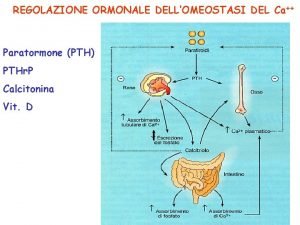
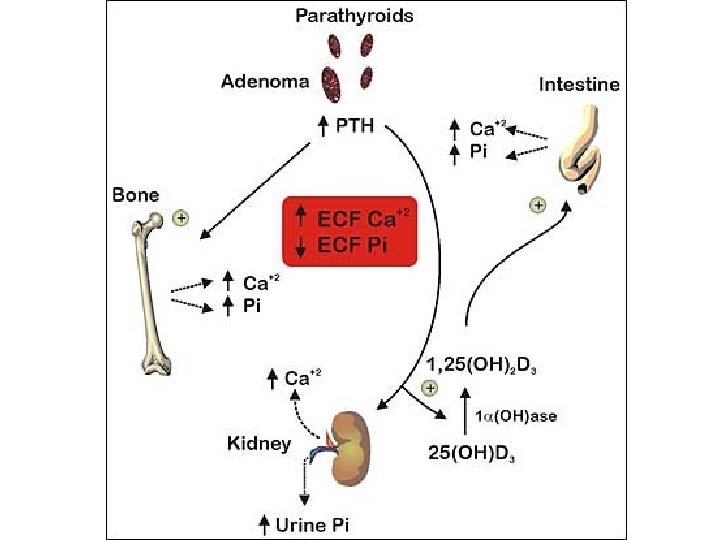
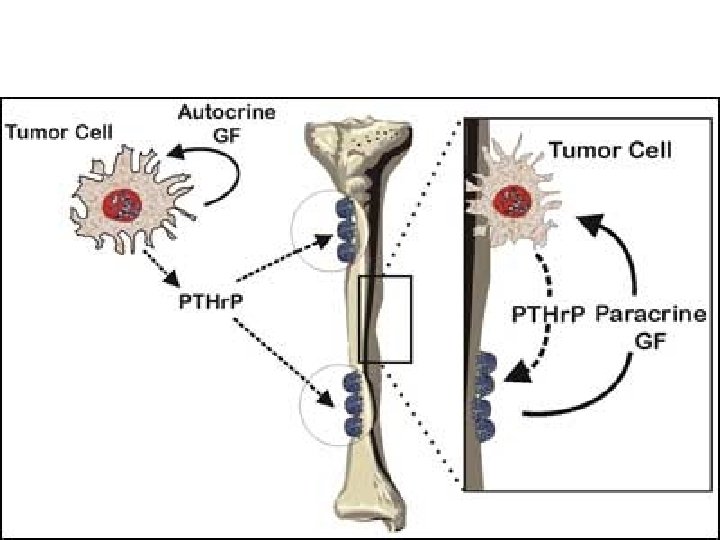
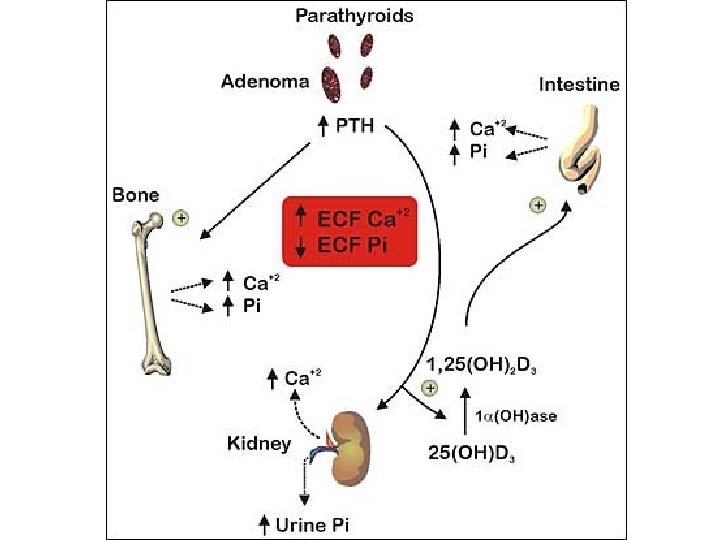
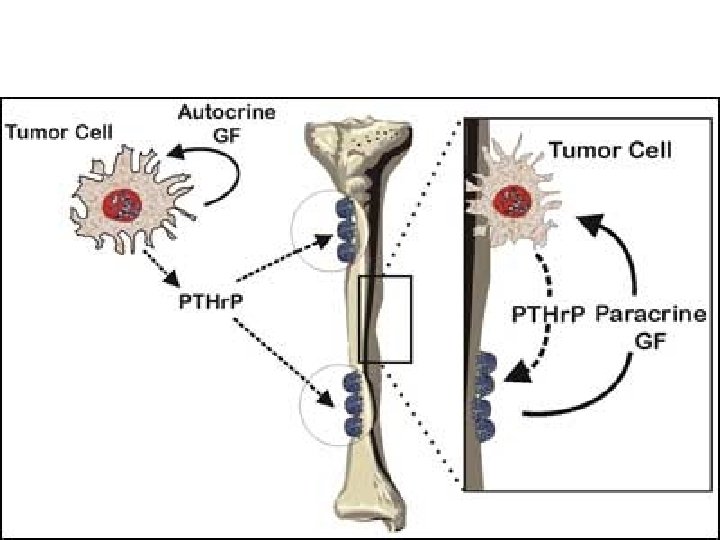
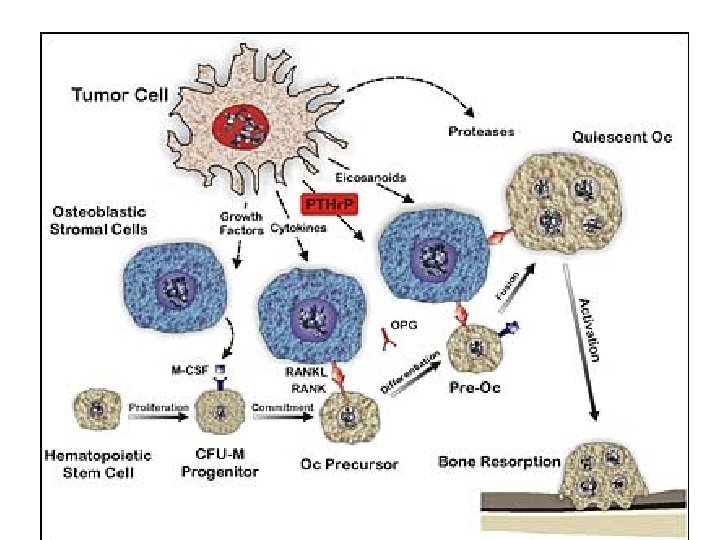
PTHr P PTH Schematic illustration of impact of






































![Κλασματική απέκρισση Ca Ca/Cr clearance ratio = [24 -hour Urine Ca x serum Cr] Κλασματική απέκρισση Ca Ca/Cr clearance ratio = [24 -hour Urine Ca x serum Cr]](https://slidetodoc.com/presentation_image_h/1a9d3865a17e81b848c87c729f0a05b5/image-72.jpg)




















- Slides: 105









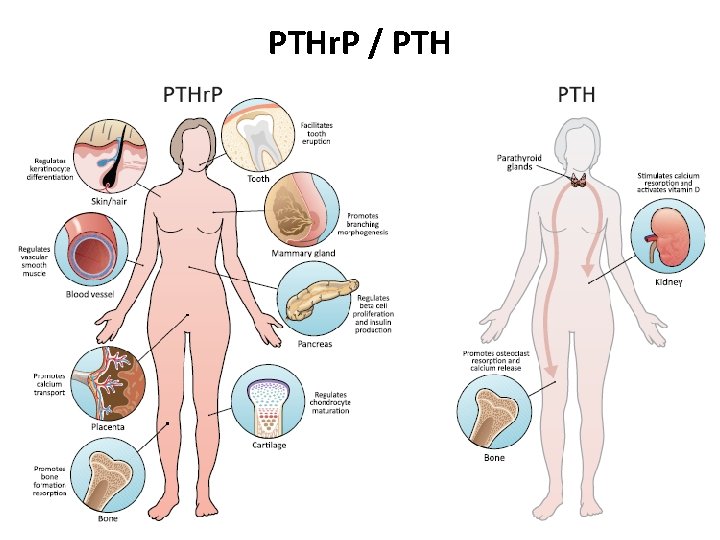
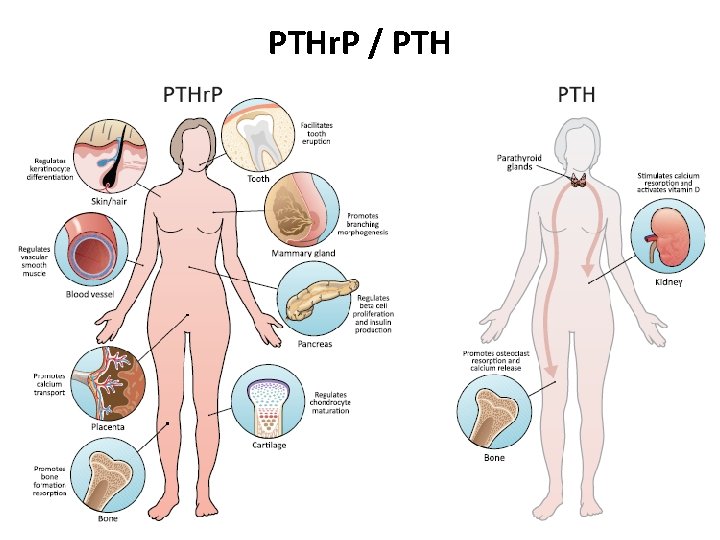
PTHr. P / PTH
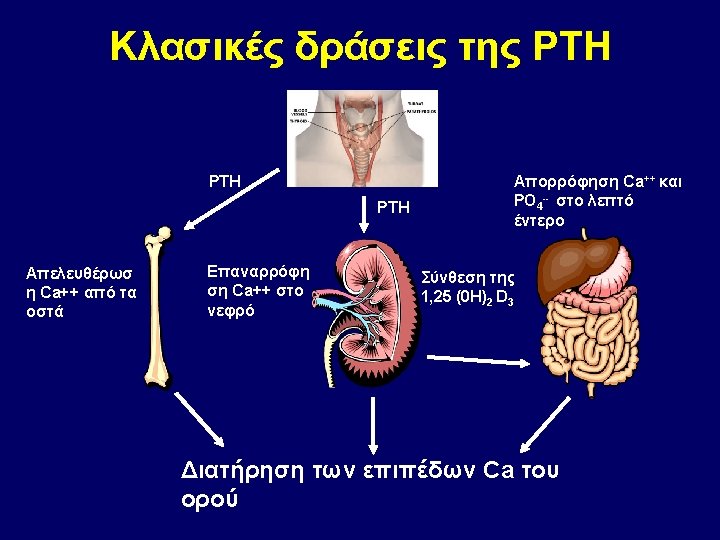


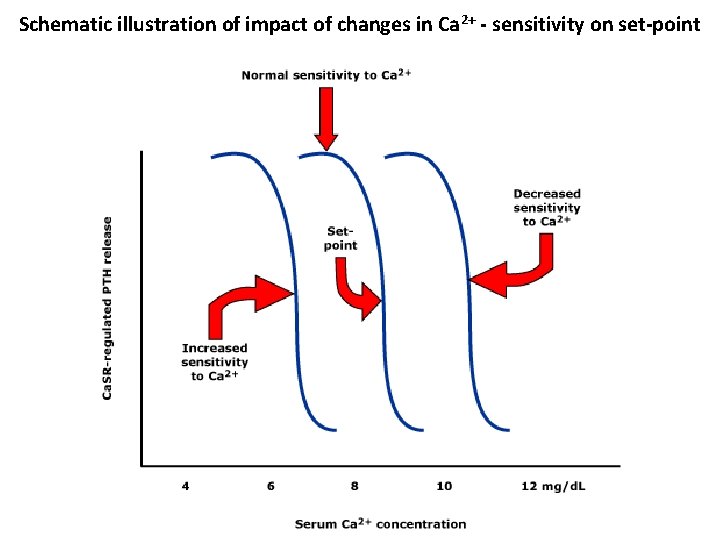
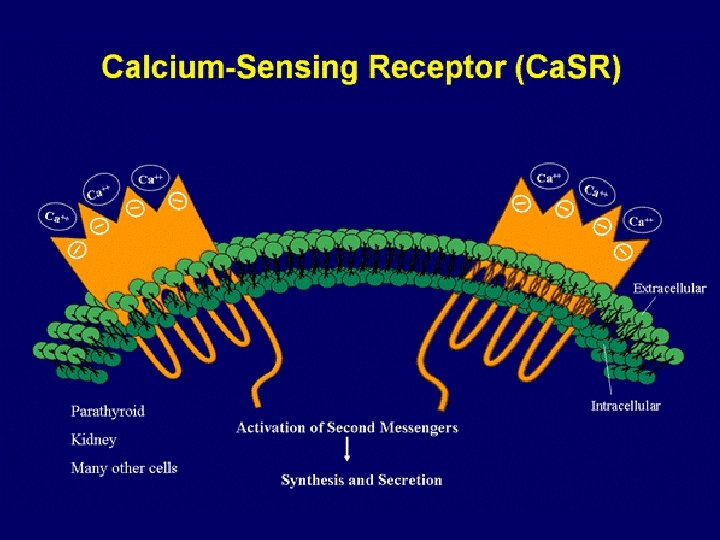
Schematic illustration of impact of changes in Ca 2+ - sensitivity on set-point
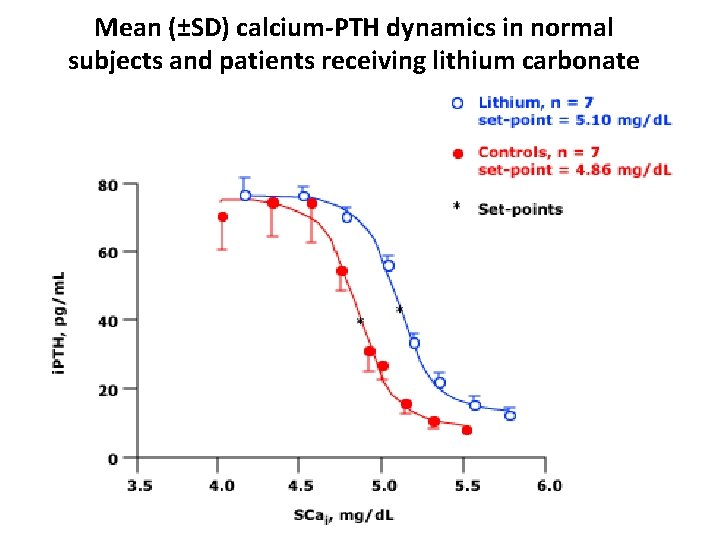
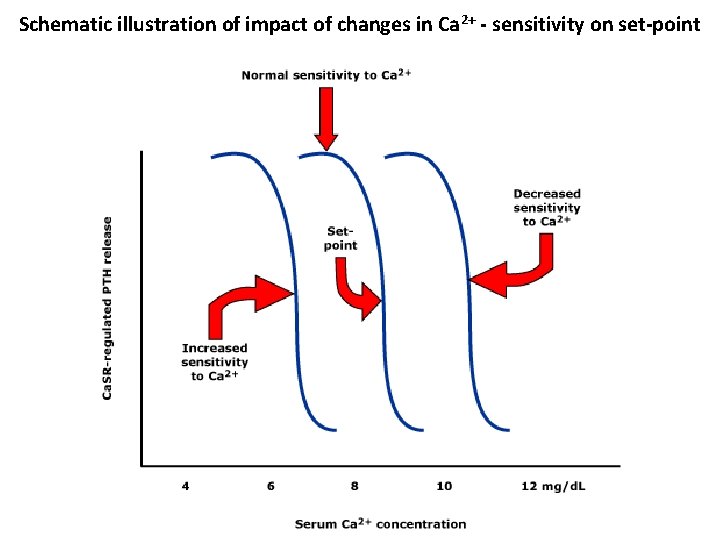
Mean (±SD) calcium-PTH dynamics in normal subjects and patients receiving lithium carbonate

