HYPOCALCEMIA Difinition Ionized calcium 4 5 mgd L

- Slides: 45
HYPOCALCEMIA
Difinition • Ionized calcium < 4. 5 mg/d. L; total calcium < 8. 5 mg/d. L if serum protein is normal
Clinical manifestations • The clinical manifestations of hypocalcemia result from increased neuromuscular irritability and include muscle cramps, carpopedal spasm (tetany), weakness, paresthesia, laryngospasm, and seizure-like activity
• Tetany can be detected by the Chvostek sign (facial spasms produced by lightly tapping over the facial nerve just in front of the ear) or by the Trousseau sign (carpal spasms exhibited when arterial blood flow to the hand is occluded for 3 to 5 minutes with a blood pressure cuff inflated to 15 mm Hg above systolic blood pressure).
• Albumin is the major reservoir of protein-bound calcium. • Disorders that alter plasma p. H or serum albumin concentration must be considered when circulating calcium concentrations are being evaluated. • The fraction of ionized calcium is inversely related to plasma p. H; alkalosis can precipitate hypocalcemia by lowering ionized calcium without changing total serum calcium. • Alkalosis may result from hyperpnea caused by anxiety or from hyperventilation related to physical exertion.
• A decrease in albumin concentration of 1 g/dl results in a decrease in protein-bound and hence total calcium concentration of about 0. 8 mg/dl. • Binding of calcium to albumin is strongly p. H-dependent between p. H 7 and p. H 8; an acute increase or decrease in p. H of 0. 1 p. H units will increase or decrease, respectively, protein bound calcium by about 0. 12 mg/dl. • Thus, in hypocalcemic patients with metabolic acidosis, rapid correction of acidemia with sodium bicarbonate can precipitate tetany, due to increased binding of calcium to albumin and a consequent decrease in the ionized calcium concentration.
