Calcium Homeostasis Calcium Homeostasis n n n 99
- Slides: 22
Calcium Homeostasis
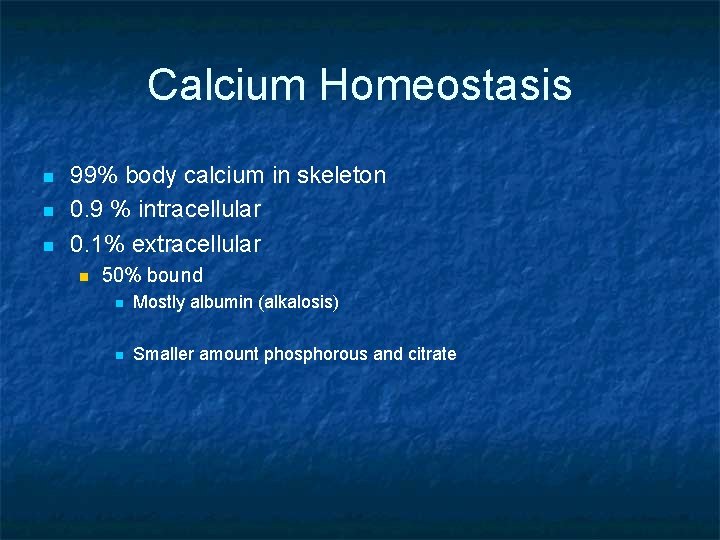
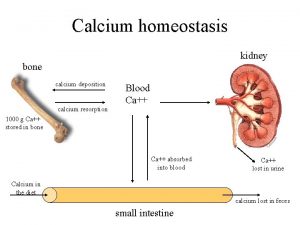
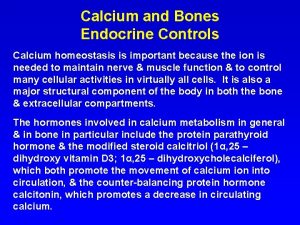
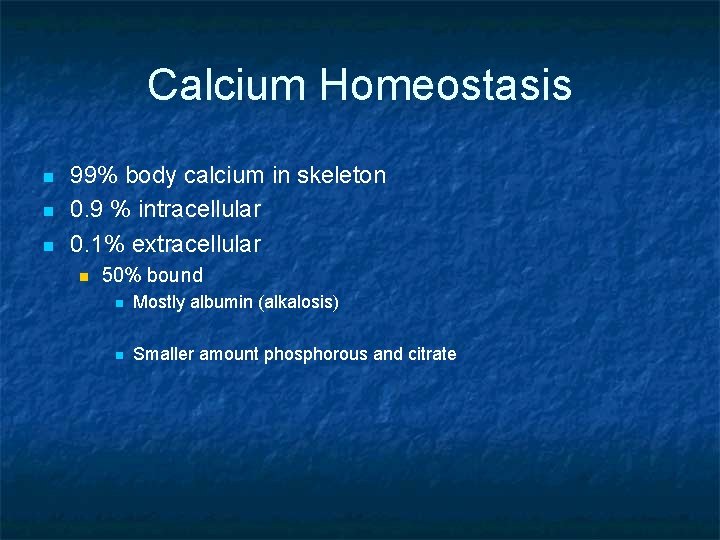
Calcium Homeostasis n n n 99% body calcium in skeleton 0. 9 % intracellular 0. 1% extracellular n 50% bound n Mostly albumin (alkalosis) n Smaller amount phosphorous and citrate
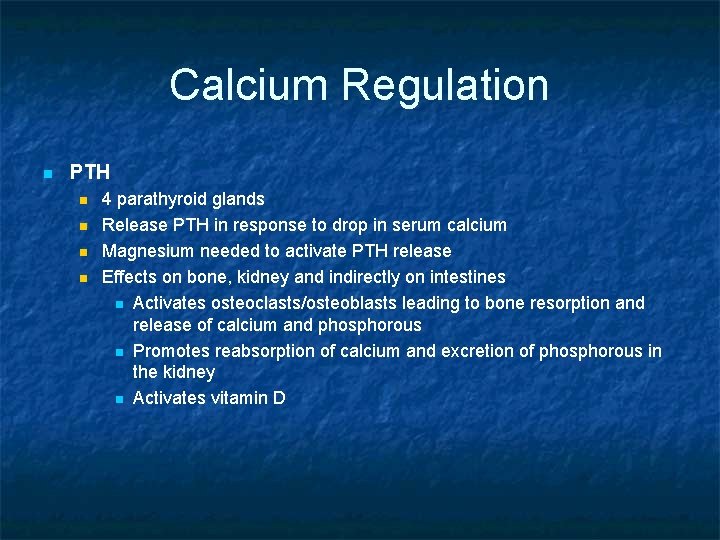
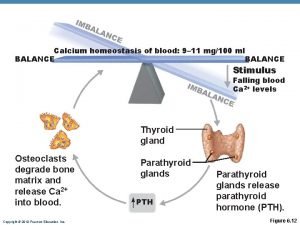
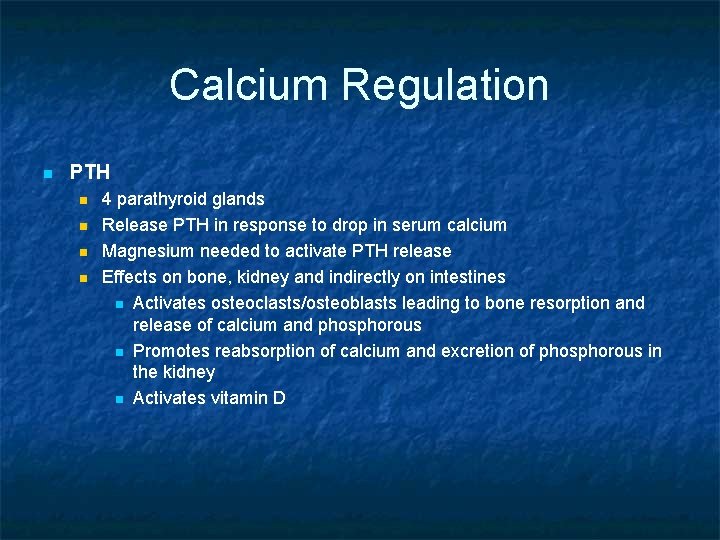
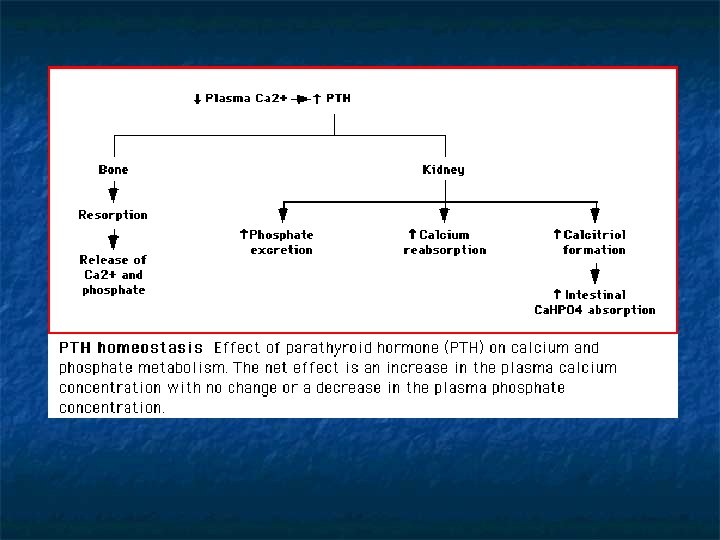
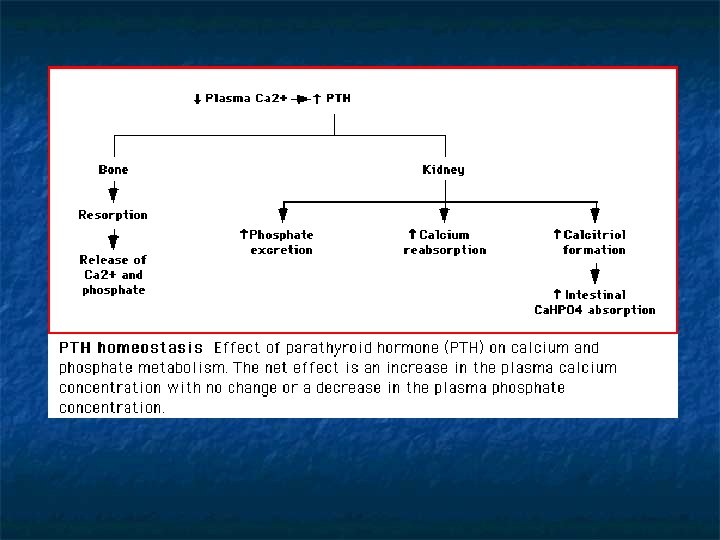
Calcium Regulation n PTH n n 4 parathyroid glands Release PTH in response to drop in serum calcium Magnesium needed to activate PTH release Effects on bone, kidney and