Size and date discrepancy of pregnancy Facilitator Pawin






- Slides: 45
Size and date discrepancy of pregnancy Facilitator: Pawin Puapornpong
Size < date Inaccurate menstrual period Fetal growth restriction oligohydramnios

Size > date Elevation of the uterus by a distended bladder Multifetal pregnancy �� Inaccurate menstrual history �� Hydramnios �� Hydatidiform mole �� Uterine myomas �� A closely attached adnexal mass �� Fetal macrosomia (late in pregnancy, DM(
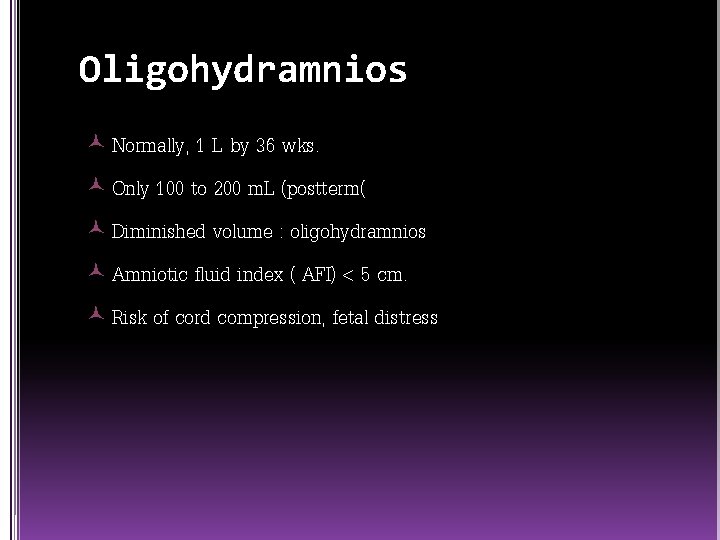
Oligohydramnios Normally, 1 L by 36 wks. Only 100 to 200 m. L (postterm( Diminished volume : oligohydramnios Amniotic fluid index ( AFI) < 5 cm. Risk of cord compression, fetal distress
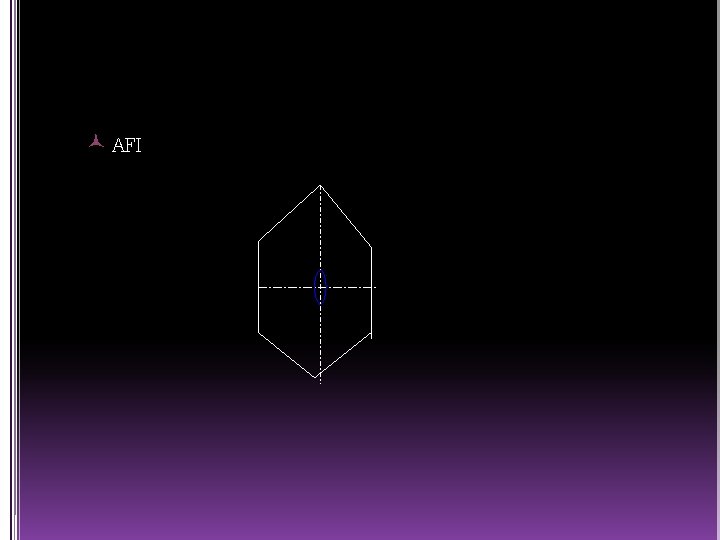
AFI
Early onset oligohydramnios Obstruction of urinary tract or renal agenesis Preterm delivery and neonatal death Adhesions between amnion and fetal parts : deformities (amputation) Pressure to fetus, muscle, skeletal deformities : clubfoot Pulmonary hypoplasia 15% Impaired lung growth and development
Oligohydramnios in late pregnancy Variable deceleration c/s for fetal distress 5 -minute apgar score < 7 Amnioinfusion during labor, prevent cord compression
Hydramnios >2 L AFI > 25 cm. CNS or GI malformation Anencephaly and esophageal atresia First half of pregnancy : transfer water and small molecules across amnion and fetal skin Second trimester : fetus urinate, swallow and inspire amnionic fluid Maternal diabetes : fetal hyperglycemia, osmotic diuresis, excess amnionic fluid
Symptoms Overdistended uterus Dyspnea Edema : compression of venous system ( lower extremieties, vulva) Diagnosis : uterine enlargement with difficulty in palpating fetal parts Differential diagnosis : ascites or a large ovarian cyst by U/S
Pregnancy outcome l Fetal malformation l Preterm delivery l Umbilical cord prolapse l Placental abruption l Uterine dysfunction l PPH l Abnormal fetal presentation
Management Minor degrees : no Px Dyspnea or abdominal pain : hospitalization Bed rest, diuretics and water-salt restriction : ineffective
l Therapeutic amniocentesis : relieve maternal distress (only transient) Membranes rupture : cord prolapse, placental abruption l Indomethacin : impair lung liquid production, enhances absorption, fetal urine production potential for closure of fetal ductus arteriosus l

Fetal growth restriction 3 to 10 % of infants Small-for-gestational age (SGA) : intrauterine growth retardation Avoid “retardation” : fetal growth restriction now preferred
definition SGA : below 10 th percentile for their GA Some are small because of constitutional factors, not pathologically growth restricted. Others define by + 2 SD with normal limits SGA < 3 rd percentile , most of them are poor outcomes.