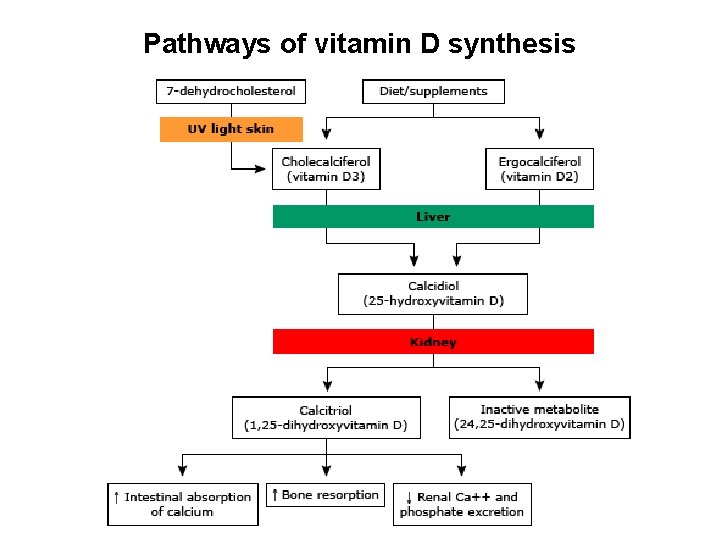
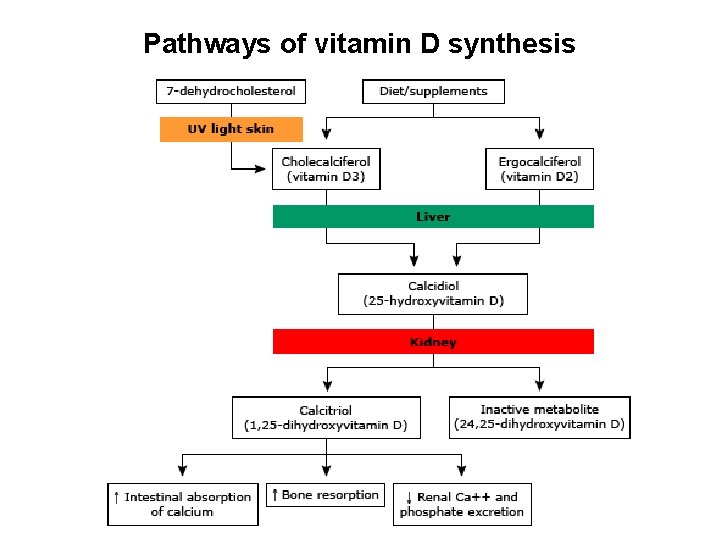
Pathways of vitamin D synthesis

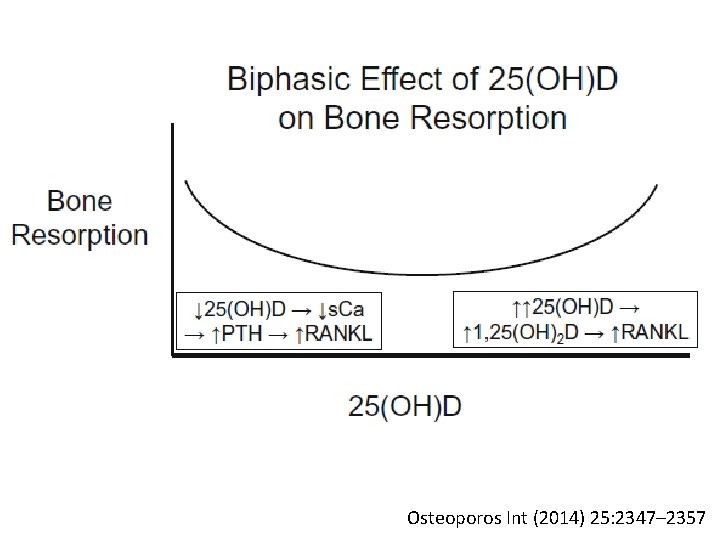
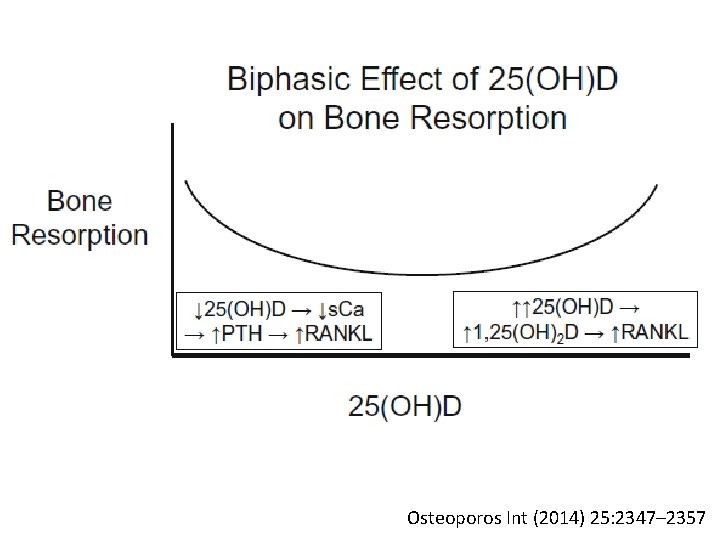
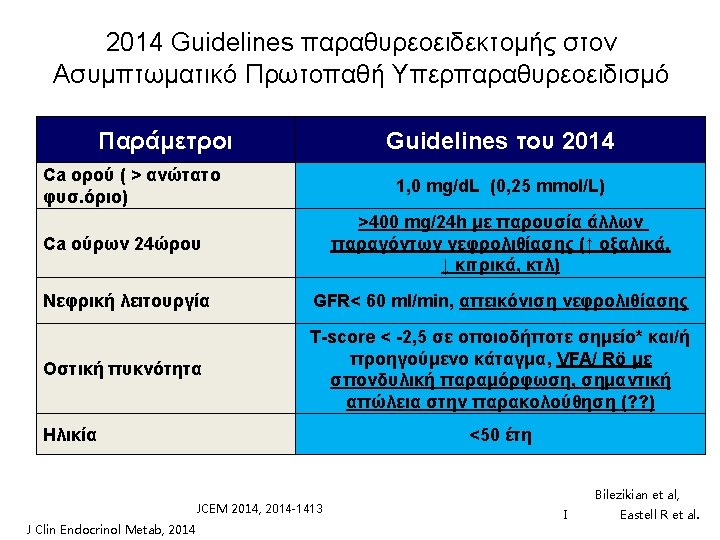
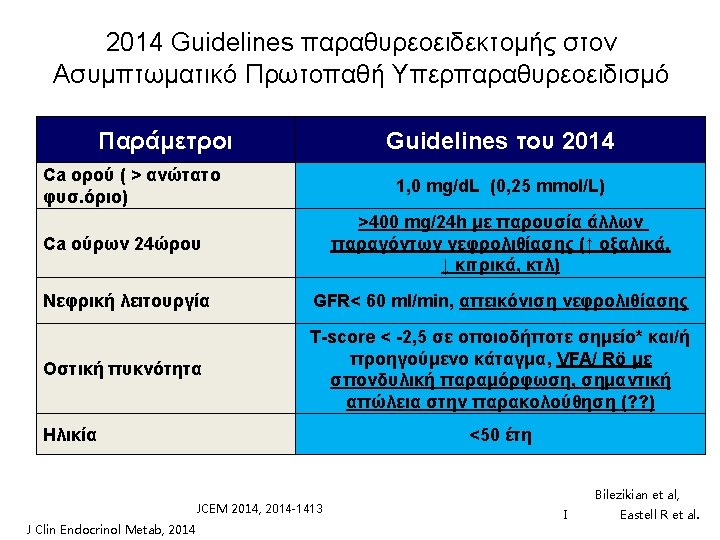
Osteoporos Int (2014) 25: 2347– 2357




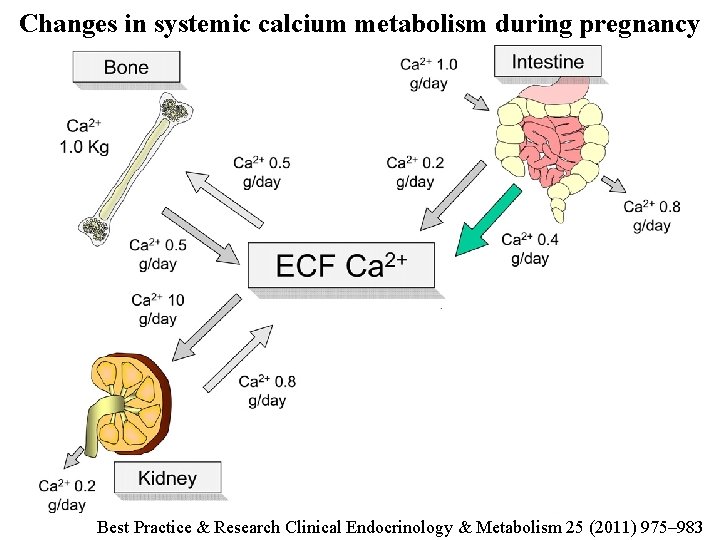
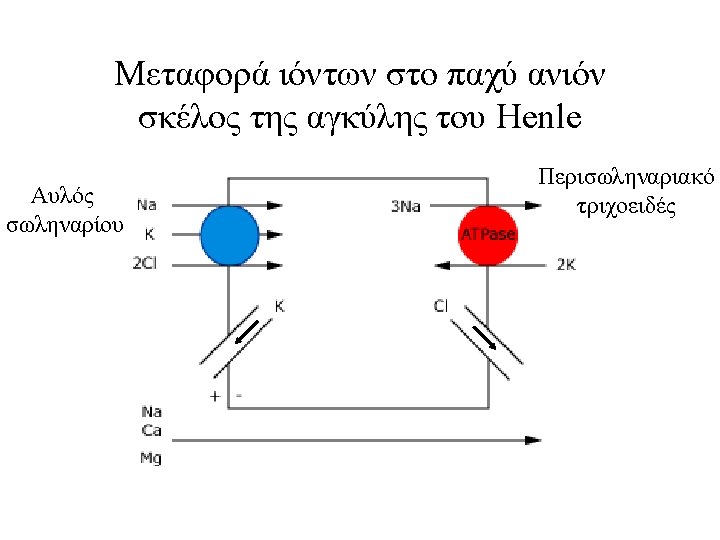
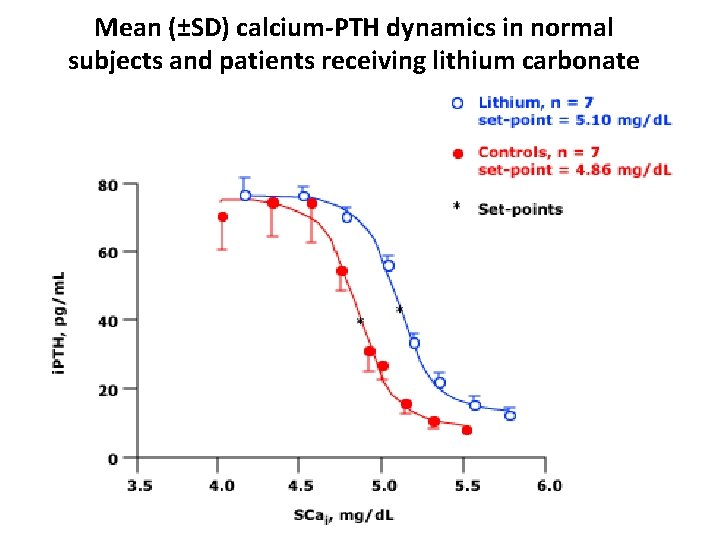
Changes in systemic calcium metabolism during pregnancy Best Practice & Research Clinical Endocrinology & Metabolism 25 (2011) 975– 983

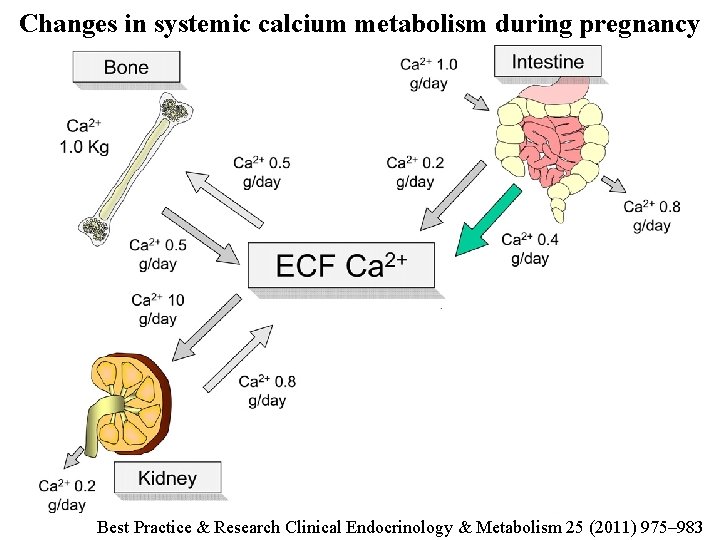
Changes in systemic calcium metabolism during lactation Best Practice & Research Clinical Endocrinology & Metabolism 25 (2011) 975– 983
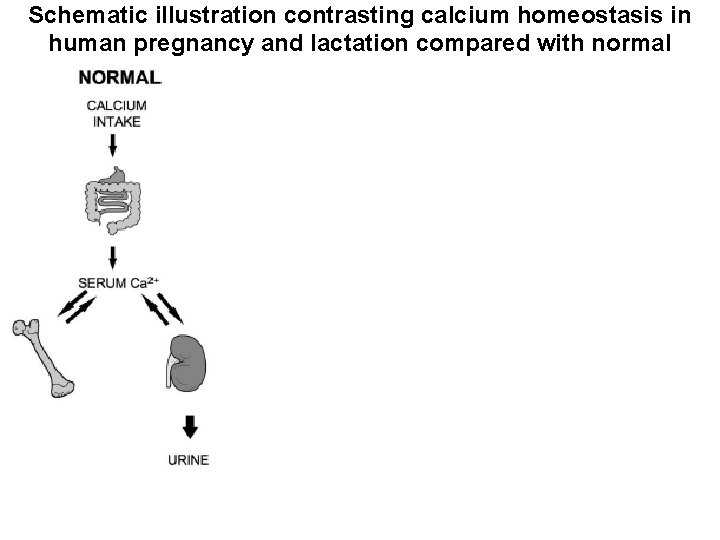
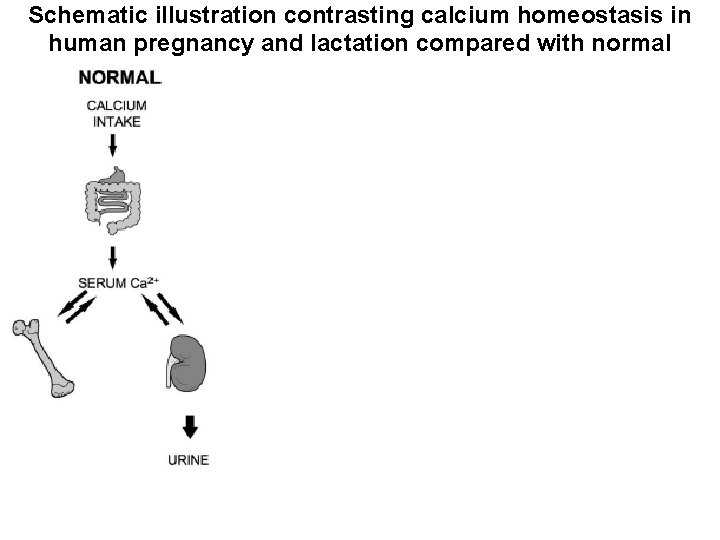
Schematic illustration contrasting calcium homeostasis in human pregnancy and lactation compared with normal Pregnancy-induced changes in maternal Ca metabolism Intestinal Ca absorption↑ Urinary Ca excretion↑ “Absorptive hypercalciuria” Total Ca ↓ Ca++ ↔ PTH ↓ PTHr. P ↑ E 2, PRL, Placental Lactogen ↑ Bone resorption markers ↑ BMD ↔↓ Fetal Ca metabolism Ca: 25 -30 g Ca higher than the mother PTH↓ Calcitonin ↑