indirectly on intestines n Activates osteoclasts/osteoblasts leading to bone resorption and release of calcium and phosphorous n Promotes reabsorption of calcium and excretion of phosphorous in the kidney n Activates vitamin D
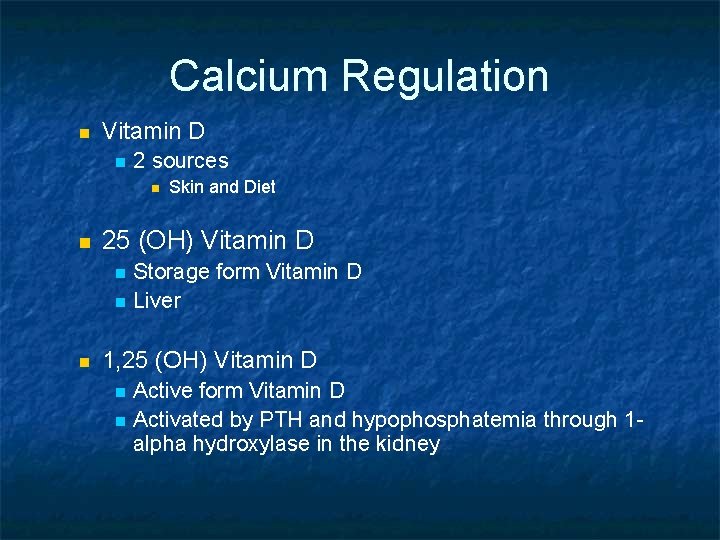
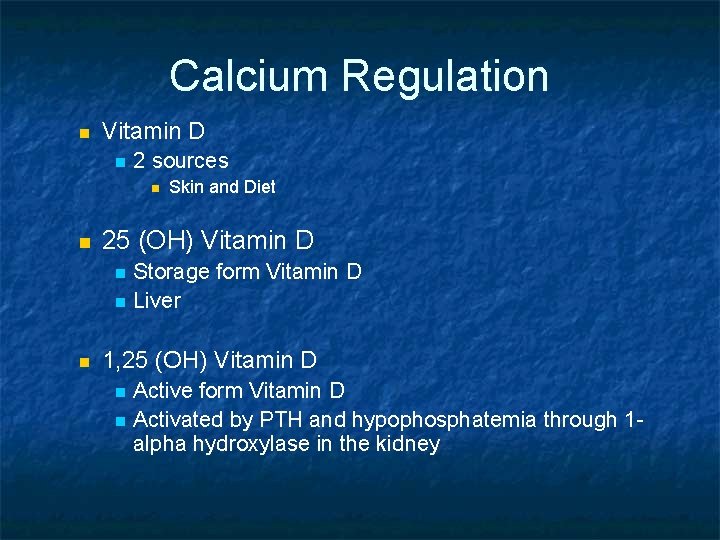
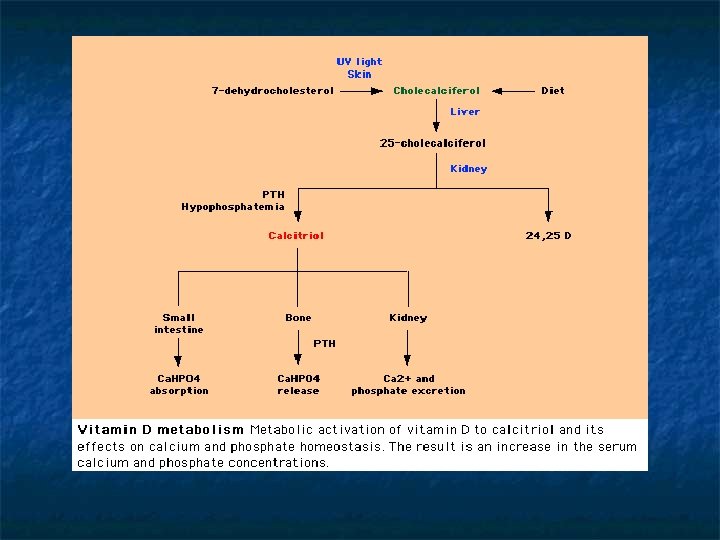
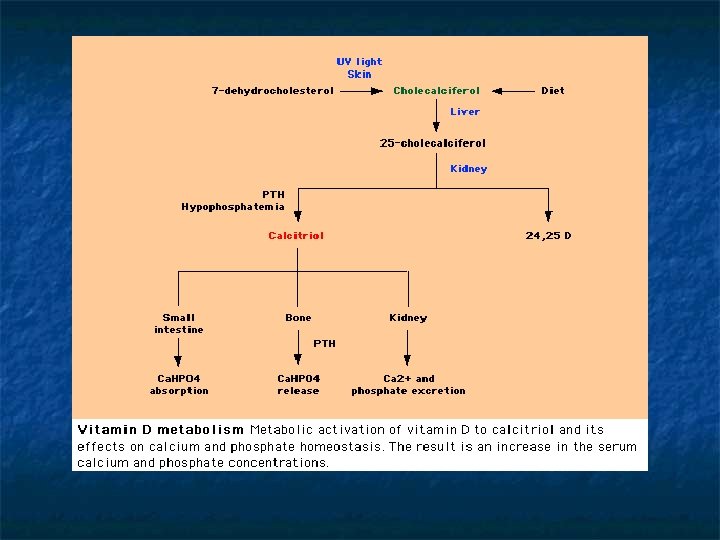
Calcium Regulation n Vitamin D n 2 sources n n 25 (OH) Vitamin D n n n Skin and Diet Storage form Vitamin D Liver 1, 25 (OH) Vitamin D n n Active form Vitamin D Activated by PTH and hypophosphatemia through 1 alpha hydroxylase in the kidney
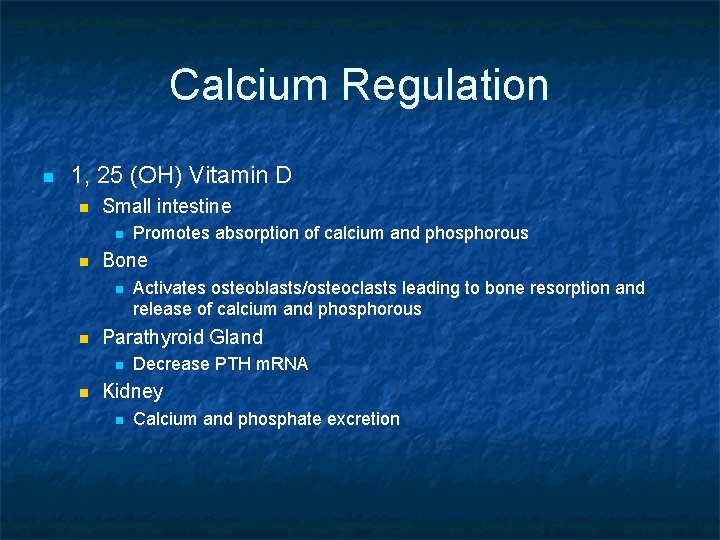
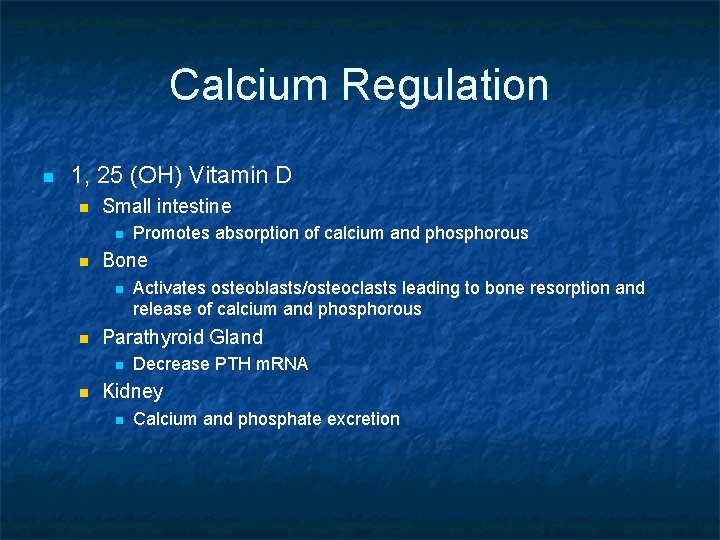
