Haz Mat for WV Hospitals Decontamination Disposal Documentation







- Slides: 45
Haz. Mat for WV Hospitals: Decontamination, Disposal, Documentation Module IV
This course was developed by En. Magine, who we wish to gratefully acknowledge. The material has been modified by WV DHHR in cooperation with the West Virginia Hospital Association’s Disaster Preparedness Task Force in the teaching of Hospital Decontamination.
Objectives • Explain decontamination procedures for victims, personnel, and equipment. • Discuss application of relevant Standard Operating Procedures. • Describe proper disposal and documentation procedures during a Decon response.

Decontamination • Removing or neutralizing contaminants – Personnel – Equipment
Types of Decon • Primary/Technical – Done at the scene, usually by Emergency Services • Secondary – Done at hospital for patients who received decon at the scene (detailed decon) • Emergency – Done at hospital for patients who have bypassed on-scene decon
Who, What, When & Why • Who/What: People & equipment – Patients – Responders – Equipment
Who, What, When & Why • Who should do Decon : – properly trained & equipped personnel • What/How to Decon: – Decon individuals who have not received primary decon and those who need secondary decon – No absolute method of decon – Only general guides for decon
Who, What, When & Why • When: Anytime you suspect contamination – Material is visible – Patient complains of pain, odor, etc. – Patient was in the release
Who, What, When & Why: Degree of Contamination • • • Amount of material on the patient Length of time it’s on the patient Concentration of material Physical state of material Ambient temperatures