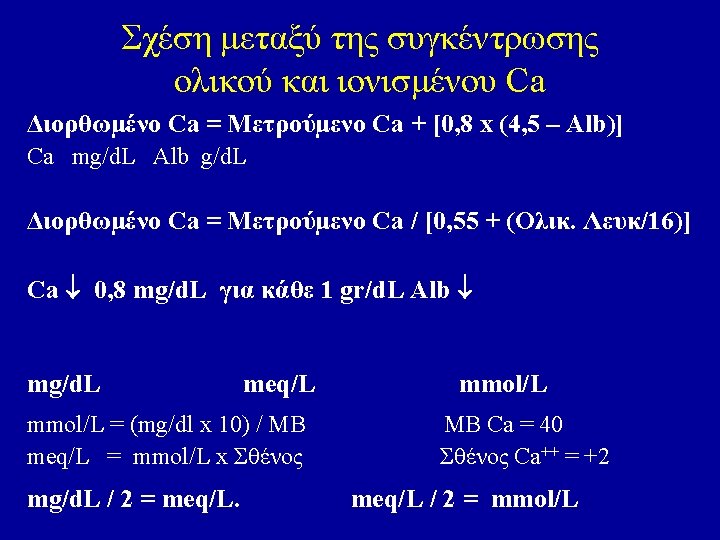

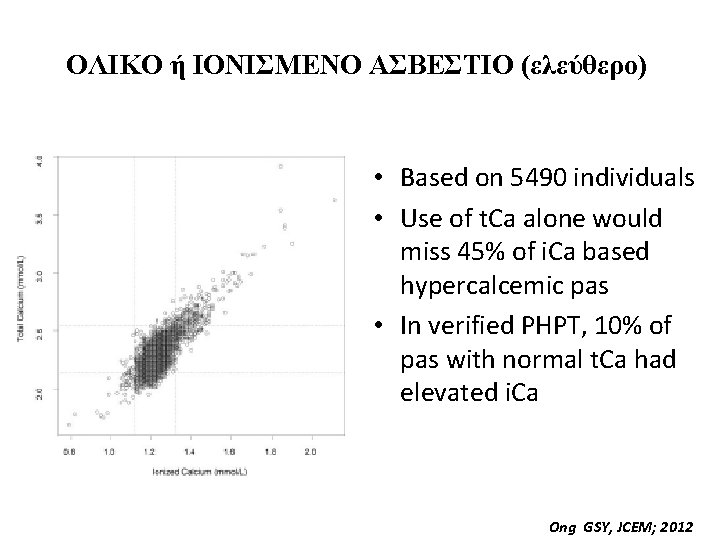
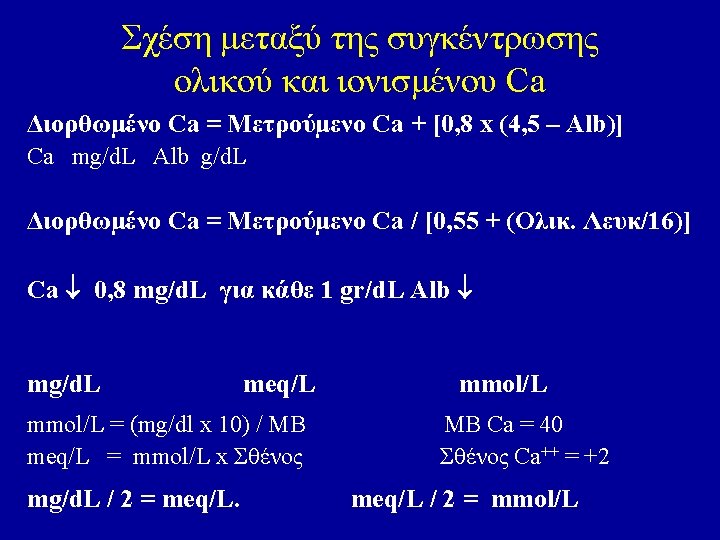
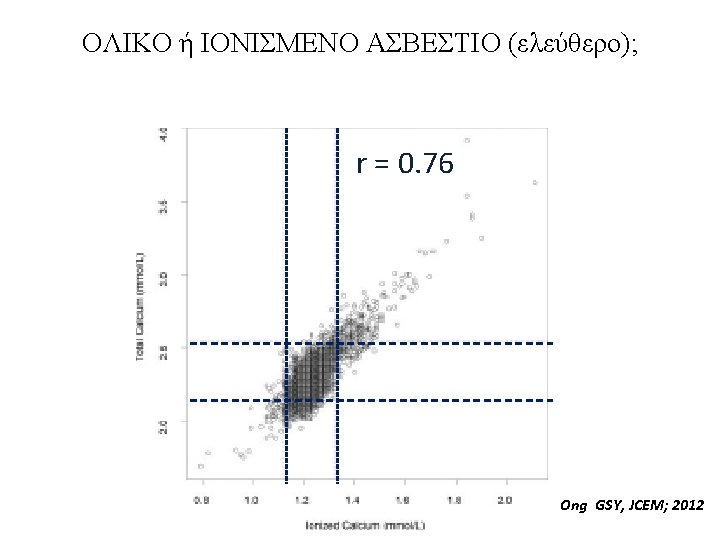
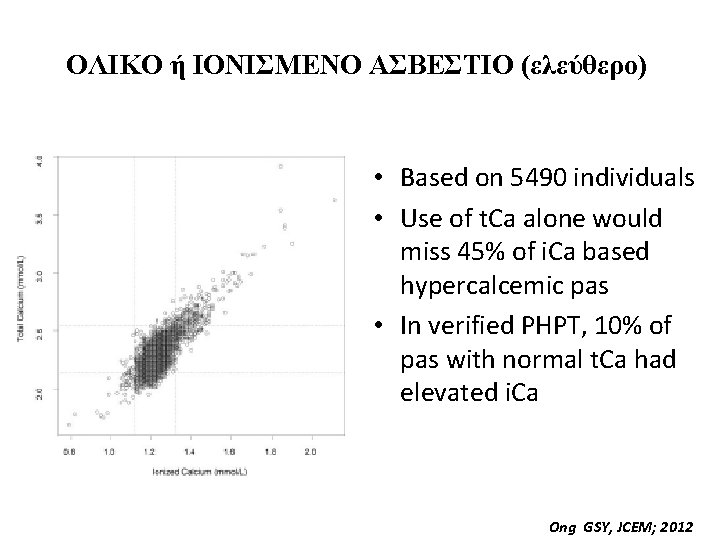
ΟΛΙΚΟ ή ΙΟΝΙΣΜΕΝΟ ΑΣΒΕΣΤΙΟ (ελεύθερο) • Based on 5490 individuals • Use of t. Ca alone would miss 45% of i. Ca based hypercalcemic pas • In verified PHPT, 10% of pas with normal t. Ca had elevated i. Ca Ong GSY, JCEM; 2012
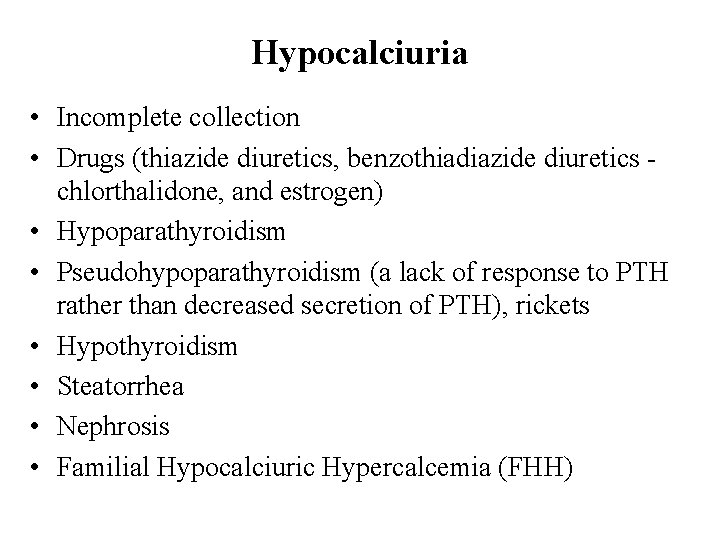
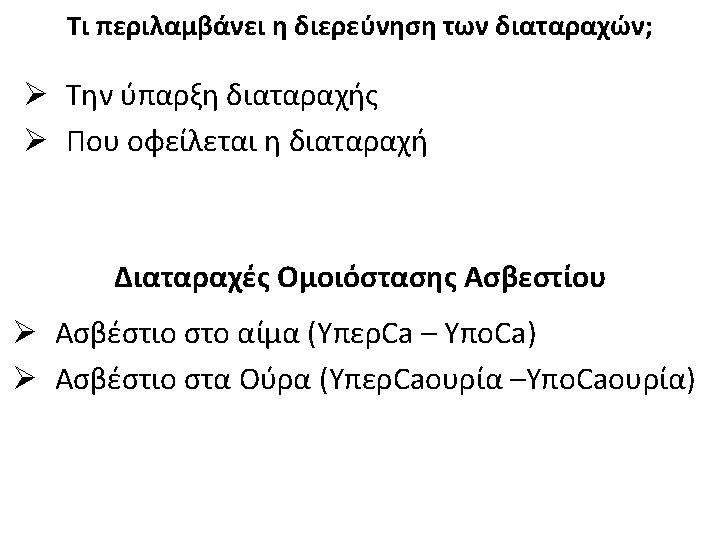
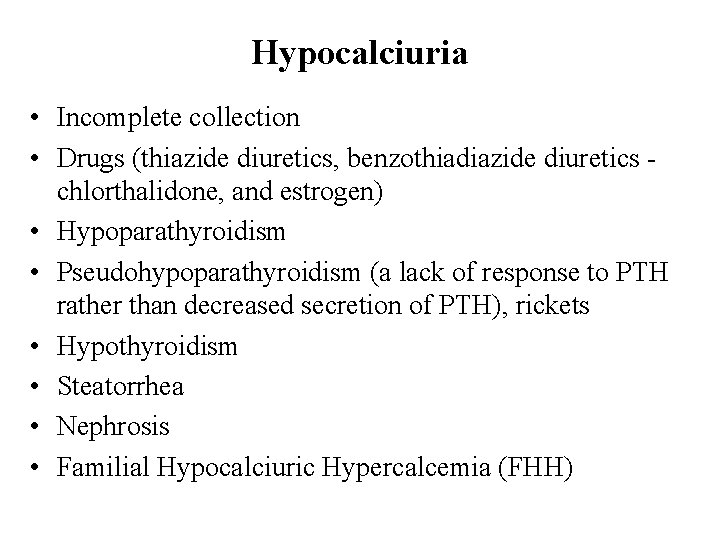
Hypocalciuria • Incomplete collection • Drugs (thiazide diuretics, benzothiadiazide diuretics chlorthalidone, and estrogen) • Hypoparathyroidism • Pseudohypoparathyroidism (a lack of response to PTH rather than decreased secretion of PTH), rickets • Hypothyroidism • Steatorrhea • Nephrosis • Familial Hypocalciuric Hypercalcemia (FHH)

Hypercalciuria • • • Hyperparathyroidism Multiple myeloma (or any osteolytic neoplasm) Osteoporosis Vitamin D overdose Renal tubular acidosis Hyperthyroidism Paget's disease Sarcoidosis Drugs (Antacids, Calcium supplements, Spironolactone, Androgens, Growth Hormone, Acetazolamide and Corticosteroids)
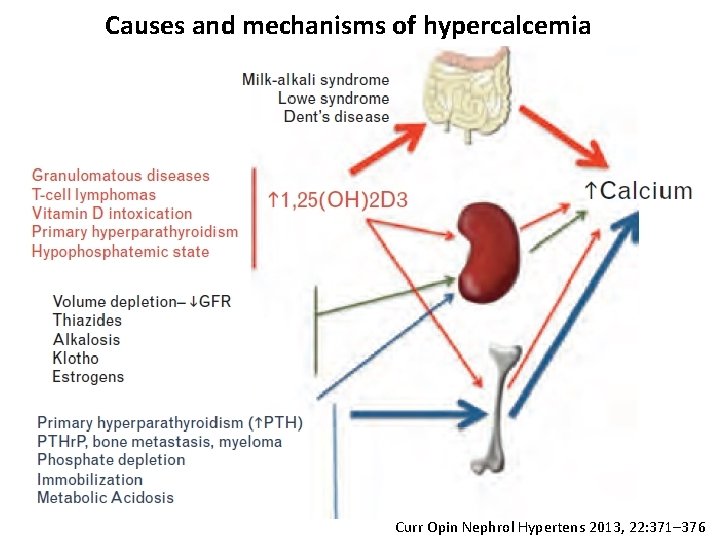
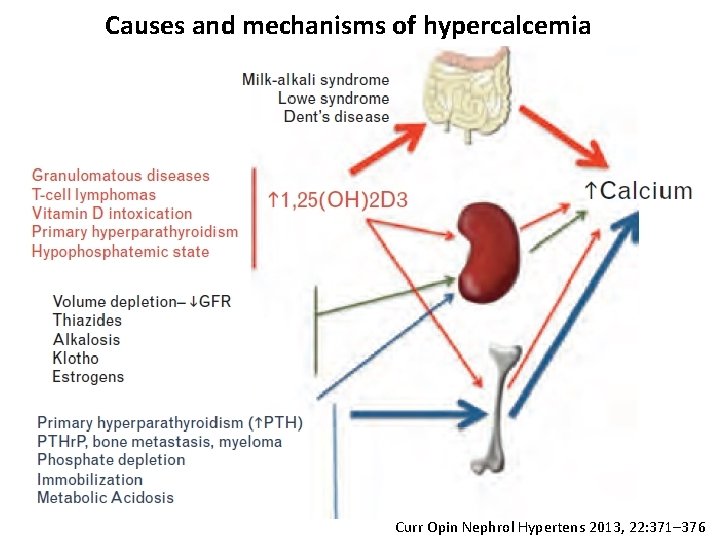
Causes and mechanisms of hypercalcemia Curr Opin Nephrol Hypertens 2013, 22: 371– 376



