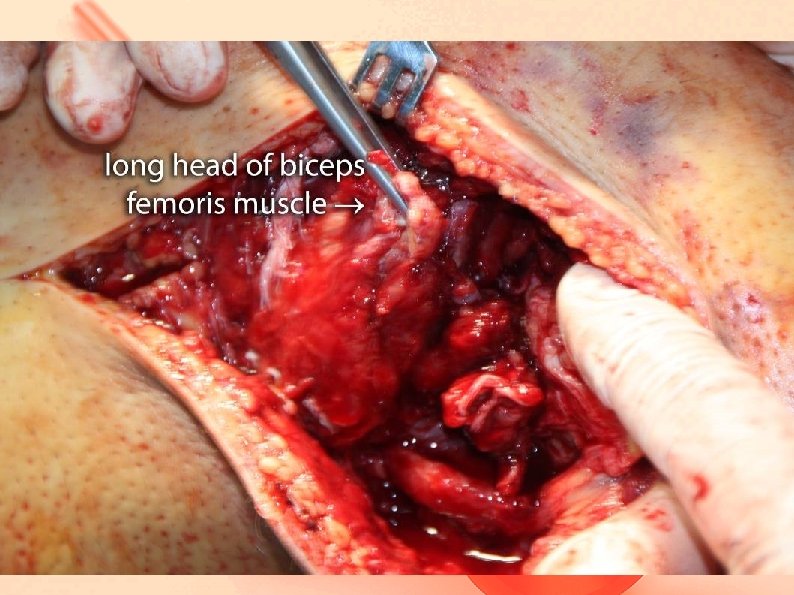
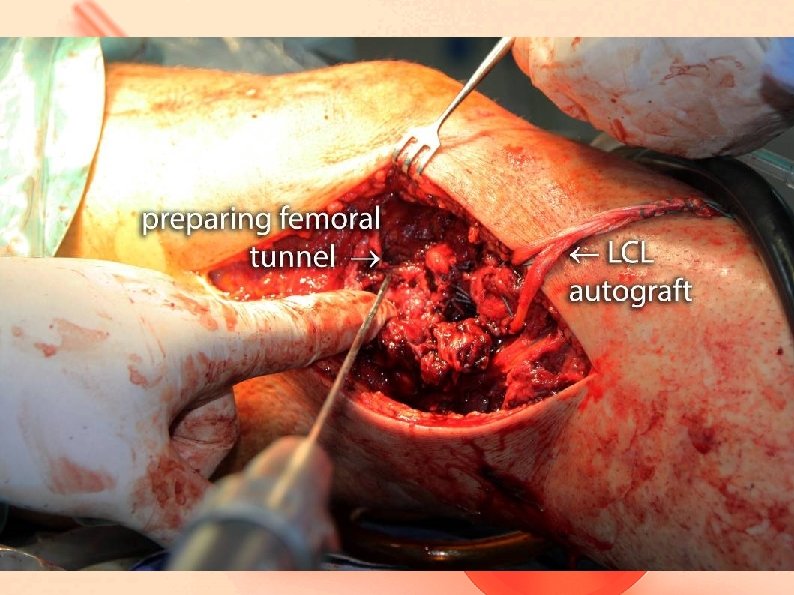
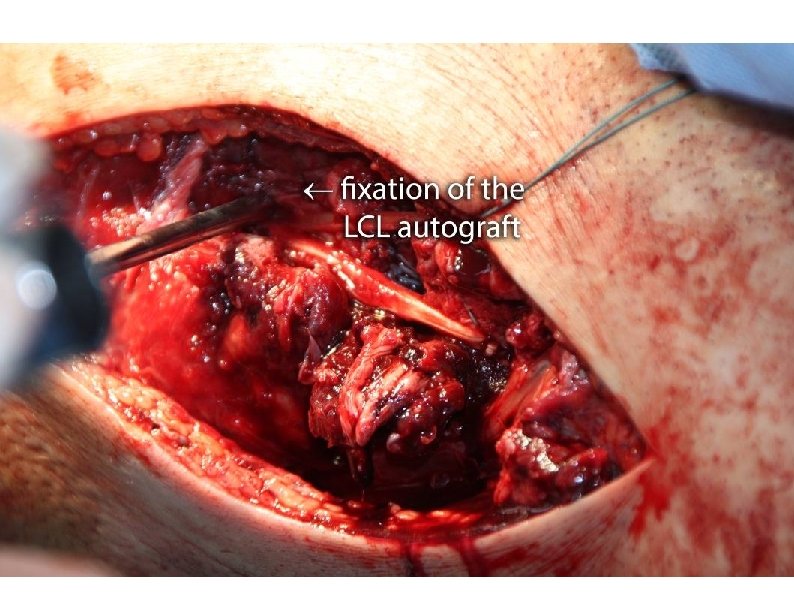
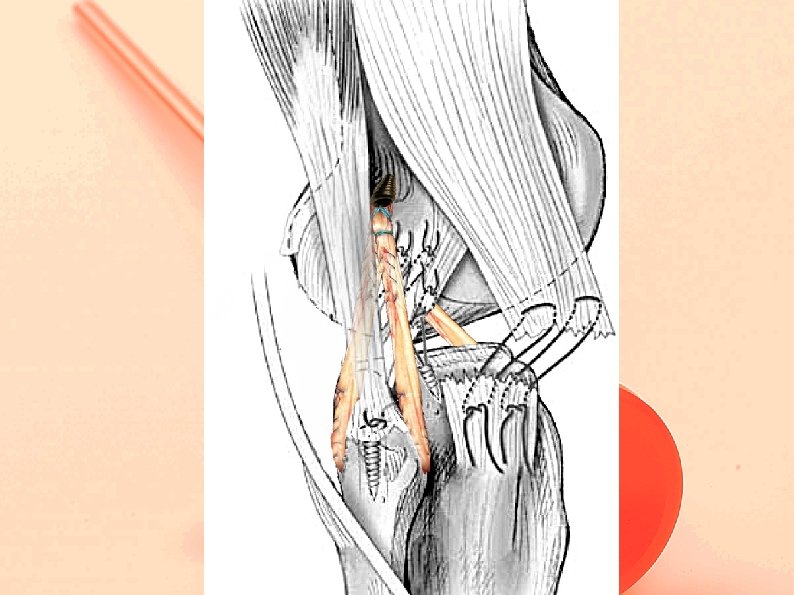
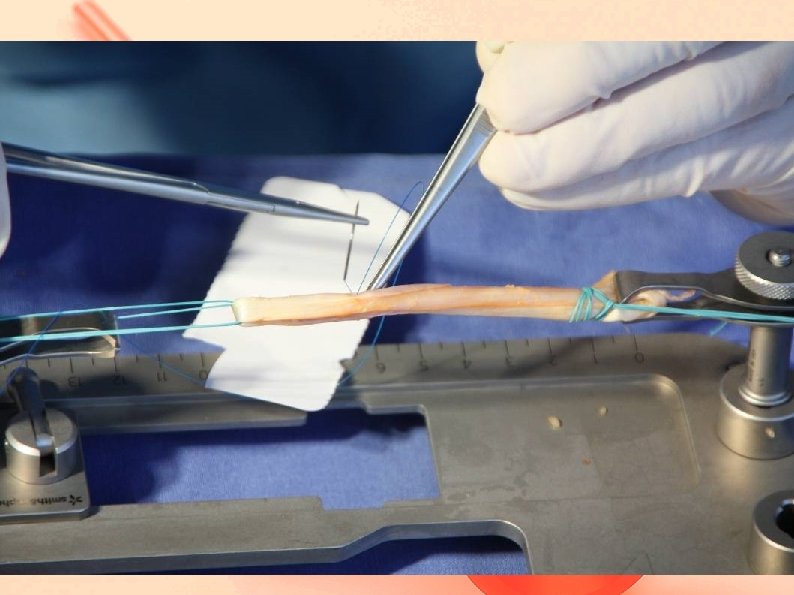
