Introduction to Cardiology Terry White RN EMTP Introduction













- Slides: 51
Introduction to Cardiology Terry White, RN, EMT-P
Introduction to Cardiology n n Cardiovascular Disease EMS System Role Cardiovascular A&P Cardiovascular Electrophysiology
Cardiovascular Disease n Single greatest cause of death and disability in the United States – includes heart disease and vascular disease n 2 million people diagnosed with an ACS/yr – 1. 5 million will experience an acute MI • Of these, 0. 5 million will die – Almost half of these (250, 000) will be sudden and within the first hour of onset of symptoms n 500, 000 people will suffer a stroke each year in the US – Nearly 1/4 of these will die
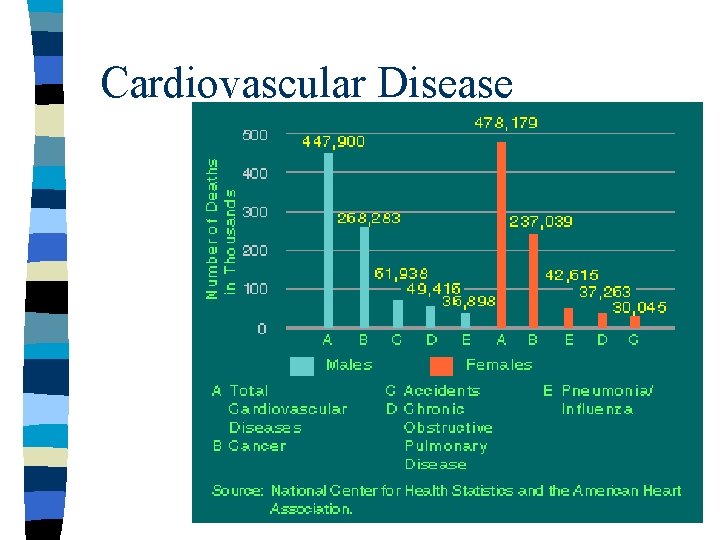
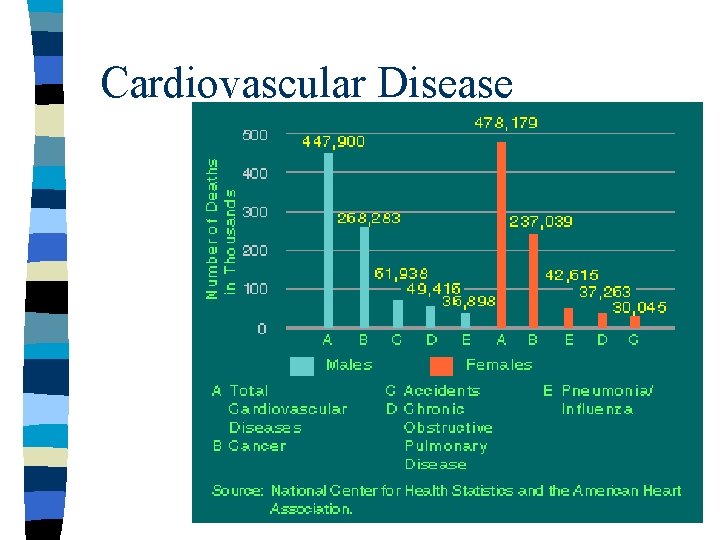
Cardiovascular Disease
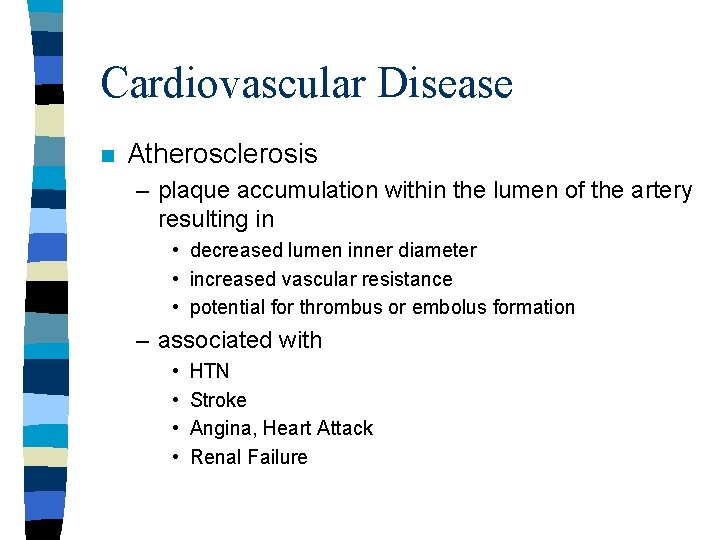
Cardiovascular Disease n Atherosclerosis – plaque accumulation within the lumen of the artery resulting in • decreased lumen inner diameter • increased vascular resistance • potential for thrombus or embolus formation – associated with • • HTN Stroke Angina, Heart Attack Renal Failure
Cardiovascular Disease n Risk Factors – – – – Age Family History Hypertension Hypercholesterolemia Male gender Smoking Diabetes n Contributing Risk Factors – – – Diet Obesity Oral contraceptives Sedentary living Personality type
EMS System Role n The original Paramedic idea was based upon the need for rapid response to, identification of and emergency care for victims of: – Sudden Cardiac Death (SCD) – Acute Myocardial Infarction (AMI)
