Hypersensitivity Reactions Allergies Refif alshawk Ph D Lec
- Slides: 21
Hypersensitivity Reactions, Allergies Refif alshawk (Ph. D) Lec 2&3 2018 -2019
Learning objectives After reading this lecture, you should be able to: Distinguish between the four types of hypersensitivities, and understand the immunological mechanisms behind each of them. For each of the four types of hypersensitivities, recognize the harmful effects of these immune responses when they become inappropriately vigorous responses (hypersensitivity reactions). Discuss the roles of environmental factors and genetics in predisposition to allergies
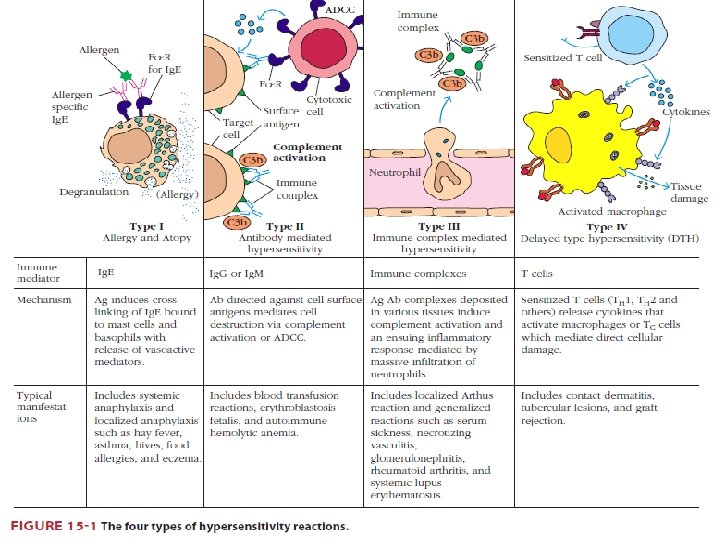
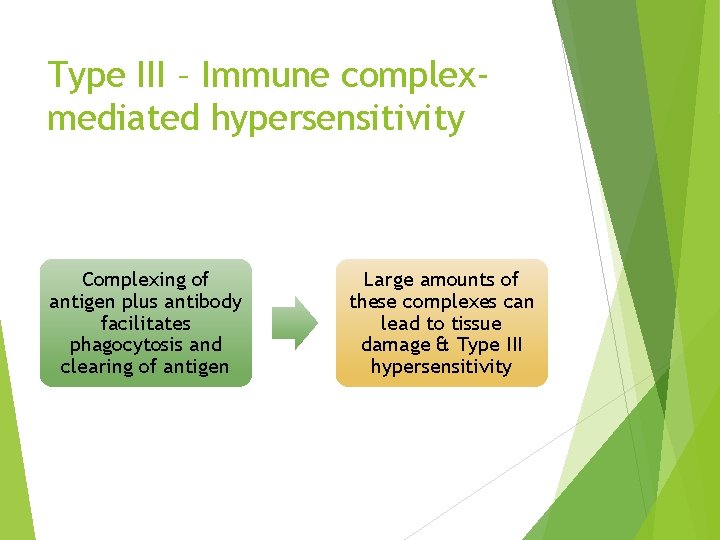
Type III – Immune complexmediated hypersensitivity Complexing of antigen plus antibody facilitates phagocytosis and clearing of antigen Large amounts of these complexes can lead to tissue damage & Type III hypersensitivity
Conditions associated with the initiation of a type III response include : (1) the presence of antigens capable of generating particularly extensive antigenantibody lattices, (2) a high intrinsic affinity of antigens for particular tissues (3) the presence of highly charged antigens (which can affect immune complex engulfment) and (4) a compromised phagocytic system.