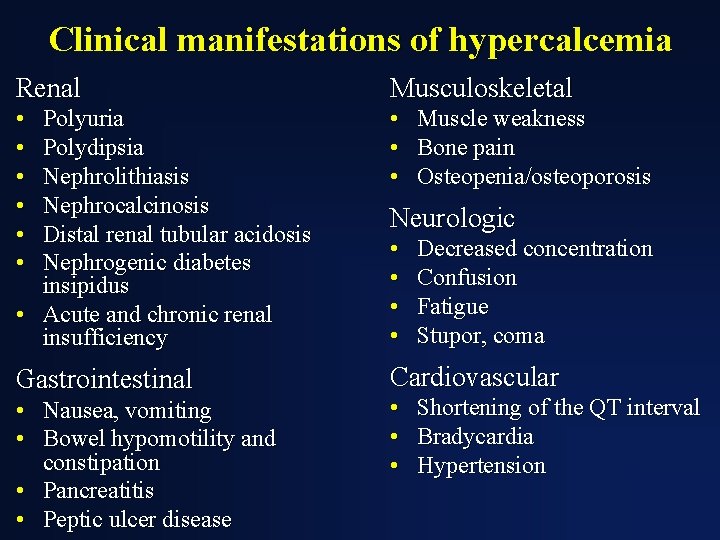
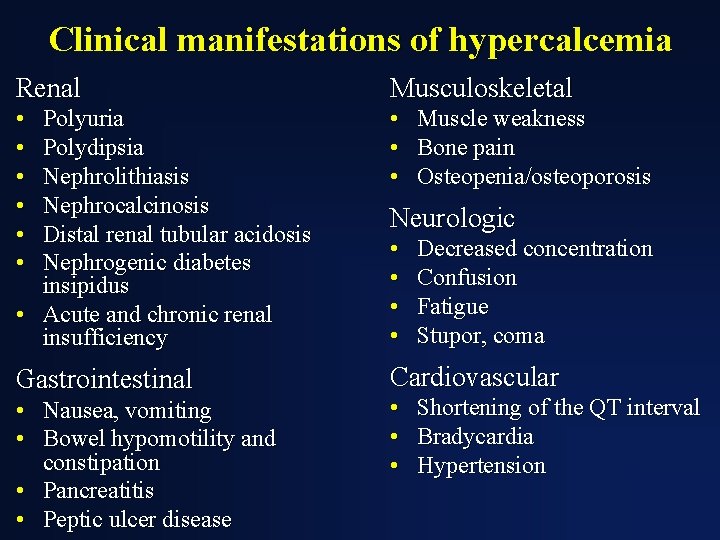
Clinical manifestations of hypercalcemia Renal Musculoskeletal • • • Polyuria Polydipsia Nephrolithiasis Nephrocalcinosis Distal renal tubular acidosis Nephrogenic diabetes insipidus • Acute and chronic renal insufficiency • • • Gastrointestinal Cardiovascular • Nausea, vomiting • Bowel hypomotility and constipation • Pancreatitis • Peptic ulcer disease Muscle weakness Bone pain Osteopenia/osteoporosis Neurologic • • Decreased concentration Confusion Fatigue Stupor, coma Shortening of the QT interval Bradycardia Hypertension


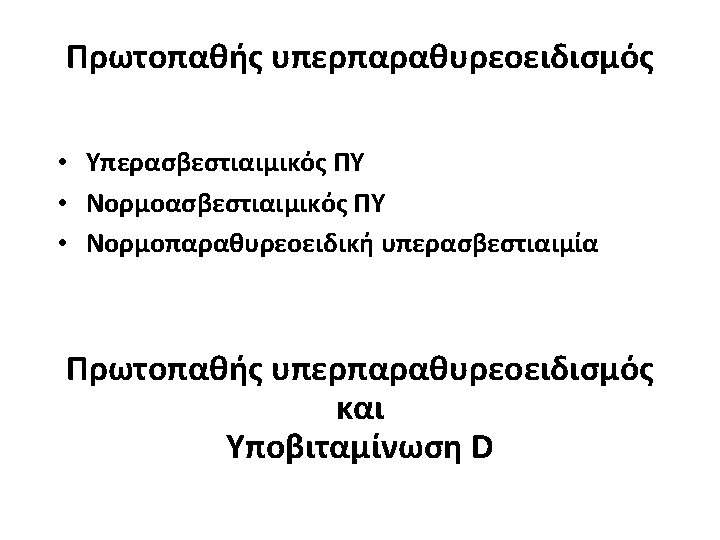

25(ΟΗ)Vit D ΑΦ Ρ Ca Ca Ούρων 24 h PTH Conclusion Vitamin D replacement in subjects with PHPT and coexistent vitamin D deficiency increase 25 (OH) D and reduce serum PTH significantly without causing hypercalcaemia and hypercalciuria. The finding of the study needs to be confirmed by a large randomized trial in patient with PHPT and coexistent vitamin D deficiency
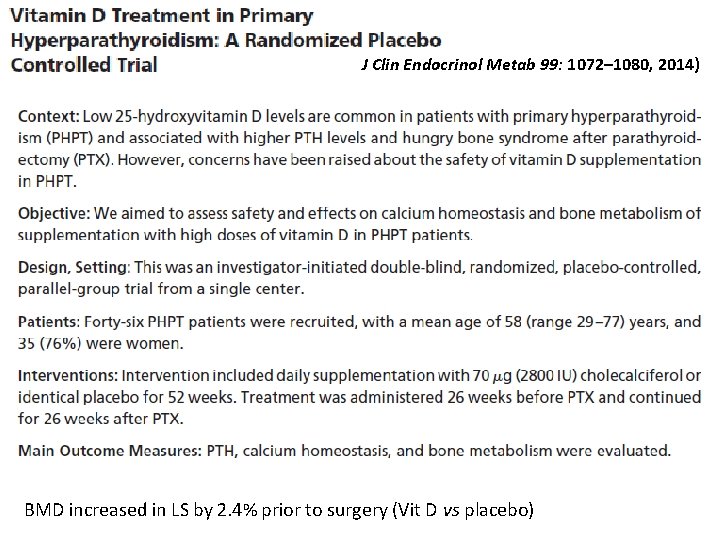
J Clin Endocrinol Metab 99: 1072– 1080, 2014) BMD increased in LS by 2. 4% prior to surgery (Vit D vs placebo)
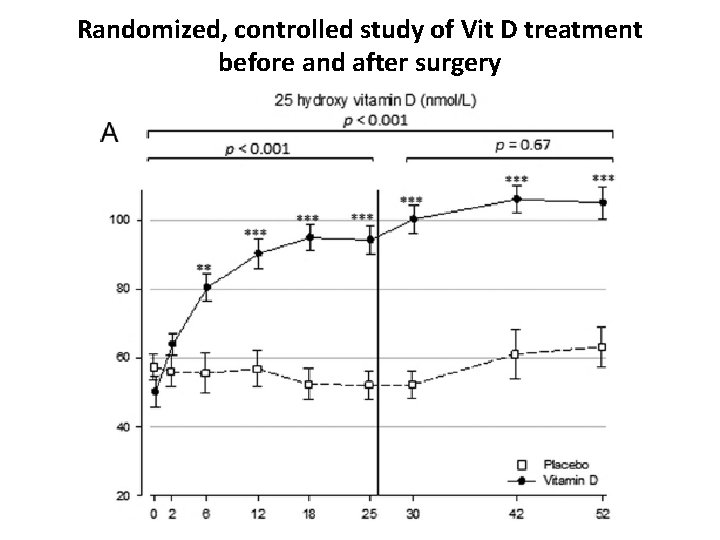
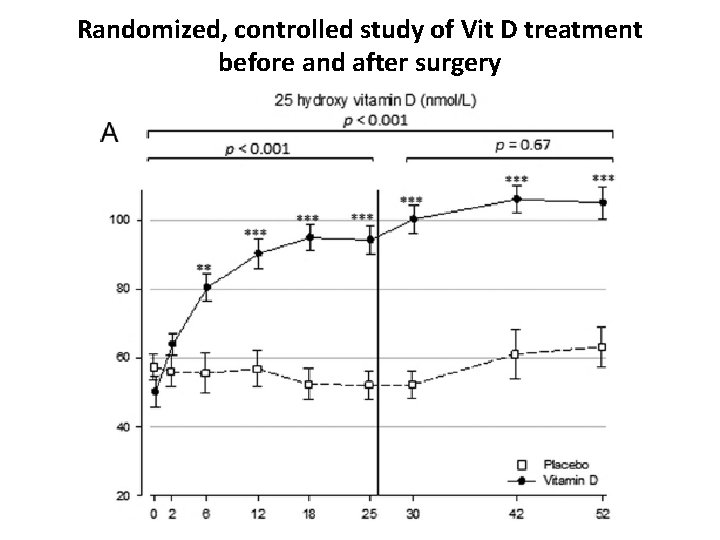
Randomized, controlled study of Vit D treatment before and after surgery
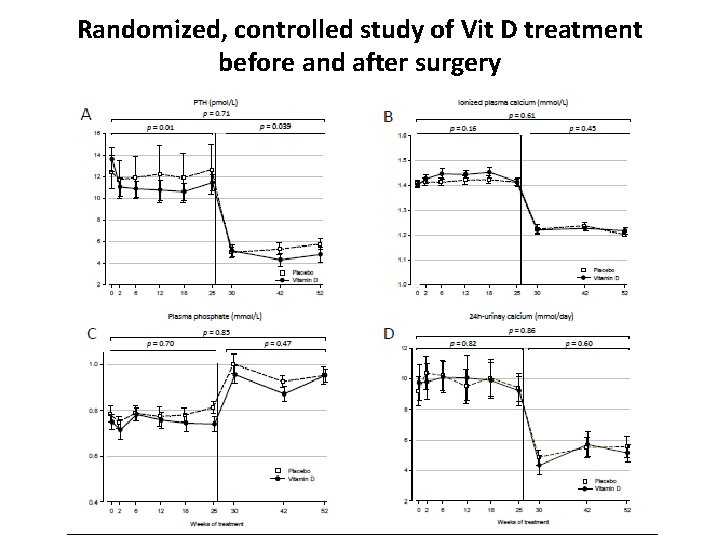
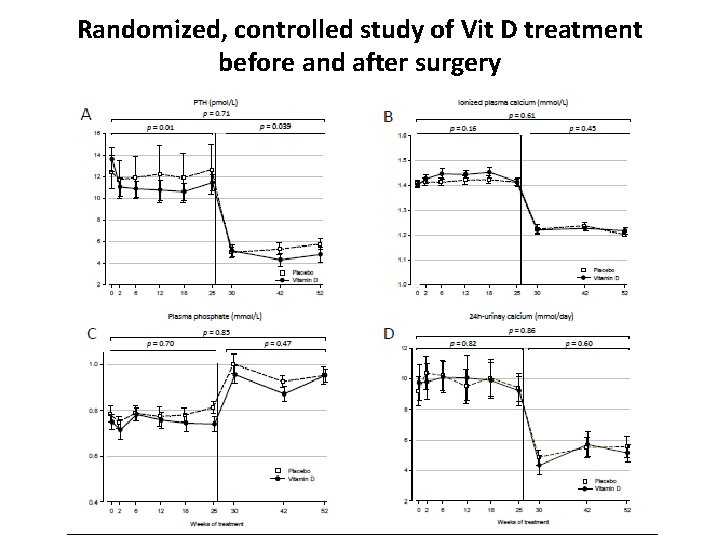
Randomized, controlled study of Vit D treatment before and after surgery
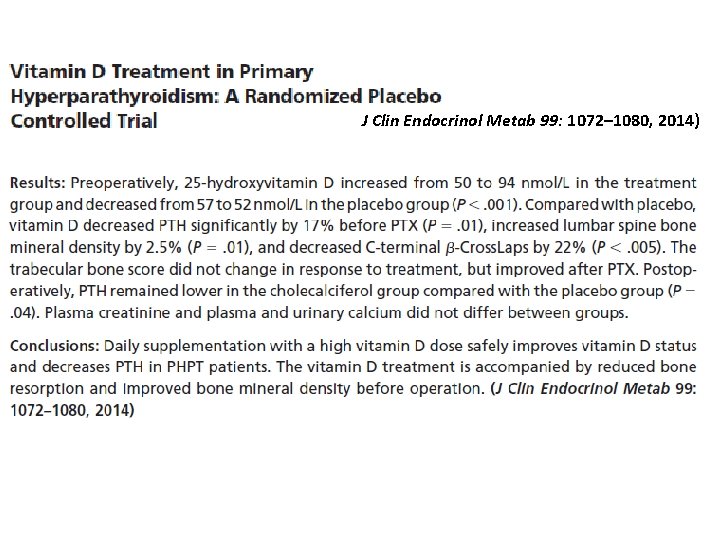
J Clin Endocrinol Metab 99: 1072– 1080, 2014)



