Hypertensive disorders in pregnancy a major cause of


- Slides: 43

Hypertensive disorders in pregnancy: a major cause of l maternal l fetal l neonatal morbidity and mortality
Pregnant women with hypertension at higher risk for l abruptio placentae l cerebrovascular events l organ failure l DIC
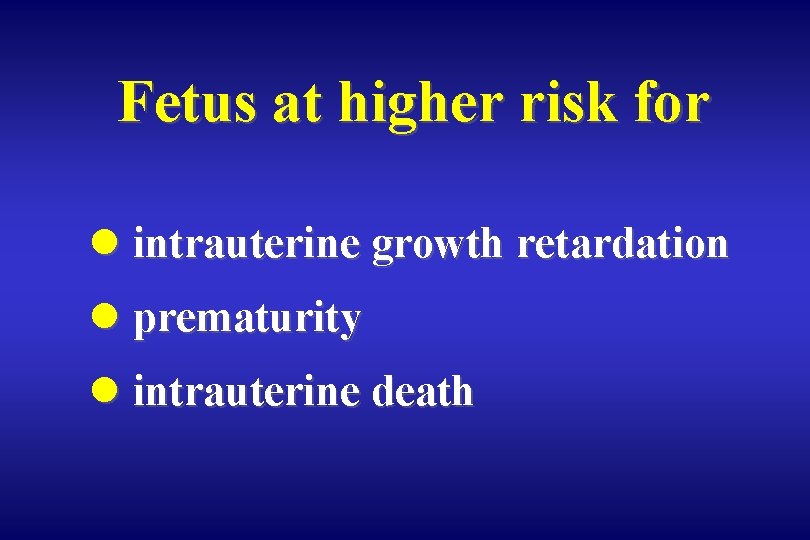
Fetus at higher risk for l intrauterine growth retardation l prematurity l intrauterine death
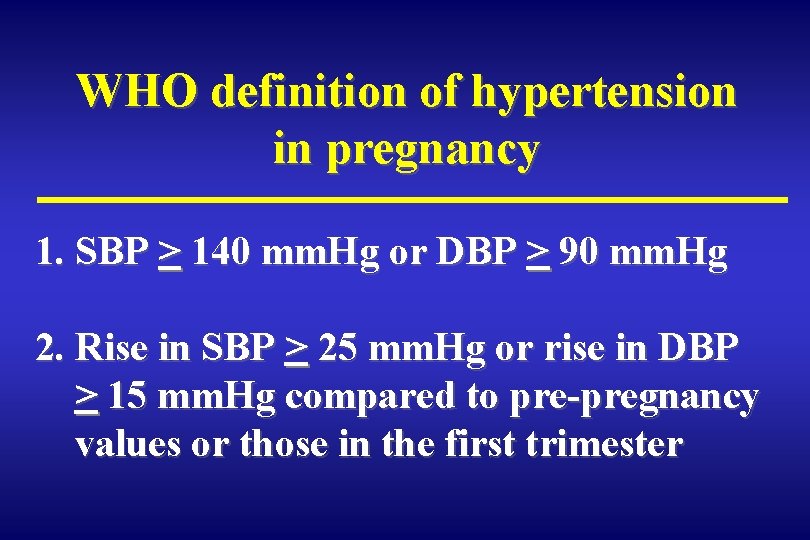
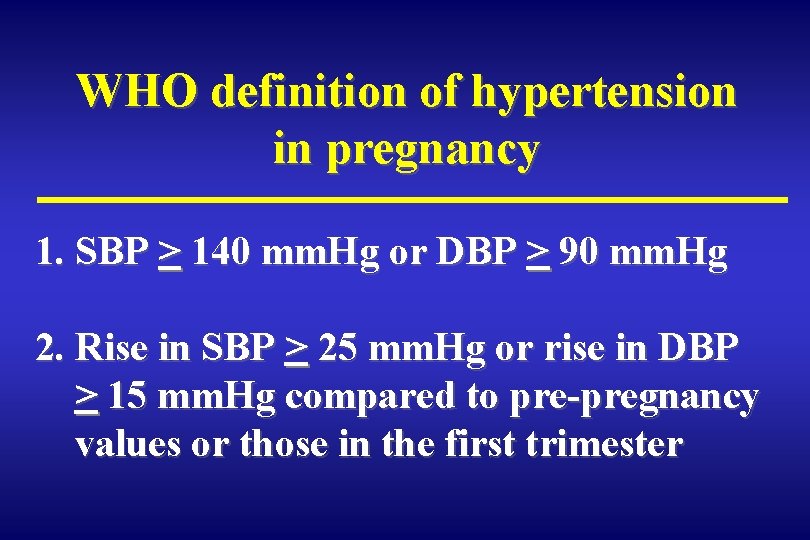
WHO definition of hypertension in pregnancy 1. SBP > 140 mm. Hg or DBP > 90 mm. Hg 2. Rise in SBP > 25 mm. Hg or rise in DBP > 15 mm. Hg compared to pre-pregnancy values or those in the first trimester
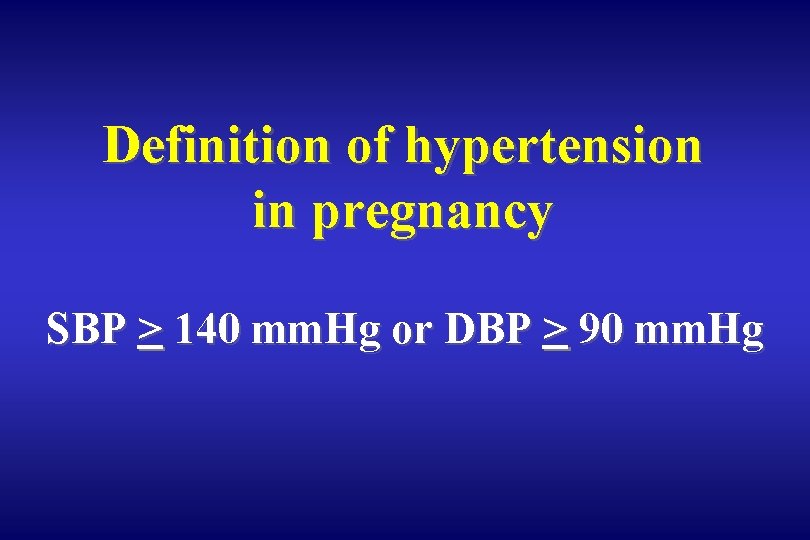
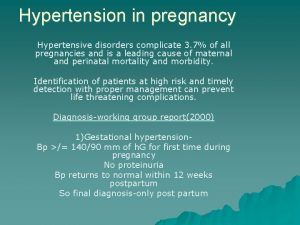
Definition of hypertension in pregnancy SBP > 140 mm. Hg or DBP > 90 mm. Hg
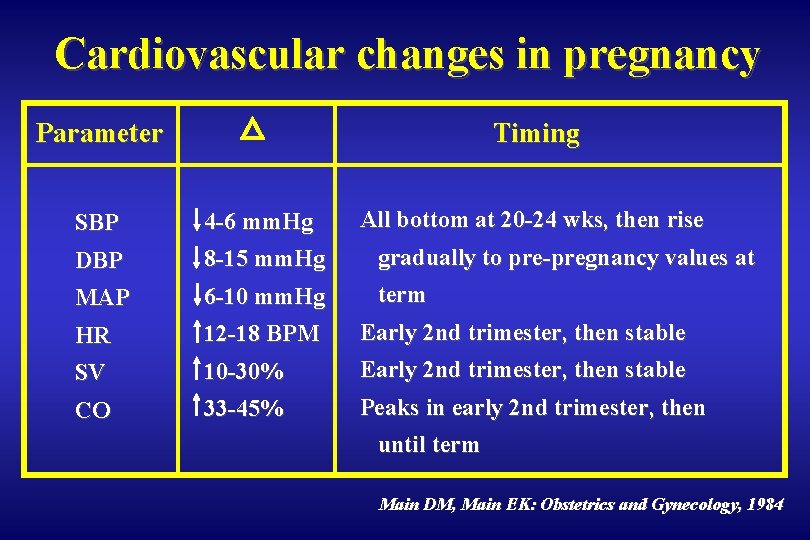
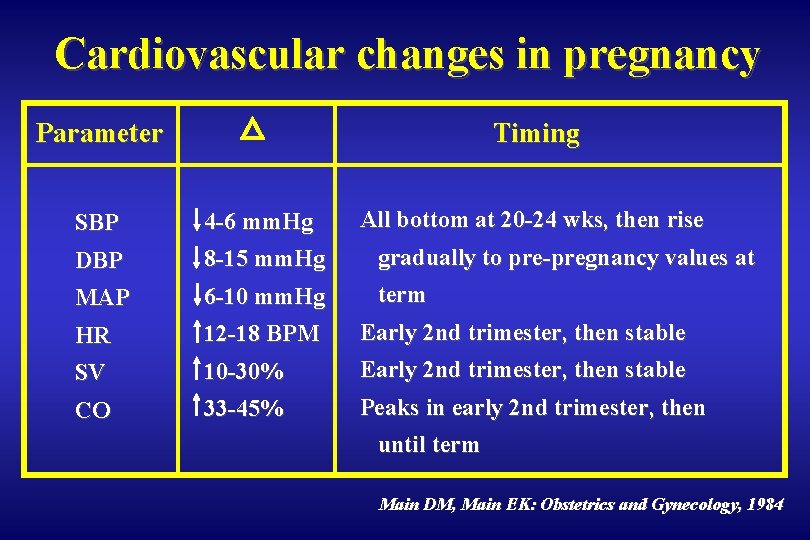
Cardiovascular changes in pregnancy Parameter Timing All bottom at 20 -24 wks, then rise SBP 4 -6 mm. Hg DBP 8 -15 mm. Hg gradually to pre-pregnancy values at MAP 6 -10 mm. Hg term HR 12 -18 BPM Early 2 nd trimester, then stable SV 10 -30% Early 2 nd trimester, then stable CO 33 -45% Peaks in early 2 nd trimester, then until term Main DM, Main EK: Obstetrics and Gynecology, 1984
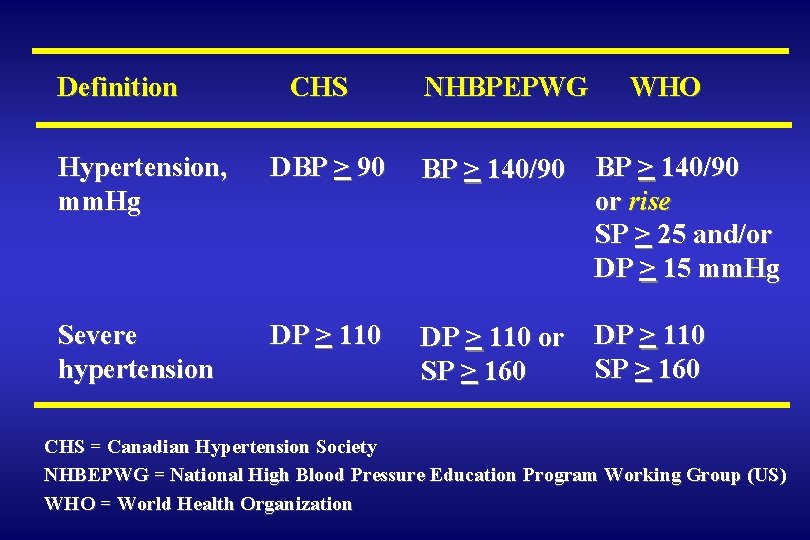
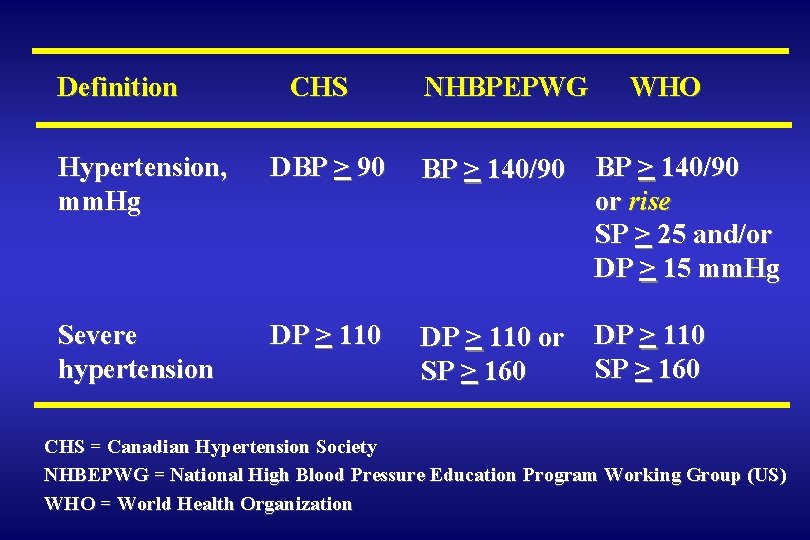
Definition CHS NHBPEPWG WHO Hypertension, mm. Hg DBP > 90 BP > 140/90 or rise SP > 25 and/or DP > 15 mm. Hg Severe hypertension DP > 110 or SP > 160 DP > 110 SP > 160 CHS = Canadian Hypertension Society NHBEPWG = National High Blood Pressure Education Program Working Group (US) WHO = World Health Organization
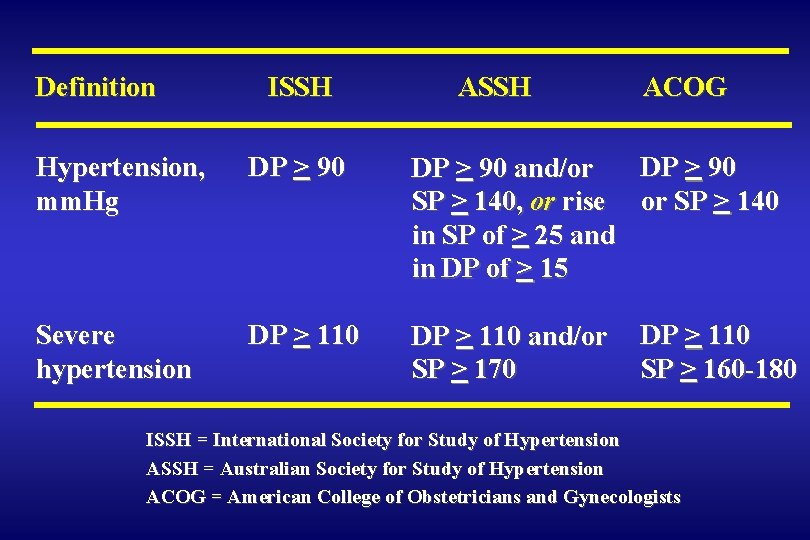
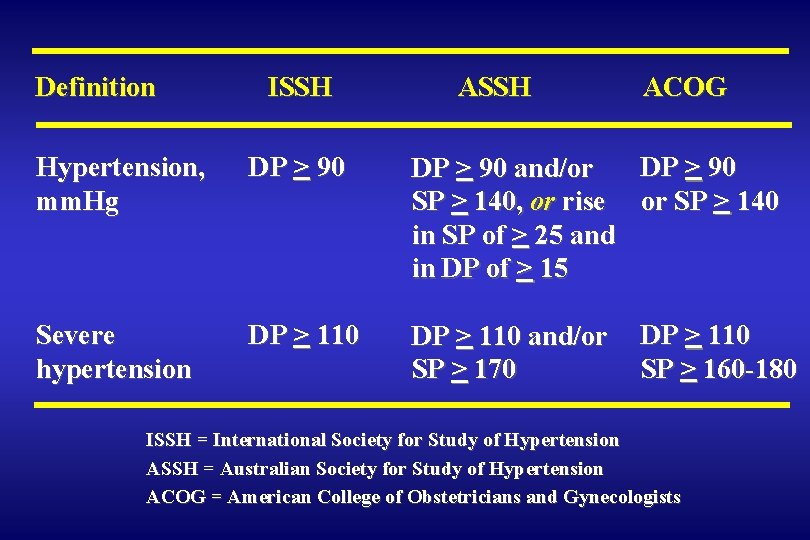
