GROWTH AND ACTIVITY AND OVERGROWTH AND UNDERACTIVITY PSY








- Slides: 79
GROWTH AND ACTIVITY AND OVER-GROWTH AND UNDERACTIVITY PSY 226 Physical Development During Early Childhood
Objectives Understand normative growth and activity during early childhood. Describe the historical progression of child obesity and several physical and social risks. Identify the key factors contributing to the child obesity epidemic and give examples. Describe the role of social learning in children’s beliefs about body types. Discuss several potential solutions to preventing or reducing child obesity.
Early Childhood Physical Developments: Ages 2 -6 years Early childhood is referred to as “the play years. ” Fast growth, high activity, rapid learning, and social exploration.
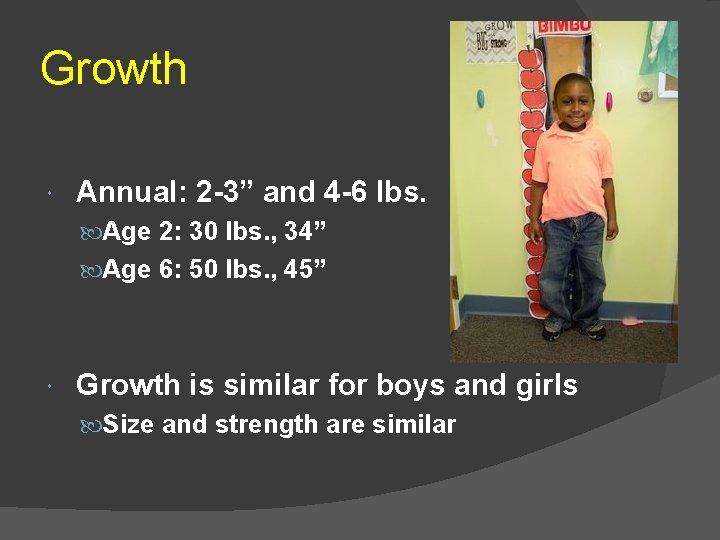
Growth Annual: 2 -3” and 4 -6 lbs. Age 2: 30 lbs. , 34” Age 6: 50 lbs. , 45” Growth is similar for boys and girls Size and strength are similar
Activity Physical play rises and peaks around 2 -3 years, then declines Children increase in their ability to sit, listen, pay attention

Activity Boys engage in more rough/tumble play Girls are less apt to wear pants? Parents activity level correlates with their child’s activity level. Parent encourage more activity from boys
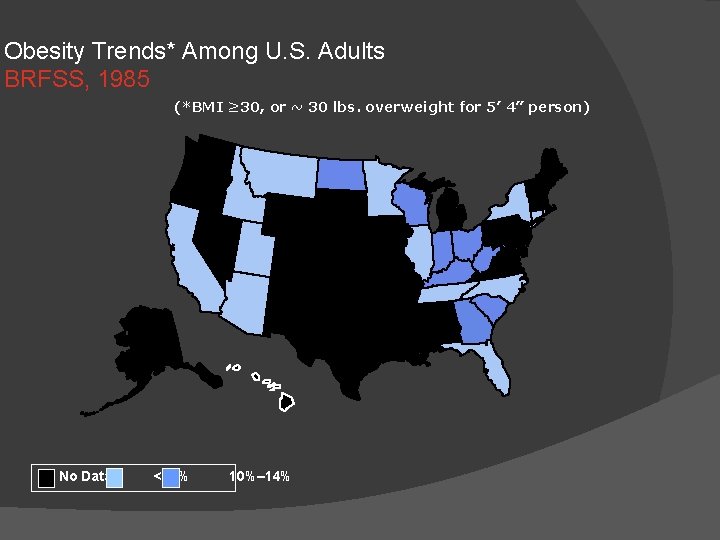
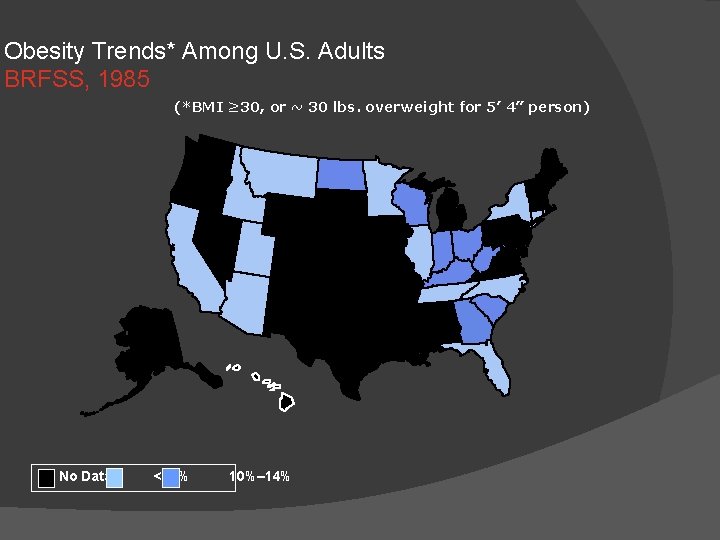
Obesity Trends* Among U. S. Adults BRFSS, 1985 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
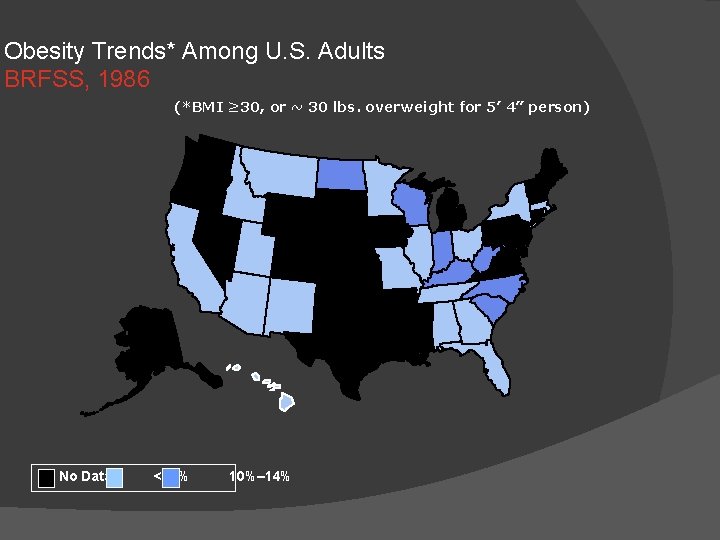
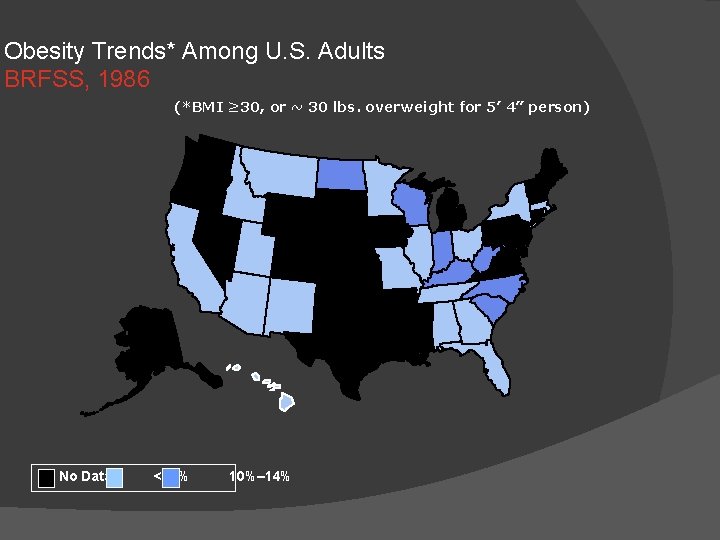
Obesity Trends* Among U. S. Adults BRFSS, 1986 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
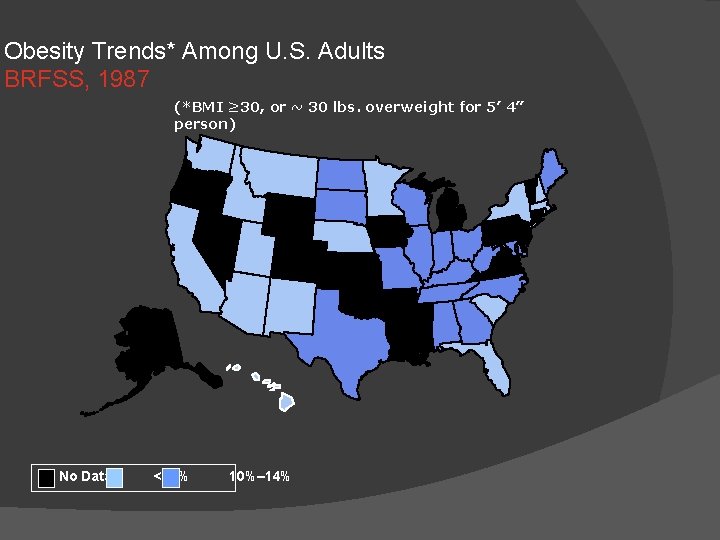
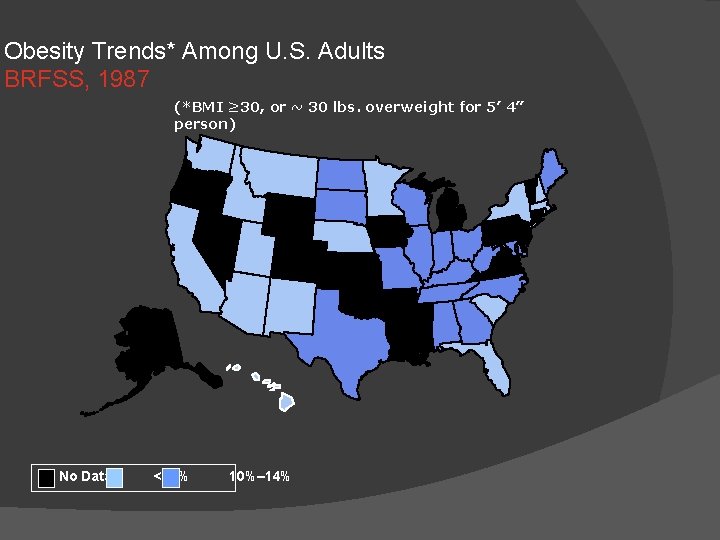
Obesity Trends* Among U. S. Adults BRFSS, 1987 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
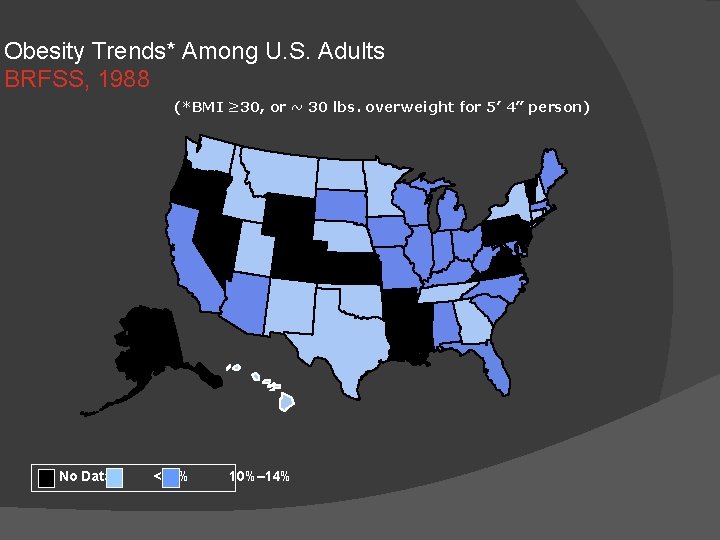
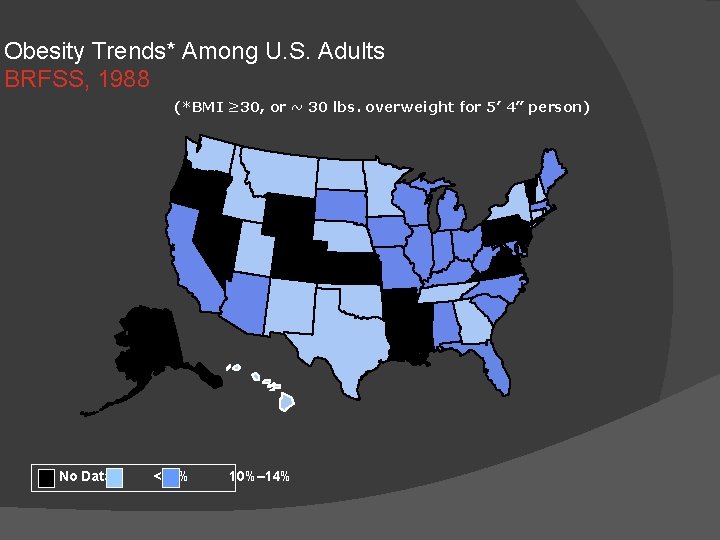
Obesity Trends* Among U. S. Adults BRFSS, 1988 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
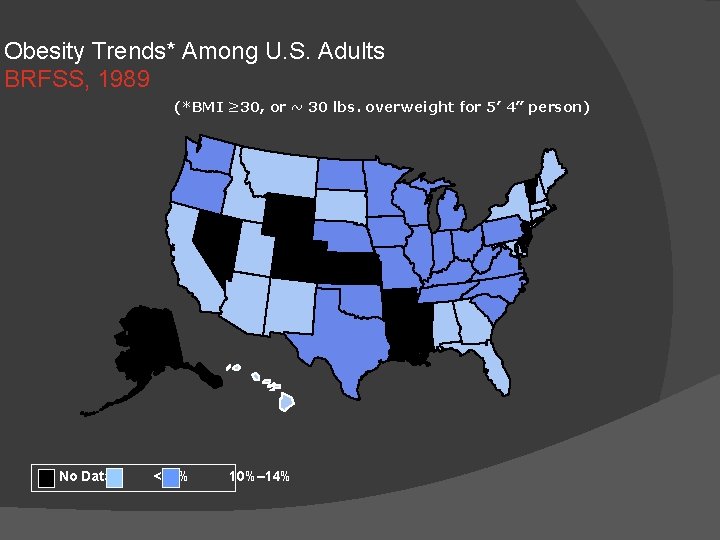
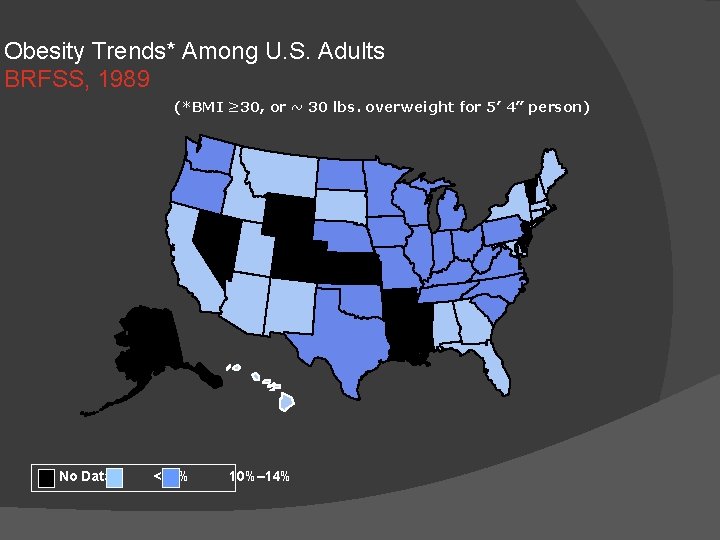
Obesity Trends* Among U. S. Adults BRFSS, 1989 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%

Obesity Trends* Among U. S. Adults BRFSS, 1990 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
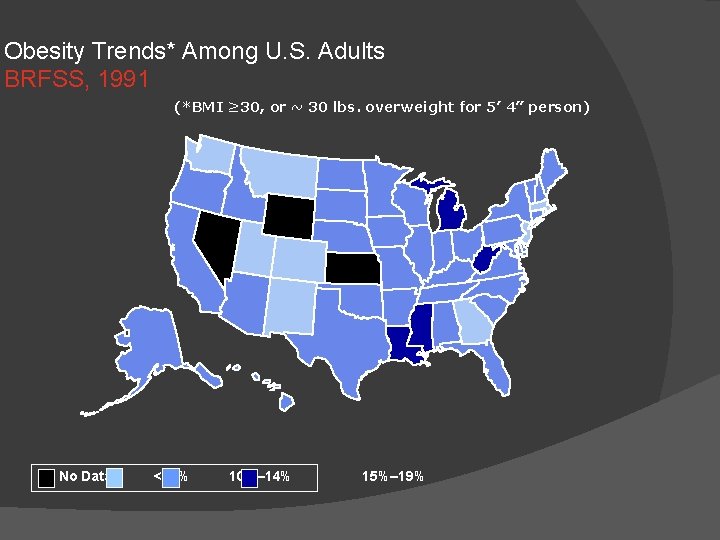
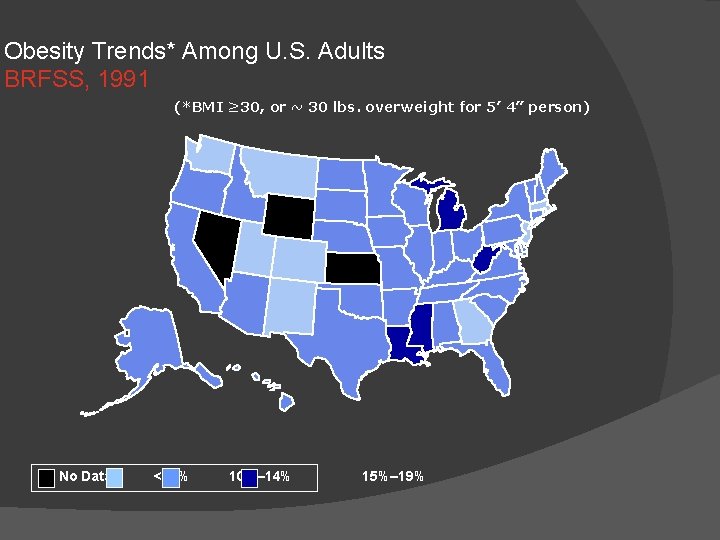
Obesity Trends* Among U. S. Adults BRFSS, 1991 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
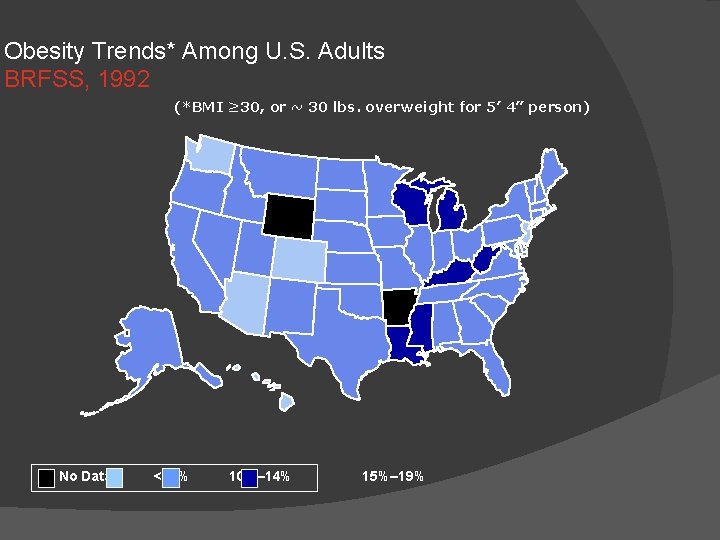
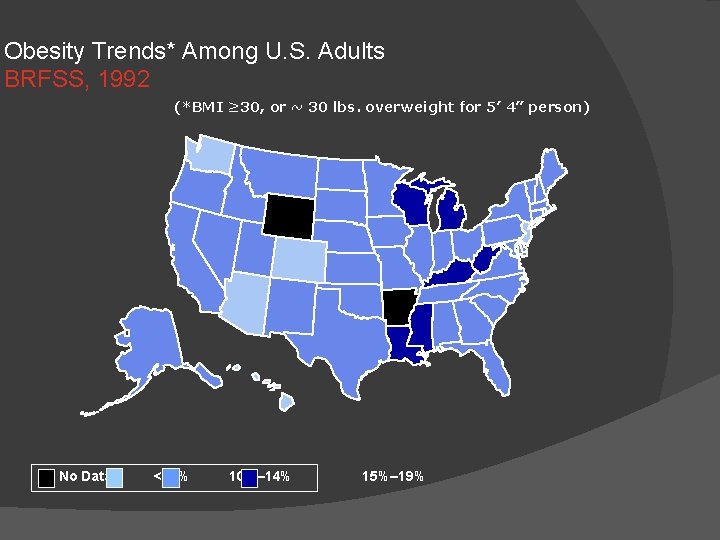