Who, What, When & Why • Why: Prevent escalation of problem – Exposure: patient is exposed to release or product – Contamination: it is on patient – Exposure of others; contamination of facility, etc.
Who, What, When & Why Consequences of No Decon • Acute/Chronic health effects • Problem gets bigger • Death!

Performing Decon • Physical removal • Chemical removal • Emergency Decon
Performing Decon • Procedures follow logical order • Go from “dirty” to “clean” • Check your plan

Decon Procedures • Anytime you suspect contamination • Use common sense – Life risk – Level of exposure
Decon Procedures • Remove all clothing from victim – Including undergarments • Use copious amounts of water – Copious=more than you have used • Large amounts: high volume

Decon Procedures • Precautions – Avoid contact w/clothing (use PPE) – Ensure privacy of victim(s) • Barriers/garments • Segregate by gender
Decon Procedures • Hospital Considerations – Did individuals receive decon prior to transport? – Protect staff/facility/equipment – Secure contaminated clothing
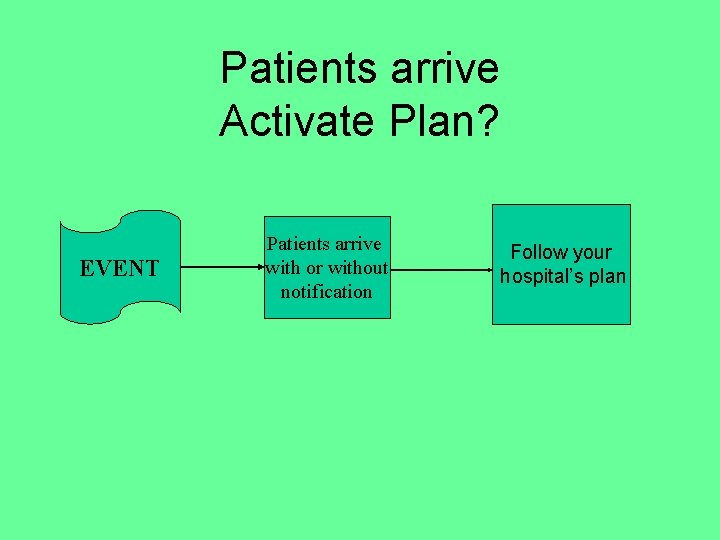
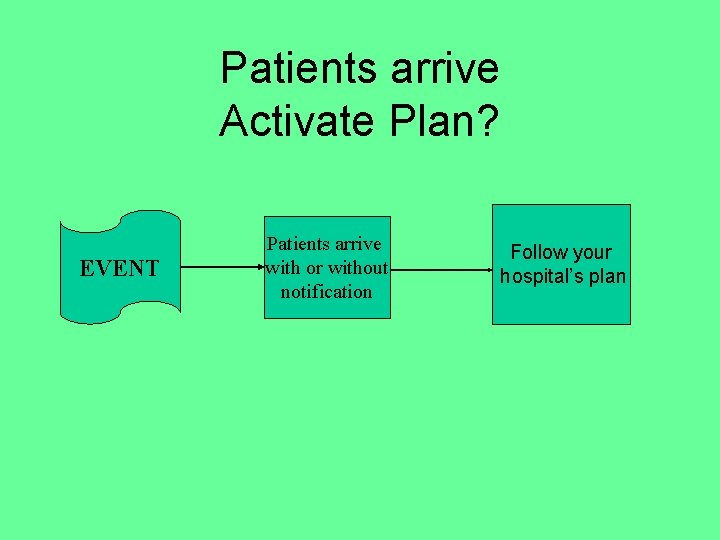
Patients arrive Activate Plan? EVENT Patients arrive with or without notification Follow your hospital’s plan
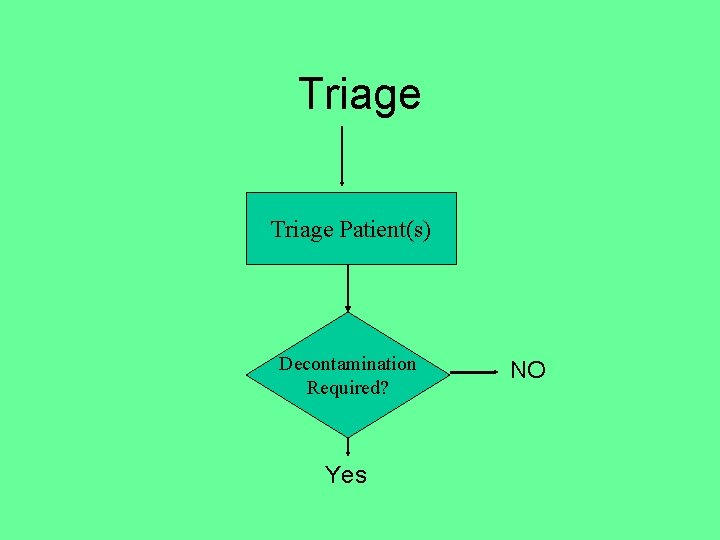
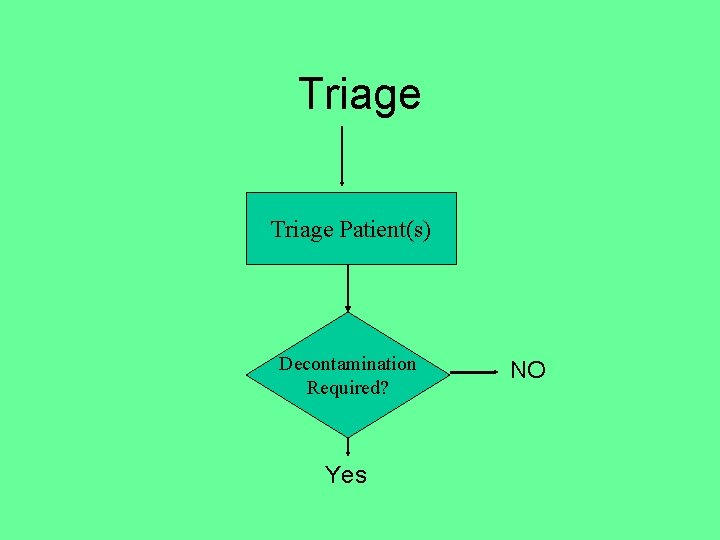
Triage Patient(s) Decontamination Required? Yes NO
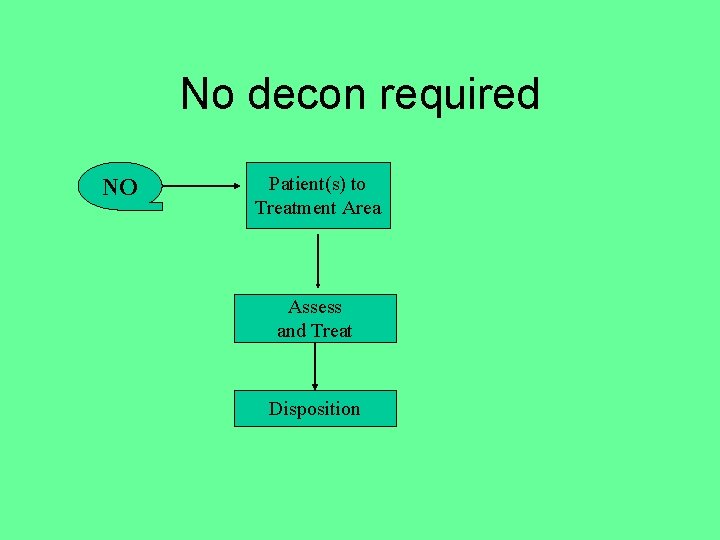
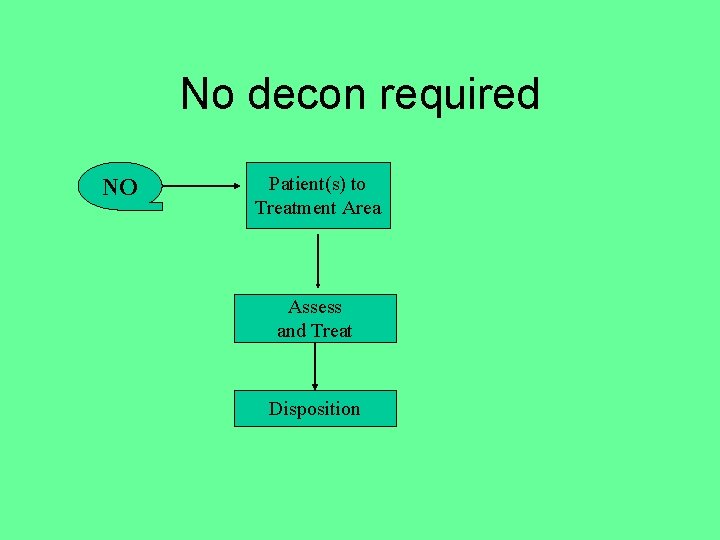
No decon required NO Patient(s) to Treatment Area Assess and Treat Disposition

Decon required Yes Activate hospital Decon protocols Collect personal belongings/ evidence** Secondary Triage Emergency Treatment required?
