Wrong Patient Wrong Procedure Wrong Site Preventing Wrong
- Slides: 41
Wrong Patient, Wrong Procedure, Wrong Site: Preventing Wrong Surgery
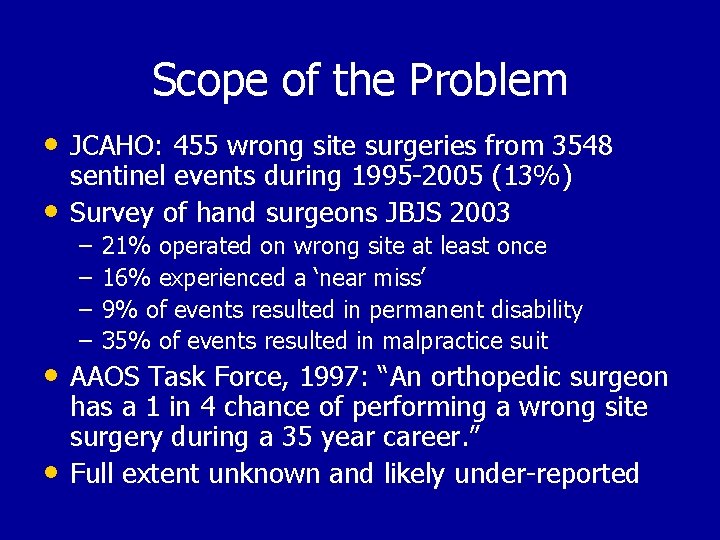
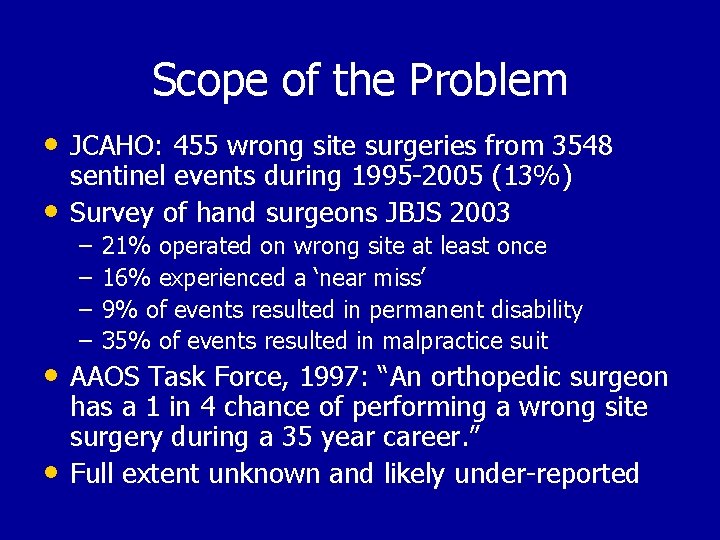
Scope of the Problem • JCAHO: 455 wrong site surgeries from 3548 • sentinel events during 1995 -2005 (13%) Survey of hand surgeons JBJS 2003 – – 21% operated on wrong site at least once 16% experienced a ‘near miss’ 9% of events resulted in permanent disability 35% of events resulted in malpractice suit • AAOS Task Force, 1997: “An orthopedic surgeon • has a 1 in 4 chance of performing a wrong site surgery during a 35 year career. ” Full extent unknown and likely under-reported
Disclosure of Medical Errors: Challenges for the Physician • Loss of patient’s trust • Effect on reputation • Fear of litigation • Difficulties communicating about the error with the patient
Mistakes “Mistakes are at the very base of human thought, embedded there, feeding the structure like root nodules. If we were not provided with the knack of being wrong, we could never get anything useful done. We are built to make mistakes, coded for error … The capacity to leap across mountains of information and lightly on the wrong side represents the highest of human endowments. ” Lewis Thomas MD 1974
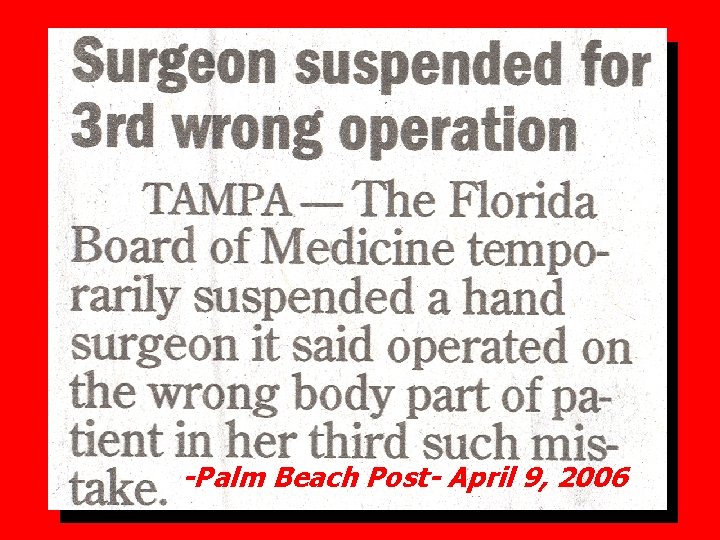
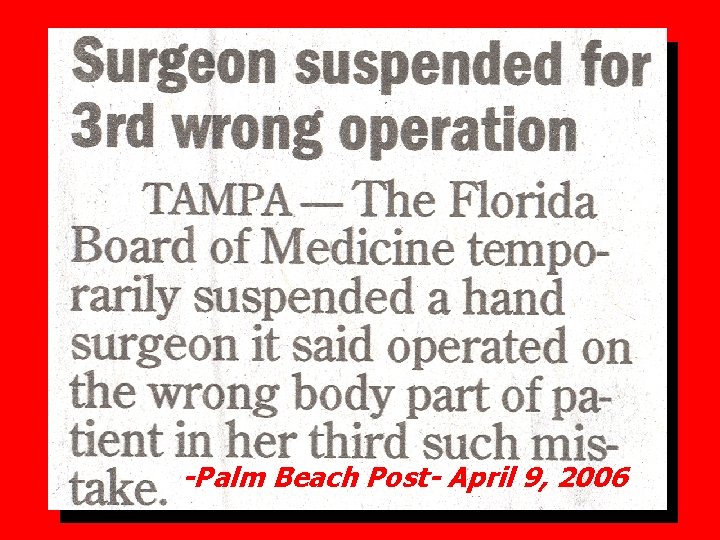
-Palm Beach Post- April 9, 2006
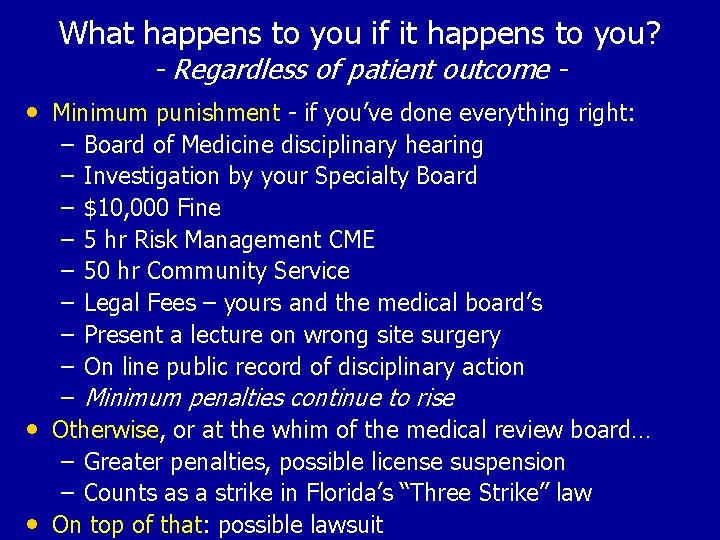
What happens to you if it happens to you? - Regardless of patient outcome - • Minimum punishment - if you’ve done everything right: – Board of Medicine disciplinary hearing – Investigation by your Specialty Board – $10, 000 Fine – 5 hr Risk Management CME – 50 hr Community Service – Legal Fees – yours and the medical board’s – Present a lecture on wrong site surgery – On line public record of disciplinary action – Minimum penalties continue to rise • Otherwise, or at the whim of the medical review board… – Greater penalties, possible license suspension – Counts as a strike in Florida’s “Three Strike” law • On top of that: possible lawsuit
Definition of Wrong Surgery • Wrong Site • Wrong Patient • Wrong Procedure • JCAHO “Sentinel Event”
The Joint Commission’s Sentinel Event Policy • Established in 1996 with these goals: – To have a positive impact in improving care – To focus attention on underlying causes and risk reduction – To increase the general knowledge about sentinel events, their causes and prevention – To maintain public confidence in the accreditation process
Sentinel Event Unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof. Serious injury specifically includes loss of limb or function. The phrase, "or the risk thereof" includes any process variation for which a recurrence would carry a significant chance of a serious adverse outcome. Called "sentinel" because they mandate immediate investigation and response (Root Cause Analysis).