EMS System Role n n n The EMT and Paramedic roles in the treatment of sudden cardiac death have been proven to make a difference in survival Contributions being recognized in acute coronary syndromes Key is a STRONG chain of survival

EMS System Role n Weak vs. Strong Chain of Survival
Anatomy & Physiology
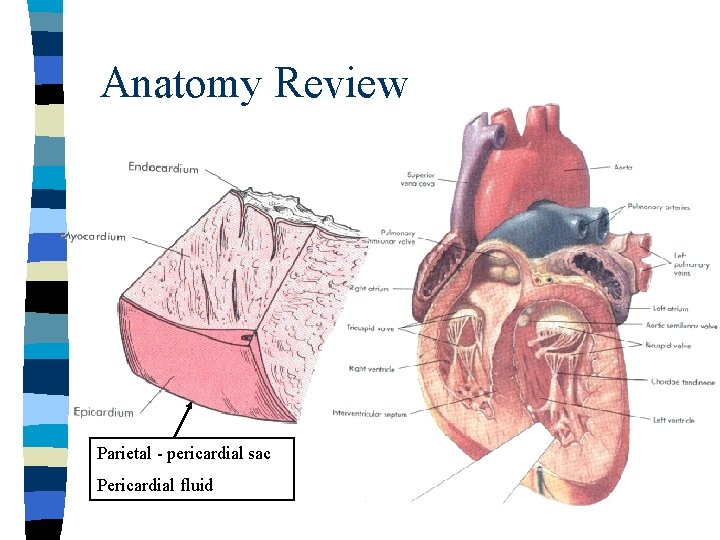
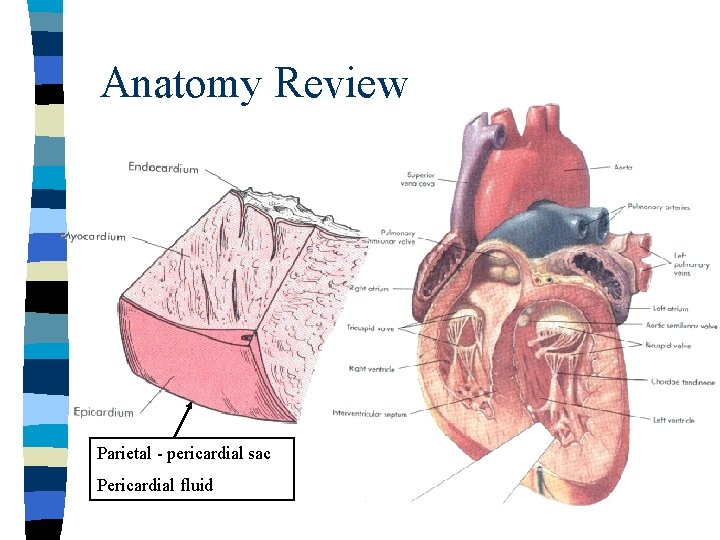
Anatomy Review Parietal - pericardial sac Pericardial fluid
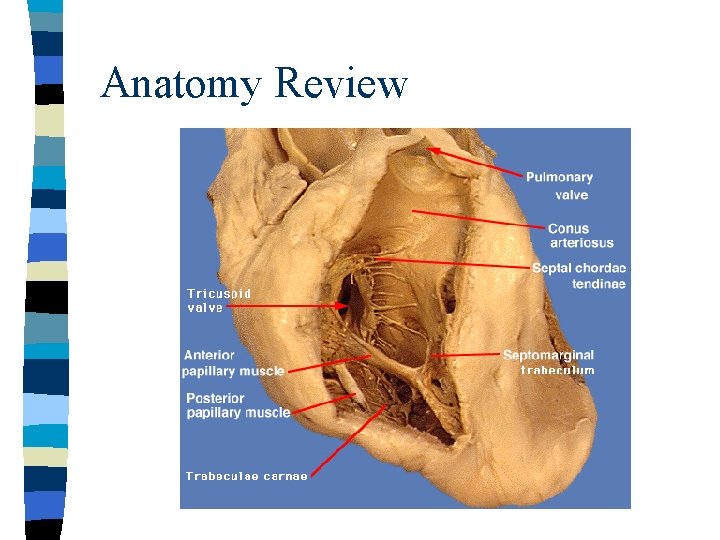
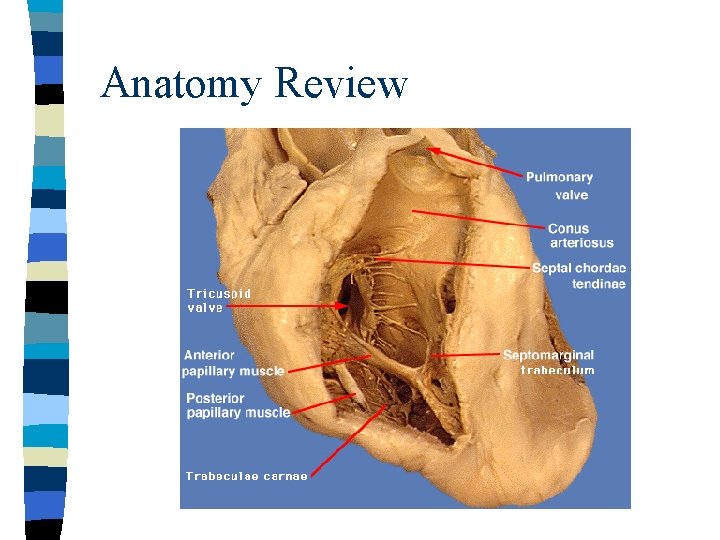
Anatomy Review

Blood Flow (mitral valve) Chordae tendinae
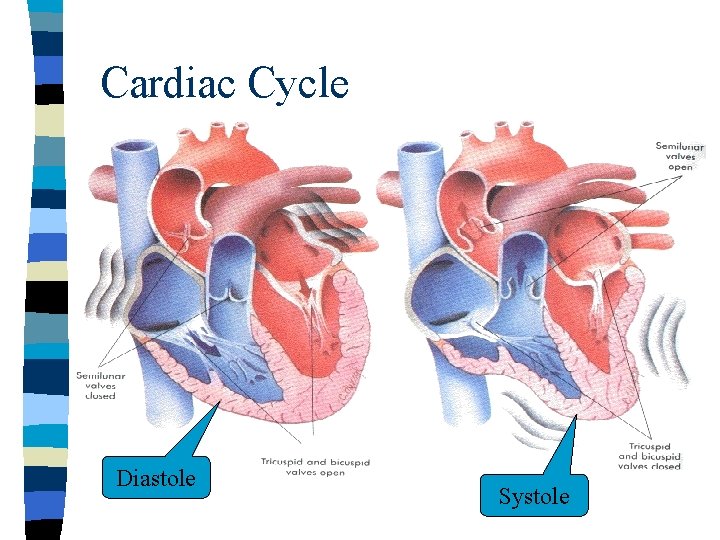
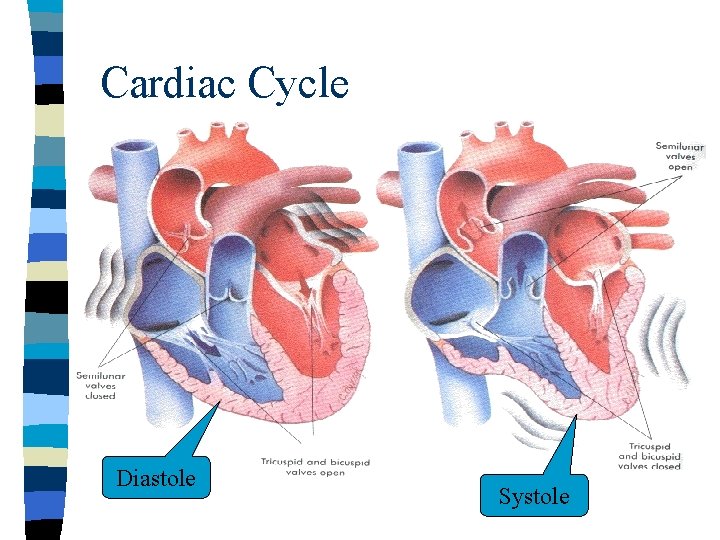
Cardiac Cycle Diastole Systole
Cardiac Output n n Stroke volume x Heart rate Also dependent upon – Stroke volume • contractility • preload – volume in ventricle at end of diastole • afterload – resistance against which left ventricle must pump – Starling’s law
Vascular System n Aorta – ascending thoracic – descending thoracic – abdominal n Vena cava – superior – inferior

Peripheral Vascular System n Arteries & Veins – 3 layers – tunica media > in arteries – flow through a vessel directly proportional to the fourth power of the radius • atherosclerosis • vascular constriction
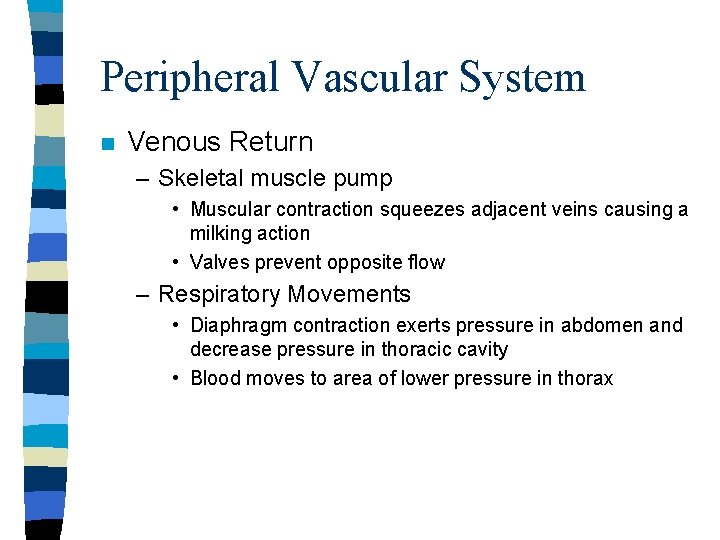
Peripheral Vascular System n Venous Return – Skeletal muscle pump • Muscular contraction squeezes adjacent veins causing a milking action • Valves prevent opposite flow – Respiratory Movements • Diaphragm contraction exerts pressure in abdomen and decrease pressure in thoracic cavity • Blood moves to area of lower pressure in thorax
Peripheral Vascular System n Venous Return – Constriction of veins • Sympathetic stimulation causes contraction of the smooth muscle walls of veins – Gravity
