The immune system gone wrong Diseases of immunity

- Slides: 44
The immune system gone wrong: Diseases of immunity
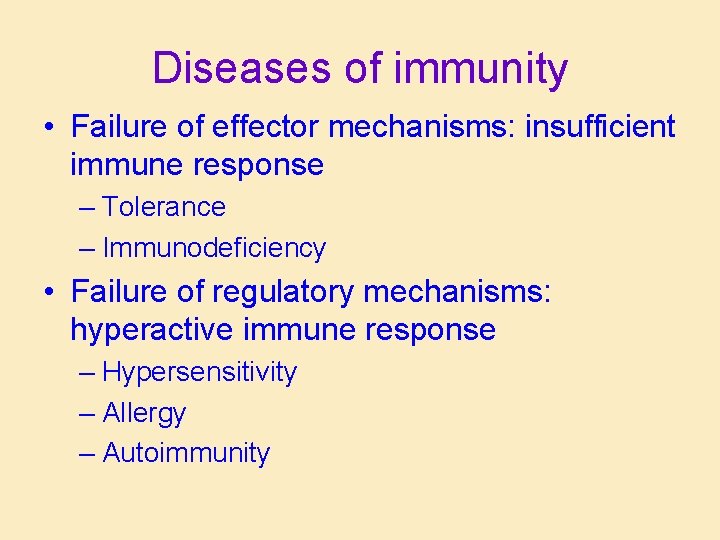
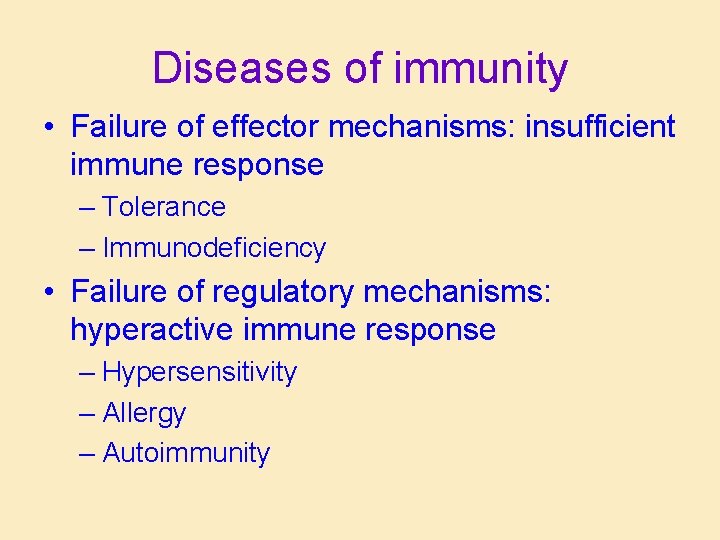
Diseases of immunity • Failure of effector mechanisms: insufficient immune response – Tolerance – Immunodeficiency • Failure of regulatory mechanisms: hyperactive immune response – Hypersensitivity – Allergy – Autoimmunity
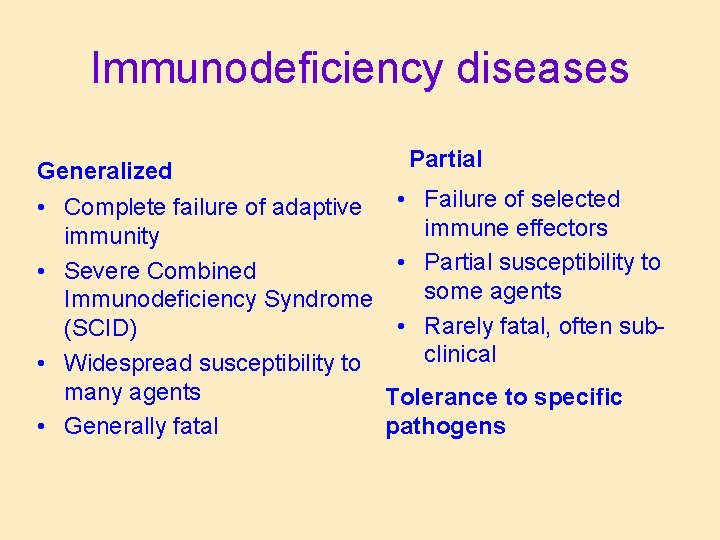
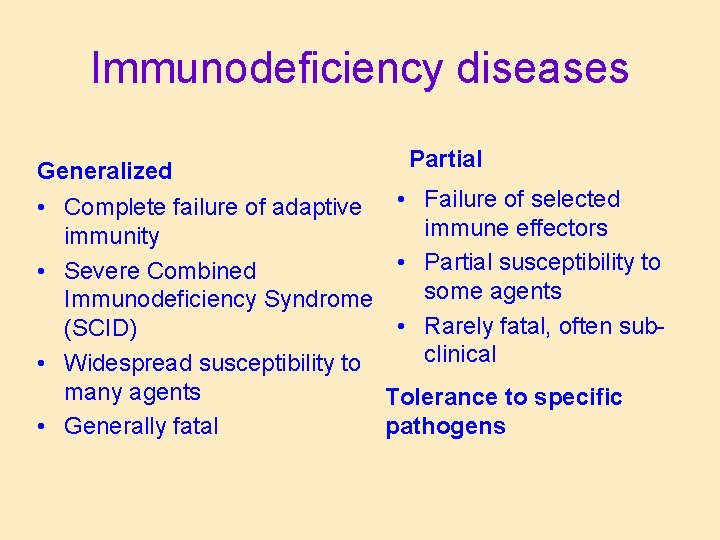
Immunodeficiency diseases Generalized • Complete failure of adaptive immunity • Severe Combined Immunodeficiency Syndrome (SCID) • Widespread susceptibility to many agents • Generally fatal Partial • Failure of selected immune effectors • Partial susceptibility to some agents • Rarely fatal, often subclinical Tolerance to specific pathogens
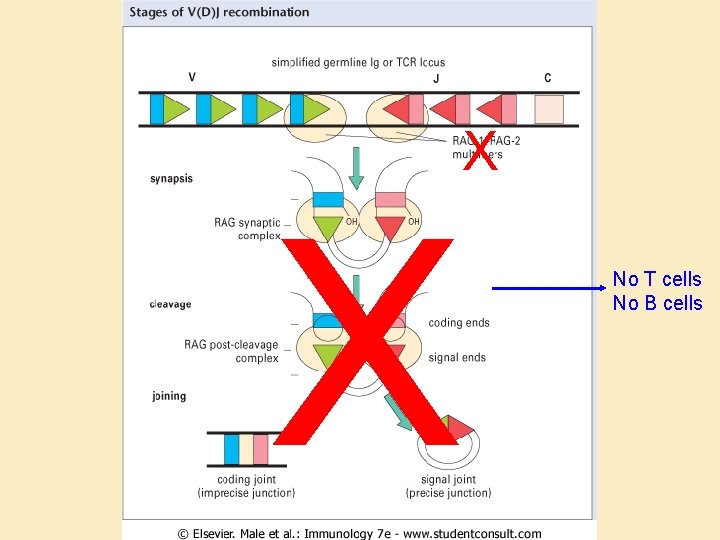
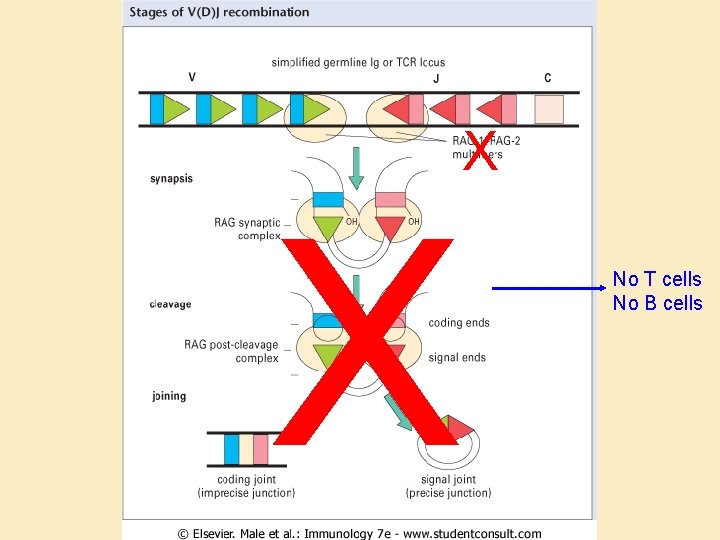
X X No T cells No B cells
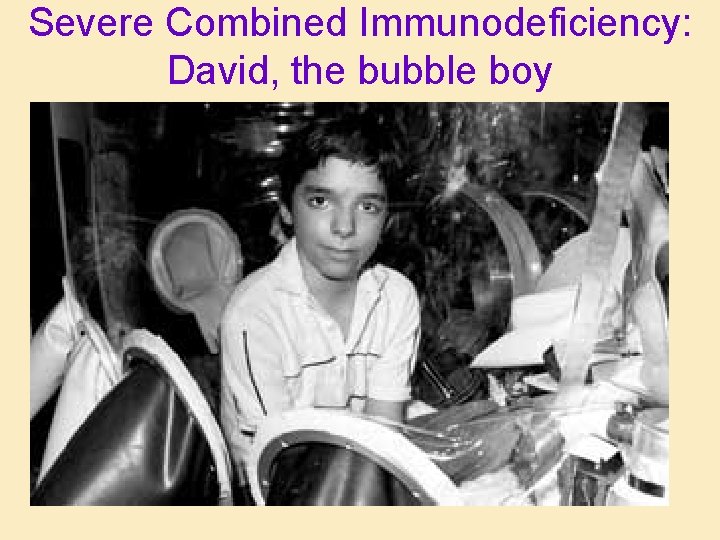
Severe Combined Immunodeficiency: David, the bubble boy
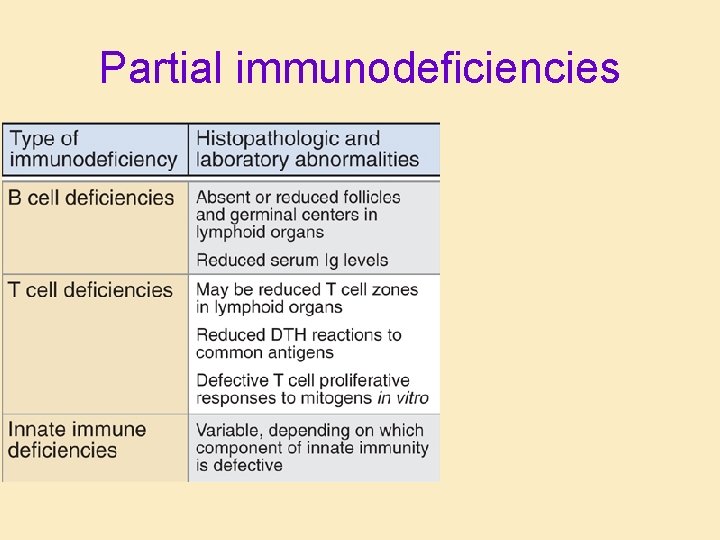
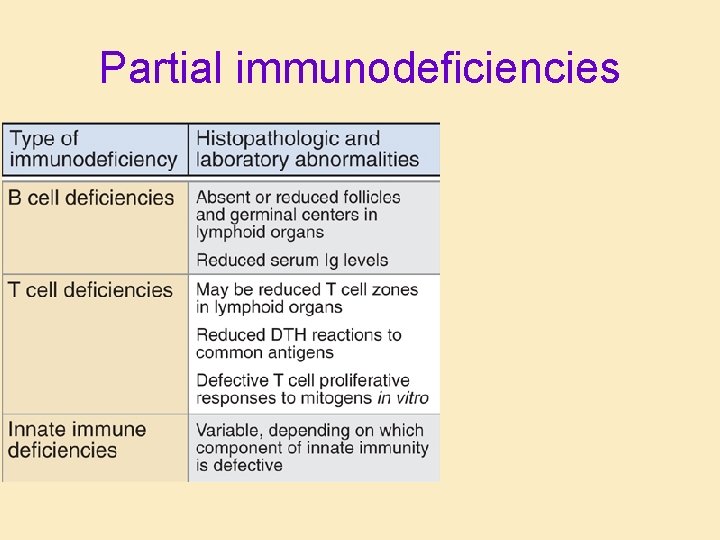
Partial immunodeficiencies
Tolerance to a single pathogen • Factors that promote tolerance – Young age – Large dose – Soluble antigen – Antigen in utero • Example: Bovine Virus Diarrhea
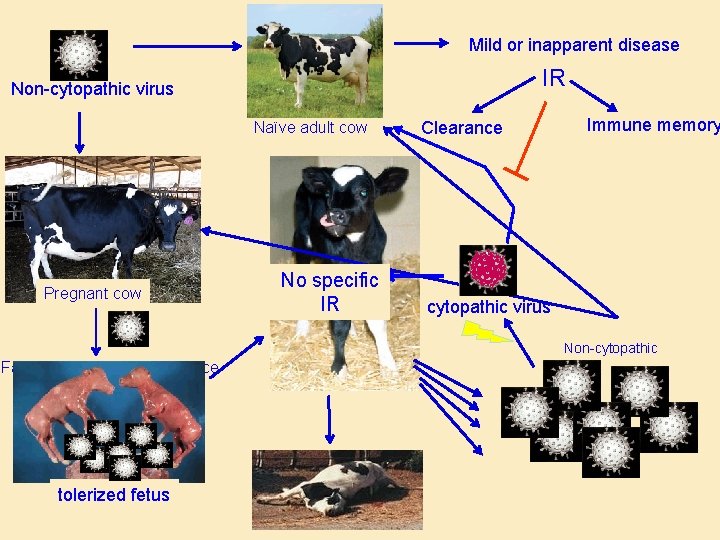
Bovine Virus Diarrhea • • Viral disease of cattle Common and widespread Most commonly subclinical: Non-cytopathic Potentially fatal: – In utero infection – Tolerance develops – Massive viral shedding – Cytopathic strains develop – Severe disease