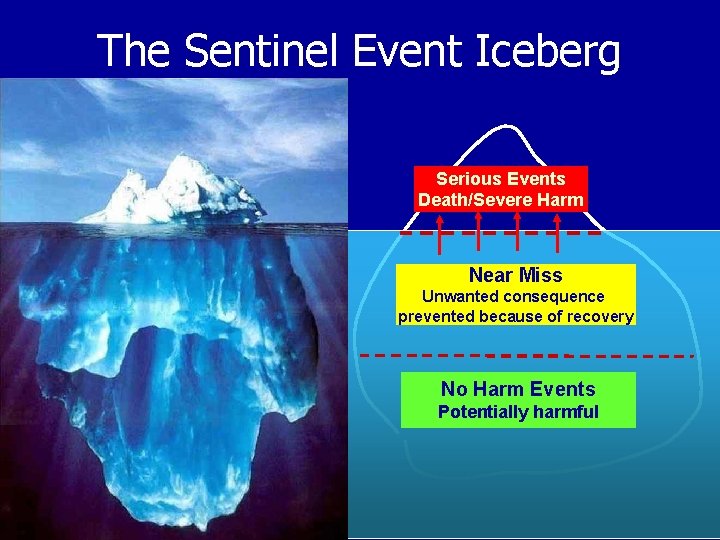
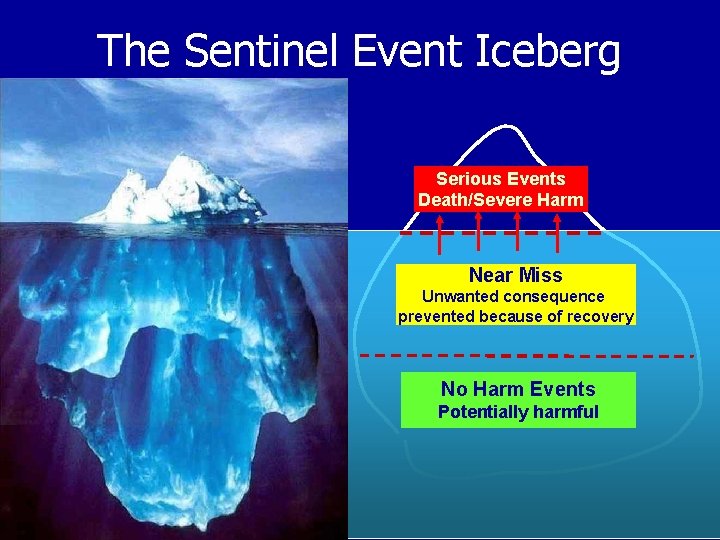
The Sentinel Event Iceberg Serious Events Death/Severe Harm Near Miss Unwanted consequence prevented because of recovery No Harm Events Potentially harmful
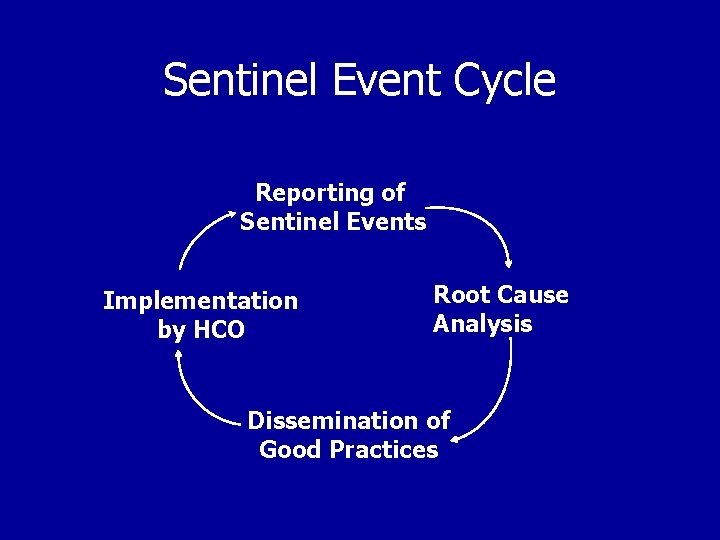
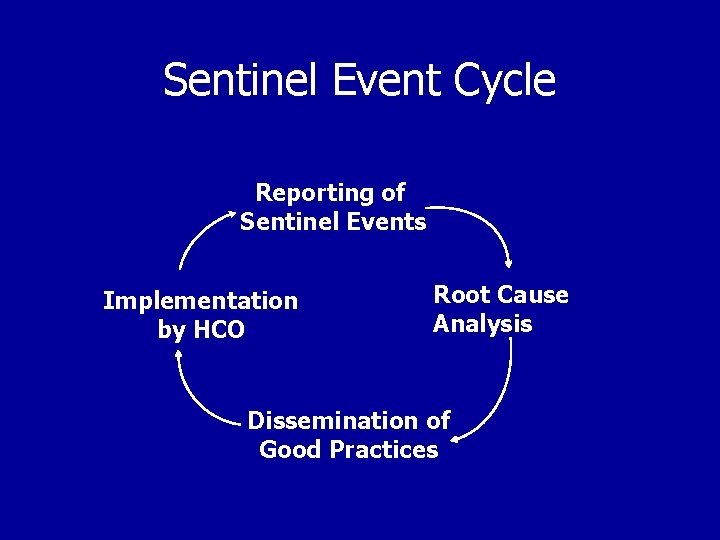
Sentinel Event Cycle Reporting of Sentinel Events Implementation by HCO Root Cause Analysis Dissemination of Good Practices
2005 JCAHO Sentinel Events Generic Event which resulted in unanticipated patient death or major permanent loss of function (unrelated to the natural course of the patient's illness or underlying condition)
2005 JCAHO Sentinel Events Specific An the event which involves one of the following: • Suicide of an inpatient or < 72 hr post discharge • Unanticipated newborn death • Infant abduction or discharge to wrong family • Rape or Abduction • Hemolytic or major transfusion reaction • Surgery on wrong patient or wrong body part • Retained surgical foreign object • Severe neonatal hyperbilirubinemia • Excessive, unplanned or wrong site radiation exposure
