InHome Therapy IHT Overview Performance Specifications Medical Necessity












- Slides: 66
In-Home Therapy (IHT) • Overview • Performance Specifications • Medical Necessity Criteria on MCE website • Anne Pelletier-Parker – Massachusetts Behavioral Health Partnership CBHI Services Kickoff Meeting September 9, 2009 1

In-Home Therapy Services In Home Therapy Services is a structured, consistent, strength-based therapeutic relationship between a licensed clinician and the youth and family for the purpose of treating the youth’s behavioral health needs. Services are delivered by one or more members of a team consisting of professional and paraprofessional staff, offering a combination of medically necessary: In-Home Therapy & CBHI Services Kickoff Meeting Therapeutic Training and Support. September 9, 2009 2
In-Home Therapy Services • Enhance and improve the family’s capacity to improve the youth’s functioning in the home and community. • Prevent the need for the youth’s admission to an inpatient hospital, psychiatric residential treatment facility or other treatment setting. CBHI Services Kickoff Meeting September 9, 2009 3
The In-Home Therapy Services provider: • operates from 8 a. m. to 8 p. m seven days per week, 365 days per year; • has 24 -hour urgent response 365 days a year; • responds to all referrals telephonically within one business day; • responds to referrals during daytime operating hours by offering a face-to-face encounter within 24 hours. • engages in assertive outreach regarding engaging in the service • engages and supports the ESP/Mobile Crisis Intervention team in an emergency. CBHI Services Kickoff Meeting September 9, 2009 4
In Home Therapy Services may be provided in any setting where the youth is naturally located, including, but not limited to, the home (including foster homes and therapeutic foster homes), schools, child care centers, respite settings, other community settings. CBHI Services Kickoff Meeting September 9, 2009 5
Intake In-Home Therapy Services provider participates in discharge planning at the referring provider location; makes every effort to meet at the time of referral or as soon as possible if the referral is initiated by the MCI Team as a diversion from out of home placement or psychiatric hospitalization; will visit the youth and family in any safe setting within 24 hours of referral from an inpatient unit, CBAT, Crisis Stabilization or Mobile Crisis Team; completes an initial, or updates an existing, risk management/safety plan during intake. CBHI Services Kickoff Meeting September 9, 2009 6
Initial Assessment The In-Home Therapy Services provider completes an initial assessment within 24 hours of meeting with the youth and family. Assessment includes: • main need /focal problem, • contributing factors to the main need from multiple life domains, • matching interventions with an emphasis on youth/family interactions and skill building. The In-Home Therapy Services provider completes the age appropriate CANS-MA version within 48 hours of the initial contact. CBHI Services Kickoff Meeting September 9, 2009 7
Treatment Planning & Documentation The In-Home Therapy Services provider, in consultation with the youth, the parent(s)/guardian(s)/caregiver(s), IHT supervisors, other involved treaters, and the IHT multidisciplinary team, completes an evidence-based/best-practice guided treatment plan, including a risk management/safety plan, within seven (7) calendar days of first contact. All parties involved, including the youth, sign the treatment/care plan. The In-Home Therapy Treatment Plan: is solution-focused; clearly defines interventions; includes measurable outcomes; assists the youth and family members in their environment to help the youth to achieve and maintain stabilization; is synchronized with other provider’s existing plans. CBHI Services Kickoff Meeting September 9, 2009 8