• Hypoproteinemia may lead to a false suggestion of hypocalcemia because the serum total calcium level is low even though the ionized Ca 2+ remains normal. • It is best to measure serum ionized calcium if hypocalcemia or hypercalcemia is suspected.
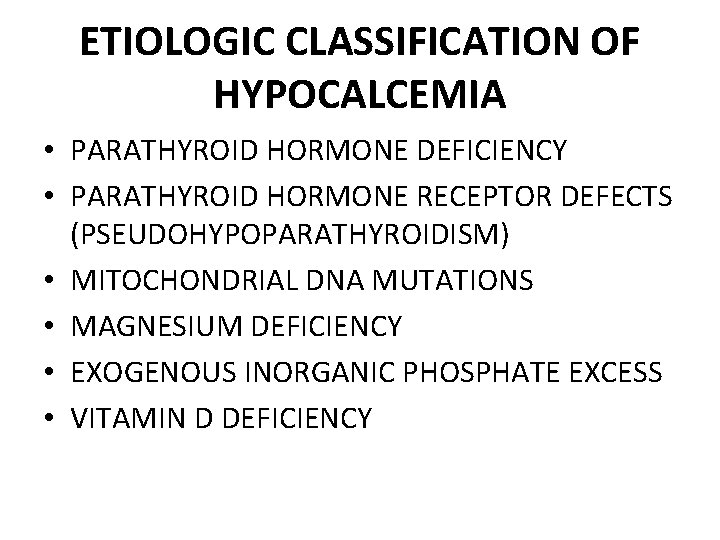
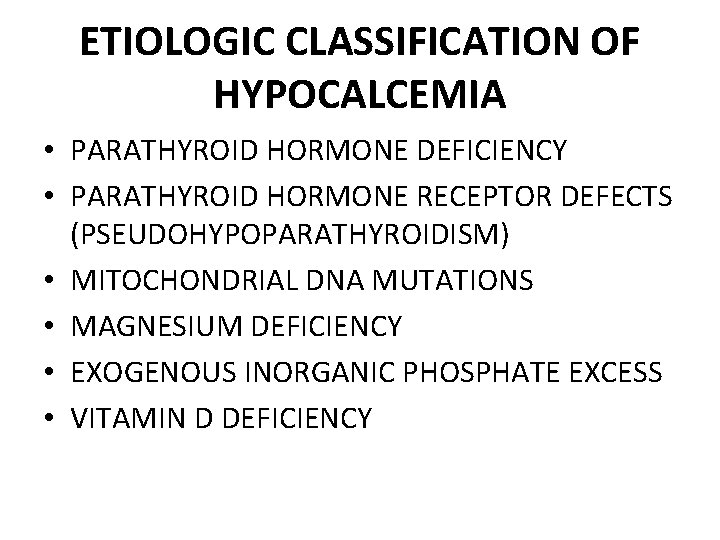
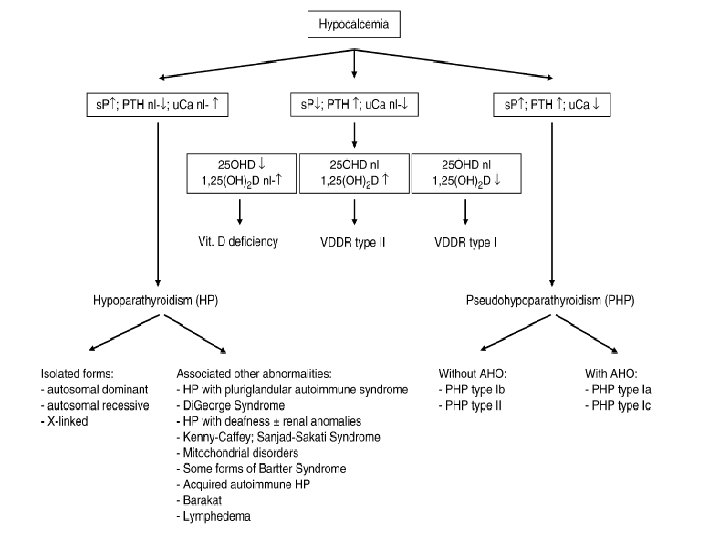
ETIOLOGIC CLASSIFICATION OF HYPOCALCEMIA • PARATHYROID HORMONE DEFICIENCY • PARATHYROID HORMONE RECEPTOR DEFECTS (PSEUDOHYPOPARATHYROIDISM) • MITOCHONDRIAL DNA MUTATIONS • MAGNESIUM DEFICIENCY • EXOGENOUS INORGANIC PHOSPHATE EXCESS • VITAMIN D DEFICIENCY
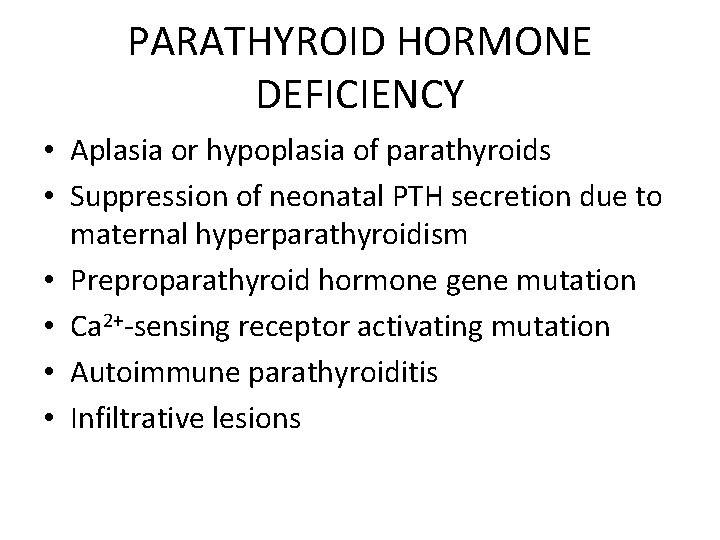
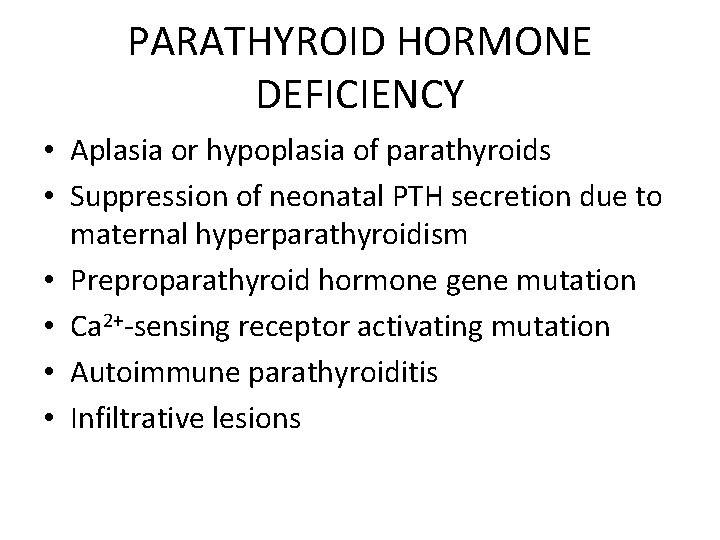
PARATHYROID HORMONE DEFICIENCY • Aplasia or hypoplasia of parathyroids • Suppression of neonatal PTH secretion due to maternal hyperparathyroidism • Preproparathyroid hormone gene mutation • Ca 2+-sensing receptor activating mutation • Autoimmune parathyroiditis • Infiltrative lesions
• Primary hypoparathyroidism causes hypocalcemia, but does not cause rickets.
Etiology of primary hypoparathyroidism • Congenital malformation (e. g. , Di. George syndrome or other complex syndromes) resulting from developmental abnormalities of the third and fourth branchial arches • Surgical procedures, such as thyroidectomy or parathyroidectomy, in which parathyroid tissue is removed either deliberately or as a complication of surgery for another goal • Autoimmunity (autoimmune polyglandular syndrome type 1), which may destroy the parathyroid gland
Pseudohypoparathyroidism • Pseudohypoparathyroidism may occur in one of four forms, all with hypocalcemia and hyperphosphatemia.
