European Resuscitation Council Incidence of Trauma in Childhood


- Slides: 33

European Resuscitation Council
Incidence of Trauma in Childhood ü Leading cause of death and disability in children older than one year all over the world
Structured approach ü Primary survey and resuscitation ü Secondary survey ü Emergency treatment ü Definitive care
Primary survey and resuscitation A - Airway and Cervical Spine stabilisation B - Breathing, Oxygenation, Ventilation and Control of pneumothorax C - Circulation and Haemorrhage control D - Disability, Neurological status, AVPU, Pupils E - Exposure and Environment
Primary survey and resuscitation Treat first what kill first
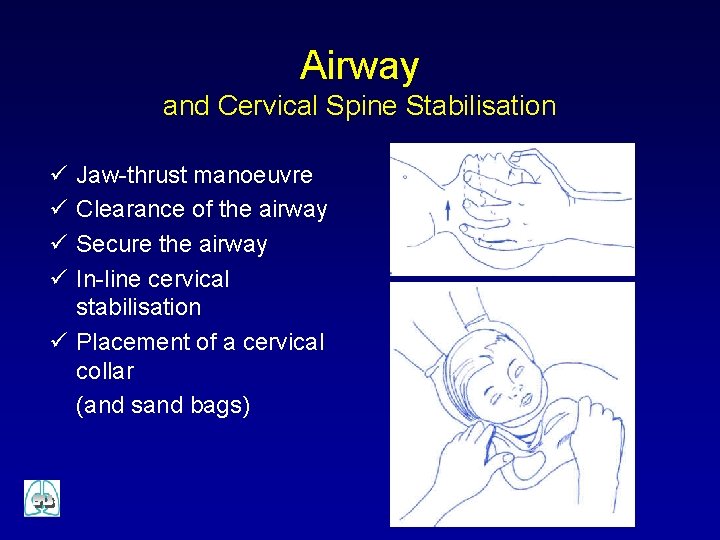
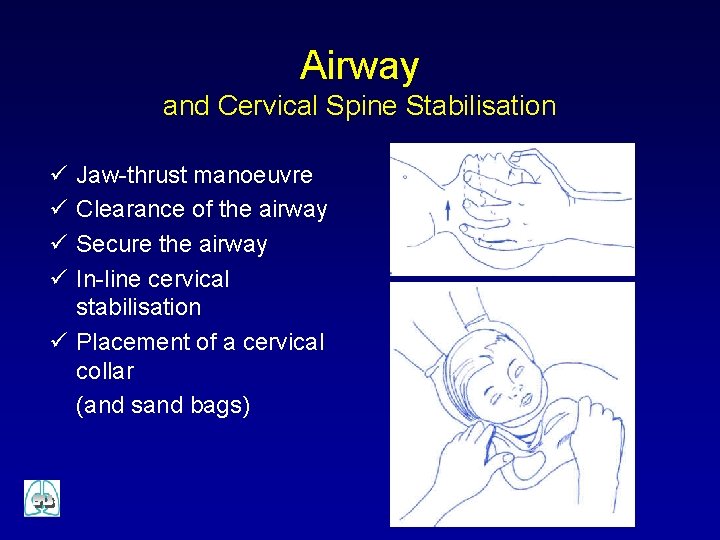