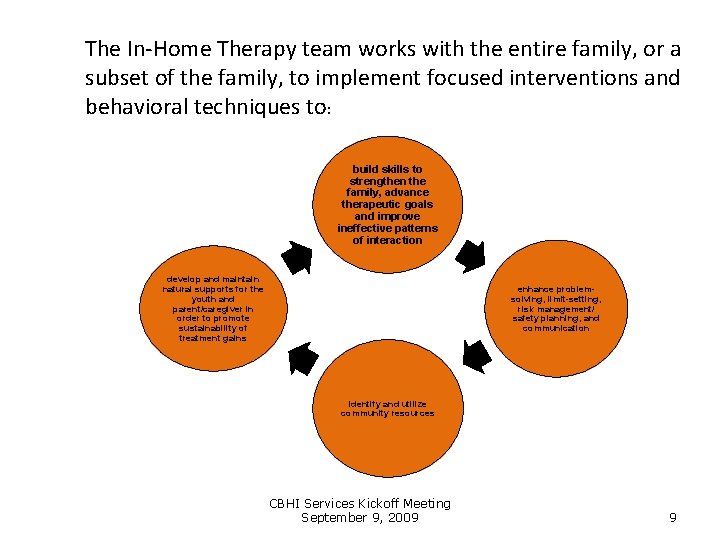
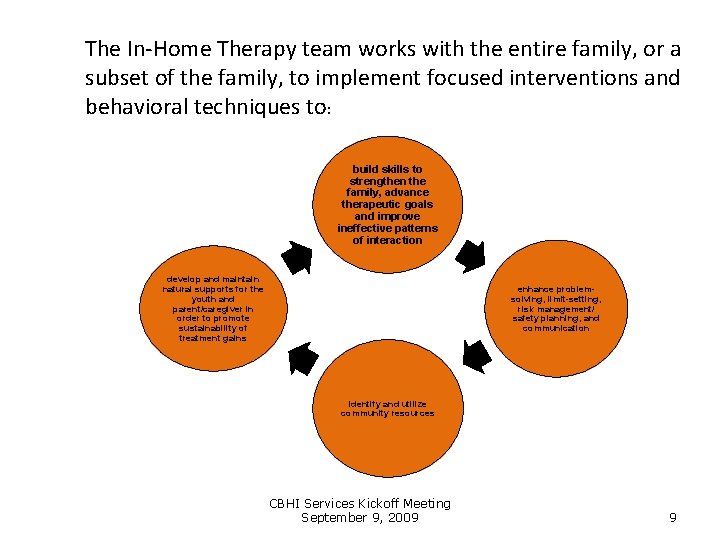
The In-Home Therapy team works with the entire family, or a subset of the family, to implement focused interventions and behavioral techniques to: build skills to strengthen the family, advance therapeutic goals and improve ineffective patterns of interaction develop and maintain natural supports for the youth and parent/caregiver in order to promote sustainability of treatment gains enhance problemsolving, limit-setting, risk management/ safety planning, and communication identify and utilize community resources CBHI Services Kickoff Meeting September 9, 2009 9
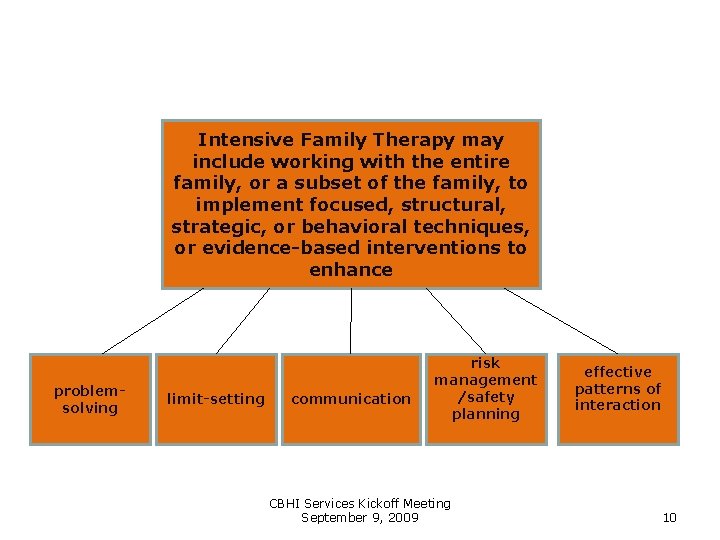
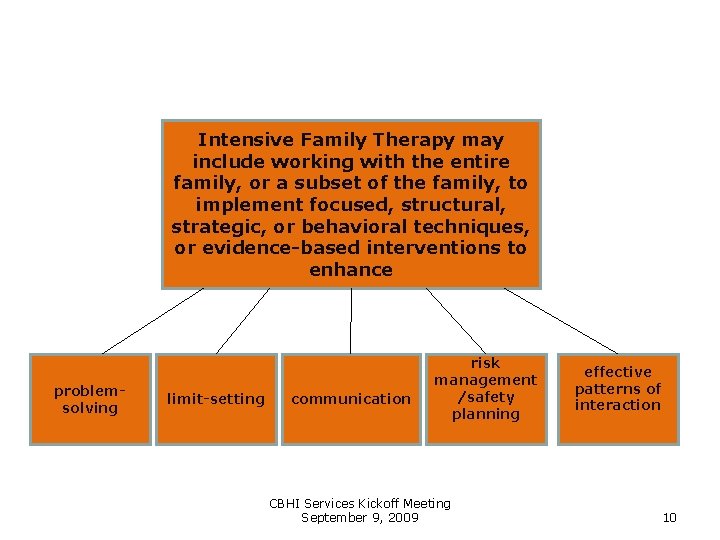
Intensive Family Therapy may include working with the entire family, or a subset of the family, to implement focused, structural, strategic, or behavioral techniques, or evidence-based interventions to enhance problemsolving limit-setting communication risk management /safety planning CBHI Services Kickoff Meeting September 9, 2009 effective patterns of interaction 10

Therapeutic Training & Support TT & S is provided by a qualified paraprofessional working under the supervision of a clinician to support implementation of the licensed clinician’s treatment plan to assist the youth and family in achieving the goals of that plan. The paraprofessional assists the clinician in implementing therapeutic objectives of the treatment plan designed to address the youth’s mental health, behavioral and emotional needs. CBHI Services Kickoff Meeting September 9, 2009 Teaches the youth to understand, direct, interpret, manage, and control feelings and emotional responses to situations and to assist the family to address the youth’s emotional and mental health needs. 11
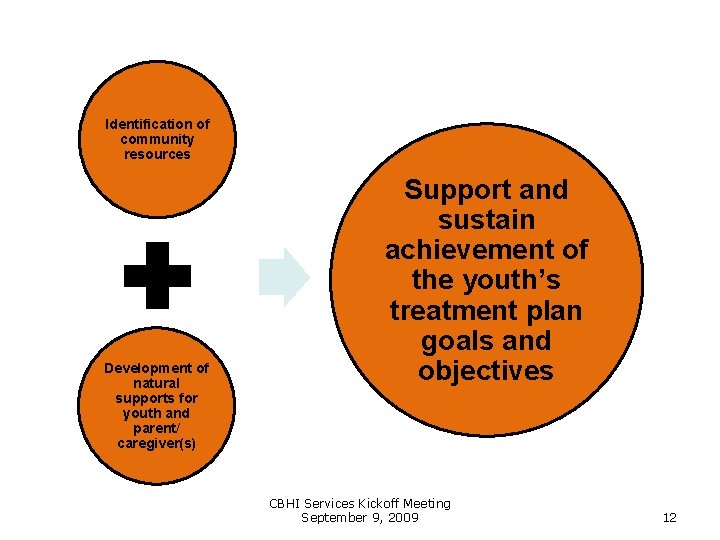
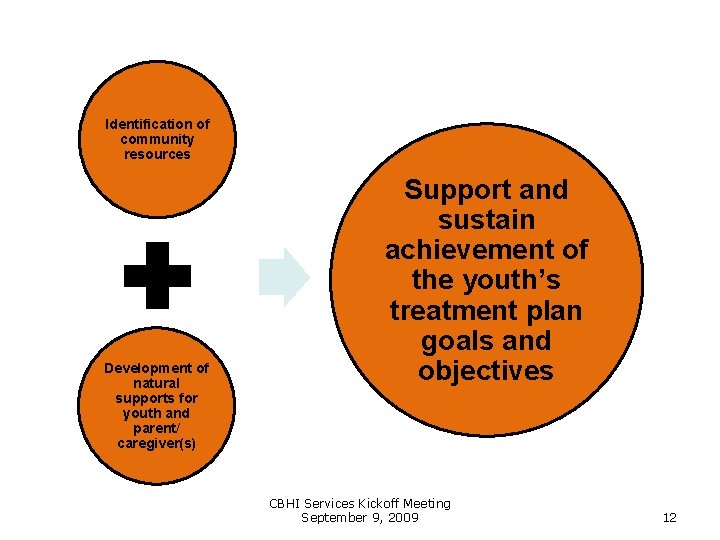
Identification of community resources Development of natural supports for youth and parent/ caregiver(s) Support and sustain achievement of the youth’s treatment plan goals and objectives CBHI Services Kickoff Meeting September 9, 2009 12
Staffing The In-Home Therapy Services team employs a multidisciplinary model, with both professionals trained in working with youth and their families, and paraprofessional staff capable of providing family members with therapeutic support for behavioral health needs. Staff are knowledgeable about: available community mental health and substance use disorder services within their natural service area, the levels of care, relevant laws and regulations, Systems of Care philosophy and Wraparound planning process, medical, legal, emergency, and community services available to the youth and family. CBHI Services Kickoff Meeting September 9, 2009 13
Staff Supervision & Consultation The In-Home Therapy Services provider ensures that a licensed, master’s level, senior clinician provides supervision commensurate with licensure level and consistent with credentialing criteria to professional and paraprofessional staff on a weekly basis. A board-certified or board-eligible child psychiatrist or a child-trained Psychiatric Nurse Mental Health Clinical Specialist is available during normal business hours within one (1) hour for consultation related to treatment planning, medication concerns, and crisis intervention. A senior-level, licensed clinician trained in working with youth is available to the staff and the supervisor 24 hours a day, seven days a week for consultation as needed. CBHI Services Kickoff Meeting September 9, 2009 14
