CASE STUDY 44 Facilitator Pawin Puapornpong Past History










- Slides: 26
CASE STUDY 44 Facilitator: Pawin Puapornpong



Past History • No underlying disease • No history of drug, food allergy • No history of smoking, alcoholism • Current medication : none
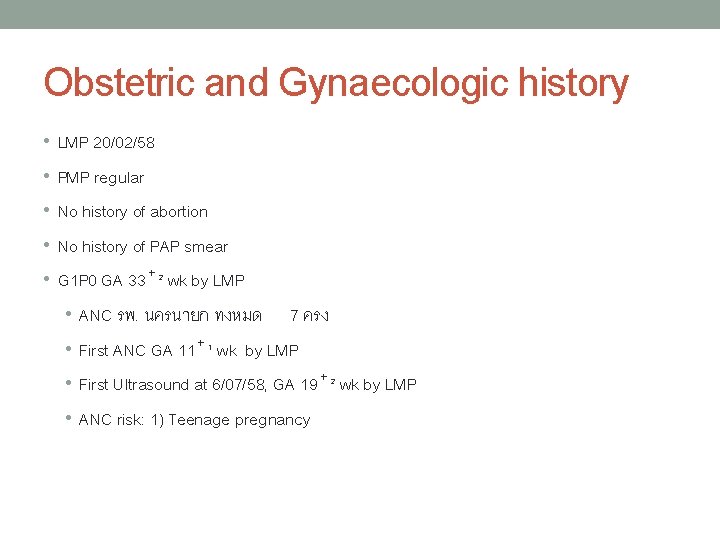
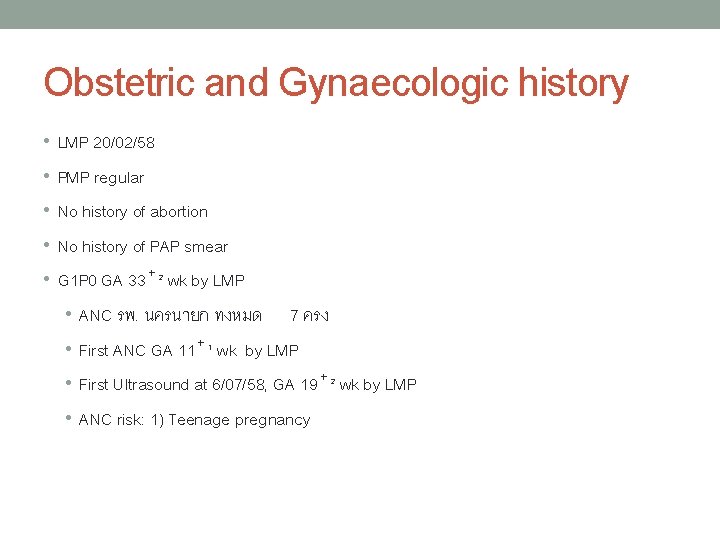
Obstetric and Gynaecologic history • LMP 20/02/58 • PMP regular • No history of abortion • No history of PAP smear • G 1 P 0 GA 33⁺² wk by LMP • ANC รพ. นครนายก ทงหมด 7 ครง • First ANC GA 11⁺¹ wk by LMP • First Ultrasound at 6/07/58, GA 19⁺² wk by LMP • ANC risk: 1) Teenage pregnancy

Obstetric and Gynaecologic history • ANC Laboratory • Female • Male Hematocrit 34% DCIP negative OF negative Blood group A, Rh+ Anti HIV negative VDRL nonreactive HBs. Ag negative DCIP negative Anti HIV negative OF negative Blood group B, Rh+ • None couple at risk for severe thalassemia*
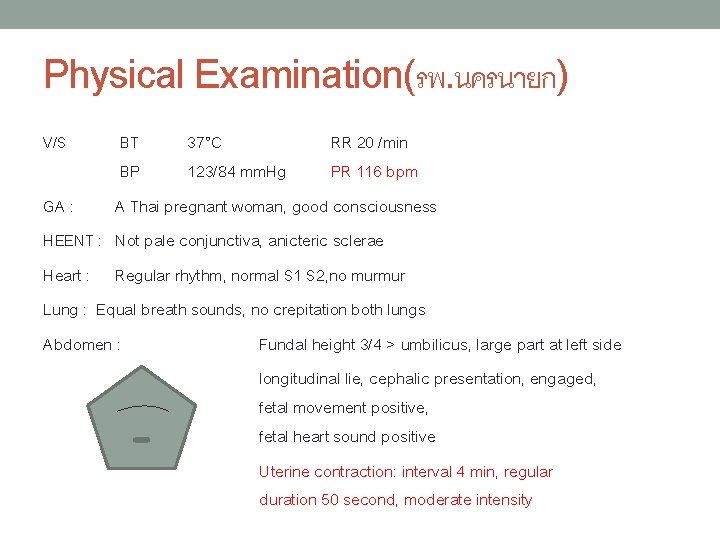
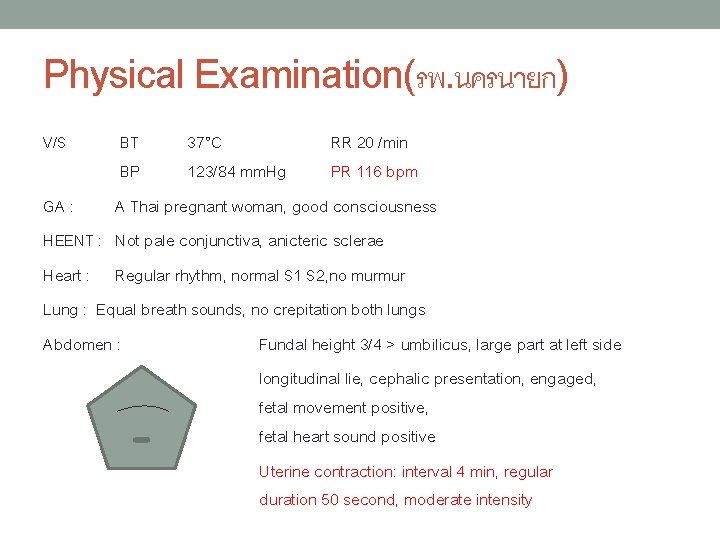
