Cancer Difficult to Define Classic definition tissue overgrowth



- Slides: 38
Cancer
Difficult to Define • Classic definition: tissue overgrowth which is independent of the laws governing the remainder of the body. Serves no purpose to the body. • Tumor – Original definition: mass greater than 2 cm – Neoplasm • Not all are cancer • Malignant vs. benign
Tumors • Benign – – – Grow slowly Well-defined capsule Are not invasive Well differentiated Low mitotic index Do not metastatize • Malignant – – Grow rapidly Not encapsulated Invade local tissue Anaplasia: poorly differentiated – High mitotic index – Metastasis (secondary tumor)
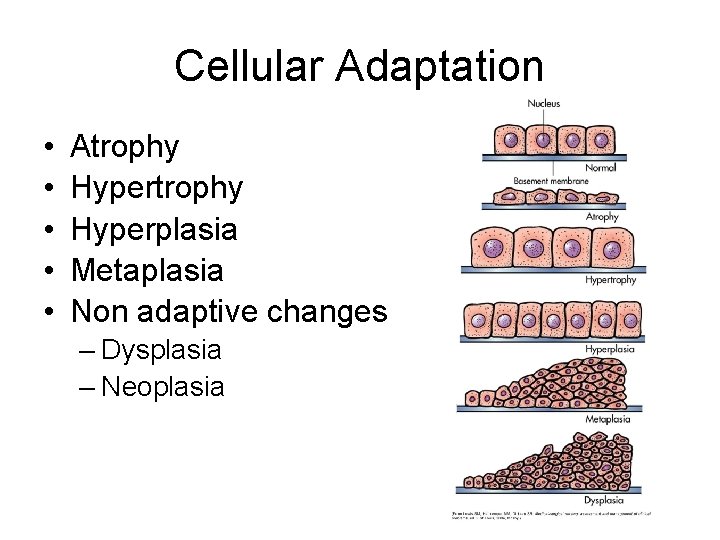
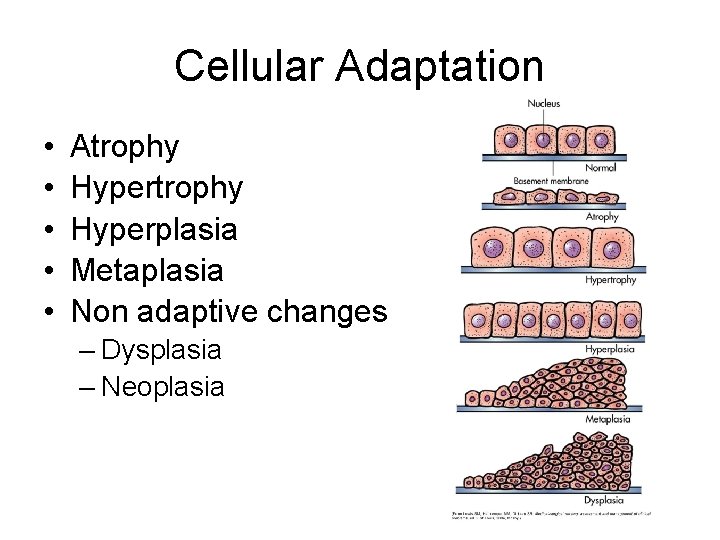
Cellular Adaptation • • • Atrophy Hyperplasia Metaplasia Non adaptive changes – Dysplasia – Neoplasia

Naming Cancers – Carcinoma: epithelial cells – Adenocarcinoma: glandular tissue – Sarcoma: connective tissue – Lymphoma: lymph tissue – Leukemia: blood forming tissue (marrow) – Fibroma – Osteoma – Chondroma
Tumor Markers • Chemicals produced by cancer cells – May be present in blood, CSF, or tumor cell membranes – Usually similar or same as tissues that gave rise to tumor or fetal proteins from that tissue • • • Pheochromocytoma: epinephrine Prostate cancer: prostate specific antigen (PSA) Liver cancer: alpha fetoprotein (AFP) CEA: GI tract cancers CA-124: ovarian cancers – Can be used to screen for cancer or measure success of treatment
Hallmarks of Cancer • • • Self-sufficiency in growth signals Insensitivity to antigrowth signals Evading apoptosis Limitless replicative potential Sustained angiogenesis Tissue invasion and metastasis
Carcinogenesis • Genetic – Protooncogenes – Tumor suppressor genes – Apoptosis genes – DNA repair genes • Stages – Initiation: mutation – Promotion: increased cell growth – Progression: invasiveness, angiogenesis
Protooncogenes • Vulnerable genes – Mutation causes oncogenes – New or inherited • Mutations – Point – Gene amplification – Chromosomal Rearrangement – Viral Insertion – HPV, HCV, EBV
Telomeres • End cap of chromosomes • Aging causes loss of telomere • Telomerase in germ cells (embryonic)
Factors in Cancer Development • • • Inflammation Family history: 2 possibilities Viruses Bacteria: H. pylori Environmental factors
Environmental Factors • • • Tobacco use Ionizing radiation UV radiation ETOH consumption Sexual and reproductive behavior Physical activity Occupational Air pollution EMFs Stress Diet
