Growth Disorders Most children evaluated for short stature


















- Slides: 50
Growth Disorders
• Most children evaluated for short stature are normal stature variants. • The slow growth patterns of these children reflect familial short stature and/or constitutional delay of growth and puberty




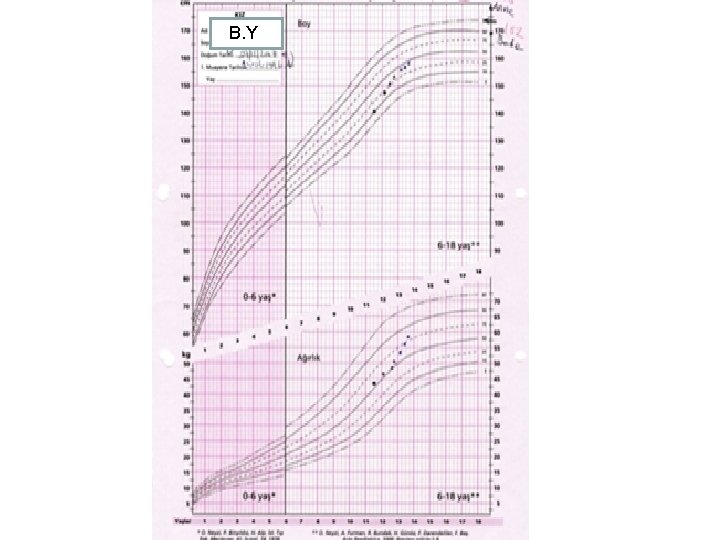
Familial short stature • Tend to be small at birth • They grow approximately parallel to the normal curve but below the 3 rd percentile from infancy • Pubertal development and the acceleration of growth occur normally and they ultimately achieve a short adult height(Father <163 cm, Mother <150 cm)
• They have no clinical or laboratory evidence of endocrine or systemic disease • Their annual growth rates are within normal limits • The bone age is appropriate for his or her chronological age

• The diagnosis of familial short stature has been perpetuated in families in which impaired growth was eventually proved to be consequence of a defined genetic disorder.
Constitutional delay in growth and puberty(CDGP) • They mature at a slower than normal rate • Height and bone age are usually delayed by 2 -4 years • Onset of pubertal maturation is understandably delayed appropriate to the child’s bone age • Often there is a history of delay in growth and pubertal development of either parent or another relative • Final adult stature, which may not be reached until the age of 20 or more years, is appropriate for parental target height range
• They are usually of normal size at birth • They grow normally for several months or years but then deviate from the “normal” growth centiles, particularly in the pre/peri-pubertal years • They grow at a normal rate for their bone age • There is a later than average adolescent “growth spurt” • Treatment: controversial • Synthetic steroids designed to have an increased anabolic-androgenic ratio: oxandrolone(oral)(hepatotoxichepatic tumors!) • No suitable equivalent for the girl

• • • A child’s current centile must be evaluated in terms of: Genetic background Gestational or past medical history Environment Physical findings Growth pattern since birth Current growth rate(height velocity)
Causes of short stature 1 - Familial or congenital conditions • Skeletal dysplasias • Chromosomal abnormalities • Forms of intrauterine growth retardation which may result in show or abnormal growth throughout later life 2 - Chronic systemic disorders: • (Due to) insufficient intake of energy and/or proteinnutritional insufficiency, malabsorption syndromes and chronic inflammatory bowel disease) • Insufficient oxygenation of tissues • Electrolyte imbalance(chronic renal failure)
3 -Endocrine abnormalities • CNS or hypothalamic abnormalities which affect regulation of the anterior pituitary • Anterior pituitary disorders, either developmental or acquired which can affect synthesis or secretion of growth hormone or the trophic hormones(TSH, LH, FSH, ACTH) • Primary dysfunction of the target organs e. g. Thyroid, adrenal or gonadal disease
• Peripheral target tissue abnormalities - a diminished or absent hormone receptor or tissue enzyme defect Laron type “dwarfism” – failure of IGF 1 generation in response to GH (A GH receptor defect) - Disorders related to the interaction of the IGF’s or other related peripheral growth factors with chondrocytes and mucopolysaccharides in epiphyseal growth cartilage Pygmies: genetic defect in IGF-1 responsiveness associated with diminished IGF-1 binding