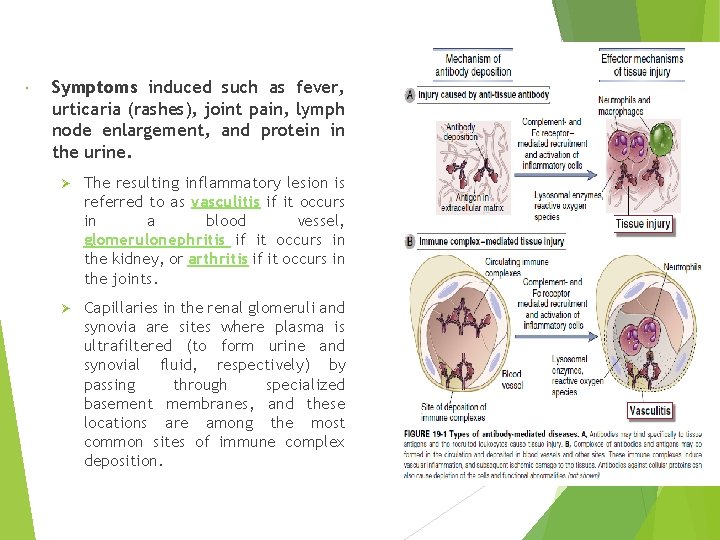
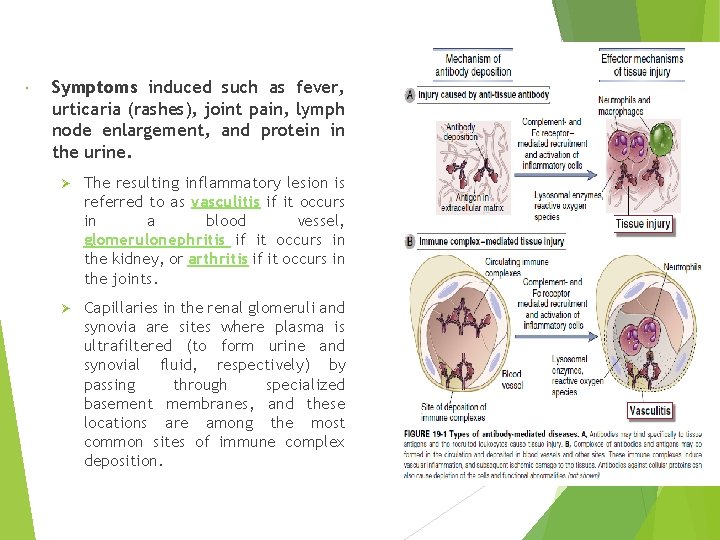
Symptoms induced such as fever, urticaria (rashes), joint pain, lymph node enlargement, and protein in the urine. Ø The resulting inflammatory lesion is referred to as vasculitis if it occurs in a blood vessel, glomerulonephritis if it occurs in the kidney, or arthritis if it occurs in the joints. Ø Capillaries in the renal glomeruli and synovia are sites where plasma is ultrafiltered (to form urine and synovial fluid, respectively) by passing through specialized basement membranes, and these locations are among the most common sites of immune complex deposition.
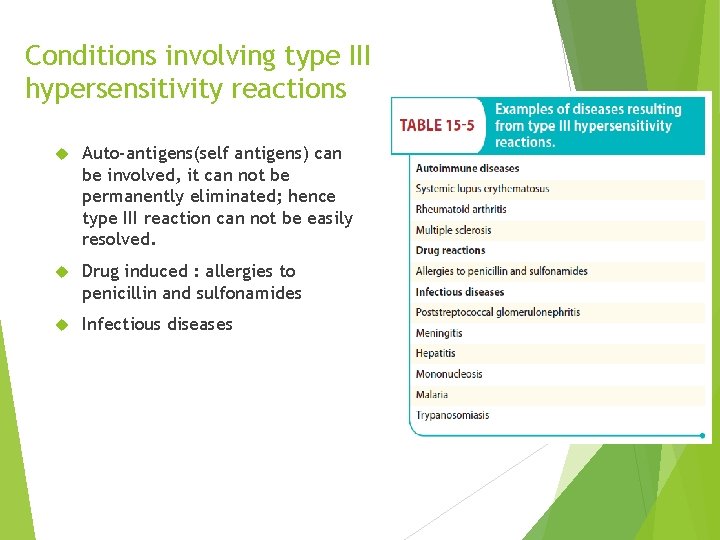
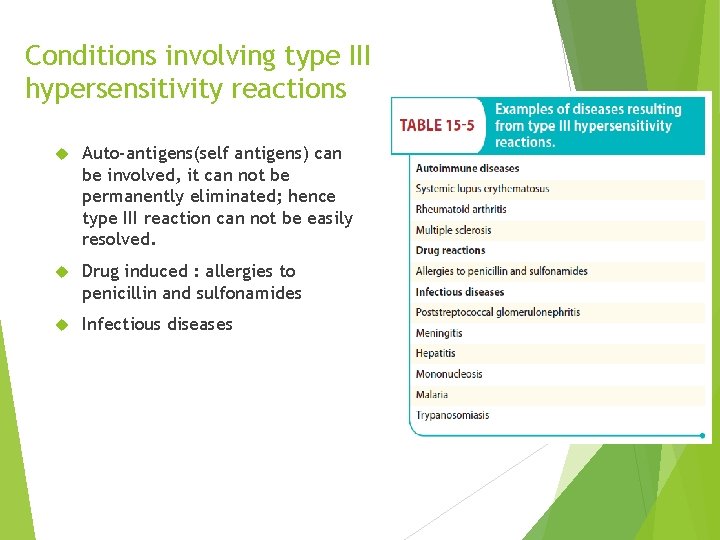
Conditions involving type III hypersensitivity reactions Auto-antigens(self antigens) can be involved, it can not be permanently eliminated; hence type III reaction can not be easily resolved. Drug induced : allergies to penicillin and sulfonamides Infectious diseases
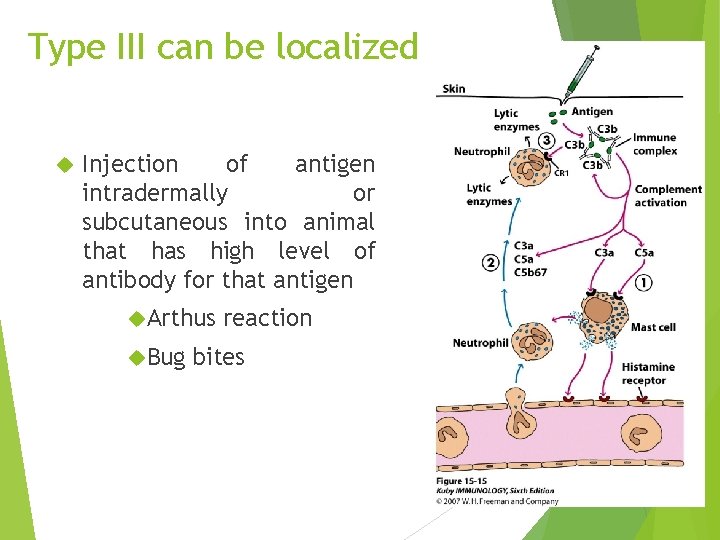
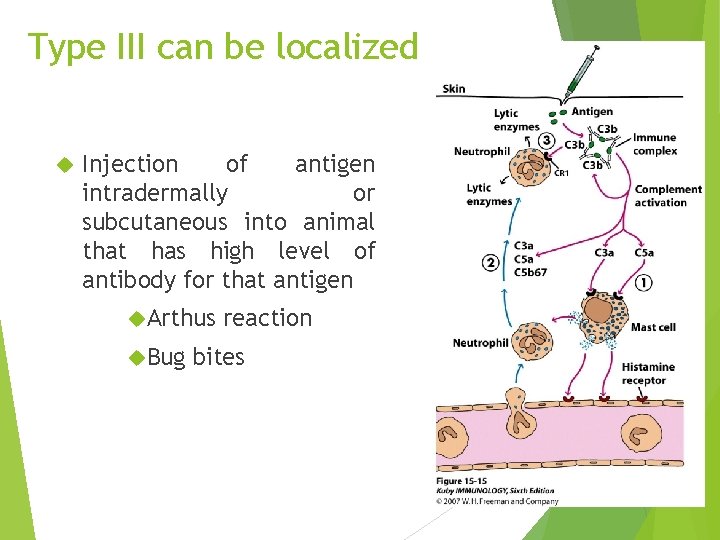
Type III can be localized Injection of antigen intradermally or subcutaneous into animal that has high level of antibody for that antigen Arthus Bug reaction bites