Pseudohypoparathyroidism • Type Ia-an abnormality of the Gsα protein linking the PTH receptor to adenylate cyclase; biologically active PTH is secreted in great quantities but does not stimulate its receptor • Type Ib-normal phenotype, normal Gsα with abnormalities in the production of adenylate cyclase • Type Ic-abnormal phenotype, normal production of adenylate cyclase, but a distal defect eliminates the effects of PTH • Type II-normal phenotype, normal production of adenylate cyclase, with a postreceptor defect, close to type Ib
• Pseudohypoparathyroidism is an autosomal dominant condition that may present at birth or later. • Other clinical manifestations of pseudohypoparathyroidism associated with Albright hereditary osteodystrophy include short stature, stocky body habitus, round facies, short fourth and fifth metacarpals, calcification of the basal ganglia, subcutaneous calcification, and, often, developmental delay.
• Albright hereditary osteodystrophy may be inherited separately so that a patient may have a normal appearance with hypocalcemia or may have the Albright hereditary osteodystrophy phenotype with normal serum calcium, phosphate, PTH, and response to PTH.
• During the first 3 days after birth, serum calcium concentrations normally decline in response to withdrawal of the maternal calcium supply via the placenta. • Sluggish PTH response in a neonate may result in a transient hypocalcemia.
• Hypocalcemia caused by attenuated PTH release is found in infants of mothers with hyperparathyroidism and hypercalcemia; the latter suppresses fetal PTH release, causing transient hypoparathyroidism in the neonatal period.
• Normal serum magnesium concentrations are required for normal parathyroid gland function and action. • Hypomagnesemia may cause a secondary hypoparathyroidism, which responds poorly to therapies other than magnesium replacement.
• Neonatal tetany is most often noted in premature or asphyxiated infants and infants of diabetic mothers.
• Excessive phosphate retention, as occurs in renal failure, also produces hypocalcemia.