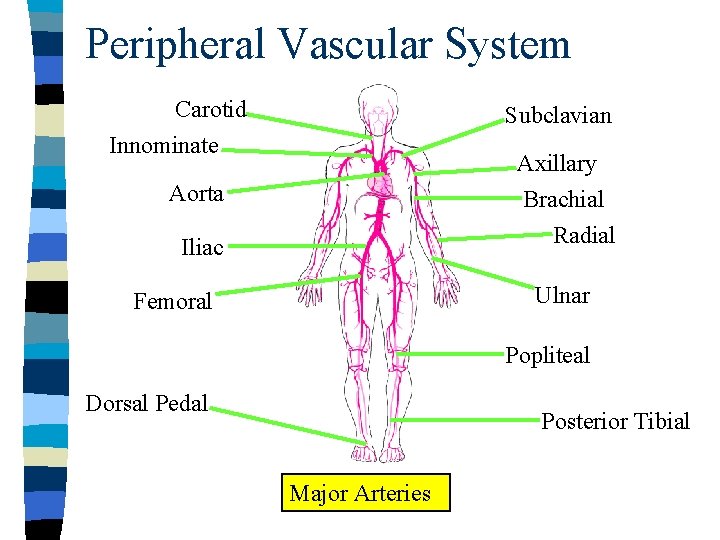
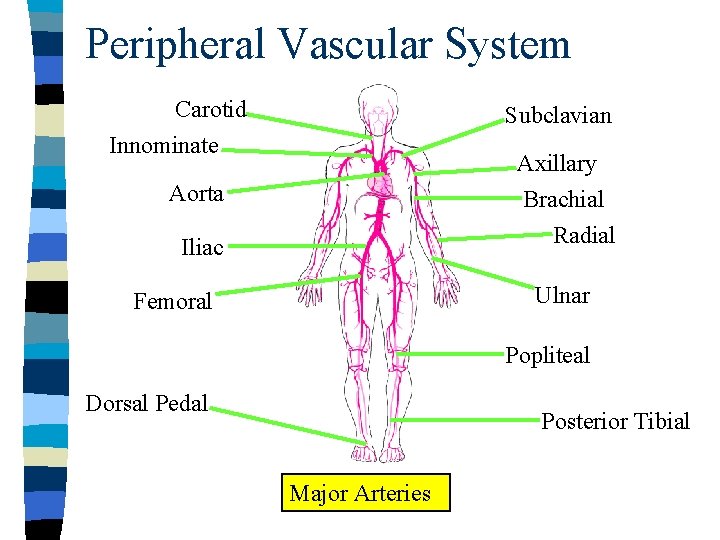
Peripheral Vascular System Carotid Subclavian Innominate Axillary Brachial Radial Aorta Iliac Ulnar Femoral Popliteal Dorsal Pedal Posterior Tibial Major Arteries

Peripheral Vascular System External Jugular Internal Jugular Subclavian Superior Vena Cava Inferior Vena Cava Axillary Iliac Femoral Saphenous Major Veins
Peripheral Vascular System n Negative Effects on Venous Return – Increasd intrathoracic pressure – PEEP/CPAP/Bi. PAP
Peripheral Vascular System n Arterial Resistance (afterload) – BP • cardiac output x systemic vascular resistance – (stroke volume x heart rate) x systemic vascular resistance – Systemic vascular resistance • vasoconstriction – Sympathetic NS effects – Medications (prescription, non-prescription, recreational) – Renin-Angiotensin-Aldosterone mechanisms • atherosclerosis

Coronary Circulation n Usually thought of as 3 arteries – Left (Main) Coronary Artery • Left circumflex artery • Left anterior descending artery – Right Coronary Artery n Areas affected
Coronary Circulation n Coronary Sinus – short trunk receiving blood from cardiac veins – empties into the right atrium between inferior vena cava and AV orifice n Cardiac veins – feed into the coronary sinus
Electrophysiology
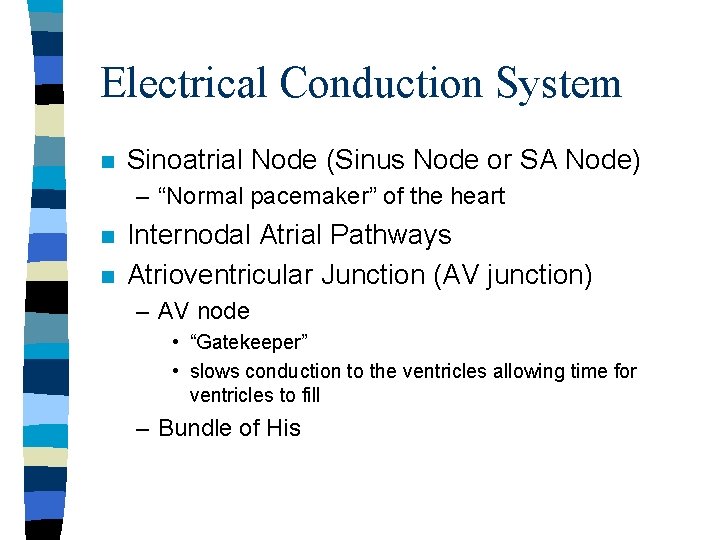
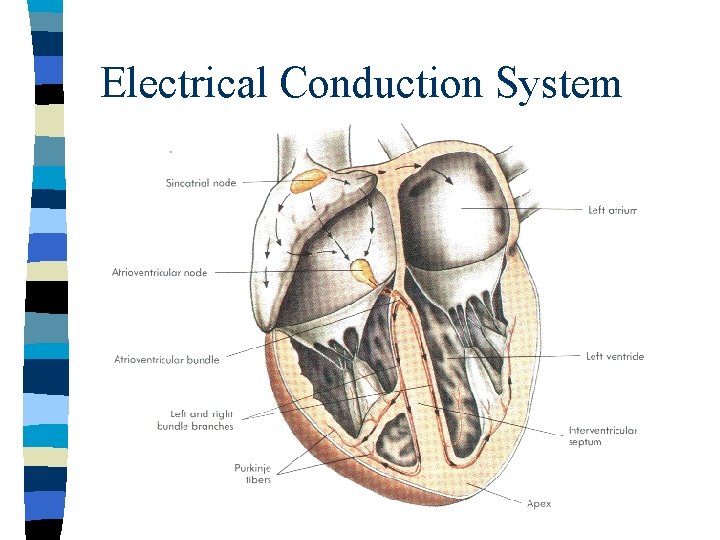
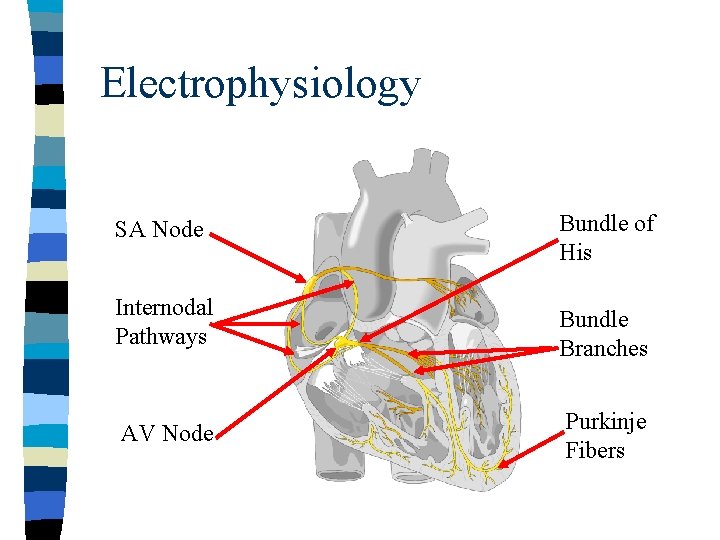
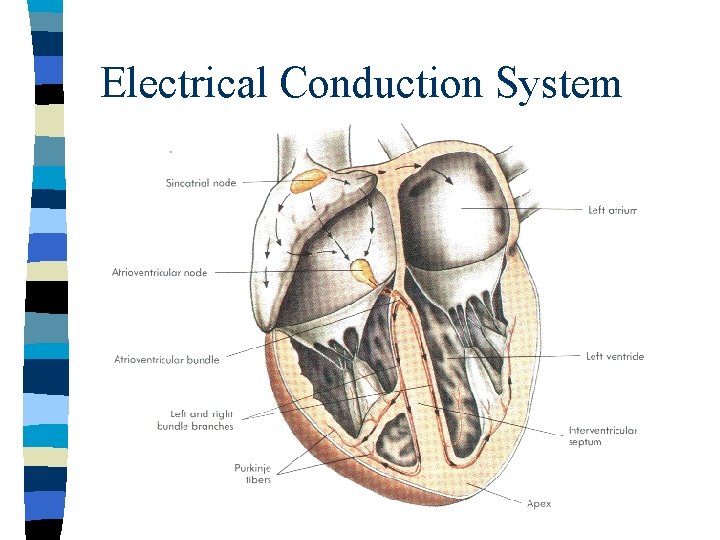
Electrical Conduction System n Sinoatrial Node (Sinus Node or SA Node) – “Normal pacemaker” of the heart n n Internodal Atrial Pathways Atrioventricular Junction (AV junction) – AV node • “Gatekeeper” • slows conduction to the ventricles allowing time for ventricles to fill – Bundle of His