Obesity Trends* Among U. S. Adults BRFSS, 1992 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
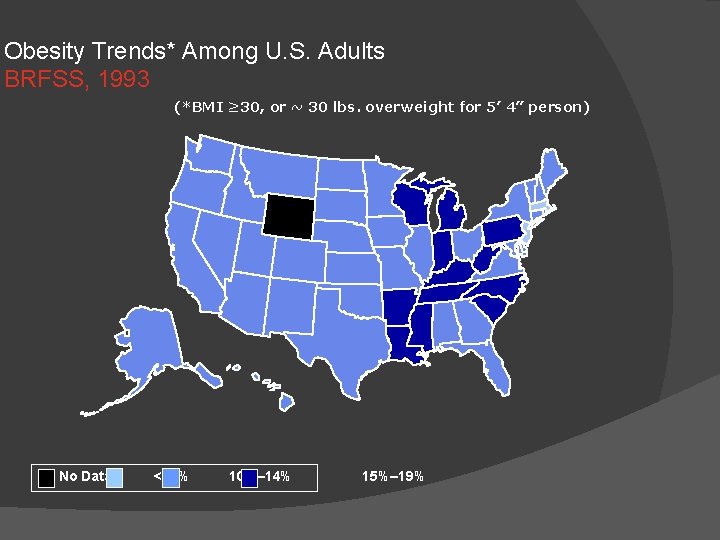
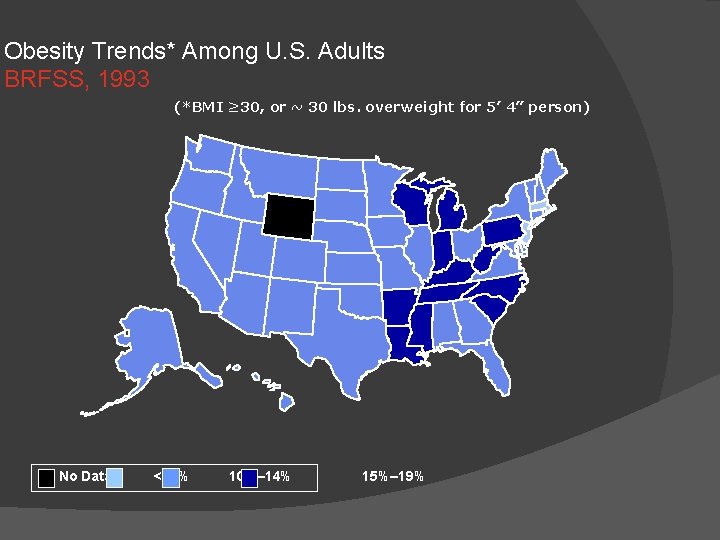
Obesity Trends* Among U. S. Adults BRFSS, 1993 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
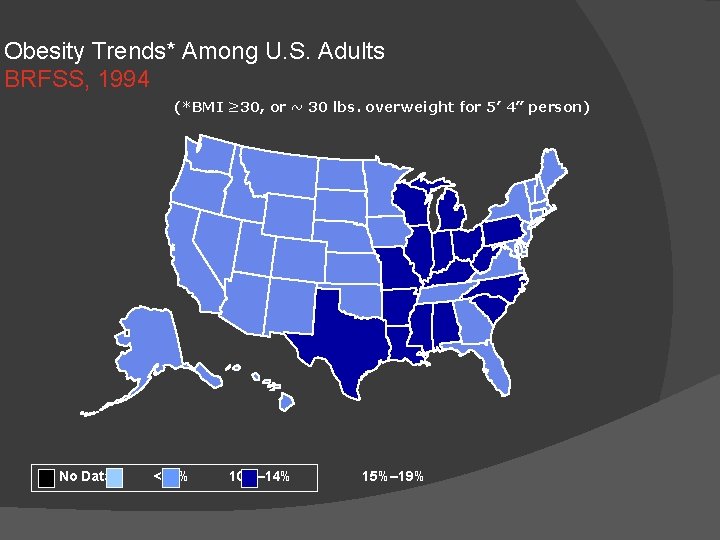
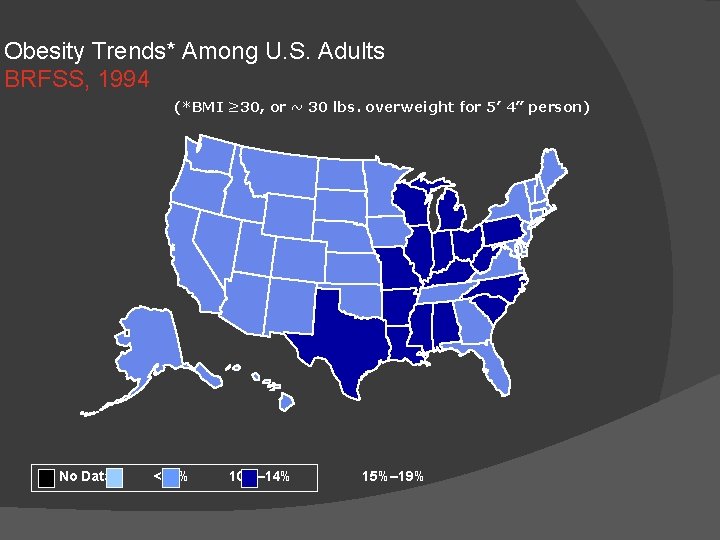
Obesity Trends* Among U. S. Adults BRFSS, 1994 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
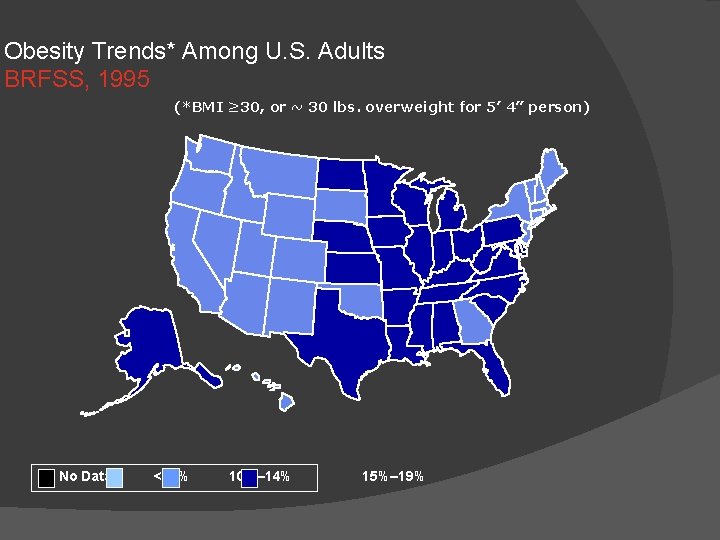
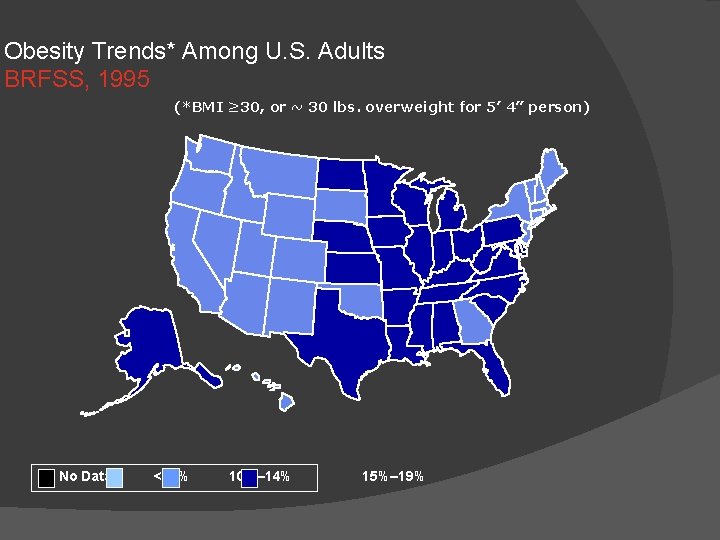
Obesity Trends* Among U. S. Adults BRFSS, 1995 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
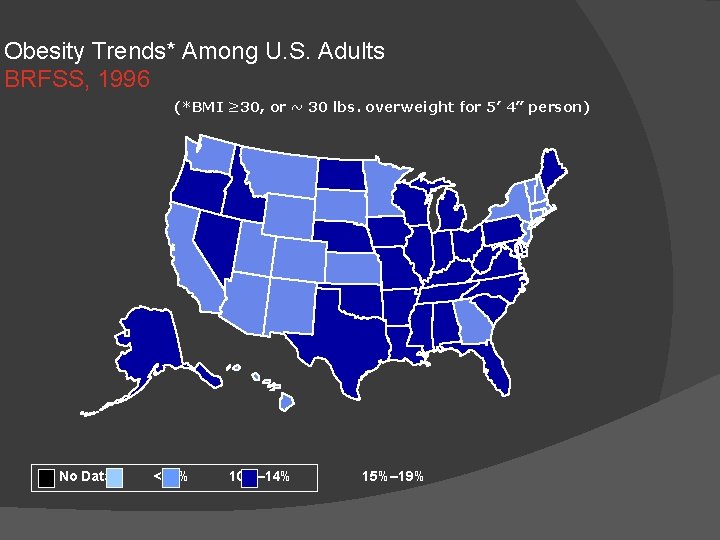
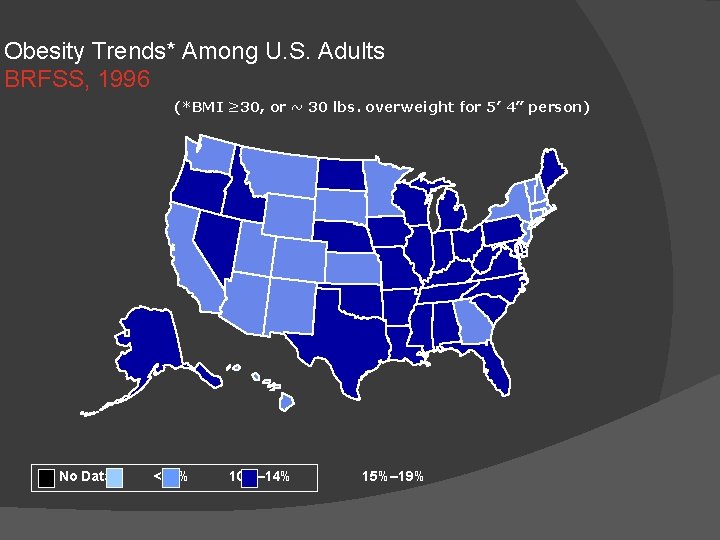
Obesity Trends* Among U. S. Adults BRFSS, 1996 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
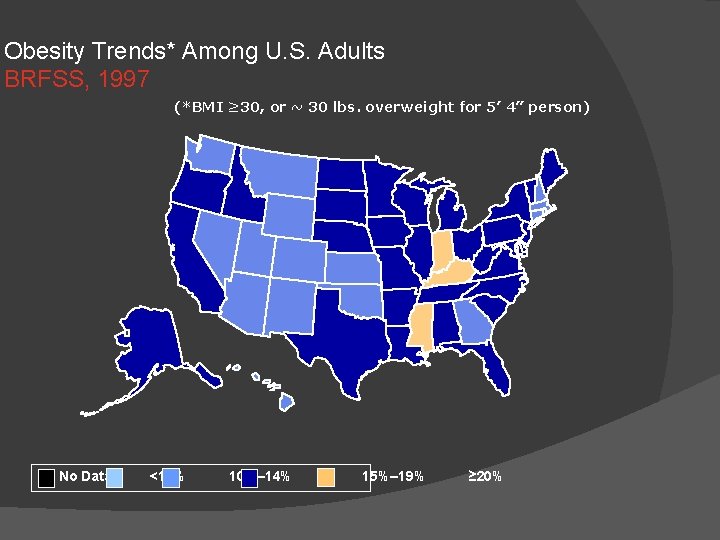
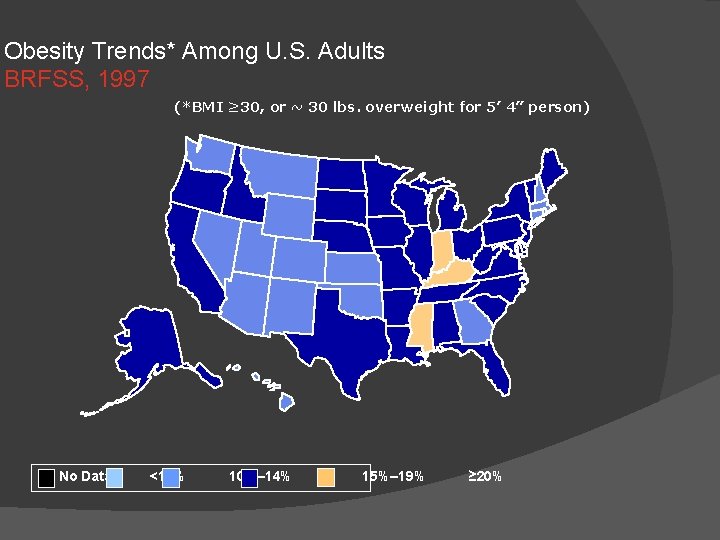
Obesity Trends* Among U. S. Adults BRFSS, 1997 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
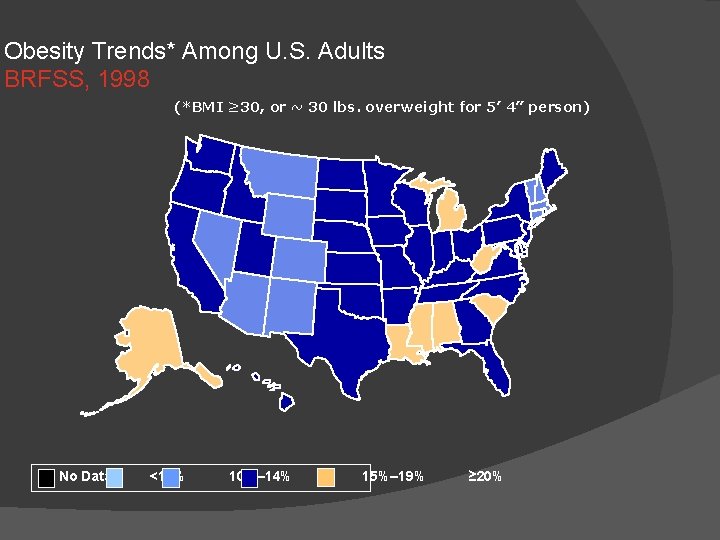
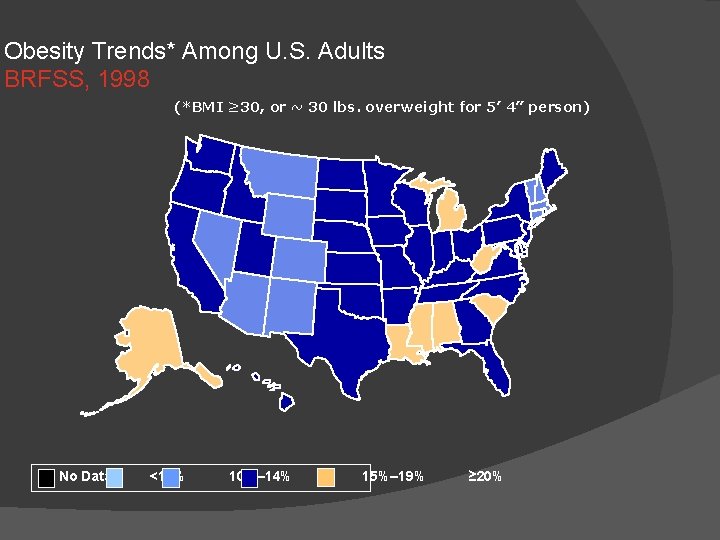
Obesity Trends* Among U. S. Adults BRFSS, 1998 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
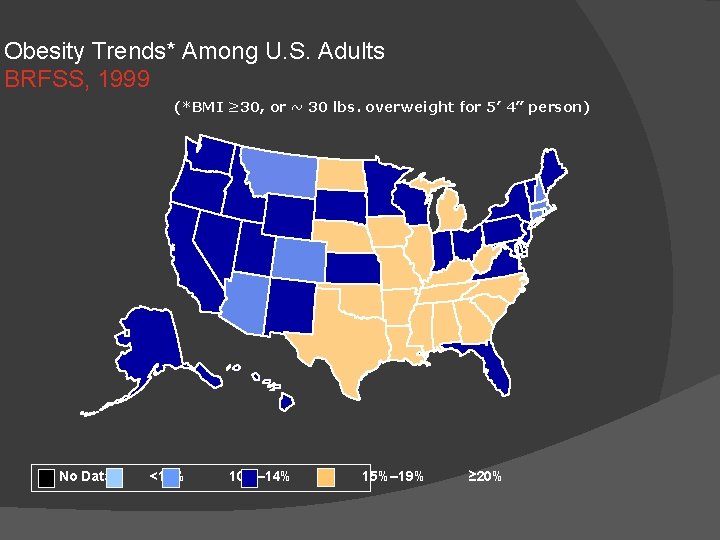
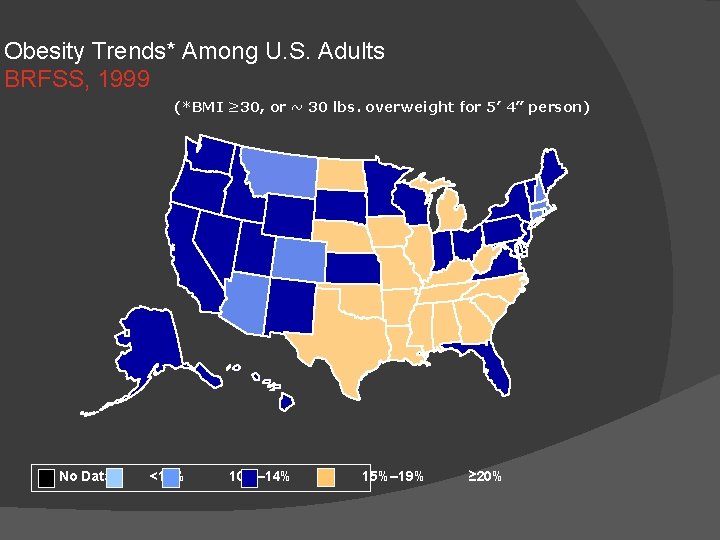
Obesity Trends* Among U. S. Adults BRFSS, 1999 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
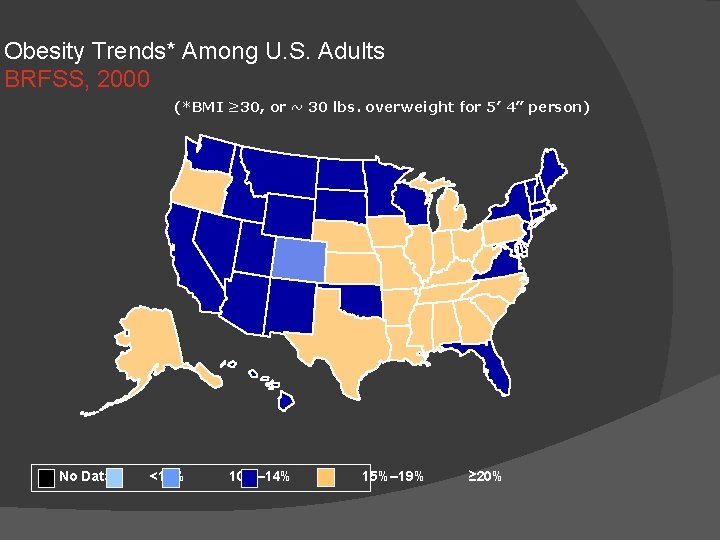
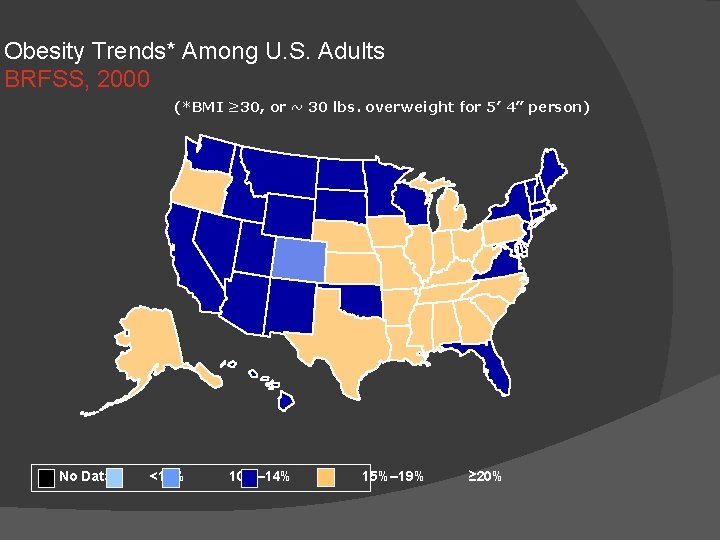
Obesity Trends* Among U. S. Adults BRFSS, 2000 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
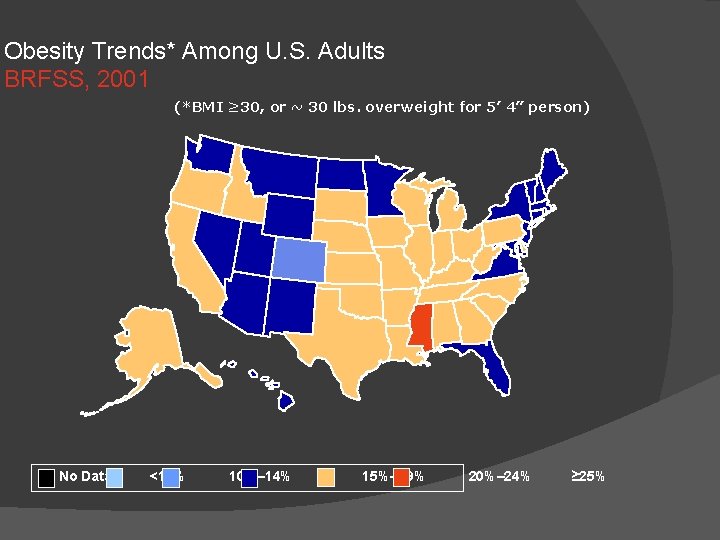
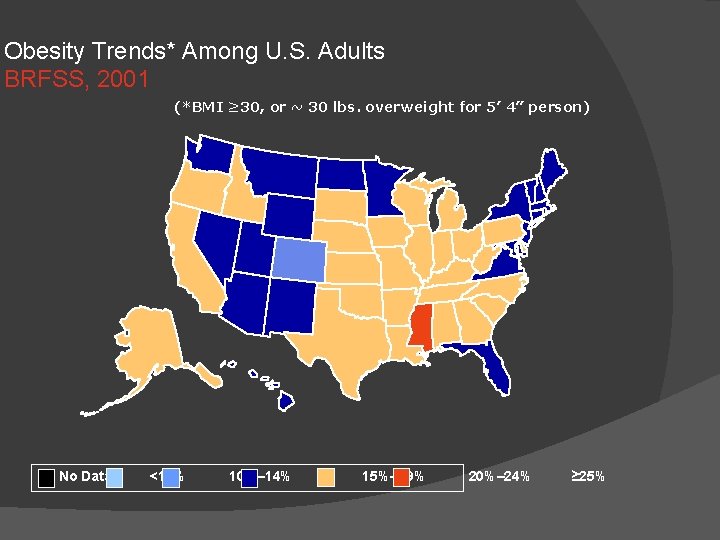
Obesity Trends* Among U. S. Adults BRFSS, 2001 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
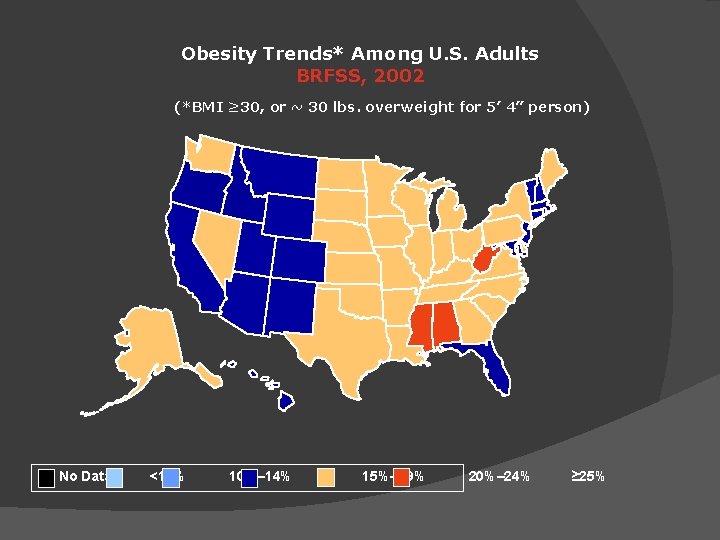
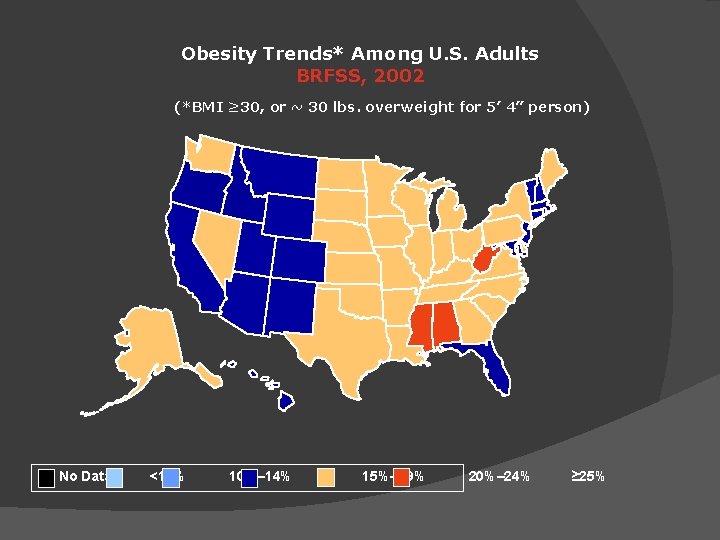
Obesity Trends* Among U. S. Adults BRFSS, 2002 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
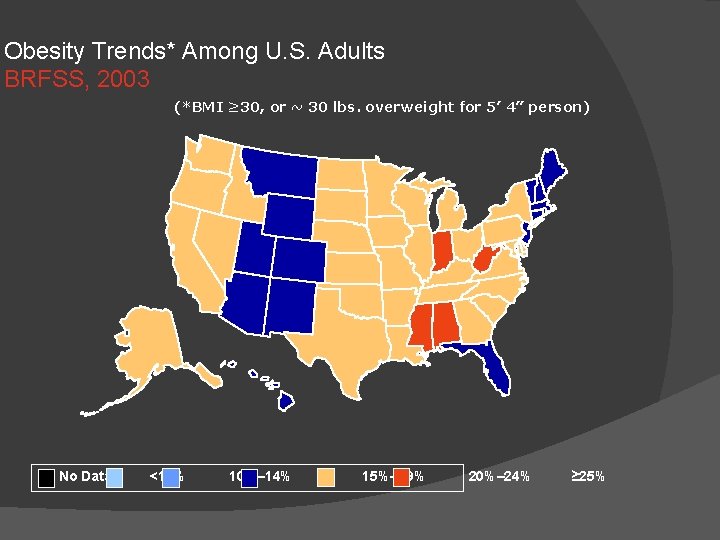
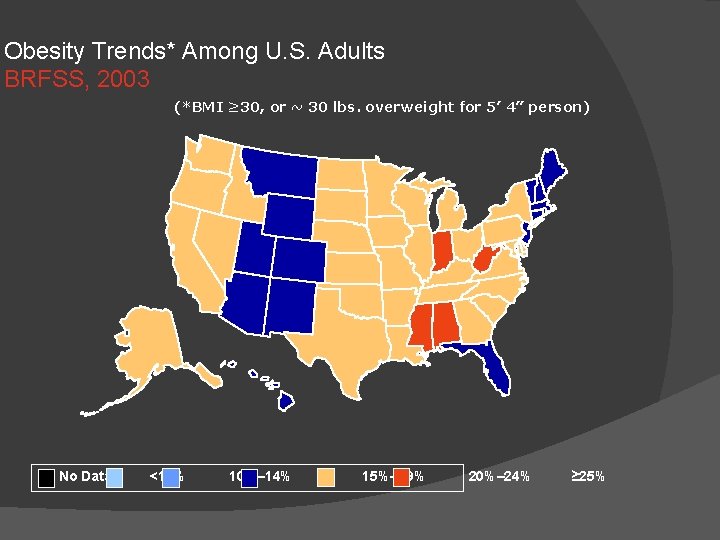
Obesity Trends* Among U. S. Adults BRFSS, 2003 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
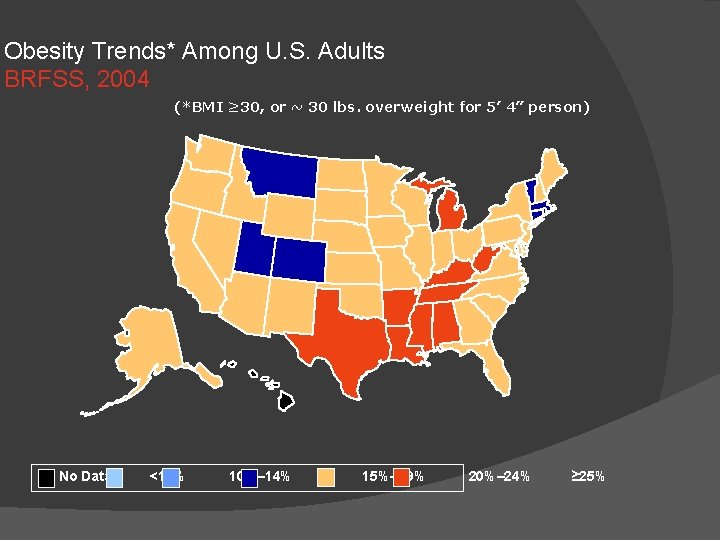
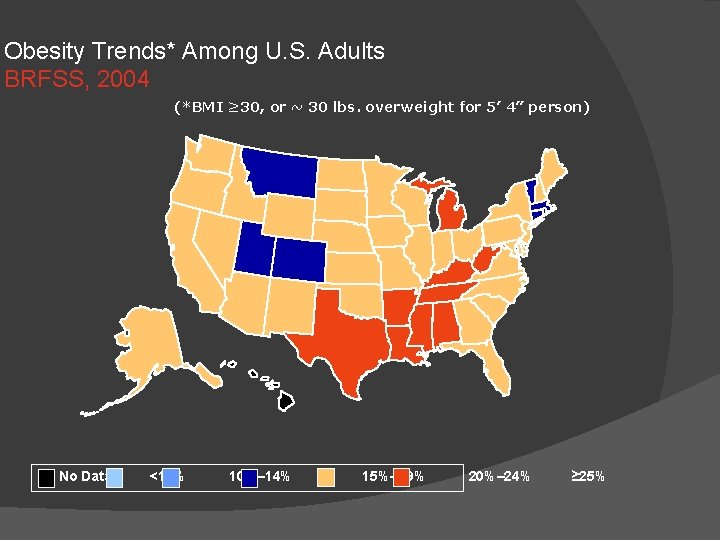
Obesity Trends* Among U. S. Adults BRFSS, 2004 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
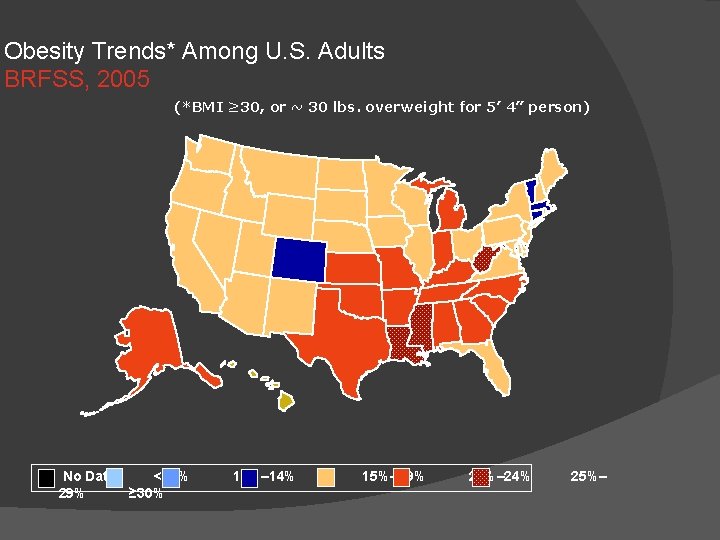
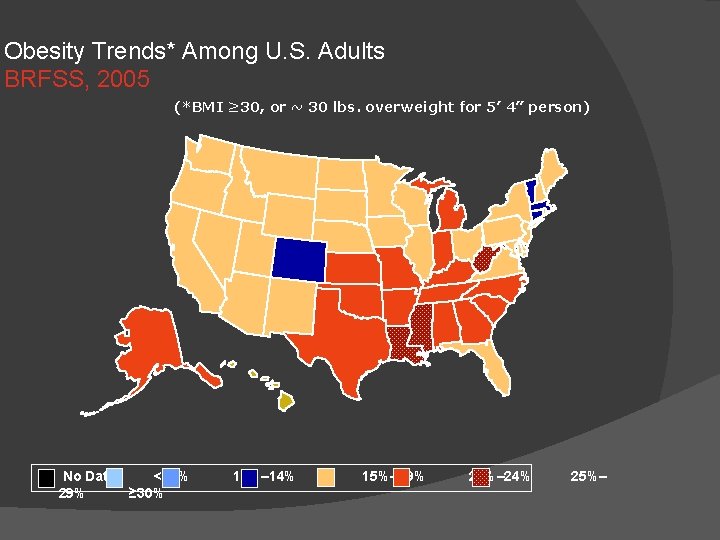
Obesity Trends* Among U. S. Adults BRFSS, 2005 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
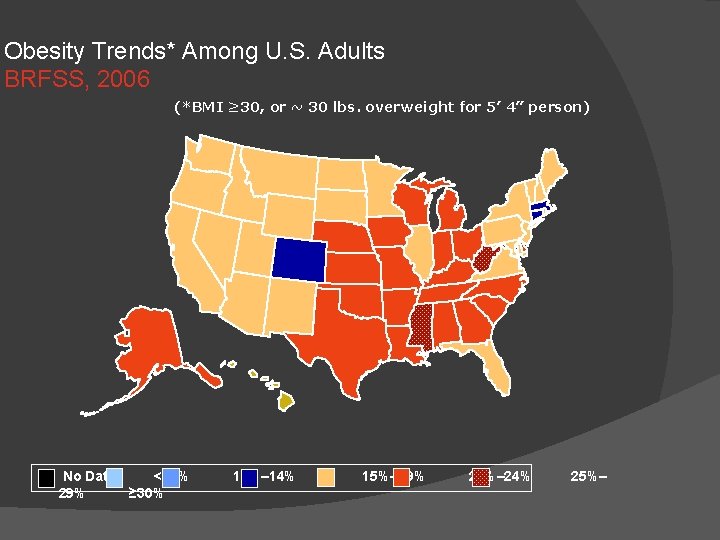
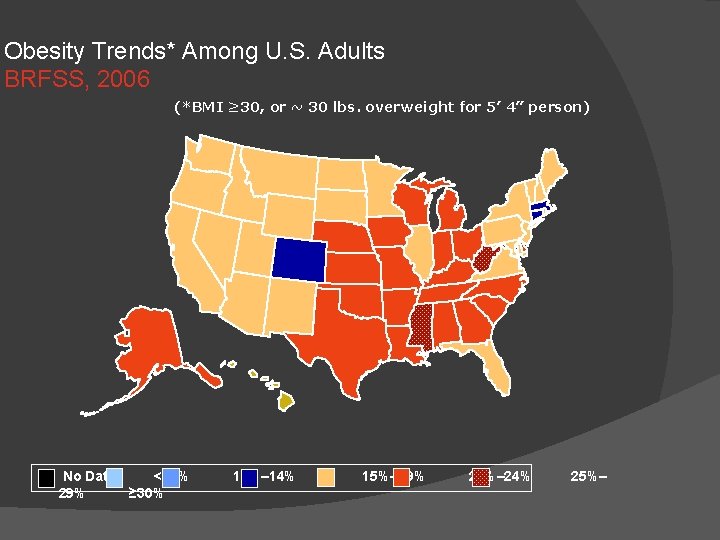