Calcium Regulation n 1, 25 (OH) Vitamin D n Small intestine n n Bone n n Activates osteoblasts/osteoclasts leading to bone resorption and release of calcium and phosphorous Parathyroid Gland n n Promotes absorption of calcium and phosphorous Decrease PTH m. RNA Kidney n Calcium and phosphate excretion
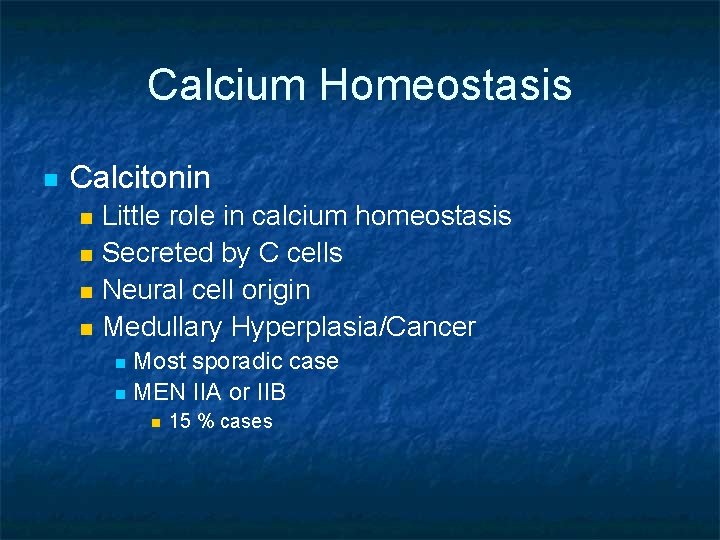
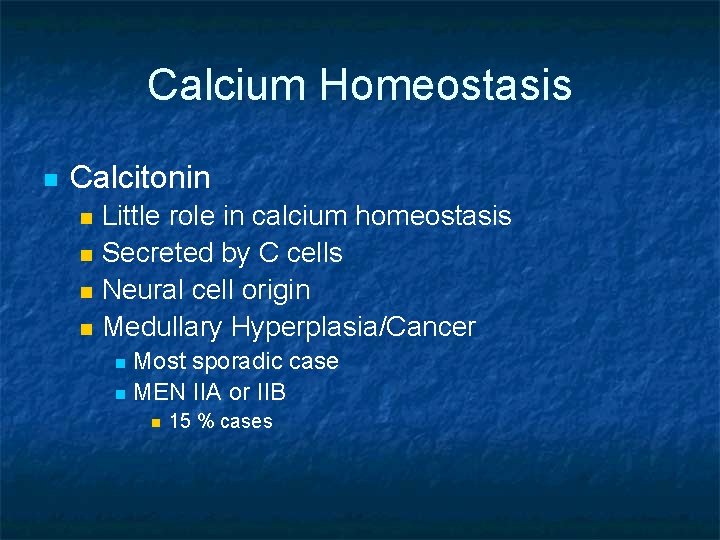
Calcium Homeostasis n Calcitonin n n Little role in calcium homeostasis Secreted by C cells Neural cell origin Medullary Hyperplasia/Cancer Most sporadic case n MEN IIA or IIB n n 15 % cases
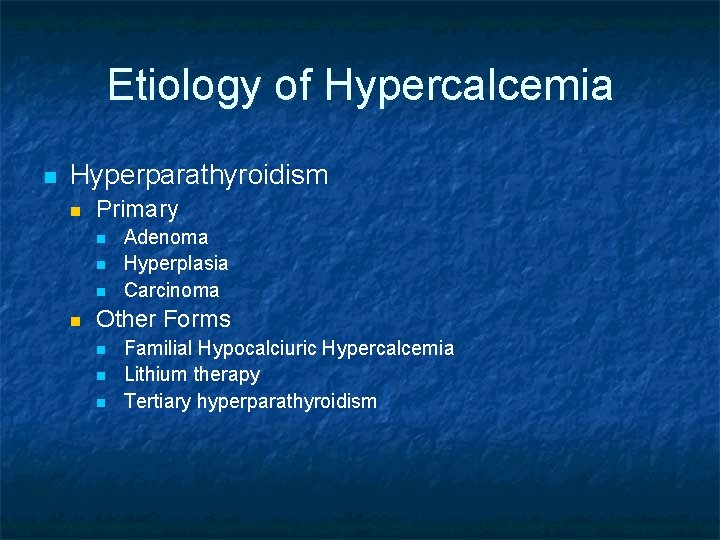
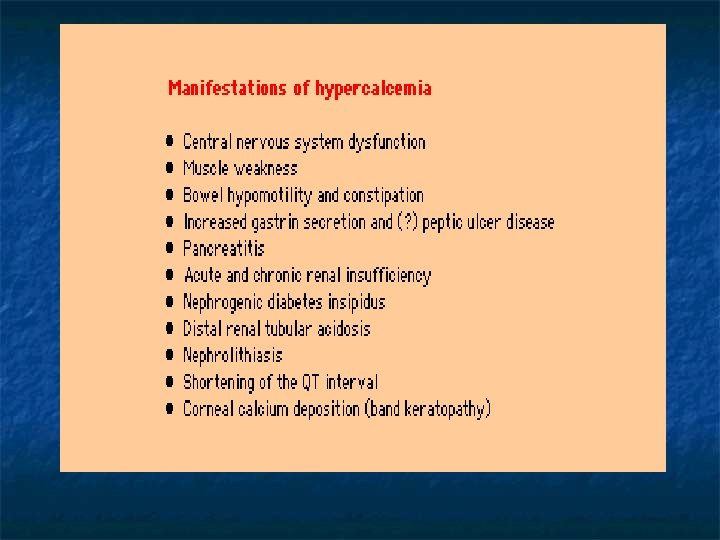
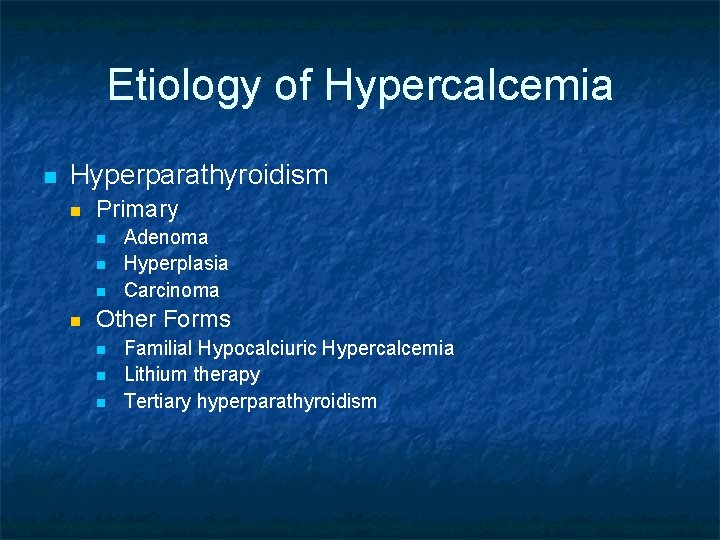
Etiology of Hypercalcemia n Hyperparathyroidism n Primary n n Adenoma Hyperplasia Carcinoma Other Forms n n n Familial Hypocalciuric Hypercalcemia Lithium therapy Tertiary hyperparathyroidism