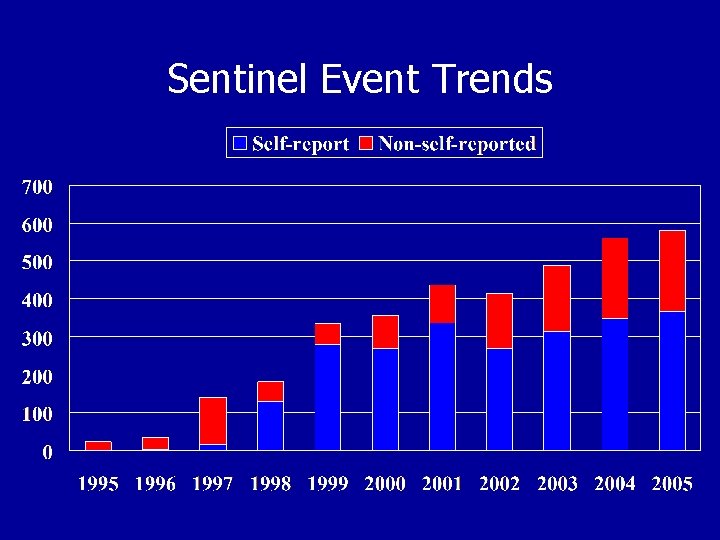
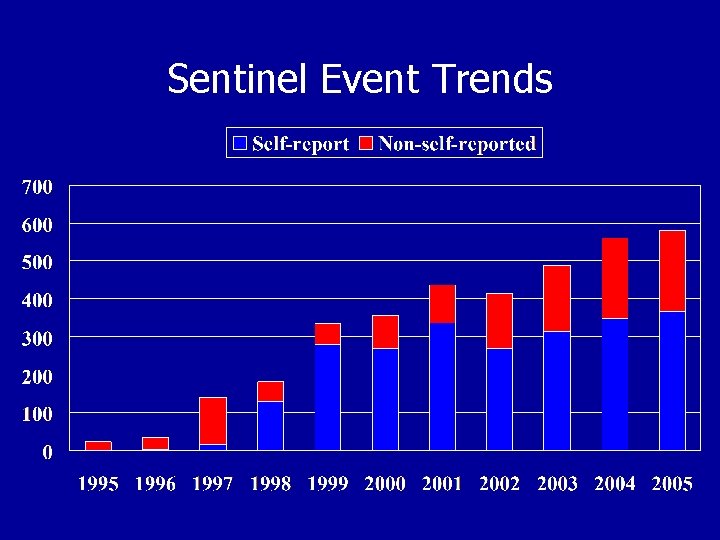
Sentinel Event Trends
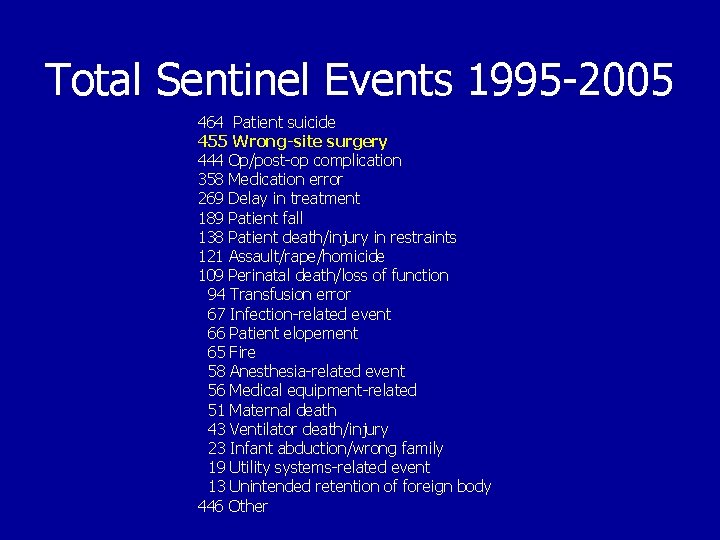
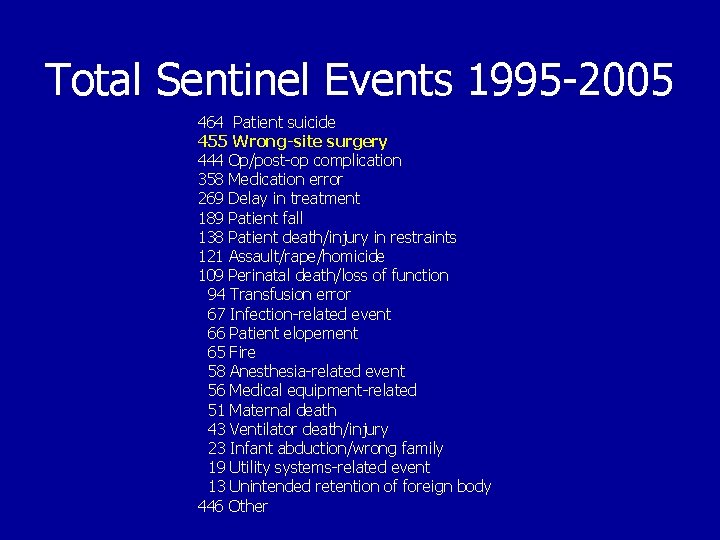
Total Sentinel Events 1995 -2005 464 Patient suicide 455 Wrong-site surgery 444 Op/post-op complication 358 Medication error 269 Delay in treatment 189 Patient fall 138 Patient death/injury in restraints 121 Assault/rape/homicide 109 Perinatal death/loss of function 94 Transfusion error 67 Infection-related event 66 Patient elopement 65 Fire 58 Anesthesia-related event 56 Medical equipment-related 51 Maternal death 43 Ventilator death/injury 23 Infant abduction/wrong family 19 Utility systems-related event 13 Unintended retention of foreign body 446 Other
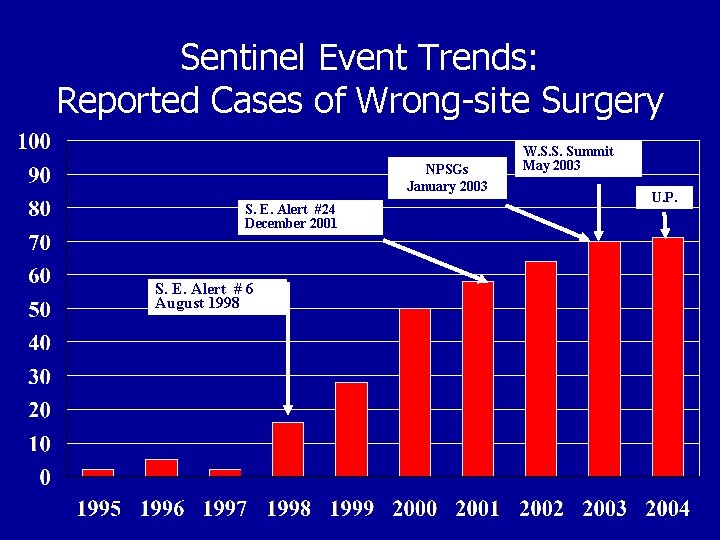
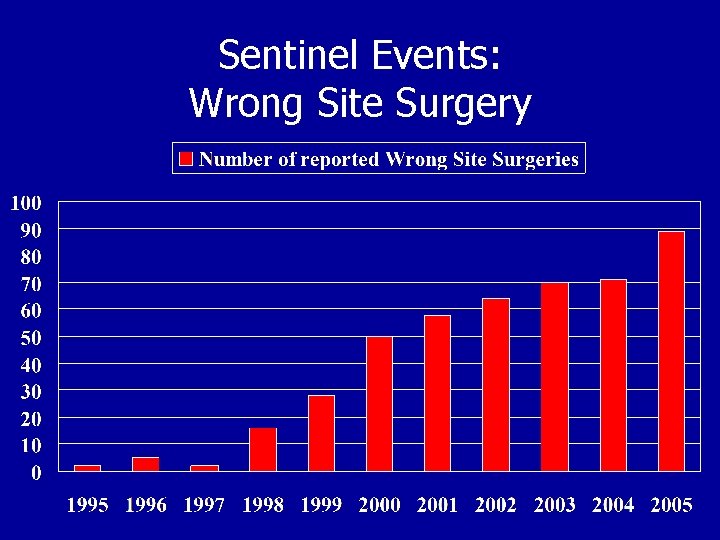
Sentinel Event Trends: Reported Cases of Wrong-site Surgery NPSGs January 2003 S. E. Alert #24 December 2001 S. E. Alert # 6 August 1998 W. S. S. Summit May 2003 U. P.