Physical Examination(รพ. นครนายก) V/S BT 37°C RR 20 /min BP 123/84 mm. Hg PR 116 bpm GA : A Thai pregnant woman, good consciousness HEENT : Not pale conjunctiva, anicteric sclerae Heart : Regular rhythm, normal S 1 S 2, no murmur Lung : Equal breath sounds, no crepitation both lungs Abdomen : Fundal height 3/4 > umbilicus, large part at left side longitudinal lie, cephalic presentation, engaged, fetal movement positive, fetal heart sound positive Uterine contraction: interval 4 min, regular duration 50 second, moderate intensity
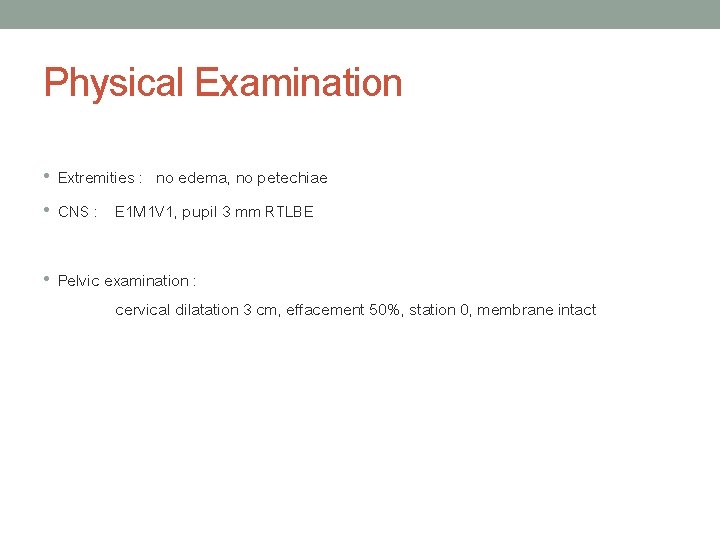
Physical Examination • Extremities : no edema, no petechiae • CNS : E 1 M 1 V 1, pupil 3 mm RTLBE • Pelvic examination : cervical dilatation 3 cm, effacement 50%, station 0, membrane intact
Diagnosis • G 1 P 0 33+1 wk by LMP with • Preterm labor pain • Fetal anomaly • Teenage pregnancy
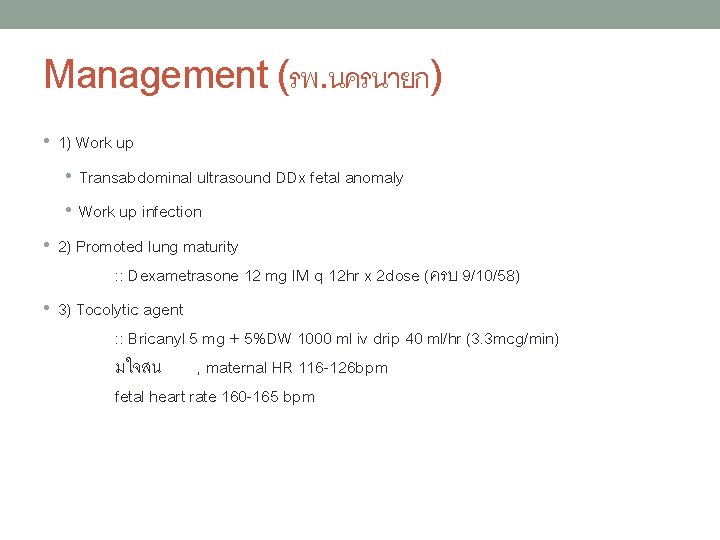