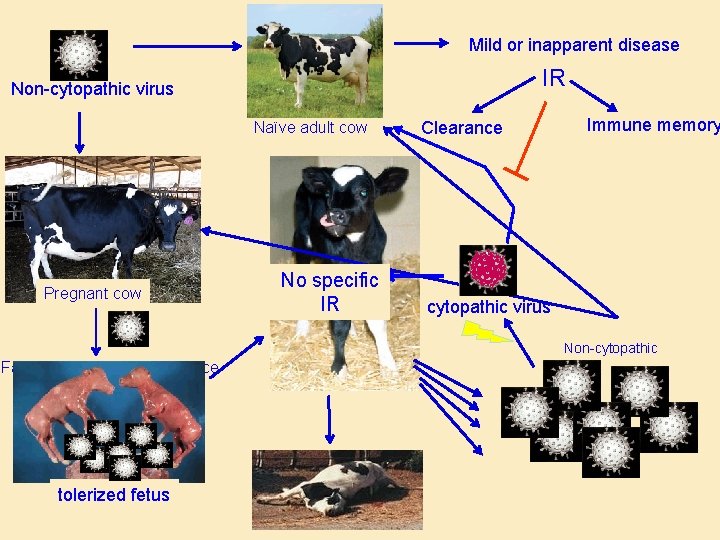
Mild or inapparent disease IR Non-cytopathic virus Naïve adult cow Pregnant cow No specific IR Clearance Immune memory cytopathic virus Non-cytopathic Factors that promote tolerance Young age Large dose Soluble antigen Antigen in utero tolerized fetus
BVD Outcome • Tolerized calves: – Apparently healthy – Shed virus – Spread infection • Cytopathic virus – Random mutants – Disease in tolerized or non-immune animals
Immune response gone wrong: Hypersensitivity • Hypersensitivity = inappropriate/unregulated response to antigen • Foreign antigen = allergy • Self antigen = autoimmunity • Common
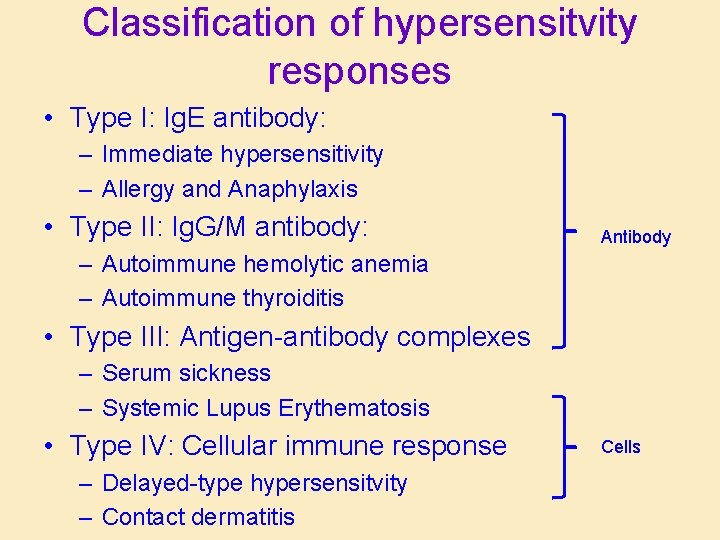
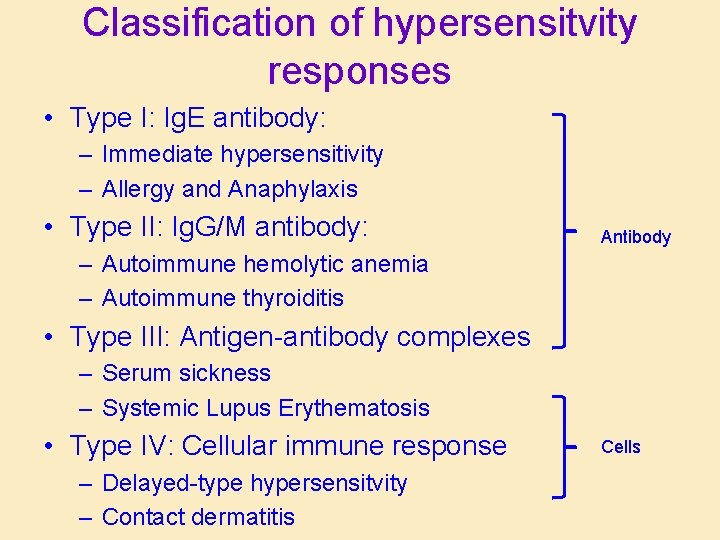
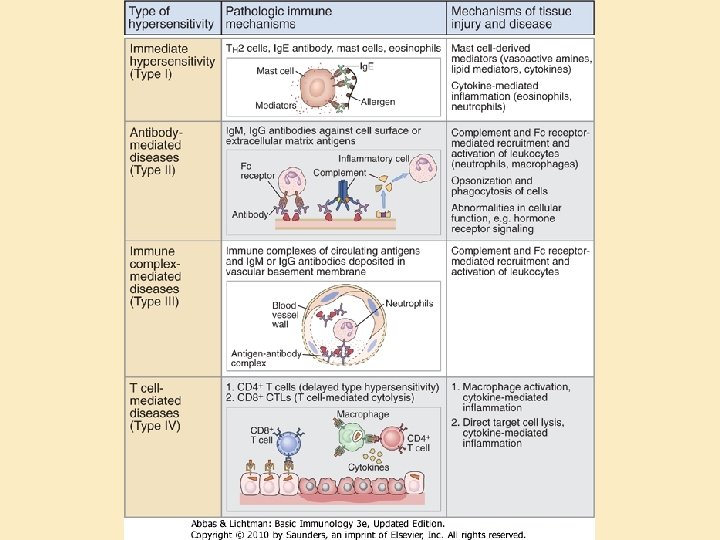
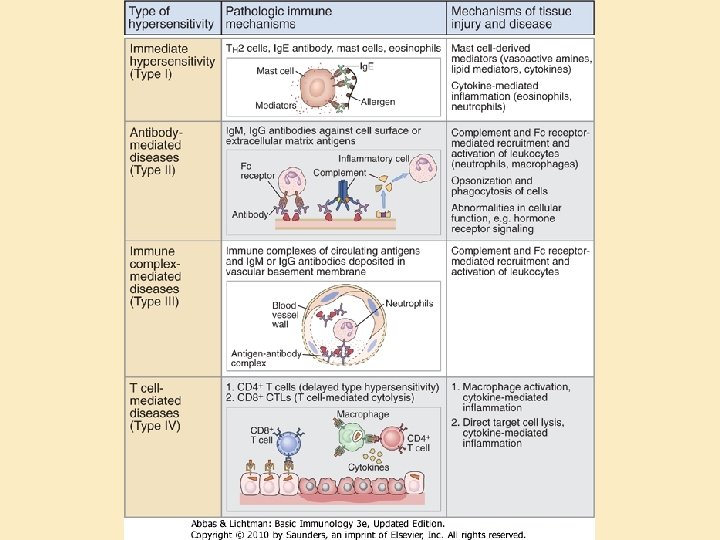
Classification of hypersensitvity responses • Type I: Ig. E antibody: – Immediate hypersensitivity – Allergy and Anaphylaxis • Type II: Ig. G/M antibody: Antibody – Autoimmune hemolytic anemia – Autoimmune thyroiditis • Type III: Antigen-antibody complexes – Serum sickness – Systemic Lupus Erythematosis • Type IV: Cellular immune response – Delayed-type hypersensitvity – Contact dermatitis Cells
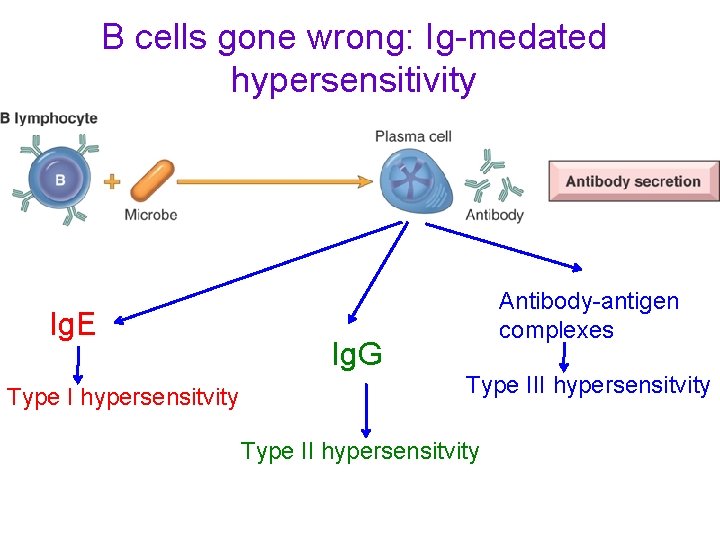
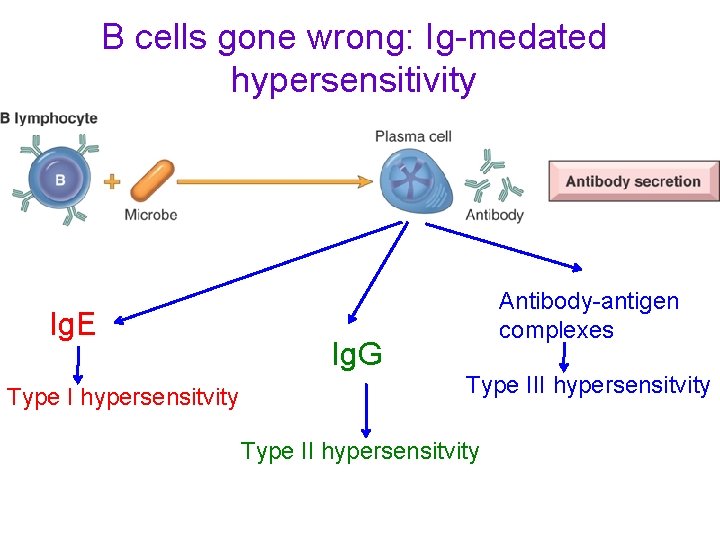
B cells gone wrong: Ig-medated hypersensitivity Ig. E Type I hypersensitvity Ig. G Antibody-antigen complexes Type III hypersensitvity Type II hypersensitvity
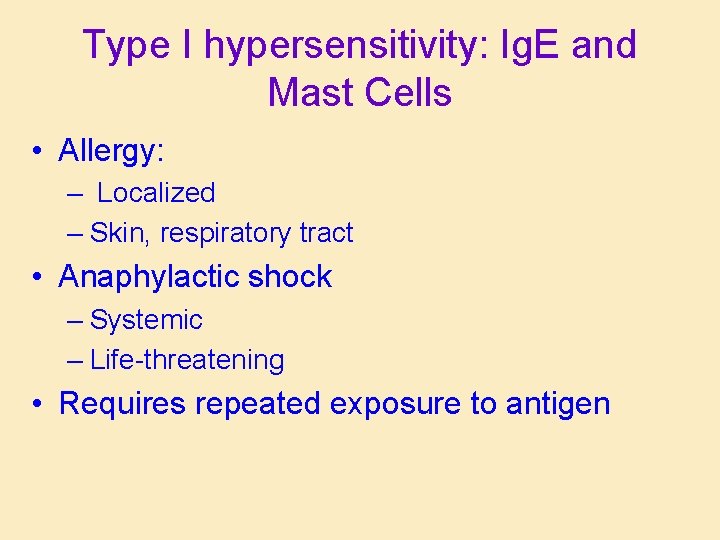
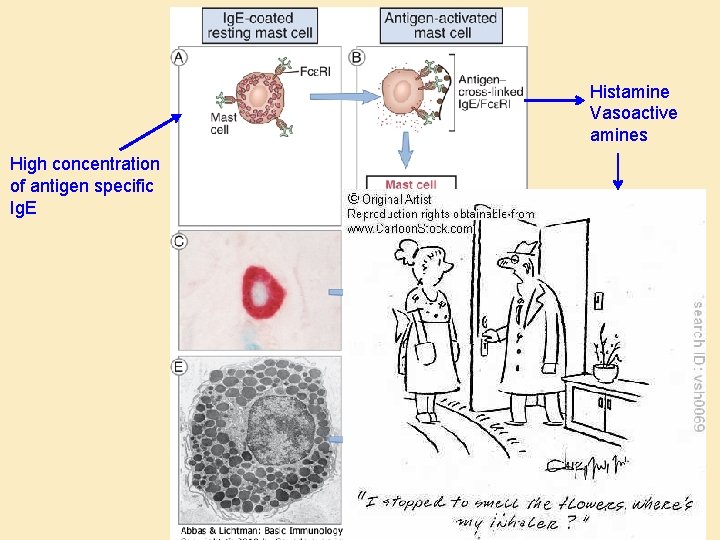