Mortality and morbidity Fetal demise, birth asphyxia, meconium aspiration, neonatal hypoglycemia and hypothermia Growth restriction due to congenital, viral, chromosomal or maternal constitutional factors remains small throughout life. but due to placental insufficiency will often catch-up growth after birth.
Symmetrical VS asymmetrical fetal growth restriction
symmetrical Early insult : chemical exposure, viral infection, aneuploidy : proportionate reduction in both head and body.
asymmetrical Late insult : placental insufficiency from hypertension, diminished glucose transfer and hepatic storage Fetal abdominal circumference (liver size) is reduced. Shunting of oxygen and nutrients to the brain : normal brain and head growth. Increase relative brain size compared with small liver.
Risk factors Constitutional small mothers Fetal infections l Rubella and CMV l Hepatitis A and B l Listeriosis, TB, syphilis Congenital malformations l karyotype abnormalities : trisomy 18, 13 l Not in trisomy 21, Turner and Klinefelter
Chemical teratogens l Cigarette, alcohol, cocaine Maternal medical complications l Chronic vascular disease l Preeclampsia l Renal disease l High altitude residence Placental and cord abnormalities Multiple fetuses
diagnosis Early confirmation of GA Maternal weight gain Uterine fundal growth Identification of risk factors Serial sonography Doppler velocimetry NST Biophysical profile
management Near term : prompt delivery Remote from term : growth remains normal, expectant until maturity, interval U/S of 2 to 3 wks. Labor : monitor for evidence of compromise, insufficient placental function aggravated by labor. Newborn : meconium aspiration, hypothermia, hypoglycemia and polycythemia

Twin pregnancy

Definition (Multi-fetal Gestation) -Twins (two babies) -Monozygotic(Division of 1 ova fertilized by the same sperm) -Dizygotic(Fertilization of 2 ova by 2 sperm) -Triplets (three babies) -Quadruplets (four babies)
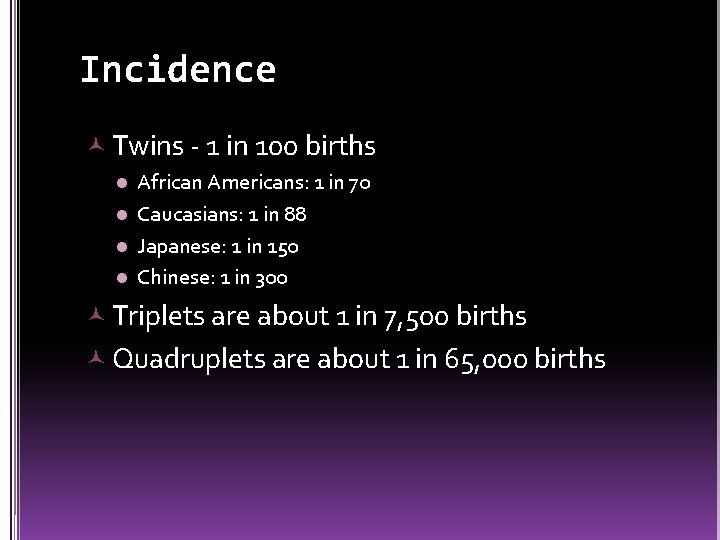