Local (Arthus reaction) and typically elicited in the skin when a low dose of antigen is injected and immune complexes form locally. Ig. G antibodies are involved, and the resulting activation of complement leads to activation of mast cells and neutrophils, mediator release, and enhanced vascular permeability. This typically occurs in about 12 hours.
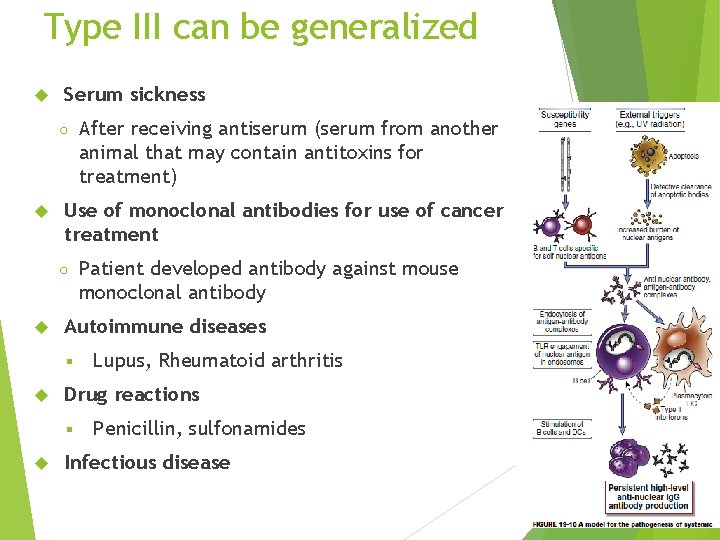
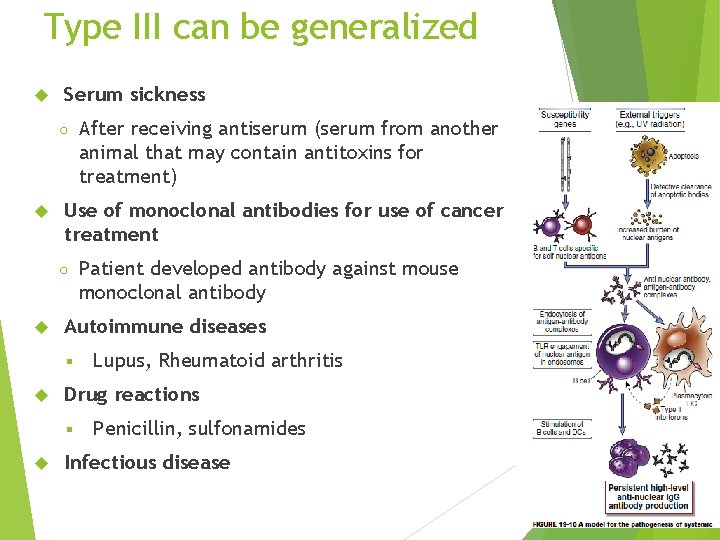
Type III can be generalized Serum sickness ○ Use of monoclonal antibodies for use of cancer treatment ○ Lupus, Rheumatoid arthritis Drug reactions § Patient developed antibody against mouse monoclonal antibody Autoimmune diseases § After receiving antiserum (serum from another animal that may contain antitoxins for treatment) Penicillin, sulfonamides Infectious disease
Systemic immune complex acute poststreptococcal glomerulonephritis is a well known immune complex disease. Its onset occurs several weeks after a group A β-hemolytic streptococcal infection, particularly of the skin, and often occurs with infection due to nephritogenic types of streptococci. It is likely that streptococcal antigen– antibody complexes are filtered out by glomeruli, fix complement, and attract neutrophils. This series of events results in an inflammatory process that damages the kidney.