Type I hypersensitivity: Ig. E and Mast Cells • Allergy: – Localized – Skin, respiratory tract • Anaphylactic shock – Systemic – Life-threatening • Requires repeated exposure to antigen
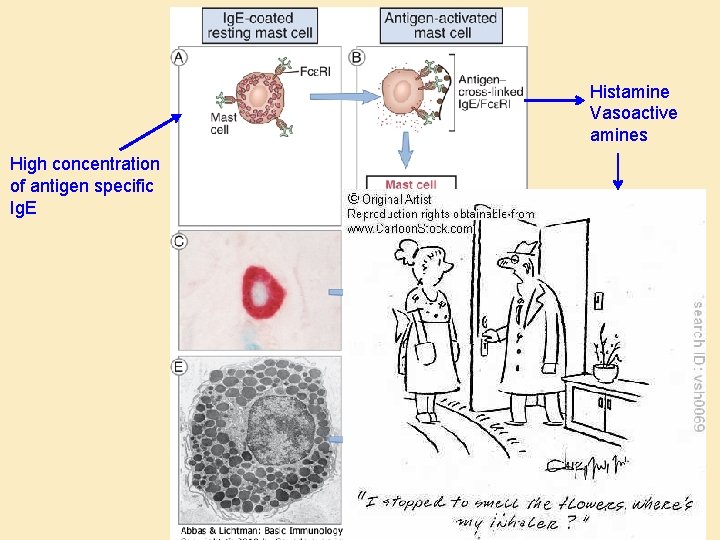
Histamine Vasoactive amines High concentration of antigen specific Ig. E
Ig. M and Ig. G-mediated hypersensitivity • Type II: Soluble antibody • Type III: Circulating immune complexes (antibody/antigen/complement)
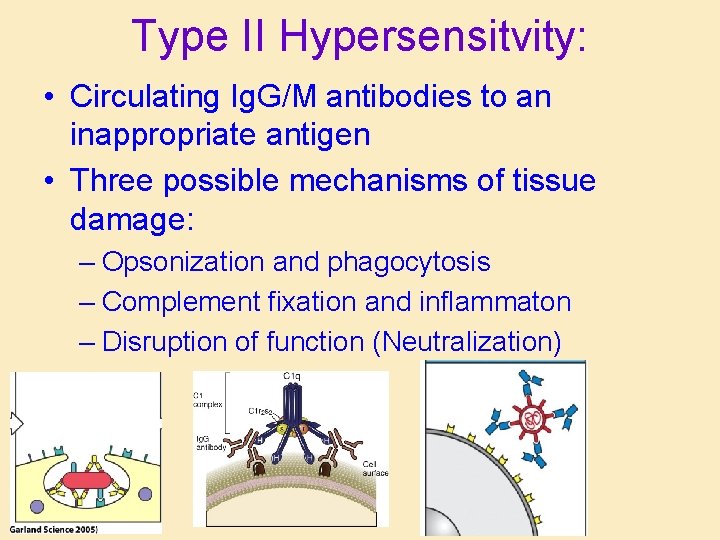
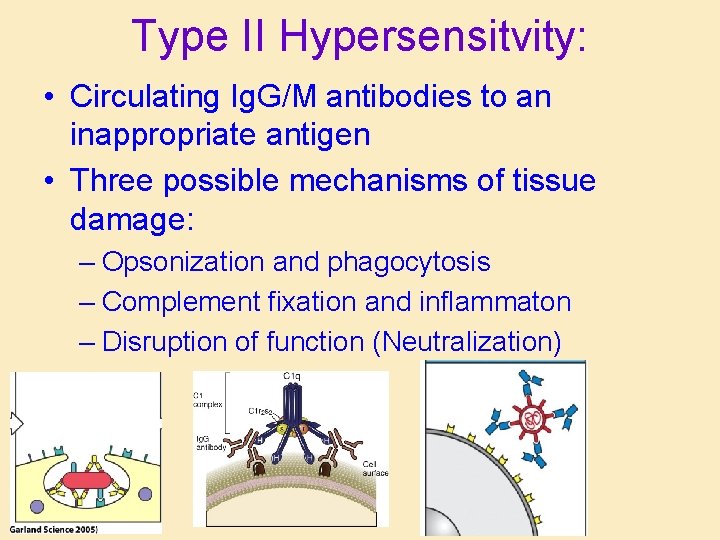
Type II Hypersensitvity: • Circulating Ig. G/M antibodies to an inappropriate antigen • Three possible mechanisms of tissue damage: – Opsonization and phagocytosis – Complement fixation and inflammaton – Disruption of function (Neutralization)
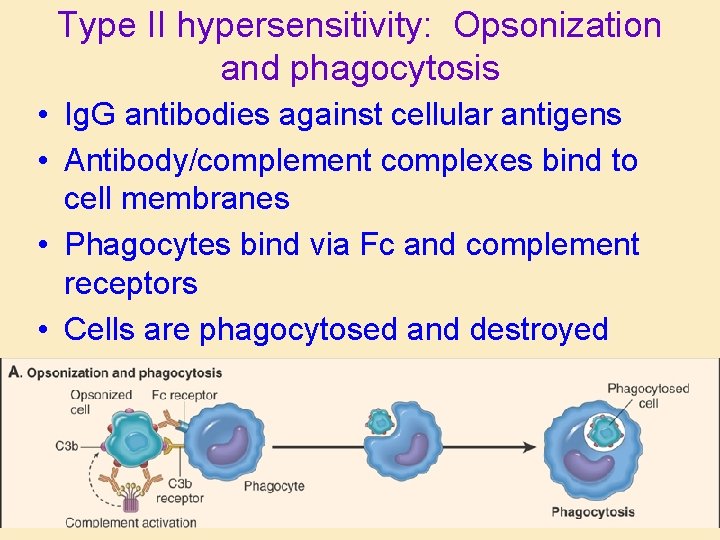
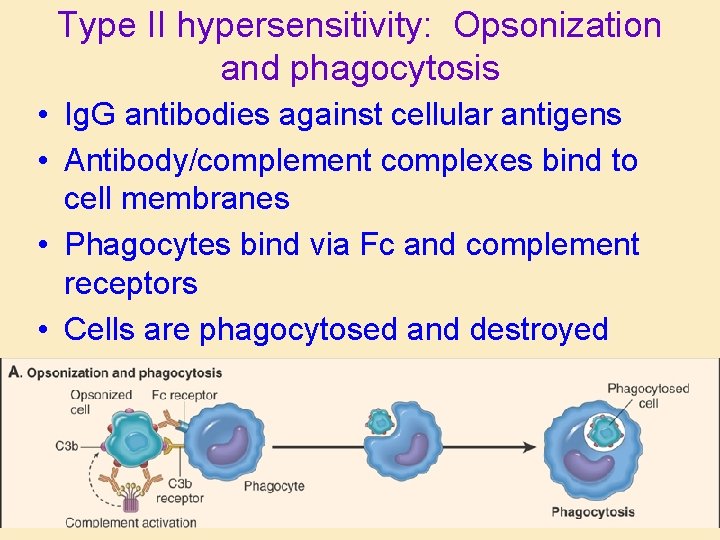
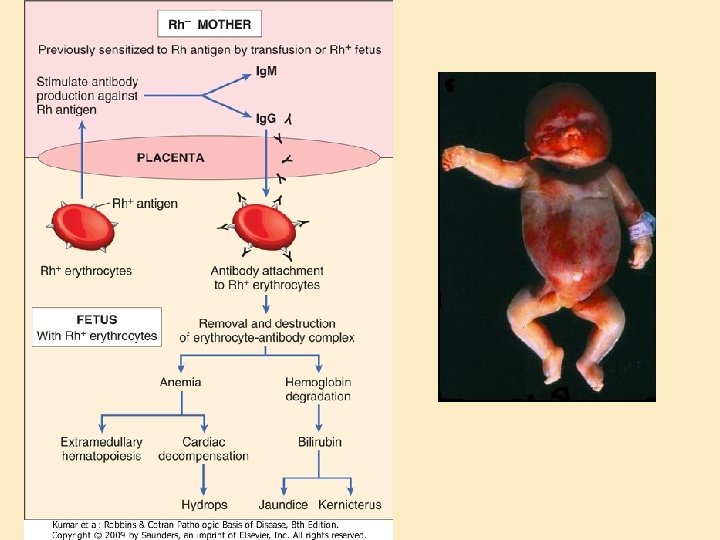
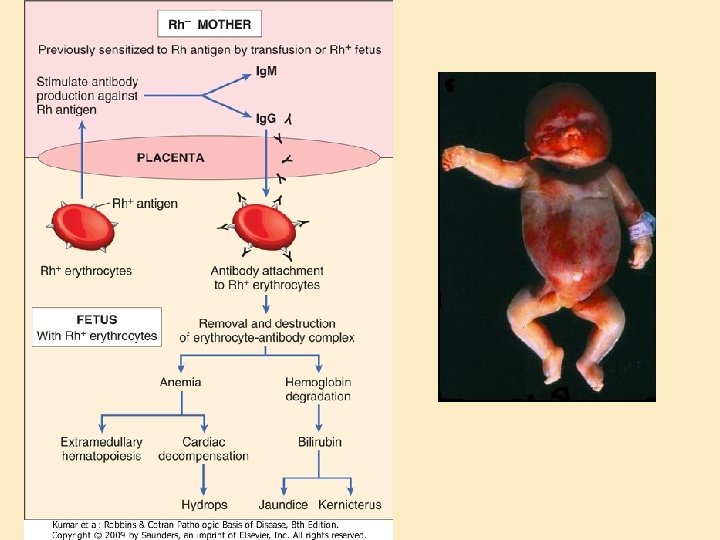
Type II hypersensitivity: Opsonization and phagocytosis • Ig. G antibodies against cellular antigens • Antibody/complement complexes bind to cell membranes • Phagocytes bind via Fc and complement receptors • Cells are phagocytosed and destroyed
Gross photo alert
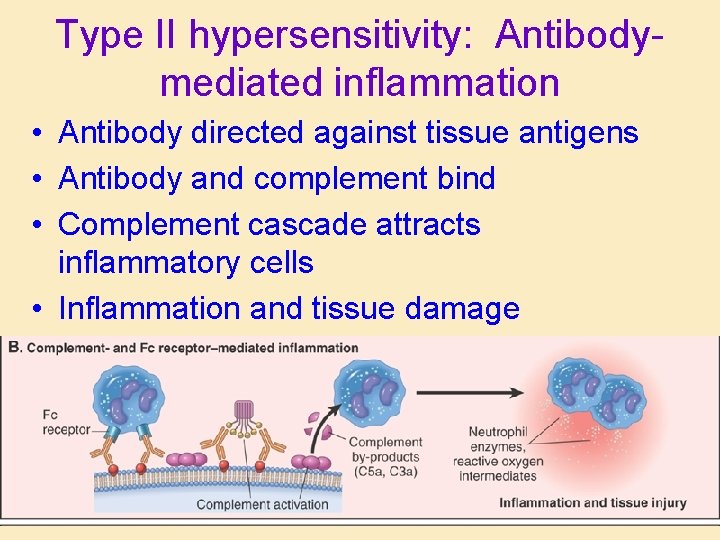
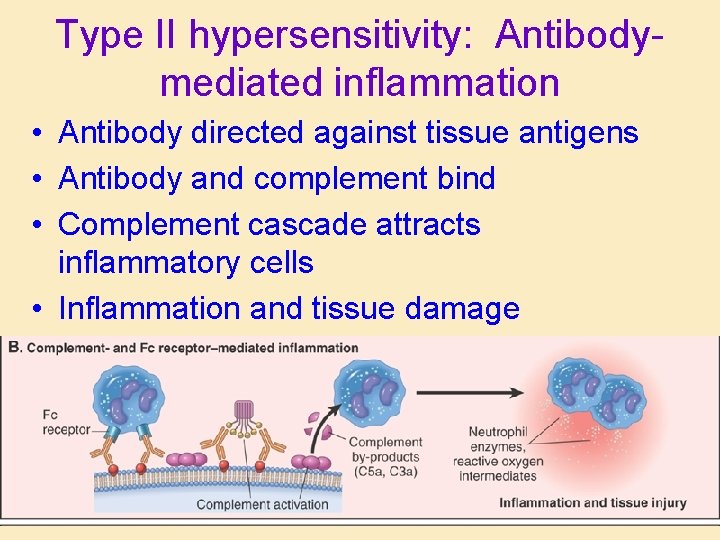
Type II hypersensitivity: Antibodymediated inflammation • Antibody directed against tissue antigens • Antibody and complement bind • Complement cascade attracts inflammatory cells • Inflammation and tissue damage
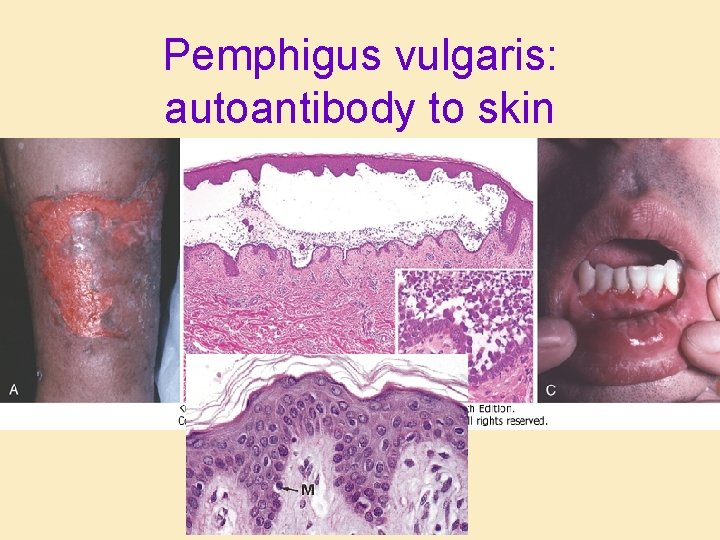
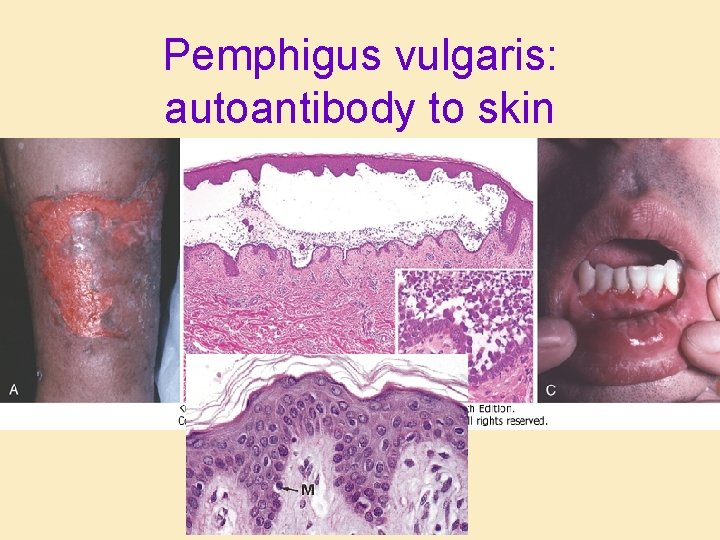