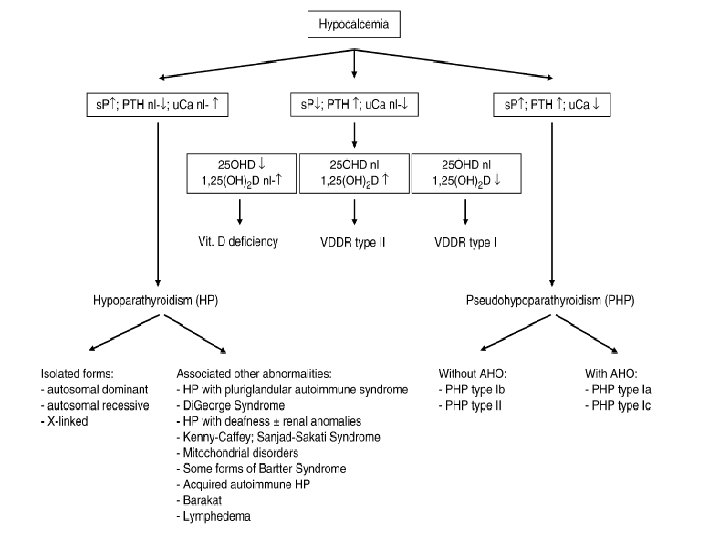
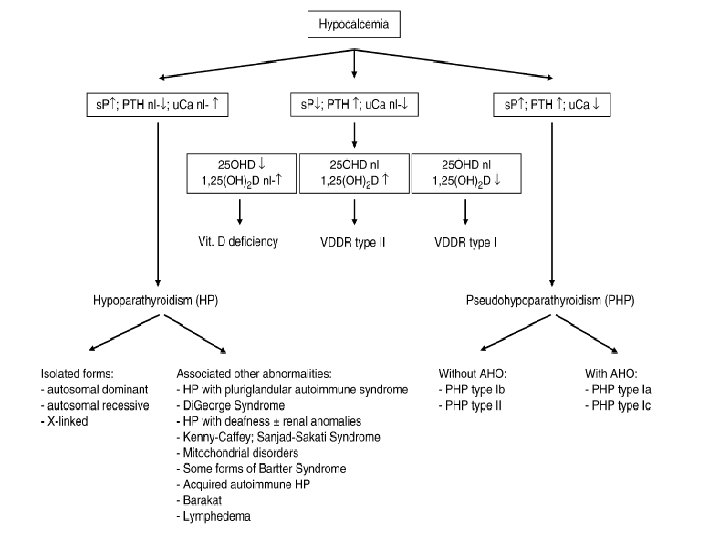
• The etiology of hypocalcemia usually can be discerned by combining features of the clinical presentation with determinations of serum ionized calcium, phosphate, alkaline phosphatase, PTH (preferably at a time when the calcium is low), magnesium, and albumin.
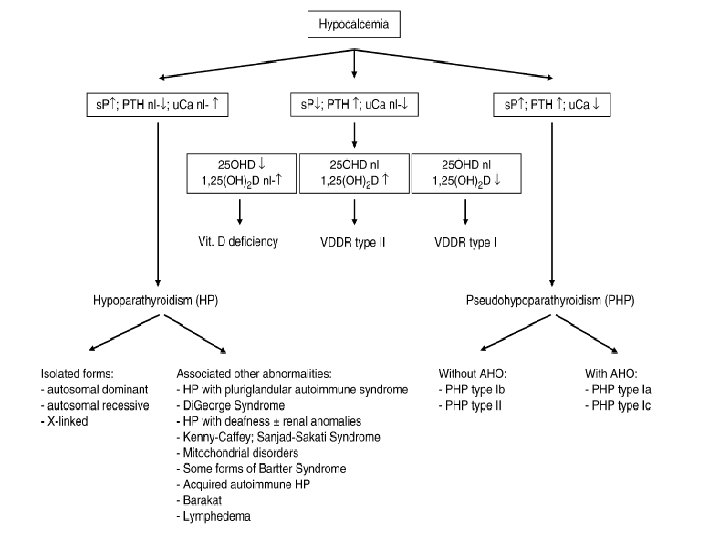
• If the PTH concentration is not elevated appropriately relevant to low serum calcium, hypoparathyroidism (transient, primary, or caused by hypomagnesemia) is present.