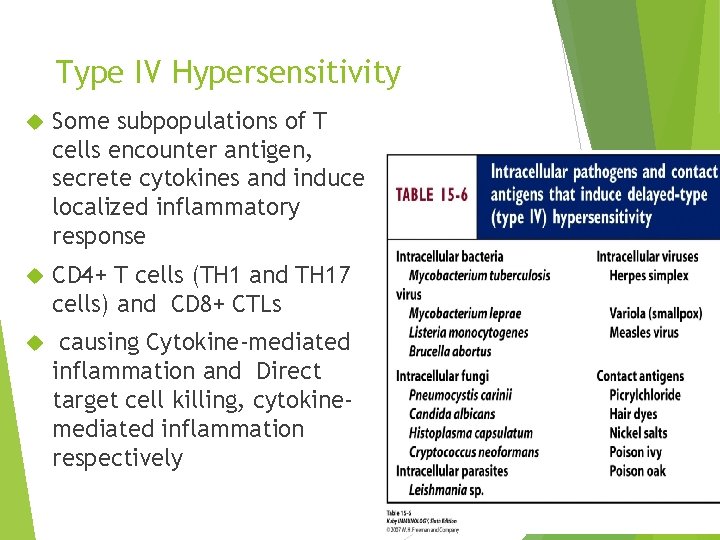
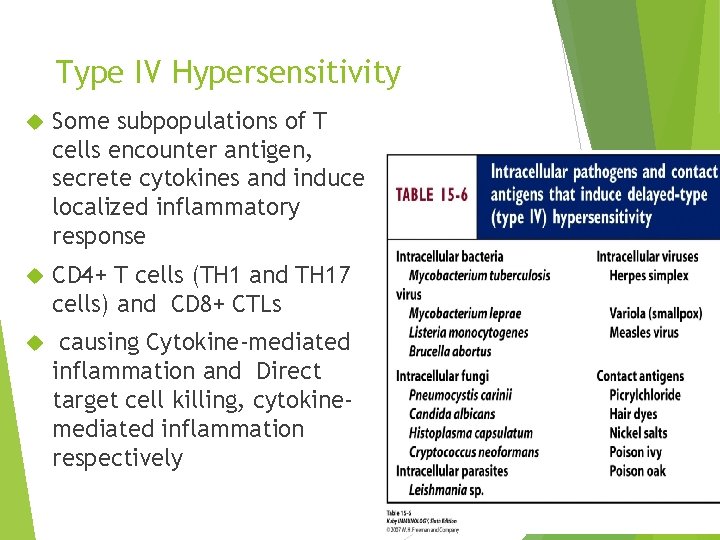
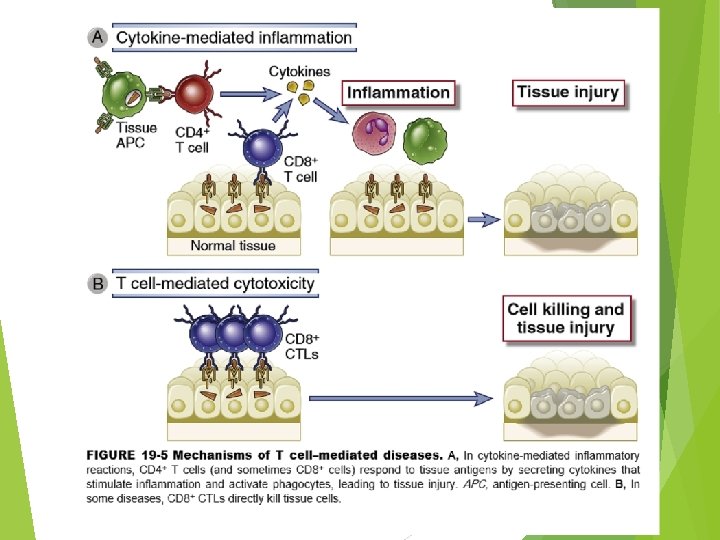
Type IV Hypersensitivity Some subpopulations of T cells encounter antigen, secrete cytokines and induce localized inflammatory response CD 4+ T cells (TH 1 and TH 17 cells) and CD 8+ CTLs causing Cytokine-mediated inflammation and Direct target cell killing, cytokinemediated inflammation respectively
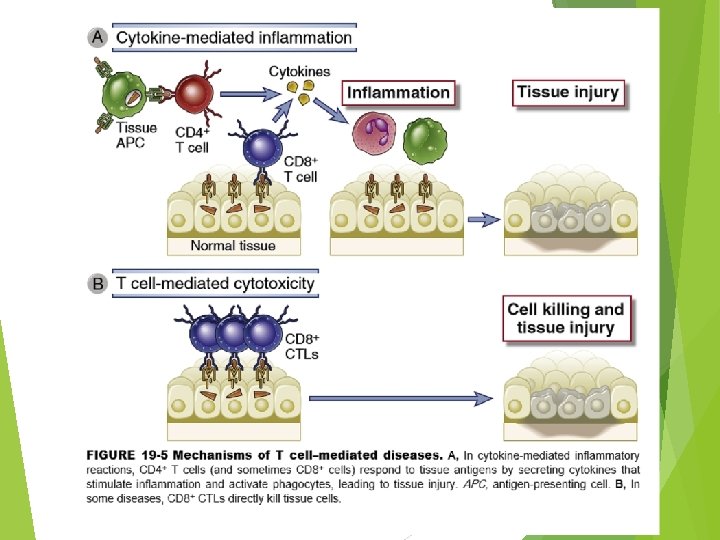
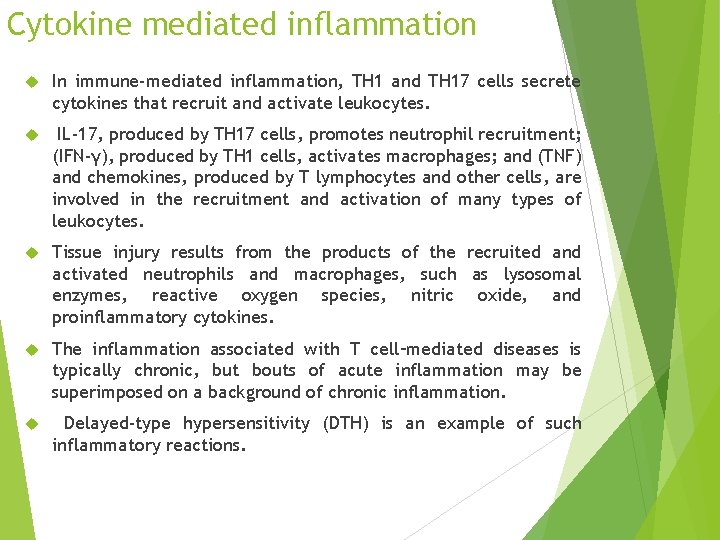
Cytokine mediated inflammation In immune-mediated inflammation, TH 1 and TH 17 cells secrete cytokines that recruit and activate leukocytes. IL-17, produced by TH 17 cells, promotes neutrophil recruitment; (IFN-γ), produced by TH 1 cells, activates macrophages; and (TNF) and chemokines, produced by T lymphocytes and other cells, are involved in the recruitment and activation of many types of leukocytes. Tissue injury results from the products of the recruited and activated neutrophils and macrophages, such as lysosomal enzymes, reactive oxygen species, nitric oxide, and proinflammatory cytokines. The