Obesity Trends* Among U. S. Adults BRFSS, 2006 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
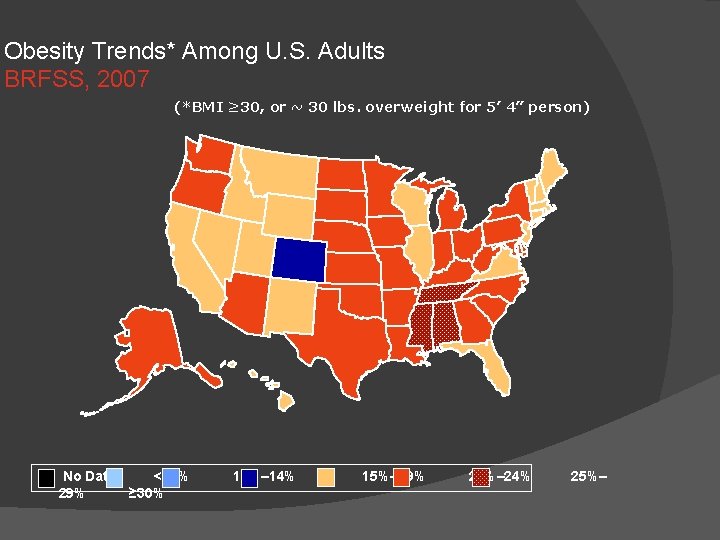
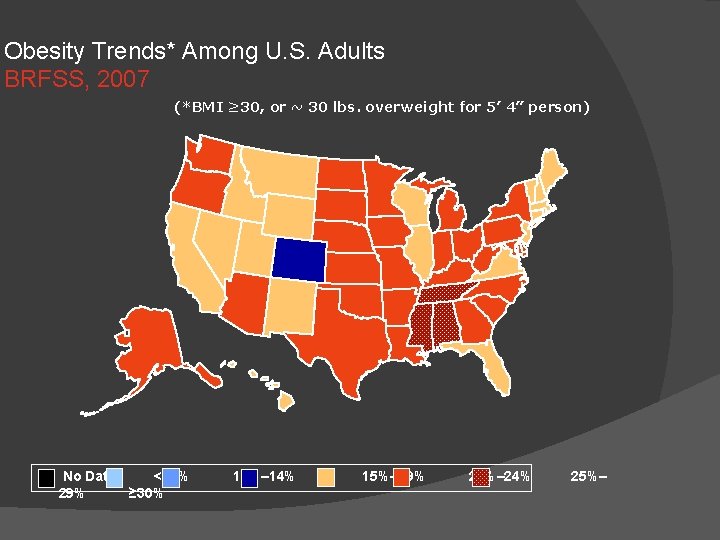
Obesity Trends* Among U. S. Adults BRFSS, 2007 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
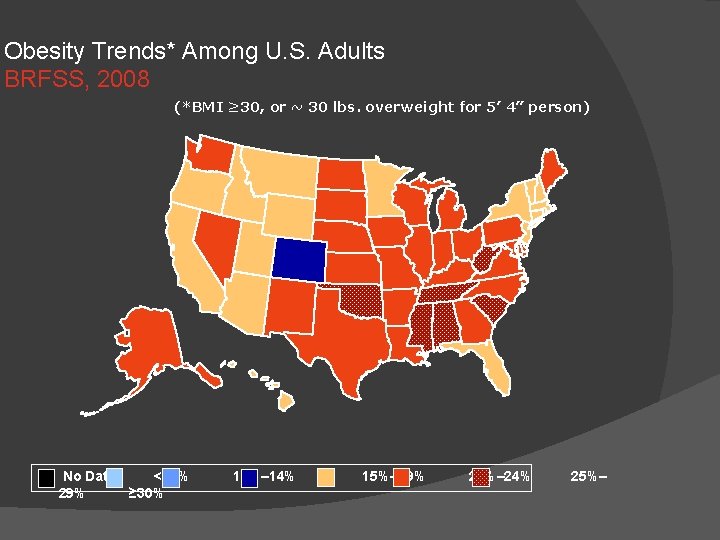
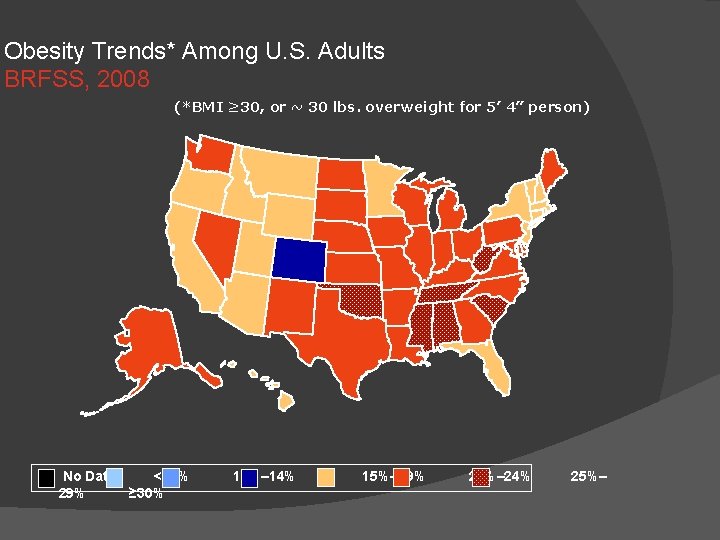
Obesity Trends* Among U. S. Adults BRFSS, 2008 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–

Obesity Trends* Among U. S. Adults BRFSS, 2009 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
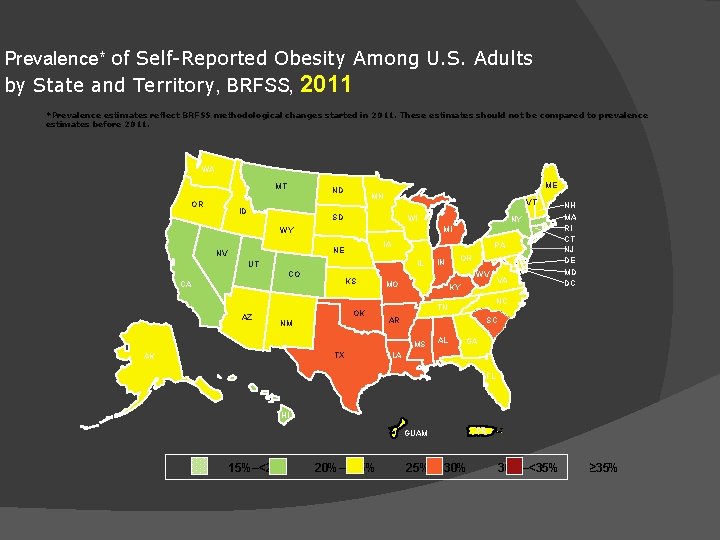
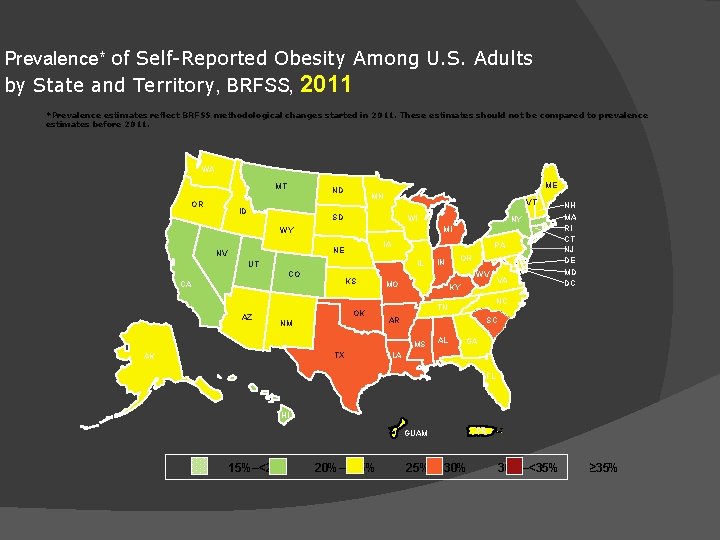
Prevalence* of Self-Reported Obesity Among U. S. Adults by State and Territory, BRFSS, 2011 *Prevalence estimates reflect BRFSS methodological changes started in 2011. These estimates should not be compared to prevalence estimates before 2011. WA MT OR ME ND ID MN VT SD WI IA NE NV PA IL UT CO KS CA AZ OK NM TX OH IN WV MO KY VA NC TN AR SC MS AK NY MI WY NH MA RI CT NJ DE MD DC AL GA LA FL HI GUAM 15%–<20% 20%–<25% 25%–<30% PR 30%–<35% ≥ 35%
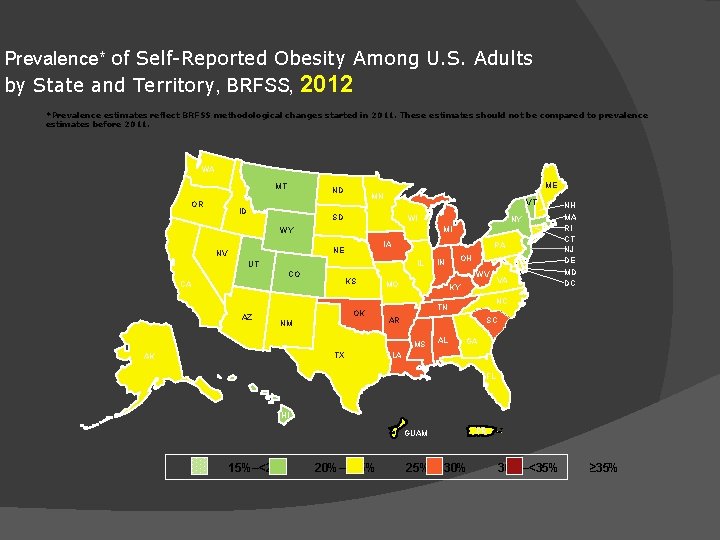
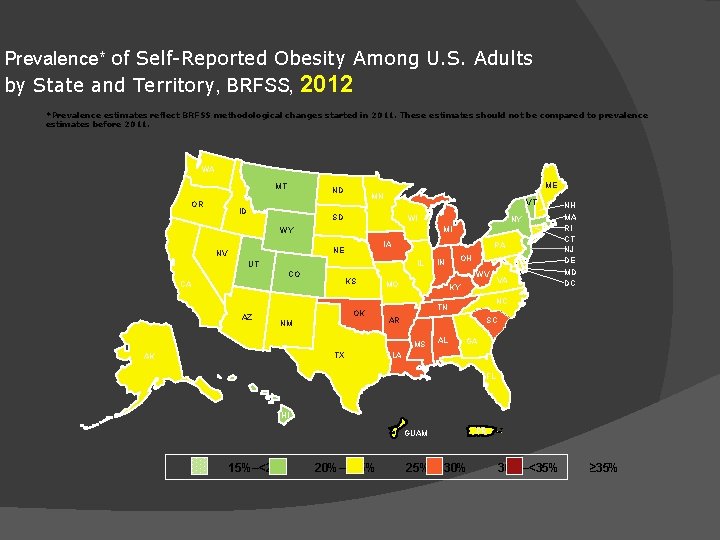
Prevalence* of Self-Reported Obesity Among U. S. Adults by State and Territory, BRFSS, 2012 *Prevalence estimates reflect BRFSS methodological changes started in 2011. These estimates should not be compared to prevalence estimates before 2011. WA MT OR ME ND ID MN VT SD WI IA NE NV PA IL UT CO KS CA AZ OK NM TX OH IN WV MO KY VA NC TN AR SC MS AK NY MI WY NH MA RI CT NJ DE MD DC AL GA LA FL HI GUAM 15%–<20% 20%–<25% 25%–<30% PR 30%–<35% ≥ 35%
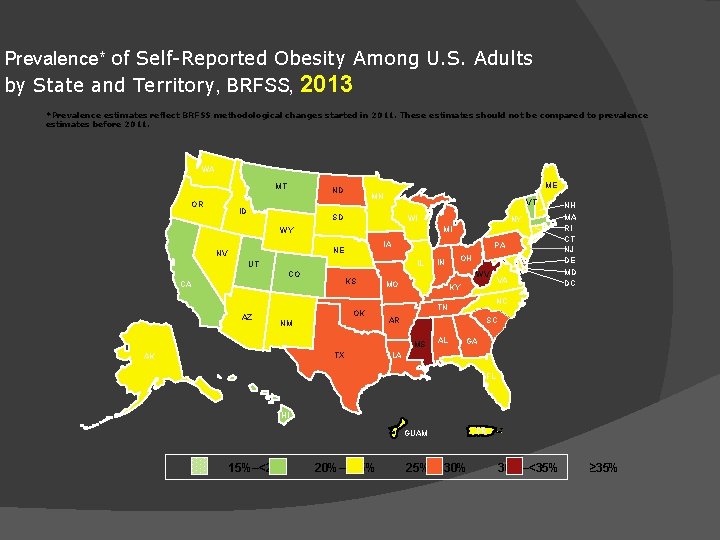
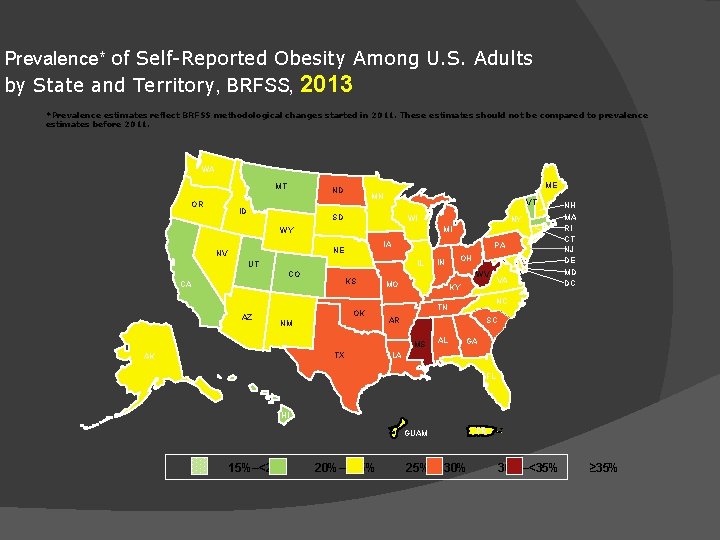
Prevalence* of Self-Reported Obesity Among U. S. Adults by State and Territory, BRFSS, 2013 *Prevalence estimates reflect BRFSS methodological changes started in 2011. These estimates should not be compared to prevalence estimates before 2011. WA MT OR ME ND ID MN VT SD WI IA NE NV PA IL UT CO KS CA AZ OK NM TX OH IN WV MO KY VA NC TN AR SC MS AK NY MI WY NH MA RI CT NJ DE MD DC AL GA LA FL HI GUAM 15%–<20% 20%–<25% 25%–<30% PR 30%–<35% ≥ 35%
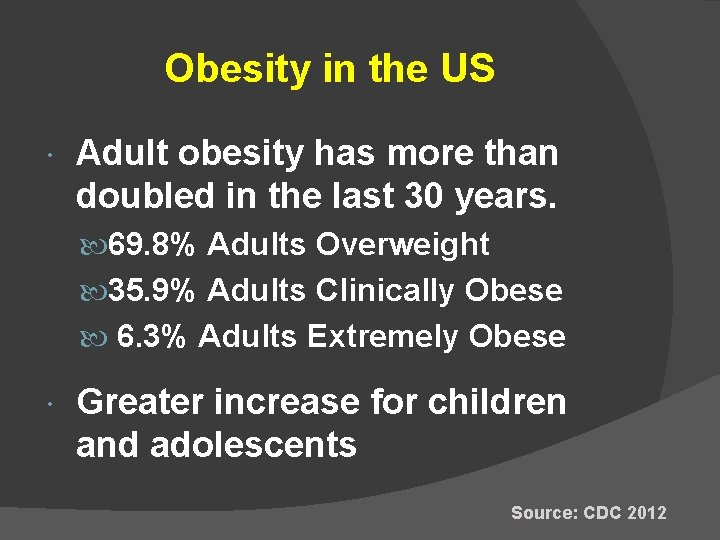
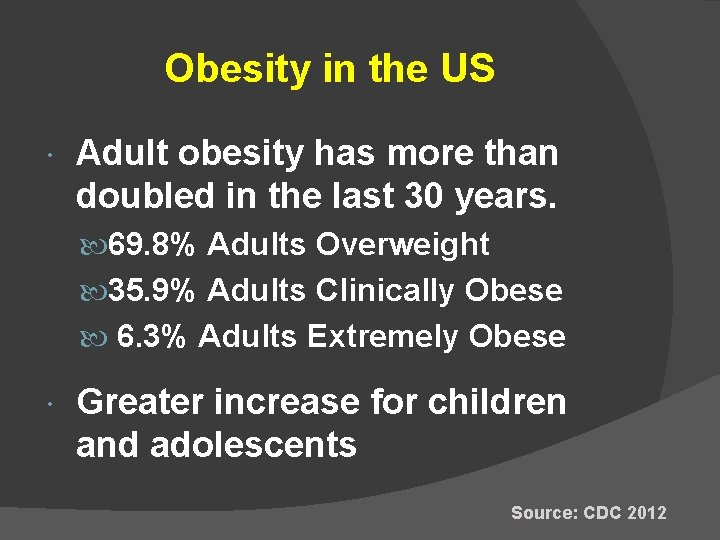
Obesity in the US Adult obesity has more than doubled in the last 30 years. 69. 8% Adults Overweight 35. 9% Adults Clinically Obese 6. 3% Adults Extremely Obese Greater increase for children and adolescents Source: CDC 2012
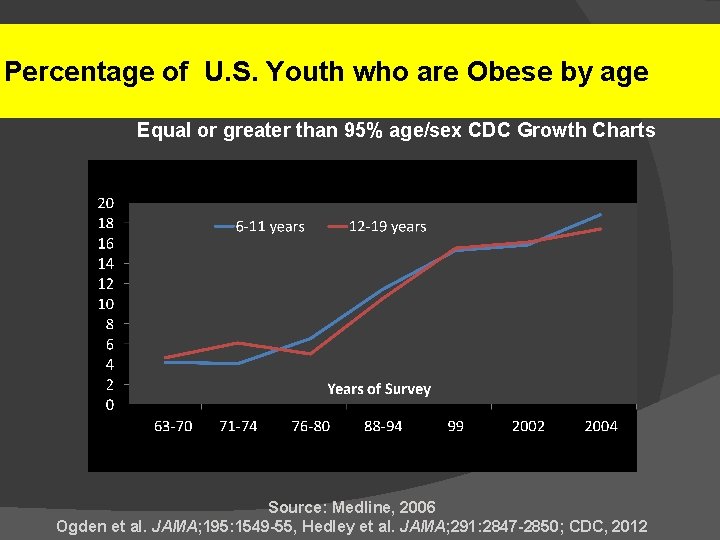
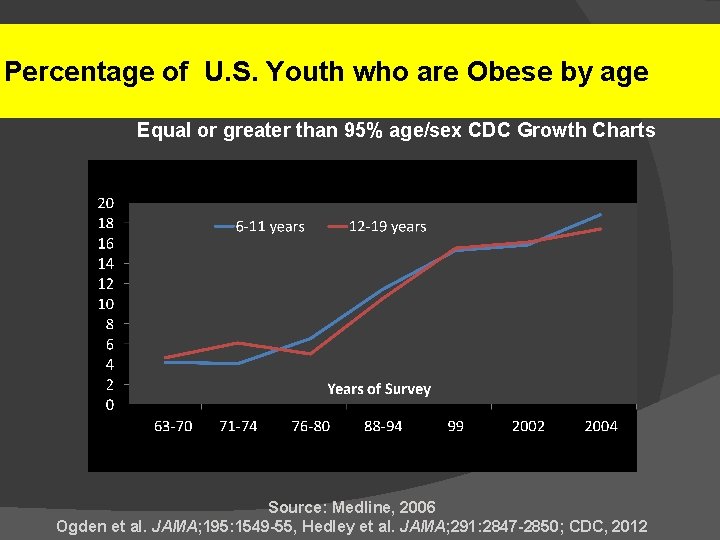
