Hypertension in pregnancy Hypertensive disorders complicate 3 7
- Slides: 13
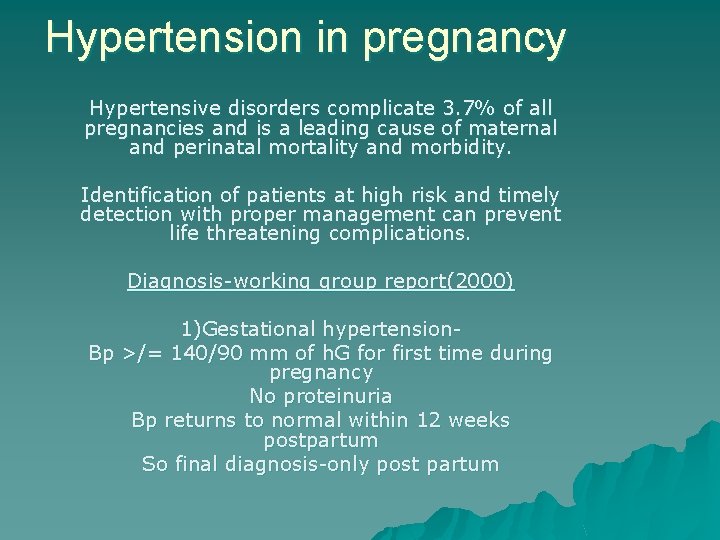
Hypertension in pregnancy Hypertensive disorders complicate 3. 7% of all pregnancies and is a leading cause of maternal and perinatal mortality and morbidity. Identification of patients at high risk and timely detection with proper management can prevent life threatening complications. Diagnosis-working group report(2000) 1)Gestational hypertension. Bp >/= 140/90 mm of h. G for first time during pregnancy No proteinuria Bp returns to normal within 12 weeks postpartum So final diagnosis-only post partum
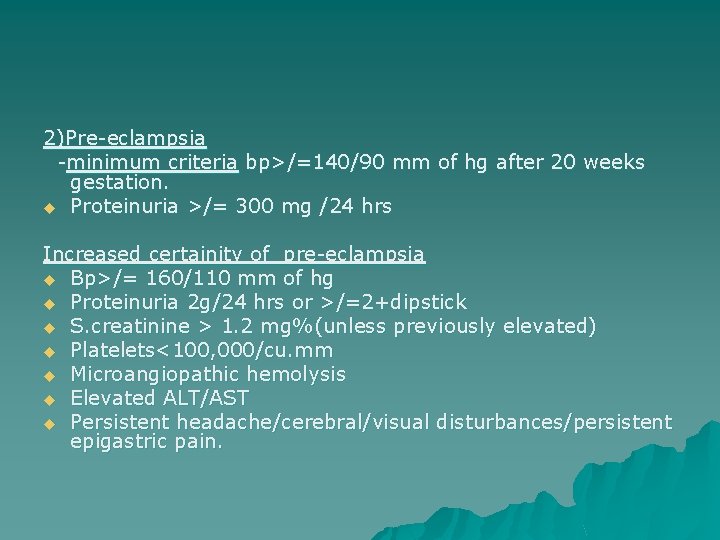
2)Pre-eclampsia -minimum criteria bp>/=140/90 mm of hg after 20 weeks gestation. u Proteinuria >/= 300 mg /24 hrs Increased certainity of pre-eclampsia u Bp>/= 160/110 mm of hg u Proteinuria 2 g/24 hrs or >/=2+dipstick u S. creatinine > 1. 2 mg%(unless previously elevated) u Platelets<100, 000/cu. mm u Microangiopathic hemolysis u Elevated ALT/AST u Persistent headache/cerebral/visual disturbances/persistent epigastric pain.
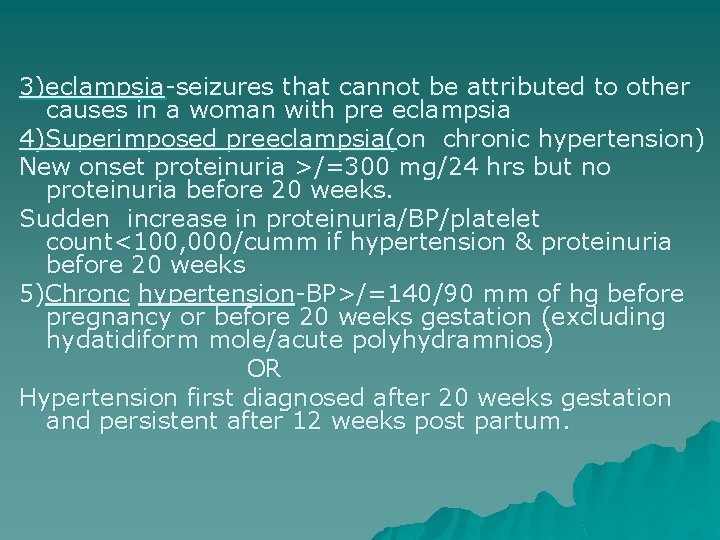
3)eclampsia-seizures that cannot be attributed to other causes in a woman with pre eclampsia 4)Superimposed preeclampsia(on chronic hypertension) New onset proteinuria >/=300 mg/24 hrs but no proteinuria before 20 weeks. Sudden increase in proteinuria/BP/platelet count<100, 000/cumm if hypertension & proteinuria before 20 weeks 5)Chronc hypertension-BP>/=140/90 mm of hg before pregnancy or before 20 weeks gestation (excluding hydatidiform mole/acute polyhydramnios) OR Hypertension first diagnosed after 20 weeks gestation and persistent after 12 weeks post partum.