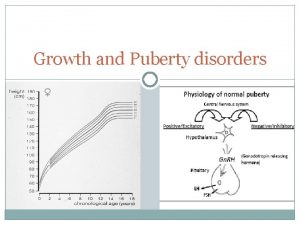
Normal human growth hormone secretion • In the first days of life, very high levels of GH occur. After 2 weeks of age, lower mean levels are found. • In pubertal children, the basal plasma GH concentration is not significantly different from that reported for adults but more peaks of GH may occur during the day with greater amplitude of GH peaks during the night • The most consistent period of GH secretion for both children and adults occurs within one hour or so after the onset of sleep. The initial surge of GH secretion often correlates with the onset of stage 3 or 4 (slow wave) sleep
Control of human growth hormone secretion • Positive releasing factor GHRH-Ghrelin • Inhibitory factor: GHRIH • Naturally occurring events that trigger GH secretion in man are exercise, physical and emotional stresses and high protein intake
Normal regulation of GH • The neurone system regulating GHRH and GHRH release receives a variety of normal impulses. Impulses arising in the hippocampus are stimulatory whereas those arising in the amygdaloid nuclei can be either stimulatory or inhibitory. The inhibitory inputs are presumed to activate GHRIH release via the anterior somatostinergic pathways, the stimulatory pathway is by way of the ventromedial(VM) nucleus of the hypotalamus
• The GH regulatory neurone system also recieves impulses from each of the ascending monoaminergic neuronal systems : dopaminergic, noradrenergic and serotonergic - L-Dopa(converted to dopamine) in the brain leads to a release of GH - Sleep induced GH release is predominantly mediated by serotonergic fibres. - Hypoglycemia induced GH release is mediated by noradrenergic pathways.
GH provocation tests • • Exercise Sleep Arginine infusion Glucagon Clonidine (alfa adrenergic receptor stimulant) ITT L-Dopa Priming(sex hormones)? ?

Physiologic effects of human growth hormone • Anabolic-promotes protein synthesis in muscle cells • Catabolic effect- on fat and carbonhydrate metabolism (short term hypoglycemic effect) inducing lipolysis in adipoctytes • Long term effect of high GH levels: plasma glucose concentration increases(increased glucose production and reduced glucose utilization)
Evalution of height measurements 1 - Growth charts 2 - Parental heights- target height 3 - Height SDS 4 - Height velocity 5 - Predicted ht SDS: X-x* SD x*: mean height for age and gender
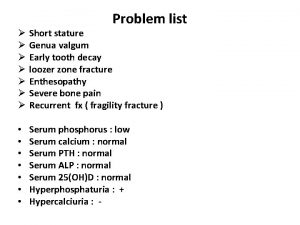
Etiology and pathogenesis of growth failure • Chromosomal assessment Turner Sydrome • FSS • IUGR “Catch up” • CDGP • Skeletal dysplasia osteochondrodysplasias(achondroplasia, hypochondroplasia)
• Chronic systemic disorders- asthma • Nutritional insufficiency • Chronic gastrointestinal diseases Coeliac disease Crohn’s disease Ulcerative colitis • Chronic renal disease • Cardiac disease • DM
Endocrine abnormalities • Primary hypothyrodism • Gonadal dysgenesis • GHD • Glucocorticoid excess • Growth failure to pyschosocial deprivation
Etiology of GHD • Congenital Acquired • İsolated MPHD