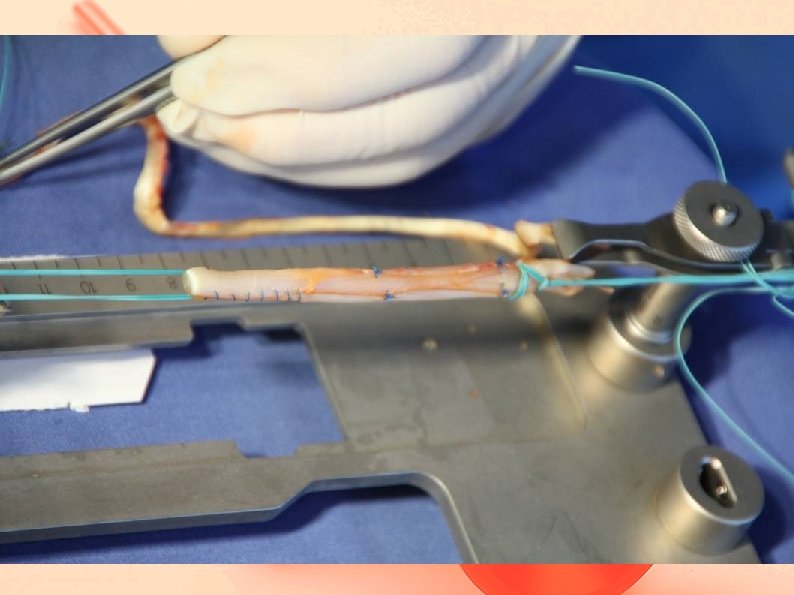
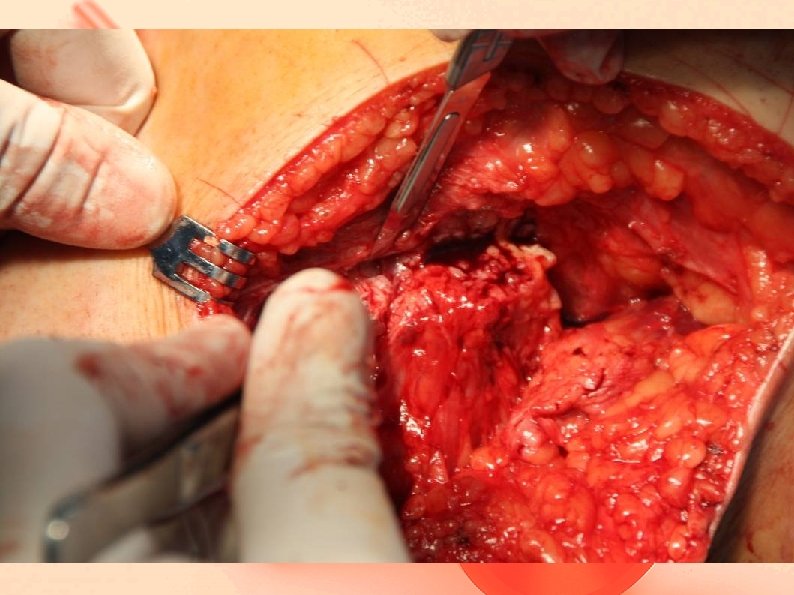
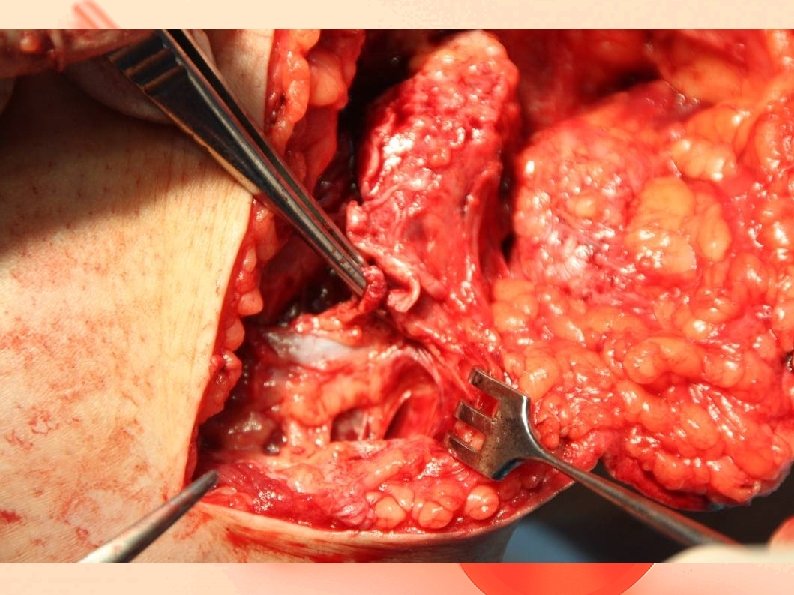
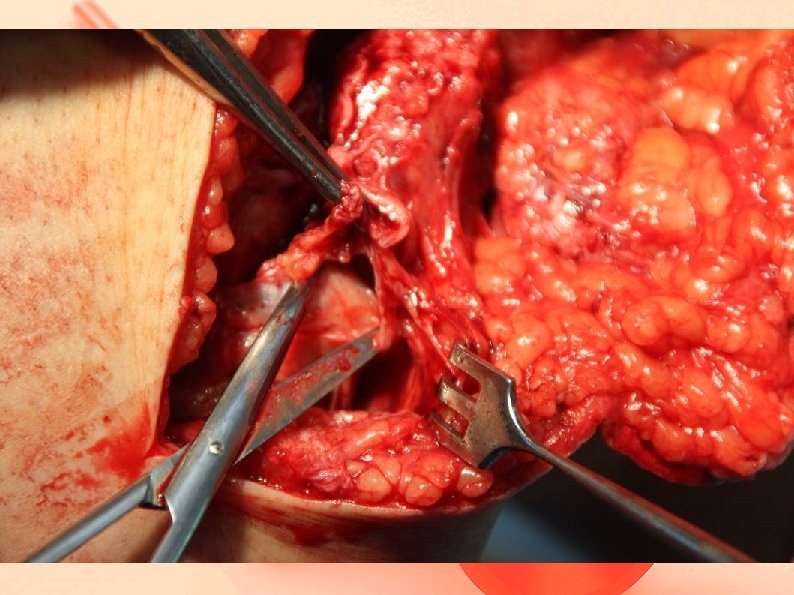
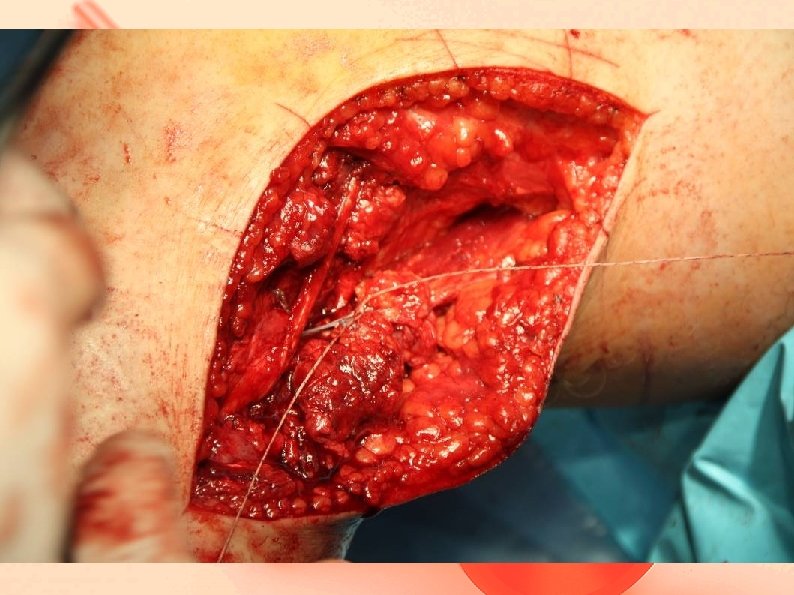