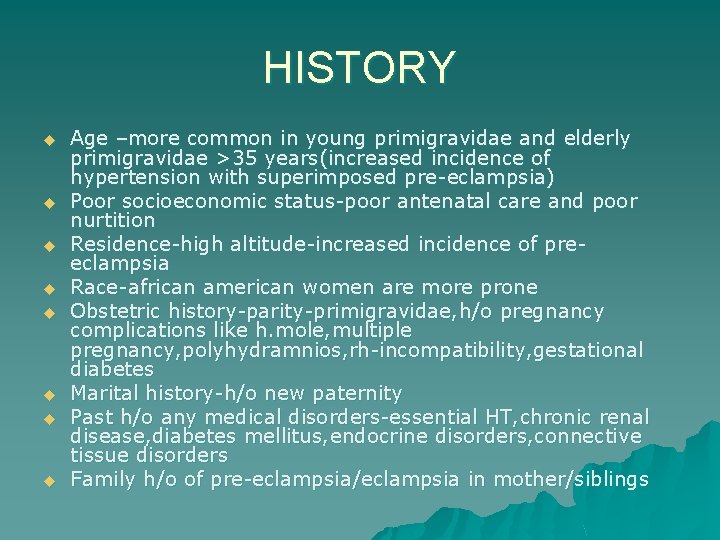
HISTORY u u u u Age –more common in young primigravidae and elderly primigravidae >35 years(increased incidence of hypertension with superimposed pre-eclampsia) Poor socioeconomic status-poor antenatal care and poor nurtition Residence-high altitude-increased incidence of preeclampsia Race-african american women are more prone Obstetric history-parity-primigravidae, h/o pregnancy complications like h. mole, multiple pregnancy, polyhydramnios, rh-incompatibility, gestational diabetes Marital history-h/o new paternity Past h/o any medical disorders-essential HT, chronic renal disease, diabetes mellitus, endocrine disorders, connective tissue disorders Family h/o of pre-eclampsia/eclampsia in mother/siblings
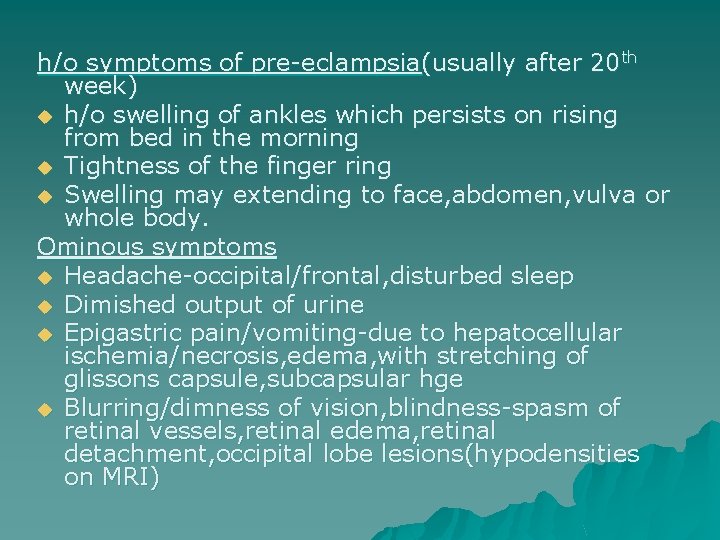
h/o symptoms of pre-eclampsia(usually after 20 th week) u h/o swelling of ankles which persists on rising from bed in the morning u Tightness of the finger ring u Swelling may extending to face, abdomen, vulva or whole body. Ominous symptoms u Headache-occipital/frontal, disturbed sleep u Dimished output of urine u Epigastric pain/vomiting-due to hepatocellular ischemia/necrosis, edema, with stretching of glissons capsule, subcapsular hge u Blurring/dimness of vision, blindness-spasm of retinal vessels, retinal edema, retinal detachment, occipital lobe lesions(hypodensities on MRI)
SIGNS Abnormal weight gain-greater than 5 pounds/month or 1 pound/week u Edema-common feature in 80% of normotensive pregnancies, so no longer incloded in the definition of pre-eclampsia u Mild edema-ignore u Sudden, severe widespread edemapathological-may indicate imminent eclampsia u
u Blood pressure measurement-ideally woman should be seated for 5 minutes before measuring BP with feet supported on the ground & arm resting on a table at the level of the heart. ( Each cm above/below-0. 8 mm hg change in bp recording) u BP recording in LLP-spuriously reduced by 10 -15 mm of hg. u The same arm should be used on each occasion u Cuff should be of appropriate size (12 cm bladder width for regular patients & 15 cm for more obese women) u Readings should be recorded to the nearest 2 mm of hg. u Use korotkoff phase 5(disappearance of sound)
To diagnose HT in pregnancy BP should be >/= 140/90 mm of hg at 2 separate readings at least 4 hrs apart. MAP=systolic BP+2* diastolic BP 3 MAP>/=105 mm of hg or ^ in MAP from previous is also diagnostic of pregnancy by 20 mmof hg HT in Diastolic BP tends to rise first followed by the systolic
P/A-the fundal height will be less than period of gestation-oligohydramnios, iugr Abdominal wall edema may be present-FHS may be difficult to localise Signs of IUD/abruption/preterm labour Fundoscopic examination-retinal edema, arteriolar constriction, alteration of normal vein to arteriole diameter from 3: 2 to 3: 1, nicking of veins by the arterioles Patient may present with eclampsia in the antenatal period(50%) Eclamptic fit-premomitory stage, tonic stage, clonic stage, stage of coma. Fits usually multiple episodes at varying intervals/status epilepticus