Organized Efforts to Reduce Wrong Site Surgery • Statement on ensuring correct patient, correct site, and correct procedure surgery Bulletin of the American College of Surgeons • • Volume 87, Number 12, December 2002. AAOS launches 2003 public service ad campaign AAOS Bulletin February 2003, an American Academy of Orthopaedic Surgeons “Sign Your Site” initiative. Despite these efforts, the number of wrong site surgeries reported to the Joint Commission’s database increased. By 2003, the Joint Commission was receiving 5 to 8 reports of wrong site surgery every month.
2003 Wrong-Site Surgery Summit Attended by leaders of all major professional associations that relate to the surgical process Results: Consensus on the following: • Wrong site, wrong patient, wrong procedure surgery is a significant, continuing problem • A System Analysis approach should be applied to the problem • A “Universal Protocol” should be adopted
System Analysis • Errors are expected • Errors occur in a dynamic environment, not in isolation • Multiple Contributing Factors – The Domino Effect – The Swiss Cheese Model
The Facility’s System is both Problem and Solution Every system is perfectly designed to achieve exactly the results it gets. Badly designed health care systems and protocols are perfectly designed to harm patients by ensuring that the inevitable rate of human error results in untoward events.
Treat Medical Errors as Systems Problems System failures - not individual human failures - are to blame. Naming the error, shaming & blaming individuals has not reduced errors. Analyze errors to improve the system to prevent the inevitable individual errors from evolving into a harmful patient event. The physician remains individually punishable for individual errors.