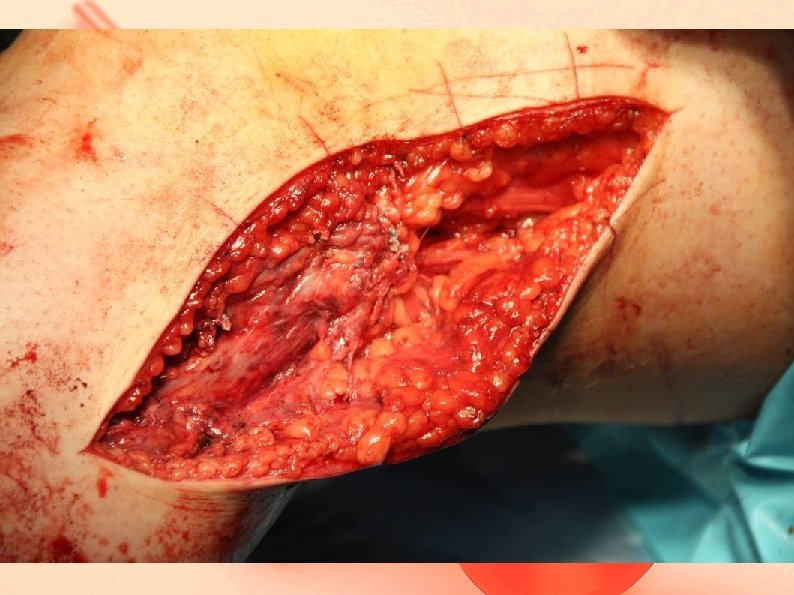
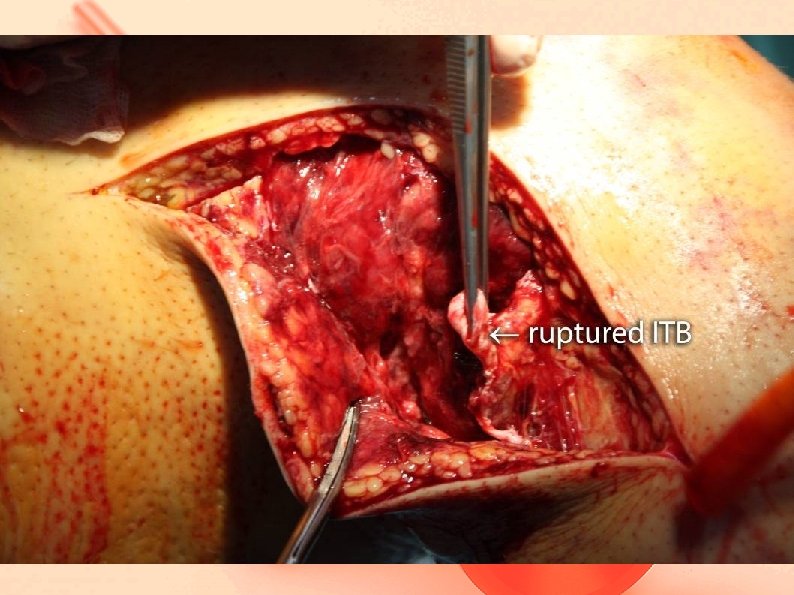
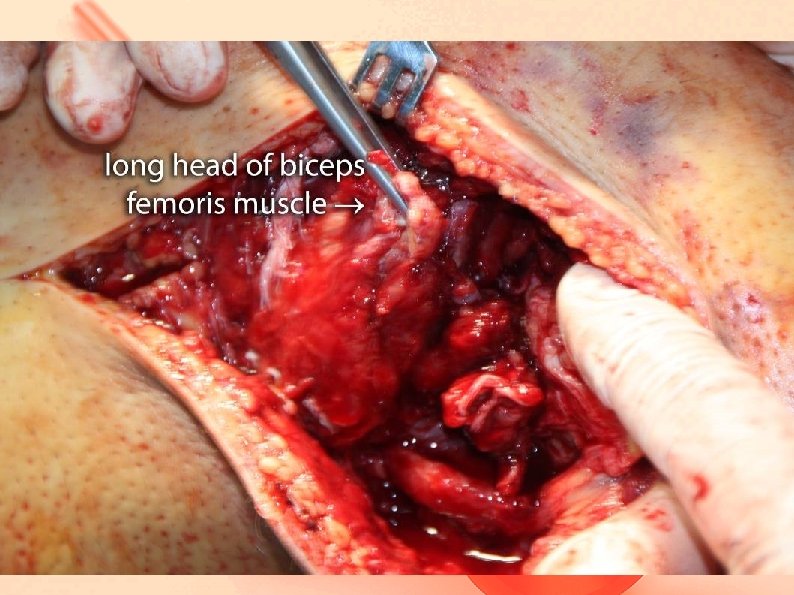
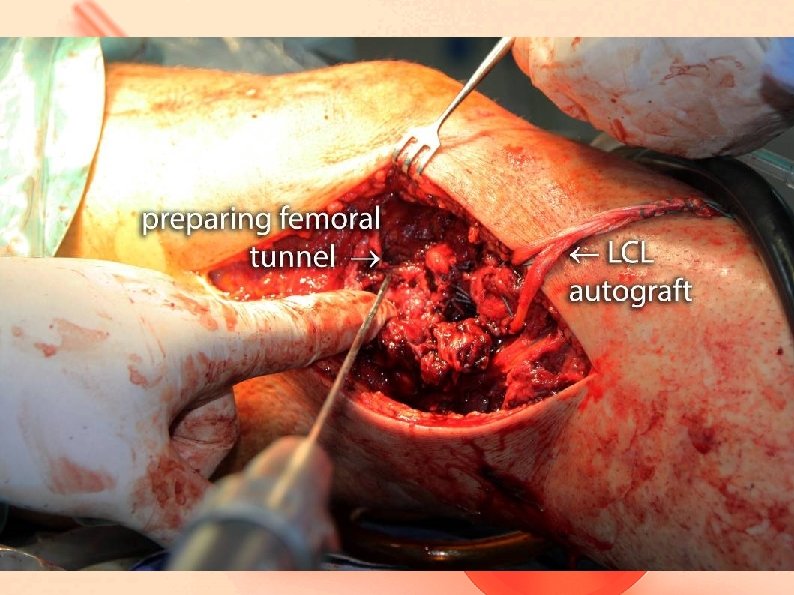
What had to be done - ACL arthroscopic reconstruction