inflammation associated with T cell–mediated diseases is typically chronic, but bouts of acute inflammation may be superimposed on a background of chronic inflammation. Delayed-type hypersensitivity (DTH) is an example of such inflammatory reactions.
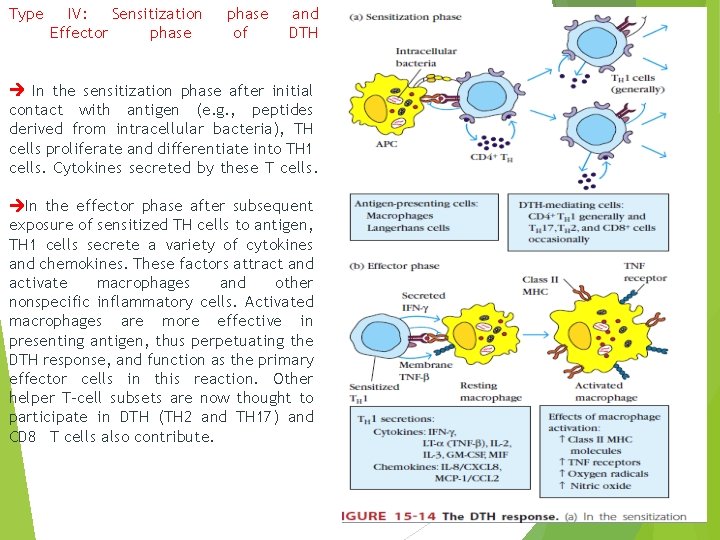
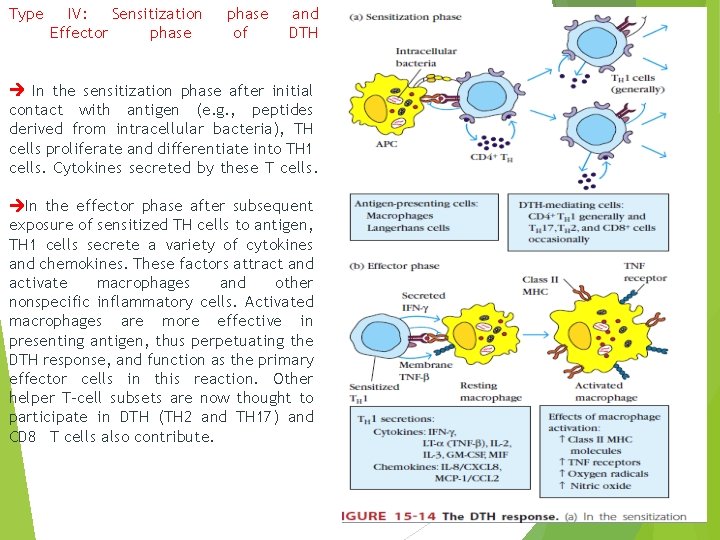
Type IV: Sensitization Effector phase of and DTH In the sensitization phase after initial contact with antigen (e. g. , peptides derived from intracellular bacteria), TH cells proliferate and differentiate into TH 1 cells. Cytokines secreted by these T cells. In the effector phase after subsequent exposure of sensitized TH cells to antigen, TH 1 cells secrete a variety of cytokines and chemokines. These factors attract and activate macrophages and other nonspecific inflammatory cells. Activated macrophages are more effective in presenting antigen, thus perpetuating the DTH response, and function as the primary effector cells in this reaction. Other helper T-cell subsets are now thought to participate in DTH (TH 2 and TH 17) and CD 8 T cells also contribute.