• Vitamin D stores can be estimated by measuring serum 25 -hydroxyvitamin D.
• Renal function is assessed by a serum creatinine measurement or determination of creatinine clearance.
Treatment • Treatment of severe tetany or seizures resulting from hypocalcemia consists of intravenous calcium gluconate (1 -2 m. L/kg of a 10% solution) given slowly over 10 minutes, while cardiac status is monitored by electrocardiogram (ECG) for bradycardia, which can be fatal.
• Long-term treatment of hypoparathyroidism involves administering vitamin D, preferably as 1, 25 -dihydroxyvitamin D, and calcium. • Therapy is adjusted to keep the serum calcium in the lower half of the normal range to avoid episodes of hypercalcemia that might produce nephrocalcinosis and to avoid pancreatitis.
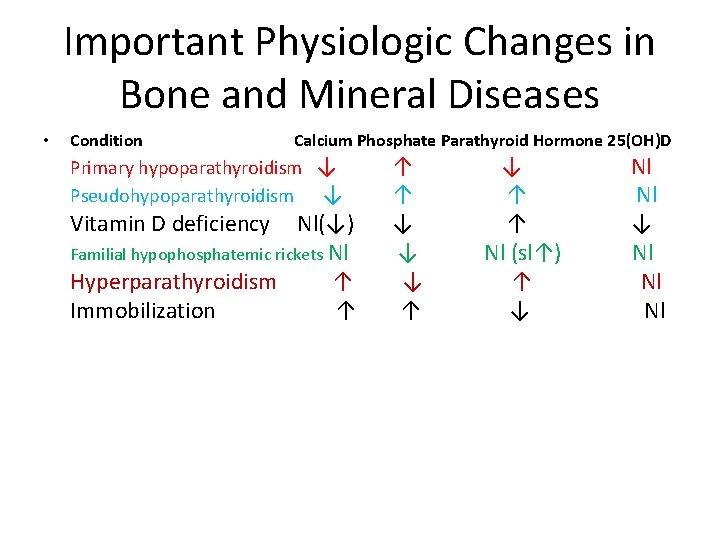
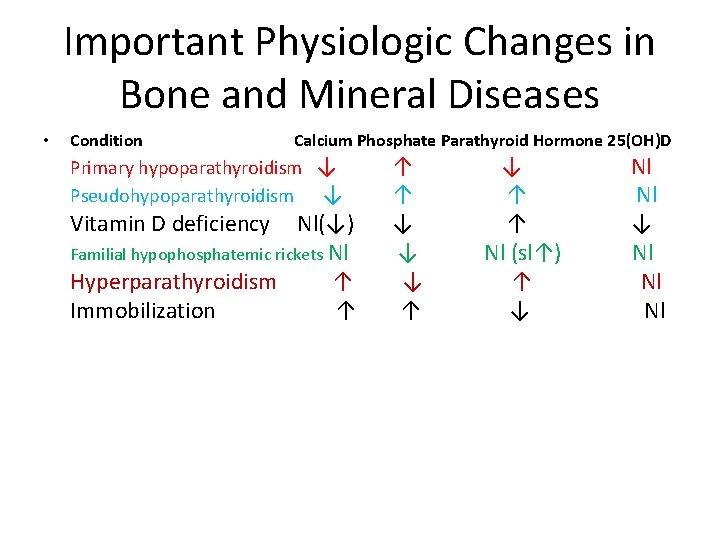
Important Physiologic Changes in Bone and Mineral Diseases • Condition Calcium Phosphate Parathyroid Hormone 25(OH)D Primary hypoparathyroidism ↓ ↑ ↓ Nl Pseudohypoparathyroidism ↓ ↑ Nl Vitamin D deficiency Nl(↓) ↓ ↑ ↓ Familial hypophosphatemic rickets Nl ↓ Nl (sl↑) Nl Hyperparathyroidism ↑ ↓ ↑ Nl Immobilization ↑ ↑ ↓ Nl