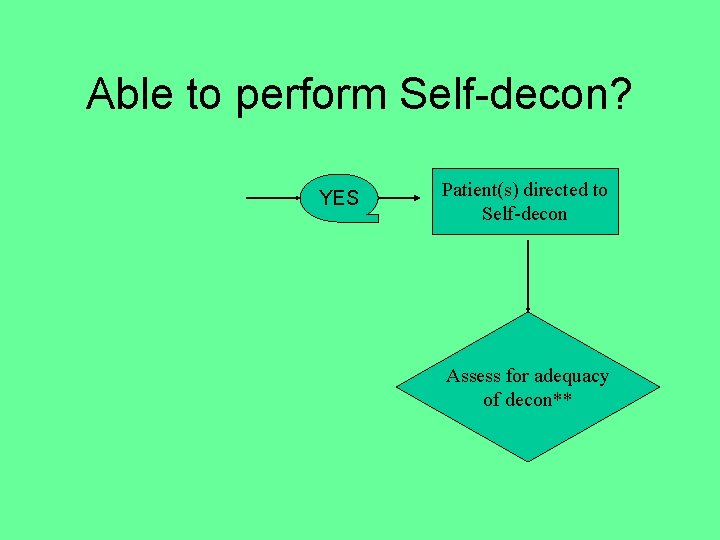
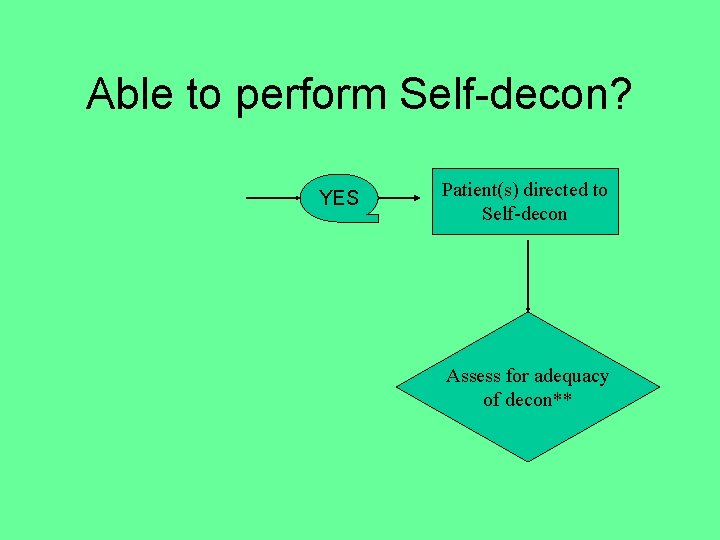
Able to perform Self-decon? YES Patient(s) directed to Self-decon Assess for adequacy of decon**
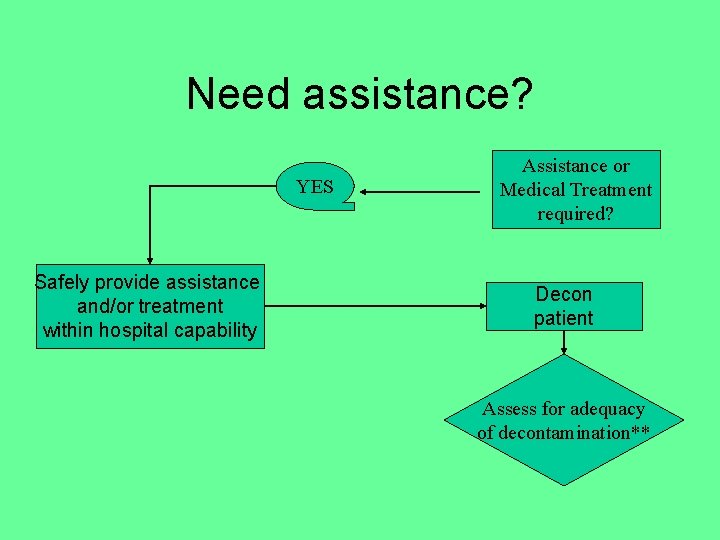
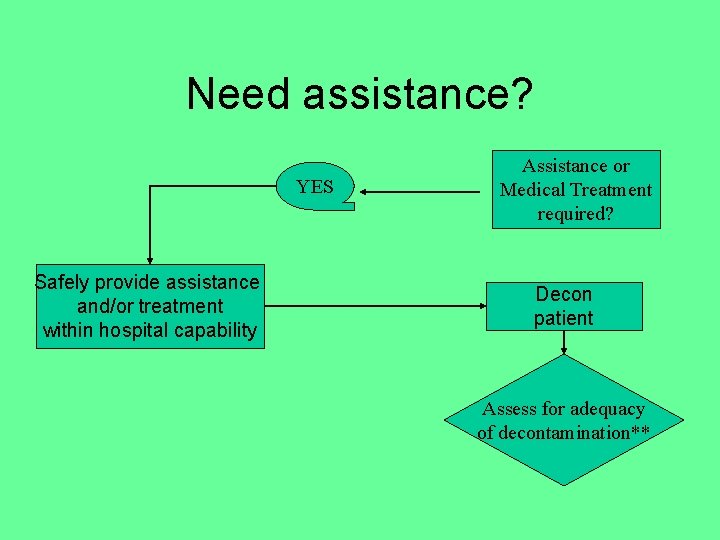
Need assistance? YES Safely provide assistance and/or treatment within hospital capability Assistance or Medical Treatment required? Decon patient Assess for adequacy of decontamination**
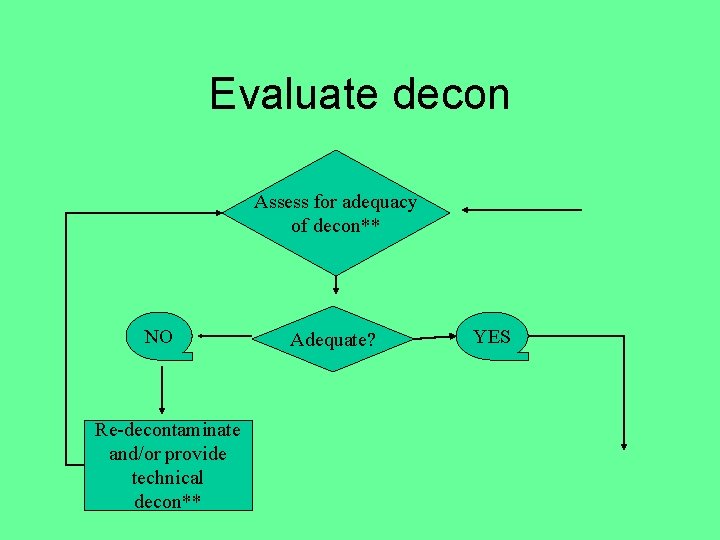
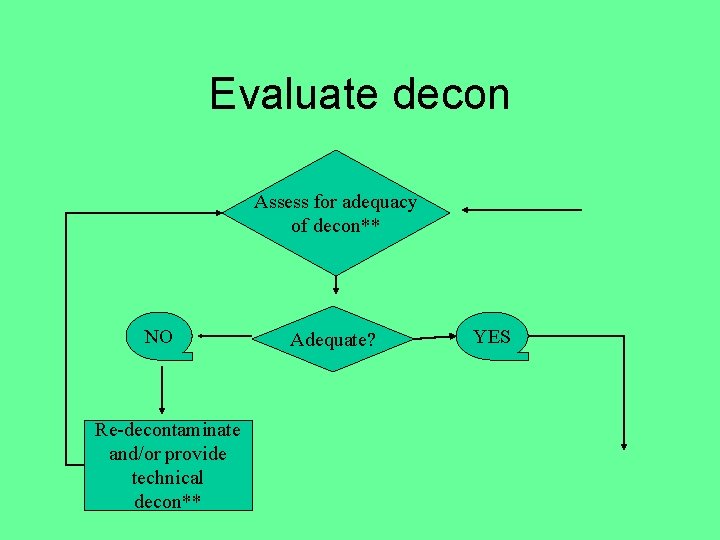
Evaluate decon Assess for adequacy of decon** NO Re-decontaminate and/or provide technical decon** Adequate? YES
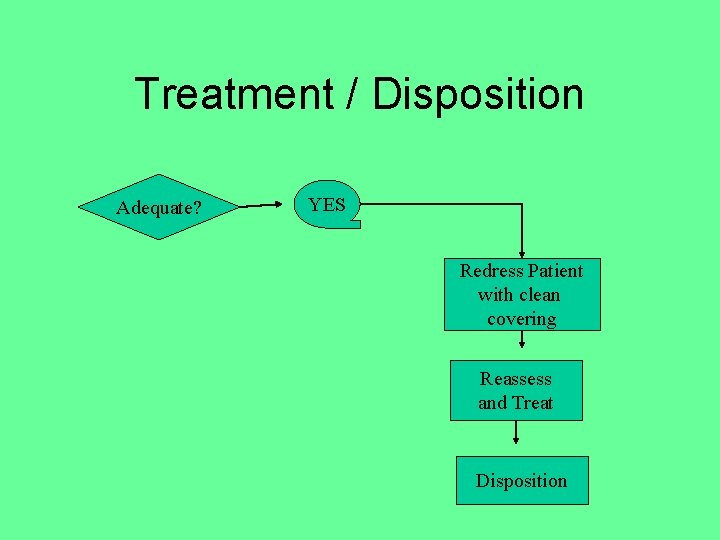
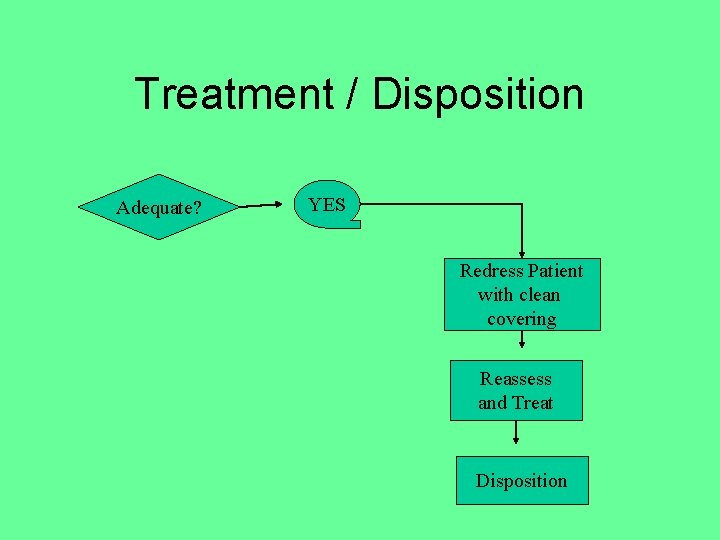
Treatment / Disposition Adequate? YES Redress Patient with clean covering Reassess and Treat Disposition