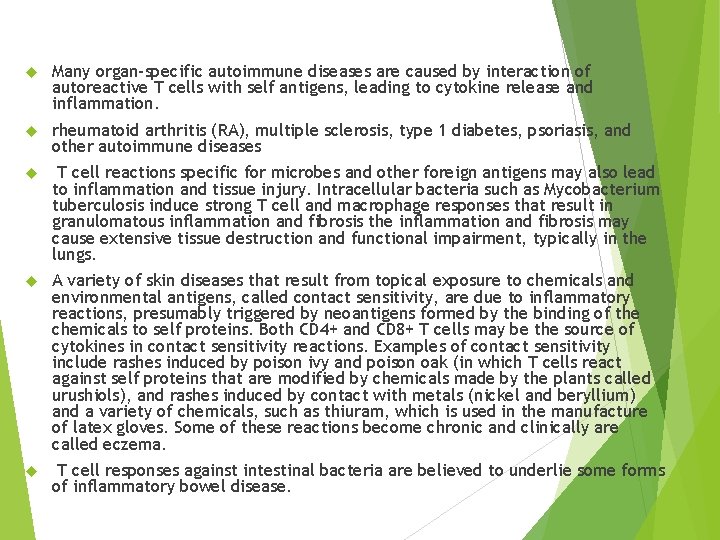
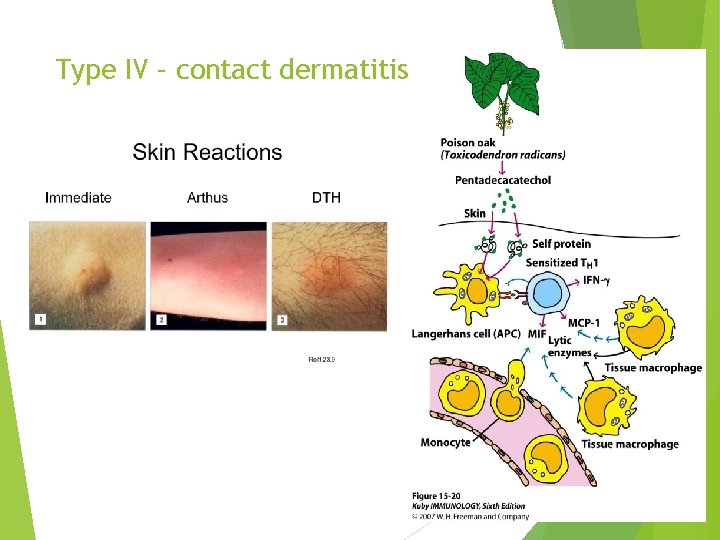
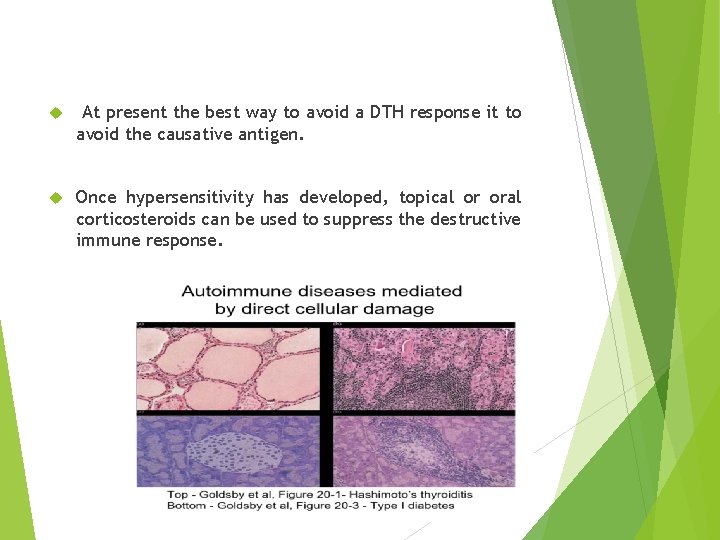
Many organ-specific autoimmune diseases are caused by interaction of autoreactive T cells with self antigens, leading to cytokine release and inflammation. rheumatoid arthritis (RA), multiple sclerosis, type 1 diabetes, psoriasis, and other autoimmune diseases T cell reactions specific for microbes and other foreign antigens may also lead to inflammation and tissue injury. Intracellular bacteria such as Mycobacterium tuberculosis induce strong T cell and macrophage responses that result in granulomatous inflammation and fibrosis the inflammation and fibrosis may cause extensive tissue destruction and functional impairment, typically in the lungs. A variety of skin diseases that result from topical exposure to chemicals and environmental antigens, called contact sensitivity, are due to inflammatory reactions, presumably triggered by neoantigens formed by the binding of the chemicals to self proteins. Both CD 4+ and CD 8+ T cells may be the source of cytokines in contact sensitivity reactions. Examples of contact sensitivity include rashes induced by poison ivy and poison oak (in which T cells react against self proteins that are modified by chemicals made by the plants called urushiols), and rashes induced by contact with metals (nickel and beryllium) and a variety of chemicals, such as thiuram, which is used in the manufacture of latex gloves. Some of these reactions become chronic and clinically are called eczema. T cell responses against intestinal bacteria are believed to underlie some forms of inflammatory bowel disease.