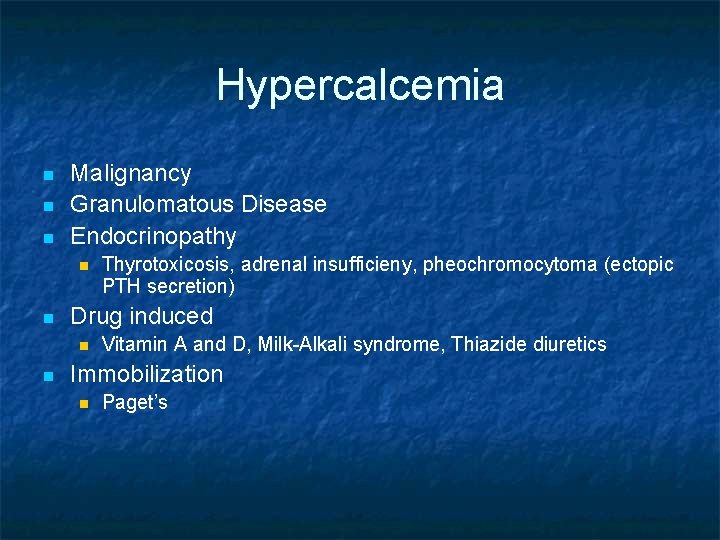
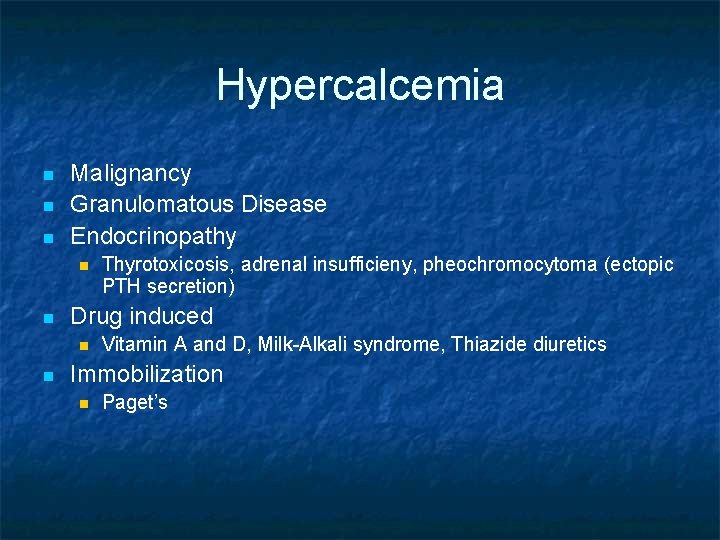
Hypercalcemia n n n Malignancy Granulomatous Disease Endocrinopathy n n Drug induced n n Thyrotoxicosis, adrenal insufficieny, pheochromocytoma (ectopic PTH secretion) Vitamin A and D, Milk-Alkali syndrome, Thiazide diuretics Immobilization n Paget’s
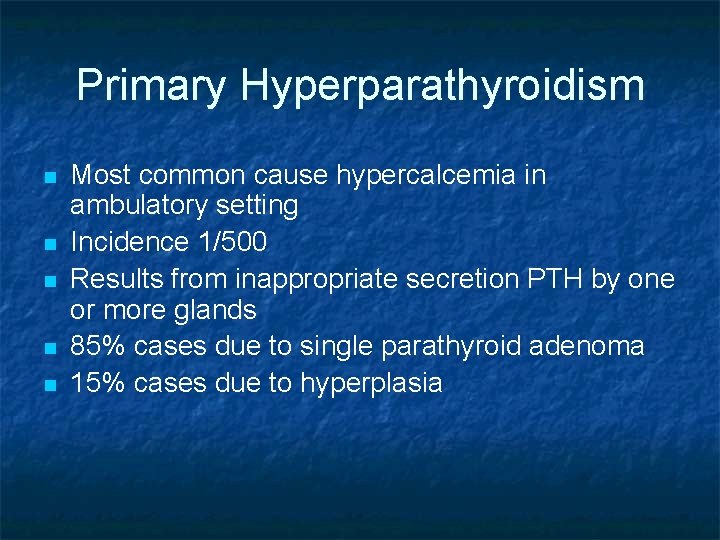
Primary Hyperparathyroidism n n n Most common cause hypercalcemia in ambulatory setting Incidence 1/500 Results from inappropriate secretion PTH by one or more glands 85% cases due to single parathyroid adenoma 15% cases due to hyperplasia
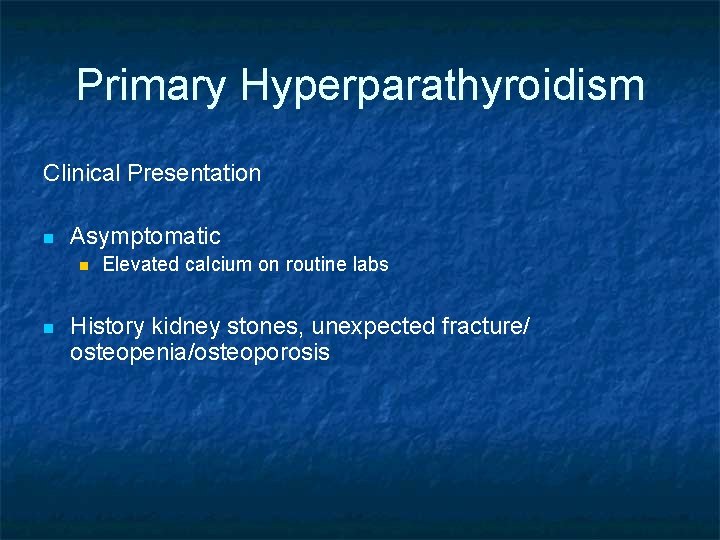
Primary Hyperparathyroidism Clinical Presentation n Asymptomatic n n Elevated calcium on routine labs History kidney stones, unexpected fracture/ osteopenia/osteoporosis