Definition ISSH ACOG Hypertension, mm. Hg DP > 90 and/or SP > 140, or rise or SP > 140 in SP of > 25 and in DP of > 15 Severe hypertension DP > 110 and/or SP > 170 DP > 110 SP > 160 -180 ISSH = International Society for Study of Hypertension ASSH = Australian Society for Study of Hypertension ACOG = American College of Obstetricians and Gynecologists
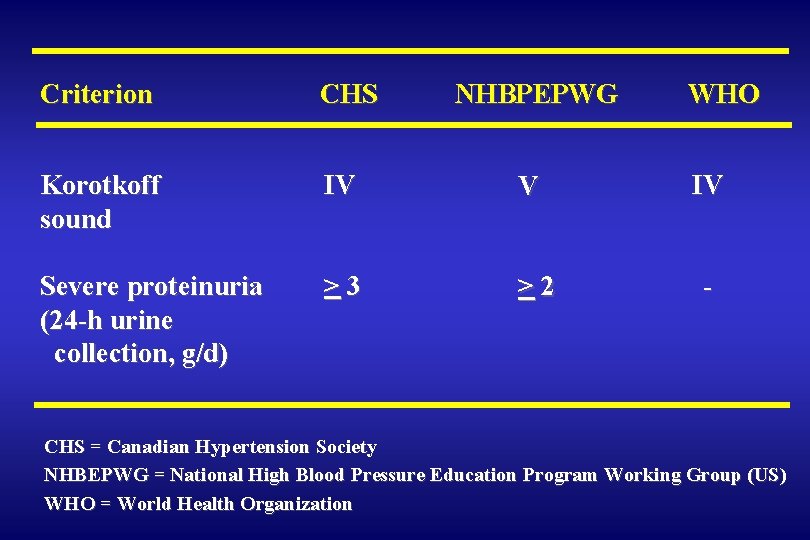
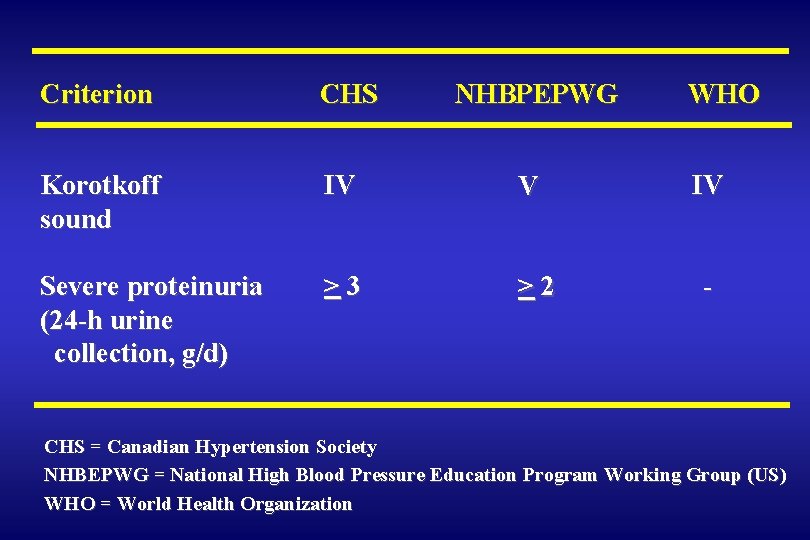
Criterion CHS NHBPEPWG WHO Korotkoff sound IV V IV Severe proteinuria (24 -h urine collection, g/d) >3 >2 - CHS = Canadian Hypertension Society NHBEPWG = National High Blood Pressure Education Program Working Group (US) WHO = World Health Organization
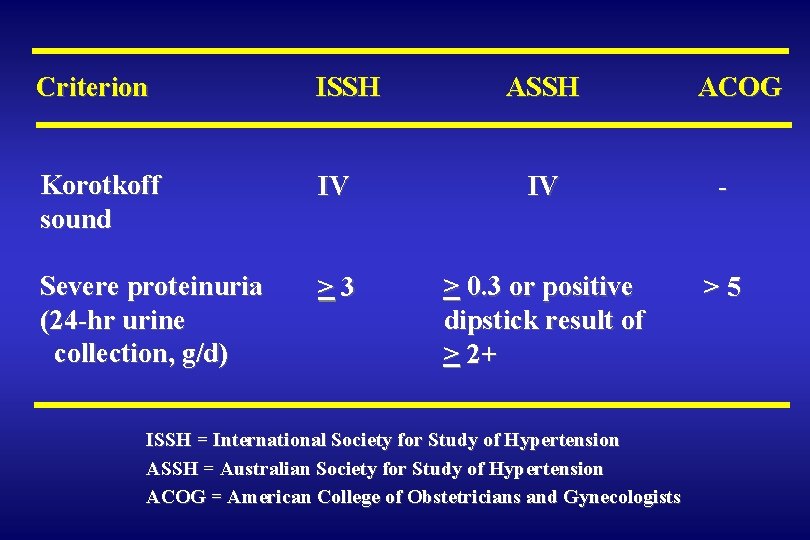
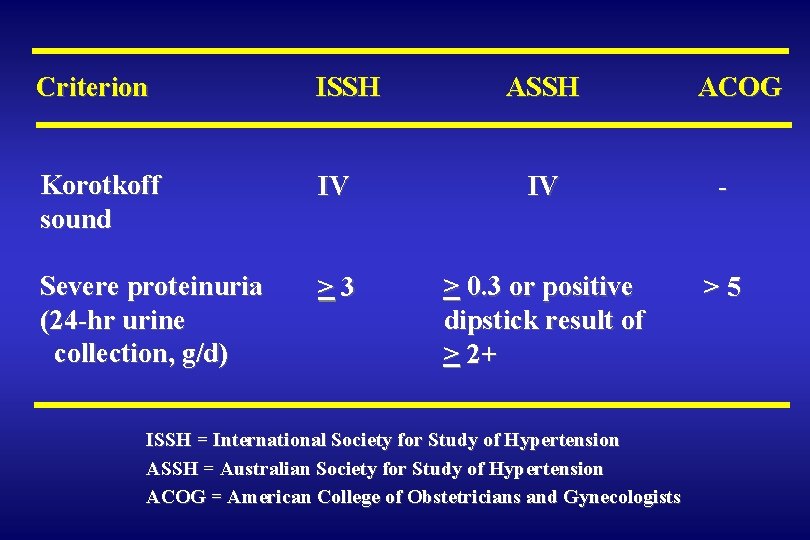
Criterion ISSH ASSH Korotkoff sound IV IV - Severe proteinuria (24 -hr urine collection, g/d) >3 > 0. 3 or positive dipstick result of > 2+ >5 ISSH = International Society for Study of Hypertension ASSH = Australian Society for Study of Hypertension ACOG = American College of Obstetricians and Gynecologists ACOG
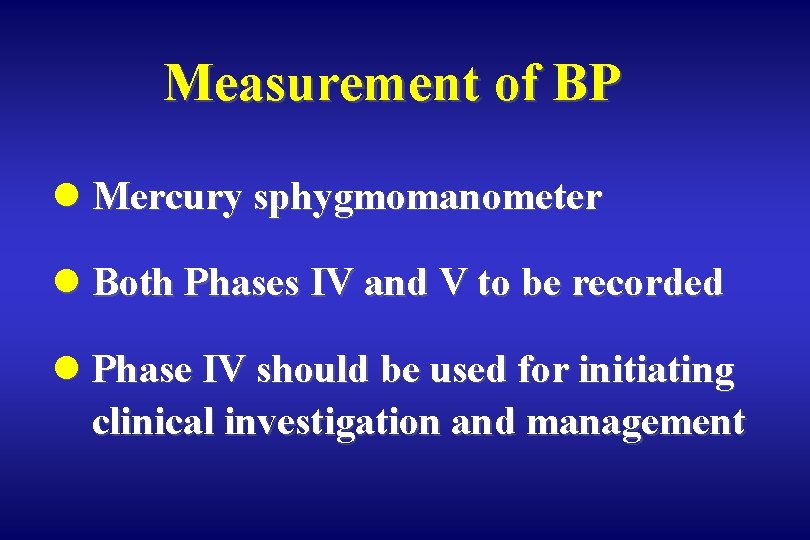
Measurement of BP l Mercury sphygmomanometer l Both Phases IV and V to be recorded l Phase IV should be used for initiating clinical investigation and management
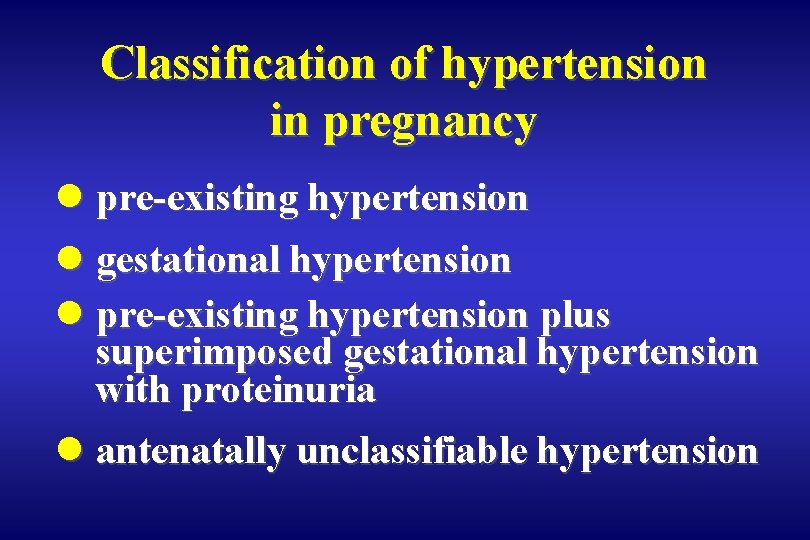
Classification of hypertension in pregnancy l pre-existing hypertension l gestational hypertension l pre-existing hypertension plus superimposed gestational hypertension with proteinuria l antenatally unclassifiable hypertension
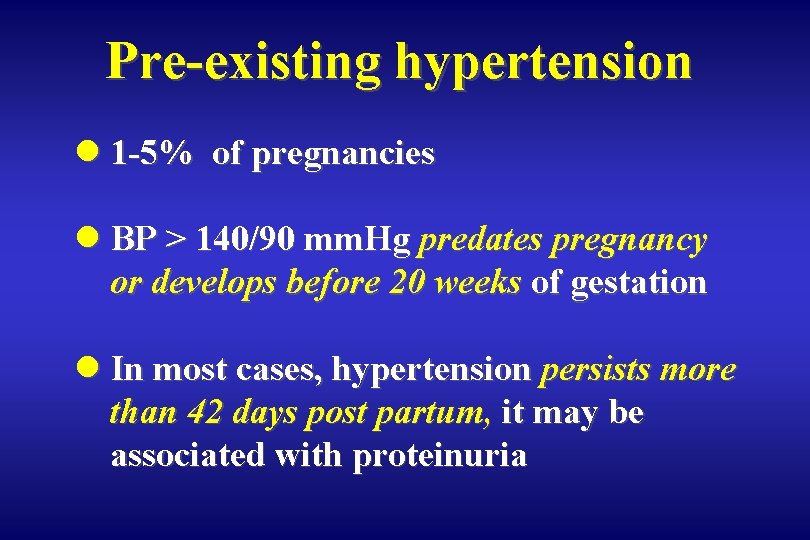
Pre-existing hypertension l 1 -5% of pregnancies l BP > 140/90 mm. Hg predates pregnancy or develops before 20 weeks of gestation l In most cases, hypertension persists more than 42 days post partum, it may be associated with proteinuria