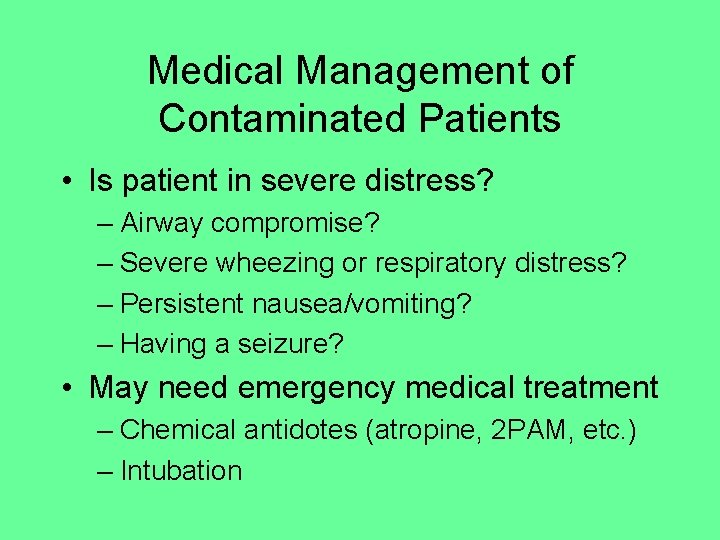
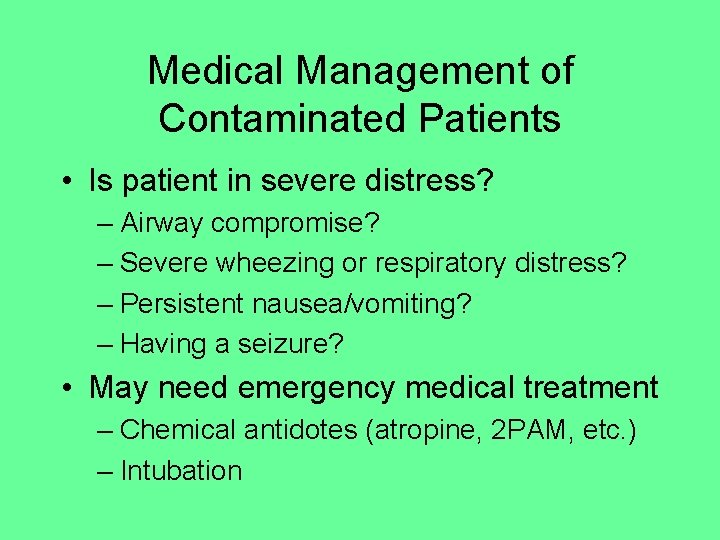
Medical Management of Contaminated Patients • Is patient in severe distress? – Airway compromise? – Severe wheezing or respiratory distress? – Persistent nausea/vomiting? – Having a seizure? • May need emergency medical treatment – Chemical antidotes (atropine, 2 PAM, etc. ) – Intubation
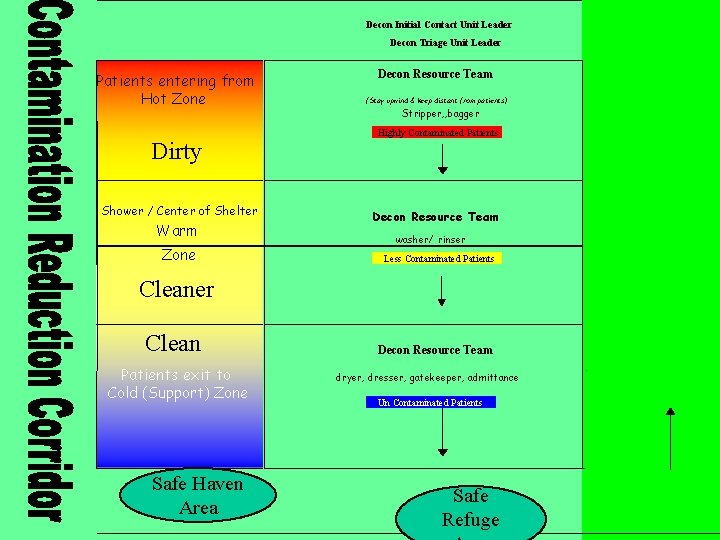
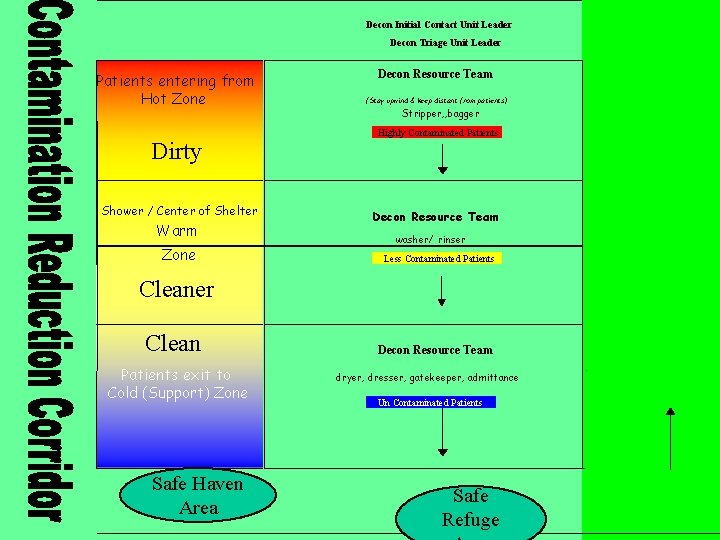
Decon Initial Contact Unit Leader Decon Triage Unit Leader Patients entering from Hot Zone Dirty Shower / Center of Shelter Warm Zone Decon Resource Team (Stay upwind & keep distant from patients) Stripper, , bagger Highly Contaminated Patients Decon Resource Team washer/ rinser Less Contaminated Patients Cleaner Clean Patients exit to Cold (Support) Zone Safe Haven Area Decon Resource Team dryer, dresser, gatekeeper, admittance Un Contaminated Patients Safe Refuge