Airway and Cervical Spine Stabilisation ü ü Jaw-thrust manoeuvre Clearance of the airway Secure the airway In-line cervical stabilisation ü Placement of a cervical collar (and sand bags)
Breathing and Ventilation ü Look - listen - feel ü Effort of breathing ü Oxygen at highest concentration ü Bag-mask ventilation ü Intubation and ventilation n impending airway compromise inadequate support from bag-mask prolonged or controlled ventilation needed
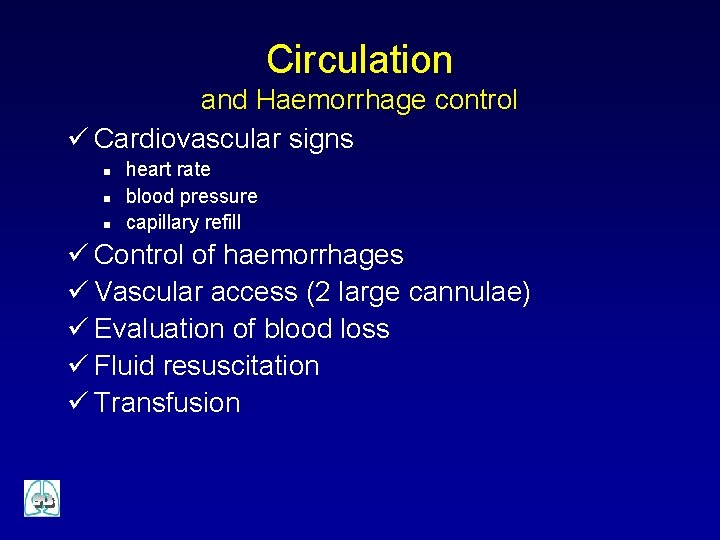
Circulation and Haemorrhage control ü Cardiovascular signs n n n heart rate blood pressure capillary refill ü Control of haemorrhages ü Vascular access (2 large cannulae) ü Evaluation of blood loss ü Fluid resuscitation ü Transfusion
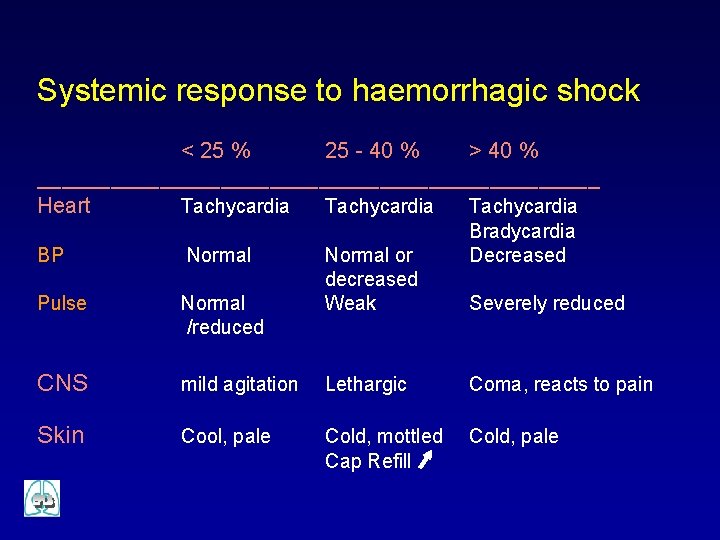
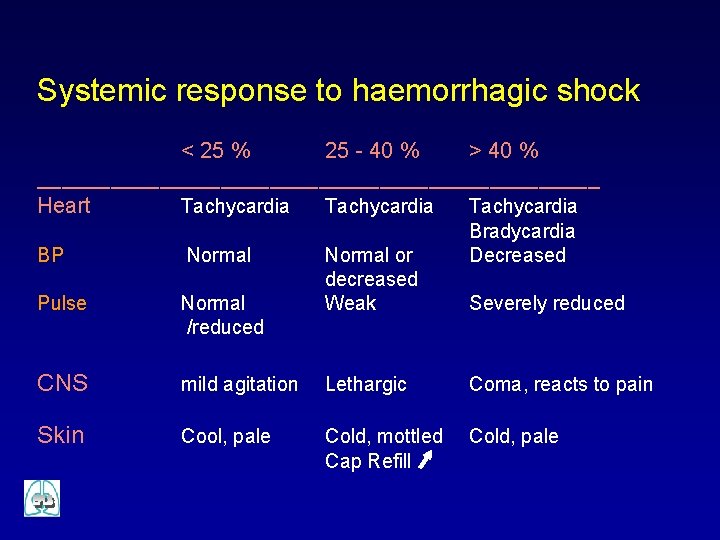