Incidence Twins - 1 in 100 births African Americans: 1 in 70 l Caucasians: 1 in 88 l Japanese: 1 in 150 l Chinese: 1 in 300 l Triplets are about 1 in 7, 500 births Quadruplets are about 1 in 65, 000 births
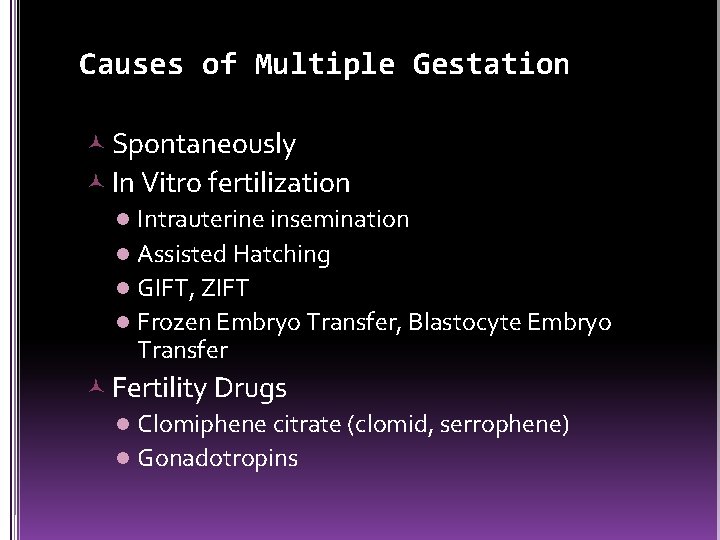
Causes of Multiple Gestation Spontaneously In Vitro fertilization l Intrauterine insemination l Assisted Hatching l GIFT, ZIFT l Frozen Embryo Transfer, Blastocyte Embryo Transfer Fertility Drugs l Clomiphene citrate (clomid, serrophene) l Gonadotropins
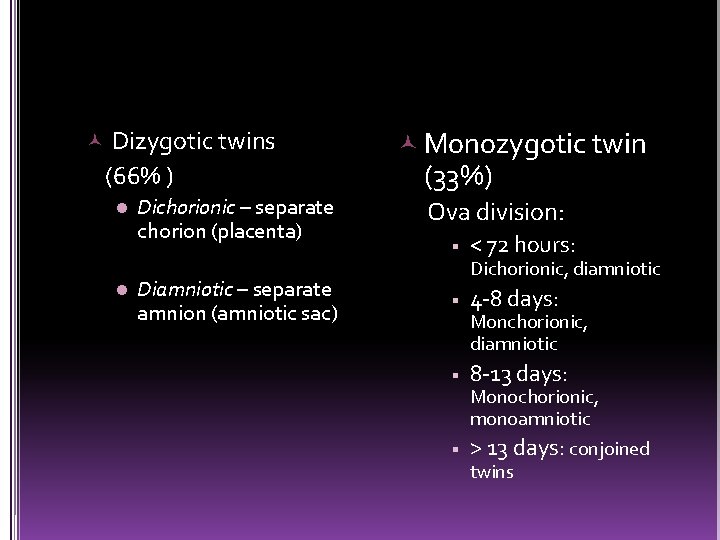
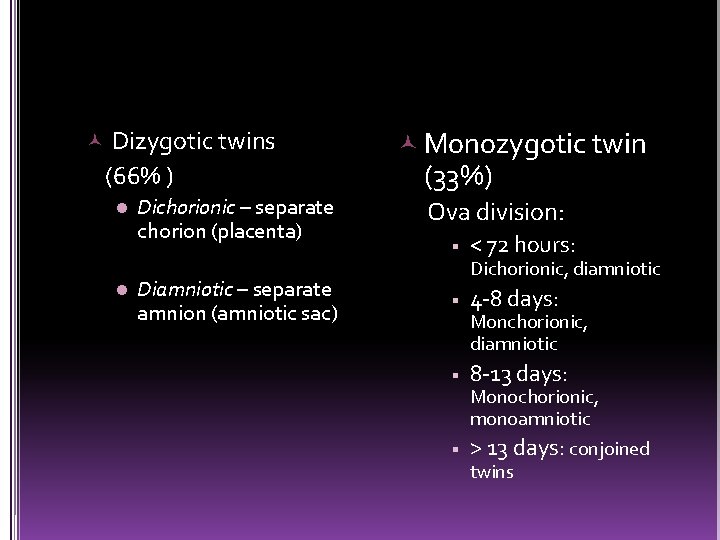
Dizygotic twins (66% ) l l Dichorionic – separate chorion (placenta) Diamniotic – separate amnion (amniotic sac) Monozygotic twin (33%) Ova division: < 72 hours: Dichorionic, diamniotic 4 -8 days: Monchorionic, diamniotic 8 -13 days: Monochorionic, monoamniotic > 13 days: conjoined twins

Average of gestation Number of babies Gestation 1 Weeks of 40 weeks 2 35 1/2 weeks 3 33 weeks 4 29 ½ weeks
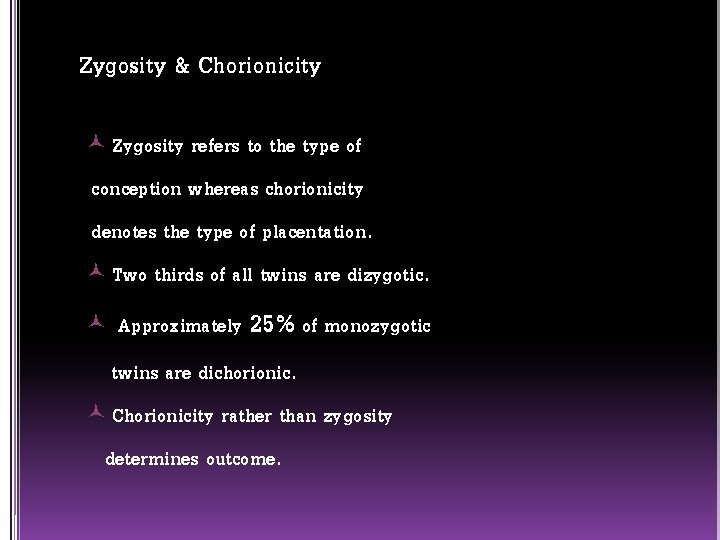