Management (รพ. นครนายก) • 1) Work up • Transabdominal ultrasound DDx fetal anomaly • Work up infection • 2) Promoted lung maturity : : Dexametrasone 12 mg IM q 12 hr x 2 dose (ครบ 9/10/58) • 3) Tocolytic agent : : Bricanyl 5 mg + 5%DW 1000 ml iv drip 40 ml/hr (3. 3 mcg/min) มใจสน , maternal HR 116 -126 bpm fetal heart rate 160 -165 bpm
Management (รพ. นครนายก) 10/10/58 ทองแขงถเทาๆเดม ลกดนด uterine contraction: 4 min, 40 second, moderate to strong intensity PV cervical os dilatation 4 cm, effacement 80%, station 0 1) พจารณาเรอง tocolytic agent เนองจากไดรบ dexamethasone ครบ 2) GBS prophylaxis : : Ampicillin 2 gm iv stat then 1 gm iv q 4 hr Refer to MSMC
REFER TO MSMC 11/10/58
Reevaluation at MSMC • 11/10/58, 12. 35 น. • ใจสน ไมมคลนไสอาเจยน ทองแขงมากขน ไมมมกเลอด ไมมนำเดน ลกดนปกตด • V/S BT 37. 2°C RR 20 /min BP 128/73 mm. Hg PR 124 bpm Abdomen : Fundal height 3/4 > umbilicus, large part at left side longitudinal lie, cephalic presentation, engaged, estimate fetal weight 1, 500 gm, fetal movement positive, fetal heart sound positive by doppler Uterine contraction: interval 4 min, duration 50 second, moderate intensity • Pelvic examination(12. 45น. ) : cervical dilatation 4 cm, effacement 50%, station 1+, soft consistency, posterior position, membrane intact