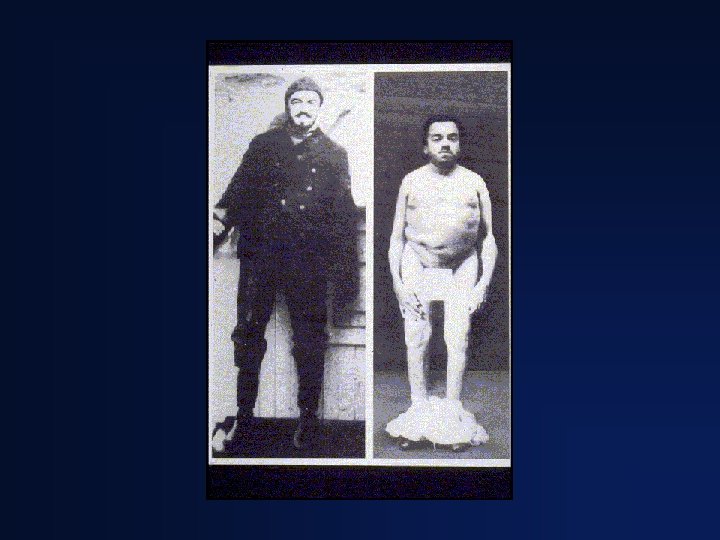

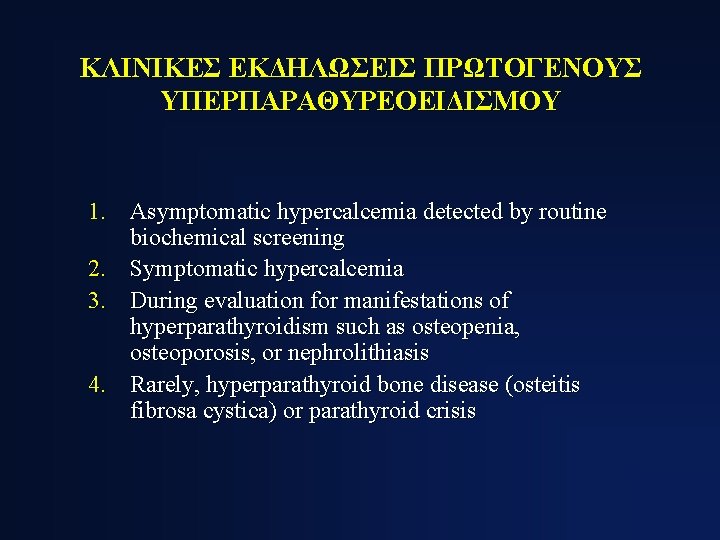
ΚΛΙΝΙΚΕΣ ΕΚΔΗΛΩΣΕΙΣ ΠΡΩΤΟΓΕΝΟΥΣ ΥΠΕΡΠΑΡΑΘΥΡΕΟΕΙΔΙΣΜΟΥ 1. Asymptomatic hypercalcemia detected by routine biochemical screening 2. Symptomatic hypercalcemia 3. During evaluation for manifestations of hyperparathyroidism such as osteopenia, osteoporosis, or nephrolithiasis 4. Rarely, hyperparathyroid bone disease (osteitis fibrosa cystica) or parathyroid crisis
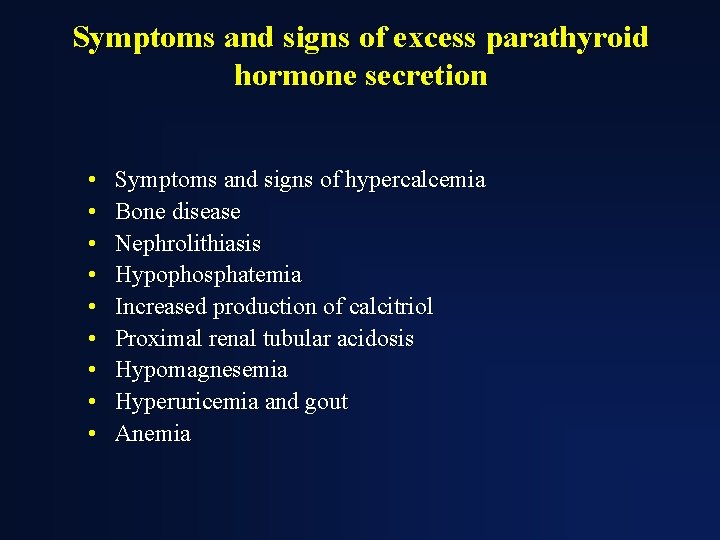
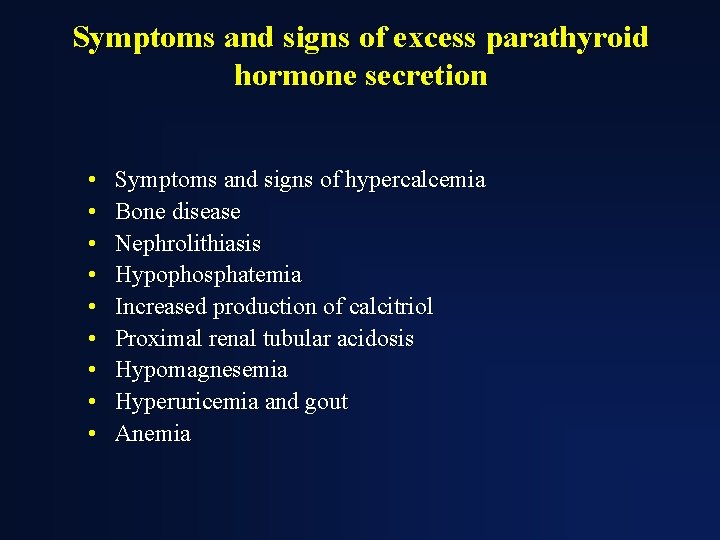
Symptoms and signs of excess parathyroid hormone secretion • • • Symptoms and signs of hypercalcemia Bone disease Nephrolithiasis Hypophosphatemia Increased production of calcitriol Proximal renal tubular acidosis Hypomagnesemia Hyperuricemia and gout Anemia


Η ΜΟΝΤΕΡΝΑ ΚΛΙΝΙΚΗ ΕΙΚΟΝΑ ΤΟΥ ΠΡΩΤΟΓΕΝΟΥΣ ΥΠΕΡΠΑΡΑΘΥΡΕΟΕΙΔΙΣΜΟΥ Cope et al. 19301965 Nεφρολιθίαση Heath et al. Mallette et 1965 -1974 al. 1965 -1974 Silverberg, Bilezikian et al. 1984 -2006 57% 51% 37% 17% Not reported 36% 40% 39% Εμφανής σκελετική νόσος 23% 10% 14% 1. 4% Ασυμπτωματικός 0. 6% 18% 22% 80% Υπερασβεστιουρία Silverberg SJ and Bilezikian JP (2006)

Η βιοχημική εικόνα του πρωτογενούς υπερπαραθυρεοειδισμού στην μοντέρνα εποχή Παράμετρος Τιμές Ασθενείς Φυσιολο. • Calcium (mg/dl) 10. 7± 0. 1 8. 4 -10. 2 • Phosphorus (mg/dl) • Alk Phos (IU/l) 2. 9± 0. 1 114± 4 2. 5 -4. 5 <100 • PTH (pg/ml) 121± 7 10 -65 • • 21± 1 59± 2 248 + 12 17 + 6 9 -52 15 -60 100 -300 4 -21 25 -OH Vit D (ng/ml) 1, 25 -OH 2 Vit D (pg/ml) Urinary calcium (mg) DPD (nmol/mmol Cr) Silverberg, Bilezikian et al.

Bone Mineral Density: % of Expected Η οστεοπυκνομετρική εικόνα του πρωτογενούς υπερπαραθυρεοειδισμού στην μοντέρνα εποχή 100 * * * Differs from ra p<. 05 90 80 70 Lumbar Spine Silverberg, Bilezikian et al. JBMR, 1989 Femoral Neck Radius


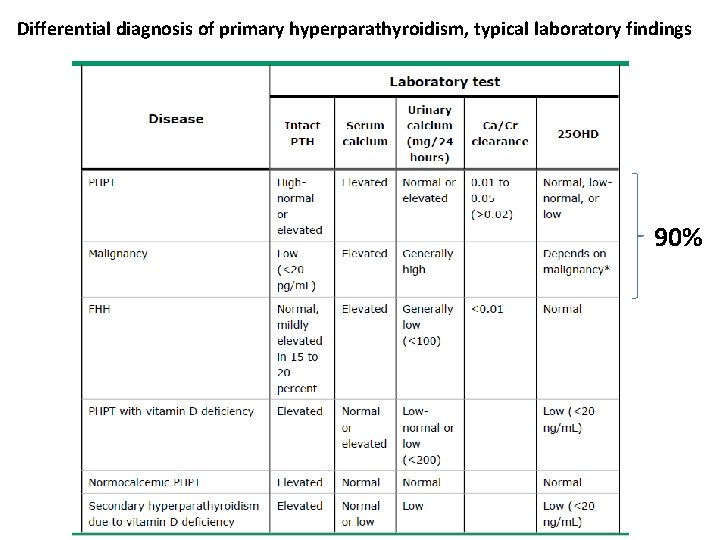
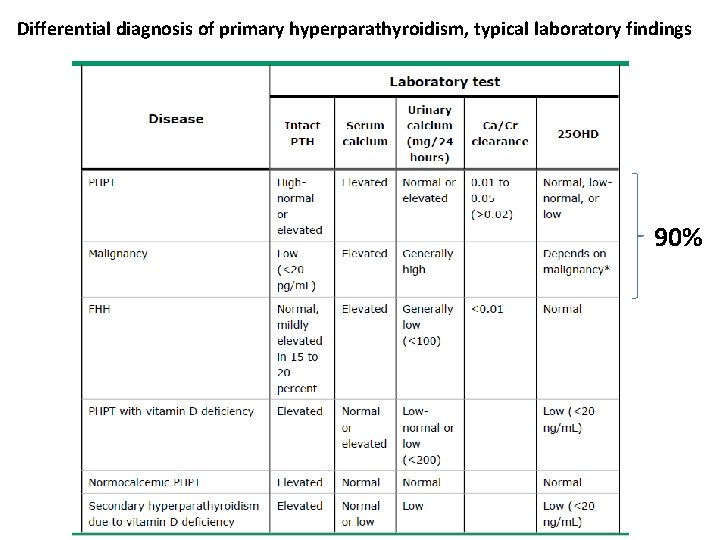
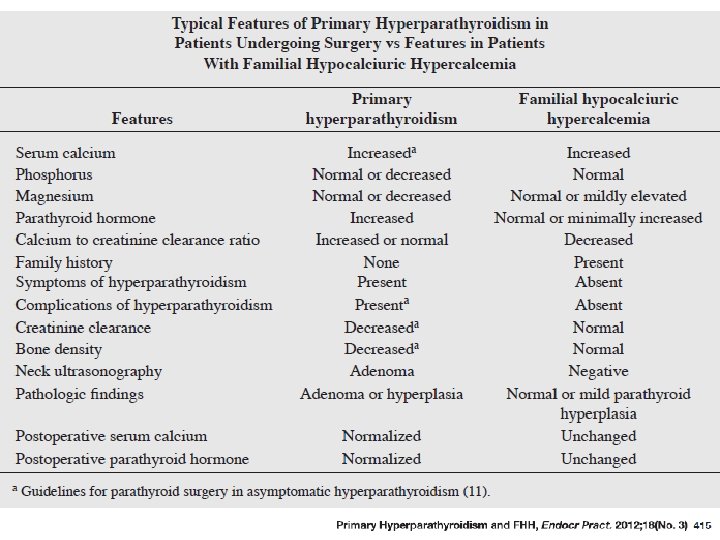
Differential diagnosis of primary hyperparathyroidism, typical laboratory findings 90%
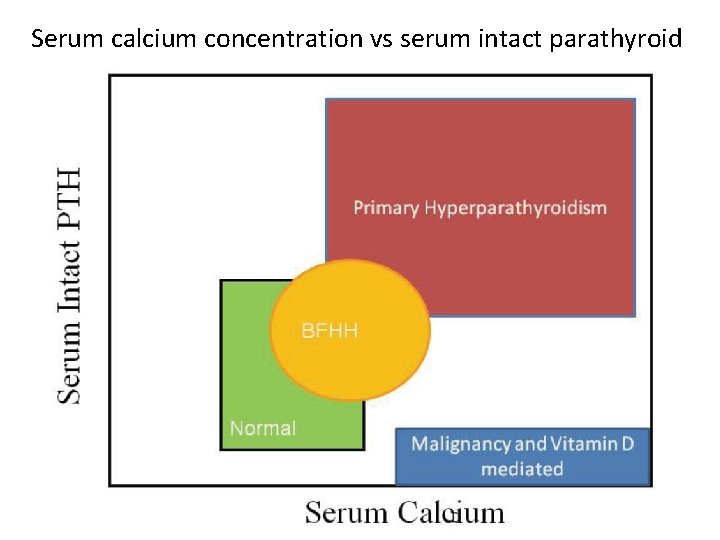
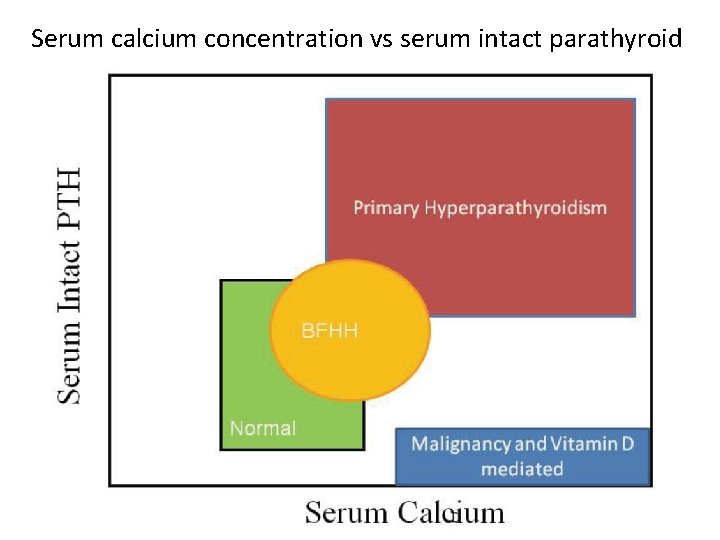
Serum calcium concentration vs serum intact parathyroid hormone
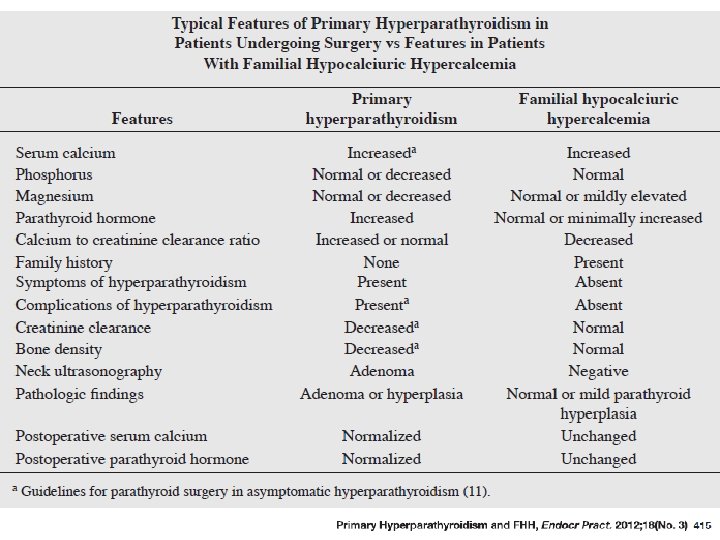
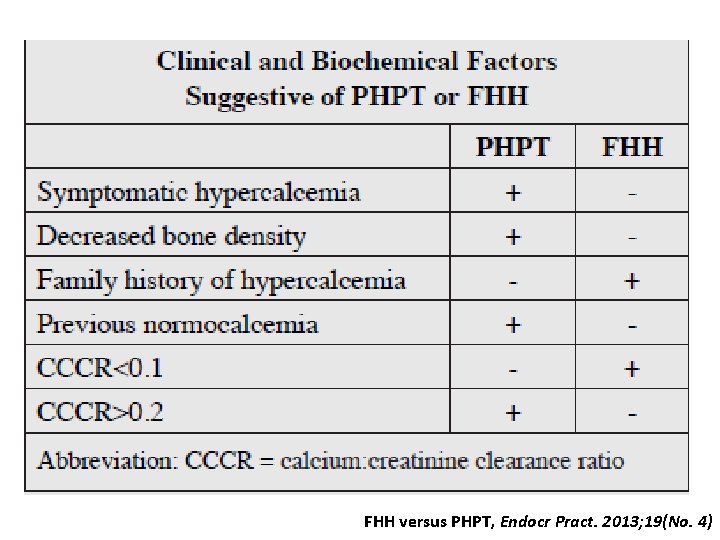
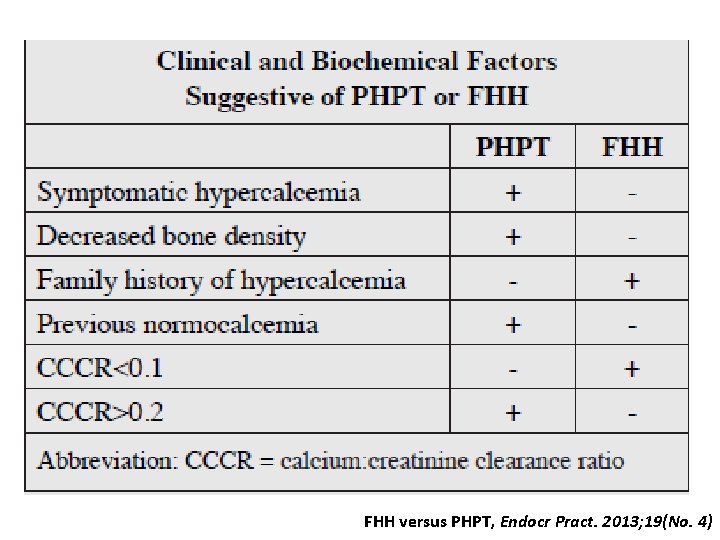
FHH versus PHPT, Endocr Pract. 2013; 19(No. 4)
![Κλασματική απέκρισση Ca CaCr clearance ratio 24 hour Urine Ca x serum Cr Κλασματική απέκρισση Ca Ca/Cr clearance ratio = [24 -hour Urine Ca x serum Cr]](https://slidetodoc.com/presentation_image_h/1a9d3865a17e81b848c87c729f0a05b5/image-72.jpg)
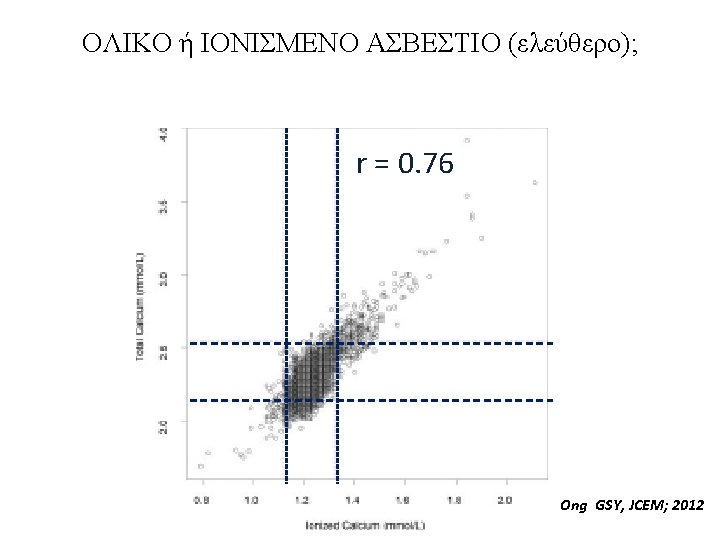
Κλασματική απέκρισση Ca Ca/Cr clearance ratio = [24 -hour Urine Ca x serum Cr] ÷ [Serum Ca x 24 hour Urine Cr] The ratio of calcium (Ca) clearance to creatinine (Cr) clearance may be used for the diagnosis of FHH using the following formula: Cl Ca/ Cl Cr = (Cau x Crs)/Cru x Cas) where Cau = urinary Ca concentration, Crs = serum Cr concentration, Cru = urinary Cr concentration, and Cas = serum Ca concentration. A ratio of 0. 01 or less is typically seen in individuals with FHH.