Systemic response to haemorrhagic shock < 25 % 25 - 40 % > 40 % _______________________ Heart Tachycardia Normal or decreased Weak Bradycardia Decreased BP Normal Pulse Normal /reduced CNS mild agitation Lethargic Coma, reacts to pain Skin Cool, pale Cold, mottled Cap Refill Cold, pale Severely reduced
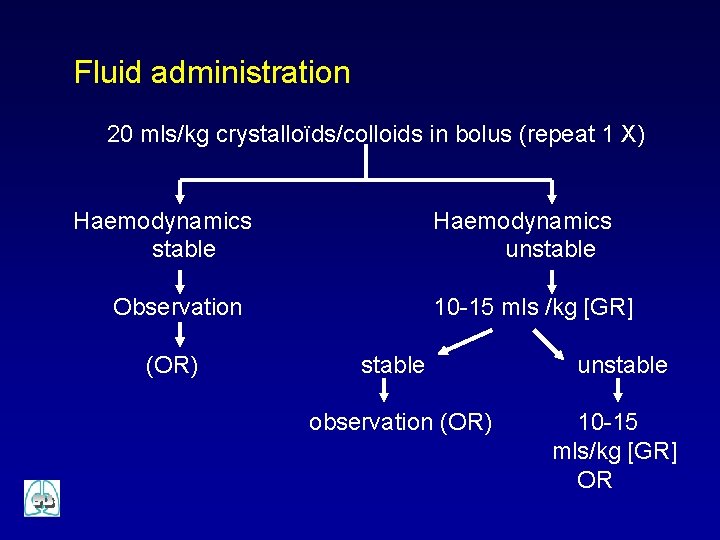
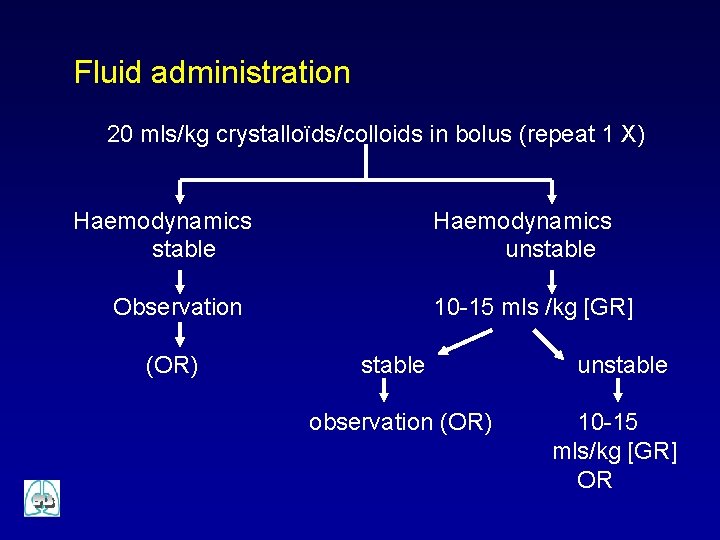
Fluid administration 20 mls/kg crystalloïds/colloids in bolus (repeat 1 X) Haemodynamics stable Haemodynamics unstable Observation (OR) 10 -15 mls /kg [GR] stable observation (OR) unstable 10 -15 mls/kg [GR] OR
Disability and Neurologic Screening Examination ü AVPU ü Pupillary size and reactivity ü Posture
Exposure ü Full exposure ü Remember the heat loss and embarrassment