u Premonitory stage-unconscious, twitching of the muscles of face , tongue and limbs, rolling f eyeballs-30 sec u Tonic stage-tonic spasm of all voluntary muscles with opisthotonus, limbs flexed, hands clenched. respiration ceases, tongue protrudes. cyanosis appears , eyeballs are fixed-30 sec u Clonic stage-voluntary muscles undergo alternate contractuion/relaxationbiting of tongue , breathing sterterous, blood stained frothy secretions fill mouth, cyansis disappears gradually-1 to 4 min u Stage of coma-for brief period or lasyts till next convulsion, pt may be in confused state foll seizure, coma may occur without prior convulsion
u r/o other causes of convulsionsepilepsy/, hysteria, encephalitis, meningitis, poisoning, cerebral malaria, neurocysticercosis, intracranial tumours u o/e-temp raised, ^ pulse, resp rate, BP u Disoriention-cerebral haemorrhage u Urine output-markedly decreased, haematuria with jaundice(HELLP syndrome), anuria-b/l renal cortical necrosis u Injuries-tongue bite, due to fall u RS-basal crepitations- pulmonary edema(aspiration), signs of hypostatic/infective pneumonia, pulmonary embolism(cyanosis, resp distress) u Shock-acute LVF-due to anoxia , muscular exhaustion u Generalised bleeding tendency-DIC u Blindness
Tests of prediction u Based on the abnormal vascular responsivity/sympathetic overactivity in women destined to develop HT later in pregnancy. u ROLL OVER TEST-28 -32 weeks u Positive predictive value-33% u Positive roll over test indicates abnormal angiotensin 2 sensitivity u Angiotensin 2 infusion test
Early prenatal detection u u u u Increased prenatal visits during 3 rd trimester If overt hypertension(>140/90 mm 0 f hg)-admit the patient and evaluate the severity of pih Pts with new onset diastolic BP of 80 -90 mm of hg or wt gain>2 pounds/week should come for return visit in 3 -4 days Once admitted-daily scrutiny for symptoms/signs of imminent eclampsia Daily wt chart 4 th hrly BP chart Clinical evaluation of fetal size, amniotic fluid volume
 Spotting differential diagnosis
Spotting differential diagnosis Capital investment analysis is the process
Capital investment analysis is the process Factors that complicate capital investment analysis
Factors that complicate capital investment analysis Factors that complicate capital investment analysis
Factors that complicate capital investment analysis Factors that complicate capital investment analysis
Factors that complicate capital investment analysis Silver wiring
Silver wiring Malignant hypertension
Malignant hypertension Meto zerok 25 mg nebenwirkungen
Meto zerok 25 mg nebenwirkungen Hypertensive urgency criteria
Hypertensive urgency criteria Malignant hypertension treatment
Malignant hypertension treatment Bonnet sign
Bonnet sign Increase bp
Increase bp Hypertensive urgency vs emergency
Hypertensive urgency vs emergency Hypertensive uveitis
Hypertensive uveitis