Electrical Conduction System n His-Purkinje System – Bundle Branches • Right bundle branch • Left bundle branch – left anterior fascicle – left posterior fascicle
Electrical Conduction System

Electrical Conduction System n Myocardial Cells – Characteristics • automaticity: cells can depolarize without any impulse from outside source (self-excitation) • excitability: cells can respond to an electrical stimulus • conductivity: cells can propagate the electrical impulse from cell to another • contractility: the specialized ability of the cardiac muscle cells to contract
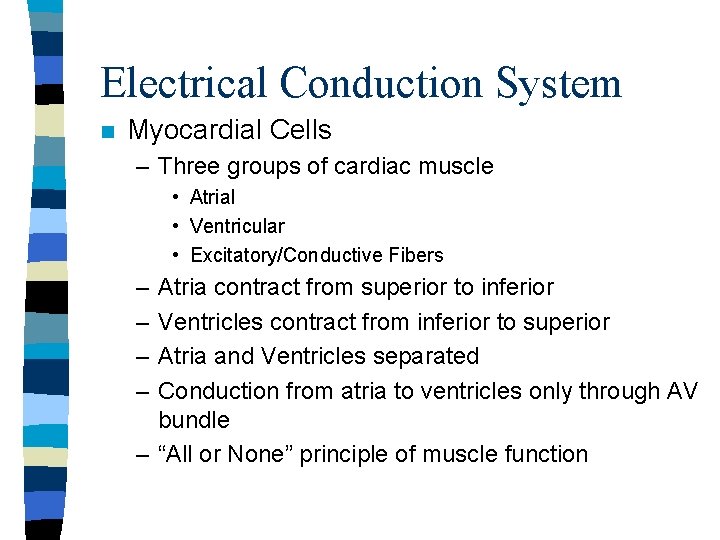
Electrical Conduction System n Myocardial Cells – Three groups of cardiac muscle • Atrial • Ventricular • Excitatory/Conductive Fibers – – Atria contract from superior to inferior Ventricles contract from inferior to superior Atria and Ventricles separated Conduction from atria to ventricles only through AV bundle – “All or None” principle of muscle function

Electrophysiology n Electrolytes – Allow for electrical and mechanical function of heart • Sodium: major extracellular cation, role in depolarization • Potassium: major intracellular cation, role in repolarization • Calcium: intracellular cation, role in depolarization and myocardial contraction • Chloride: extracellular anion • Magnesium: intracellular cation

Electrophysiology n Depolarization – Reversal of charges at the cell membrane (opposite charge from resting state) – Resting Potential • more intracellular negatively charged anions than extracellular • approximately -90 m. V in myocardial cell – Action Potential • stimulus to myocardial cell allows sodium to enter cell changing to positive intracellular charge • approximately +20 m. V in myocardial cell • slow influx of Calcium follows