Zygosity & Chorionicity Zygosity refers to the type of conception whereas chorionicity denotes the type of placentation. Two thirds of all twins are dizygotic. Approximately 25% of monozygotic twins are dichorionic. Chorionicity rather than zygosity determines outcome.
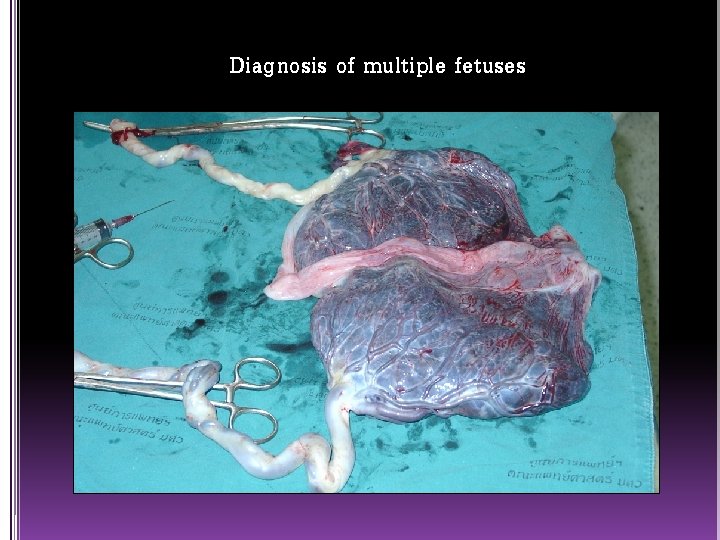
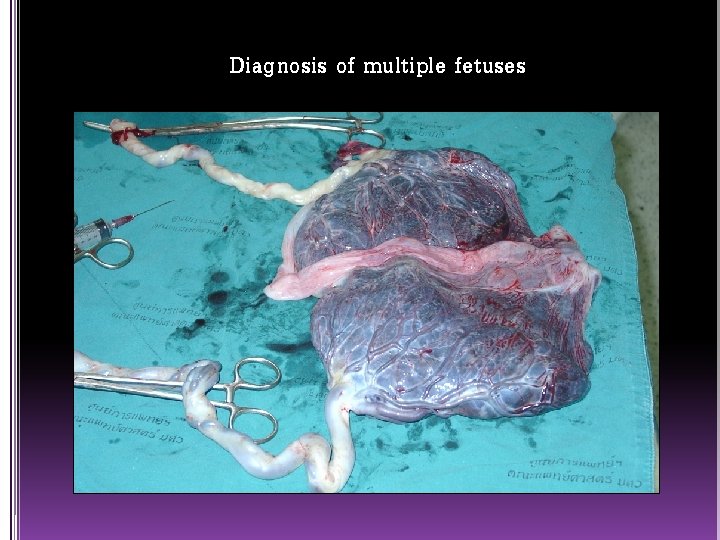
Diagnosis of multiple fetuses
History Patient profile: Etiological factors; with positive past history and family history specially maternal (advanced maternal age, high parity, large maternal size) ART Early pregnancy: Hyperemesis, abnormal bleeding
Mid-pregnancy: Greater weight gain than expected abdominal size > period of amenorrhea, early PIH symptoms. Late pregnancy: Pressure symptoms (dyspnea, dyspepsia(
Examination Abdominal: Size > Date especially in midpregnancy exclude other causes. Palpation: Multiple fetal parts Auscultation of FHS: 2 different recordings by 2 observers and a difference > 10 bpm
Ultrasonography Detect multifetal gestation 99% before 26 weeks. Confirm fetal number [ perpendicular 2 sacs or 2 fetal heads in 2 planes. [ Confirm fetal lives Diagnosis of vanishing twin syndrome. Diagnose type