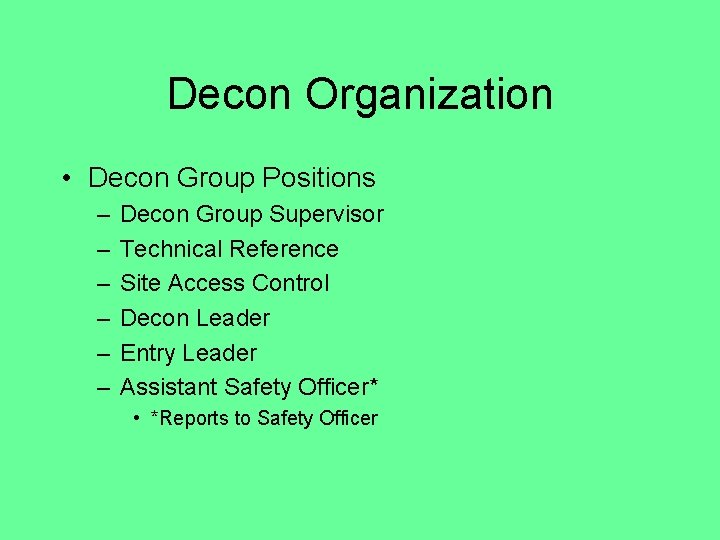
Decon Organization • Decon Group Positions – – – Decon Group Supervisor Technical Reference Site Access Control Decon Leader Entry Leader Assistant Safety Officer* • *Reports to Safety Officer
Decon Resource Team
Decontamination Procedures
Mass Decon Hospital Based
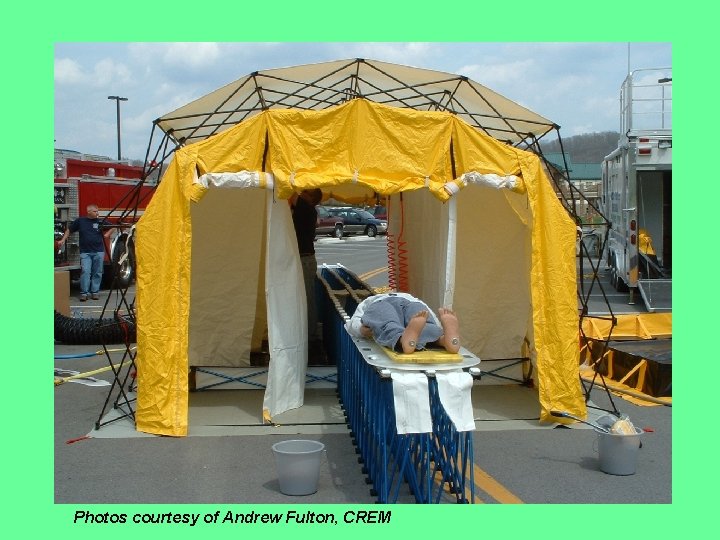
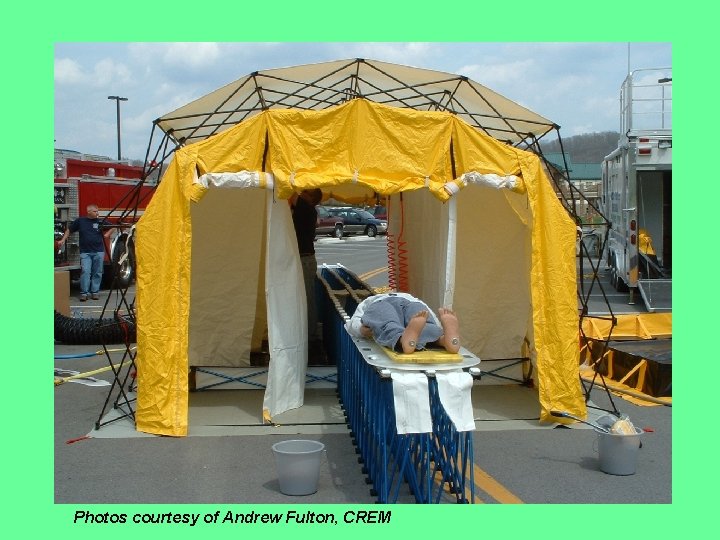
Photos courtesy of Andrew Fulton, CREM


What do you do/ if one of the Decon Resource Team goes down?
Reasons for Documentation of Decon Activities • Cost recovery • Exposure records
Disposal of Contaminated Items All contaminated items are to be bagged and in a secure location until they can properly removed and de-contaminated /disposed of by a licensed firm or government agency.