Discharge Planning and Documentation A discharge planning meeting is scheduled whenever the authorized decision maker decides that services are no longer desired, or the family, determines that the youth has met his/her goals and no longer needs the service, or the youth no longer meets the medical necessity criteria for In-Home Therapy. Discharge plan includes, at minimum: identification of the youth’s needs according to life domains, a list of services that are in place post-discharge and providers arranged to deliver each service, – a list of prescribed medications, dosages, and possible side effects, treatment recommendations consistent with the service plan of any involved state agency. CBHI Services Kickoff Meeting September 9, 2009 15
Eligibility • All Mass. Health benefit plans CBHI Services Kickoff Meeting September 9, 2009 16
FST enhanced and expanded to IHT • For Mass. Health, FST is being enhanced, expanded, and renamed In-Home Therapy • Mass. Health will no longer purchase FST beginning 11/1/2009 • FST will remain a viable service for the non. Mass. Health population depending on specific insurer CBHI Services Kickoff Meeting September 9, 2009 17
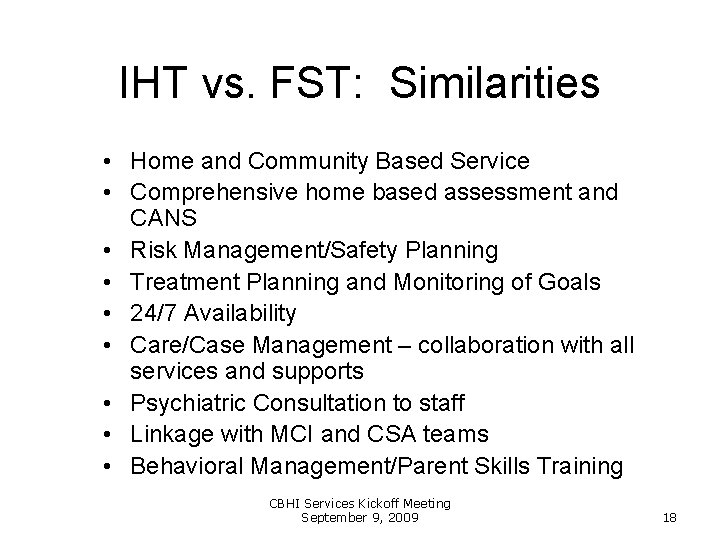
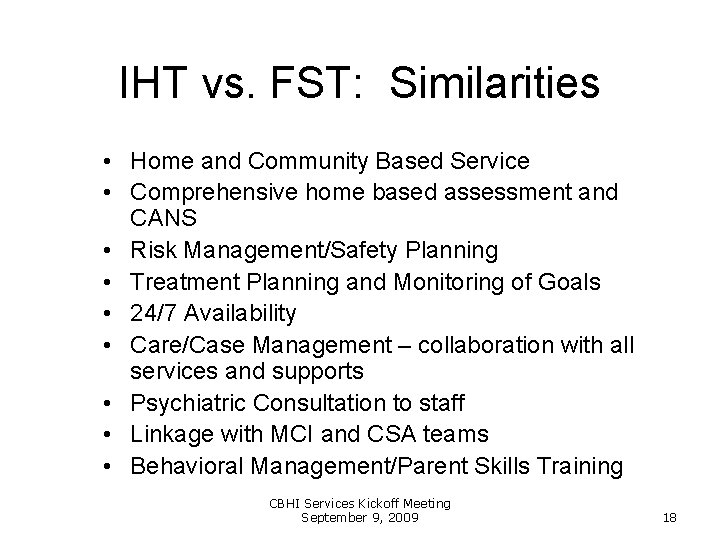
IHT vs. FST: Similarities • Home and Community Based Service • Comprehensive home based assessment and CANS • Risk Management/Safety Planning • Treatment Planning and Monitoring of Goals • 24/7 Availability • Care/Case Management – collaboration with all services and supports • Psychiatric Consultation to staff • Linkage with MCI and CSA teams • Behavioral Management/Parent Skills Training CBHI Services Kickoff Meeting September 9, 2009 18
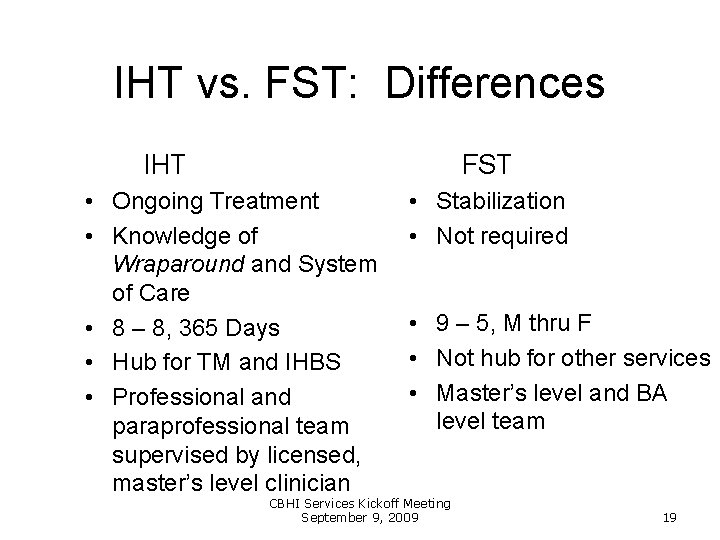
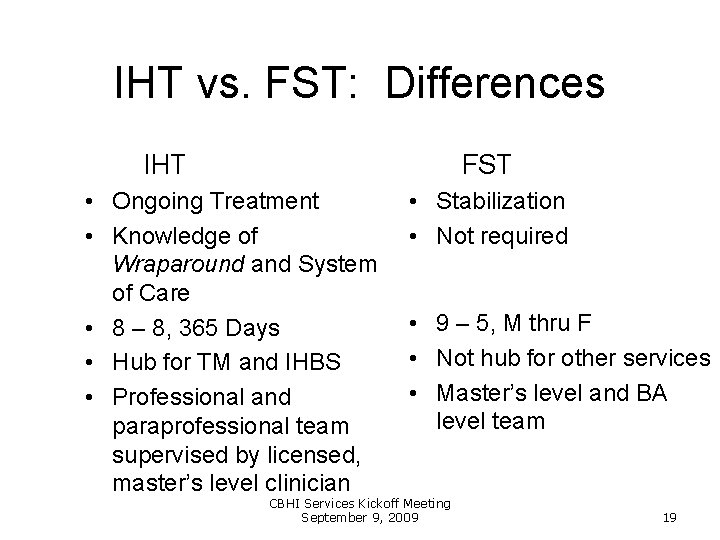
IHT vs. FST: Differences IHT FST • Ongoing Treatment • Knowledge of Wraparound and System of Care • 8 – 8, 365 Days • Hub for TM and IHBS • Professional and paraprofessional team supervised by licensed, master’s level clinician • Stabilization • Not required • 9 – 5, M thru F • Not hub for other services • Master’s level and BA level team CBHI Services Kickoff Meeting September 9, 2009 19
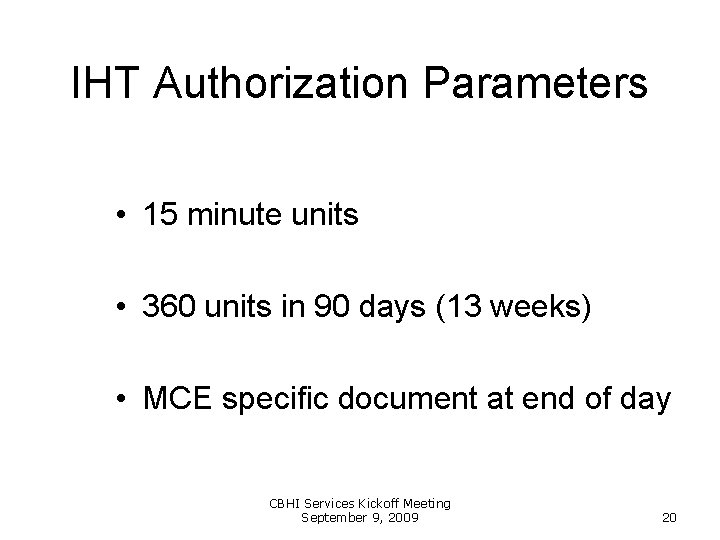
IHT Authorization Parameters • 15 minute units • 360 units in 90 days (13 weeks) • MCE specific document at end of day CBHI Services Kickoff Meeting September 9, 2009 20
In-Home Therapy Services Worcester, Massachusetts September 9, 2009 Rick Shepler, Ph. D. , PCC-S Center for Innovative Practices a part of the Institute for the Study and Prevention of Violence Kent State University All materials copyrighted 2009, Richard Shepler, Ph. D 21

In-Home Therapy • Either a Master’s level clinician or a team approach • Intensive family therapy in the home or other community/natural setting to: – Enhance problem-solving, limit-setting communication – Build skills to strengthen the family – Identify and utilize community resources – Develop and maintain natural supports – Risk management/safety planning All materials copyrighted 2009, Richard Shepler, Ph. D 22
In-Home Therapy, con’t • Includes: – Assessment (comprehensive home-based, inclusive of – – – CANS) Development of a youth- and family-centered treatment plan Intensive Family Therapy Coaching Skills training Referral and linkage Identification of community resources and development of natural supports • Available to Mass. Health enrolled youth All materials copyrighted 2009, Richard Shepler, Ph. D 23