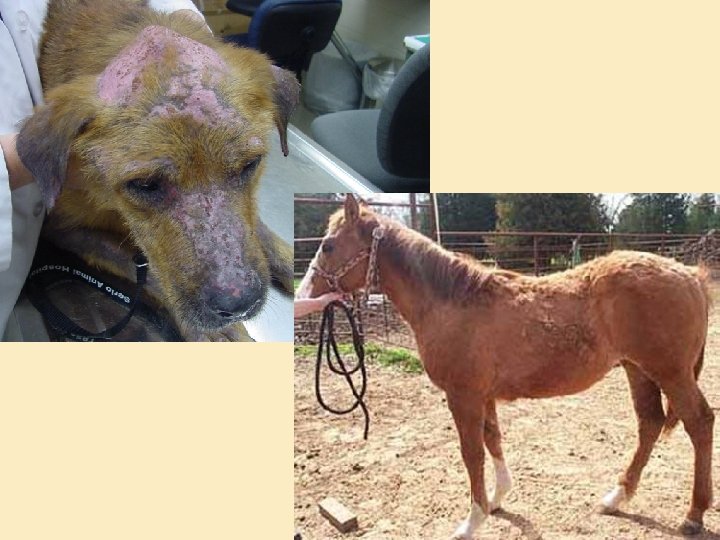
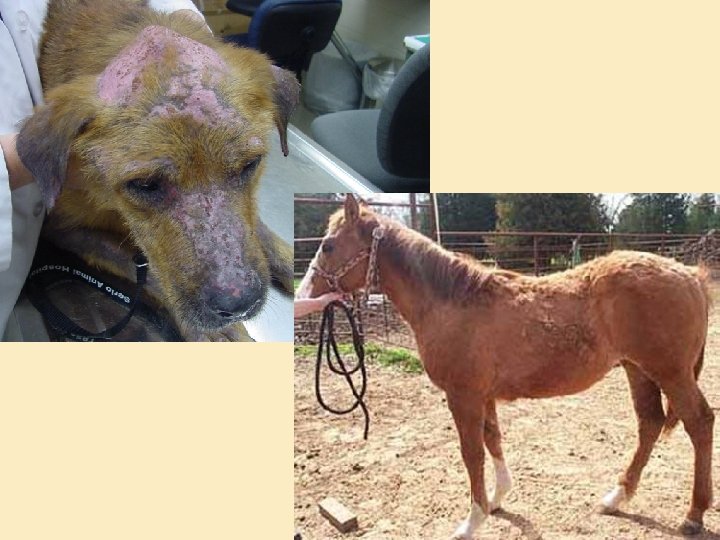
Pemphigus vulgaris: autoantibody to skin
Type II hypersensitivity: disruption of function • Neutralizing antibody • Directed against cellular receptors: – Interfere with ligand binding: prevent activation: Myasthenia gravis – Mimic ligand: activate receptor; Grave’s disease
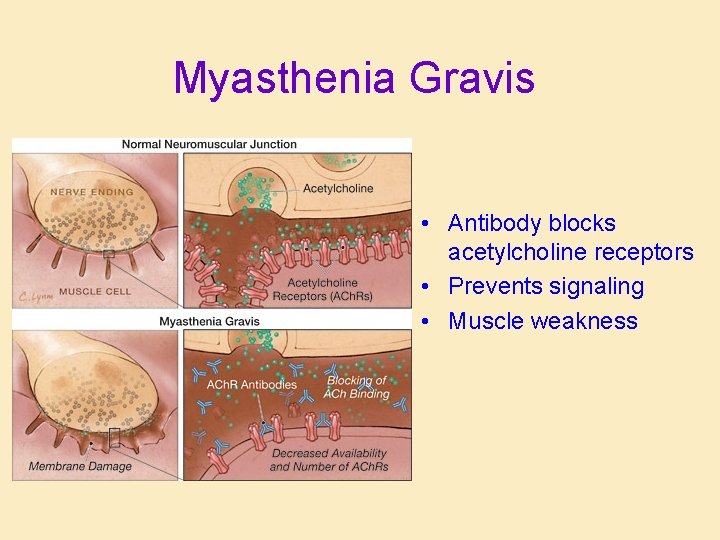
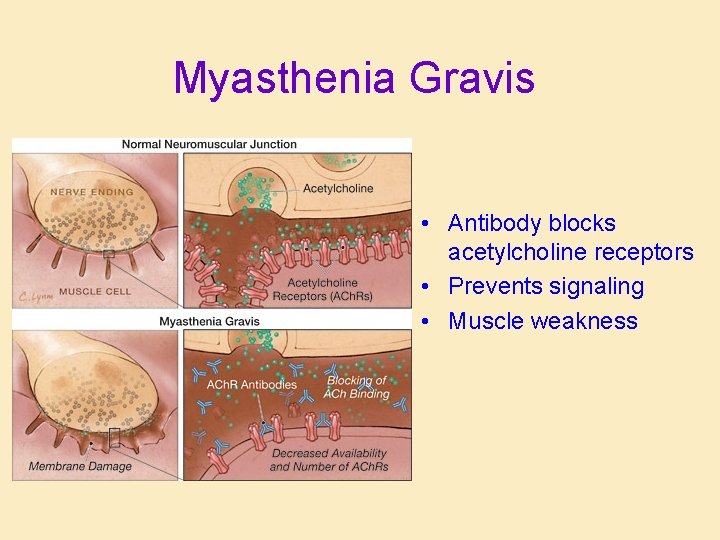
Myasthenia Gravis • Antibody blocks acetylcholine receptors • Prevents signaling • Muscle weakness
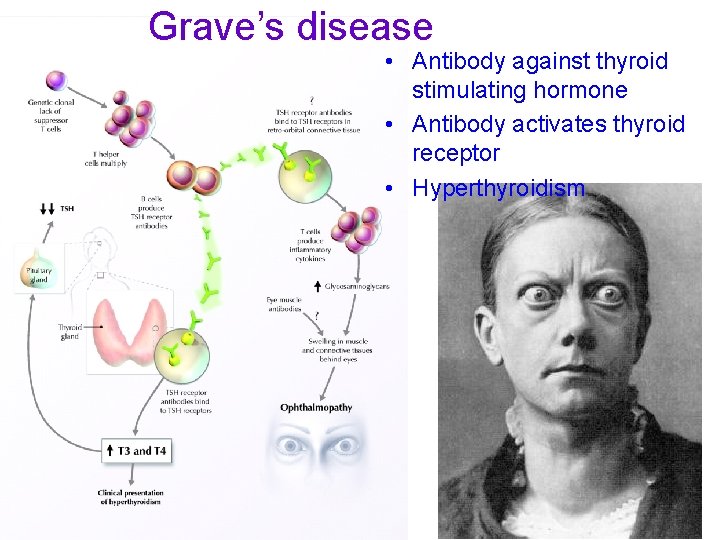
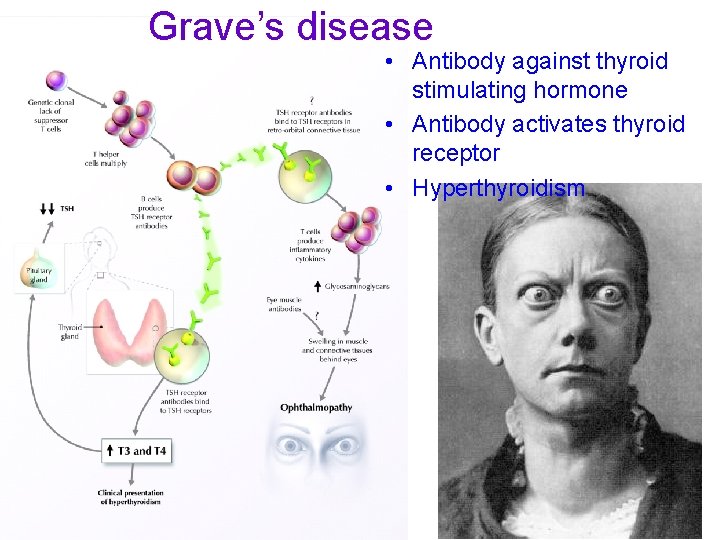
Grave’s disease • Antibody against thyroid stimulating hormone • Antibody activates thyroid receptor • Hyperthyroidism
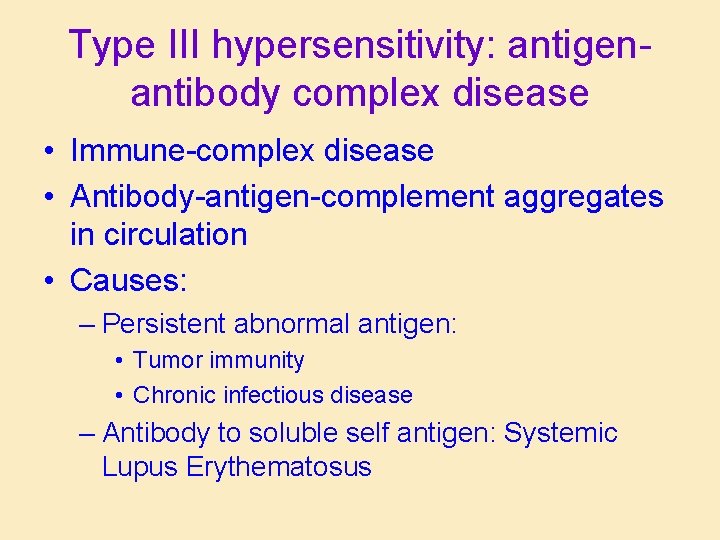
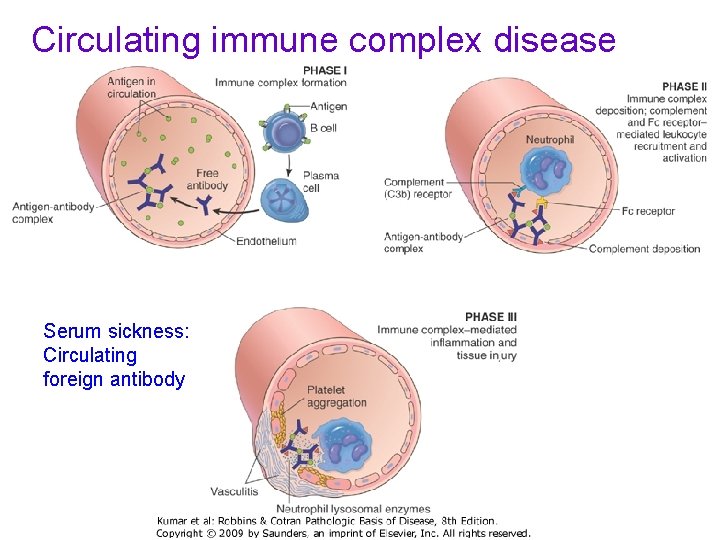
Type III hypersensitivity: antigenantibody complex disease • Immune-complex disease • Antibody-antigen-complement aggregates in circulation • Causes: – Persistent abnormal antigen: • Tumor immunity • Chronic infectious disease – Antibody to soluble self antigen: Systemic Lupus Erythematosus
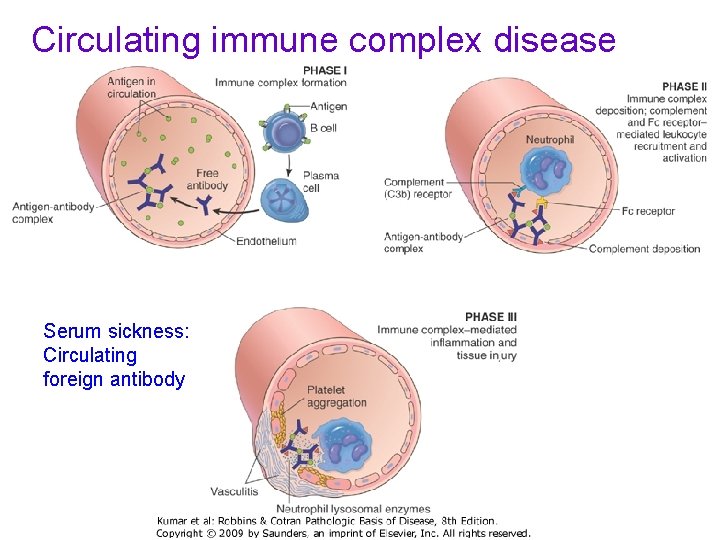
Circulating immune complex disease Serum sickness: Circulating foreign antibody
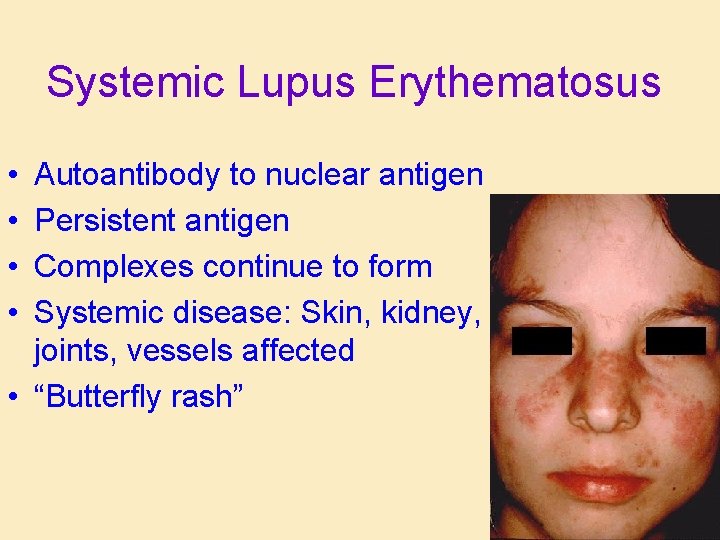
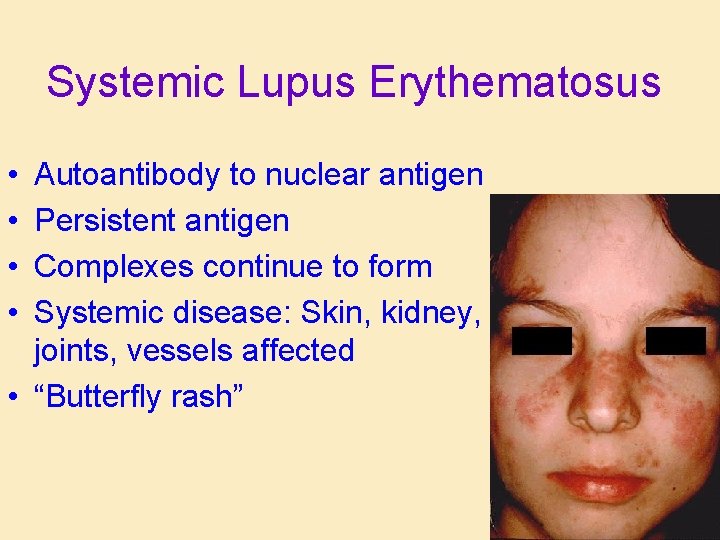
Systemic Lupus Erythematosus • • Autoantibody to nuclear antigen Persistent antigen Complexes continue to form Systemic disease: Skin, kidney, joints, vessels affected • “Butterfly rash”
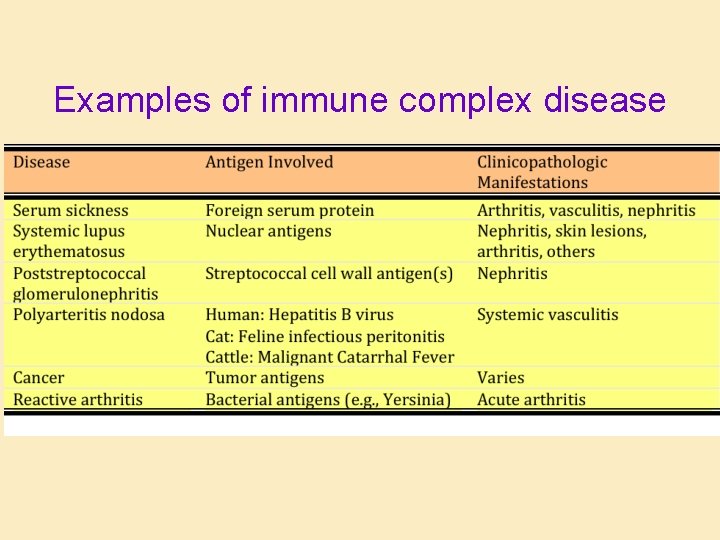
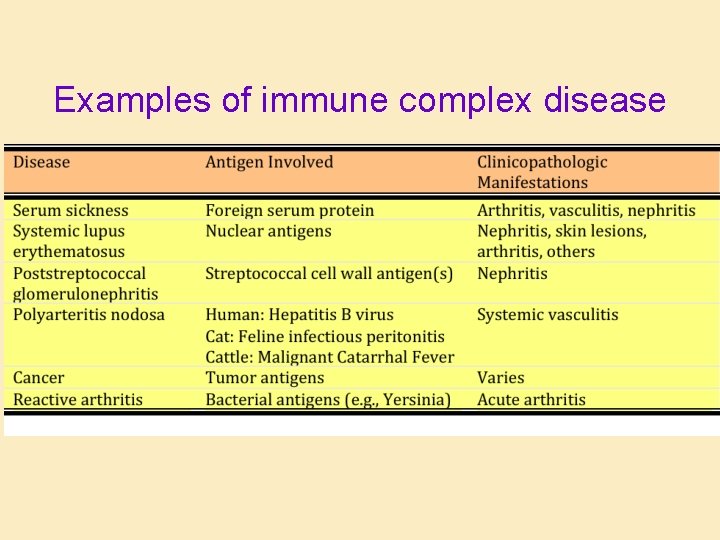