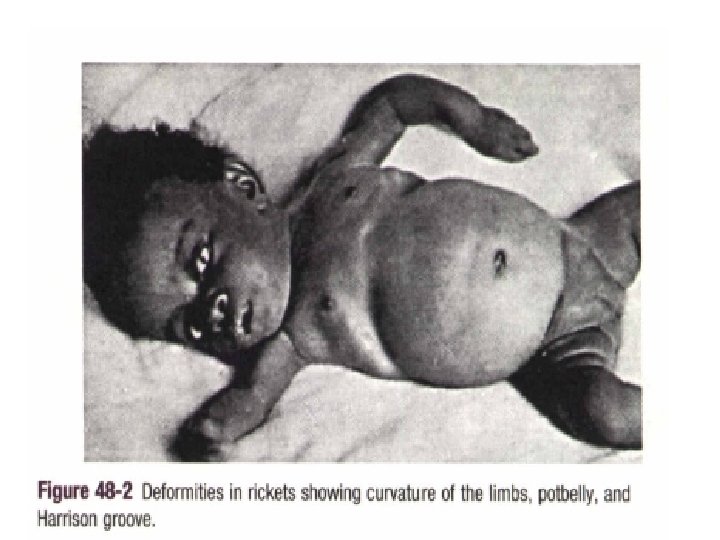
RICKETS • Rickets is defined as decreased or defective bone mineralization in growing children; osteomalacia is the same condition in adults. • The proportion of osteoid (the organic portion of bone) is excessive. • As a result, the bone becomes soft and the metaphyses of the long bones widen.
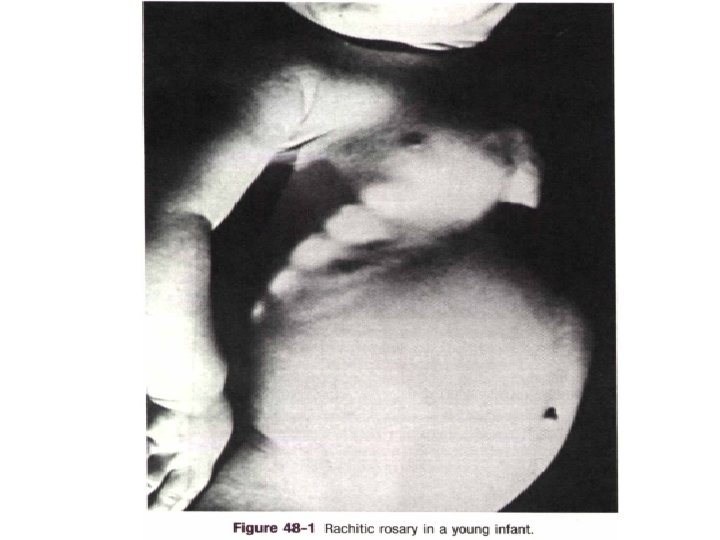
Clinical manifestations • Most manifestations of rickets are due to skeletal changes. • Craniotabes • Rachitic rosary • Growth plate widening is also responsible for the enlargement at the wrists and ankles. • Harrison groove
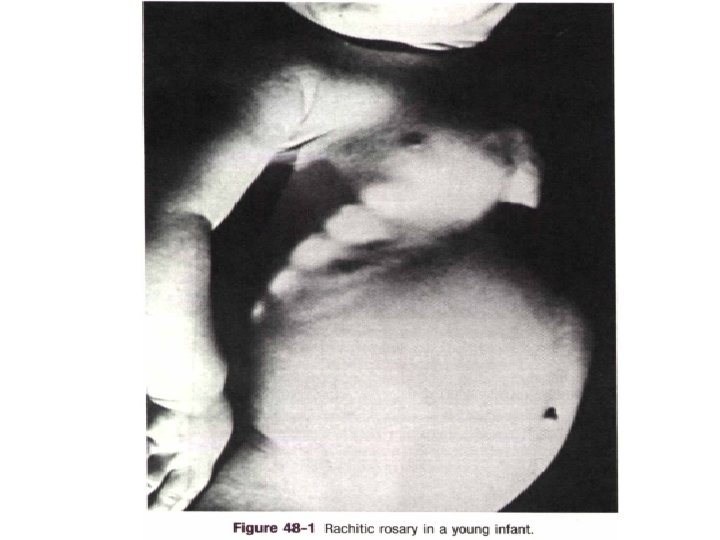
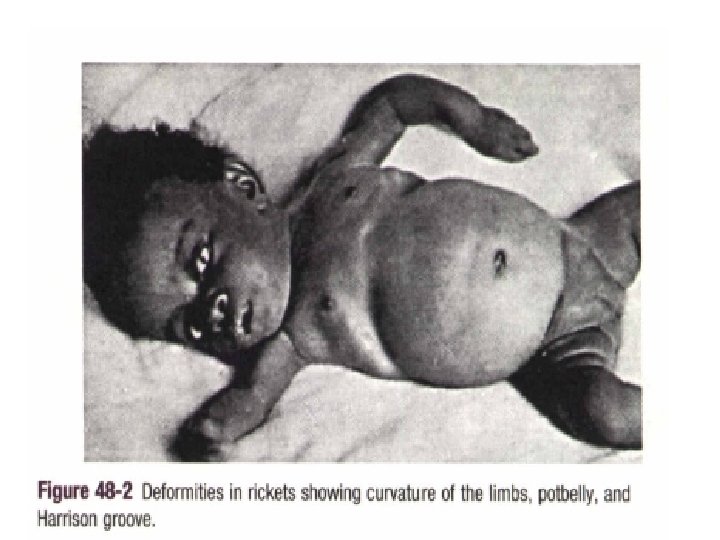

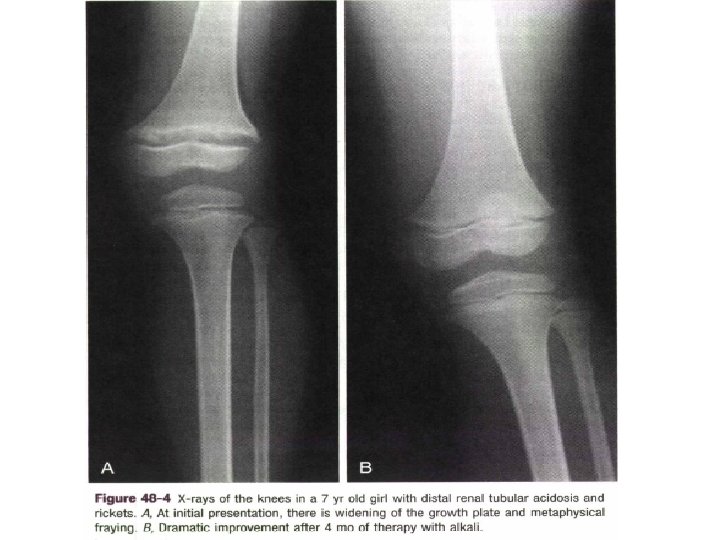
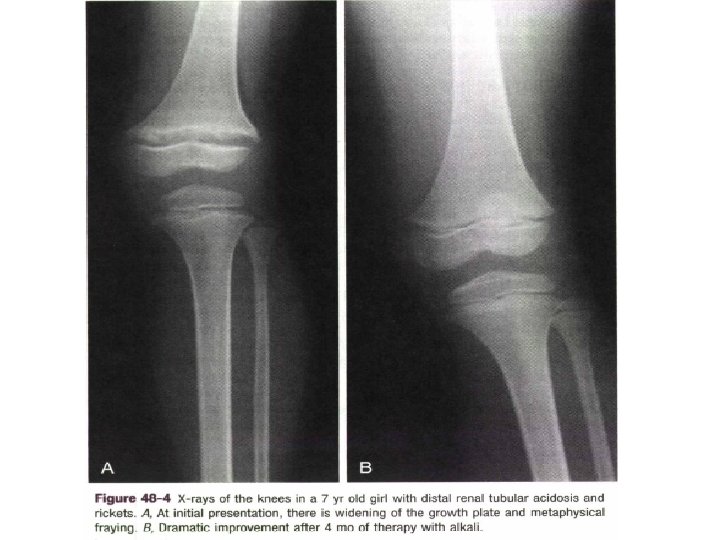
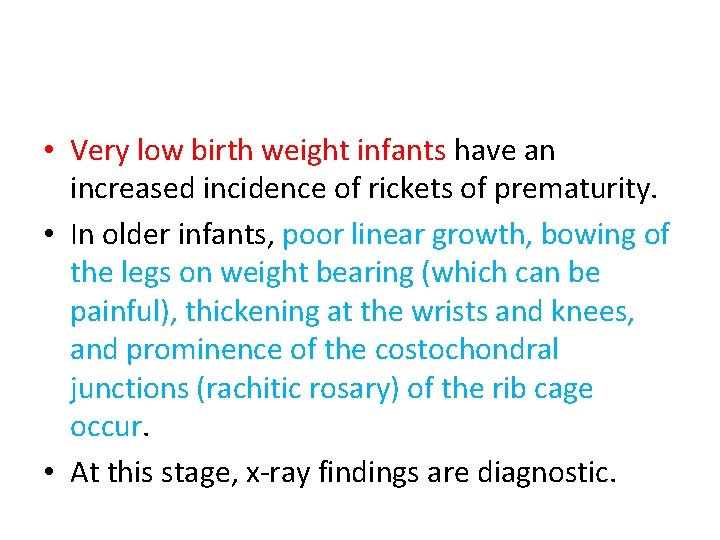
• Very low birth weight infants have an increased incidence of rickets of prematurity. • In older infants, poor linear growth, bowing of the legs on weight bearing (which can be painful), thickening at the wrists and knees, and prominence of the costochondral junctions (rachitic rosary) of the rib cage occur. • At this stage, x-ray findings are diagnostic.