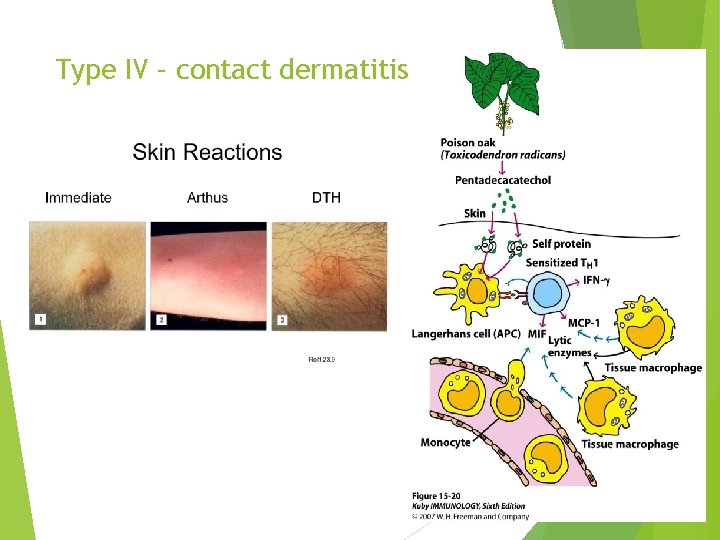
Type IV – contact dermatitis
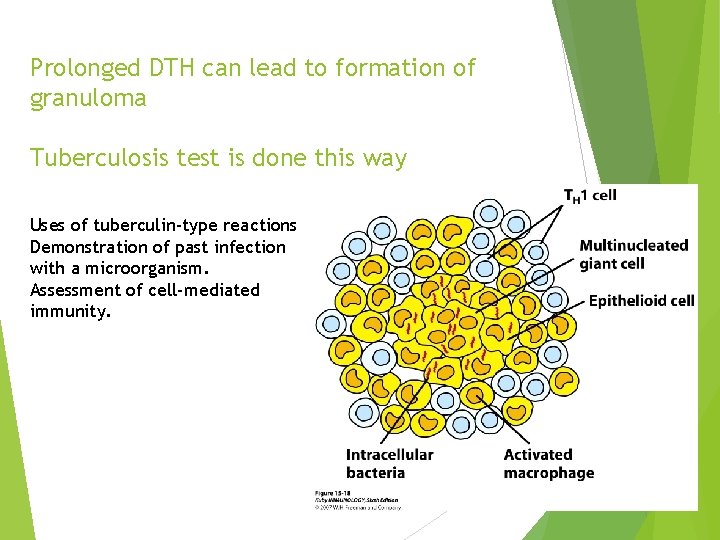
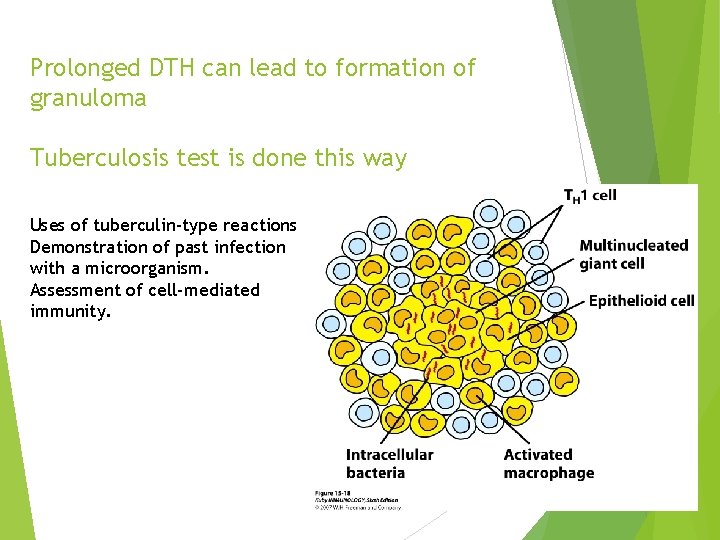
Prolonged DTH can lead to formation of granuloma Tuberculosis test is done this way Uses of tuberculin-type reactions Demonstration of past infection with a microorganism. Assessment of cell-mediated immunity.