Diagnostic approach to hypercalcemia
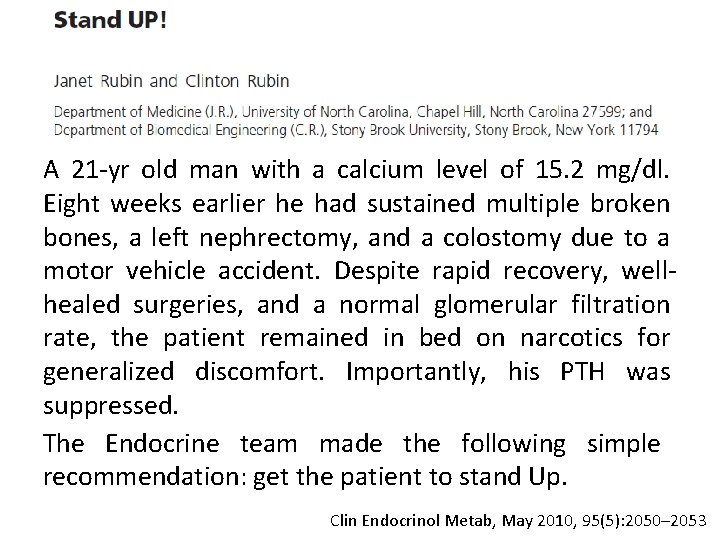
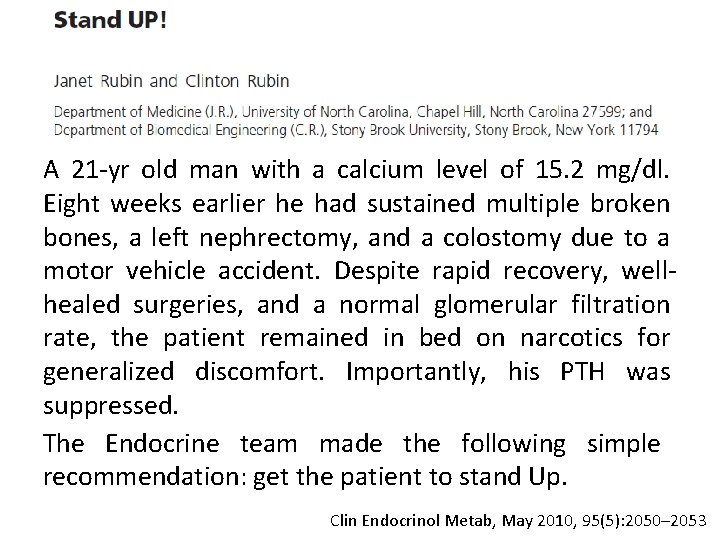
A 21 -yr old man with a calcium level of 15. 2 mg/dl. Eight weeks earlier he had sustained multiple broken bones, a left nephrectomy, and a colostomy due to a motor vehicle accident. Despite rapid recovery, wellhealed surgeries, and a normal glomerular filtration rate, the patient remained in bed on narcotics for generalized discomfort. Importantly, his PTH was suppressed. The Endocrine team made the following simple recommendation: get the patient to stand Up. Clin Endocrinol Metab, May 2010, 95(5): 2050– 2053

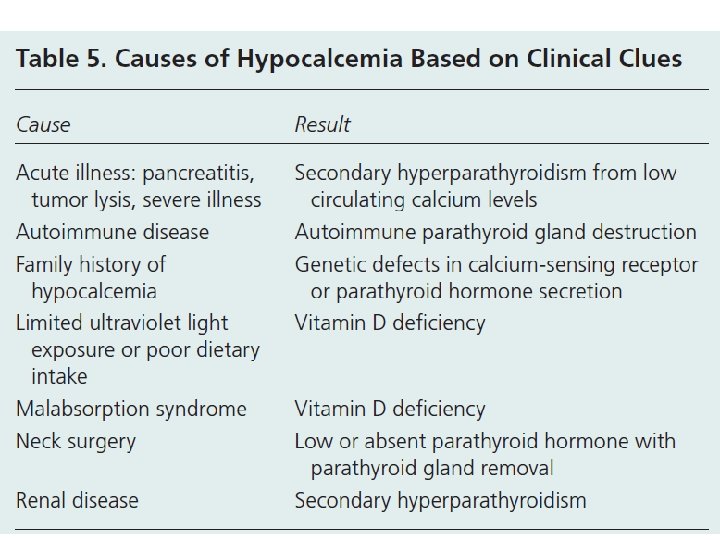
Causes and mechanisms of hypocalcemia Curr Opin Nephrol Hypertens 2013, 22: 371– 376
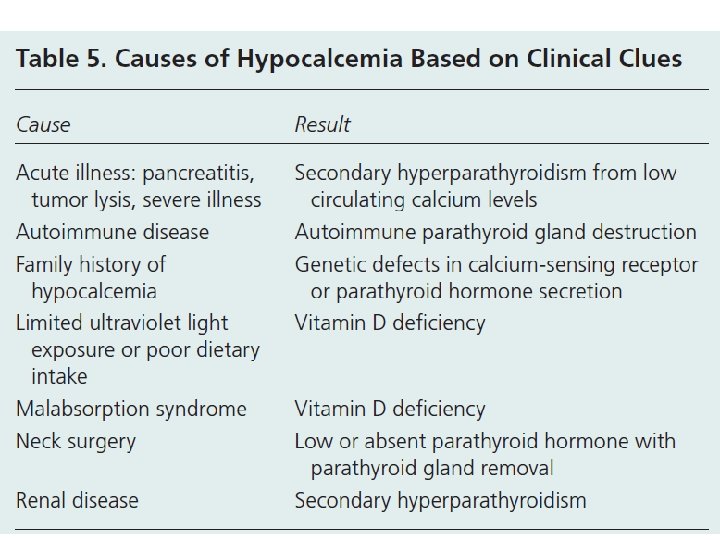