Cancer Mets and Staging • Common mets sites: BBLL – Brain – Bones – Liver – Lungs • Staging systems (various): carcinoma – Stage 1: confined to organ – Stage 2: locally invasive – Stage 3: lymph node invasion – Stage 4: spread to distant sites
Neoplasm-Host Interaction • Cosmetic • Tissue Compression or destruction – Ischemia – Altered or impaired function • • Increased Metabolic Demand – Cachexia Blood Supply Growth factors Immune Response
Clinical Manifestations • Pain: usually in late stage – Fear, anxiety, sleep, fatigue, culture – Likely caused by cytokine action on C/PNS • Fatigue • Cachexia (TNF-α) – Increased metabolic load – Alterations in taste – Protein degradation – ↓Low albumin, ↓clotting, ↓immune, anemia
Clinical Manifestations • Anemia – Fatigue, pallor, dyspnea on exertion • Thrombocytopenia (Platelets < 150, 000) – Bleeding • Leukopenia (WBC < 5, 000) – Infection

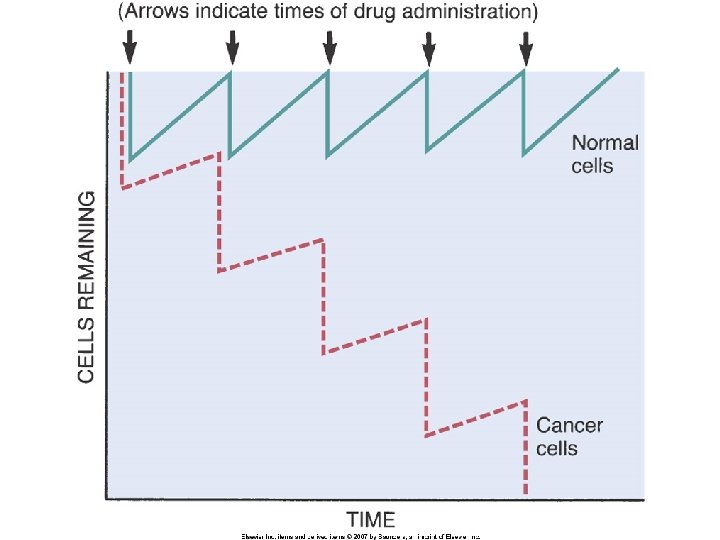
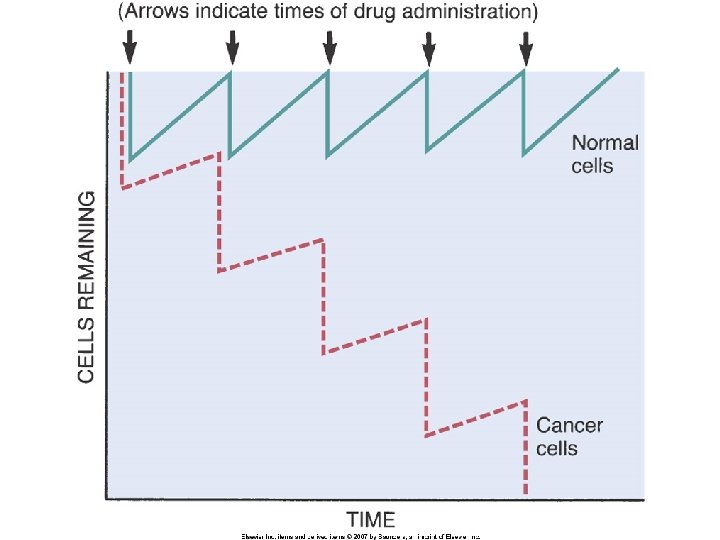
Cancer Treatment • Chemotherapy – Usually targets high growth cells – Single agent – Combination – Dose intensity: kill the cancer before we kill pt – Compartments: only kills mitotic cells • Cell undergoing mitosis • Cells in gap phase • Cells that do not divide
Cancer Treatment • Radiation • Surgery – Local surgery – Sentinel nodes (skip metastasis) – Debulking • Hormonal Therapy • Immunotherapy
Cancer Immunotherapy • • Immunomodulating Agents Interferons Antigens (Tumor painting) Effector Cells and lymphokines – LAK • Monoclonal Antibodies • Dendritic Cell activation
Side Effects of Cancer Treatment • Cells are same as body cells • Treatment usually causes collateral damage • GI tract: – Nausea – Stomatitis – Thrush/Diarrhea – Anorexia – Malabsorption
Side Effects • Bone marrow suppression – Anemia – Leukopenia – Thrombocytopenia • Hair and Skin • Reproductive tract – Gamete banking • Secondary tumors • Remission • “Cancer survivor”
Major Drug Classes • Cytotoxic drugs: kills quickly growing cells – Many Cytotoxic cells are so toxic, they must be handled with gloves and administered in central lines – Star: Methotrexate: mimics folic acid • Cancer cells can’t replicate DNA • Glucocorticoids: – Directly kill cancer cells of lymph tissue – Decrease nausea when combined with antiemetics – Promote appetite and sense of well-being
Major Drug Classes • Hormone Modifiers: usually antagononize sex hormones in prostate and breast cancer • Immunostimulants • Targeted drugs: target specific cancer antigens or pathways.