Examples of immune complex disease
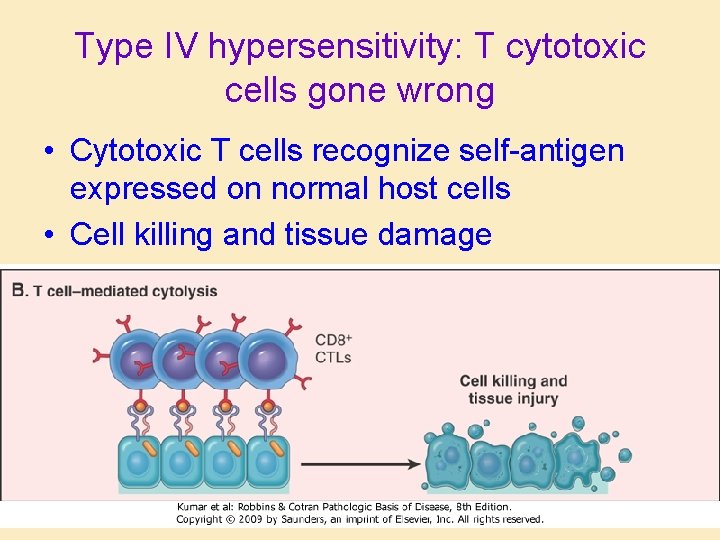
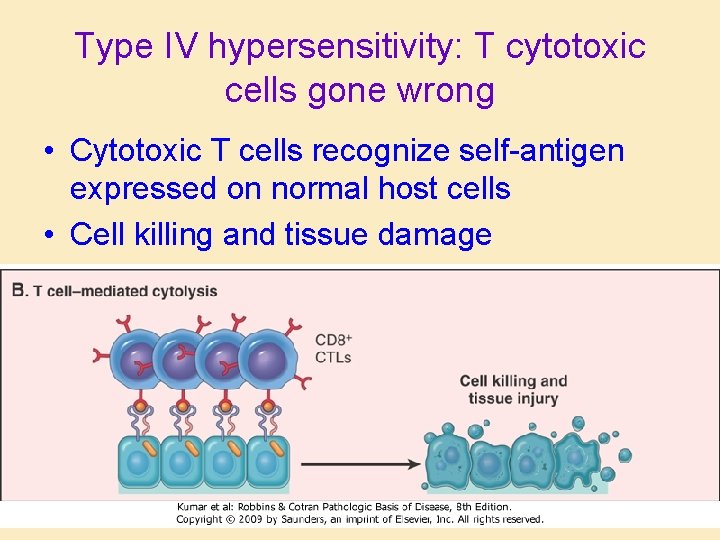
Type IV hypersensitivity: T cytotoxic cells gone wrong • Cytotoxic T cells recognize self-antigen expressed on normal host cells • Cell killing and tissue damage
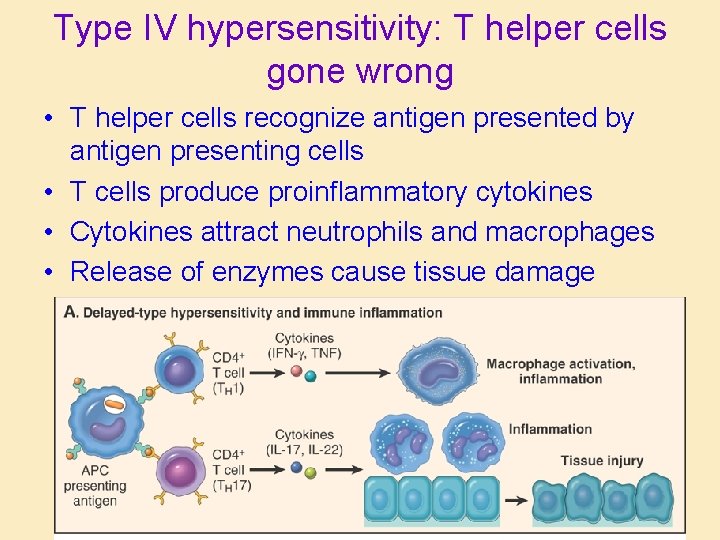
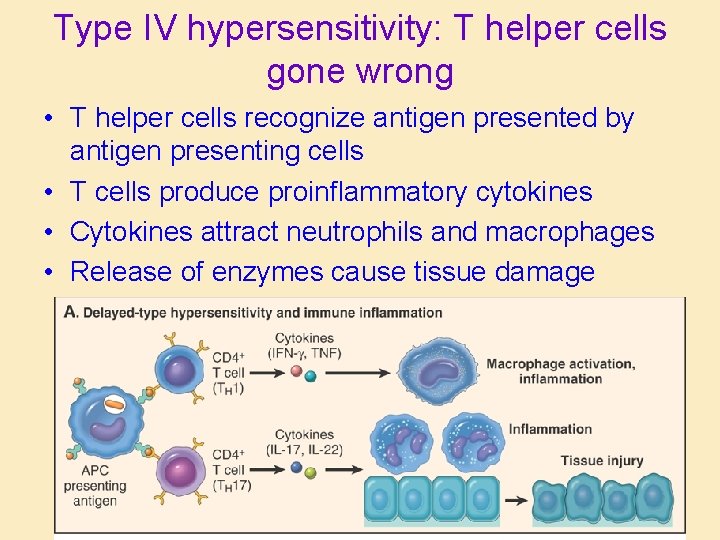
Type IV hypersensitivity: T helper cells gone wrong • T helper cells recognize antigen presented by antigen presenting cells • T cells produce proinflammatory cytokines • Cytokines attract neutrophils and macrophages • Release of enzymes cause tissue damage
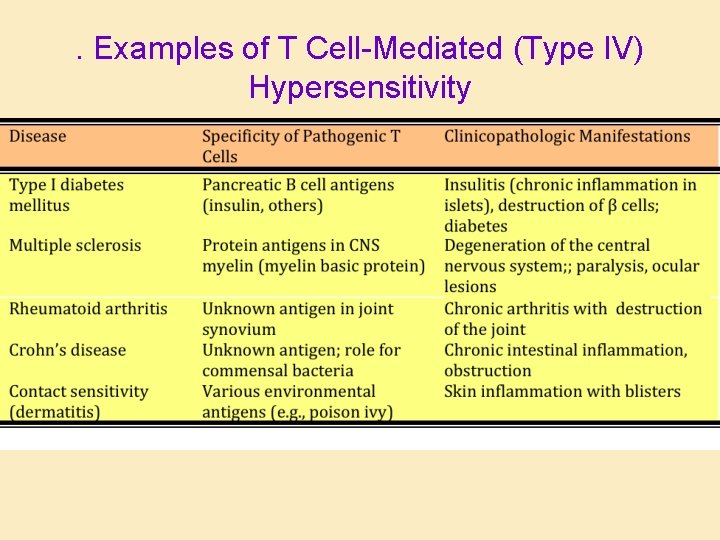
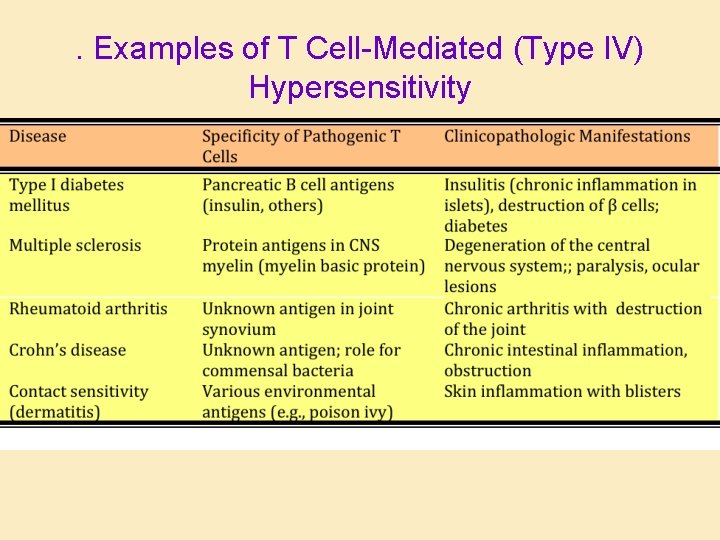
. Examples of T Cell-Mediated (Type IV) Hypersensitivity
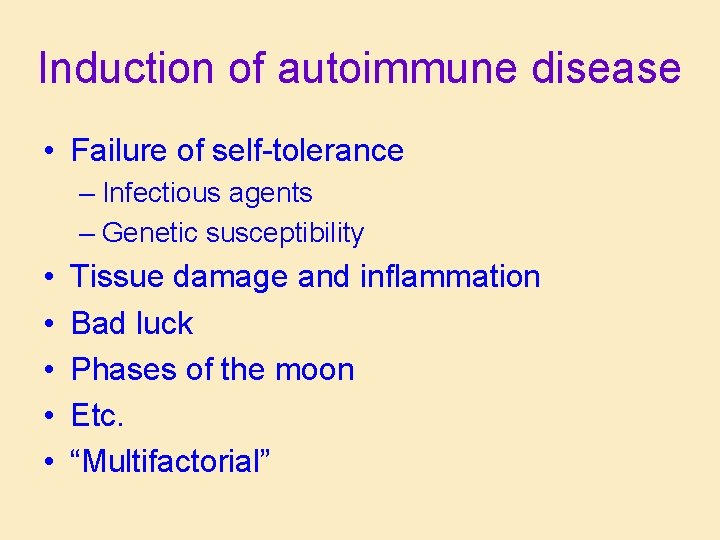
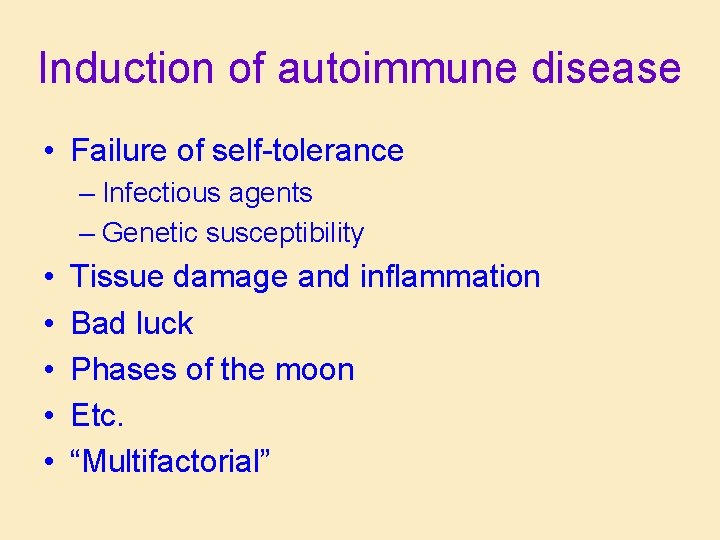
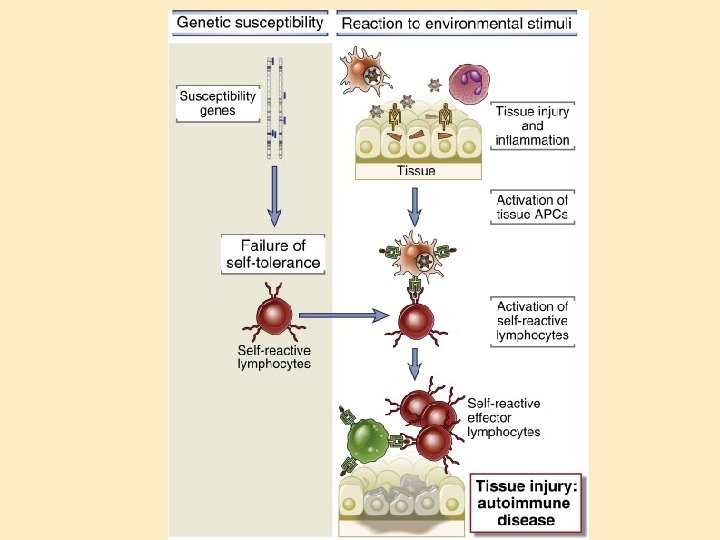
Induction of autoimmune disease • Failure of self-tolerance – Infectious agents – Genetic susceptibility • • • Tissue damage and inflammation Bad luck Phases of the moon Etc. “Multifactorial”
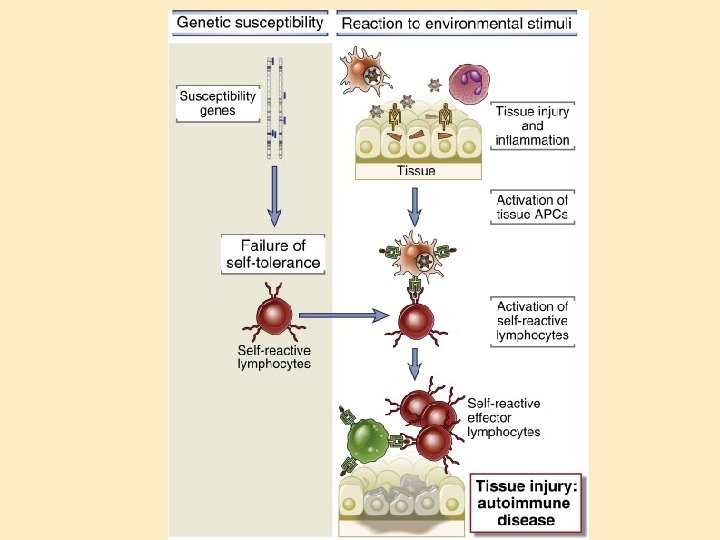
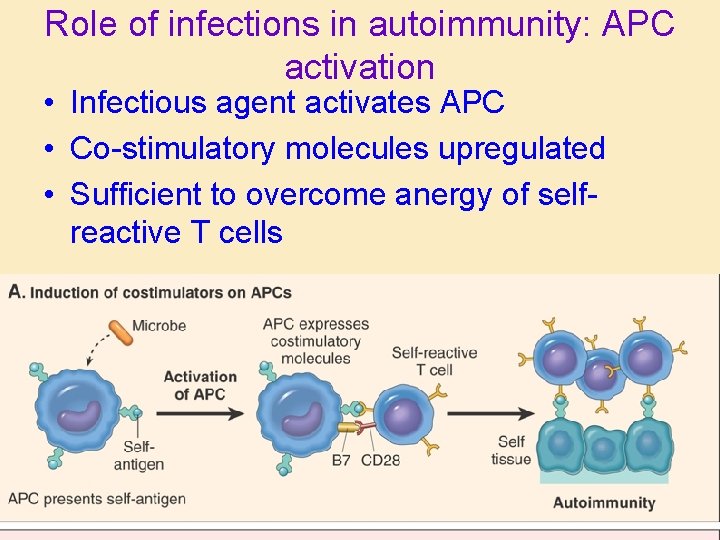
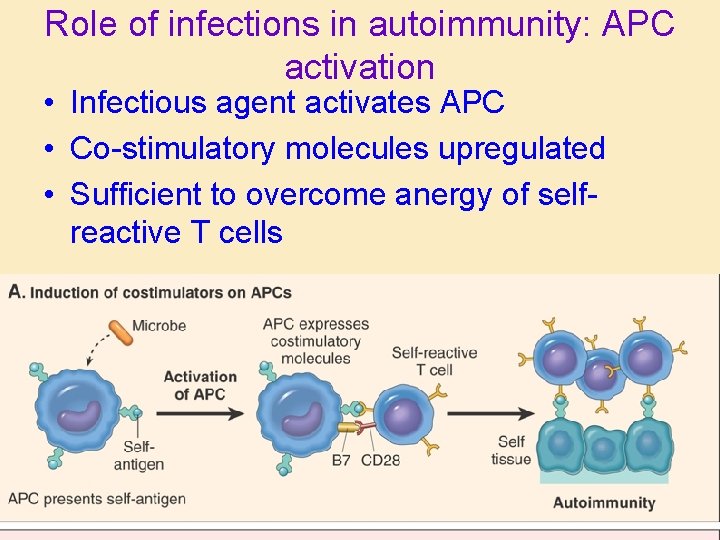
Role of infections in autoimmunity: APC activation • Infectious agent activates APC • Co-stimulatory molecules upregulated • Sufficient to overcome anergy of selfreactive T cells
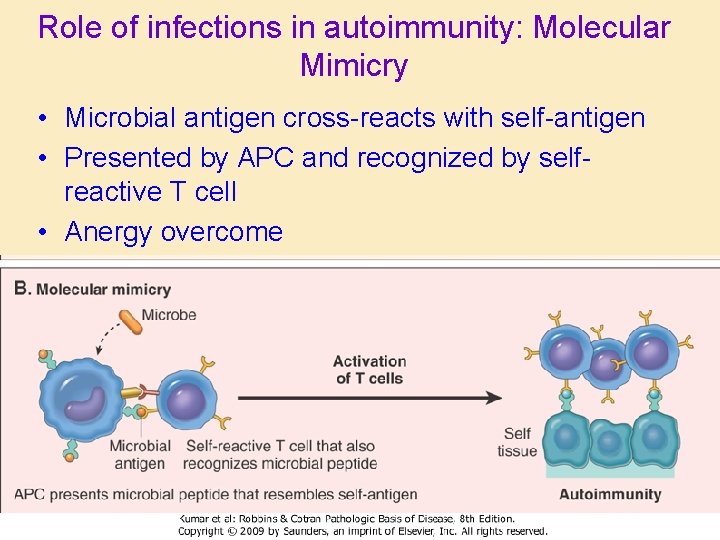
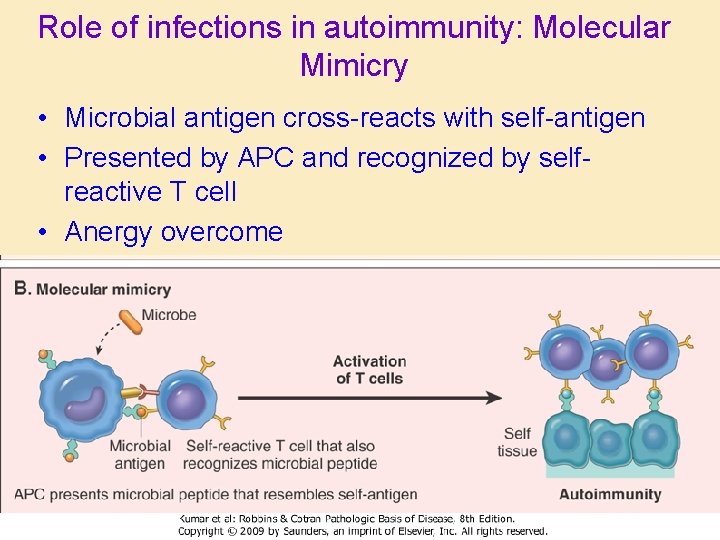
Role of infections in autoimmunity: Molecular Mimicry • Microbial antigen cross-reacts with self-antigen • Presented by APC and recognized by selfreactive T cell • Anergy overcome