Electrophysiology n Depolarization – Complete depolarization normally results in muscle contraction n Threshold – minimal stimulus required to produce excitation of myocardial cells
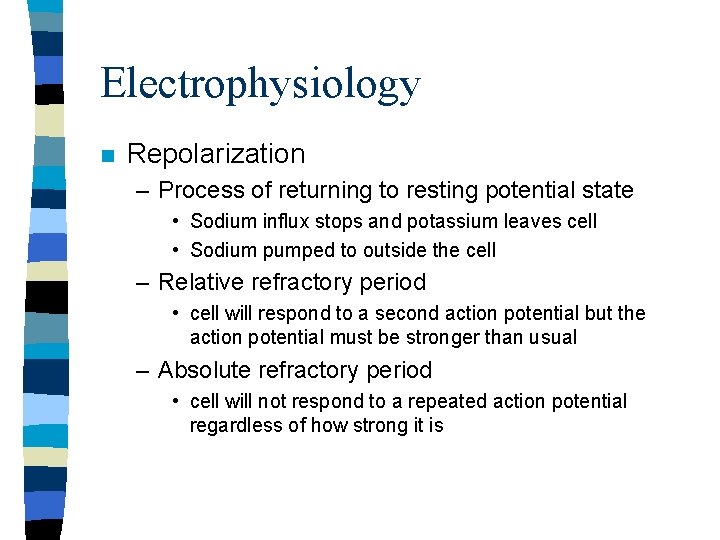
Electrophysiology n Repolarization – Process of returning to resting potential state • Sodium influx stops and potassium leaves cell • Sodium pumped to outside the cell – Relative refractory period • cell will respond to a second action potential but the action potential must be stronger than usual – Absolute refractory period • cell will not respond to a repeated action potential regardless of how strong it is
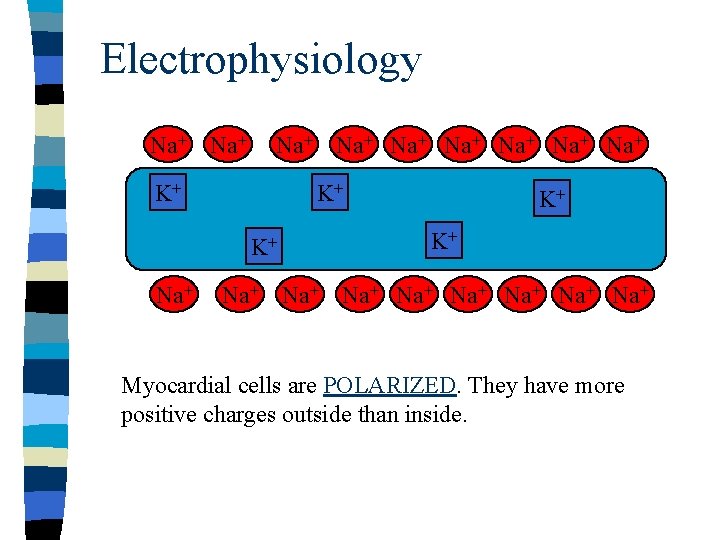
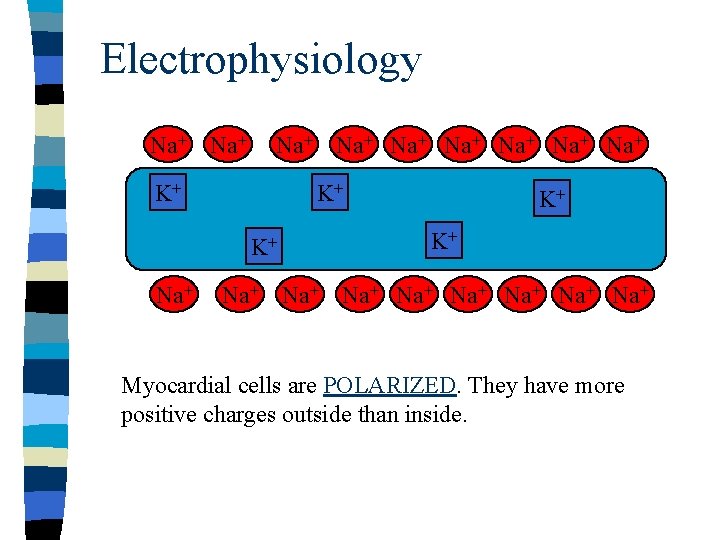
Electrophysiology Na+ Na+ Na+ K+ K+ K+ Na+ Na+ Na+ Myocardial cells are POLARIZED. They have more positive charges outside than inside.
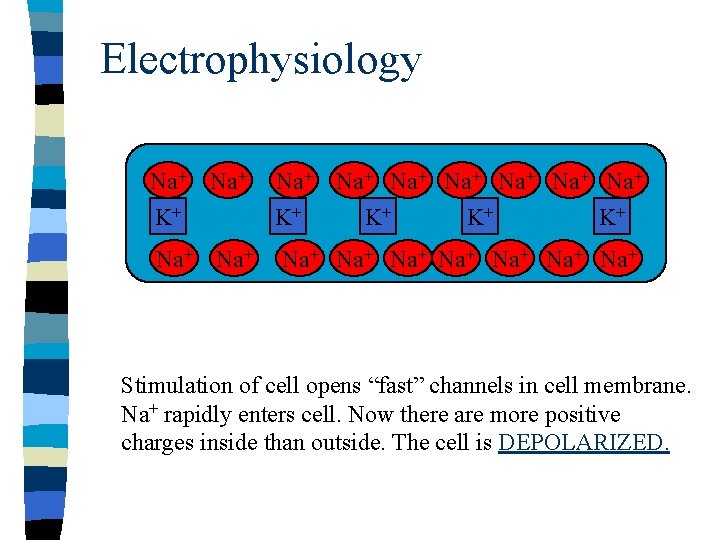
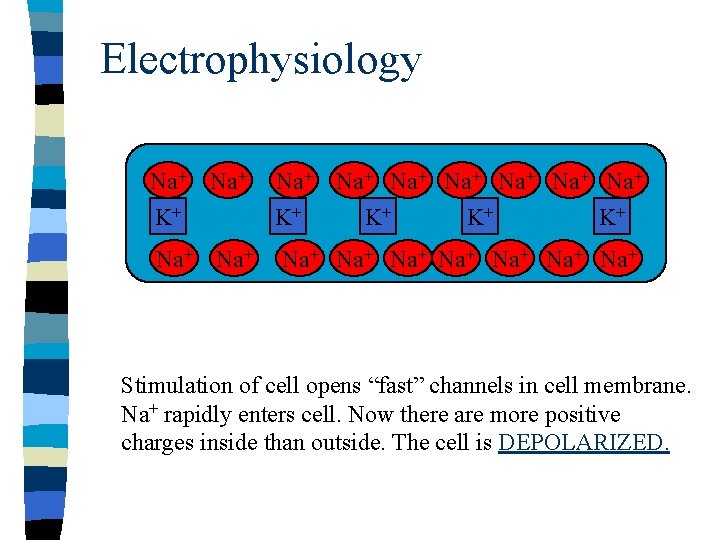
Electrophysiology Na+ K+ Na+ Na+ K+ K+ Na+ Na+ Na+ Stimulation of cell opens “fast” channels in cell membrane. Na+ rapidly enters cell. Now there are more positive charges inside than outside. The cell is DEPOLARIZED.
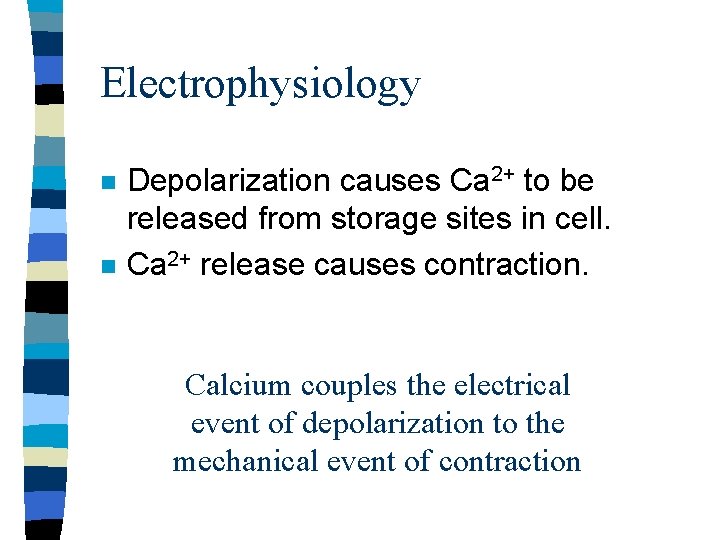
Electrophysiology n n Depolarization causes Ca 2+ to be released from storage sites in cell. Ca 2+ release causes contraction. Calcium couples the electrical event of depolarization to the mechanical event of contraction

Electrophysiology Na+ Na+ K+ Na+ Na+ Na+ K+ Na+ Cell then REPOLARIZES by pumping out K+ then Na+ to restore normal charge balance.