Percentage of U. S. Youth who are Obese by age Equal or greater than 95% age/sex CDC Growth Charts Source: Medline, 2006 Ogden et al. JAMA; 195: 1549 -55, Hedley et al. JAMA; 291: 2847 -2850; CDC, 2012
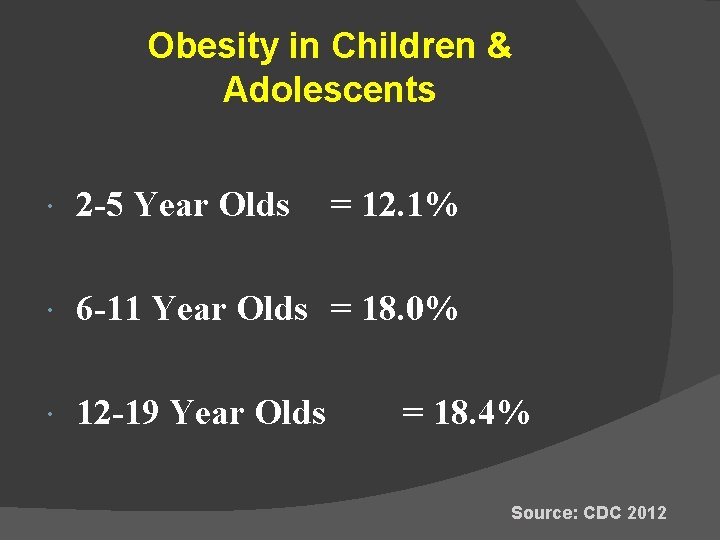
Obesity in Children & Adolescents 2 -5 Year Olds = 12. 1% 6 -11 Year Olds = 18. 0% 12 -19 Year Olds = 18. 4% Source: CDC 2012
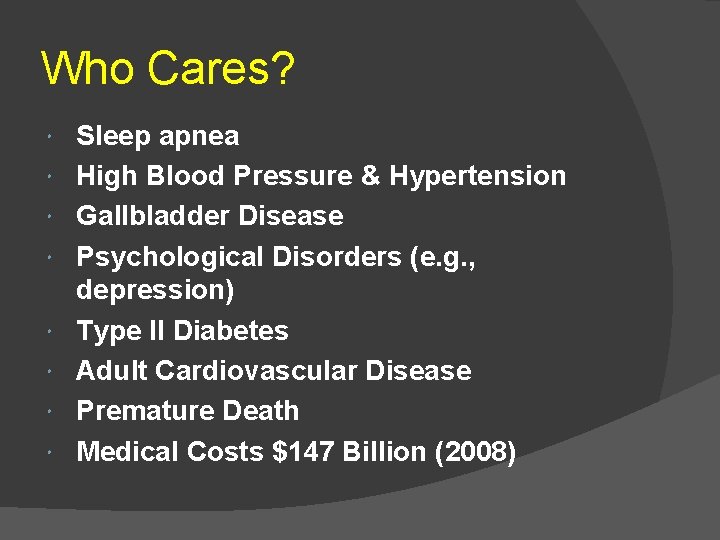
Who Cares? Sleep apnea High Blood Pressure & Hypertension Gallbladder Disease Psychological Disorders (e. g. , depression) Type II Diabetes Adult Cardiovascular Disease Premature Death Medical Costs $147 Billion (2008)
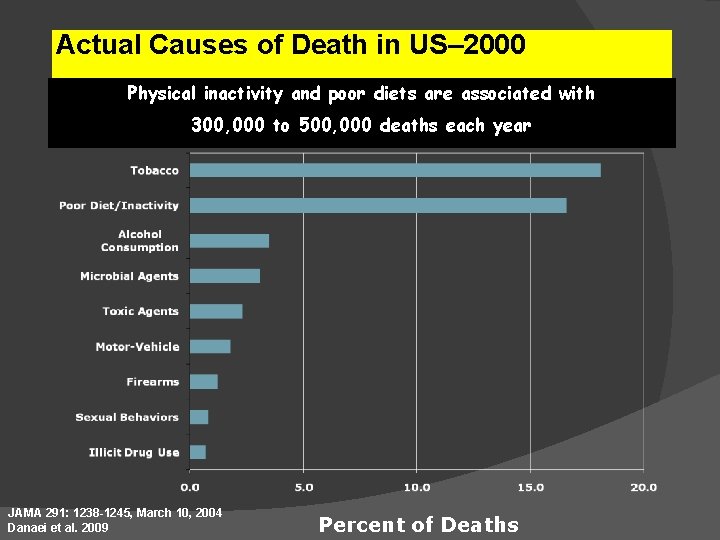
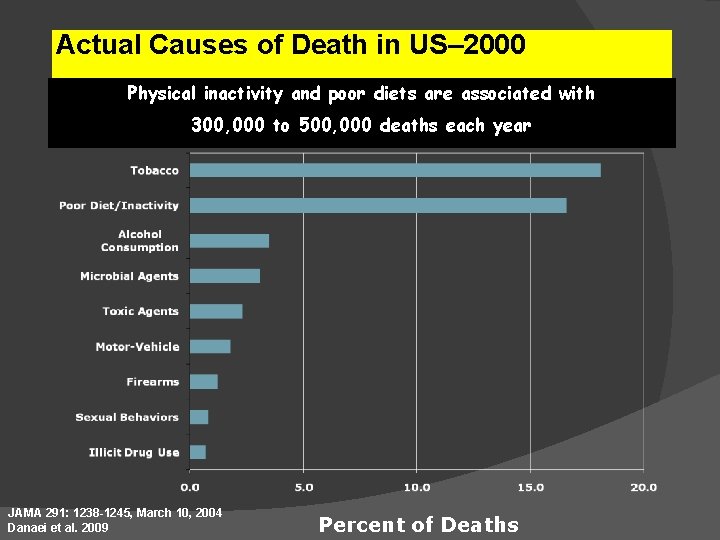
Actual Causes of Death in US– 2000 Physical inactivity and poor diets are associated with 300, 000 to 500, 000 deaths each year JAMA 291: 1238 -1245, March 10, 2004 Danaei et al. 2009 Percent of Deaths

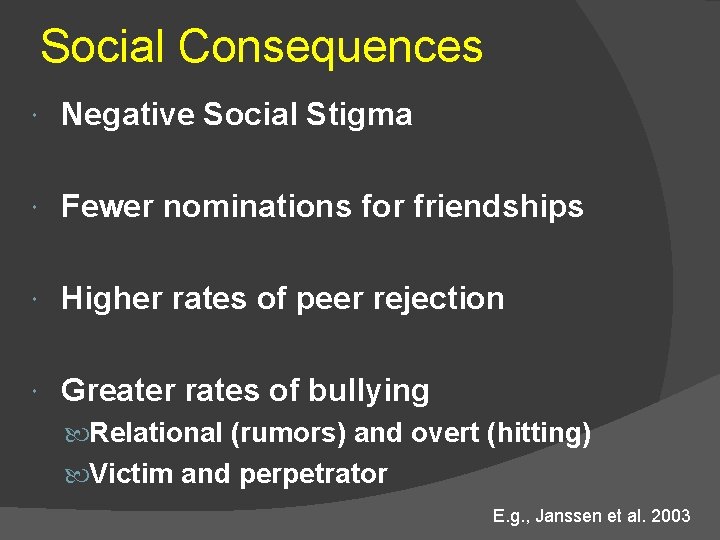
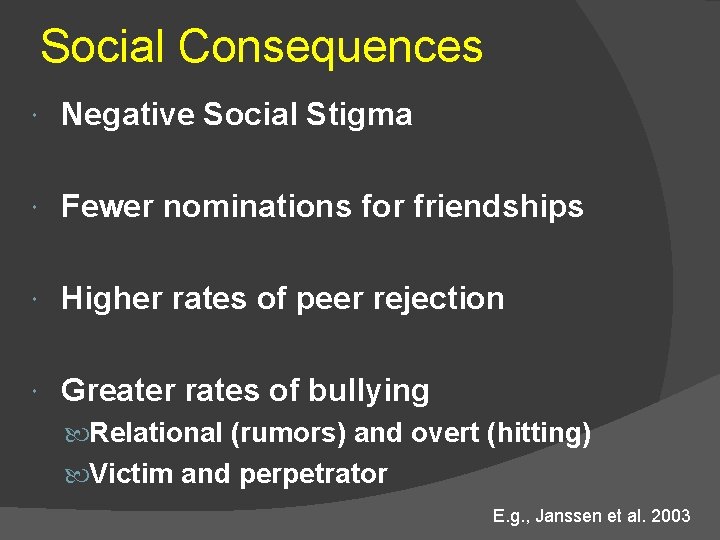
Social Consequences Negative Social Stigma Fewer nominations for friendships Higher rates of peer rejection Greater rates of bullying Relational (rumors) and overt (hitting) Victim and perpetrator E. g. , Janssen et al. 2003
Reasons for the Super. Sizing? Energy Input > Energy Output Hint: It’s not genes… Toxic Food Environment Sedentary Lifestyle
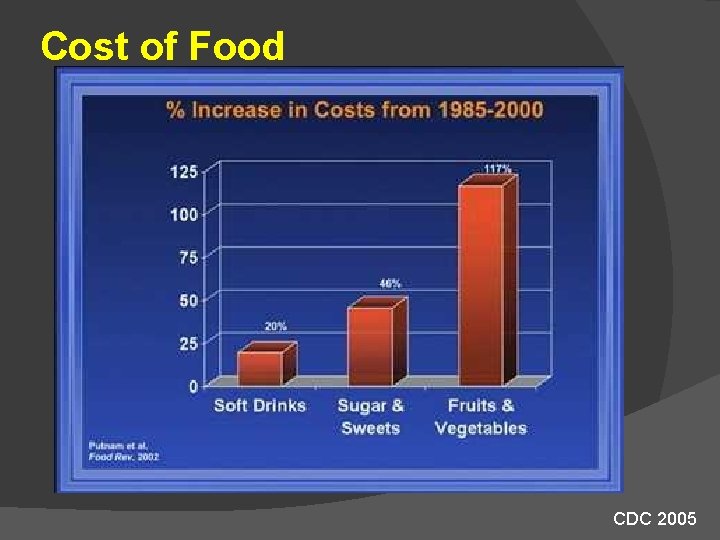
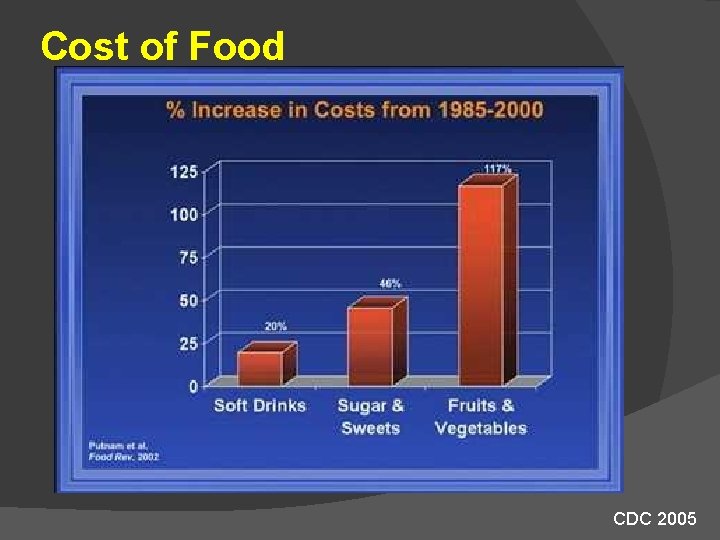
Cost of Food CDC 2005

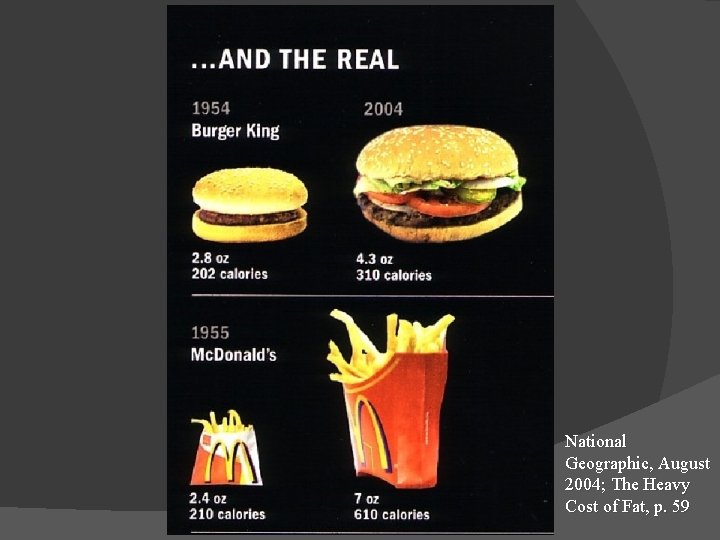
The American Landscape “Super Size Me” Fries = 640 cal. ; 29 g fat; 45% fat Big Mac = 549 cal. ; 29 g fat; 48% fat Coke (42 oz. ) = 540 calories Total = 1729 calories; 58 g fat
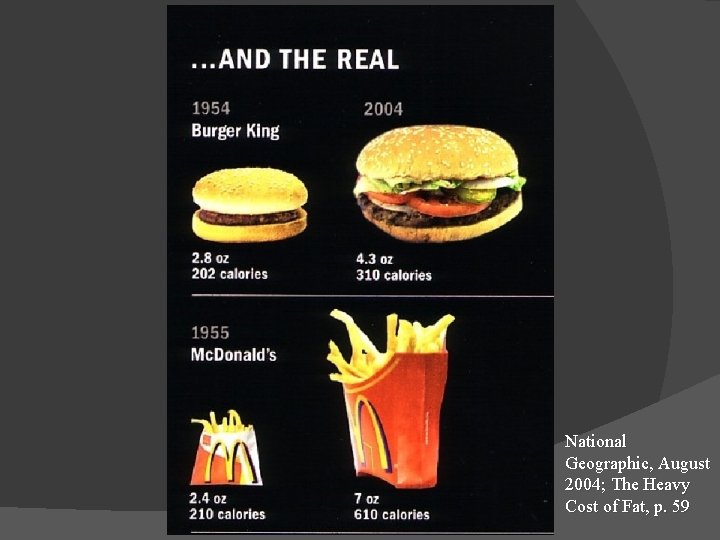
National Geographic, August 2004; The Heavy Cost of Fat, p. 59

Marketing and Media

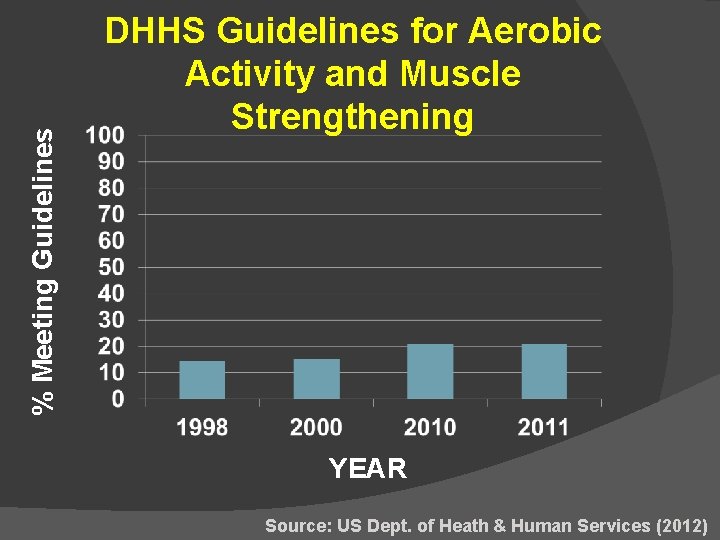
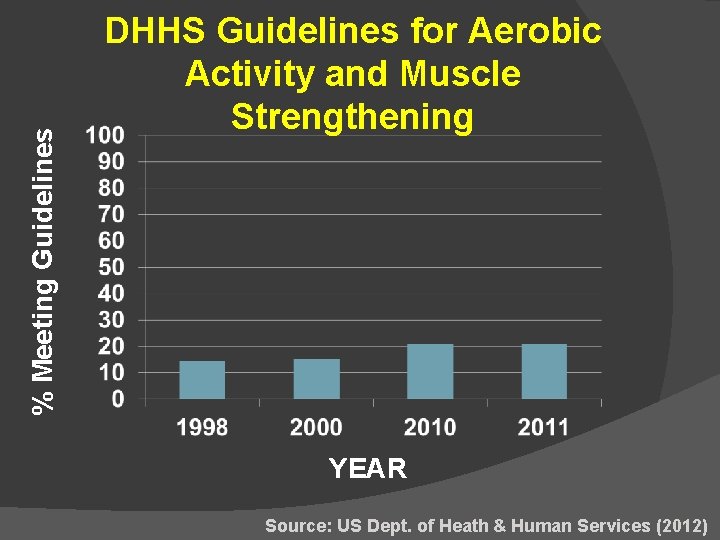
% Meeting Guidelines DHHS Guidelines for Aerobic Activity and Muscle Strengthening YEAR Source: US Dept. of Heath & Human Services (2012)
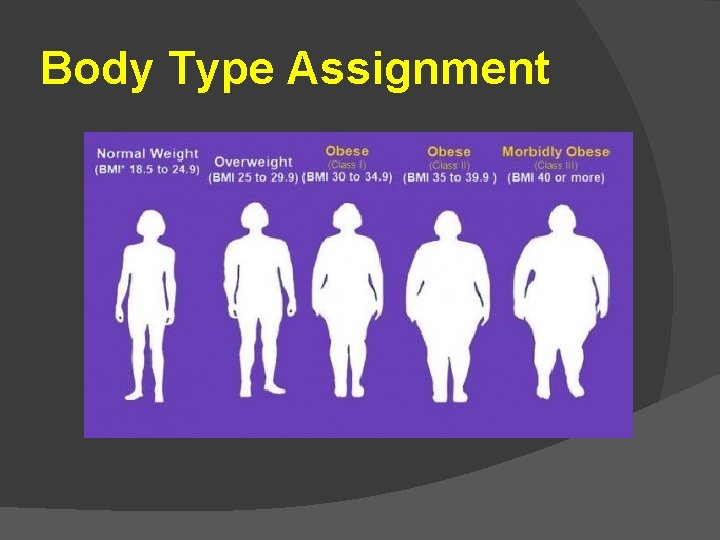
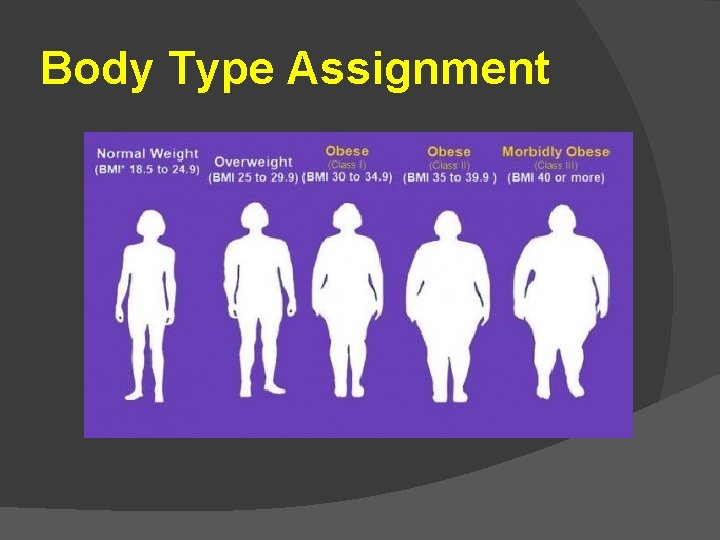
Body Type Assignment
Family-Based Solutions… Given the body types and messages… What Can Parents Do to Help Their Children Stay Healthy?
CDC State-Level Guidelines for Addressing Obesity 1) Address both nutrition and physical activity. 2) Change environments and policies that affect those behaviors (e. g. , access to supermarkets and areas facilitating physical activity). Work across multiple settings (e. g. , medical-care sites, school, worksites, and community organizations). 3) Change individual behaviors (e. g. , improved diet, greater consumption of fruits and vegetables as well).