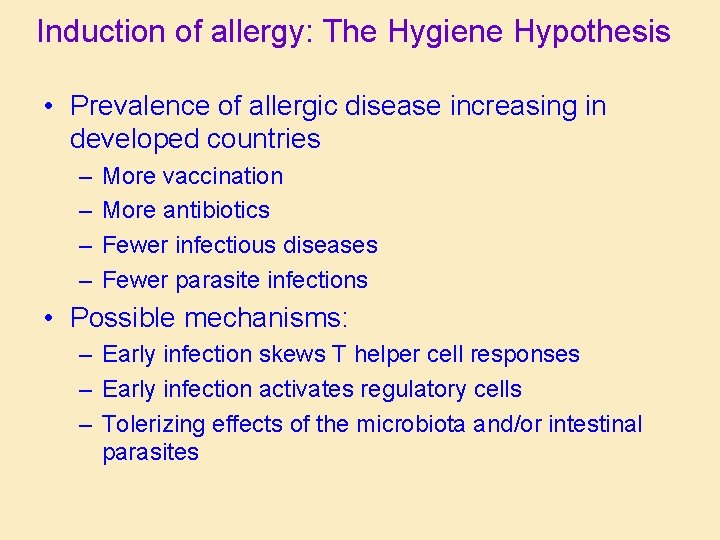
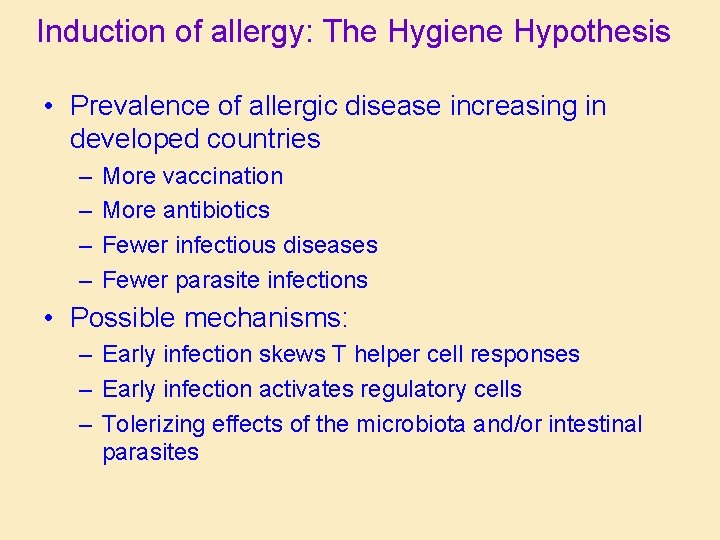
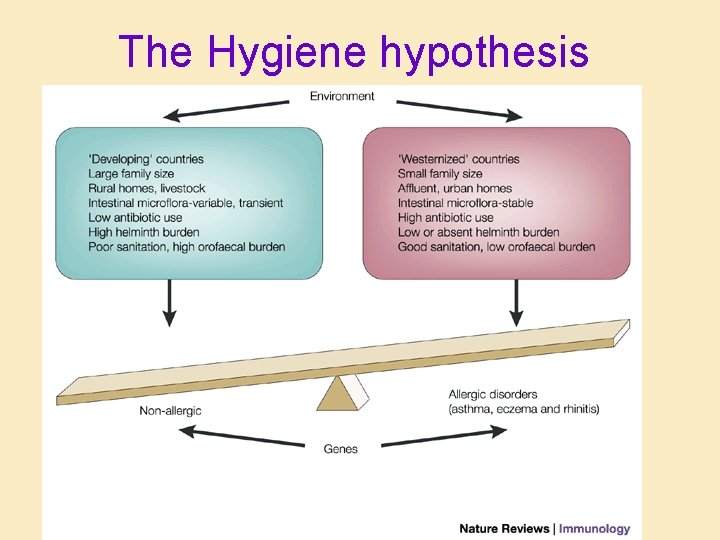
Induction of allergy: The Hygiene Hypothesis • Prevalence of allergic disease increasing in developed countries – – More vaccination More antibiotics Fewer infectious diseases Fewer parasite infections • Possible mechanisms: – Early infection skews T helper cell responses – Early infection activates regulatory cells – Tolerizing effects of the microbiota and/or intestinal parasites
A few diseases associated with “improved hygiene” • Atopic dermatitis • Asthma • Inflammatory bowel diseases • Autoimmune arthritis • Type 1 Diabetes mellitus • • Multiple sclerosis Helicobacter pylori Neoplasia Increased susceptibility to infectious agents
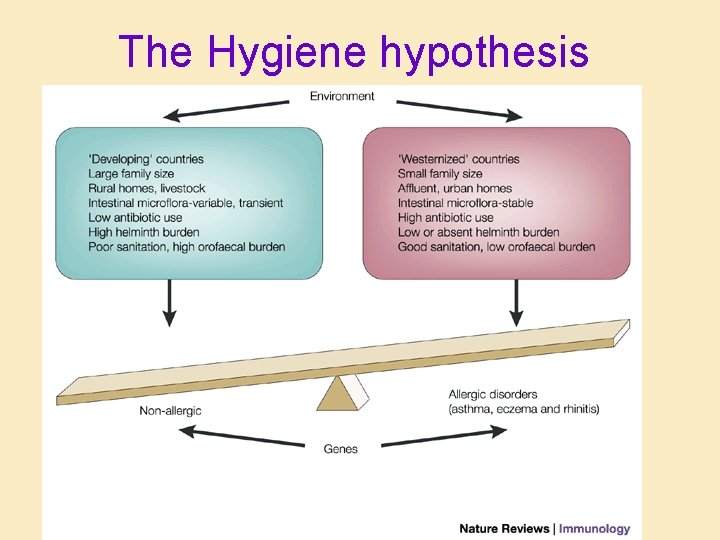
The Hygiene hypothesis

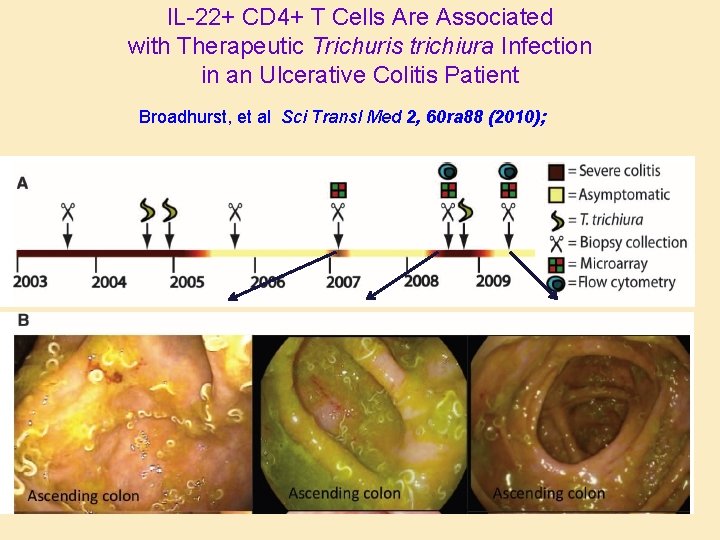
Parasitic helminths and therapy • Inverse correlation between allergy and parasite burden • Increase in allergic disease associated with anthelmintic treatment • Parasites for treatment of: – Inflammatory bowel disease – Autoimmune arthritis – Multiple sclerosis
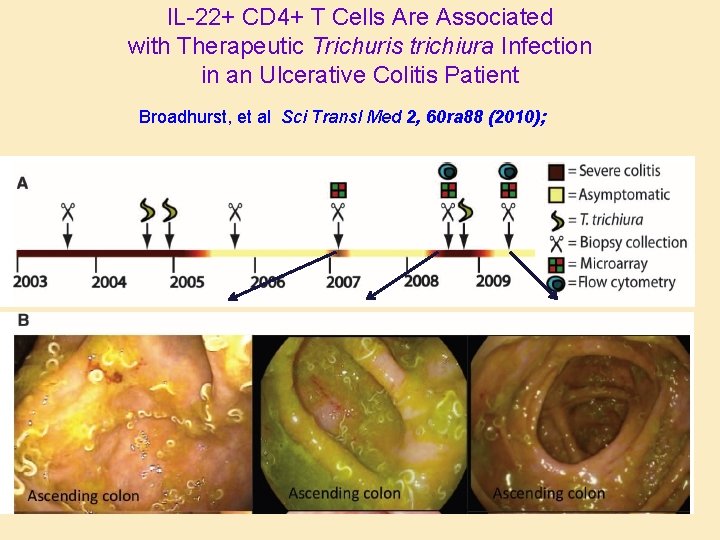
IL-22+ CD 4+ T Cells Are Associated with Therapeutic Trichuris trichiura Infection in an Ulcerative Colitis Patient Broadhurst, et al Sci Transl Med 2, 60 ra 88 (2010); Gross photo alert
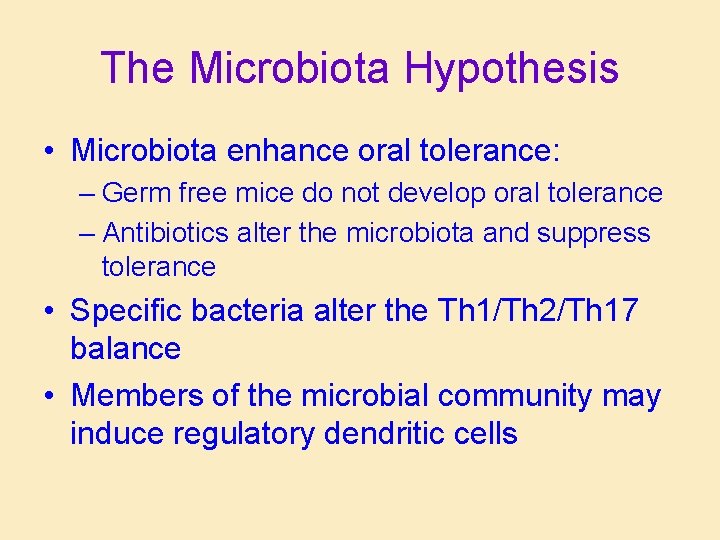
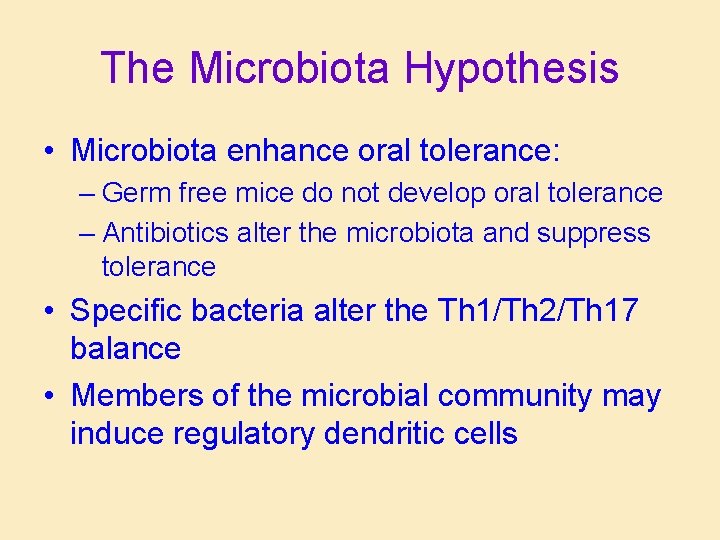