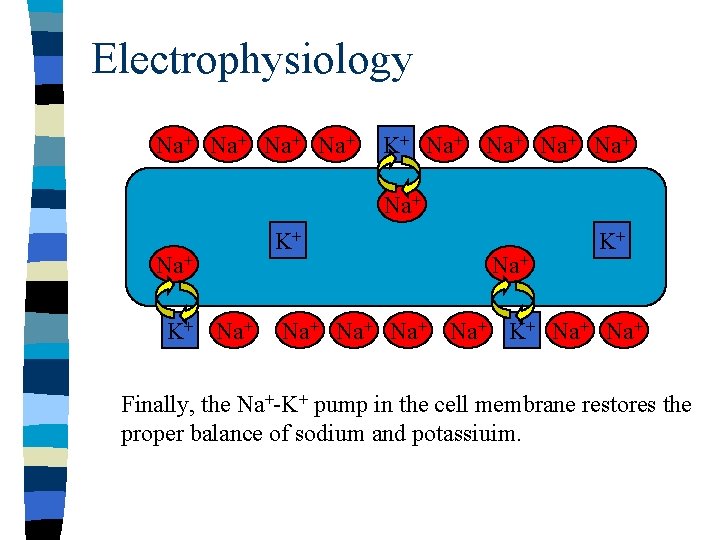
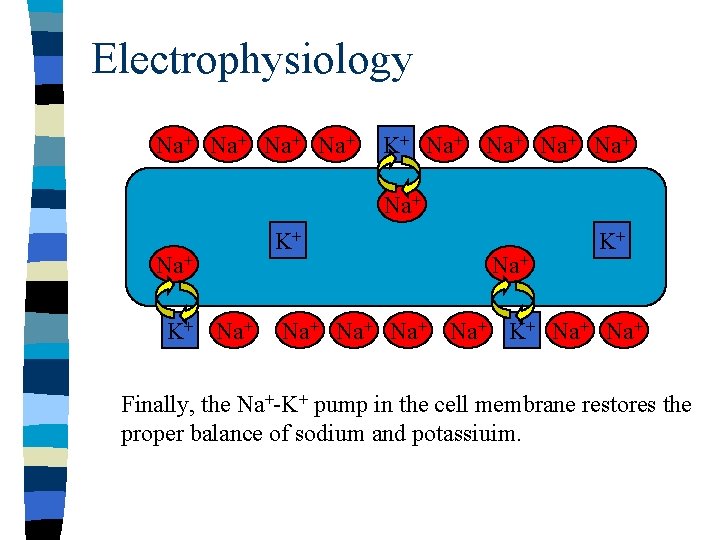
Electrophysiology Na+ Na+ K+ Na+ K+ Na+ Na+ K+ Na+ Finally, the Na+-K+ pump in the cell membrane restores the proper balance of sodium and potassiuim.
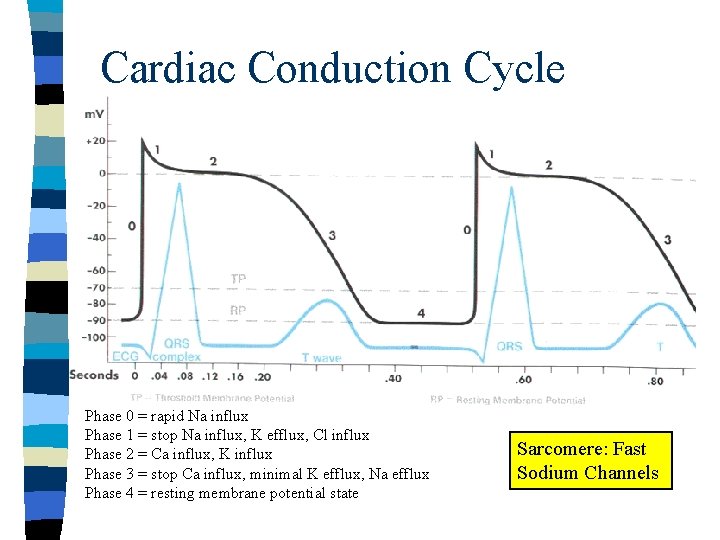
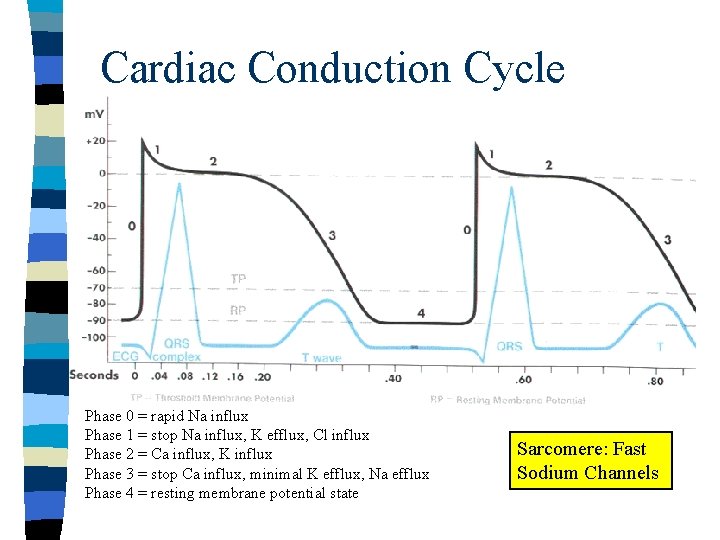
Cardiac Conduction Cycle Phase 0 = rapid Na influx Phase 1 = stop Na influx, K efflux, Cl influx Phase 2 = Ca influx, K influx Phase 3 = stop Ca influx, minimal K efflux, Na efflux Phase 4 = resting membrane potential state Sarcomere: Fast Sodium Channels
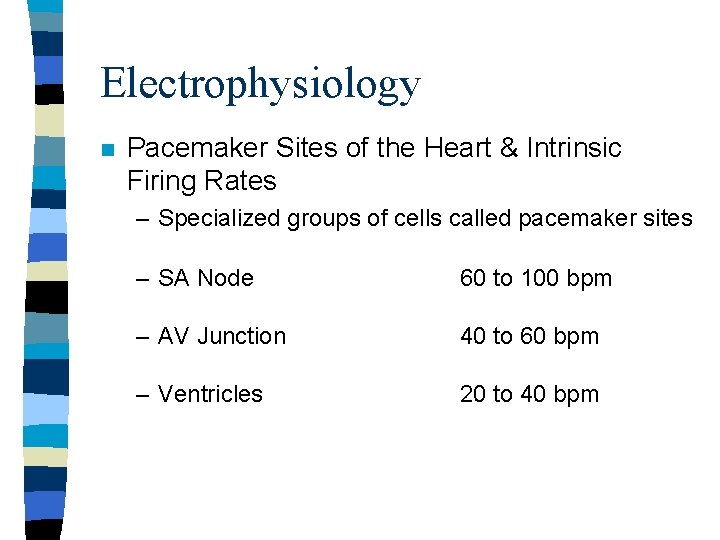
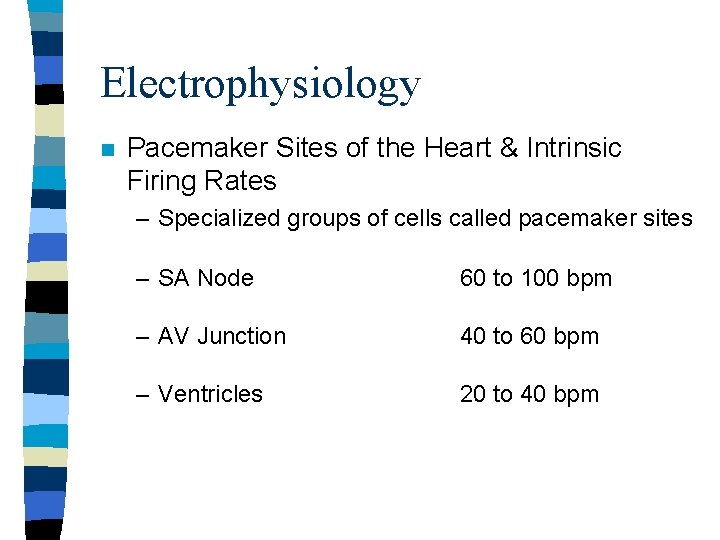
Electrophysiology n Pacemaker Sites of the Heart & Intrinsic Firing Rates – Specialized groups of cells called pacemaker sites – SA Node 60 to 100 bpm – AV Junction 40 to 60 bpm – Ventricles 20 to 40 bpm
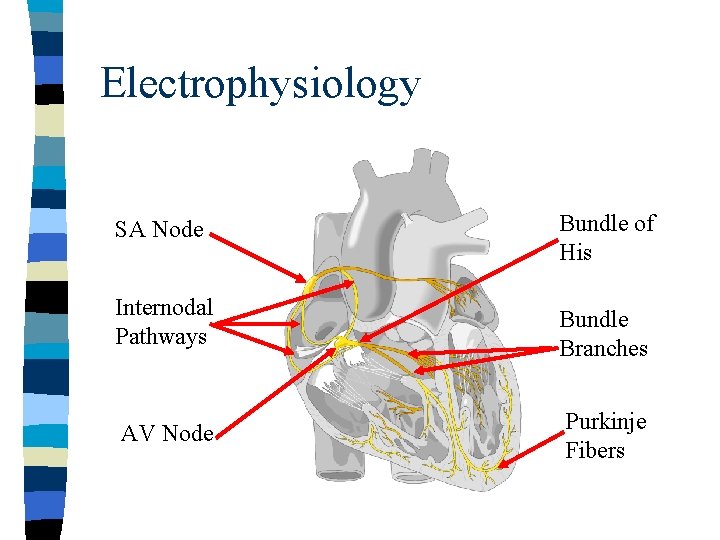