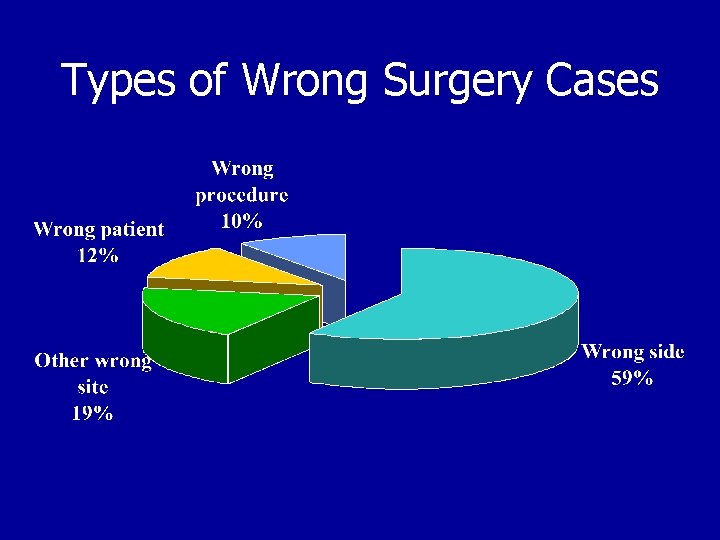
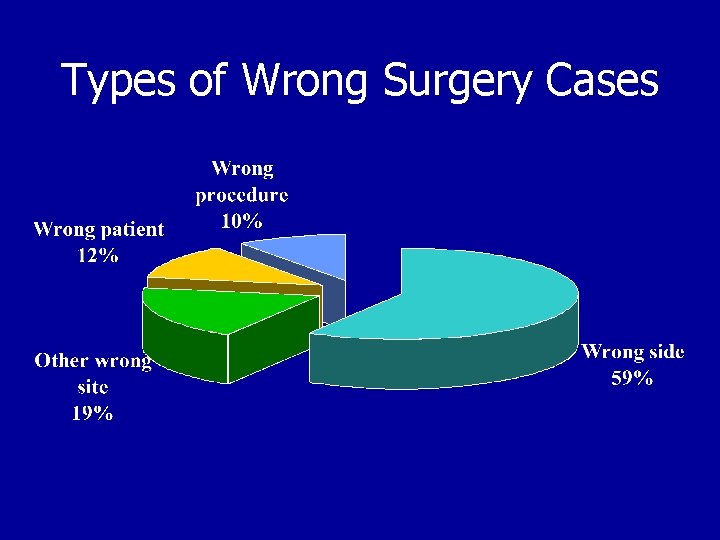
Types of Wrong Surgery Cases
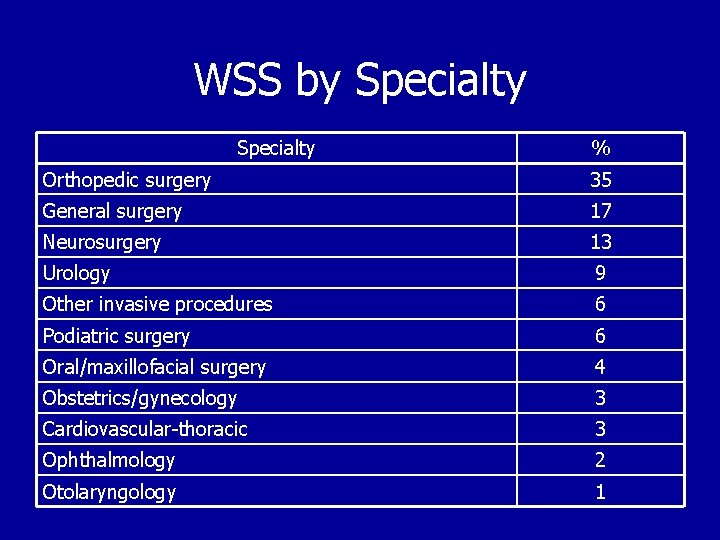
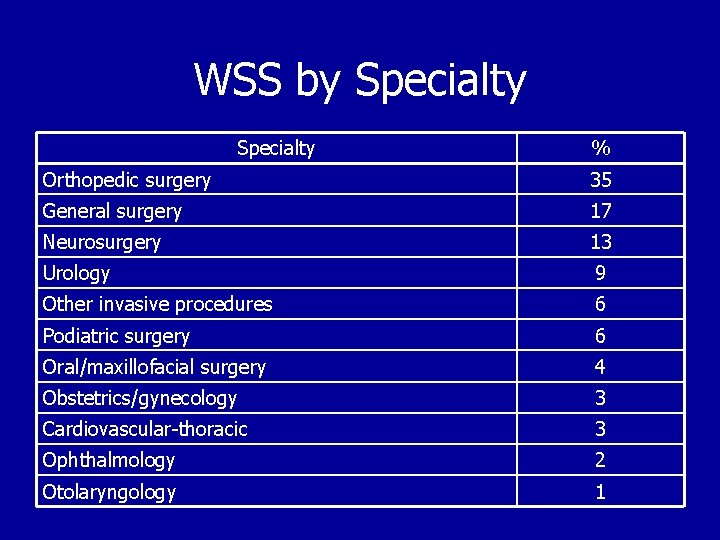
WSS by Specialty % Orthopedic surgery 35 General surgery 17 Neurosurgery 13 Urology 9 Other invasive procedures 6 Podiatric surgery 6 Oral/maxillofacial surgery 4 Obstetrics/gynecology 3 Cardiovascular-thoracic 3 Ophthalmology 2 Otolaryngology 1
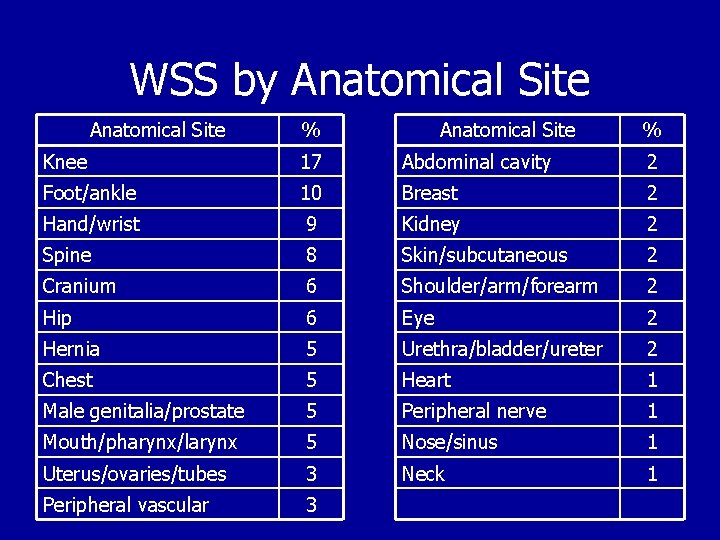
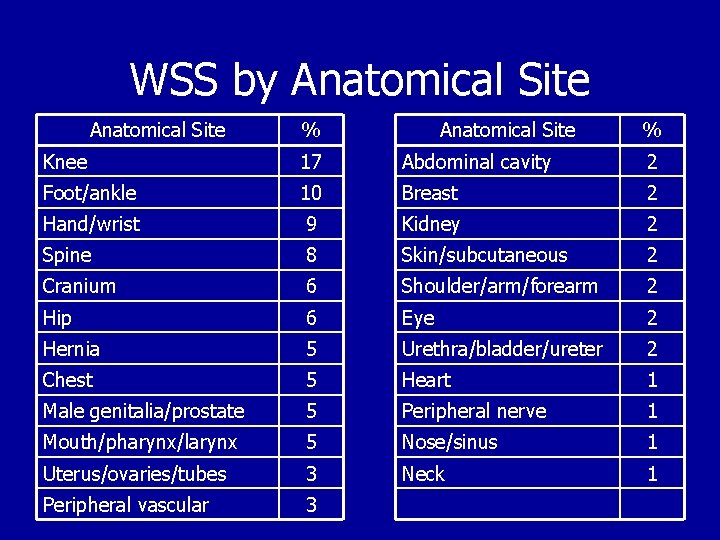
WSS by Anatomical Site % Knee 17 Abdominal cavity 2 Foot/ankle 10 Breast 2 Hand/wrist 9 Kidney 2 Spine 8 Skin/subcutaneous 2 Cranium 6 Shoulder/arm/forearm 2 Hip 6 Eye 2 Hernia 5 Urethra/bladder/ureter 2 Chest 5 Heart 1 Male genitalia/prostate 5 Peripheral nerve 1 Mouth/pharynx/larynx 5 Nose/sinus 1 Uterus/ovaries/tubes 3 Neck 1 Peripheral vascular 3
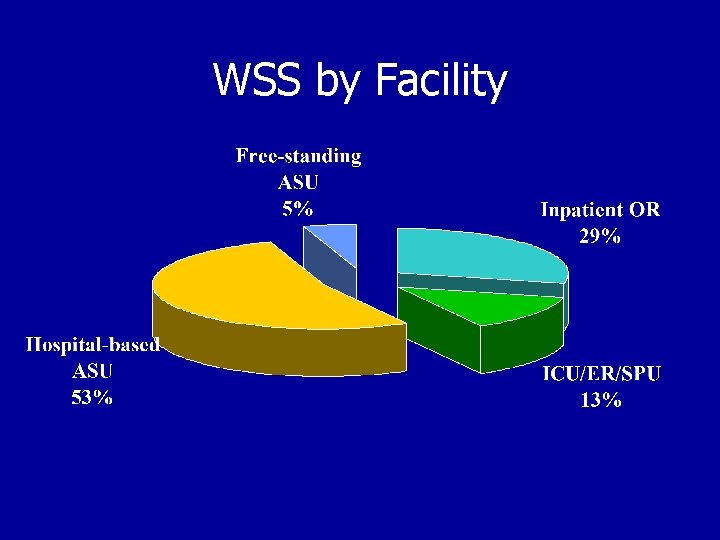
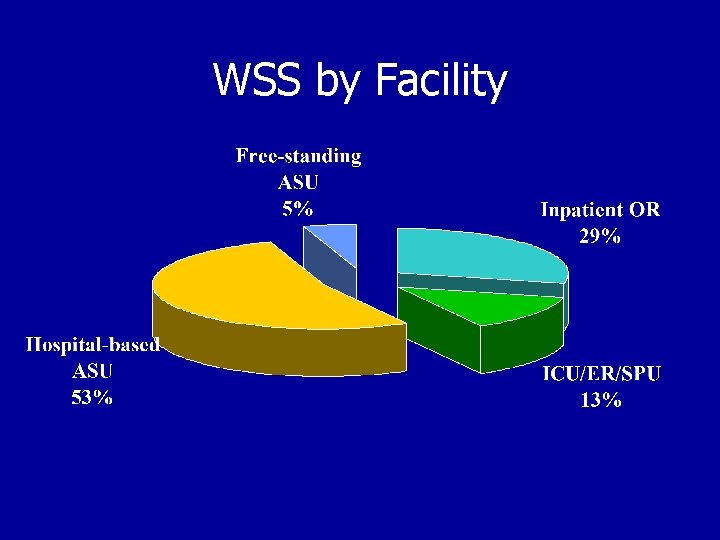
WSS by Facility
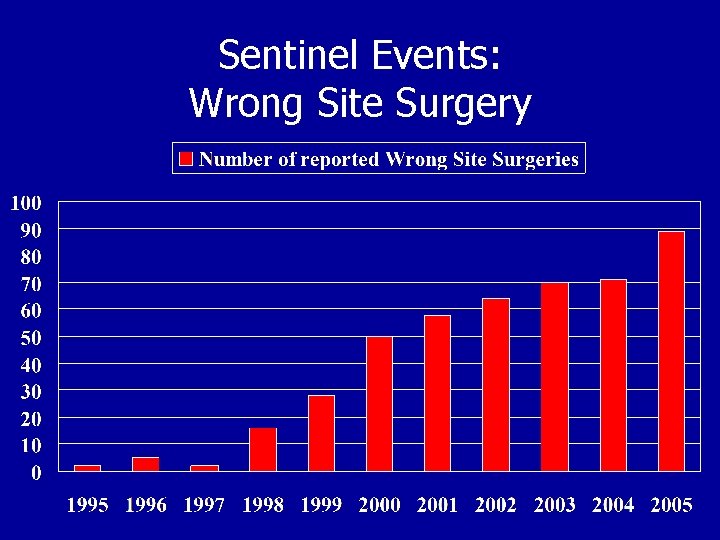
Sentinel Events: Wrong Site Surgery
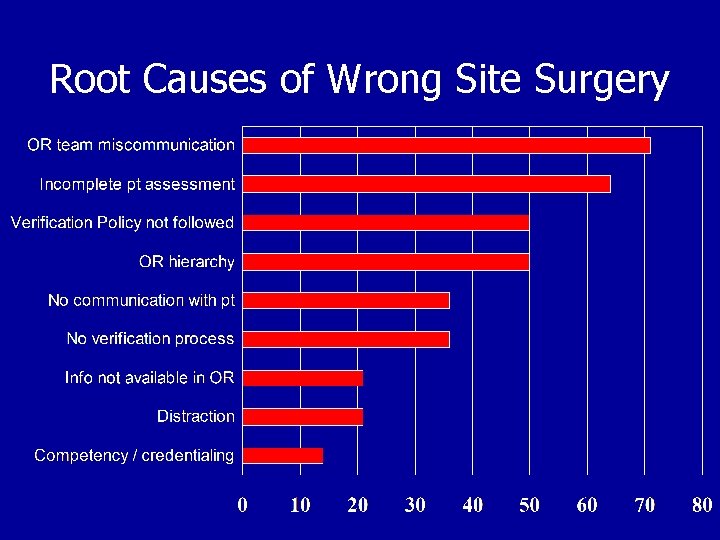
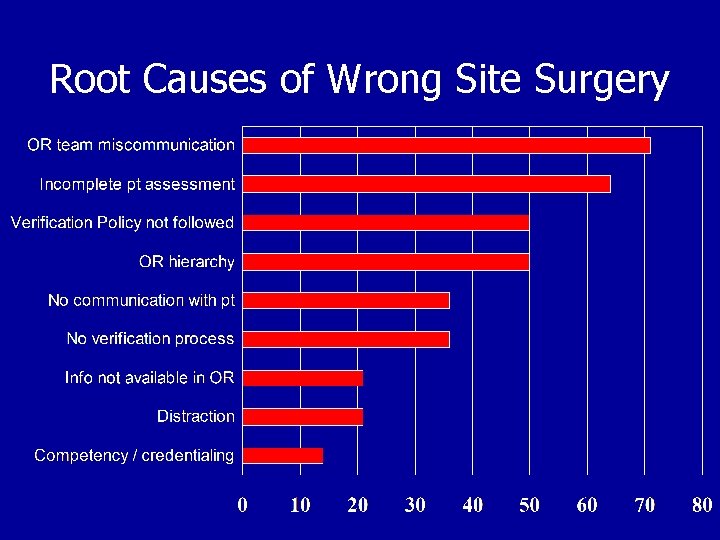
Root Causes of Wrong Site Surgery
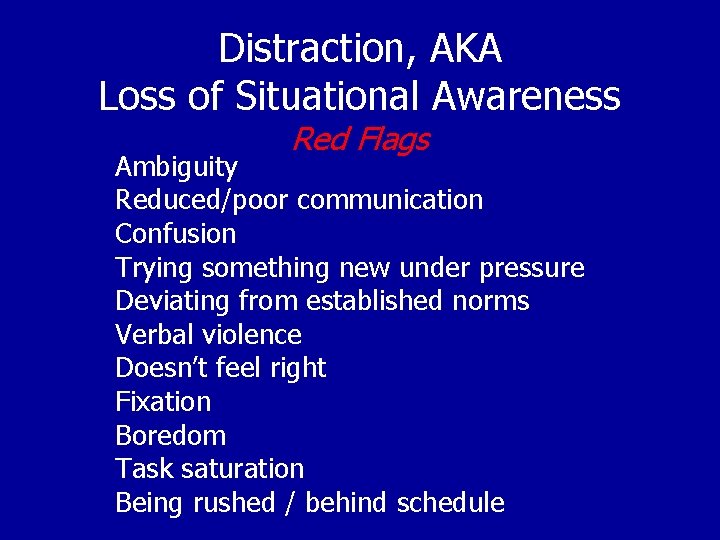
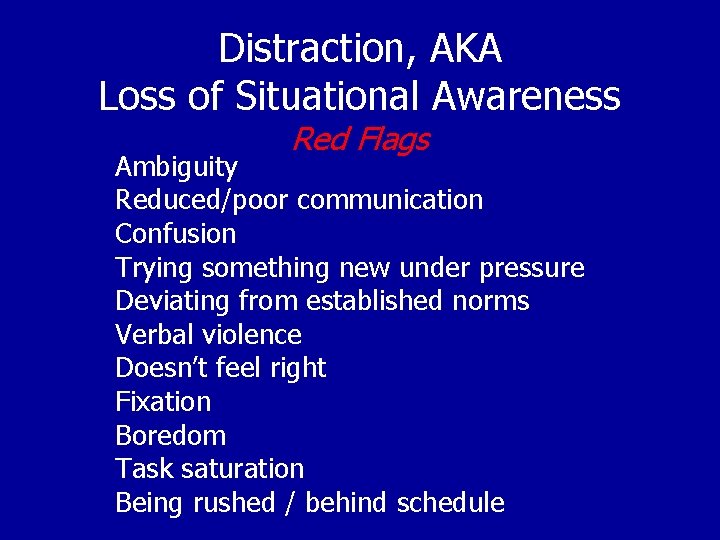
Distraction, AKA Loss of Situational Awareness Red Flags Ambiguity Reduced/poor communication Confusion Trying something new under pressure Deviating from established norms Verbal violence Doesn’t feel right Fixation Boredom Task saturation Being rushed / behind schedule