Diagnosis • G 1 P 0 33+1 wk by LMP with • Preterm labor pain • Fetal anomaly • Teenage pregnancy

Differential Diagnosis
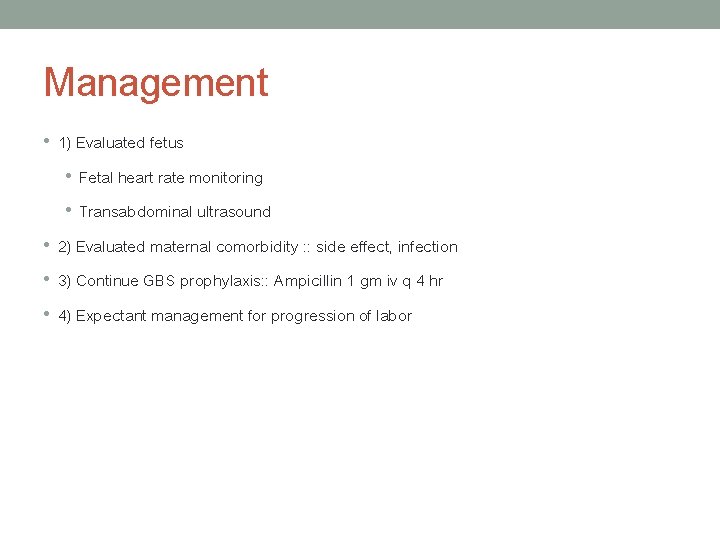
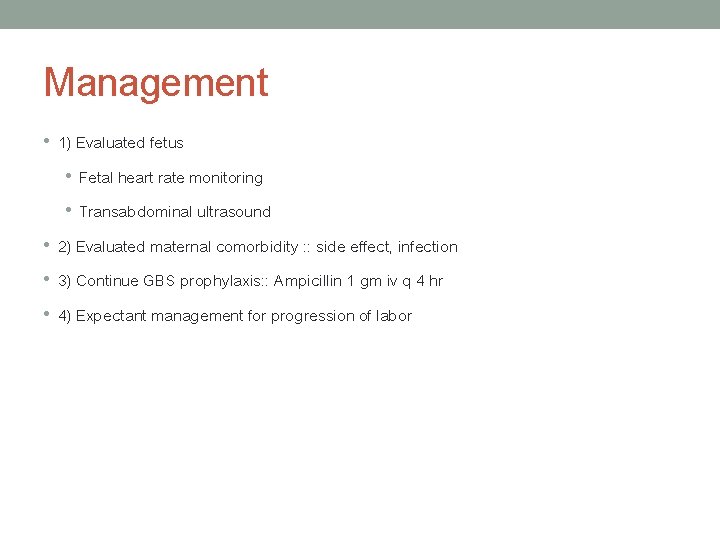
Management • 1) Evaluated fetus • Fetal heart rate monitoring • Transabdominal ultrasound • 2) Evaluated maternal comorbidity : : side effect, infection • 3) Continue GBS prophylaxis: : Ampicillin 1 gm iv q 4 hr • 4) Expectant management for progression of labor
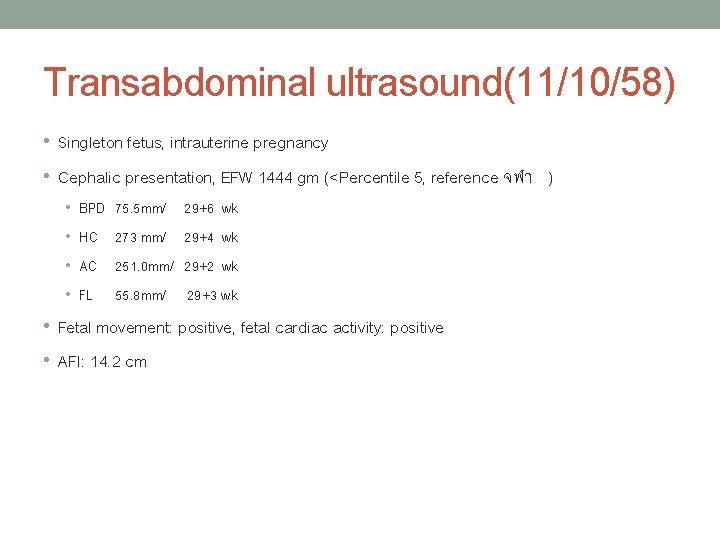
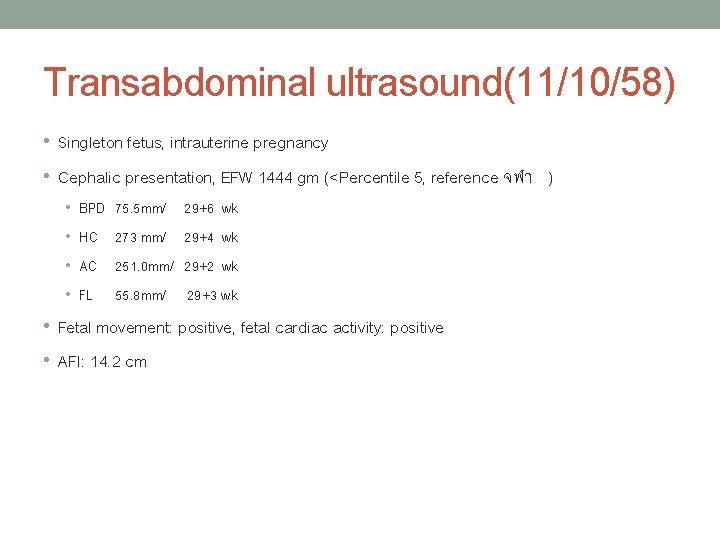
Transabdominal ultrasound(11/10/58) • Singleton fetus, intrauterine pregnancy • Cephalic presentation, EFW 1444 gm (<Percentile 5, reference จฬา ) • BPD 75. 5 mm/ 29+6 wk • HC 273 mm/ 29+4 wk • AC 251. 0 mm/ 29+2 wk • FL 55. 8 mm/ 29+3 wk • Fetal movement: positive, fetal cardiac activity: positive • AFI: 14. 2 cm


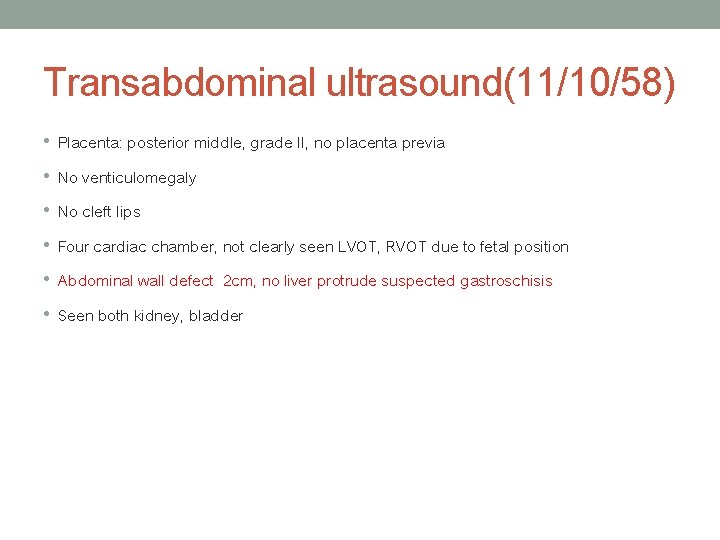