Electrophysiology SA Node Bundle of His Internodal Pathways Bundle Branches AV Node Purkinje Fibers

Electrophysiology Ca 2+ Na+ Na+ K+ K+ K+ Na+ Na+ Na+ Ca 2+ Specialized cells in conducting system (pacemaker cells) undergo spontaneous diastolic depolarization. During diastole, calcium leaks into cell through calcium channels.
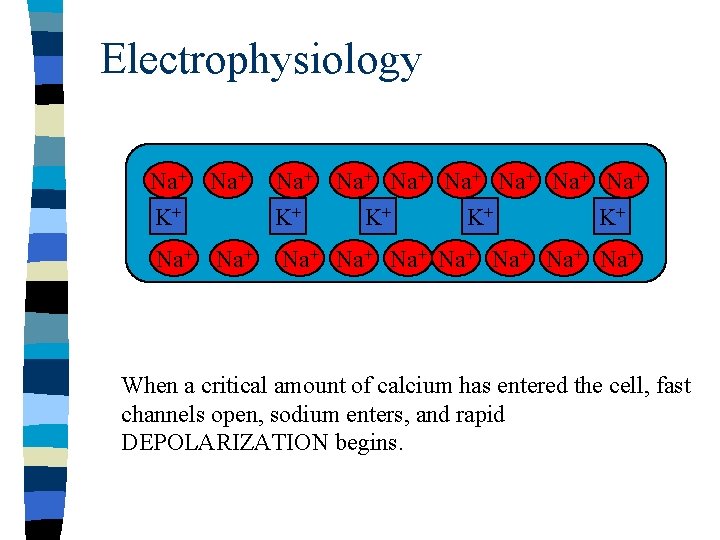
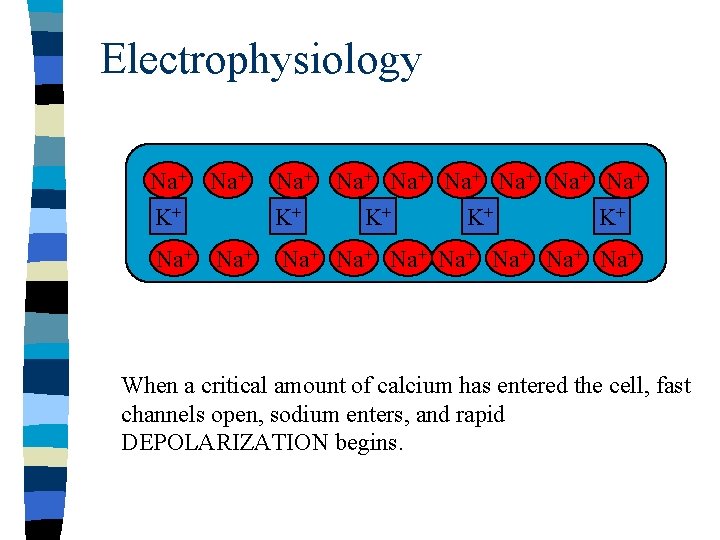
Electrophysiology Na+ K+ Na+ Na+ K+ K+ Na+ Na+ Na+ When a critical amount of calcium has entered the cell, fast channels open, sodium enters, and rapid DEPOLARIZATION begins.

Electrophysiology n Electrical impulse from depolarizing pacemaker cell spreads to working myocardial cells and stimulates them. Depolarization and contraction result.
Electrophysiology The SA Node is the heart’s primary pacemaker WHY?
Electrophysiology If the SA Node does not fire, what site will take over? What will happen to the heart rate?