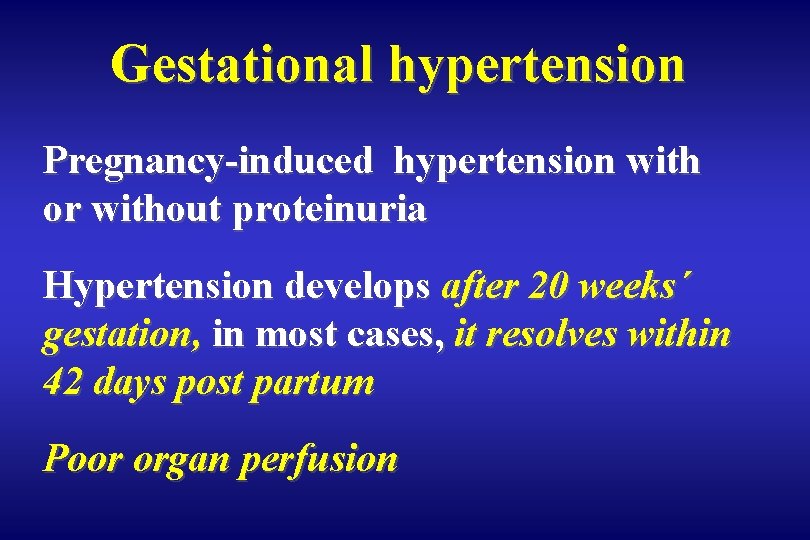
Gestational hypertension Pregnancy-induced hypertension with or without proteinuria Hypertension develops after 20 weeks´ gestation, in most cases, it resolves within 42 days post partum Poor organ perfusion
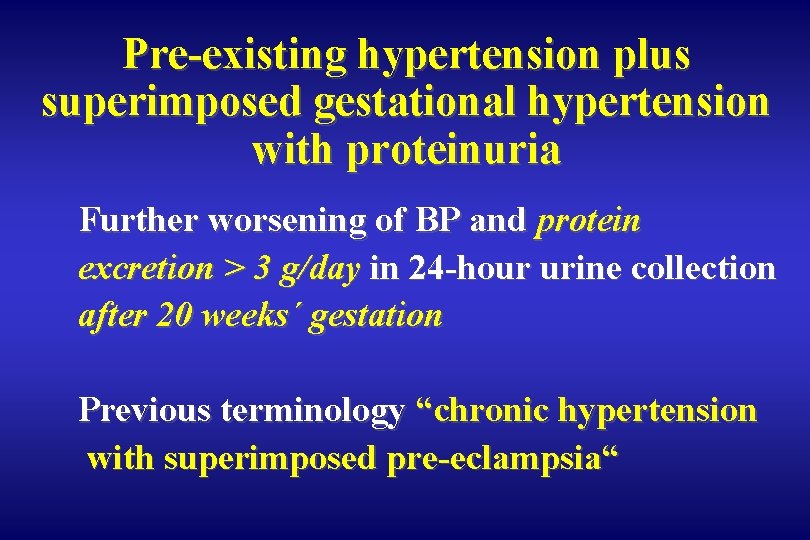
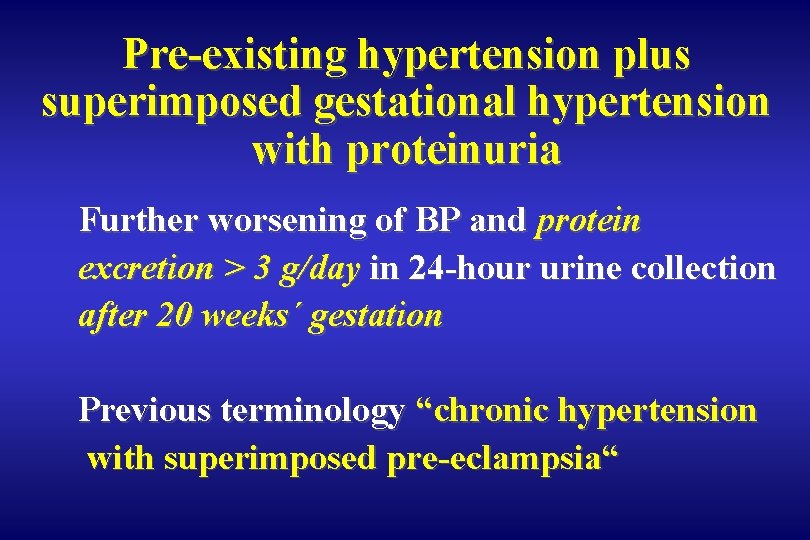
Pre-existing hypertension plus superimposed gestational hypertension with proteinuria Further worsening of BP and protein excretion > 3 g/day in 24 -hour urine collection after 20 weeks´ gestation Previous terminology “chronic hypertension with superimposed pre-eclampsia“
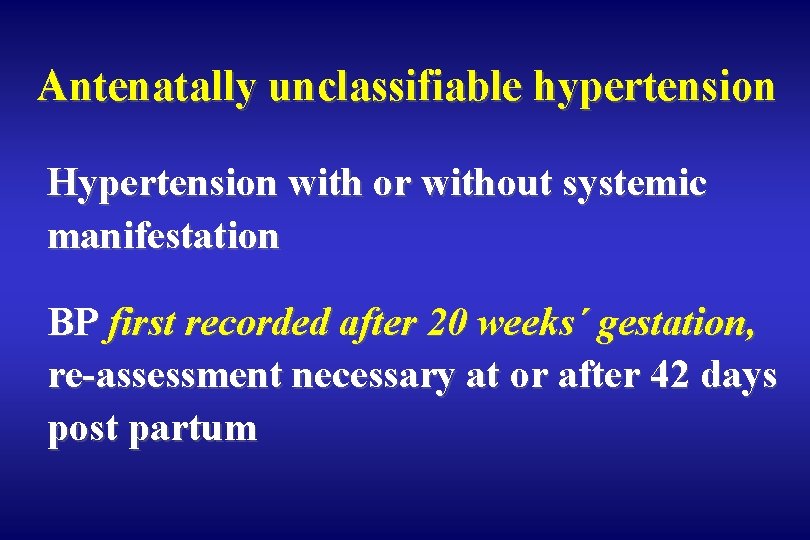
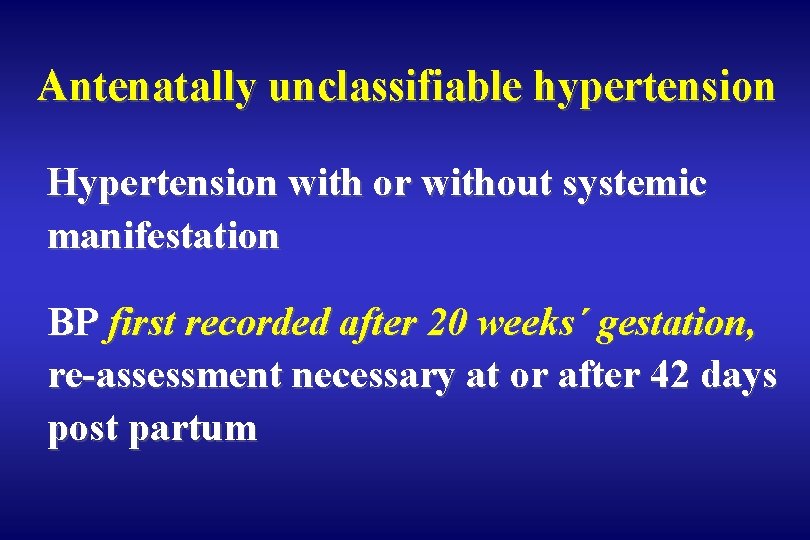
Antenatally unclassifiable hypertension Hypertension with or without systemic manifestation BP first recorded after 20 weeks´ gestation, re-assessment necessary at or after 42 days post partum
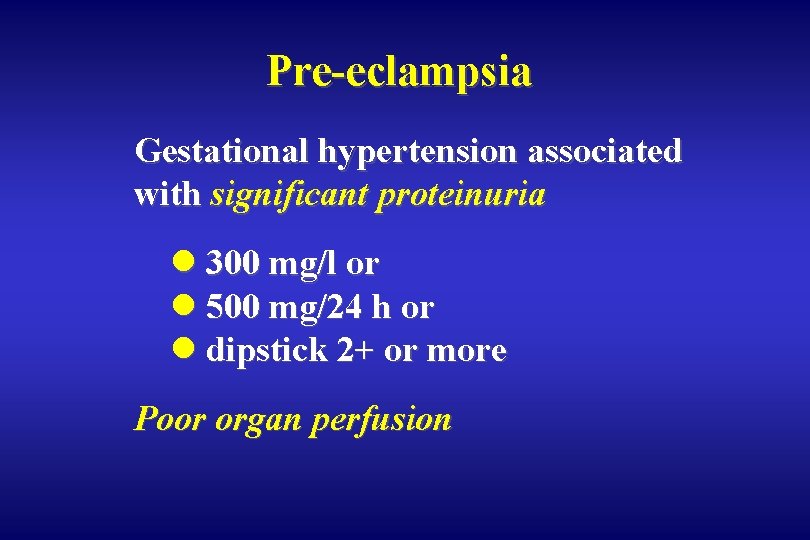
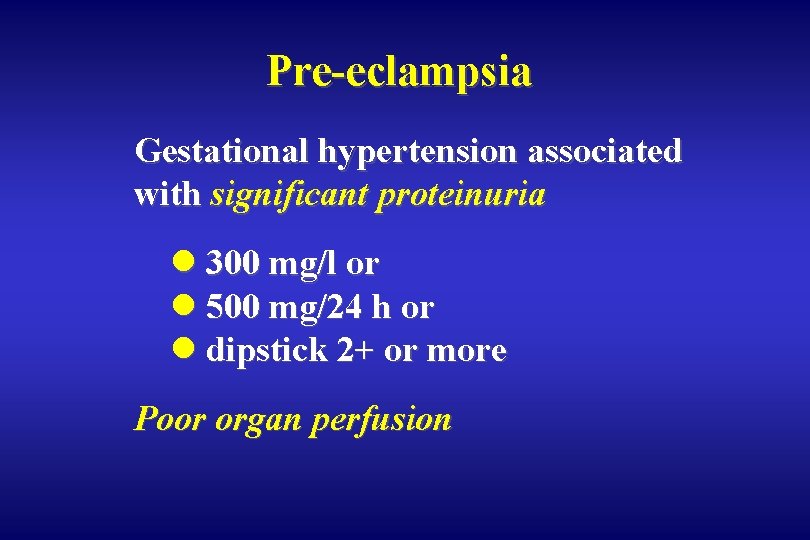
Pre-eclampsia Gestational hypertension associated with significant proteinuria l 300 mg/l or l 500 mg/24 h or l dipstick 2+ or more Poor organ perfusion
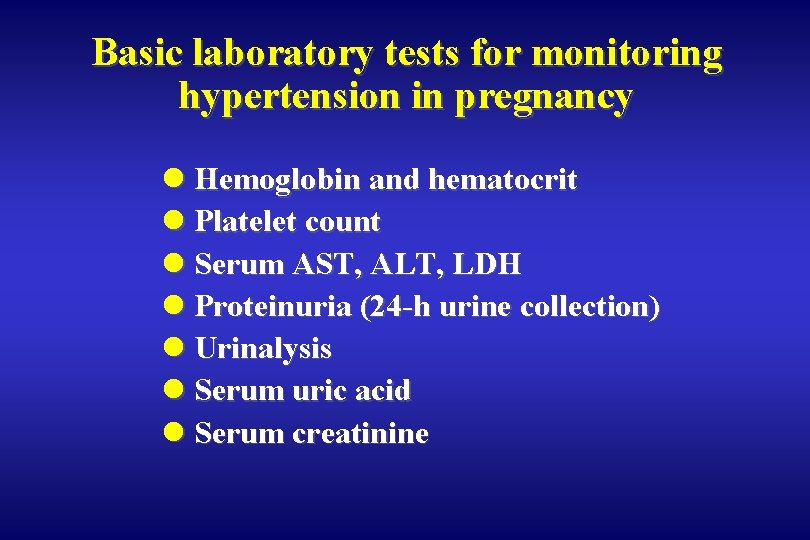
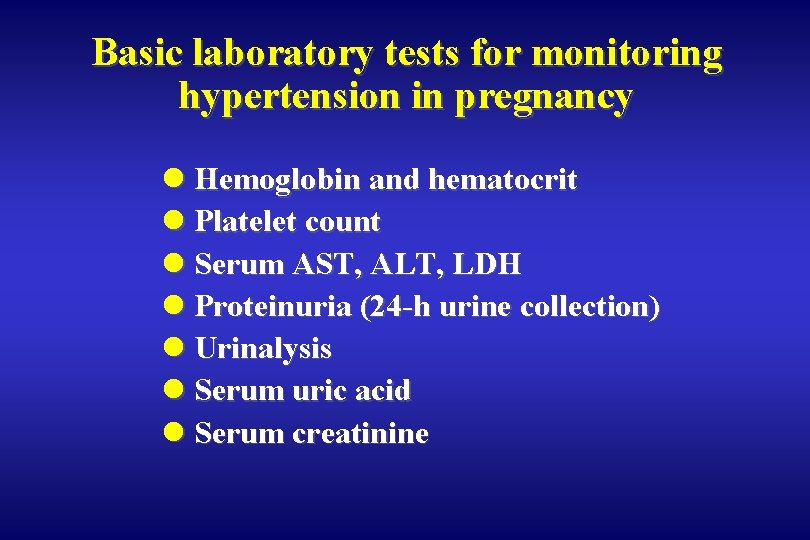
Basic laboratory tests for monitoring hypertension in pregnancy l Hemoglobin and hematocrit l Platelet count l Serum AST, ALT, LDH l Proteinuria (24 -h urine collection) l Urinalysis l Serum uric acid l Serum creatinine
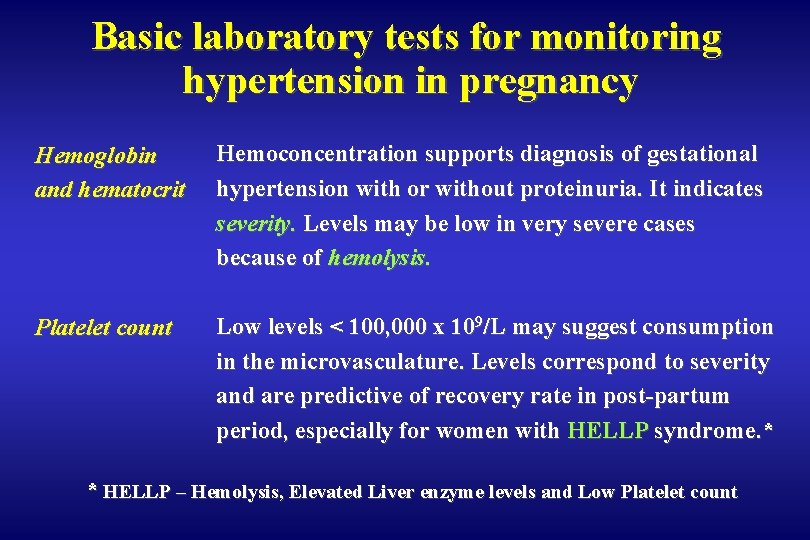
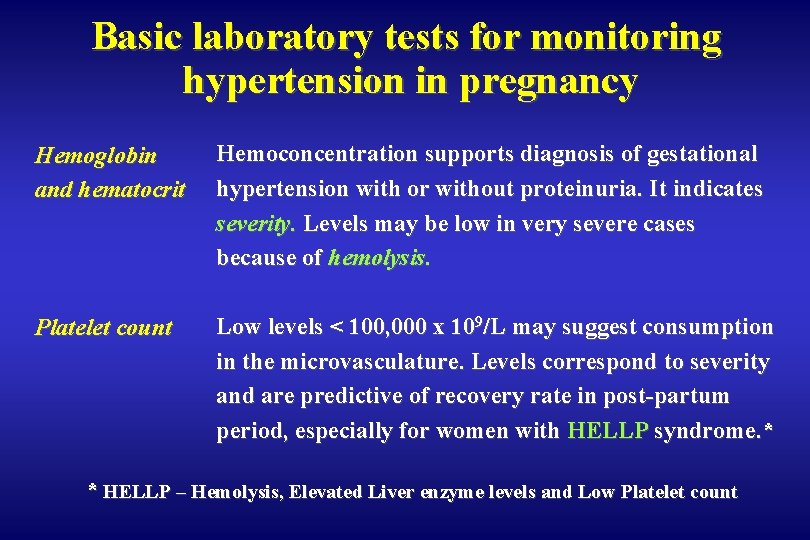
Basic laboratory tests for monitoring hypertension in pregnancy Hemoglobin and hematocrit Hemoconcentration supports diagnosis of gestational hypertension with or without proteinuria. It indicates severity. Levels may be low in very severe cases because of hemolysis. Platelet count Low levels < 100, 000 x 109/L may suggest consumption in the microvasculature. Levels correspond to severity and are predictive of recovery rate in post-partum period, especially for women with HELLP syndrome. * * HELLP – Hemolysis, Elevated Liver enzyme levels and Low Platelet count