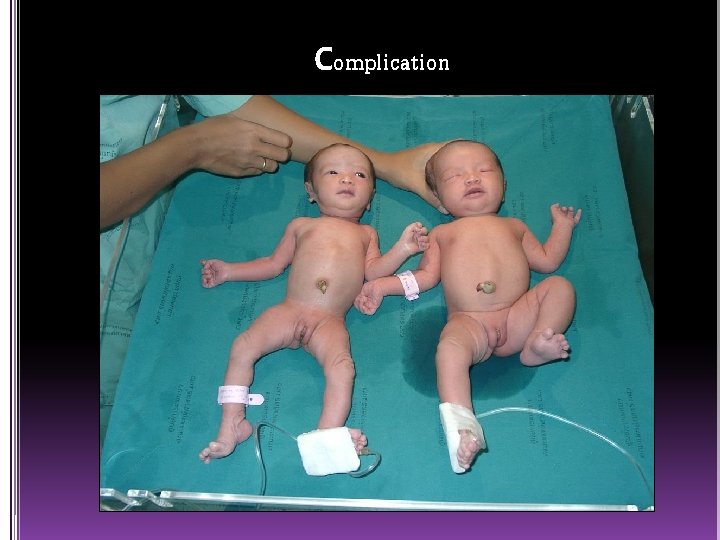
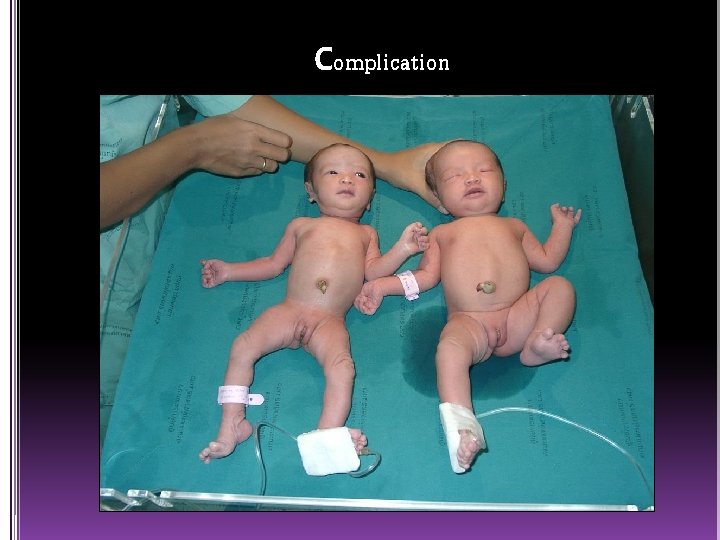
Complication
Conjoined twins or Siamese twins *Anterior (thoracopagus( *Posterior (pygopagus( *Cephalic (craniopagus( *Caudal (ischiopagus(
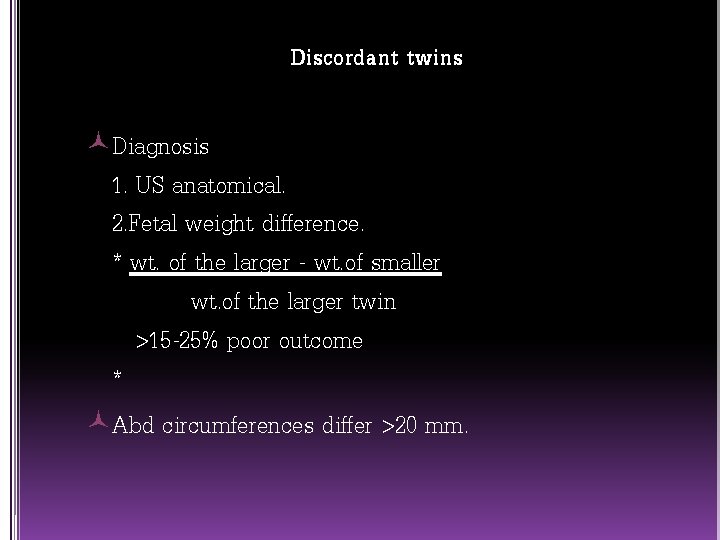
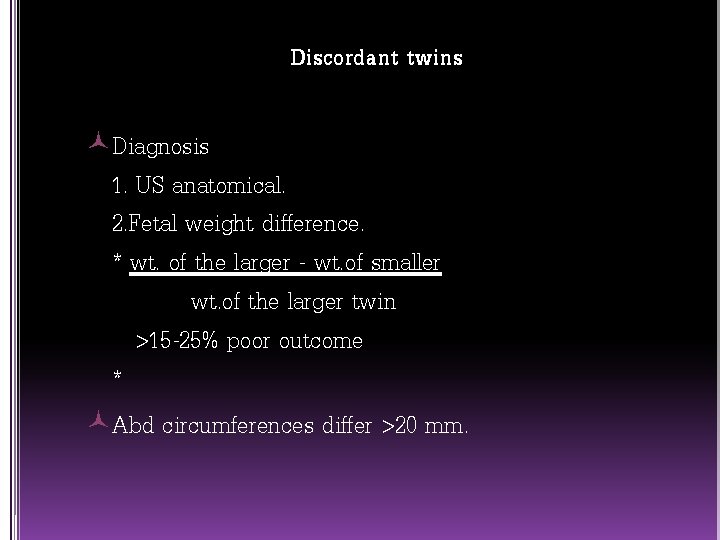
Discordant twins Diagnosis 1. US anatomical. 2. Fetal weight difference. * wt. of the larger - wt. of smaller wt. of the larger twin >15 -25% poor outcome * Abd circumferences differ >20 mm.
Twin-Twin Transfusion Syndrome Incidence : 4 - 20% of MC twins �� It is characterised by an imbalance of blood flow between the twins �� The former criterion of > 20% discordance is no longer used in the diagnosis
Twin-Twin Transfusion Syndrome Monochorionicity. Marked discordance in amniotic fluid volume between the twins. Discordance in size with the larger twin in the polyhydramniotic sac. Fetal anomalies are excluded.