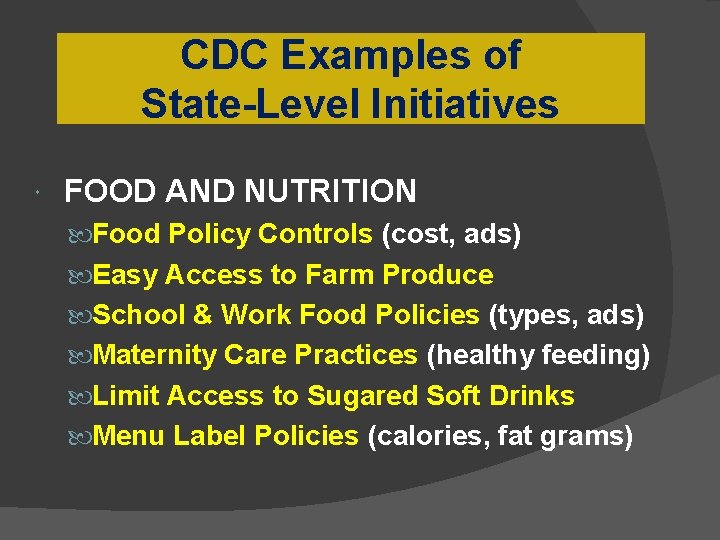
CDC Examples of State-Level Initiatives FOOD AND NUTRITION Food Policy Controls (cost, ads) Easy Access to Farm Produce School & Work Food Policies (types, ads) Maternity Care Practices (healthy feeding) Limit Access to Sugared Soft Drinks Menu Label Policies (calories, fat grams)
CDC Examples of State-Level Initiatives PHYSICAL ACTIVITY Community Design for Activity Active Transport to School (walk, bike) School-Based PE (regular, MVPA) Child Care Policies (food, exercise)
Children’s After-school Program Participation and the Development of BMI and Obesity
Why Should After-school Programs Affect BMI/Obesity? Controlled eating Opportunities for physical recreation and health education
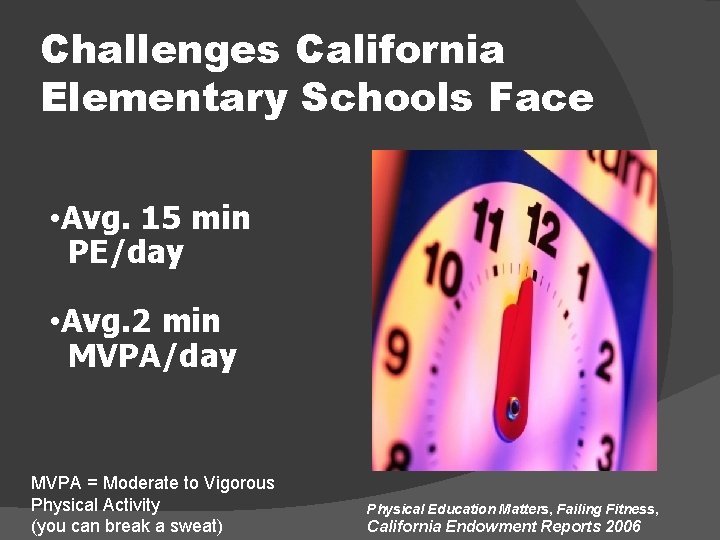
Challenges California Elementary Schools Face • Avg. 15 min PE/day • Avg. 2 min MVPA/day MVPA = Moderate to Vigorous Physical Activity (you can break a sweat) Physical Education Matters, Failing Fitness, California Endowment Reports 2006
Why Should After-school Programs Affect BMI/Obesity? Healthy Role Models Healthier Lifestyle More “palatable” than traditional treatments
Why Should After-school Programs Affect Peer Relations ASPs are Social Contexts Additional Time with Peers ○ Average 87 Days/Year (261 Hours/Year) ASP Context and Classroom are Socially Interdependent ASP Activities are Socially Valued
Study of Children’s After-School Time 4 -Year Longitudinal Study
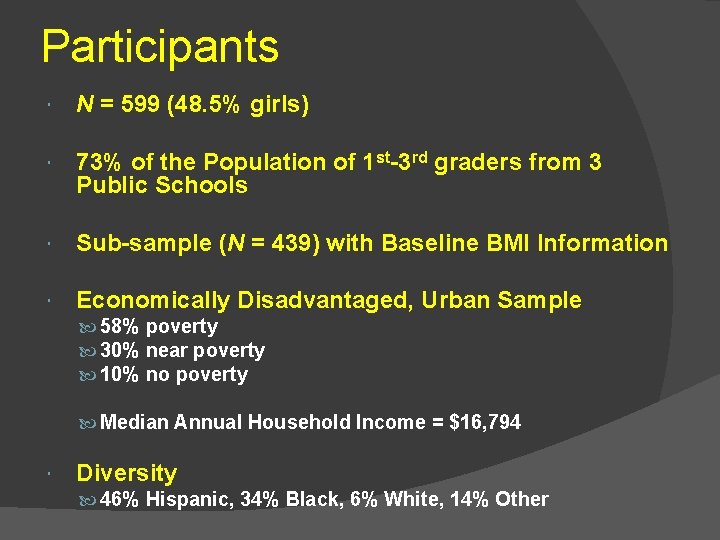
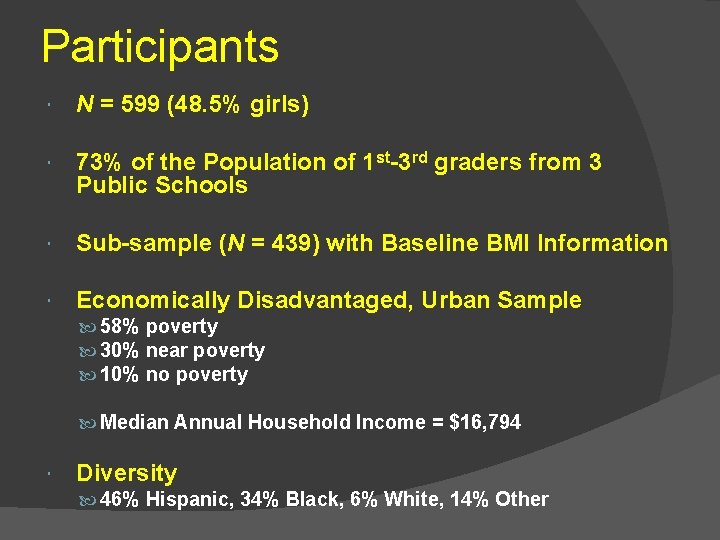
Participants N = 599 (48. 5% girls) 73% of the Population of 1 st-3 rd graders from 3 Public Schools Sub-sample (N = 439) with Baseline BMI Information Economically Disadvantaged, Urban Sample 58% poverty 30% near poverty 10% no poverty Median Annual Household Income = $16, 794 Diversity 46% Hispanic, 34% Black, 6% White, 14% Other
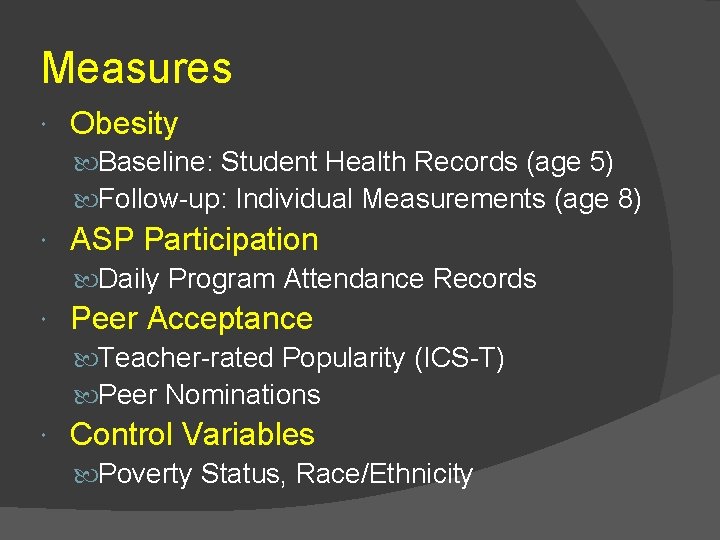
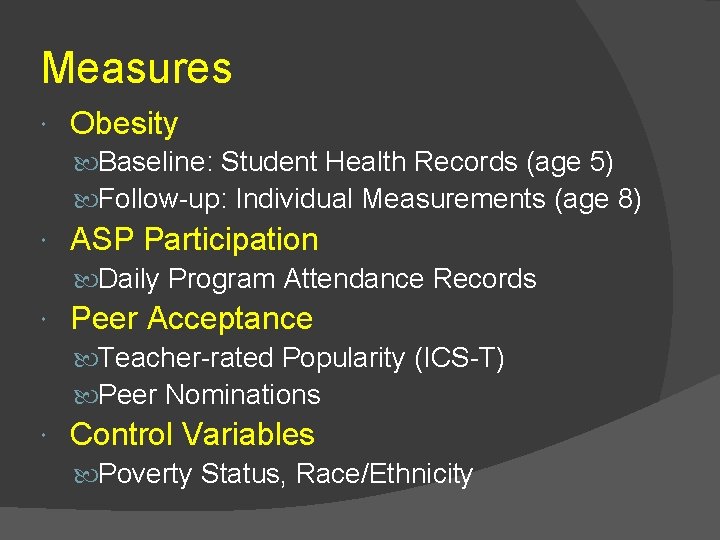
Measures Obesity Baseline: Student Health Records (age 5) Follow-up: Individual Measurements (age 8) ASP Participation Daily Program Attendance Records Peer Acceptance Teacher-rated Popularity (ICS-T) Peer Nominations Control Variables Poverty Status, Race/Ethnicity
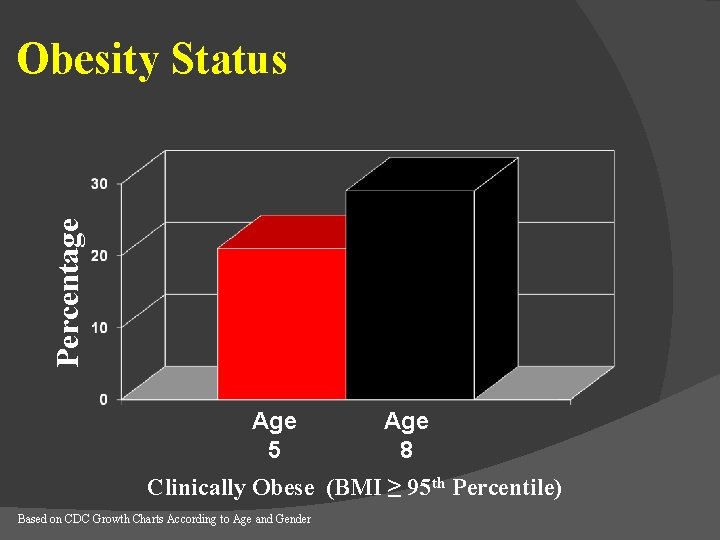
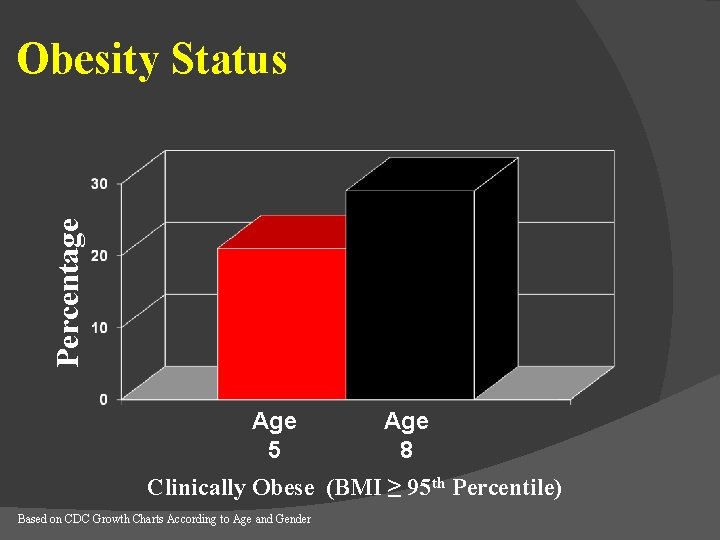
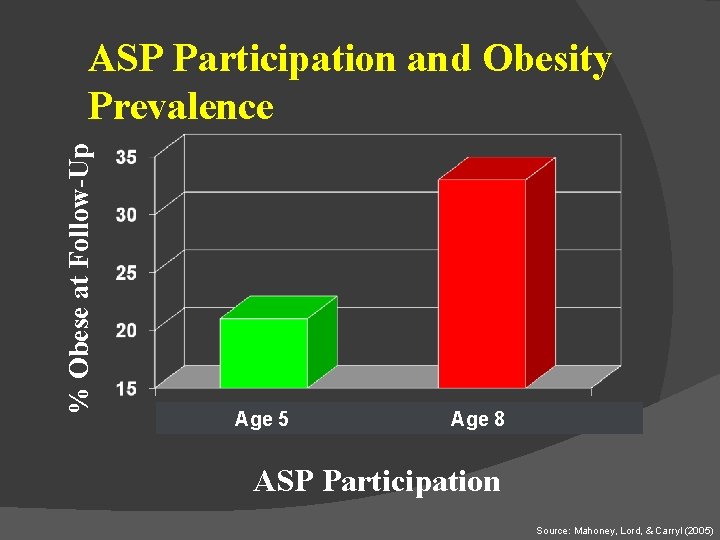
Percentage Obesity Status Age 5 Age 8 Clinically Obese (BMI ≥ 95 th Percentile) Based on CDC Growth Charts According to Age and Gender
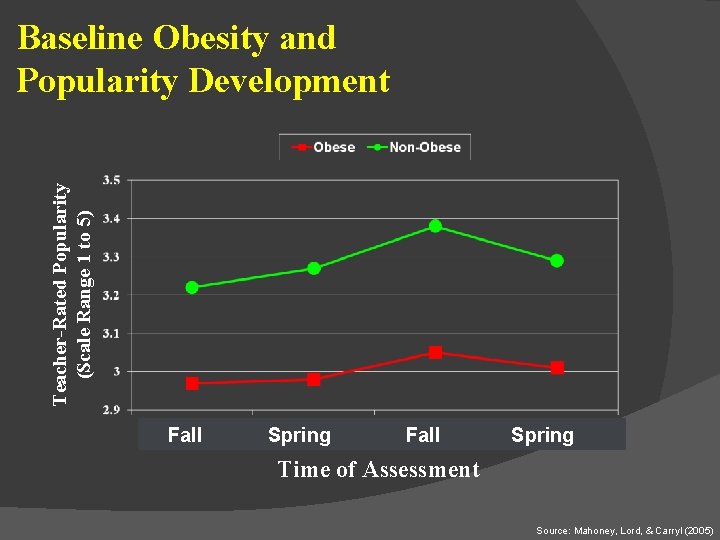
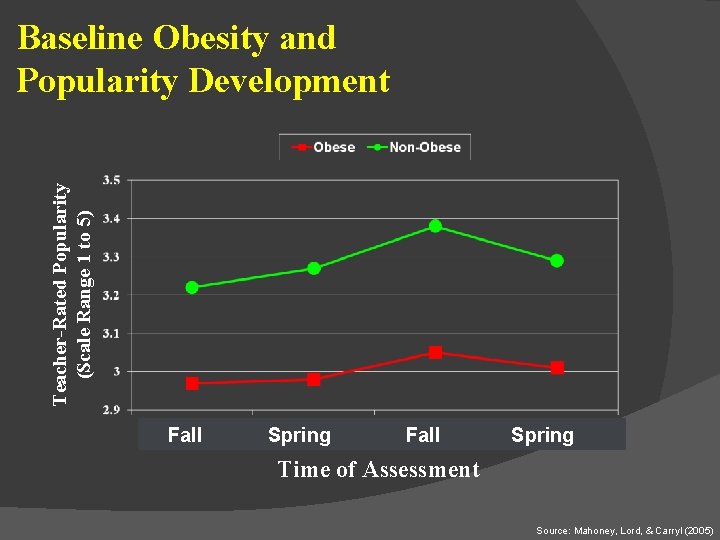