In-Home Therapy (IHT): Pivotal service in a comprehensive system of care • IHT expands the continuum of care to increase the availability of the less restrictive service options for youth at-risk of out-of-home placement due to issues related to his or her mental health All materials copyrighted 2009, Richard Shepler, Ph. D 24
Continuum of Service Intensity • A continuum of intensity based on mental health needs of the youth • Opens up range of youth to be served All materials copyrighted 2009, Richard Shepler, Ph. D 25
Typical Youth/Family Served • Youth with serious emotional challenges with functional impairments • Youth at-risk of placement or have significant safety issues • Youth with multiple system involvement • System has not engaged youth and family effectively All materials copyrighted 2009, Richard Shepler, Ph. D 26

Typical Youth Served • Multiple risk factors • Few protective factors • Skill set deficits: e. g. problem solving; communication; emotional regulation • Youth who need additional supports, active facilitation, and accommodations for success (school, home, community) All materials copyrighted 2009, Richard Shepler, Ph. D 27
Parents and Families • High in stressors – Low in resources and supports • High family conflict • Current parenting skill set unsuccessful in dealing with youth's mental health needs • Trust issues with the “system” • Difficulty with service access (work, transportation, poverty) All materials copyrighted 2009, Richard Shepler, Ph. D 28
IHT Benefits: Youth and Families • Reduced out of home placements • Mental health stabilization • Family Stability • Reduced involvement in Juvenile Justice System • Increased school success All materials copyrighted 2009, Richard Shepler, Ph. D 29
IHT Benefits: Other Systems • IHT actively assesses and manages risk and safety concerns • Cost savings to other systems • Increases positive outcomes for other childserving systems (school success; decreased arrest rates, decreased abuse and neglect, etc. ) All materials copyrighted 2009, Richard Shepler, Ph. D 30
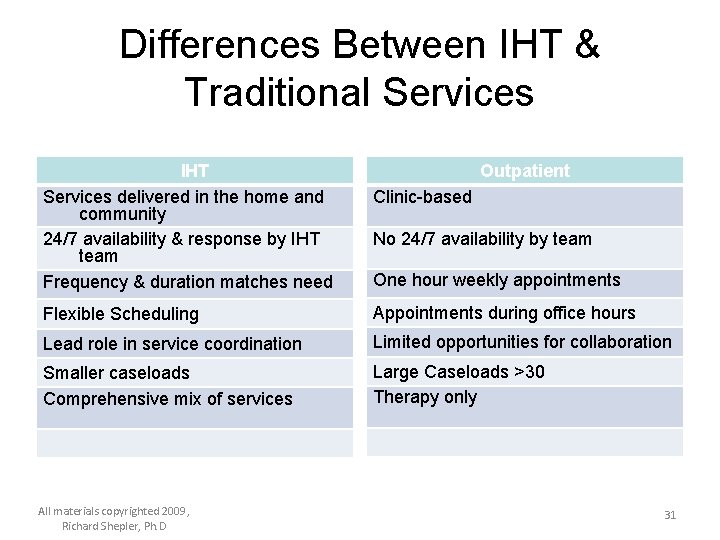
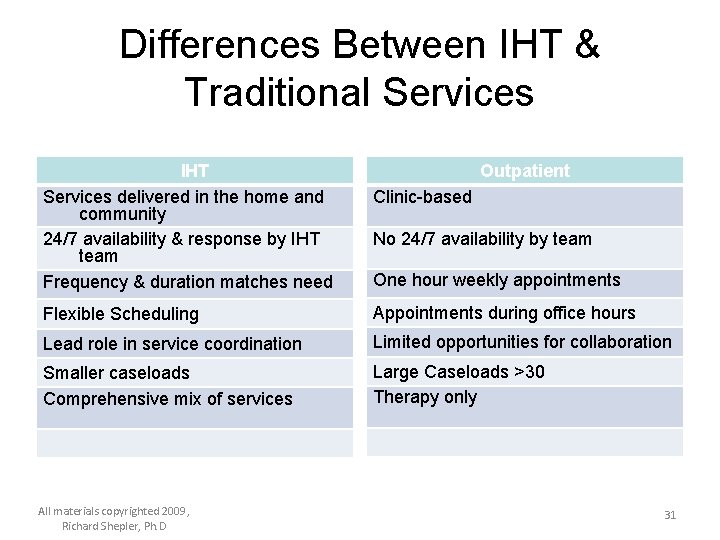
Differences Between IHT & Traditional Services IHT Services delivered in the home and community 24/7 availability & response by IHT team Frequency & duration matches need Outpatient Clinic-based No 24/7 availability by team One hour weekly appointments Flexible Scheduling Appointments during office hours Lead role in service coordination Limited opportunities for collaboration Smaller caseloads Comprehensive mix of services Large Caseloads >30 Therapy only All materials copyrighted 2009, Richard Shepler, Ph. D 31
IHT: Key Components 1. 2. 3. 4. 5. 6. 7. Access and availability Eco-systemic assessment and intervention Intensity of service matches family need Active risk management and safety planning Active intervention monitoring Active support to family Respectful and culturally mindful engagement 8. Cross-system collaboration and advocacy 9. Supervisor availability and team consultation All materials copyrighted 2009, Richard Shepler, Ph. D 32

IHT: Service of Access • Service delivered where the youth lives and functions: home, school, and community at times that are convenient to the family • Access to information – Family dynamics and interactional patterns – Recovery environments • Access to people – – – Family School Court Community Informal supports • Access for interventions: implemented where behaviors occur All materials copyrighted 2009, Richard Shepler, Ph. D 33
Ecosystemic Assessment and Intervention • Behavioral health interventions that impact the youth in context of his or her functional environments – Home – School – Peers – Community All materials copyrighted 2009, Richard Shepler, Ph. D 34