• Incidence 1/4000 -10000 live births • (50 -60%) idiopathic • Hereditary (aut. recessive or dominant)
Developmental defects • Pituitary aplasia-hypoplasia • Midline abnormalities - Severe holoprosencephaly septooptic dysplasia (SOD): Hypoplasia of the optic nerves dysgenesis or agenesis of the infundibulum and septum pellucidum +/pituitary hormone deficiency -Cleft lip palate -Single upper central incisor syndrome
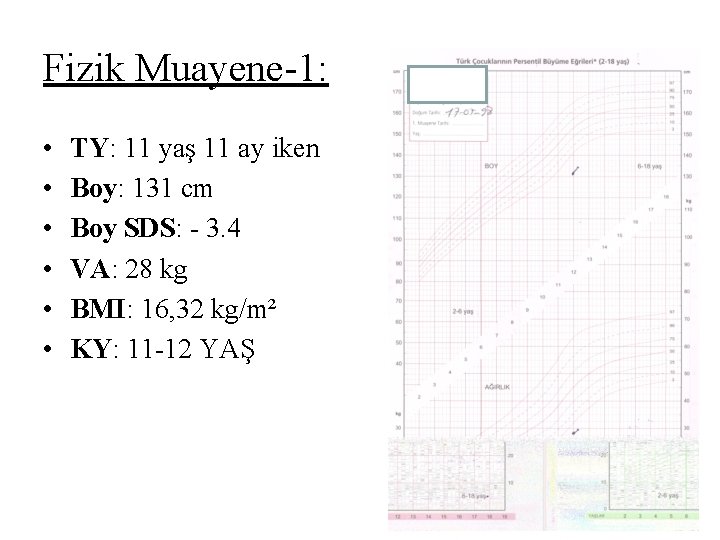
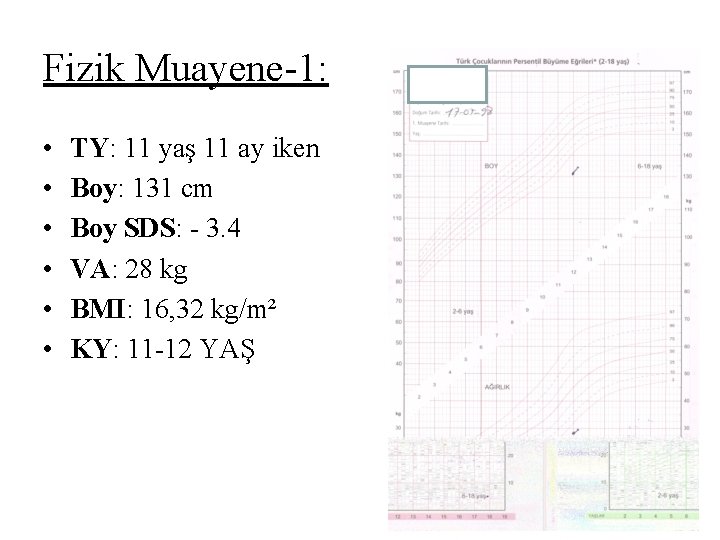
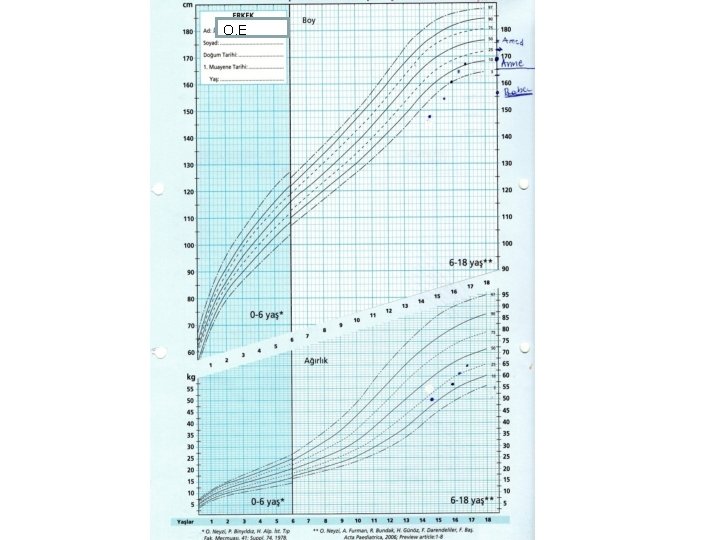
Fizik Muayene-1: • • • TY: 11 yaş 11 ay iken Boy: 131 cm Boy SDS: - 3. 4 VA: 28 kg BMI: 16, 32 kg/m² KY: 11 -12 YAŞ
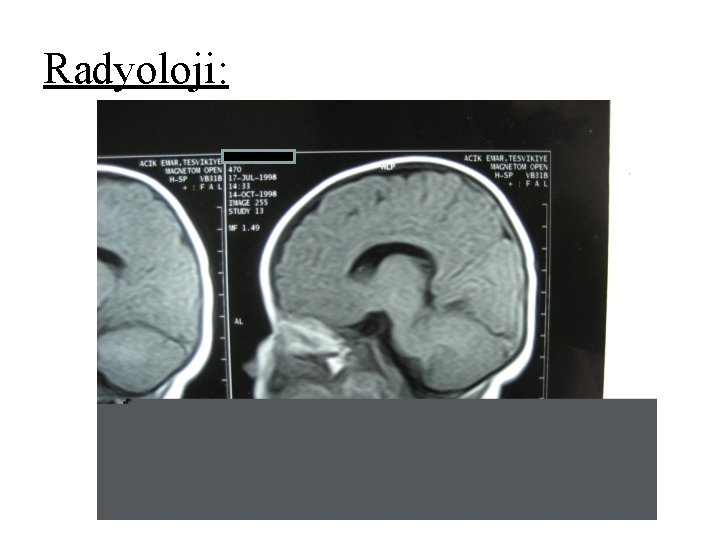
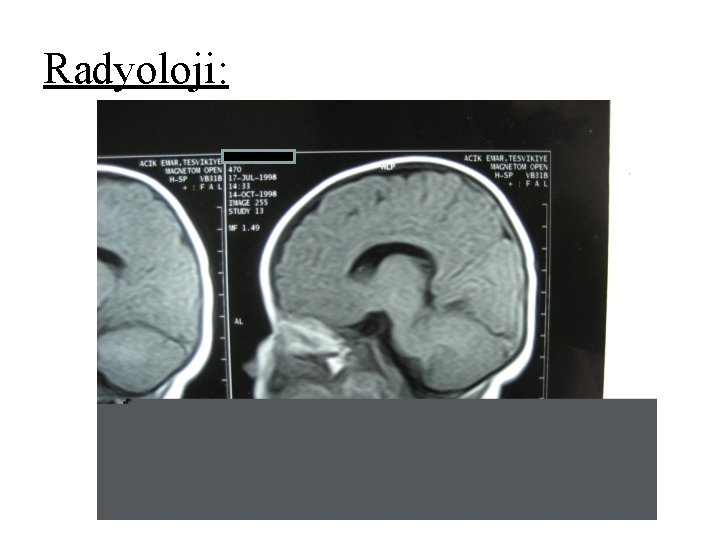
Radyoloji:

BH gene defects • All patients with classical GH gene deletions have complete GHD(IGHD IA, IB, 2, 3(+hypogammaglobulinemic))
GH gene regulation: • Pit 1 (pituitary transcription factor): stimulatory effect on GH gene transcription • Pit 1 mutations - Severe deficiencies in GH PRI - Often develop secondary hypothyrodism • Prop 1 (Prophet of pit 1) mutations combined pituitary hormone deficiency(secondary hypogonadism)

Davis 2010
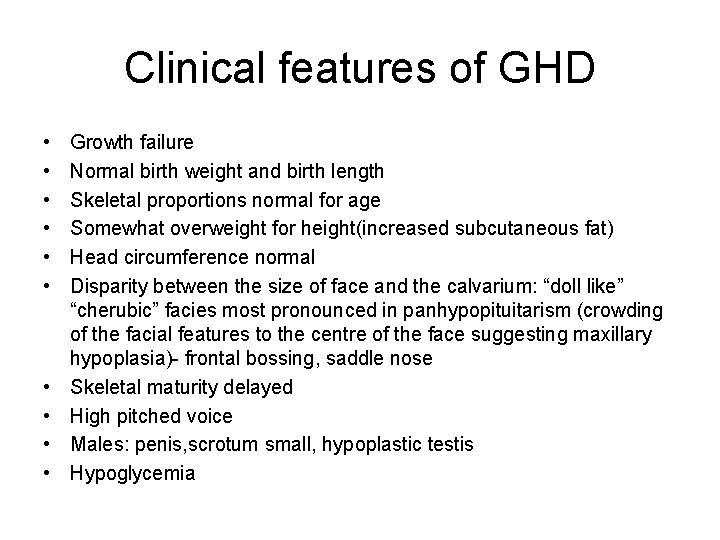
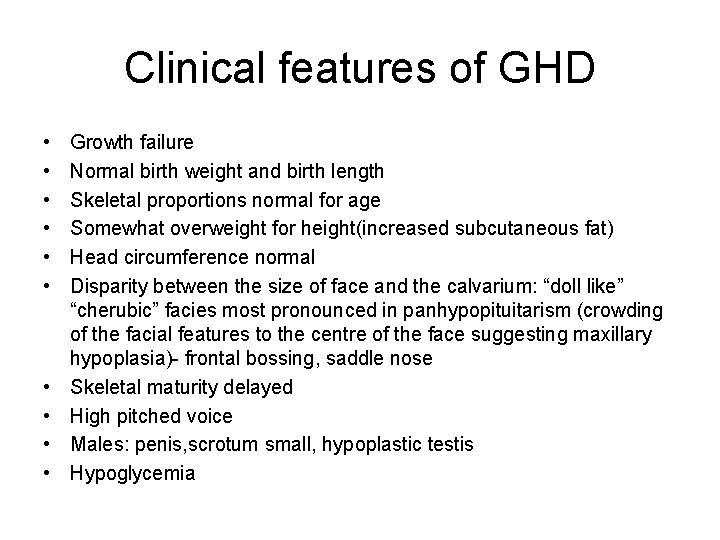
Clinical features of GHD • • • Growth failure Normal birth weight and birth length Skeletal proportions normal for age Somewhat overweight for height(increased subcutaneous fat) Head circumference normal Disparity between the size of face and the calvarium: “doll like” “cherubic” facies most pronounced in panhypopituitarism (crowding of the facial features to the centre of the face suggesting maxillary hypoplasia)- frontal bossing, saddle nose Skeletal maturity delayed High pitched voice Males: penis, scrotum small, hypoplastic testis Hypoglycemia



• Radiological assessment: Skull x rays, CT, MRI • IGF 1 measurement, physiological tests of GH secretion
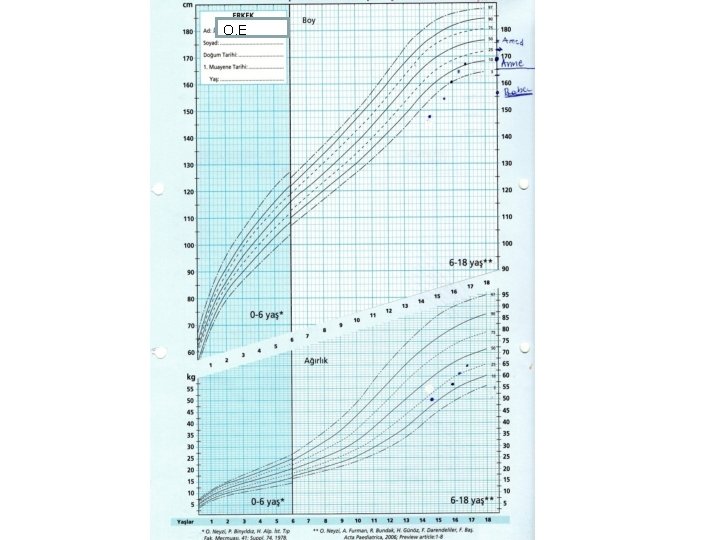
O. E