The Microbiota Hypothesis • Microbiota enhance oral tolerance: – Germ free mice do not develop oral tolerance – Antibiotics alter the microbiota and suppress tolerance • Specific bacteria alter the Th 1/Th 2/Th 17 balance • Members of the microbial community may induce regulatory dendritic cells
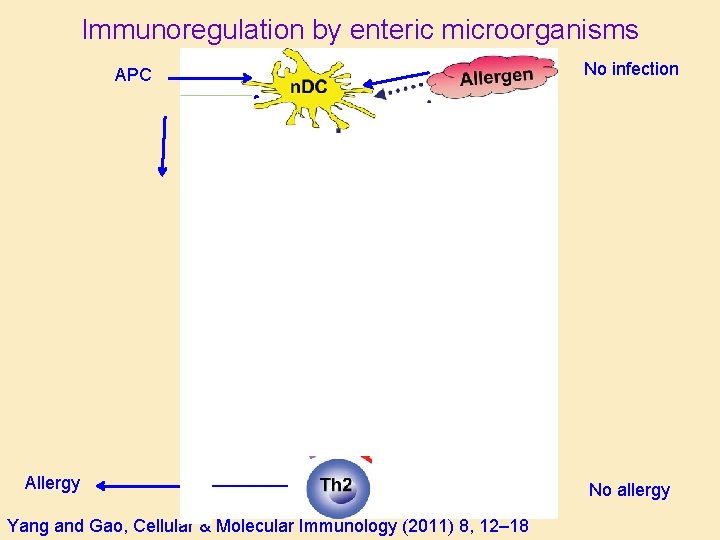
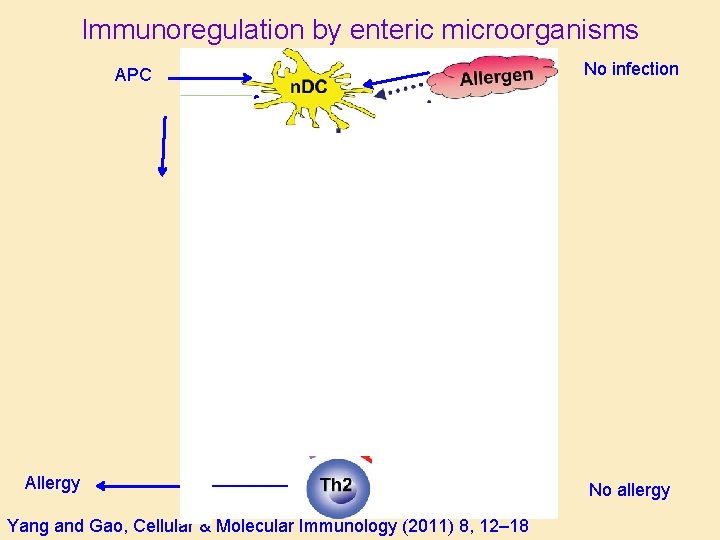
Immunoregulation by enteric microorganisms APC Allergy Yang and Gao, Cellular & Molecular Immunology (2011) 8, 12– 18 No infection No allergy
 A subsequent
A subsequent Difference between acquired immunity and innate immunity
Difference between acquired immunity and innate immunity Plastic surgery gone wrong
Plastic surgery gone wrong Something must have gone wrong
Something must have gone wrong Plexr gone wrong
Plexr gone wrong Botox injection dubai
Botox injection dubai You put the wrong emphasis on the wrong syllable
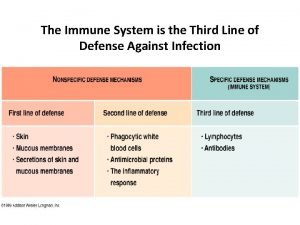
You put the wrong emphasis on the wrong syllable What is the third line of defense in the immune system
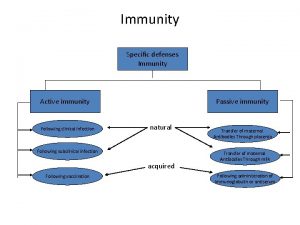
What is the third line of defense in the immune system Flow chart
Flow chart Third line of defense immune system
Third line of defense immune system Innate immunity first line of defense
Innate immunity first line of defense Chapter 35 immune system and disease
Chapter 35 immune system and disease 1st 2nd and 3rd line of defense immune system
1st 2nd and 3rd line of defense immune system Ap bio immune system
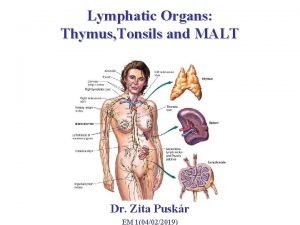
Ap bio immune system Lesson 12.1 lymphatic ducts and vessels