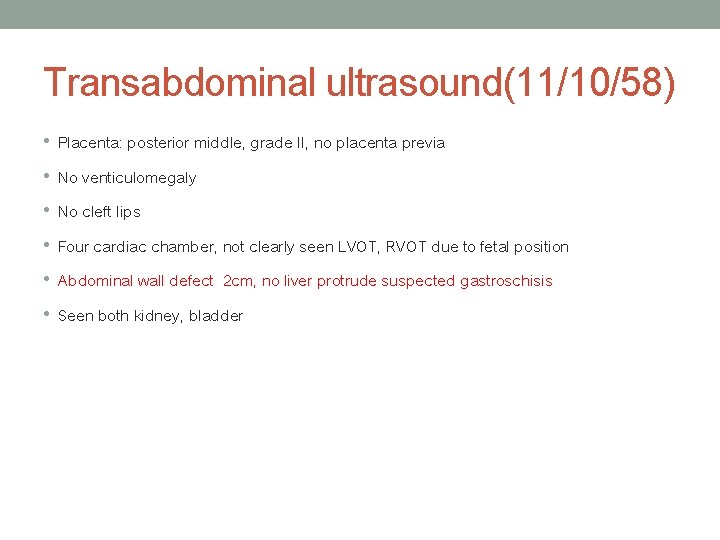
Transabdominal ultrasound(11/10/58) • Placenta: posterior middle, grade II, no placenta previa • No venticulomegaly • No cleft lips • Four cardiac chamber, not clearly seen LVOT, RVOT due to fetal position • Abdominal wall defect 2 cm, no liver protrude suspected gastroschisis • Seen both kidney, bladder
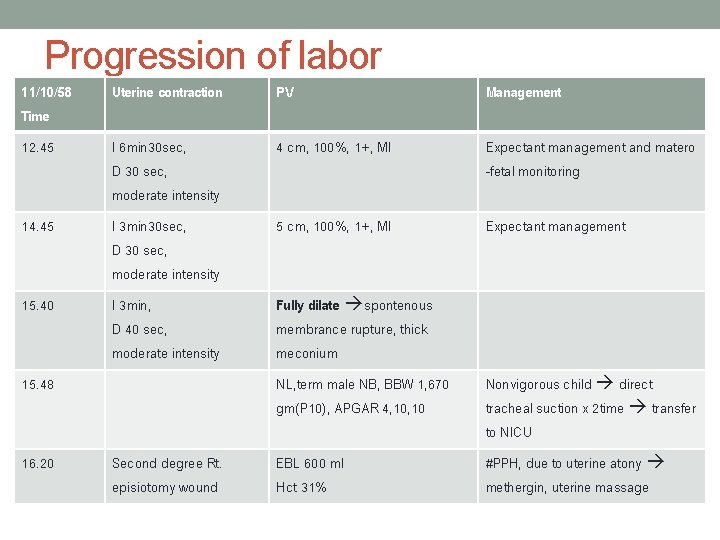
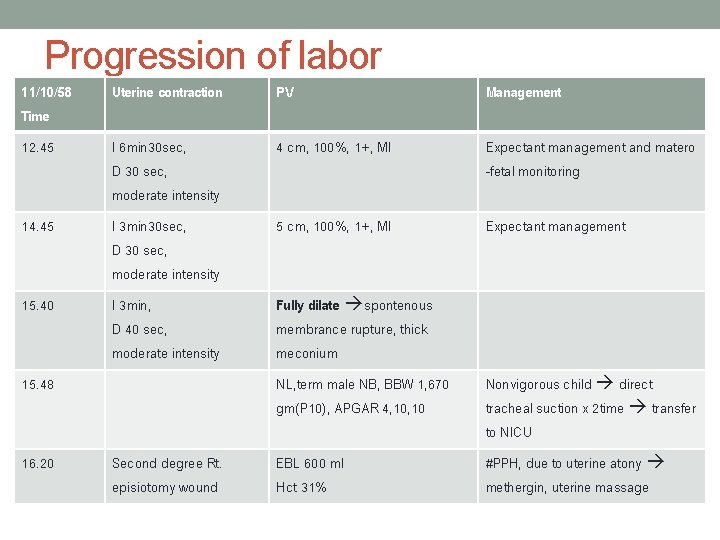
Progression of labor 11/10/58 Time Uterine contraction PV Management 12. 45 I 6 min 30 sec, D 30 sec, moderate intensity 4 cm, 100%, 1+, MI Expectant management and matero -fetal monitoring 14. 45 I 3 min 30 sec, D 30 sec, moderate intensity 5 cm, 100%, 1+, MI Expectant management 15. 40 I 3 min, D 40 sec, moderate intensity Fully dilate spontenous membrance rupture, thick meconium 15. 48 16. 20 Second degree Rt. episiotomy wound NL, term male NB, BBW 1, 670 gm(P 10), APGAR 4, 10 Nonvigorous child direct tracheal suction x 2 time transfer to NICU EBL 600 ml Hct 31% #PPH, due to uterine atony methergin, uterine massage