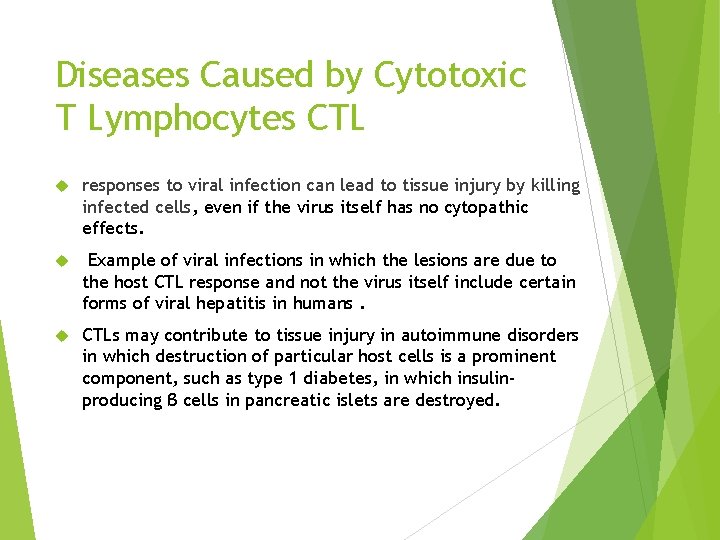
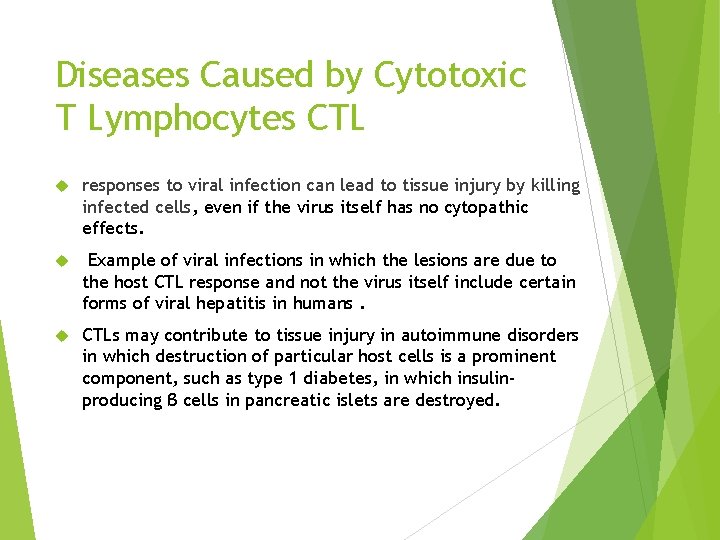
Diseases Caused by Cytotoxic T Lymphocytes CTL responses to viral infection can lead to tissue injury by killing infected cells, even if the virus itself has no cytopathic effects. Example of viral infections in which the lesions are due to the host CTL response and not the virus itself include certain forms of viral hepatitis in humans. CTLs may contribute to tissue injury in autoimmune disorders in which destruction of particular host cells is a prominent component, such as type 1 diabetes, in which insulinproducing β cells in pancreatic islets are destroyed.
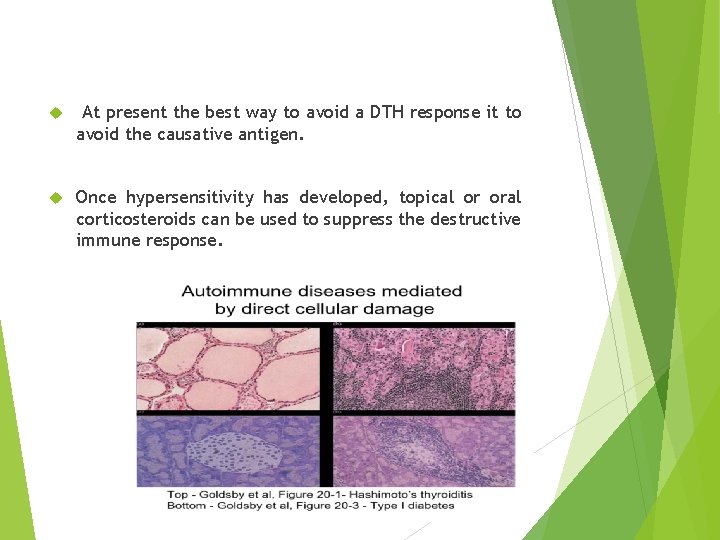
At present the best way to avoid a DTH response it to avoid the causative antigen. Once hypersensitivity has developed, topical or oral corticosteroids can be used to suppress the destructive immune response.
Refferences : v Immunology , Kuby, seventh edition 2013 v Immunology , Kuby, eighth edition 2019 v Medical microbiology, Jawetz, 26 th edition v Cellular and Molecular Immunology, Abul K. Abbas, 8 th edition.