Intensity of Service Matches Family Need • Based on youth and family need and functional impairment • Caseload size should reflect program intensity: The greater the need the greater intensity the smaller the caseload All materials copyrighted 2009, Richard Shepler, Ph. D 35
Active Risk Management & Safety Planning • Active risk management; safety assessment, planning and monitoring • Family is involved and informed • 24/7 on call: The In-Home Therapy Services provider has 24 hour urgent response accessible by phone to the youth and family, 365 days a year. • Immediate crisis response from In-Home Therapists with face to face response as needed All materials copyrighted 2009, Richard Shepler, Ph. D 36

Active Intervention Monitoring • IHT actively monitors interventions • Treatment persistence All materials copyrighted 2009, Richard Shepler, Ph. D 37
Active Supports • Resource poor and resource drained families • Pile up of stressors and life circumstances • Need active system support until we can re-build informal supports All materials copyrighted 2009, Richard Shepler, Ph. D 38
Respectful and Culturally Mindful Engagement • Appreciative perspective: Families are doing the best they can do, at any given time, given their current capacities and abilities, and life circumstances. • Strengths and Culture Discovery (Van. Den. Berg): IHT providers strive to understand appreciate the family’s values, culture, strengths, and life realities. • Validation and Valuing: The youth and family are validated for their courage, efforts, and persistence, knowing that progress is sometimes very difficult, and that “hanging in there” is sometimes all that is possible at any given point in a family’s life. (Resiliency Ohio, 2008) All materials copyrighted 2009, Richard Shepler, Ph. D 39

Partnering with Youth & Families • The whole is greater than the sum of its parts. Working together accomplishes more than working apart • We need to pool our resources and expertise • Mutual Expertise: Youth and families are experts on their lives and you are an expert in your field. • Engage parents and young adults in transition as coconsultants All materials copyrighted 2009, Richard Shepler, Ph. D 40
IHT Lessons Learned: Engagement • Mutual assessment process: youth and families are assessing us as we are assessing them • Misinterpreting a family’s self protection as resistance • Public testimony versus private testimony All materials copyrighted 2009, Richard Shepler, Ph. D 41
Cross-system Collaboration and Advocacy • Pro-active cross-system collaboration and service coordination • Skillful advocacy efforts are promoted to assist with accommodations and system navigation - while respecting other childserving system’s mandates All materials copyrighted 2009, Richard Shepler, Ph. D 42
Supervisory Support, Availability and Team Consultation • Access and availability for IHT staff when needed • Pro-active consultation and strong clinical support • Supervisor should have a designated responsibility to the team All materials copyrighted 2009, Richard Shepler, Ph. D 43
Phases of Home-based Intervention Engagement and Assessment • Engagement (youth, family, & collaborative partners) • Risk Management and Safety Planning • Assessment Treatment • Individual and family treatments and supports • Skill Building, Skill Consolidation, and Generalization Enhancement of Positive Support Network • Linkages, Closure, & Follow-up Discharge • In Ohio the average LOS for Intensive Home-Based Treatment is 4. 5 months All materials copyrighted 2009, Richard Shepler, Ph. D 44