Lesson 12.1 lymphatic ducts and vessels Lesson 12 blood and immune system
Lesson 12 blood and immune system Immune system lymph nodes
Immune system lymph nodes Immunity assignment slideshare
Immunity assignment slideshare Overreactions of the immune system
Overreactions of the immune system Lymphatic vs immune system
Lymphatic vs immune system Phagocitize
Phagocitize Defination of immune system
Defination of immune system 3 lines of defence immune system
3 lines of defence immune system The main function of immune system
The main function of immune system Tonsil histology
Tonsil histology Thymus
Thymus Immune complex
Immune complex Thalassemia facies
Thalassemia facies 1what's the purpose of the body's immune system?
1what's the purpose of the body's immune system? Chapter 13 lymphatic system and immunity
Chapter 13 lymphatic system and immunity Chapter 16 lymphatic system and immunity
Chapter 16 lymphatic system and immunity Lymph is composed of
Lymph is composed of Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Capnia medical term
Capnia medical term Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Female reproductive system diseases
Female reproductive system diseases Spalding sign
Spalding sign Difference between innate and learned behavior
Difference between innate and learned behavior Chapter 55 care of the patient with an immune disorder
Chapter 55 care of the patient with an immune disorder Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer Immune checkpoint inhibitors mechanism of action
Immune checkpoint inhibitors mechanism of action