Teacher-Rated Popularity (Scale Range 1 to 5) Baseline Obesity and Popularity Development Fall Spring Time of Assessment Source: Mahoney, Lord, & Carryl (2005)
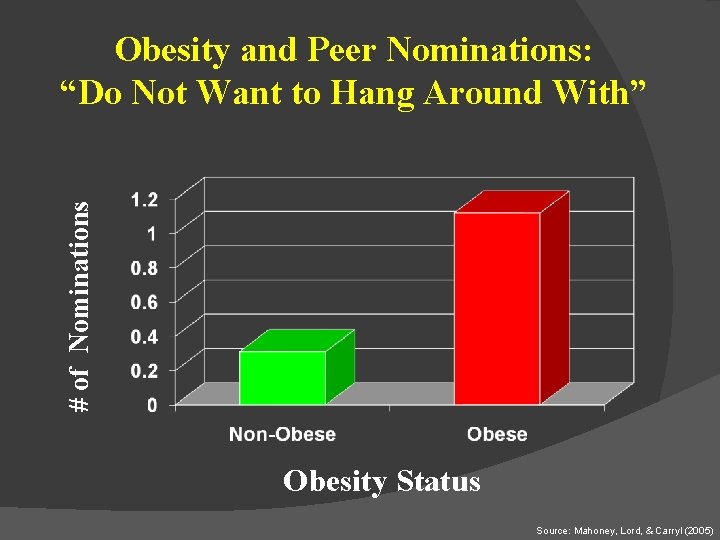
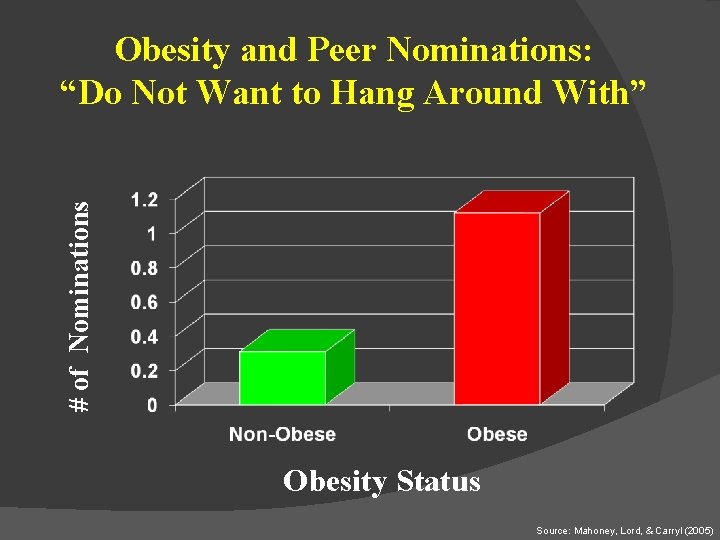
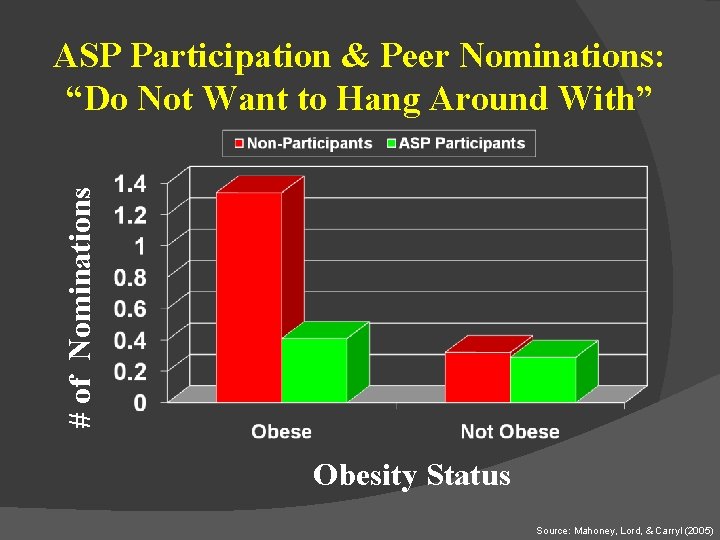
# of Nominations Obesity and Peer Nominations: “Do Not Want to Hang Around With” Obesity Status Source: Mahoney, Lord, & Carryl (2005)
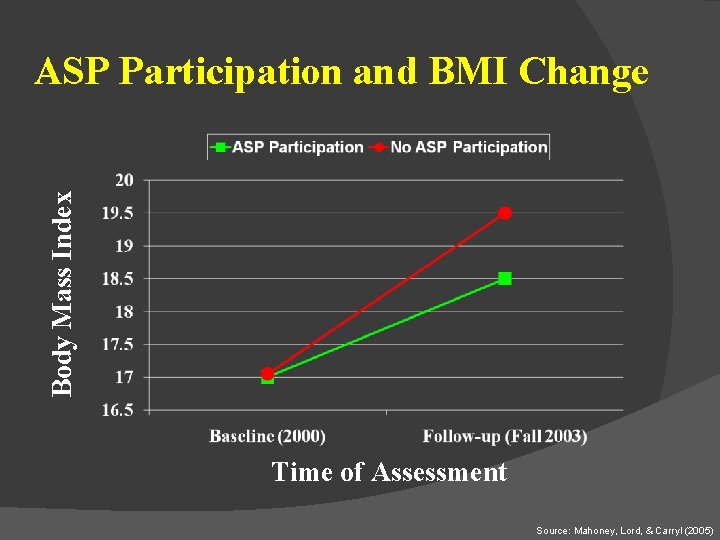
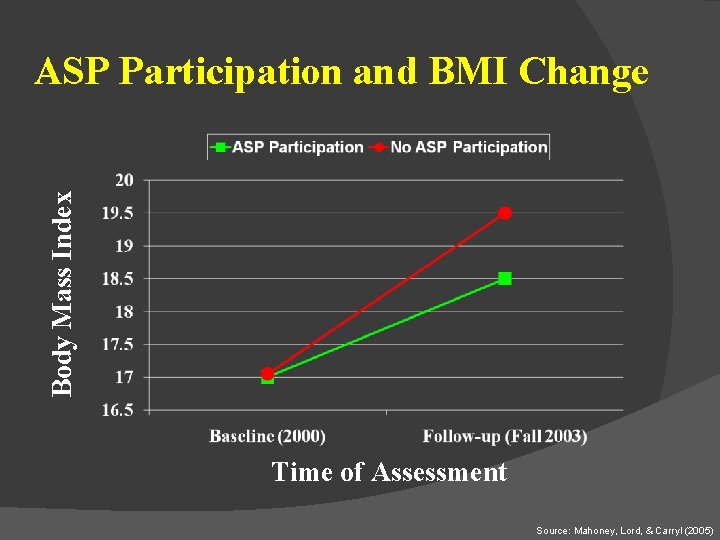
Body Mass Index ASP Participation and BMI Change Time of Assessment Source: Mahoney, Lord, & Carryl (2005)
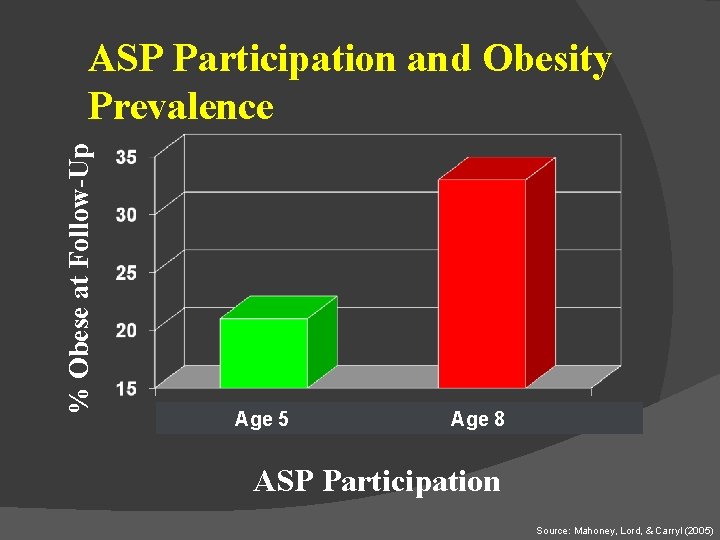
% Obese at Follow-Up ASP Participation and Obesity Prevalence Age 5 Age 8 ASP Participation Source: Mahoney, Lord, & Carryl (2005)
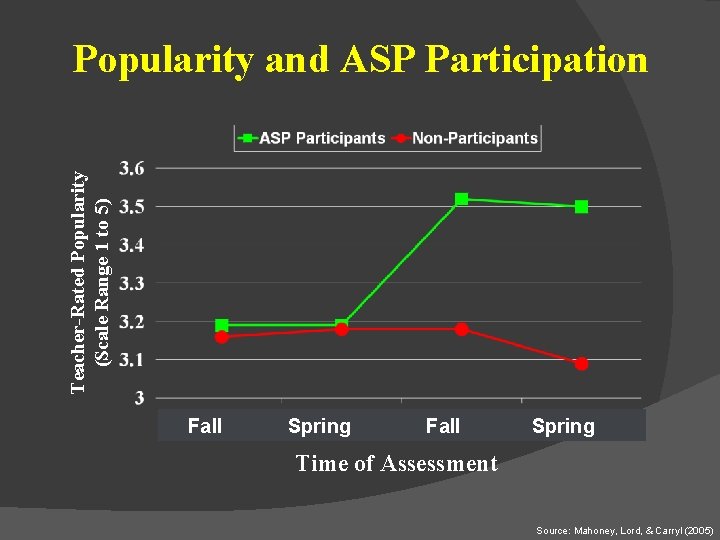
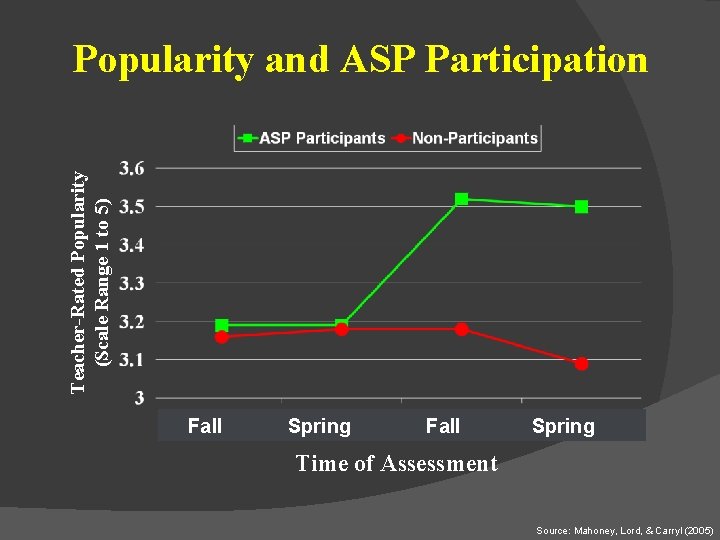
Teacher-Rated Popularity (Scale Range 1 to 5) Popularity and ASP Participation Fall Spring Time of Assessment Source: Mahoney, Lord, & Carryl (2005)
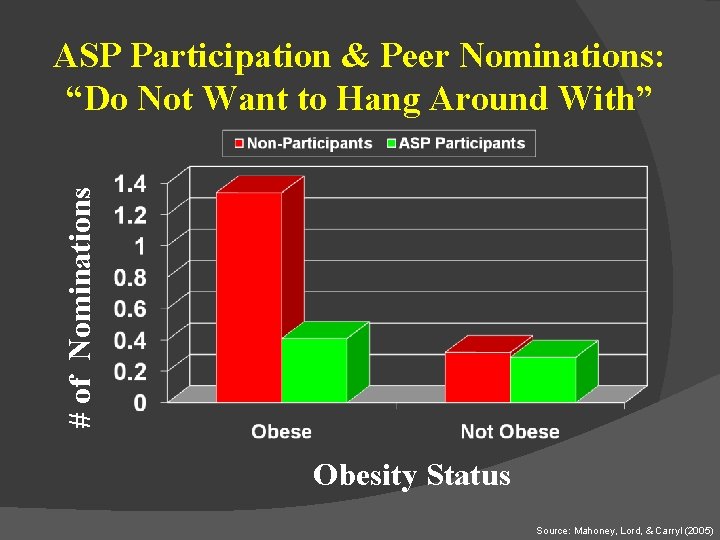
# of Nominations ASP Participation & Peer Nominations: “Do Not Want to Hang Around With” Obesity Status Source: Mahoney, Lord, & Carryl (2005)
Summary Child Obesity Prevalent and increasing Indicative of low peer acceptance over time Participation in After-school Programs Less marked increase in BMI Lower prevalence of obesity at follow-up Increased popularity Fewer negative peer nominations

Adolescent Summer Arrangements and the Development of Obesity
Why Focus on Summertime? Longest Consecutive Period of Out-of -school Time 23% of the Calendar Year Less than 1 in 10, 000 publications on summertime
Summertime Can Contribute to Obesity Not always a healthy time Summer weight gain for youth
Methodology: Sample PSID-CDS is Nationally Representative Subsample: N = 1766 Ages 10 -18 at Wave II (2002 -2003) Male 49% Race/Ethnicity ○ 62% White ○ 16% African American ○ 13% Hispanic or Latino
Regular Child Care Arrangements: Parent Interview “Now I'm going to ask you some questions about child care arrangements last summer. Please tell me which of these you used for _X_ on a regular basis during last summer”
Do Summer Care Arrangements Predict Subsequent Obesity? Parent Care Self Care Relative Care Organized Activities
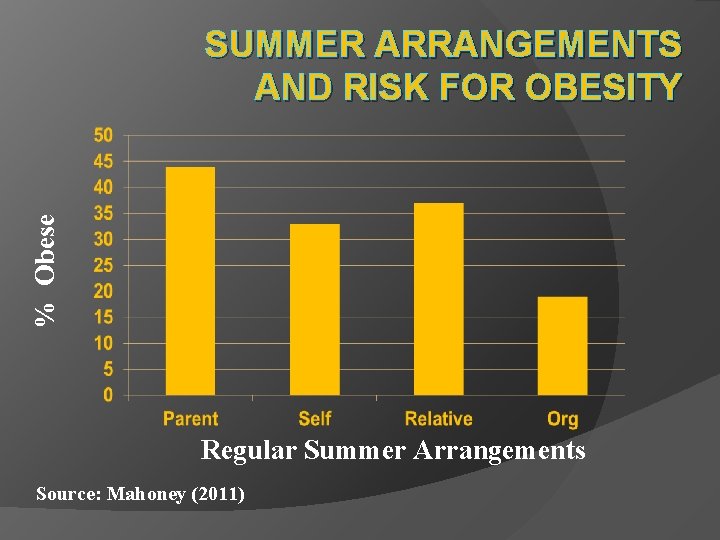
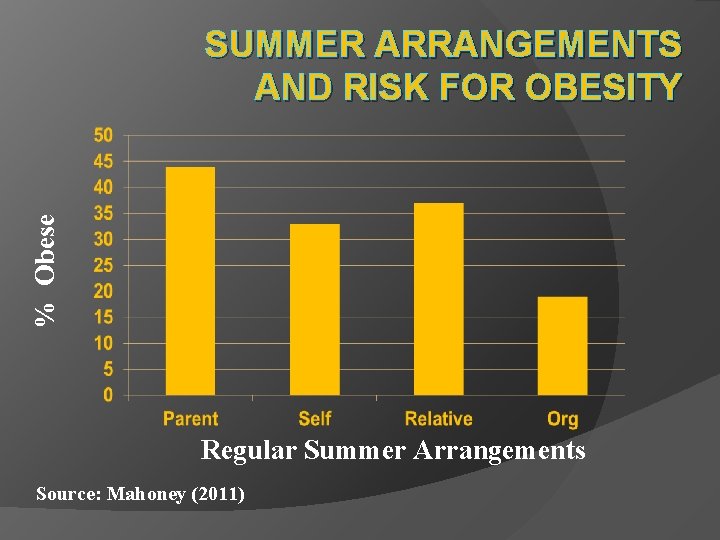
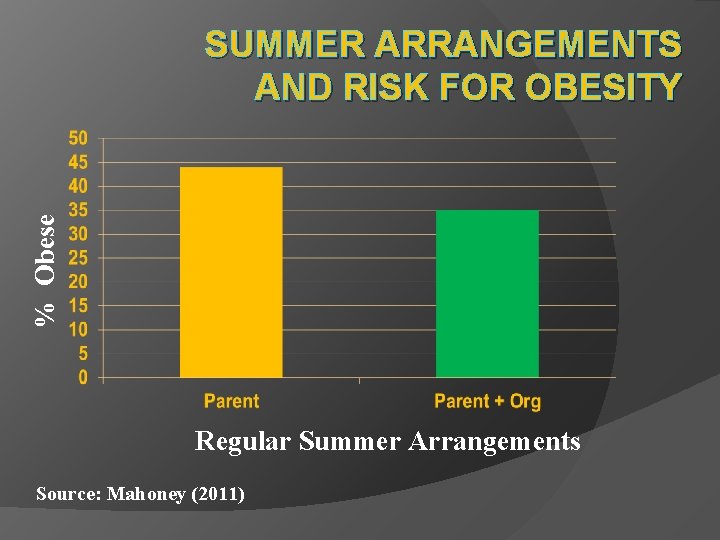
% Obese SUMMER ARRANGEMENTS AND RISK FOR OBESITY Regular Summer Arrangements Source: Mahoney (2011)
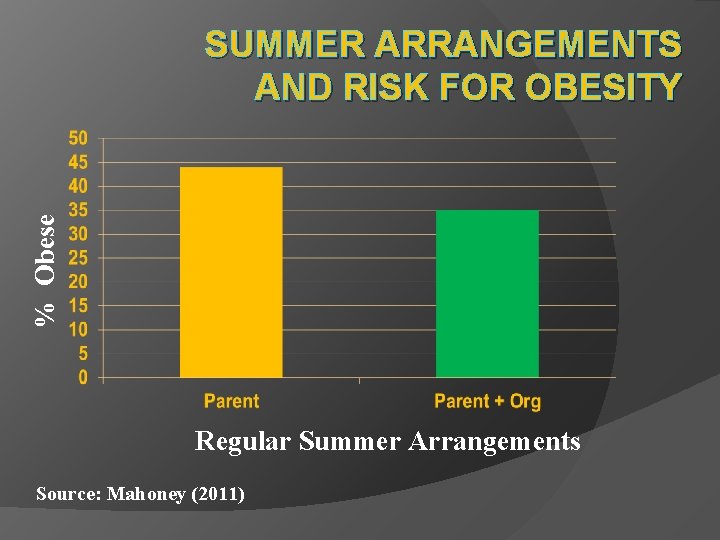