Multidimensional Assessment I. Diagnoses: youth who meet the criteria for Mental Health Disorder and related symptom manifestation II. Developmental Functioning: (cognitive, emotional, & behavioral maturity) III. Contextual Functioning: Individual functioning in relevant life domains, including risk and protective factors, and risk and recovery environments IV. Safety Risks: Self and other harm, personal, family, and community safety All materials copyrighted 2009, Richard Shepler, Ph. D 45

Comprehensive Array of Services: IHT Core Services • • Risk management and safety planning Skill building Individual & Family Interventions Cross-System Interventions and Service Coordination • Resource and support building activities All materials copyrighted 2009, Richard Shepler, Ph. D 46
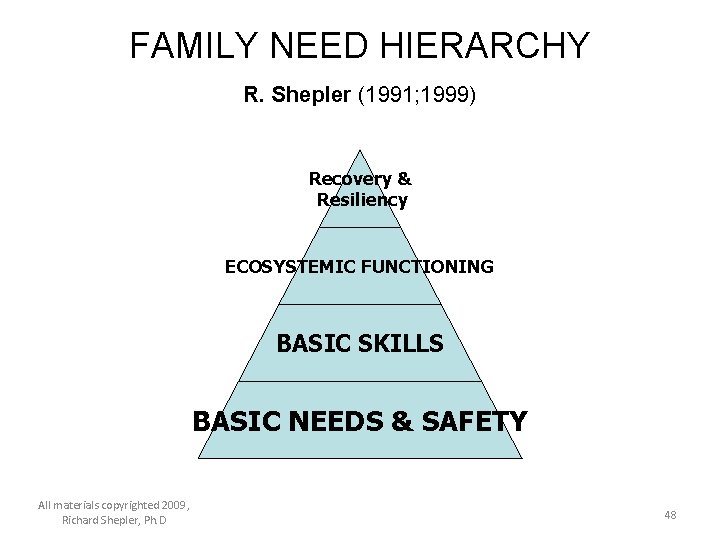
Organizational Framework • Need framework for organizing the myriad of information obtained in the home environment • A family need hierarchy is utilized to assist in assessing and prioritizing the youth’s and family needs • Strategies and interventions are matched to the most salient need, progressing to more complex needs once the primary needs are met All materials copyrighted 2009, Richard Shepler, Ph. D 47
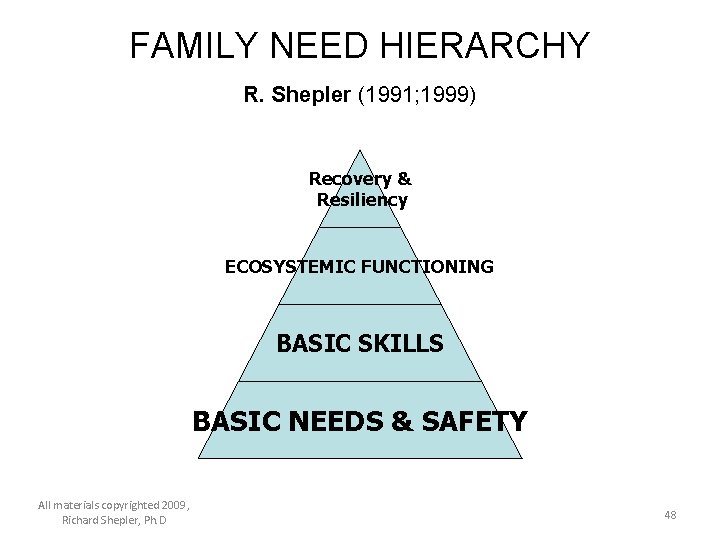
FAMILY NEED HIERARCHY R. Shepler (1991; 1999) Recovery & Resiliency ECOSYSTEMIC FUNCTIONING BASIC SKILLS BASIC NEEDS & SAFETY All materials copyrighted 2009, Richard Shepler, Ph. D 48
Basic Needs, Safety, and Stabilization • Are there material needs that are unmet? (Food; Shelter) • Are there current safety and/or symptom concerns that need stabilization? • Are there significant risk factors that are barriers to recovery? All materials copyrighted 2009, Richard Shepler, Ph. D 49
Basic Needs and Safety (con. ) Ø Assist with basic needs: Active Case Management and Advocacy Ø Establish basic safety: Risk management; safety planning; symptom stabilization Ø Risk reduction: Reduce risk factors and environmental stressors. All materials copyrighted 2009, Richard Shepler, Ph. D 50
Basic Skills • Does the youth and family know how to do what you are asking them to do? • What skills does the youth need to be successful? All materials copyrighted 2009, Richard Shepler, Ph. D 51

Skill Set Development • Emotional regulation skills (CBT; DBT; ART; etc) • Communication skills: individual and family • Conflict management skills: Negotiation, compromise, problem solving skills: conflict resolution; mediation • Self knowledge: Triggers; symptom management • Personal safety skills All materials copyrighted 2009, Richard Shepler, Ph. D 52

Ecosystemic Functioning • What family or system dynamics are barriers to the youth and family’s success? • How well does the youth function in key life domains/ (home, school, peers, community) • Goal: Improve functioning in major life contexts (family, school, community, social, vocational, etc) All materials copyrighted 2009, Richard Shepler, Ph. D 53
Family Context: Set Stage for Change • • • Create family recovery environment Decrease family conflicts Rebuild bonds and relationships Increase positive family communication Increase supervision and monitoring All materials copyrighted 2009, Richard Shepler, Ph. D 54
Community Context: Building Connections • Educate community professionals (schools, juvenile court, children services, etc) on the impacts of mental health challenges • Facilitate reasonable expectations • Facilitate accommodations • Facilitate connections and opportunities All materials copyrighted 2009, Richard Shepler, Ph. D 55
Recovery and Resiliency • What resources and supports are necessary for ongoing growth and development? Ø Ø Ø Ø Empowered parents Supports: informal and formal; for youth and family Positive peers and activities Mentors Pro-social activities Positive connections (School; community) Opportunities to give back Services: • Wraparound process: ICC • Possible step-down services: therapeutic mentoring • Medications; Psychiatrist All materials copyrighted 2009, Richard Shepler, Ph. D 56