using ST graft Revision and decompression of CPN PLC reconstruction using anchor sutures Long head of biceps femoris insertion using anchor sutures LCL reconstruction using GR graft ITB suture


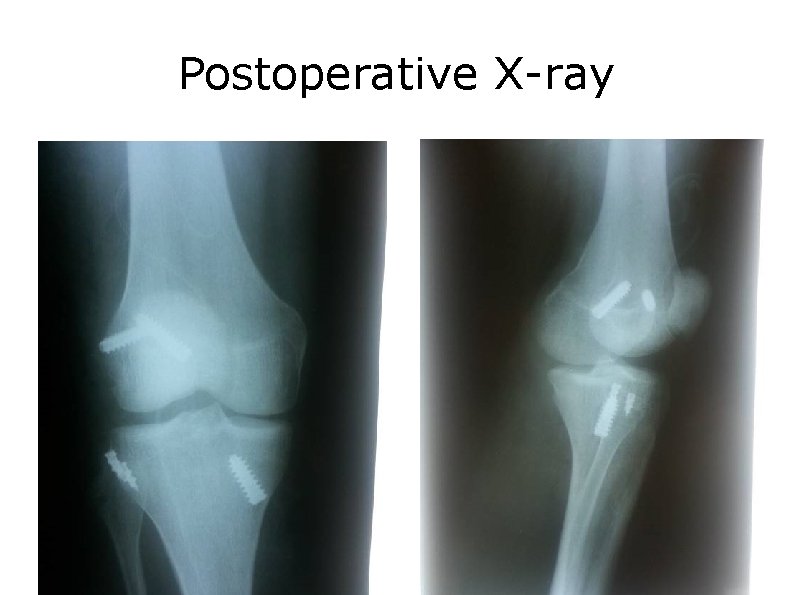
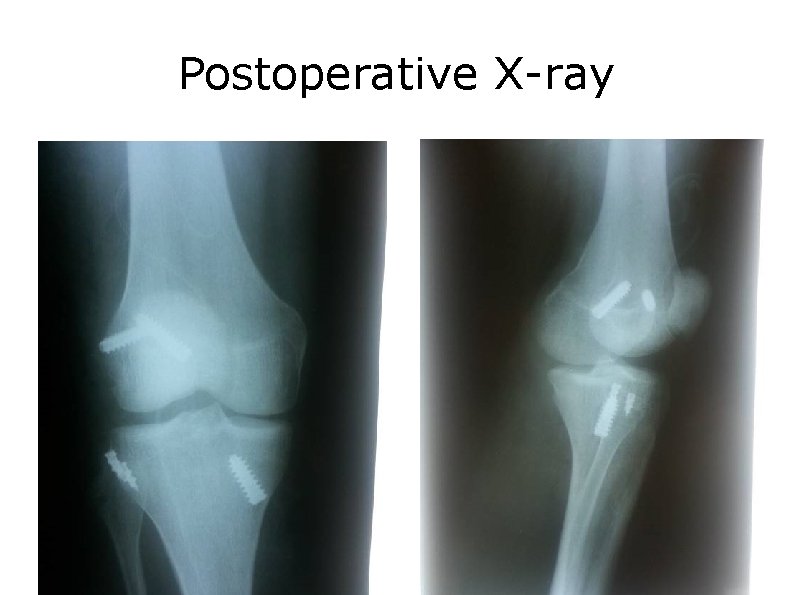
Postoperative X-ray
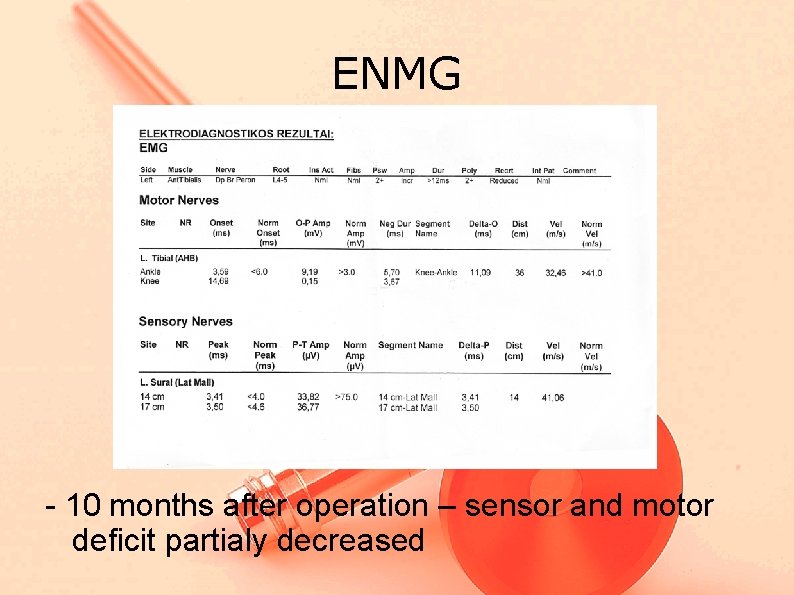
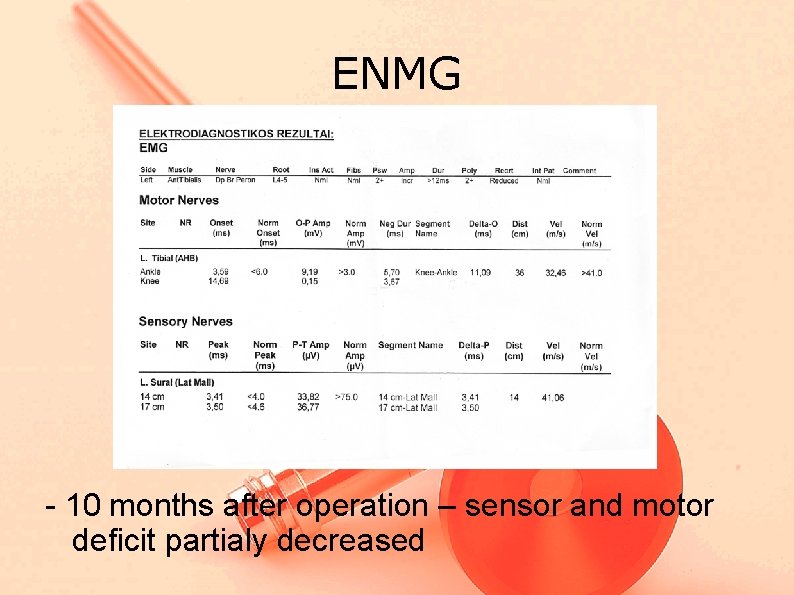
ENMG - 10 months after operation – sensor and motor deficit partialy decreased
Results • Video



Outcome - Result was evaluated using “IKDC 2000” - Patient was questioned before surgery and 10 months after surgery - IKDC score increased from 25, 3 to 60, 9.
Case II 21 year male car accident injury. Right knee was involved. The dislocated limb was immobilized with brace. MRI – ACL, LCL, PLC, ITB injury was diagnosed neurology – partial CPN palsy.