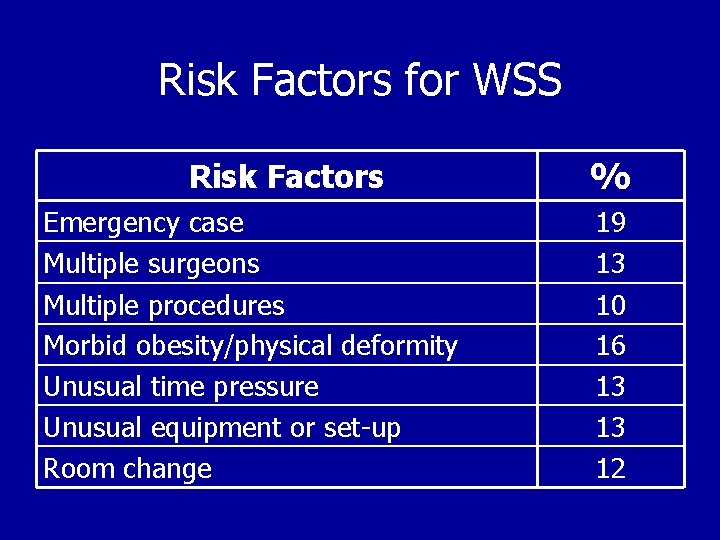
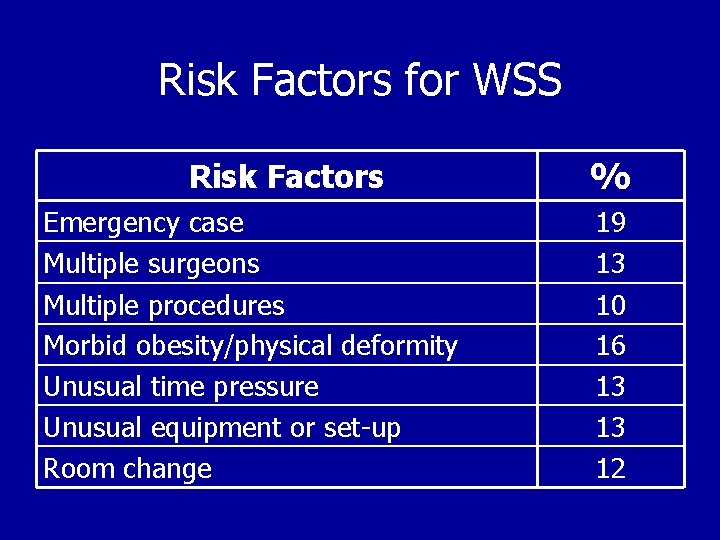
Risk Factors for WSS Risk Factors Emergency case Multiple surgeons Multiple procedures Morbid obesity/physical deformity Unusual time pressure Unusual equipment or set-up Room change % 19 13 10 16 13 13 12
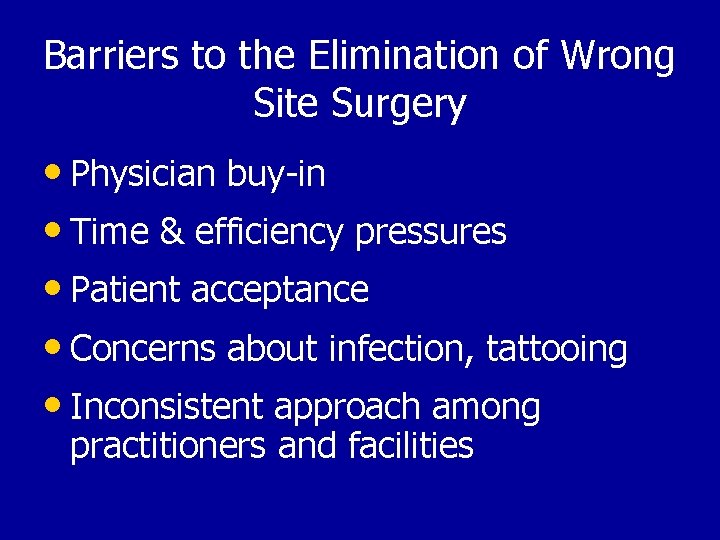
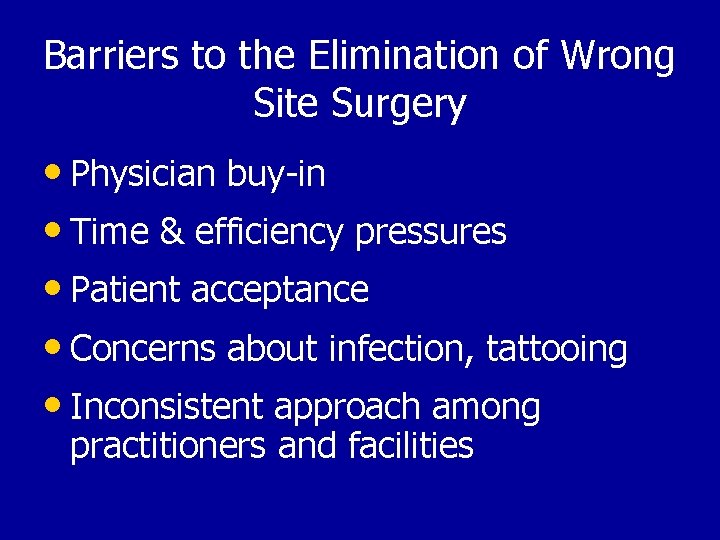
Barriers to the Elimination of Wrong Site Surgery • Physician buy-in • Time & efficiency pressures • Patient acceptance • Concerns about infection, tattooing • Inconsistent approach among practitioners and facilities
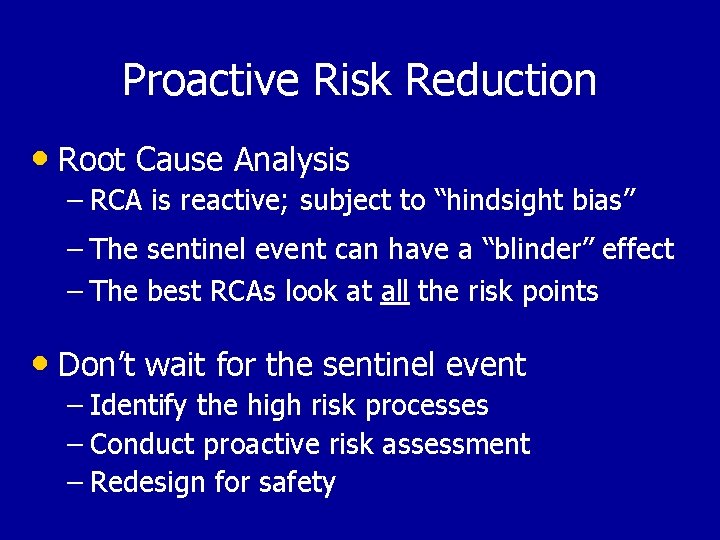
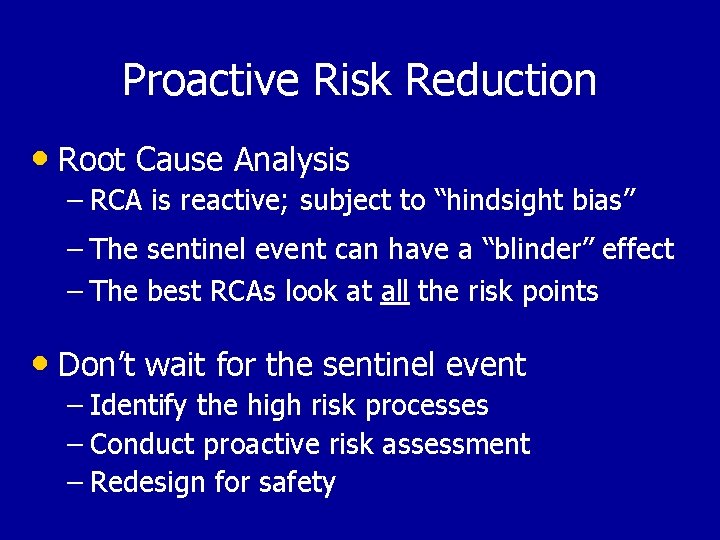
Proactive Risk Reduction • Root Cause Analysis – RCA is reactive; subject to “hindsight bias” – The sentinel event can have a “blinder” effect – The best RCAs look at all the risk points • Don’t wait for the sentinel event – Identify the high risk processes – Conduct proactive risk assessment – Redesign for safety
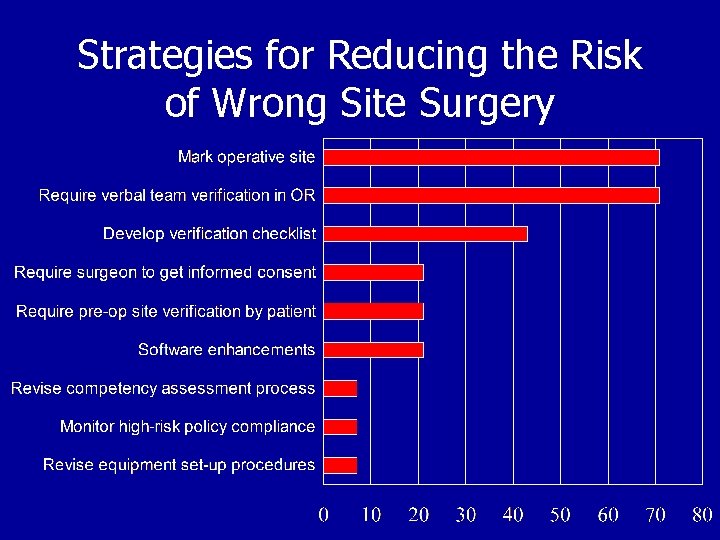
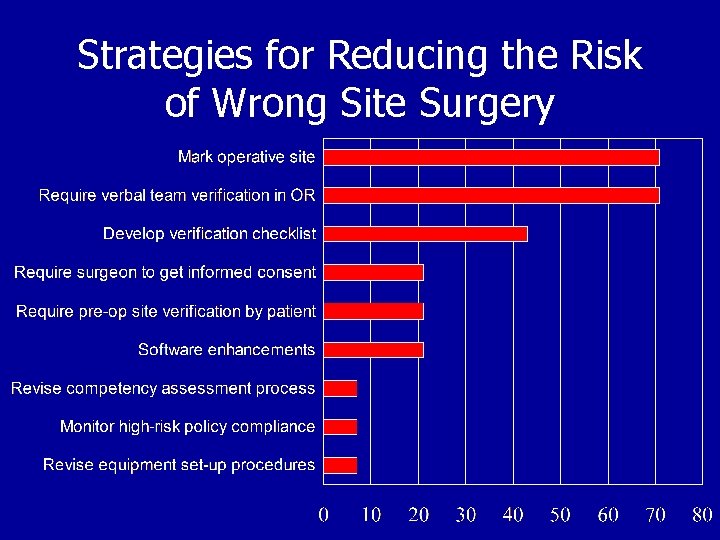
Strategies for Reducing the Risk of Wrong Site Surgery
Joint Commission UNIVERSAL PROTOCOL Guidelines to Prevent Wrong Site Surgery Triple Verification Process: • Preoperative verification • Mark the operative site • Final verification or “Time Out”