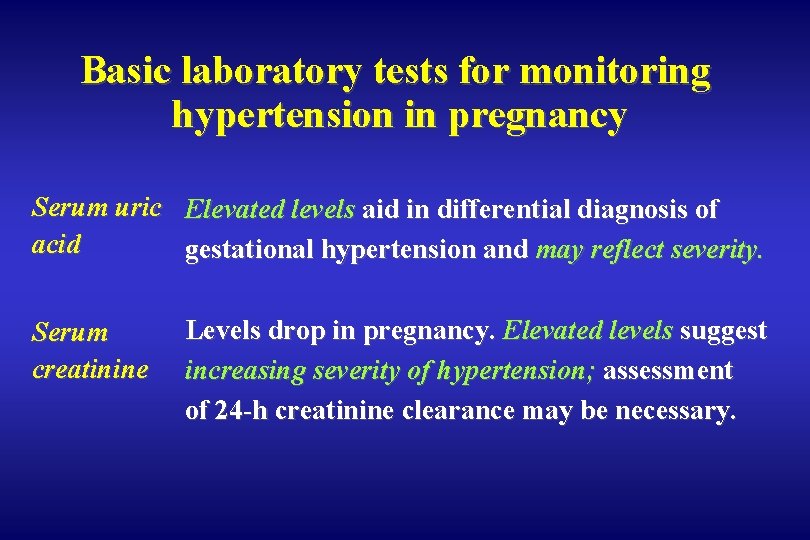
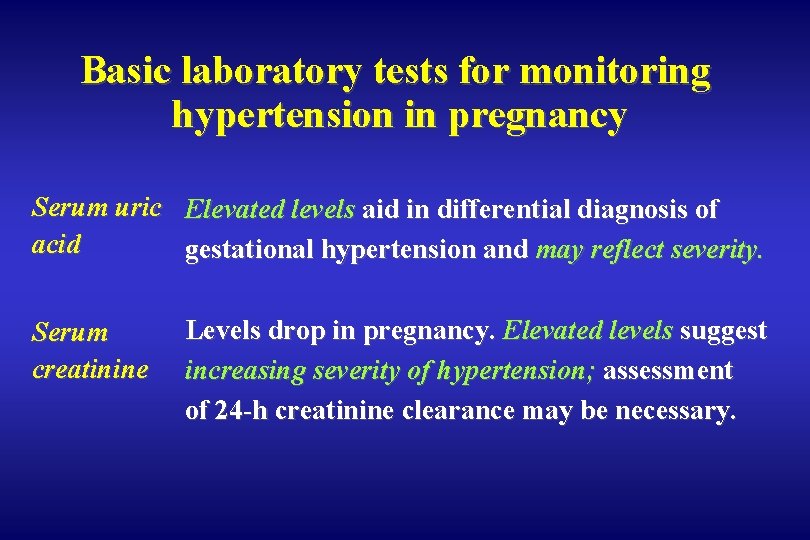
Basic laboratory tests for monitoring hypertension in pregnancy Serum uric Elevated levels aid in differential diagnosis of acid gestational hypertension and may reflect severity. Serum creatinine Levels drop in pregnancy. Elevated levels suggest increasing severity of hypertension; assessment of 24 -h creatinine clearance may be necessary.
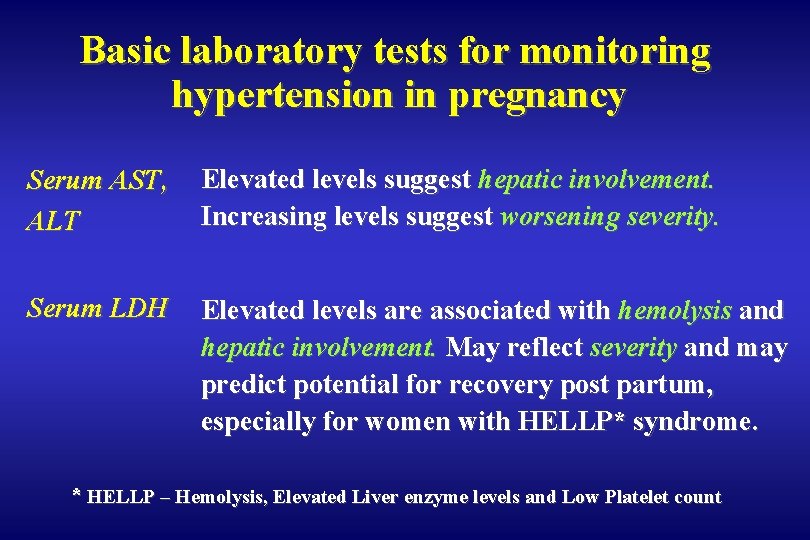
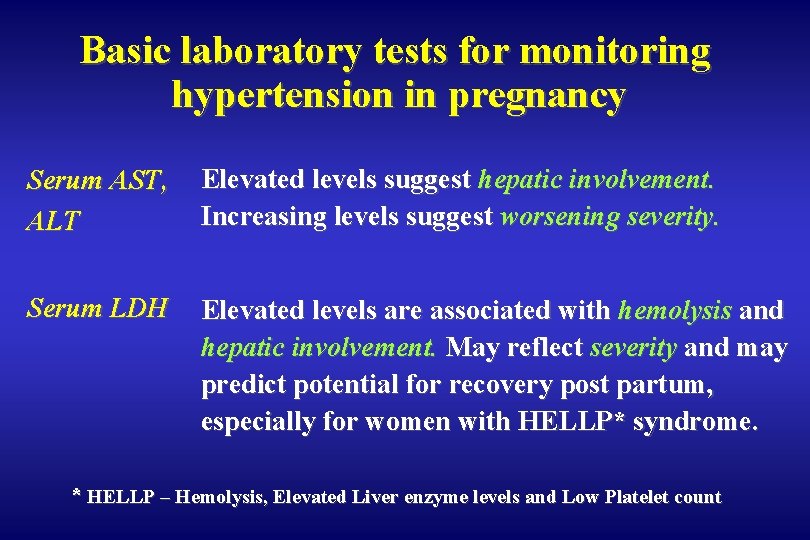
Basic laboratory tests for monitoring hypertension in pregnancy Serum AST, ALT Elevated levels suggest hepatic involvement. Increasing levels suggest worsening severity. Serum LDH Elevated levels are associated with hemolysis and hepatic involvement. May reflect severity and may predict potential for recovery post partum, especially for women with HELLP* syndrome. * HELLP – Hemolysis, Elevated Liver enzyme levels and Low Platelet count
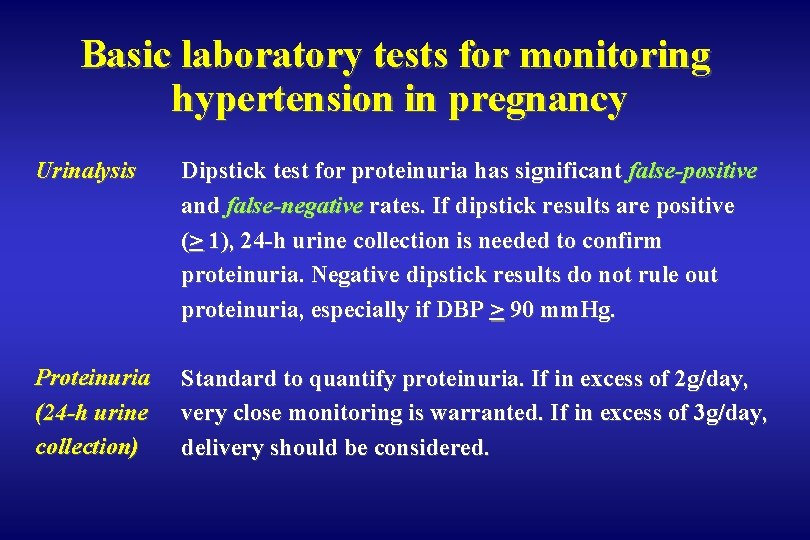
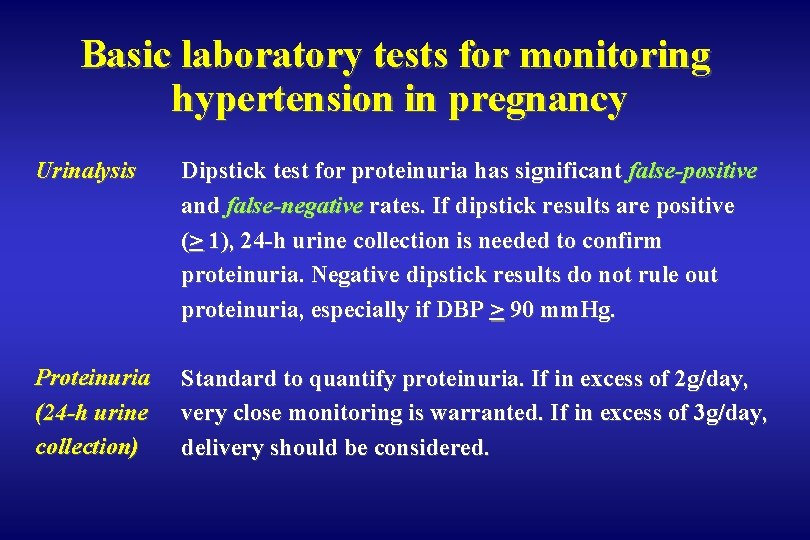
Basic laboratory tests for monitoring hypertension in pregnancy Urinalysis Dipstick test for proteinuria has significant false-positive and false-negative rates. If dipstick results are positive (> 1), 24 -h urine collection is needed to confirm proteinuria. Negative dipstick results do not rule out proteinuria, especially if DBP > 90 mm. Hg. Proteinuria (24 -h urine collection) Standard to quantify proteinuria. If in excess of 2 g/day, very close monitoring is warranted. If in excess of 3 g/day, delivery should be considered.