Primary Hyperparathyroidism n Evaluation/Diagnosis n n n Elevated calcium and i-PTH, low or normal phosphorous Alkaline phosphatase Creatinine 24 hour urine calcium/creatinine Renal US Bone Density
Primary Hyperparathyroidism n Treatment n Surgical n Indication for parathyroidectomy n n n 1 mg/dl above labs upper limit of normal Signs/symptoms hypercalcemia Kidney stones Hypercalciuria Minimally Invasive n PTH monitored intraoperatively
Primary Hyperparathyroidism n Medical Treatment n n n Monitor Hydration In general calcium intake should not be restricted Vitamin D supplementation Newer agents n cinacalcet, bisphonates
Hypocalcemia PTH deficiency n acquired n Thyroidectomy n Parathyroidectomy n Hypomagnesemia n Irradiation n Infiltrative n Developmental defect of parathyroid glands (Di. George) n Autosomal dominant hypocalcemia (activating mutation of calcium receptor gene)
Hypocalcemia n PTH Resistance n Pseudohypoparathyroidism n Congenital defect n Absent metacarpal, short stature, round face, mental disability n Target organ unresponsiveness to PTH n Serum PTH levels high
Hypocalcemia Vitamin D n Deficiency n Nutritional deficiency and lack of skin exposure n Osteomalacia n n Adult Proximal muscle weakness n Rickets Type 1 n Hereditary vitamin D deficiency due to lack of 1 -alpha hydroxylase n Renal insufficiency
Hypocalcemia Vitamin D n Resistance n Rickets Type II n Target organ unresponsiveness to vitamin D due to defect in receptor