Case II - Surgery was performed 8 days after injury - No signs of nerve repair was noted - Huge knee varus instability >15 degrees - External rotation 50 degrees - Pivot shift +++ - Lachman ++ - Anterior drawer ++




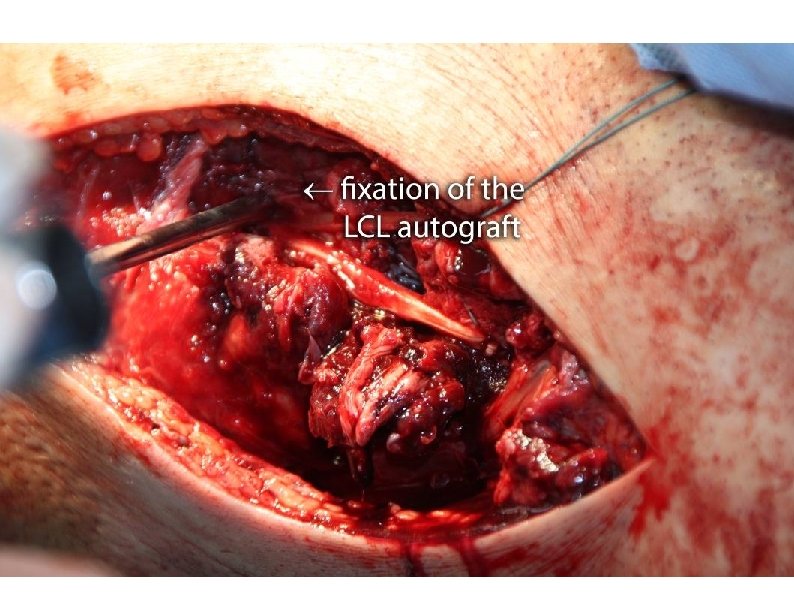

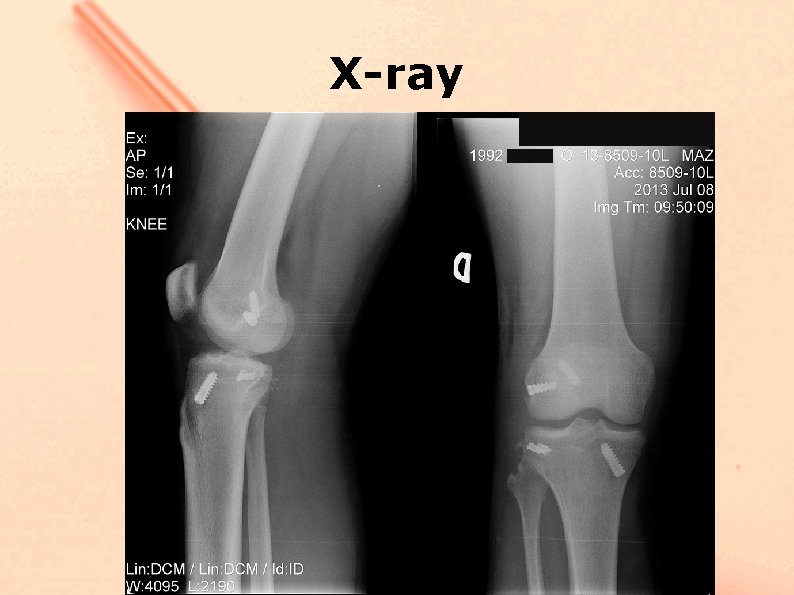
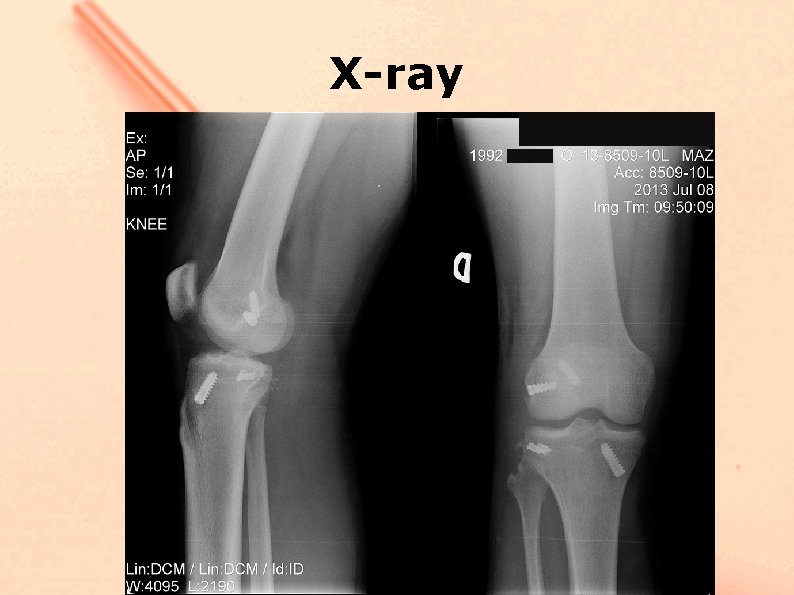
X-ray
Outcome - Result was evaluated using “IKDC 2000” - Patient was questioned 4 months after surgery - IKDC score was 87, 4.
Take home message - Early aggressive surgery gives better outcome results for grade III injuries - Common peroneal nerve revision in most cases is inevitable - Cases require accurate preoperative examination and careful planing.