Causes of hypocalcemia

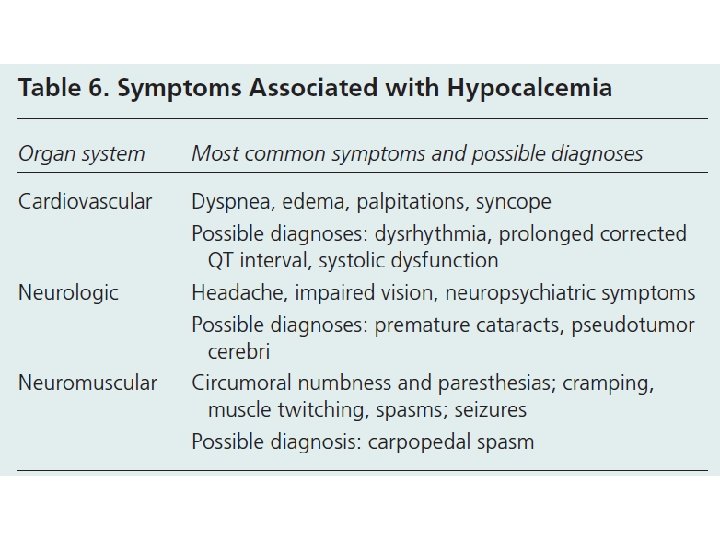

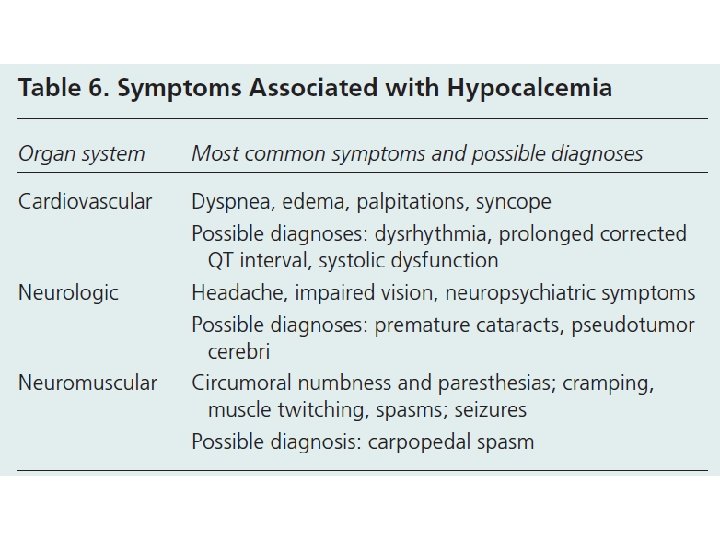
Clinical manifestations of hypocalcemia Prolonged QT interval due to hypocalcemia
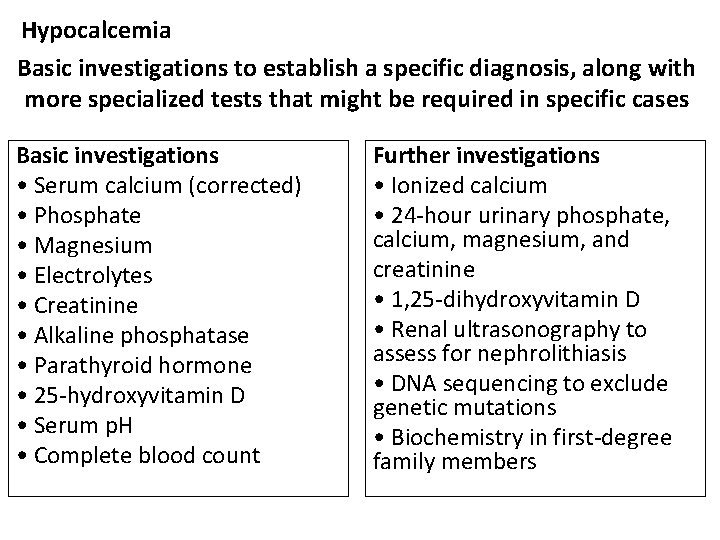
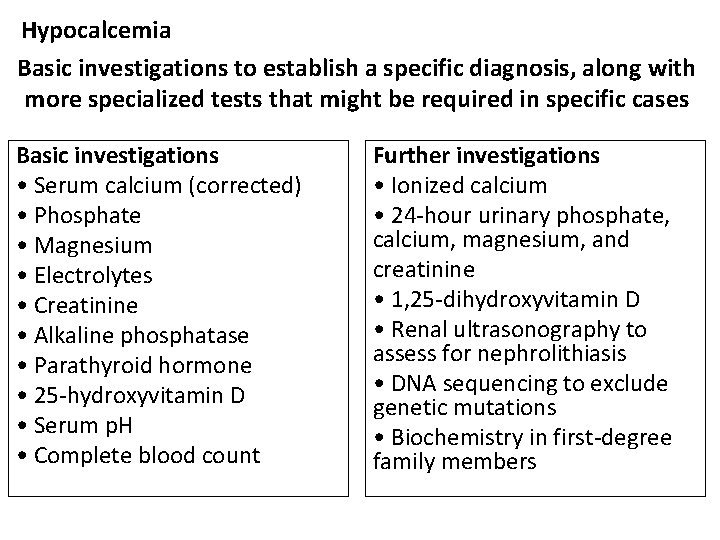
Hypocalcemia Basic investigations to establish a specific diagnosis, along with more specialized tests that might be required in specific cases Basic investigations • Serum calcium (corrected) • Phosphate • Magnesium • Electrolytes • Creatinine • Alkaline phosphatase • Parathyroid hormone • 25 -hydroxyvitamin D • Serum p. H • Complete blood count Further investigations • Ionized calcium • 24 -hour urinary phosphate, calcium, magnesium, and creatinine • 1, 25 -dihydroxyvitamin D • Renal ultrasonography to assess for nephrolithiasis • DNA sequencing to exclude genetic mutations • Biochemistry in first-degree family members
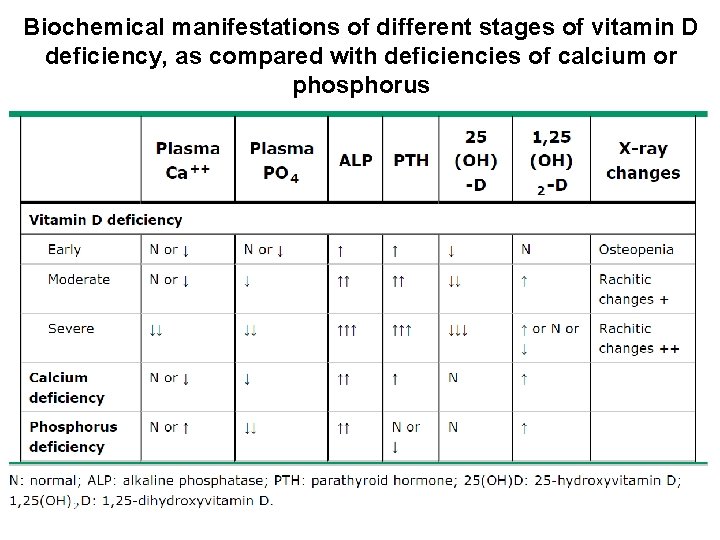
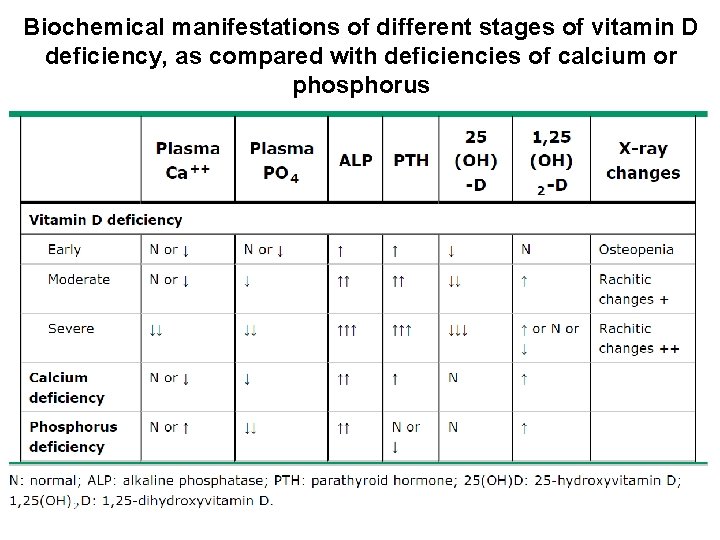
Biochemical manifestations of different stages of vitamin D deficiency, as compared with deficiencies of calcium or phosphorus
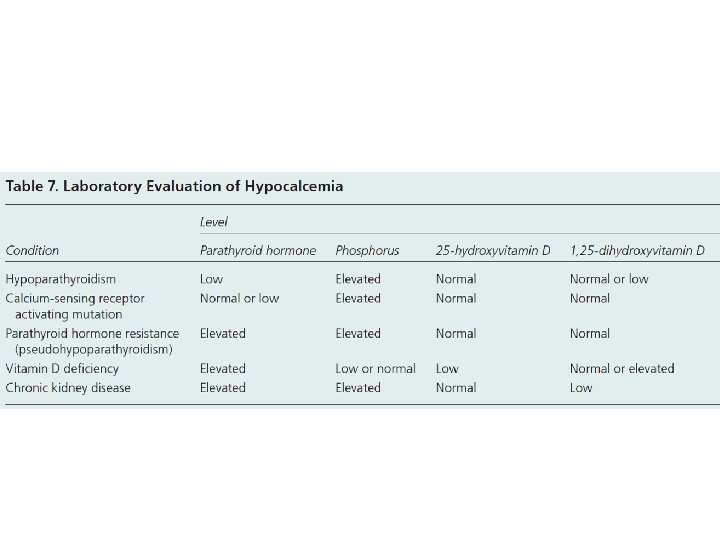
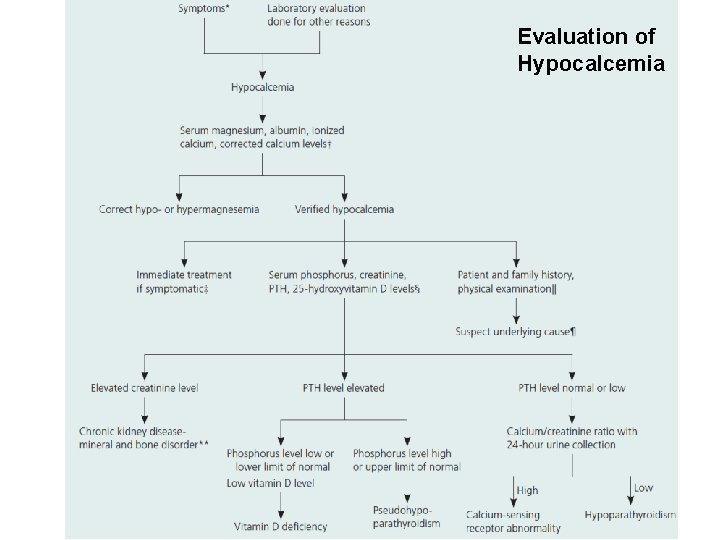
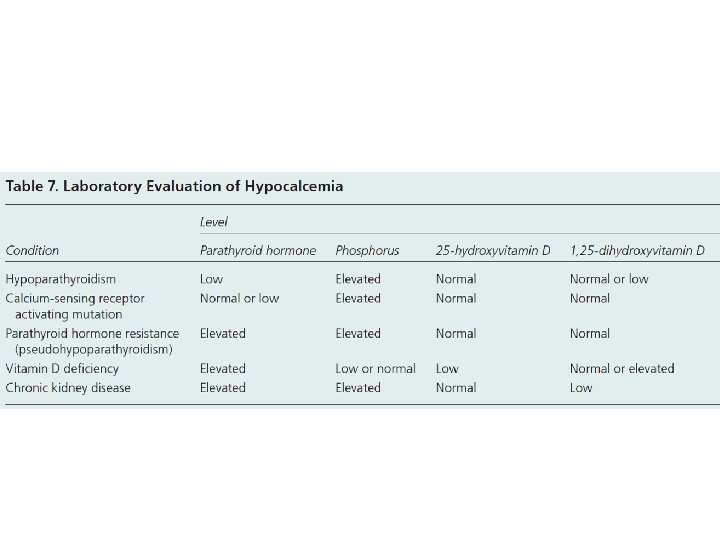
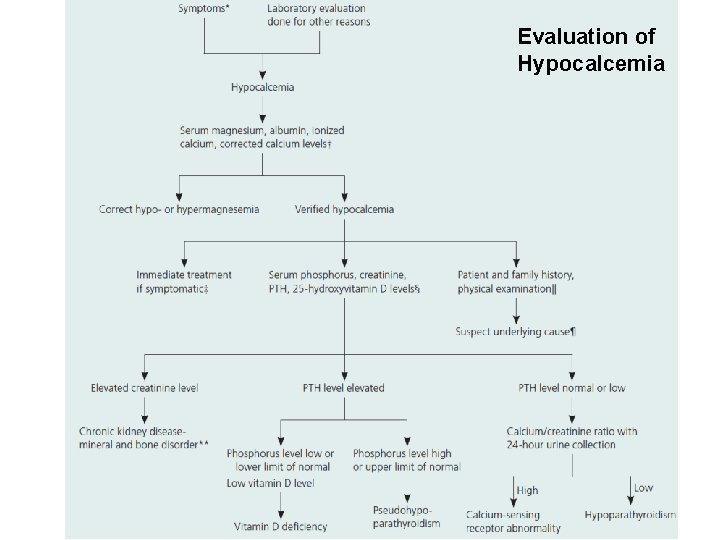
Evaluation of Hypocalcemia





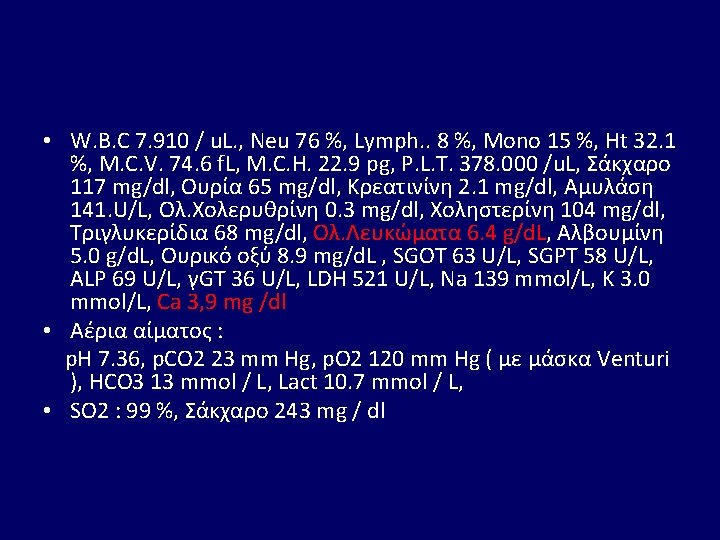
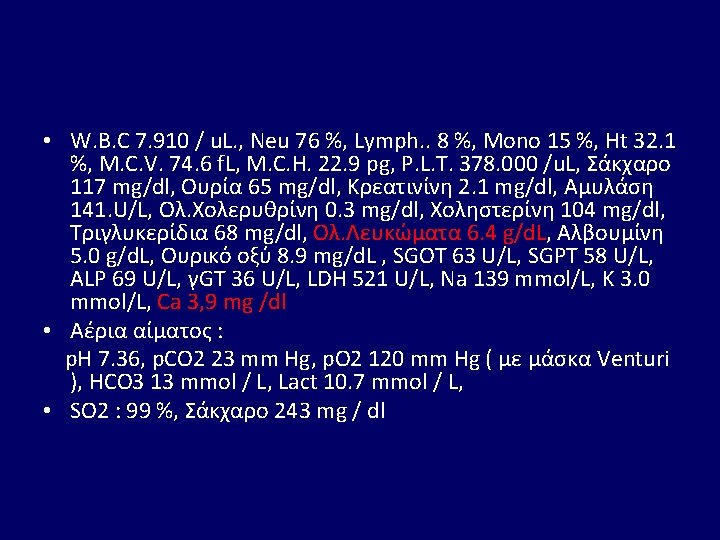
• W. B. C 7. 910 / u. L. , Neu 76 %, Lymph. . 8 %, Mono 15 %, Ht 32. 1 %, M. C. V. 74. 6 f. L, M. C. H. 22. 9 pg, P. L. T. 378. 000 /u. L, Σάκχαρο 117 mg/dl, Ουρία 65 mg/dl, Κρεατινίνη 2. 1 mg/dl, Αμυλάση 141. U/L, Ολ. Χολερυθρίνη 0. 3 mg/dl, Χοληστερίνη 104 mg/dl, Τριγλυκερίδια 68 mg/dl, Ολ. Λευκώματα 6. 4 g/d. L, Αλβουμίνη 5. 0 g/d. L, Ουρικό οξύ 8. 9 mg/d. L , SGOT 63 U/L, SGPT 58 U/L, ALP 69 U/L, γGT 36 U/L, LDH 521 U/L, Na 139 mmol/L, K 3. 0 mmol/L, Ca 3, 9 mg /dl • Αέρια αίματος : p. H 7. 36, p. CO 2 23 mm Hg, p. O 2 120 mm Hg ( με μάσκα Venturi ), HCO 3 13 mmol / L, Lact 10. 7 mmol / L, • SO 2 : 99 %, Σάκχαρο 243 mg / dl






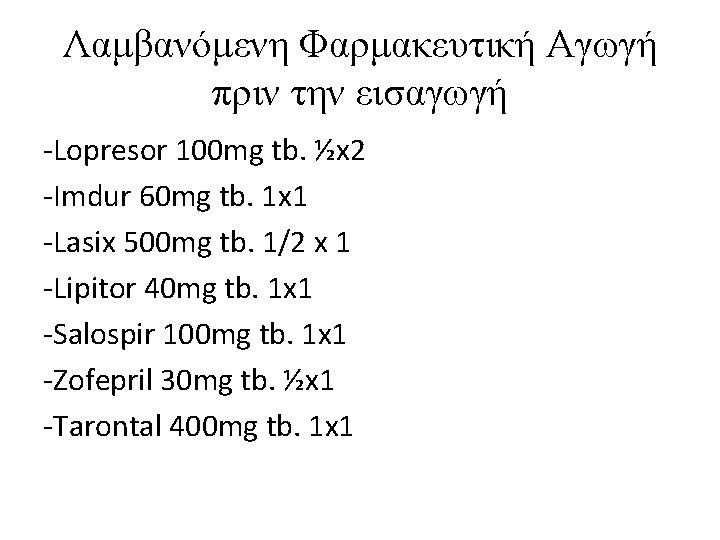
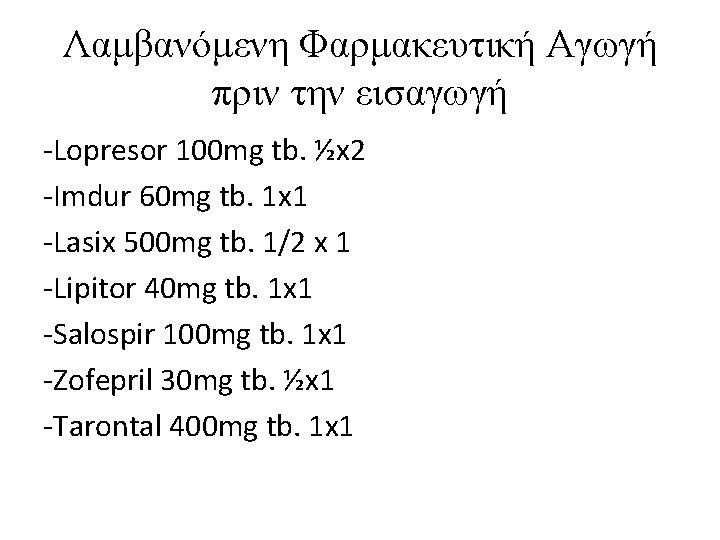
Λαμβανόμενη Φαρμακευτική Αγωγή πριν την εισαγωγή -Lopresor 100 mg tb. ½x 2 -Imdur 60 mg tb. 1 x 1 -Lasix 500 mg tb. 1/2 x 1 -Lipitor 40 mg tb. 1 x 1 -Salospir 100 mg tb. 1 x 1 -Zofepril 30 mg tb. ½x 1 -Tarontal 400 mg tb. 1 x 1
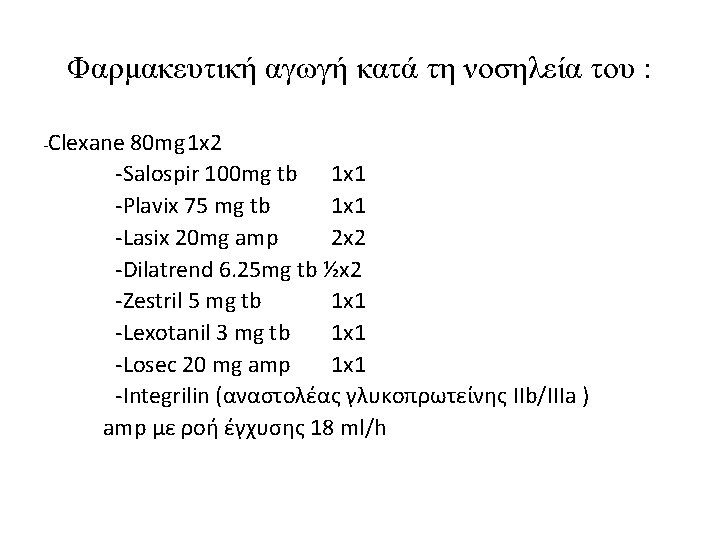
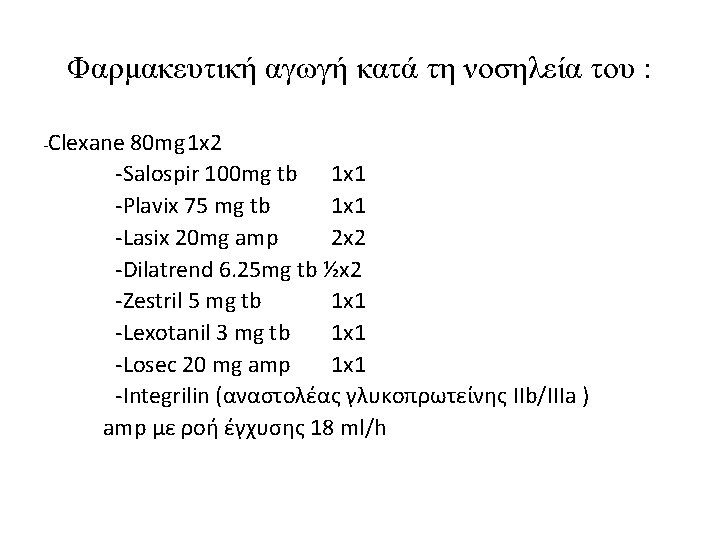
Φαρμακευτική αγωγή κατά τη νοσηλεία του : -Clexane 80 mg 1 x 2 -Salospir 100 mg tb 1 x 1 -Plavix 75 mg tb 1 x 1 -Lasix 20 mg amp 2 x 2 -Dilatrend 6. 25 mg tb ½x 2 -Zestril 5 mg tb 1 x 1 -Lexotanil 3 mg tb 1 x 1 -Losec 20 mg amp 1 x 1 -Integrilin (αναστολέας γλυκοπρωτείνης IIb/IIIa ) amp με ροή έγχυσης 18 ml/h