Universal Protocol Preop verification process Verification of person, place, procedure: – At the time the surgery/procedure is scheduled. – At the time of admission or entry into the facility. – Any time the responsibility for care of the patient is transferred to another caregiver. – With the patient involved, awake and aware, if possible. – Before the patient leaves the preoperative area or enters the procedure/surgical room.
Universal Protocol Preoperative Verification Checklist Review prior to the start of the procedure: – Relevant documentation (e. g. , H&P, consent). – Relevant images, properly labeled and displayed. – Any required implants and special equipment.
Universal Protocol Marking the Operative Site Mark at or near the incision site. Don’t mark any non-operative site. Unambiguous mark (Initials, “YES” or incision; not “X”) Mark must be visible after the patient is prepped and draped. Mark must survive a skin prep. Method and type of mark should be consistent. Mark all cases having laterality, multiple structures or levels. Mark vertebral level on intraoperative radiographs. Operating surgeon does the marking (ACS). Mark with the patient involved, awake and aware, if possible. “Time Out” final verification of the site mark. Have protocol for patients who refuse site marking.
Universal Protocol - Exemptions • Single organ (e. g. , C-section, cardiac surgery). • Interventional (e. g. , cardiac catheterization). • Teeth—BUT, indicate operative tooth name(s) on • documentation OR mark the operative tooth (teeth) on the dental radiographs or dental diagram. Premature infants, for whom the mark may cause a permanent tattoo.