% Obese SUMMER ARRANGEMENTS AND RISK FOR OBESITY Regular Summer Arrangements Source: Mahoney (2011)
Summary Adolescent summertime arrangements are significantly associated with obesity Obesity highest for parent care Participation in summer activities predicts lower prevalence of obesity
Objectives Understand normative growth and activity during early childhood. Describe the historical progression of child obesity and several physical and social risks. Identify the key factors contributing to the child obesity epidemic and give examples. Describe the role of social learning in children’s beliefs about body types. Discuss several potential solutions to preventing or reducing child obesity.
 Small intestinal bacterial overgrowth
Small intestinal bacterial overgrowth Euro psy
Euro psy Ucf online psychology degree
Ucf online psychology degree Psy 2055
Psy 2055 Psy 2055
Psy 2055 Psy2055
Psy2055 Psy
Psy Psy sanin
Psy sanin Psy
Psy Psy
Psy Psy
Psy Psy
Psy Psy 226
Psy 226 Psy
Psy Psy academy
Psy academy Nukleus caudatus
Nukleus caudatus Psy walsh
Psy walsh Pes charakteristika
Pes charakteristika Bradla sklonovanie
Bradla sklonovanie 11 psy
11 psy Regression psy
Regression psy Psy
Psy Psy 335 purdue
Psy 335 purdue Growth analysis definition
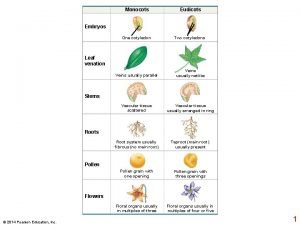
Growth analysis definition Primary growth and secondary growth in plants
Primary growth and secondary growth in plants Primary growth and secondary growth in plants
Primary growth and secondary growth in plants Vascular ray
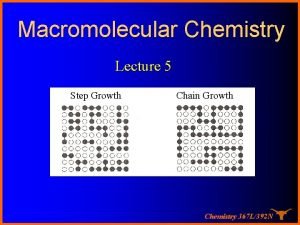
Vascular ray Growthchain
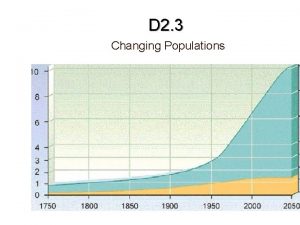
Growthchain Geometric growth graph
Geometric growth graph Neoclassical growth theory vs. endogenous growth theory
Neoclassical growth theory vs. endogenous growth theory Organic vs inorganic growth
Organic vs inorganic growth Crumpled reminder activity
Crumpled reminder activity Activity coefficient
Activity coefficient Reactants, products, and leftovers
Reactants, products, and leftovers Aoa vs aon
Aoa vs aon Activity 1 introductory activity
Activity 1 introductory activity Activity 1 activity 2
Activity 1 activity 2 Activity 2
Activity 2 3
3 Stages of human growth and development pictures
Stages of human growth and development pictures St. marys county land use and zoning lawyer
St. marys county land use and zoning lawyer Interest rates and economic growth
Interest rates and economic growth Theory of growth and development
Theory of growth and development Human growth and development
Human growth and development Tillering stage of rice
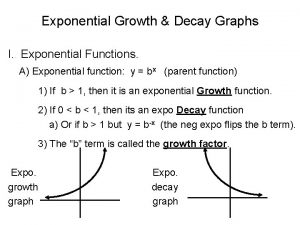