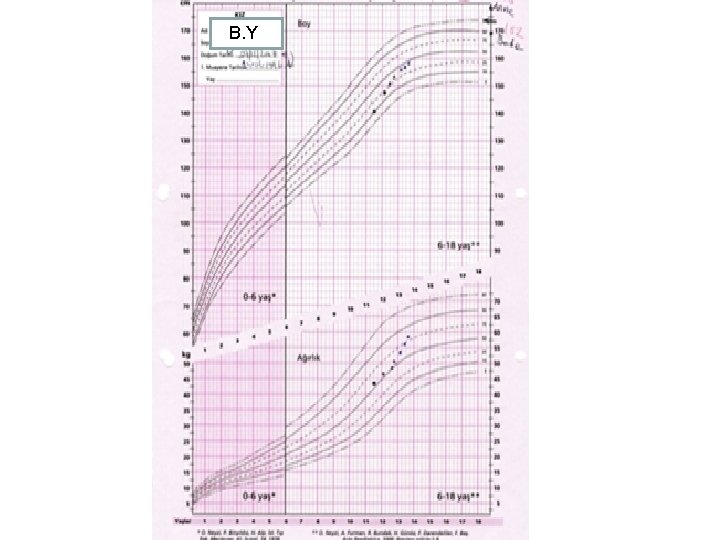
B. Y

 Tall+short h
Tall+short h Short stature definition
Short stature definition Head and chest circumference chart
Head and chest circumference chart Aristotle tragic hero elements
Aristotle tragic hero elements Stature def
Stature def Def stature
Def stature Falling action of the scarlet letter
Falling action of the scarlet letter Stature
Stature Ready to be evaluated pqeb
Ready to be evaluated pqeb Small business subcontracting is only evaluated
Small business subcontracting is only evaluated Small business participation commitment document
Small business participation commitment document Chapter 14 evaluating channel member performance
Chapter 14 evaluating channel member performance A form requesting the purchase of merchandise.
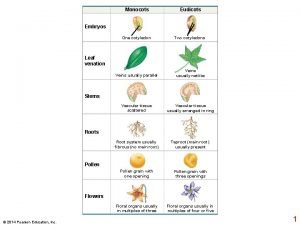
A form requesting the purchase of merchandise. Plant growth definition
Plant growth definition Root hair structure
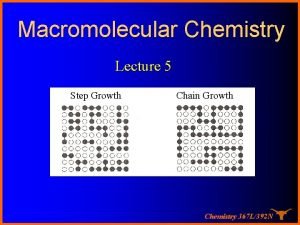
Root hair structure Growthchain
Growthchain Primary growth and secondary growth in plants
Primary growth and secondary growth in plants Chapter 35 plant structure growth and development
Chapter 35 plant structure growth and development Geometric vs exponential growth
Geometric vs exponential growth Neoclassical growth theory vs. endogenous growth theory
Neoclassical growth theory vs. endogenous growth theory Difference between organic and inorganic growth
Difference between organic and inorganic growth Short-term play therapy for children
Short-term play therapy for children Socially maladjusted vs emotional disturbance
Socially maladjusted vs emotional disturbance Long run economic growth graph
Long run economic growth graph Short essay on population growth
Short essay on population growth Kontinuitetshantering
Kontinuitetshantering Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Personlig tidbok
Personlig tidbok Sura för anatom
Sura för anatom Densitet vatten
Densitet vatten Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Debattartikel mall
Debattartikel mall Magnetsjukhus
Magnetsjukhus Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Lufttryck formel
Lufttryck formel Publik sektor
Publik sektor Jag har gått inunder stjärnor text
Jag har gått inunder stjärnor text Presentera för publik crossboss
Presentera för publik crossboss Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Vem räknas som jude
Vem räknas som jude Treserva lathund
Treserva lathund Fimbrietratt
Fimbrietratt Claes martinsson
Claes martinsson Cks
Cks