Universal Protocol - Time Out - • Immediately before starting the procedure • In the location where the procedure will be done • Must involve the entire operative team – Surgeon, Scrub, Circulator, Anesthesia • Use active communication and be documented • Must include: – – – Correct patient identity Correct side and site Agreement on the procedure to be done Correct patient position Availability of implants, equipment or special requirements • Protocols for reconciling differences in staff responses
If a Wrong Site Event Occurs… • Act in accord with patient’s best interest • Documentation and Notification – Patient and Family – Appropriate Hospital Personnel – Document explicitly as “Wrong Site Surgery” • Work to improve the system
Resources • JCAHO. Universal Protocol for Preventing Wrong Site, • • Wrong Procedure, Wrong Person Surgery. http: //www. jcaho. org/accredited+organizations/patient+ safety/universal+protocol/wss_universal+protocol. htm Department of Veterans Affairs. Ensuring correct surgery; 2002. VHA Directive 2002 -070. http: //www. patientsafety. gov/Correct. Surg. Dir. pdf American Academy of Orthopaedic Surgeons. Advisory statement on wrong site surgery. http: //www. aaos. org/wordhtml/papers/advistmt/1015. ht m
Resources • American Academy of Orthopaedic Surgeons. • • Report of the task force on wrong-site surgery. http: //www. aaos. org/wordhtml/meded/tasksite. htm North American Spine Society. Prevention of wrong-site surgery: sign, mark & x-ray (SMa. X). http: //www. spine. org/smax. cfm Association of Operating Room Nurses. AORN position statement on correct site surgery. http: //www. aorn. org/about/positions/correctsite. htm