Management of hypertension in pregnancy depends on l BP levels l gestational age l associated maternal and fetal risk factors
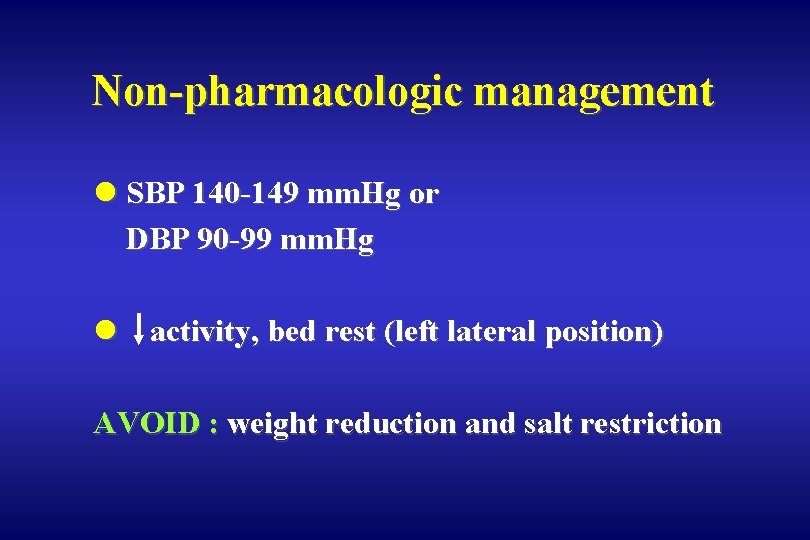
Non-pharmacologic management l SBP 140 -149 mm. Hg or DBP 90 -99 mm. Hg l activity, bed rest (left lateral position) AVOID : weight reduction and salt restriction

Emergency management of hypertension in pregnancy l SBP ≥ 170 or DBP ≥ 110 mm. Hg hydralazine, labetalol, methyldopa or nifedipine
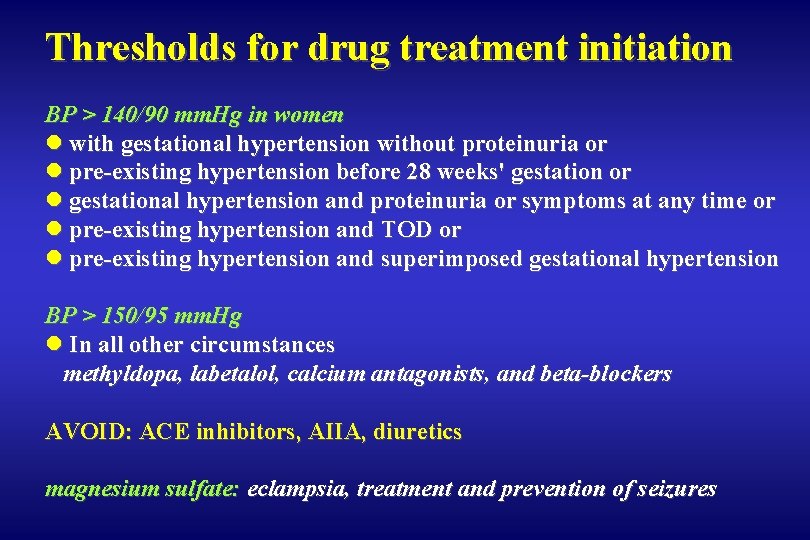
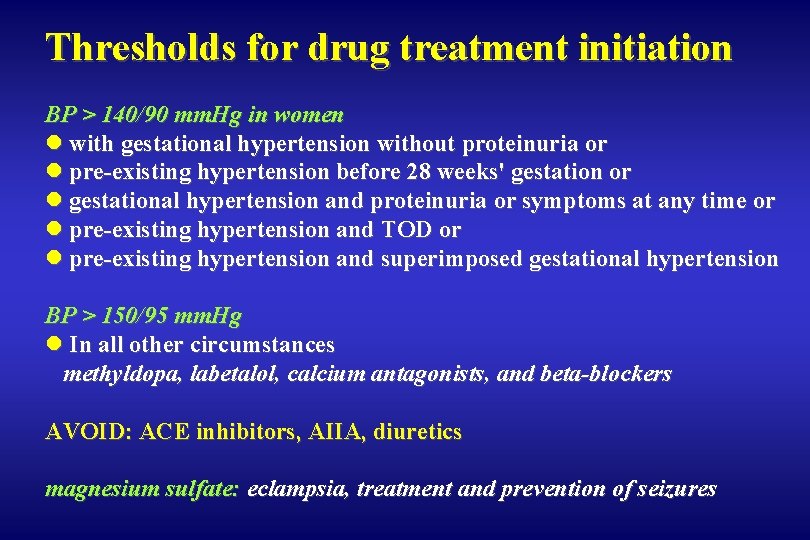
Thresholds for drug treatment initiation BP > 140/90 mm. Hg in women l with gestational hypertension without proteinuria or l pre-existing hypertension before 28 weeks' gestation or l gestational hypertension and proteinuria or symptoms at any time or l pre-existing hypertension and TOD or l pre-existing hypertension and superimposed gestational hypertension BP > 150/95 mm. Hg l In all other circumstances methyldopa, labetalol, calcium antagonists, and beta-blockers AVOID: ACE inhibitors, AIIA, diuretics magnesium sulfate: eclampsia, treatment and prevention of seizures
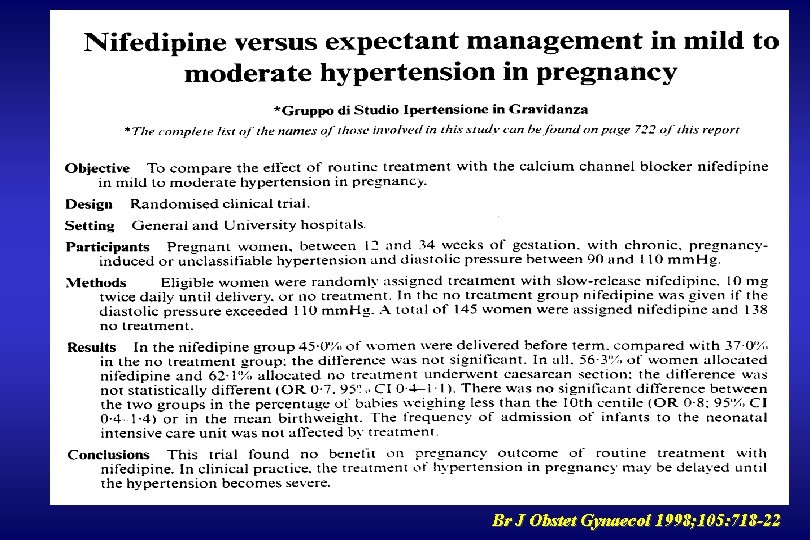
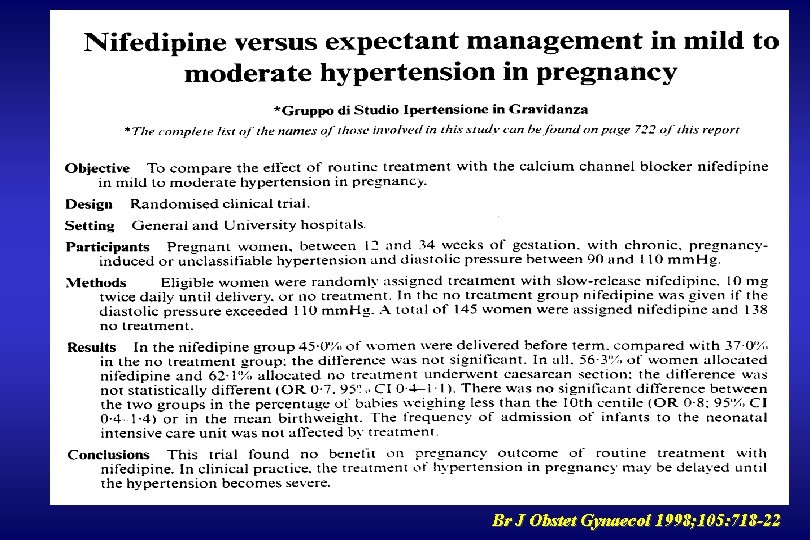
Br J Obstet Gynaecol 1998; 105: 718 -22
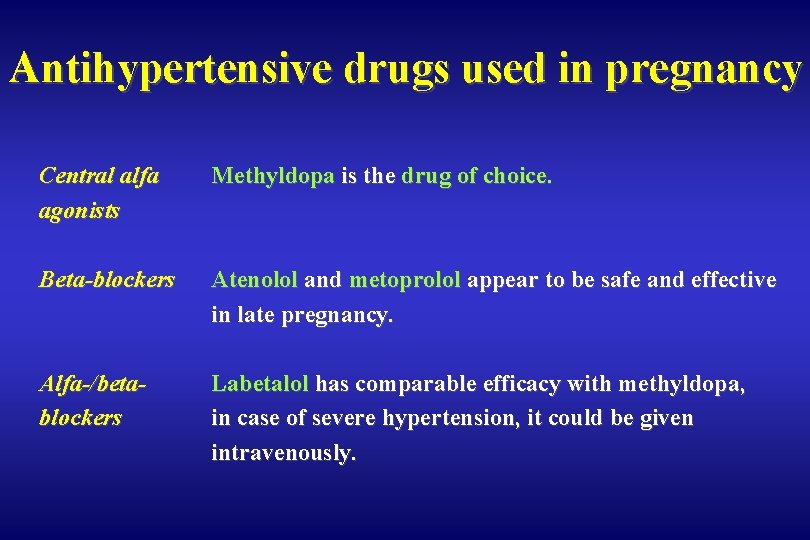
Antihypertensive drugs used in pregnancy Women with pre-existing hypertension are advised to continue their current medication except for ACE inhibitors and AIIA
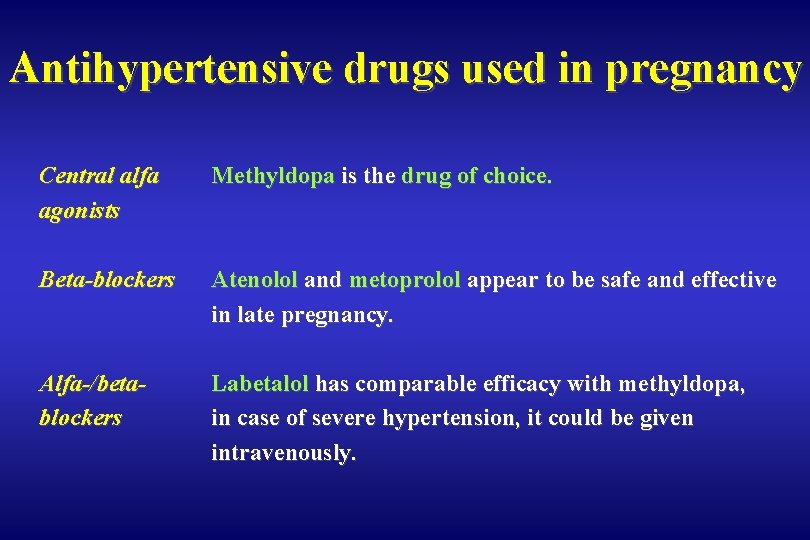
Antihypertensive drugs used in pregnancy Central alfa agonists Methyldopa is the drug of choice. Beta-blockers Atenolol and metoprolol appear to be safe and effective in late pregnancy. Alfa-/betablockers Labetalol has comparable efficacy with methyldopa, in case of severe hypertension, it could be given intravenously.