Diagnosis: Warning Signs • • Lump or swelling A sore that doesn't heal Recent change in a wart/mole Unusual bleeding or discharge Changes in bladder or bowel habits Nagging cough or hoarseness Difficulty in swallowing or dyspepsia
Diagnosis: Clinical Aspects • Persistence of symptoms • Cancer markers • Identification of Mass – usually radiology – X-ray, CT, MRI, nuclear scans, PET scan – Visual (-scope) • Morphologic confirmation!!!!! – Biopsy and cytology
Leukemia • Cancer of blood producing cells • Types – AML: Acute Myelogenous Leukemia – ALL: Acute Lymphocytic Leukemia – CML: Chronic Myelogenous Leukemia – CLL: Chronic Lymphocytic Leukemia • Acute: undifferentiated, rapid onset • Chronic: mature cells, slow onset

ALL • Most common child leukemia (80%) • Mortality in adults is much higher • ALL is caused by loss of differentiation – Stuck dividing, don’t leave marrow – Accumulate, crowd out other cells • Numerous subtypes based on genetic factors – Cure rate 60% to 90%
AML • Accumulation of blast cells – Replace normal RBC, granulocytes and platelets • More common as get older; peaks in 60’s
Acute Leukemia Manifestations • • • Fatigue Bleeding Infection Anorexia Spleen, liver, node enlargement CNS: H/A, vomiting, palsy, sensory impairment
Eval & Treatment • CBC with peripheral smears • Bone marrow biopsy – Sedation/Anesthetic/Analgesia – Pressure to prevent bleeding • Chemotherapy • Stem cell transplant • Supportive therapy – Transfusions, abx, allopurinol
CLL • Monoclonal expansion of B cells • Deficit in mature B cells • Accumulation of cells in marrow does not interfere with normal blood production • Most common manifestations are infections and secondary cancers • Rare under age 45
CML • Begins in a stem cell, but favors myeloid differentiation • Myeloid function is relatively normal • Manifestations similar to AML, but take longer to appear
Eval & Treatment • CBC • Bone marrow biopsy • CLL: treatment relieves symptoms but no significant increase in lifespan
Myeloma • Cancer of Plasma Cells – Increase in ? • Manifestations – – Skeletal pain Renal failure Infections Bone destruction: hypercalcemia • Eval: bone scan, CT, MRI • TX: chemotherapy and Stem cell transplant
 Small intestinal bacterial overgrowth
Small intestinal bacterial overgrowth Jaringan epitel dapat ditemukan di
Jaringan epitel dapat ditemukan di Fibrocartilage description
Fibrocartilage description Callus culture steps
Callus culture steps Definition of cancer according to who
Definition of cancer according to who What makes a good college application