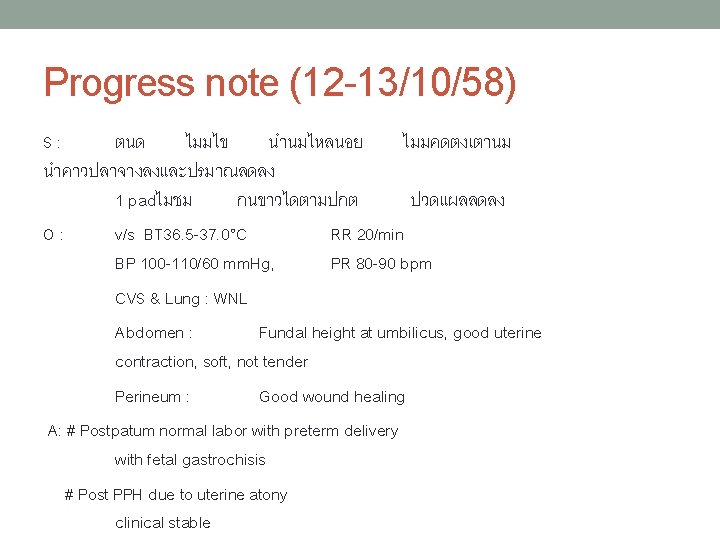
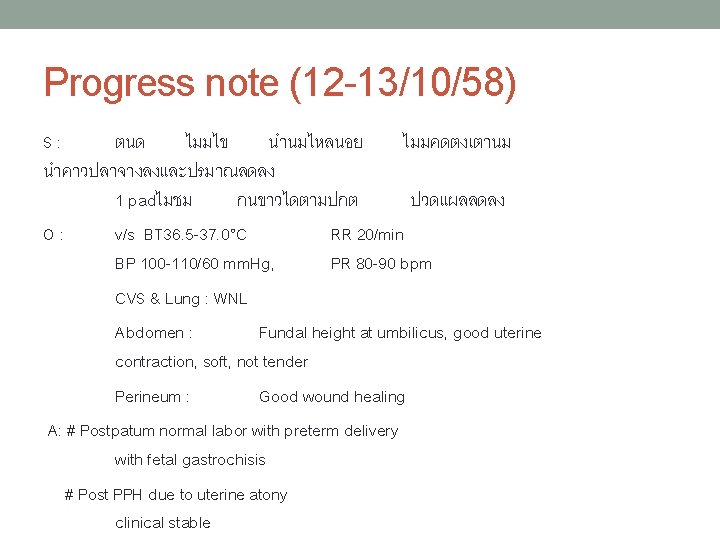
Progress note (12 -13/10/58) S: ตนด ไมมไข นำนมไหลนอย ไมมคดตงเตานม นำคาวปลาจางลงและปรมาณลดลง 1 padไมชม กนขาวไดตามปกต ปวดแผลลดลง O: v/s BT 36. 5 -37. 0°C RR 20/min BP 100 -110/60 mm. Hg, PR 80 -90 bpm CVS & Lung : WNL Abdomen : Fundal height at umbilicus, good uterine contraction, soft, not tender Perineum : Good wound healing A: # Postpatum normal labor with preterm delivery with fetal gastrochisis # Post PPH due to uterine atony clinical stable


Gastroschisis • Full thickness abdominal wall • Incidence 1: 20, 00 -40, 000 • Imaging – multiple loop of bowel are seen floating free in amniotic fluid (typical cauliflower appearance) - located in right umbilical cord - dilated loop of bowel in late pregnancy • Associated: : Associated Duodenum atresia, FGR • DDx - Rupture omphalocele - Umbilical cord cyst - Urachal cyst - Bladder or cloacal extrophy
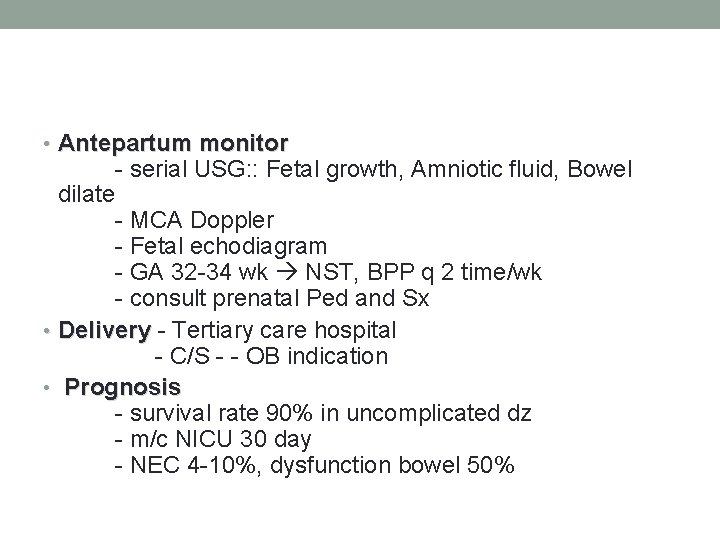