Components of Documentation • Date, time and location • Names of all response personnel – What jobs were they assigned? • Incident conditions, observations and statements • Material name/s, weather conditions
Components of Documentation • Actions taken, resources used, costs incurred • Statements & Observations of witnesses • Diagrams, photos, and video
Decon Exposure Records Mike Zolotoff Salazar, Robert • Keep exposure records! – Employer must keep for 30 years • All responders: keep own copies
Decon Exposure Records • Date, time and location of incident • Chemical name • Decon or medical aid given
Post Event Monitoring • Personnel (Work w/Employee Health Services) – Respiratory Monitoring – Chronic and Acute exposure and affects – Chemical Exposure Records for files
Role of the FRO • Safely and competently respond • Within appropriate – – Level – Resources and – Capabilities
Summary of Module IV - Decon • Decon of victims – Who, What, When, Why – How to decon – Directed, self decon vs. Mass decon – Documentation – Disposal • Some may need medical management
Questions?
 Mat för unga idrottare
Mat för unga idrottare Supernova
Supernova Sterile processing decontamination ppe
Sterile processing decontamination ppe Contamination vs cross contamination
Contamination vs cross contamination Government decontamination service
Government decontamination service Steelco decontamination equipment
Steelco decontamination equipment Sphair decontamination
Sphair decontamination Ewald tube
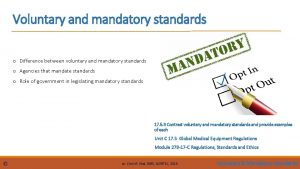
Ewald tube Difference between mandatory and voluntary standards
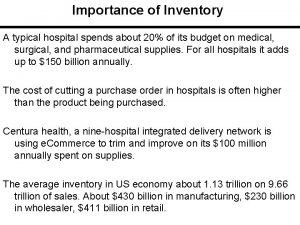
Difference between mandatory and voluntary standards Inventory cycle time
Inventory cycle time Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs Lean hospitals mark graban
Lean hospitals mark graban Joint commission international
Joint commission international Dnv vs joint commission
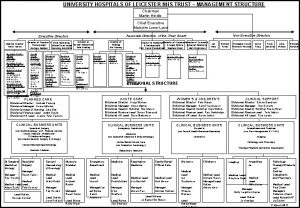
Dnv vs joint commission University hospitals
University hospitals Worcestershire acute hospitals nhs trust
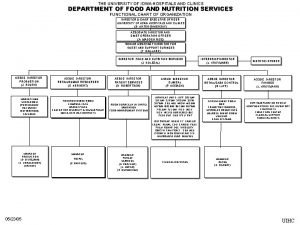
Worcestershire acute hospitals nhs trust University of iowa hospitals and clinics
University of iowa hospitals and clinics Process governance
Process governance Fhpl network hospitals in hyderabad
Fhpl network hospitals in hyderabad Echs empanelled hospitals in visakhapatnam
Echs empanelled hospitals in visakhapatnam Bcp for hospitals
Bcp for hospitals Bed management in hospitals
Bed management in hospitals National accreditation board for hospitals
National accreditation board for hospitals Strengths of hospitals
Strengths of hospitals Portsmouth trust values
Portsmouth trust values Administrator plus hospital software
Administrator plus hospital software Va hospitals in alaska
Va hospitals in alaska What are the uses of computer in hospital
What are the uses of computer in hospital Clinical data repository
Clinical data repository Lokmanya orthopedic hospital pune
Lokmanya orthopedic hospital pune Lean hospitals
Lean hospitals Louisiana department of health and hospitals
Louisiana department of health and hospitals Medisep hospitals in kerala
Medisep hospitals in kerala Uhcw floor plan
Uhcw floor plan Yaratma olarak sanat temsilcileri
Yaratma olarak sanat temsilcileri Envolver affirmative tu command
Envolver affirmative tu command Ertsey attila autonóm ház
Ertsey attila autonóm ház Video de aliento
Video de aliento Lesion primera y segunda motoneurona
Lesion primera y segunda motoneurona Di lo que haces haz lo que dices y demuéstralo
Di lo que haces haz lo que dices y demuéstralo Proyectos de 5s
Proyectos de 5s Ejemplos de argumentos de confianza del emisor
Ejemplos de argumentos de confianza del emisor Pianoverb
Pianoverb Oracion del catequista señor haz que yo sea tu testigo
Oracion del catequista señor haz que yo sea tu testigo Ven di sal haz ten weapons
Ven di sal haz ten weapons Sió csárda
Sió csárda