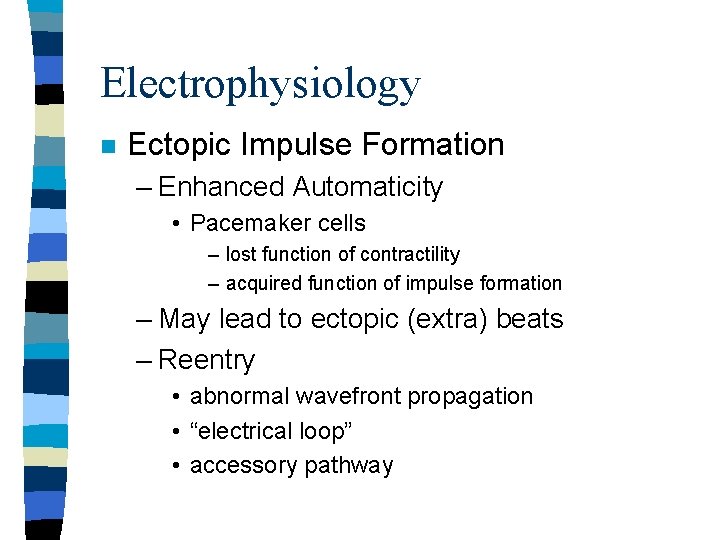
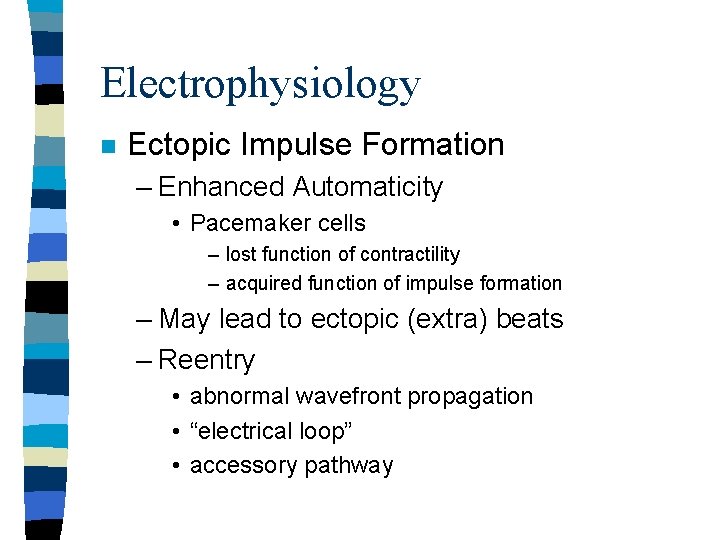
Electrophysiology n Ectopic Impulse Formation – Enhanced Automaticity • Pacemaker cells – lost function of contractility – acquired function of impulse formation – May lead to ectopic (extra) beats – Reentry • abnormal wavefront propagation • “electrical loop” • accessory pathway

Effects of ANS on Electrophysiology n n n Medulla Carotid Sinus and Baroreceptors Parasympathetic Nervous System – Acetylcholine – Cholinesterase n Sympathetic Nervous System – Alpha – Beta • Inotropic effect • Dromotropic effect • Chronotropic effect
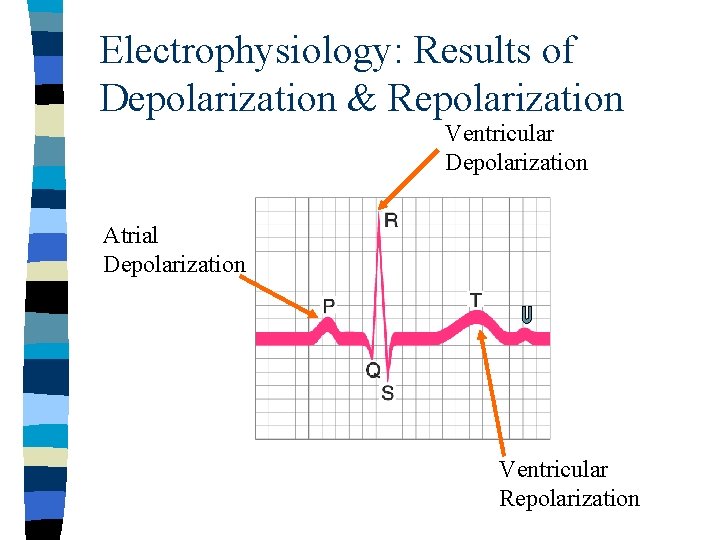
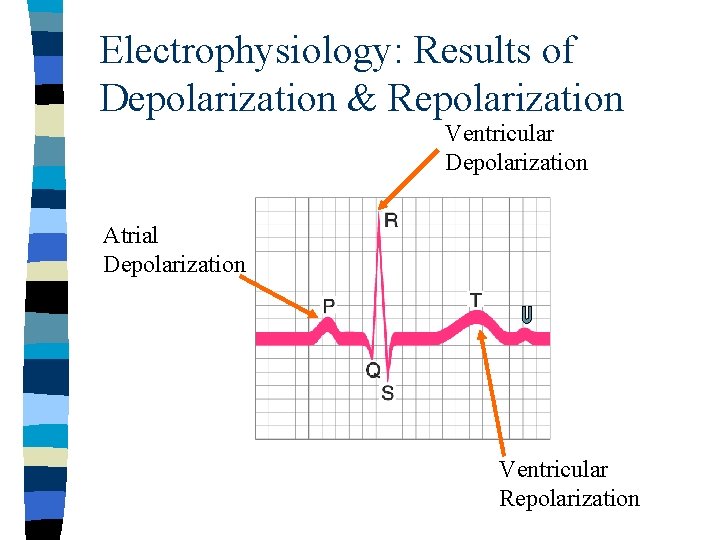
Electrophysiology: Results of Depolarization & Repolarization Ventricular Depolarization Atrial Depolarization Ventricular Repolarization
 The emtp quiz
The emtp quiz Westcliffe cardiology shipley
Westcliffe cardiology shipley Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn
Accp cardiology prn Acc sports cardiology
Acc sports cardiology Service line strategy
Service line strategy Egsys
Egsys Muse cardiology
Muse cardiology Elias hanna cardiology
Elias hanna cardiology Craig ainsworth cardiology
Craig ainsworth cardiology Hall-garcia cardiology associates
Hall-garcia cardiology associates Enloe cardiology
Enloe cardiology Inculprate
Inculprate Dicom structured reporting
Dicom structured reporting Accp cardiology prn journal club
Accp cardiology prn journal club Two voice poem examples funny
Two voice poem examples funny Ellen white biography
Ellen white biography Vance jennings
Vance jennings Terry goh
Terry goh Terry stop
Terry stop Terry
Terry Maya nazon
Maya nazon Terry fox elementary school
Terry fox elementary school Pengertian pengambilan keputusan menurut george r terry
Pengertian pengambilan keputusan menurut george r terry Terry laster
Terry laster Robot drag race
Robot drag race Terry eagleton what is a novel
Terry eagleton what is a novel Kaley jay terry
Kaley jay terry Terry betts
Terry betts Terry hayes md
Terry hayes md Dr terry weaver
Dr terry weaver Finally, it has arrived
Finally, it has arrived Intermediate math problems for students by m. colwell
Intermediate math problems for students by m. colwell Dr terry correll
Dr terry correll Terry tadlock
Terry tadlock Terry biddington
Terry biddington Chapter 26 milady review questions
Chapter 26 milady review questions Terry howerton
Terry howerton Maggie strus
Maggie strus Parrot ate the guava as it was ripe identify the ambiguity
Parrot ate the guava as it was ripe identify the ambiguity Viessmann manufacturing company
Viessmann manufacturing company Terry fox essay
Terry fox essay The man behind the moon by shelton pacer genre
The man behind the moon by shelton pacer genre Loop #2 of hill’s generic strategy framework
Loop #2 of hill’s generic strategy framework Nttml
Nttml Terry gage
Terry gage Freddie mercury testamento
Freddie mercury testamento Ken wilber terry killam
Ken wilber terry killam Terry landscaping & lawn care
Terry landscaping & lawn care Terry goh singapore
Terry goh singapore Dasar dasar pengambilan keputusan menurut george r terry
Dasar dasar pengambilan keputusan menurut george r terry