What makes a good college application Why software difficult to build
Why software difficult to build Beaumol
Beaumol Scripture the way of the transgressor is hard
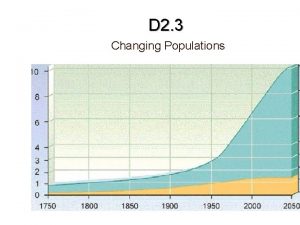
Scripture the way of the transgressor is hard You can easily forget how different life was 50 years ago.
You can easily forget how different life was 50 years ago. The james lange theory of emotion states that
The james lange theory of emotion states that Tell me all about this name that is difficult to say
Tell me all about this name that is difficult to say English paragraph reading
English paragraph reading Momentum is a measure of how difficult it is to
Momentum is a measure of how difficult it is to Crucial conversations chapter 5
Crucial conversations chapter 5 Difficult conversation role play scenarios
Difficult conversation role play scenarios Difficult conversation preparation worksheet
Difficult conversation preparation worksheet Managing difficult negotiations
Managing difficult negotiations The most difficult persuasive task is to
The most difficult persuasive task is to How difficult can this be
How difficult can this be Why is city driving more difficult
Why is city driving more difficult Economics unit 1 lesson 2 difficult choices
Economics unit 1 lesson 2 difficult choices Lower segment caesarean section ppt
Lower segment caesarean section ppt Types of difficult conversations
Types of difficult conversations Why was italian unification difficult to achieve
Why was italian unification difficult to achieve Thyromental distance
Thyromental distance Deakin special consideration
Deakin special consideration Dealing successfully with difficult changes in your life.
Dealing successfully with difficult changes in your life. Used for quick, temporarypost, spar or stake.
Used for quick, temporarypost, spar or stake. How to deal with difficult people
How to deal with difficult people Stork case
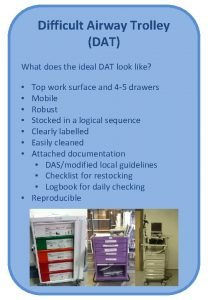
Stork case Difficult airway trolley
Difficult airway trolley Why is software difficult to build ?
Why is software difficult to build ? Seas calculator monash
Seas calculator monash Difficult or impossible to understand
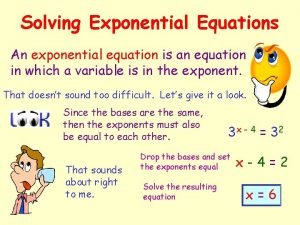
Difficult or impossible to understand Solving exponential equations with different bases
Solving exponential equations with different bases Thy thou thee
Thy thou thee Difficult words to spell
Difficult words to spell Lesson 3 expressing emotions in healthful ways
Lesson 3 expressing emotions in healthful ways