IHT Discharge • When to discharge: – Presenting mental health symptoms no longer causing functional impairments – Child no longer at-risk of placement – Safety issues are stabilized – Treatment gains have reached a plateau – Family voice and choice – Youth needs higher level of care for safety – Treatment plan goals have been met All materials copyrighted 2009, Richard Shepler, Ph. D 57
Lessons Learned: IHT Discharge • Common Issues: – Difficult for family to let go of valued service – Pressures from community to remain involved – No viable step-down options – Family crises at termination or as services wind down – There is still lots of work to do • Keep in mind: – Medicaid pays for episodes of treatment – IHT is based on medical necessity and therefore is typically time limited All materials copyrighted 2009, Richard Shepler, Ph. D 58
Common Concerns and Challenges • • • Bugs Contagion Animals Weapons Neighborhoods Distractions: phones; TV; visitors • Getting comfortable so you can do the work • Need to adopt standard safety precautions All materials copyrighted 2009, Richard Shepler, Ph. D 59
Lessons Learned: Managing Challenges • Remember you are a guest in family’s home • You are in control of the mental health service. The family is in control of their home. • Be respectful of the family’s values and culture • Do not demand or challenge. Make simple request if needed. • Relate to the family how the challenging situation affects you and what would be helpful. All materials copyrighted 2009, Richard Shepler, Ph. D 60
Lessons Learned from the Field • • • Engagement is key Confidentiality in the field Reporting obligations Where to do sessions Transporting All materials copyrighted 2009, Richard Shepler, Ph. D 61
Lessons Learned: Administrative Supervision • Don’t let administrative supervision (productivity and paperwork) take time away for clinical supervision and case consultation time • Managing caseloads and LOS • Protecting electronic information – Client communications via internet – Texting • Traveling with information • Managing ethical situations All materials copyrighted 2009, Richard Shepler, Ph. D 62
Lessons Learned: Implementation • Build policies that support the worker: – – – Dedicated supervisor Cell phones Flex-time policies Flex funds when possible Adjusted productivity expectations Policies and trainings that support worker safety , ethics, and burnout • Ongoing coaching and training • Supervisor with previous in-home experience is critical All materials copyrighted 2009, Richard Shepler, Ph. D 63
Lessons Learned: Implementation • Clearly identify the target population and where your service fits into the overall continuum of care in your community • What stakeholders need to be on board…who are the champions and what do they expect • Significant community wide education about the program • Be careful of the overpromise • Identifying and maintaining key referral sources • Plan and budget for turnover All materials copyrighted 2009, Richard Shepler, Ph. D 64
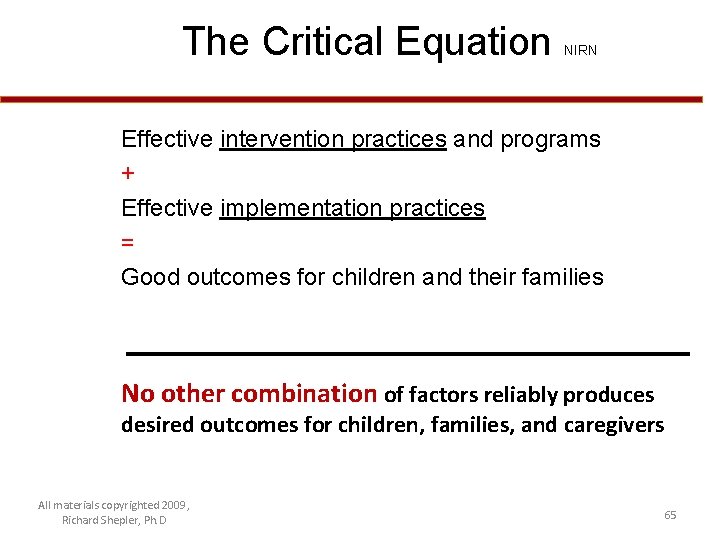
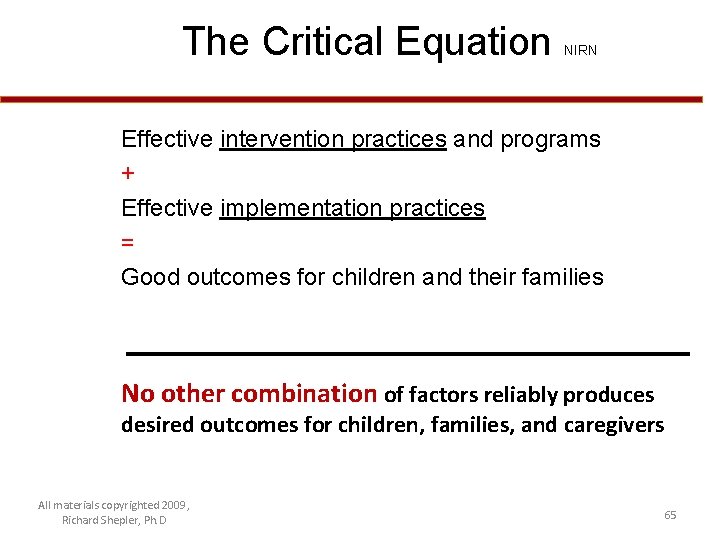
The Critical Equation NIRN Effective intervention practices and programs + Effective implementation practices = Good outcomes for children and their families No other combination of factors reliably produces desired outcomes for children, families, and caregivers All materials copyrighted 2009, Richard Shepler, Ph. D 65