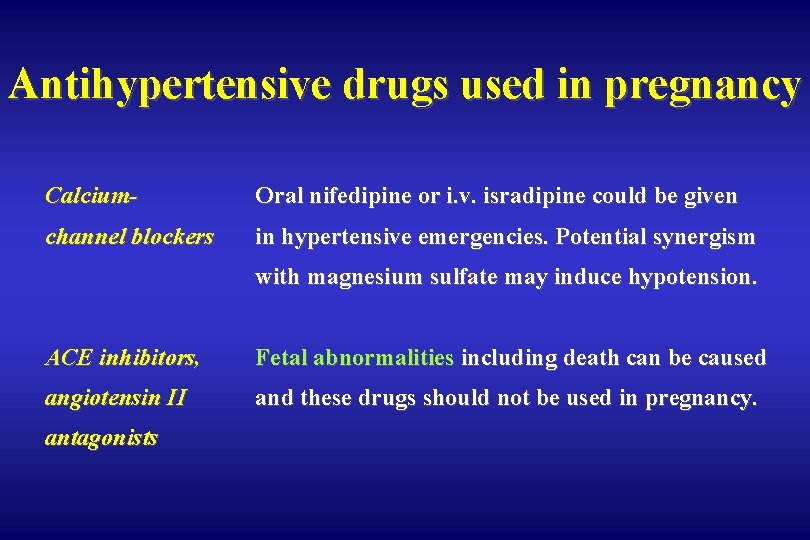
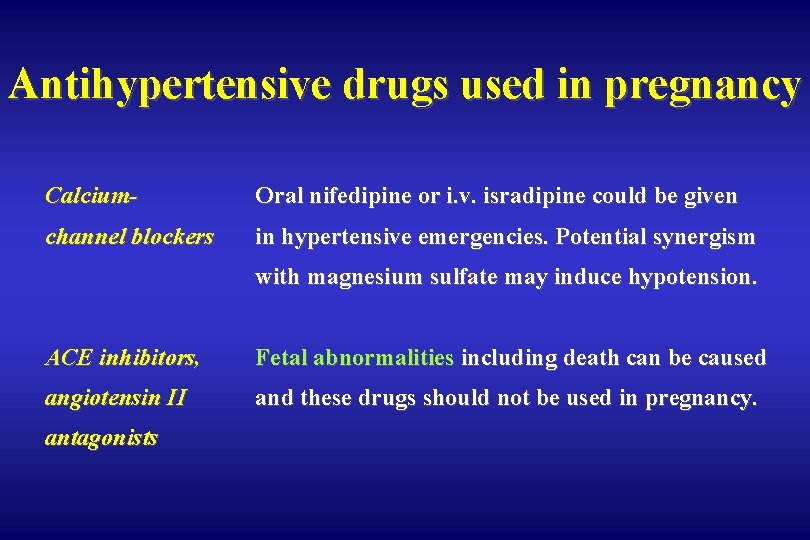
Antihypertensive drugs used in pregnancy Calcium- Oral nifedipine or i. v. isradipine could be given channel blockers in hypertensive emergencies. Potential synergism with magnesium sulfate may induce hypotension. ACE inhibitors, Fetal abnormalities including death can be caused angiotensin II and these drugs should not be used in pregnancy. antagonists
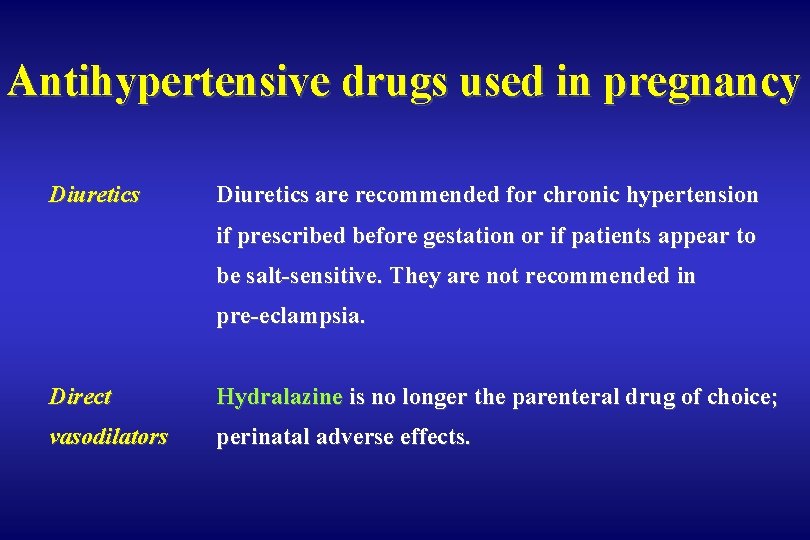
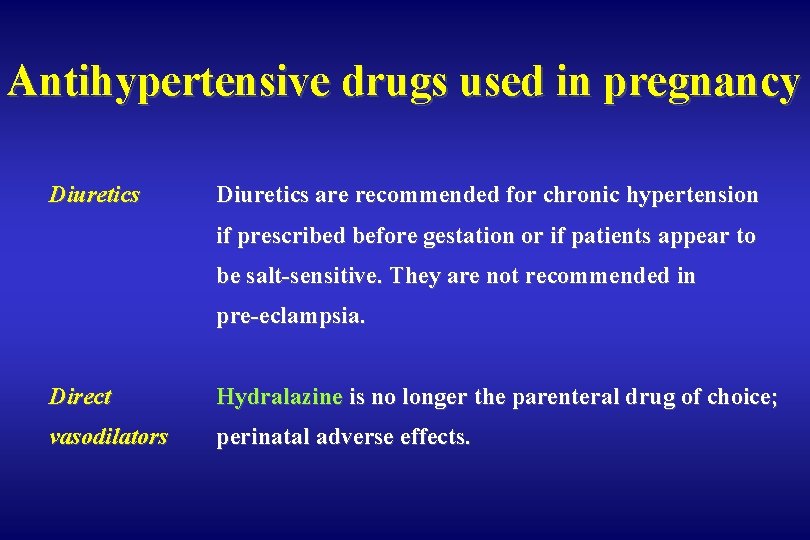
Antihypertensive drugs used in pregnancy Diuretics are recommended for chronic hypertension if prescribed before gestation or if patients appear to be salt-sensitive. They are not recommended in pre-eclampsia. Direct Hydralazine is no longer the parenteral drug of choice; vasodilators perinatal adverse effects.
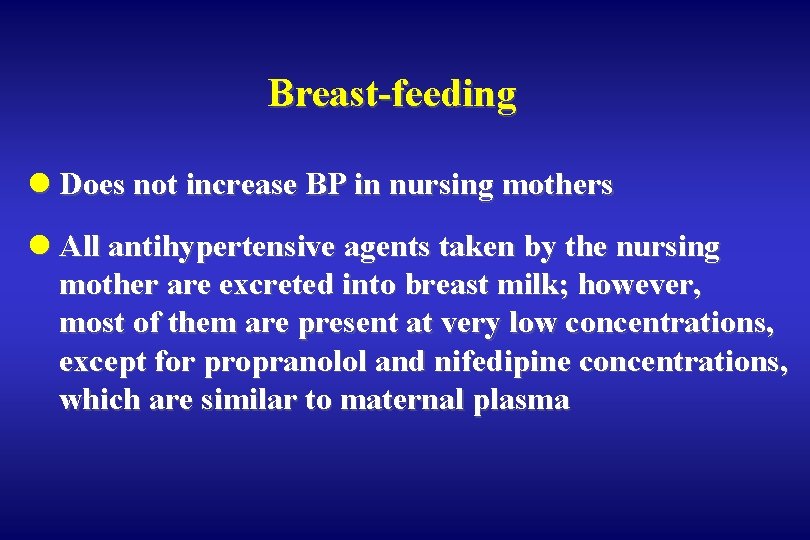
Breast-feeding l Does not increase BP in nursing mothers l All antihypertensive agents taken by the nursing mother are excreted into breast milk; however, most of them are present at very low concentrations, except for propranolol and nifedipine concentrations, which are similar to maternal plasma
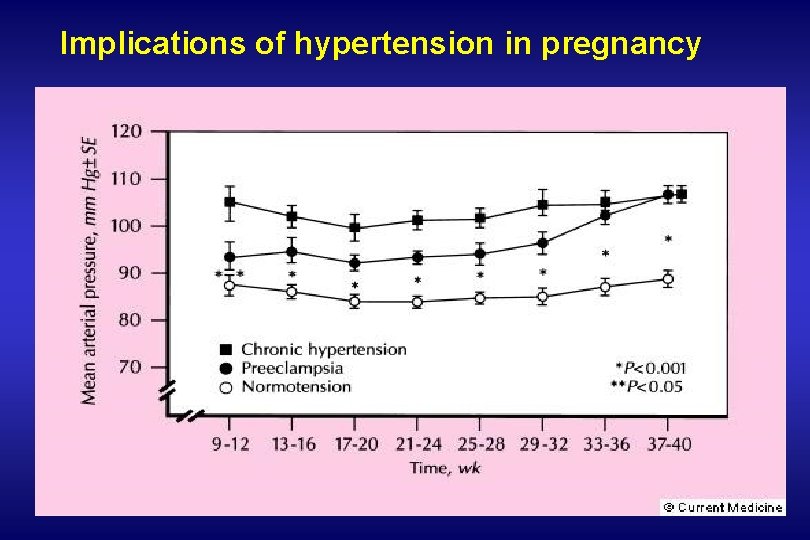
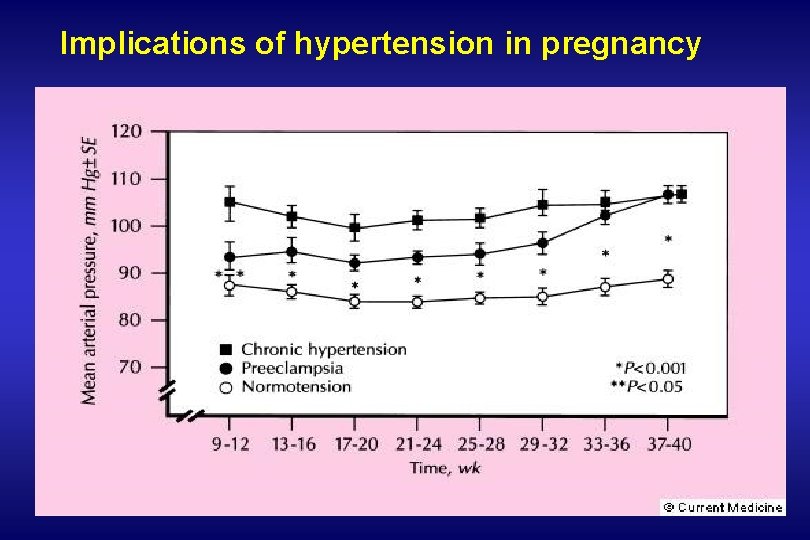
Implications of hypertension in pregnancy
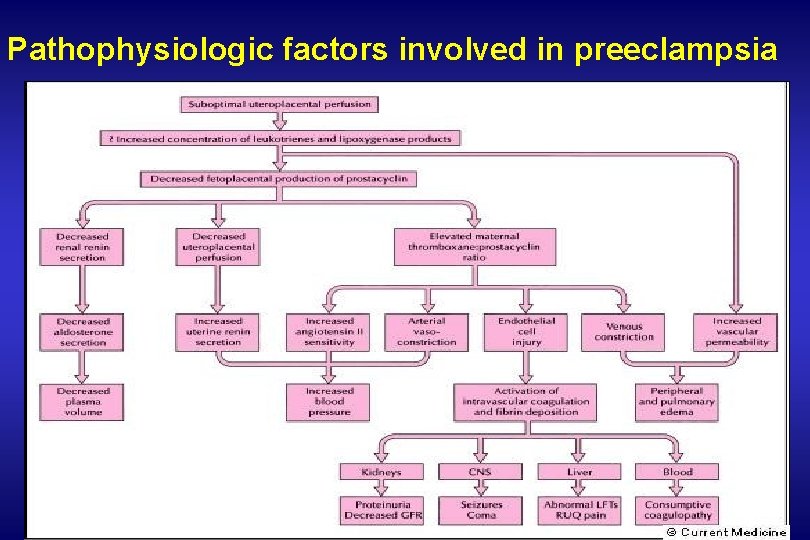
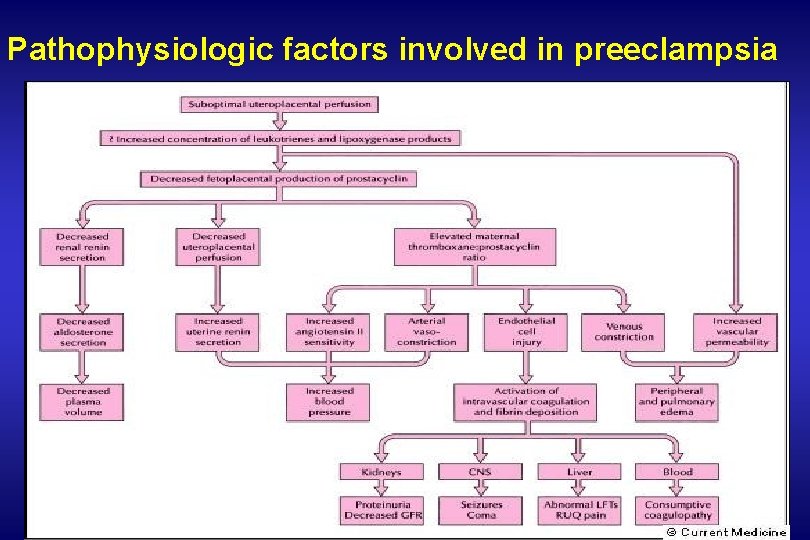
Pathophysiologic factors involved in preeclampsia
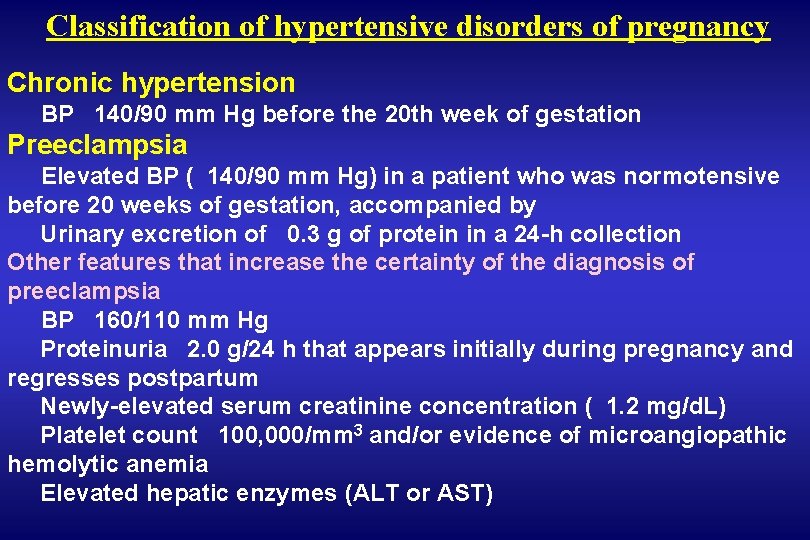
Classification of hypertensive disorders of pregnancy Chronic hypertension BP 140/90 mm Hg before the 20 th week of gestation Preeclampsia Elevated BP ( 140/90 mm Hg) in a patient who was normotensive before 20 weeks of gestation, accompanied by Urinary excretion of 0. 3 g of protein in a 24 -h collection Other features that increase the certainty of the diagnosis of preeclampsia BP 160/110 mm Hg Proteinuria 2. 0 g/24 h that appears initially during pregnancy and regresses postpartum Newly-elevated serum creatinine concentration ( 1. 2 mg/d. L) Platelet count 100, 000/mm 3 and/or evidence of microangiopathic hemolytic anemia Elevated hepatic enzymes (ALT or AST)
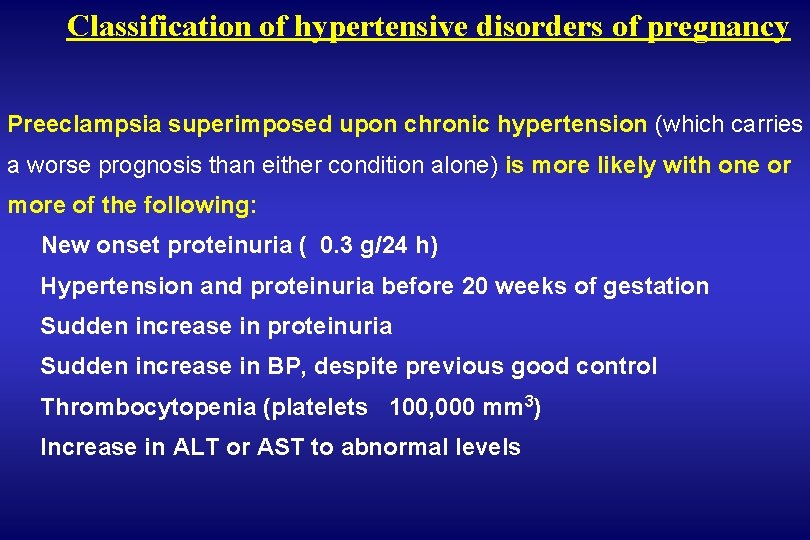
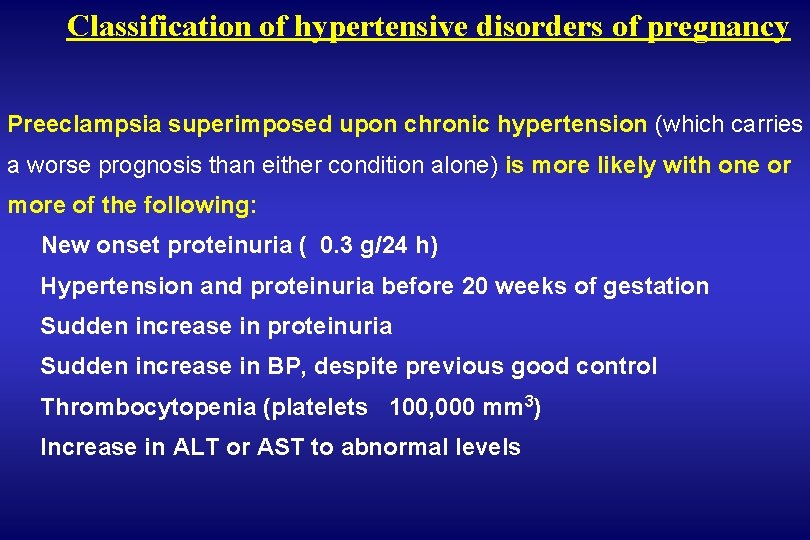
Classification of hypertensive disorders of pregnancy Preeclampsia superimposed upon chronic hypertension (which carries a worse prognosis than either condition alone) is more likely with one or more of the following: New onset proteinuria ( 0. 3 g/24 h) Hypertension and proteinuria before 20 weeks of gestation Sudden increase in proteinuria Sudden increase in BP, despite previous good control Thrombocytopenia (platelets 100, 000 mm 3) Increase in ALT or AST to abnormal levels