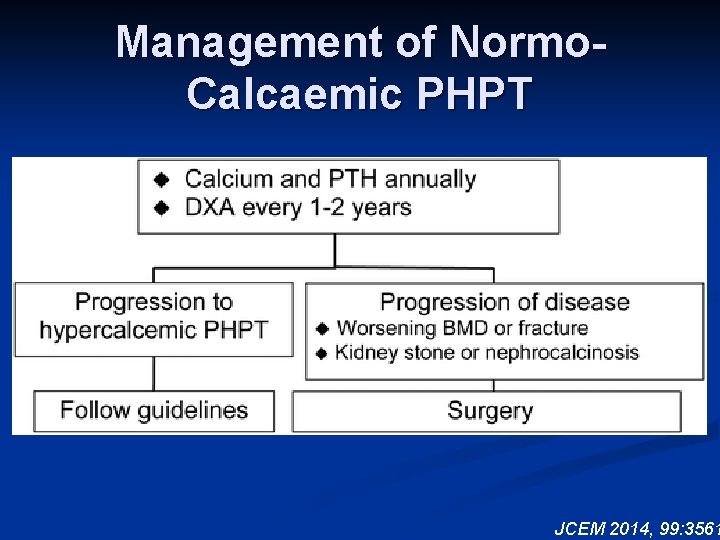
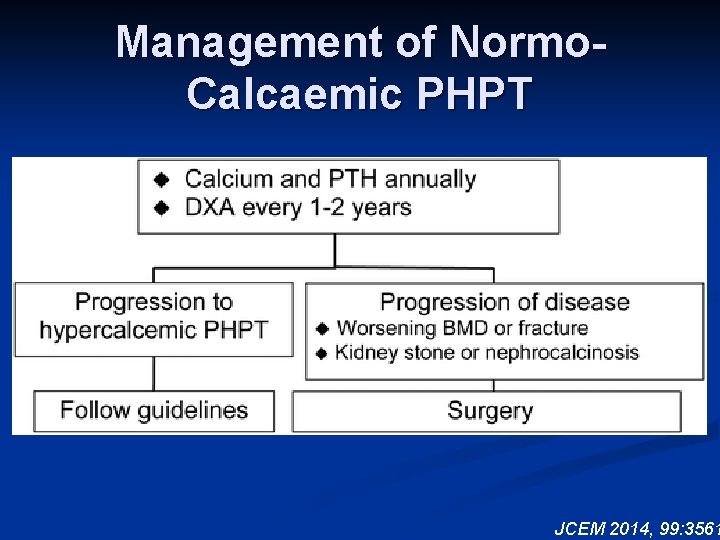
Management of Normo. Calcaemic PHPT JCEM 2014, 99: 3561


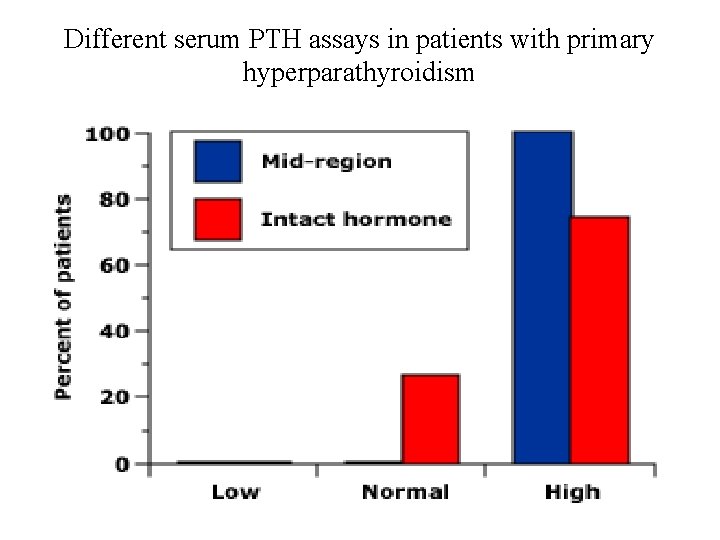
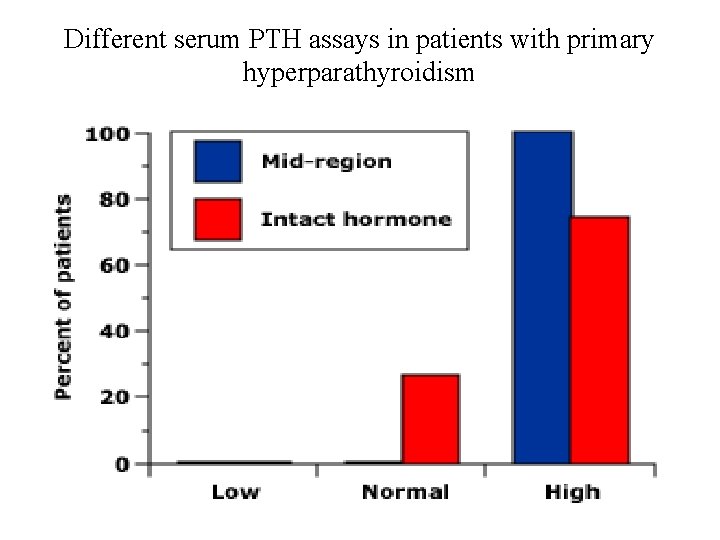
Different serum PTH assays in patients with primary hyperparathyroidism

Different serum (PTH) assays in patients with hypercalcemia of malignancy
 Calcitonin and pth are antagonistic hormones
Calcitonin and pth are antagonistic hormones Pth stable coin
Pth stable coin Serum pth
Serum pth Bone fluid
Bone fluid Pth and calcitonin
Pth and calcitonin Pth function
Pth function Vitamin d and pth
Vitamin d and pth Giorgio spiazzi
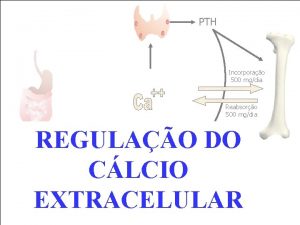
Giorgio spiazzi Bilan calcium
Bilan calcium Mineralização
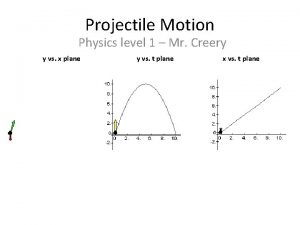
Mineralização Projectile motion formula
Projectile motion formula Compare and contrast essay words
Compare and contrast essay words Total depravity definition
Total depravity definition 1st corinthians 12
1st corinthians 12 Accounting illustration
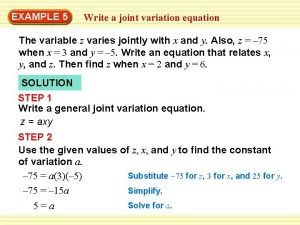
Accounting illustration Example of varies jointly
Example of varies jointly Illustration
Illustration 4 parts of a print ad
4 parts of a print ad Acid rain in germany illustration
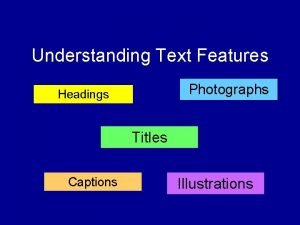
Acid rain in germany illustration Heading text feature
Heading text feature Water pollution and unequal distribution illustration
Water pollution and unequal distribution illustration Neetons second law
Neetons second law Nolco and mcit illustration
Nolco and mcit illustration Pointer illustration
Pointer illustration Aquifer
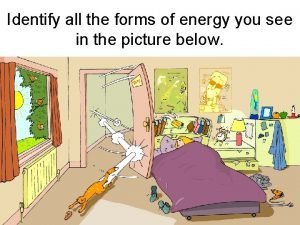
Aquifer List 3 unsafe activities shown in the illustration
List 3 unsafe activities shown in the illustration Pictures of cold fronts
Pictures of cold fronts Types of external conflict
Types of external conflict Pie structure
Pie structure Spousal lifetime access trust diagram
Spousal lifetime access trust diagram Energy transformation of blender
Energy transformation of blender Parts of projectile motion illustration
Parts of projectile motion illustration Production illustration
Production illustration Clock energy transformation
Clock energy transformation Example of rhetorical modes
Example of rhetorical modes Mil picture analysis
Mil picture analysis The bridge illustration
The bridge illustration Bioflix activity: how synapses work -- events at a synapse
Bioflix activity: how synapses work -- events at a synapse Les arbres des villes poésie georges drouillat
Les arbres des villes poésie georges drouillat What is the multiplier effect in travel and tourism
What is the multiplier effect in travel and tourism Traverse stage diagram
Traverse stage diagram Illustration of the steps in restriction digestion and pcr
Illustration of the steps in restriction digestion and pcr Core in the earth
Core in the earth Cyanmethemoglobin colour
Cyanmethemoglobin colour Objectives of work immersion sample
Objectives of work immersion sample I look carefully on the titles illustration
I look carefully on the titles illustration Pie paragraph structure examples
Pie paragraph structure examples Apollinaire les sapins
Apollinaire les sapins What is betty doing wrong lab safety
What is betty doing wrong lab safety Meeting illustration
Meeting illustration Metamorphic rock to igneous rock
Metamorphic rock to igneous rock Illustration of molecules
Illustration of molecules Examples of points lines and planes
Examples of points lines and planes Confidence interval illustration
Confidence interval illustration Janet waking poem
Janet waking poem Precipitation illustration
Precipitation illustration Paraphrasing mini lesson
Paraphrasing mini lesson Ssq illustration software
Ssq illustration software Jelaskan teori domino munculnya resiko kerugian
Jelaskan teori domino munculnya resiko kerugian Task 1 rewrite the following text in a more academic style
Task 1 rewrite the following text in a more academic style The plan of salvation diagram
The plan of salvation diagram Charles law examples
Charles law examples Activity 1.picture identification
Activity 1.picture identification Bergres
Bergres The bridge illustration
The bridge illustration Rees and ecker method procedure drawing
Rees and ecker method procedure drawing List 3 unsafe activities shown in the illustration
List 3 unsafe activities shown in the illustration Science lab safety comic strip
Science lab safety comic strip Shitao landscape
Shitao landscape Two neutral conducting pop cans are touching each other
Two neutral conducting pop cans are touching each other Very descriptive
Very descriptive Energy transformation of blender
Energy transformation of blender Bridge illustration gospel
Bridge illustration gospel Persuasion pattern of development
Persuasion pattern of development Juxtaposition illustration
Juxtaposition illustration Daisyworld model report with illustration
Daisyworld model report with illustration Holiness illustration
Holiness illustration Mapping illustration
Mapping illustration Identify media and graphic software
Identify media and graphic software Ritual or expressive model of communication
Ritual or expressive model of communication State charle's law.
State charle's law. Secondary sources meaning
Secondary sources meaning Parallel circuit short circuit
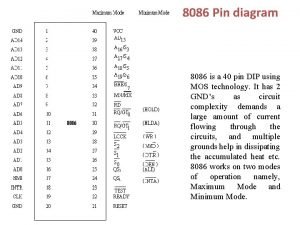
Parallel circuit short circuit 40 pin diagram
40 pin diagram Xccbx
Xccbx Isp lever
Isp lever Schematic diagram of soxhlet extractor
Schematic diagram of soxhlet extractor Hydraulic schematic symbols
Hydraulic schematic symbols Mass spectrometry schematic diagram
Mass spectrometry schematic diagram Hydraulic pump diagram
Hydraulic pump diagram Schematic design proposal
Schematic design proposal Layout nand
Layout nand 5687 preamp schematic
5687 preamp schematic Lighting designers baltimore
Lighting designers baltimore ø electrical symbol
ø electrical symbol Noise ensemble schematic
Noise ensemble schematic Free cooling chiller schematic
Free cooling chiller schematic Edm arc generator schematic
Edm arc generator schematic Two technicians are discussing schematic symbols
Two technicians are discussing schematic symbols Pneumatic schematic examples
Pneumatic schematic examples Block diagram of a measurement system
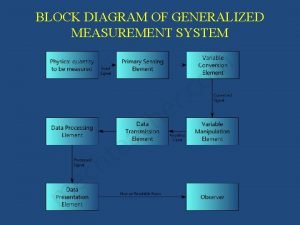
Block diagram of a measurement system Schematic diagram of series circuit
Schematic diagram of series circuit Schematic play
Schematic play Kelsey-hayes abs module diagram
Kelsey-hayes abs module diagram Swapping chapter 6
Swapping chapter 6 Schematic diagram of group 2 cations
Schematic diagram of group 2 cations