Hypocalcemia Calcium Deposition n Extravascular Deposition n n Hyperphosphatemia due to tumor lysis, rhabdo, renal failure Pancreatitis “Hungry bone syndrome” Intravascular deposition n n Citrate in blood transfusion lactate
Hypocalcemia n Treatment n Calcium n n Vitamin D n n PO vs IV 25 and/or 1, 25 (OH) Vitamin D Magnesium
 Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Homeostasis blood calcium level
Homeostasis blood calcium level What is maintaining an internal balance
What is maintaining an internal balance Homeostasis blood calcium level (about 10 mg/100ml)
Homeostasis blood calcium level (about 10 mg/100ml) Blood calcium level
Blood calcium level Calcium homeostasis diagram
Calcium homeostasis diagram Homeostasis in body
Homeostasis in body Diferencia entre alostasis y homeostasis
Diferencia entre alostasis y homeostasis Prueba sorpresa
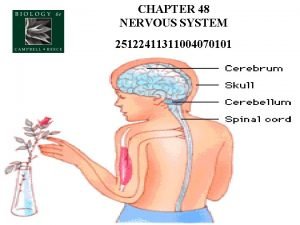
Prueba sorpresa Nervous system homeostasis
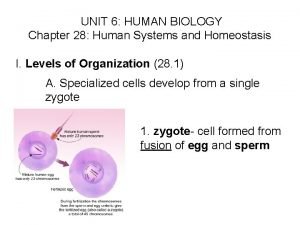
Nervous system homeostasis Chapter 28 human systems and homeostasis
Chapter 28 human systems and homeostasis Positive feedback
Positive feedback Homeostasis
Homeostasis Homeostasis definition ap psychology
Homeostasis definition ap psychology Homeostasis animal example
Homeostasis animal example Distribucion de calcio en el organismo
Distribucion de calcio en el organismo Section 5-2 review active transport
Section 5-2 review active transport Kobe kuiz
Kobe kuiz Mengapa homeostasis perlu dijaga
Mengapa homeostasis perlu dijaga Homeostasis of blood sugar
Homeostasis of blood sugar Mapa conceptual sobre la homeostasis
Mapa conceptual sobre la homeostasis Homer simpson homeostasis lab
Homer simpson homeostasis lab