• In nutritional vitamin D deficiency, calcium is not absorbed adequately from the intestine. • Poor vitamin D intake (food fads or poor maternal diet affecting breast milk vitamin D) or avoidance of sunlight in infants exclusively breastfed may contribute to the development of rickets.
• Fat malabsorption resulting from hepatobiliary disease (biliary atresia, neonatal hepatitis) or other causes (cystic fibrosis) also may produce vitamin D deficiency because vitamin D is a fat -soluble vitamin.
• Defects in vitamin D metabolism by the kidney (renal failure, autosomal recessive deficiency of 1α-hydroxylation, vitamin D-dependent rickets) or liver (defect in 25 -hydroxylation) also can cause rickets.
• In familial hypophosphatemic rickets, the major defect in mineral metabolism is failure of the kidney to reabsorb filtered phosphate adequately so that serum phosphate decreases, and urinary phosphate is high. • The diagnosis of this X-linked disease usually is made within the first few years of life. • Disease typically is more severe in males.
• The etiology of rickets usually can be determined by assessment of the mineral and vitamin D status (25 -hydroxyvitamin D < 8 ng/m. L suggests nutritional vitamin D deficiency). • Further testing of mineral balance or measurement of other vitamin D metabolites may be required.
• Several chemical forms of vitamin D can be used for treatment of the different rachitic conditions, but their potencies vary widely. • Required dosages depend on the condition being treated.
• Rickets usually is treated with 1, 25 hydroxyvitamin D and supplemental calcium. • In hypophosphatemic rickets, phosphate supplementation (not calcium) must accompany vitamin D therapy, which is given to suppress secondary hyperparathyroidism.
• Adequate therapy restores normal skeletal growth and produces resolution of the radiographic signs of rickets. • Nutritional rickets is treated with vitamin D in one large dose or multiple smaller replacement doses. • Surgery may be required to straighten legs in untreated patients with long-standing disease.