Tillering stage of rice Exponential growth vs decay
Exponential growth vs decay Late childhood mental development
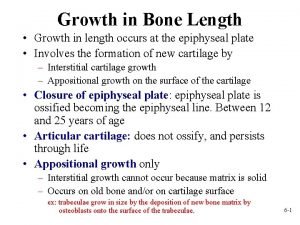
Late childhood mental development Appositional and interstitial growth of cartilage
Appositional and interstitial growth of cartilage Pretest growth development and sexuality
Pretest growth development and sexuality Development and maturation
Development and maturation Stages of development and growth
Stages of development and growth 6 life stages
6 life stages Half life examples science
Half life examples science How to know if its exponential growth or decay
How to know if its exponential growth or decay Exponential growth function
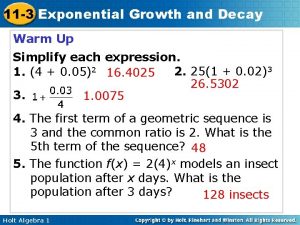
Exponential growth function Exponential growth and decay algebra 1
Exponential growth and decay algebra 1 Growth or decay exponential
Growth or decay exponential Growth and decay exponential functions
Growth and decay exponential functions Exponential decay function
Exponential decay function Conclusion of growth and development
Conclusion of growth and development Ppst domain 7
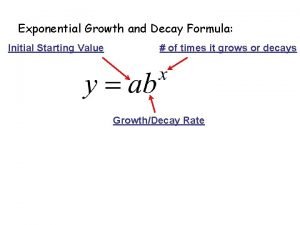
Ppst domain 7 Example of exponential growth equation
Example of exponential growth equation Describe a normal healthy nail
Describe a normal healthy nail Milady nail structure and growth
Milady nail structure and growth Interstitial and appositional growth of cartilage
Interstitial and appositional growth of cartilage An embryonic industry is one that
An embryonic industry is one that Money growth formula
Money growth formula Intensive integrative and diversification growth strategies
Intensive integrative and diversification growth strategies Copyright
Copyright Section 8-2 cell division
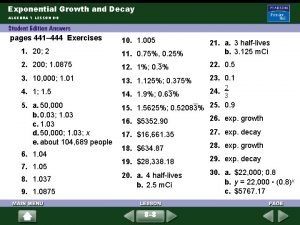
Section 8-2 cell division 9-3 exponential growth and decay
9-3 exponential growth and decay 7-7 exponential growth and decay
7-7 exponential growth and decay Growth and decay exponential functions
Growth and decay exponential functions 7-1 exponential functions growth and decay
7-1 exponential functions growth and decay Exponential growth and carrying capacity
Exponential growth and carrying capacity What is the difference between growth and decay
What is the difference between growth and decay Exponential growth and decay formula
Exponential growth and decay formula Compare linear, exponential, and quadratic growth
Compare linear, exponential, and quadratic growth Chapter 11 growth and expansion
Chapter 11 growth and expansion Customer perspective examples
Customer perspective examples