Classification of hypertensive disorders of pregnancy Eclampsia Occurrence of seizures that cannot be attributed to other causes in a patient with preeclampsia Gestational hypertension Transient hypertension of pregnancy (if preeclampsia is not present at time of delivery and BP returns to normal by 12 weeks postpartum) Chronic hypertension (if the elevated BP seen during pregnancy persists longer than 12 weeks postpartum)
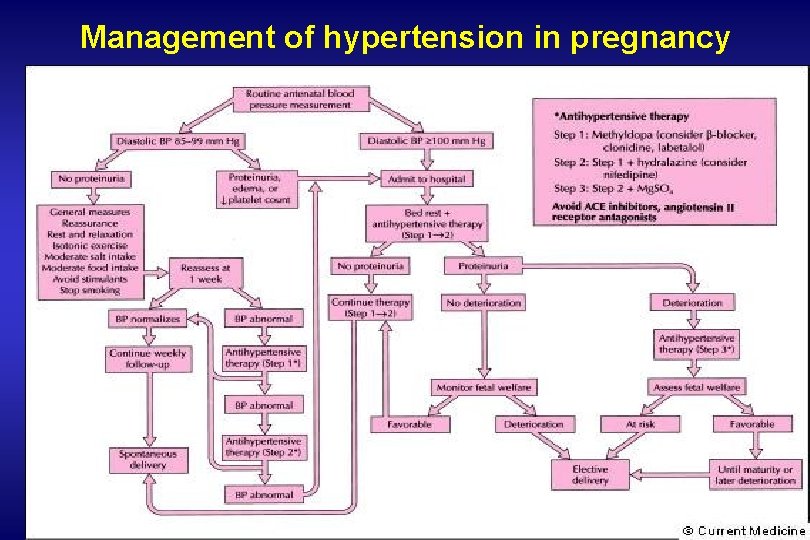
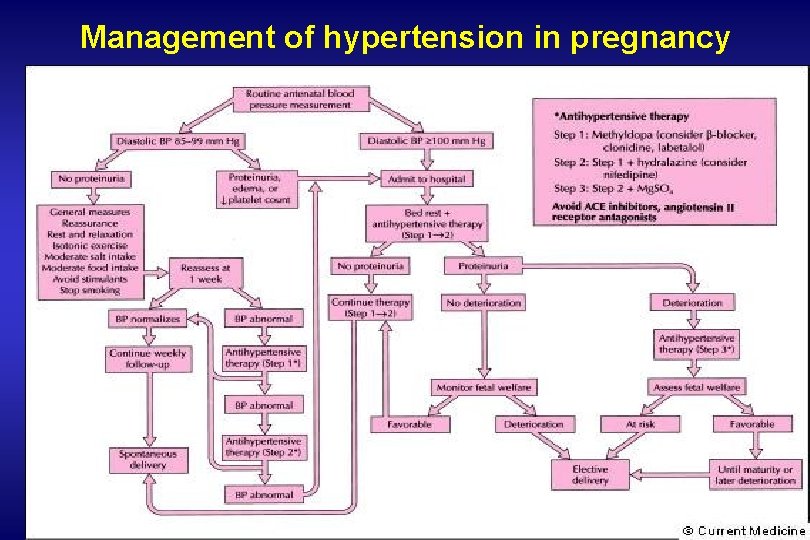
Management of hypertension in pregnancy
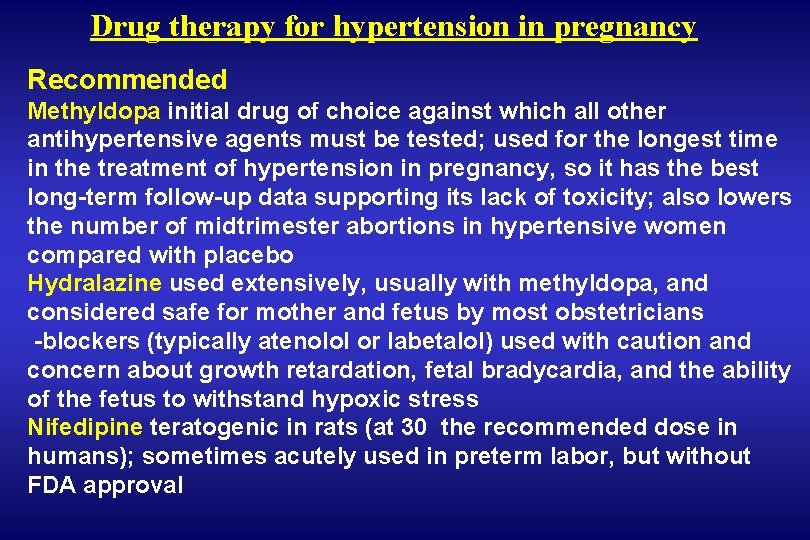
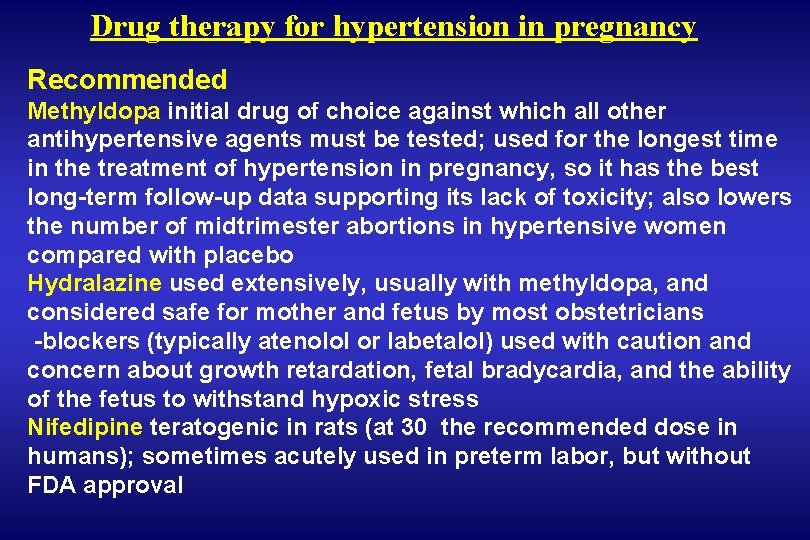
Drug therapy for hypertension in pregnancy Recommended Methyldopa initial drug of choice against which all other antihypertensive agents must be tested; used for the longest time in the treatment of hypertension in pregnancy, so it has the best long-term follow-up data supporting its lack of toxicity; also lowers the number of midtrimester abortions in hypertensive women compared with placebo Hydralazine used extensively, usually with methyldopa, and considered safe for mother and fetus by most obstetricians -blockers (typically atenolol or labetalol) used with caution and concern about growth retardation, fetal bradycardia, and the ability of the fetus to withstand hypoxic stress Nifedipine teratogenic in rats (at 30 the recommended dose in humans); sometimes acutely used in preterm labor, but without FDA approval
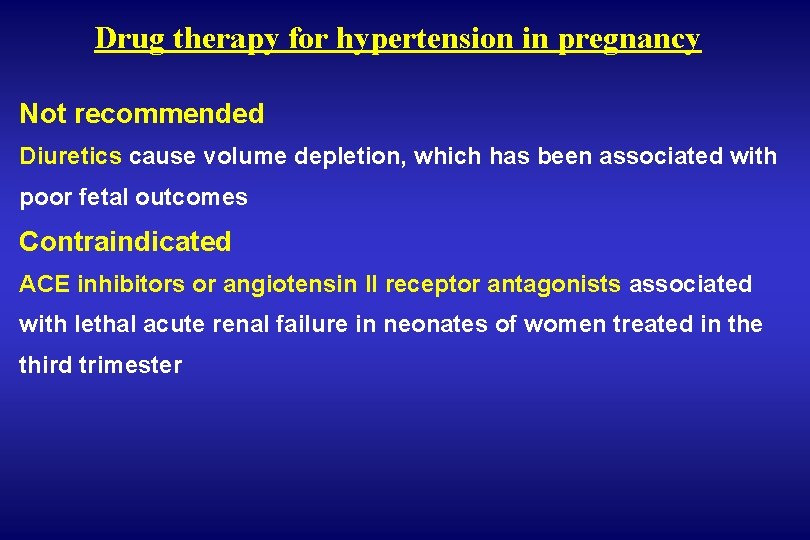
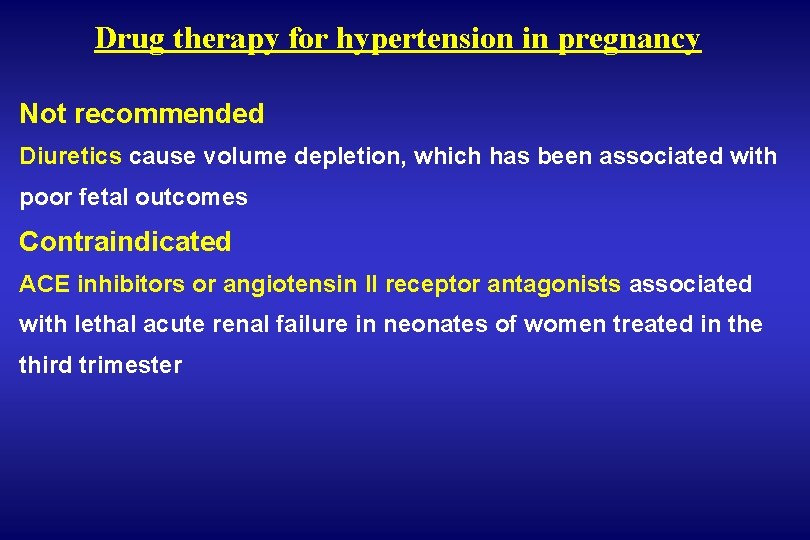
Drug therapy for hypertension in pregnancy Not recommended Diuretics cause volume depletion, which has been associated with poor fetal outcomes Contraindicated ACE inhibitors or angiotensin II receptor antagonists associated with lethal acute renal failure in neonates of women treated in the third trimester
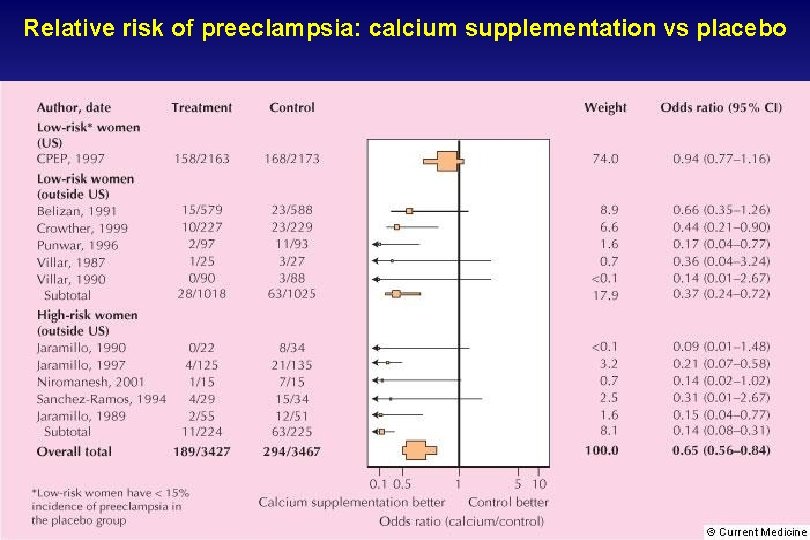
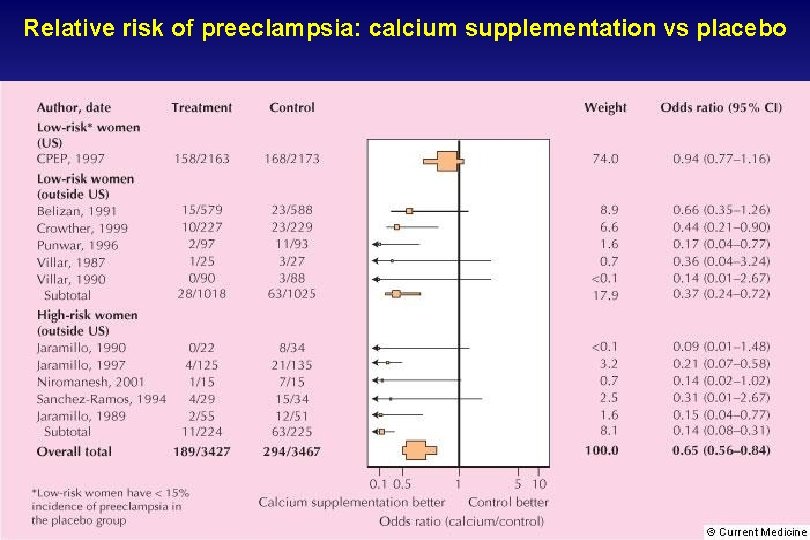
Relative risk of preeclampsia: calcium supplementation vs placebo
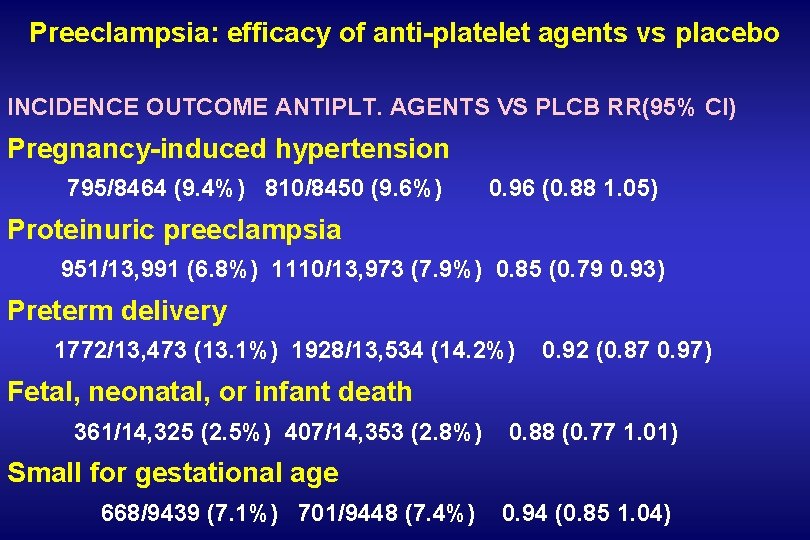
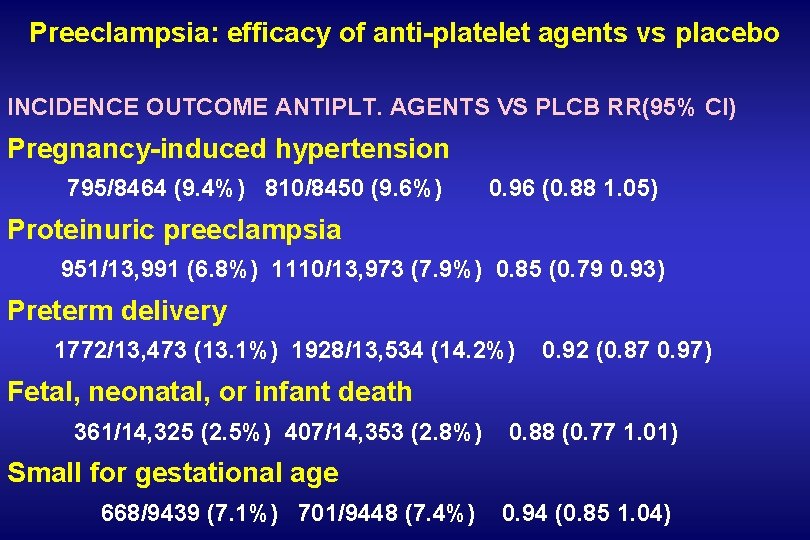
Preeclampsia: efficacy of anti-platelet agents vs placebo INCIDENCE OUTCOME ANTIPLT. AGENTS VS PLCB RR(95% CI) Pregnancy-induced hypertension 795/8464 (9. 4%) 810/8450 (9. 6%) 0. 96 (0. 88 1. 05) Proteinuric preeclampsia 951/13, 991 (6. 8%) 1110/13, 973 (7. 9%) 0. 85 (0. 79 0. 93) Preterm delivery 1772/13, 473 (13. 1%) 1928/13, 534 (14. 2%) 0. 92 (0. 87 0. 97) Fetal, neonatal, or infant death 361/14, 325 (2. 5%) 407/14, 353 (2. 8%) 0. 88 (0. 77 1. 01) Small for gestational age 668/9439 (7. 1%) 701/9448 (7. 4%) 0. 94 (0. 85 1. 04)