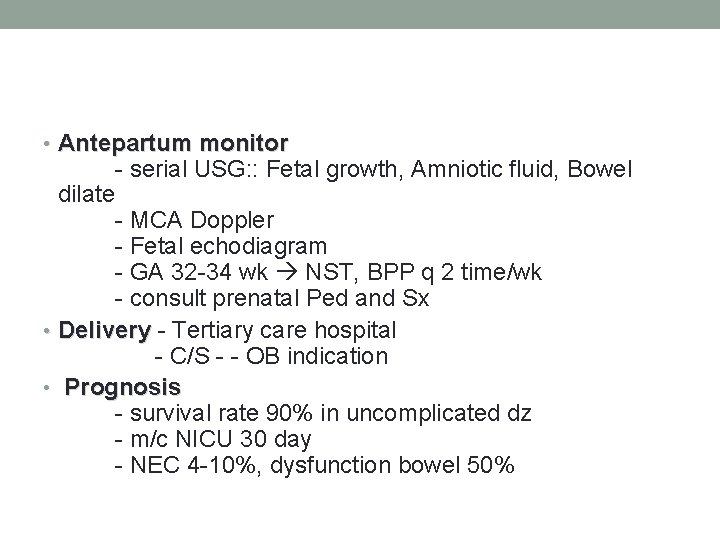
• Antepartum monitor dilate - serial USG: : Fetal growth, Amniotic fluid, Bowel - MCA Doppler - Fetal echodiagram - GA 32 -34 wk NST, BPP q 2 time/wk - consult prenatal Ped and Sx • Delivery - Tertiary care hospital - C/S - - OB indication • Prognosis - survival rate 90% in uncomplicated dz - m/c NICU 30 day - NEC 4 -10%, dysfunction bowel 50%

 Pawin slots
Pawin slots Pawin numthavaj
Pawin numthavaj Best case worst case average case
Best case worst case average case Fbi virtual case file case study
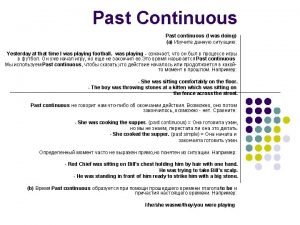
Fbi virtual case file case study Forms of past tense
Forms of past tense Perfect past progressive
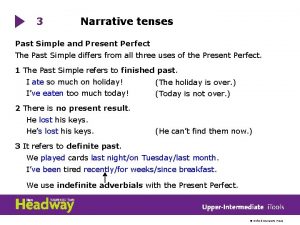
Perfect past progressive Simple past vs past continuous
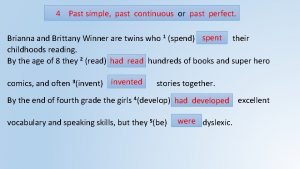
Simple past vs past continuous Exercise past simple past continuous and past perfect
Exercise past simple past continuous and past perfect Past simple past perfect and past continuous
Past simple past perfect and past continuous Present simple tense таблица
Present simple tense таблица 3a grammar narrative tenses answers
3a grammar narrative tenses answers Past continuous vs past simple
Past continuous vs past simple Past perfect simple vs past perfect continuous
Past perfect simple vs past perfect continuous What is narrative tense
What is narrative tense Ego 4 u passive
Ego 4 u passive Unwrap core standard
Unwrap core standard Vdoe math pathways
Vdoe math pathways Unjustified restrictive gatekeeping
Unjustified restrictive gatekeeping Authority style teaching
Authority style teaching Facilitator course distance learning
Facilitator course distance learning Focus group facilitator training
Focus group facilitator training Facilitátor feladatai
Facilitátor feladatai Motivation letter workshop
Motivation letter workshop Mfibank
Mfibank Thank you message for facilitator
Thank you message for facilitator Thank you facilitator
Thank you facilitator Entrepreneurship facilitator
Entrepreneurship facilitator