Contact Information • Rick Shepler, Ph. D. , PCC-S 330 -806 -6976 rshepler@kent. edu All materials copyrighted 2009, Richard Shepler, Ph. D 66
 Medical equipment technical specifications
Medical equipment technical specifications Iht spirit system
Iht spirit system Iht werkwijze
Iht werkwijze Tema iht kurikulum 2013
Tema iht kurikulum 2013 Tema iht kurikulum 2013
Tema iht kurikulum 2013 Pengertian iht
Pengertian iht Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system price
Bioness integrated therapy system price What are the major humanistic therapies
What are the major humanistic therapies Chapter 14 medical overview
Chapter 14 medical overview Police necessity
Police necessity Modal verbs of obligation and permission
Modal verbs of obligation and permission Irrigation necessity
Irrigation necessity Chapter 9 modals part 1
Chapter 9 modals part 1 Necessity of fuse
Necessity of fuse Pengertian necessity entrepreneur
Pengertian necessity entrepreneur Expressing ability
Expressing ability What year did george washington attacks ft necessity
What year did george washington attacks ft necessity Business necessity definition
Business necessity definition False necessity trap
False necessity trap Importance of netiquette
Importance of netiquette Dol starter working
Dol starter working May can
May can Medical family therapy
Medical family therapy Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Small bowel obstruction medical nutrition therapy
Small bowel obstruction medical nutrition therapy Drawing up test specifications
Drawing up test specifications Mla format specifications
Mla format specifications Tdot standard specifications
Tdot standard specifications Apwa standards
Apwa standards High level requirements
High level requirements Form-based specifications
Form-based specifications Form-based specifications
Form-based specifications Application specifications
Application specifications Packaging quality assurance
Packaging quality assurance Tos example
Tos example Nao robot specifications
Nao robot specifications Boxn wagon dimensions
Boxn wagon dimensions Eps geofoam specifications
Eps geofoam specifications Tdot standard specifications
Tdot standard specifications Design of trusses
Design of trusses Caltrans 2010 standard specifications
Caltrans 2010 standard specifications Motion specifications in computer graphics
Motion specifications in computer graphics Xml constraints
Xml constraints Spot weld symbol definition
Spot weld symbol definition Jayco sterling 2012
Jayco sterling 2012 Use case specifications
Use case specifications Functional view specification in iot
Functional view specification in iot Transmisi rantai rol
Transmisi rantai rol Kytc standard specifications
Kytc standard specifications Typical primary coil resistance specifications
Typical primary coil resistance specifications Edifact specifications
Edifact specifications Real op amp vs ideal
Real op amp vs ideal Describe the process specification structured decisions.
Describe the process specification structured decisions. Process specification diagram
Process specification diagram A goal of producing process specifications is to
A goal of producing process specifications is to Amba specification
Amba specification Quality control raw materials
Quality control raw materials Tdot standard specifications
Tdot standard specifications Job specifications definition
Job specifications definition Mef specifications
Mef specifications Chlorine railcar
Chlorine railcar Table of specifications bloom's taxonomy
Table of specifications bloom's taxonomy Vce visual communication
Vce visual communication Car specifications explained
Car specifications explained Inspire data specifications
Inspire data specifications