 Molar pregnancy symptoms
Molar pregnancy symptoms The cardiovascular system chapter 11
The cardiovascular system chapter 11 Hypertensive crisis classification
Hypertensive crisis classification Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Thyroid storm pathophysiology
Thyroid storm pathophysiology Hypokalemia
Hypokalemia Hypertensive emergency
Hypertensive emergency Site:slidetodoc.com
Site:slidetodoc.com Herzinsuffizienz endstadium symptome
Herzinsuffizienz endstadium symptome Hypertensive urgency
Hypertensive urgency Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Hypertensive encephalopathy
Hypertensive encephalopathy Keith wagner grading
Keith wagner grading Hypertensive uveitis
Hypertensive uveitis Htn emergency vs urgency
Htn emergency vs urgency Hypertensive emergency
Hypertensive emergency Bav brutale
Bav brutale Hypertensive emergency vs urgency
Hypertensive emergency vs urgency Imprinting biology example
Imprinting biology example Underlying cause and immediate cause
Underlying cause and immediate cause Proximate cause and ultimate cause
Proximate cause and ultimate cause Proximate causes of behavior
Proximate causes of behavior Punic wars summary
Punic wars summary The life today is too fast demanding
The life today is too fast demanding The 4 causes of ww1
The 4 causes of ww1 Causes of post term pregnancy
Causes of post term pregnancy Pregnancy and infant cohort monitoring and evaluation
Pregnancy and infant cohort monitoring and evaluation Extremieties
Extremieties 1 week darkening areola early pregnancy pictures
1 week darkening areola early pregnancy pictures Anemia in pregnancy
Anemia in pregnancy Causes of post term pregnancy
Causes of post term pregnancy Yolk sac ultrasound
Yolk sac ultrasound Partial molar pregnancy
Partial molar pregnancy Lightening pregnancy
Lightening pregnancy Prelying
Prelying Folic acid dose in pregnancy
Folic acid dose in pregnancy Restitution pregnancy
Restitution pregnancy Metoprolol svt
Metoprolol svt Horse placenta anatomy
Horse placenta anatomy 30 / 4
30 / 4 Bpp ultrasound score
Bpp ultrasound score Specific objectives of teenage pregnancy
Specific objectives of teenage pregnancy Lactation without pregnancy pictures
Lactation without pregnancy pictures Episiotomy types
Episiotomy types