Suggested treatment in TTTS Serial amnioreduction Amniotic septostomy Laser ablation Selective fetocide
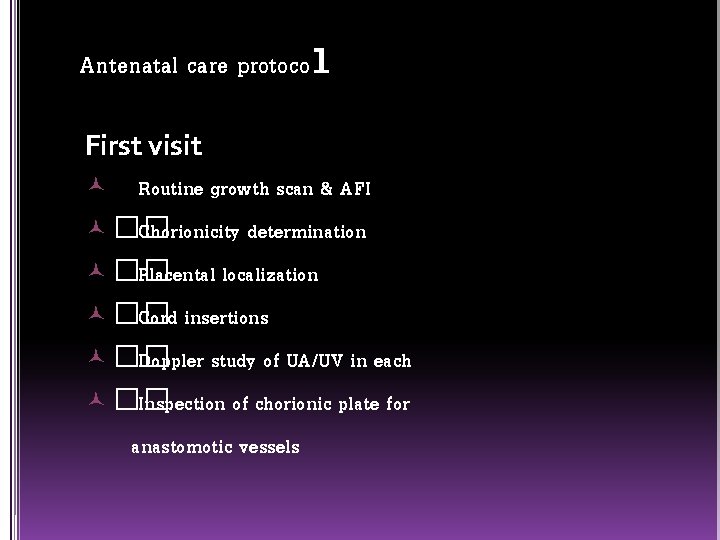
Antenatal care protocol First visit Routine growth scan & AFI �� Chorionicity determination �� Placental localization �� Cord insertions �� Doppler study of UA/UV in each �� Inspection of chorionic plate for anastomotic vessels
Subsequent visit As the first visit Prenatal diagnosis as indicated No agreement on the ideal frequency of ultrasound examinations in twins. DC : 4 weekly from 24 weeks MC : 2 weekly from 18 weeks Note any change in anastomotic flow patterns
Delivery bed with lithotomy stirrups Obstetric forceps (Piper’s forceps if breech delivery planned) or vacuum apparatus Premixed oxytocin infusion Methergine, 15 -methyl PGF 2 , or both Immediate availability of blood Capabilities and staff for emergency cesarean section
Uterine overdistension causes hypotonic uterine dysfunction. Increased risk of postpartum hemorrhage due to uterine atony. multifetal gestation is not a contraindication to labor induction, but is a condition that warrants special attention.
Thank you for your attention
 Size date discrepancy pregnancy
Size date discrepancy pregnancy Interslot
Interslot Pawin numthavaj
Pawin numthavaj Early pregnancy pictures of spotting during pregnancy
Early pregnancy pictures of spotting during pregnancy Record date ex dividend date
Record date ex dividend date Dividend ex date
Dividend ex date Wonnacott discrepancy matrix
Wonnacott discrepancy matrix Const char *s =
Const char *s = 1/18
1/18 What is visitor pre registration in picme
What is visitor pre registration in picme Wonnacott discrepancy matrix
Wonnacott discrepancy matrix Discrepancy
Discrepancy Blood bank
Blood bank Group 1 abo discrepancy
Group 1 abo discrepancy Jeanette tetrault
Jeanette tetrault Develop discrepancy example
Develop discrepancy example Discrepancy
Discrepancy Discrepancy example
Discrepancy example Abo discrepancy
Abo discrepancy Testnav mcas
Testnav mcas Cultural social
Cultural social Enterprise income verification
Enterprise income verification Abo discrepancy examples
Abo discrepancy examples Gdp deflator
Gdp deflator Discrepancy assertion
Discrepancy assertion Financial discrepancy
Financial discrepancy Unwrap core standard
Unwrap core standard Virginia equity math
Virginia equity math Family facilitator guide utah
Family facilitator guide utah Facilitator style of teaching
Facilitator style of teaching Facilitator course distance learning
Facilitator course distance learning Focus group facilitator training
Focus group facilitator training Facilitátor feladatai
Facilitátor feladatai Request letter for training facilitator
Request letter for training facilitator Fldg model
Fldg model How to thank a training facilitator
How to thank a training facilitator Thank you note for facilitator
Thank you note for facilitator Entrepreneurship facilitator
Entrepreneurship facilitator Fasset ofo codes
Fasset ofo codes Family law facilitator
Family law facilitator Qualities of facilitator
Qualities of facilitator Facilitator feedback survey
Facilitator feedback survey How to thank a facilitator
How to thank a facilitator How to thank a training facilitator
How to thank a training facilitator Peer facilitator quotes
Peer facilitator quotes Stemmehører facilitator
Stemmehører facilitator