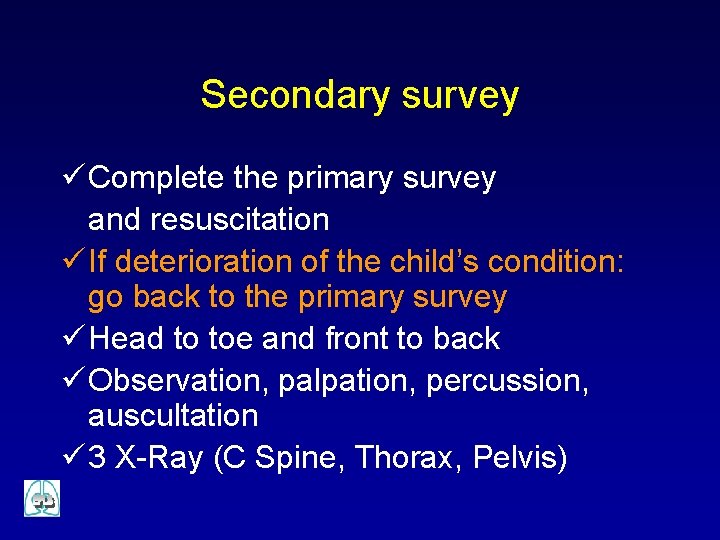
Secondary survey ü Complete the primary survey and resuscitation ü If deterioration of the child’s condition: go back to the primary survey ü Head to toe and front to back ü Observation, palpation, percussion, auscultation ü 3 X-Ray (C Spine, Thorax, Pelvis)
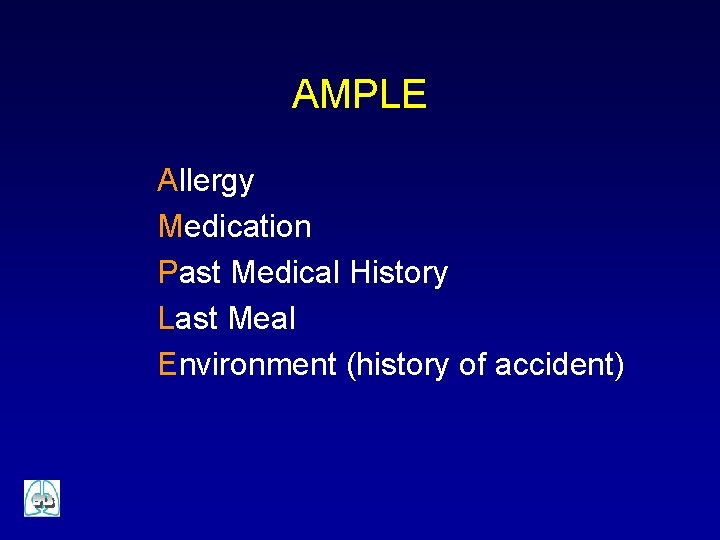
AMPLE Allergy Medication Past Medical History Last Meal Environment (history of accident)
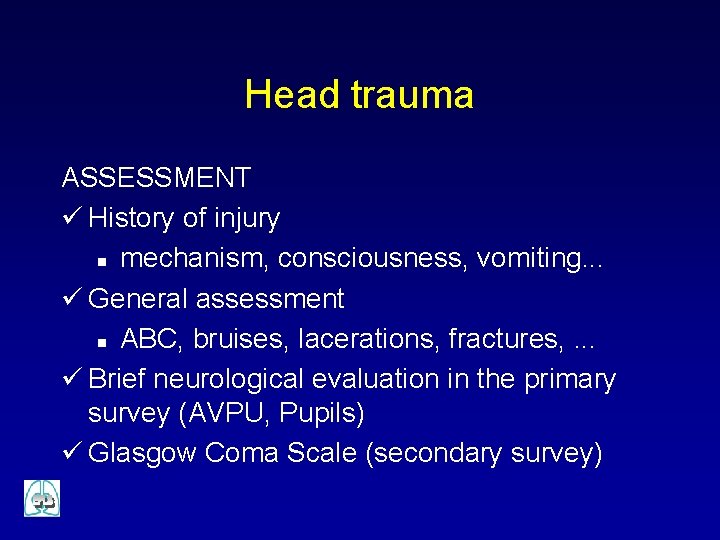
Head trauma ASSESSMENT ü History of injury n mechanism, consciousness, vomiting. . . ü General assessment n ABC, bruises, lacerations, fractures, . . . ü Brief neurological evaluation in the primary survey (AVPU, Pupils) ü Glasgow Coma Scale (secondary survey)
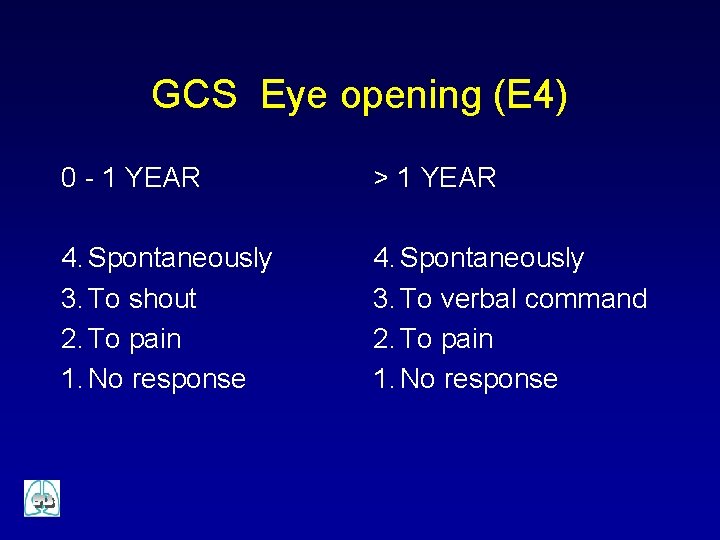
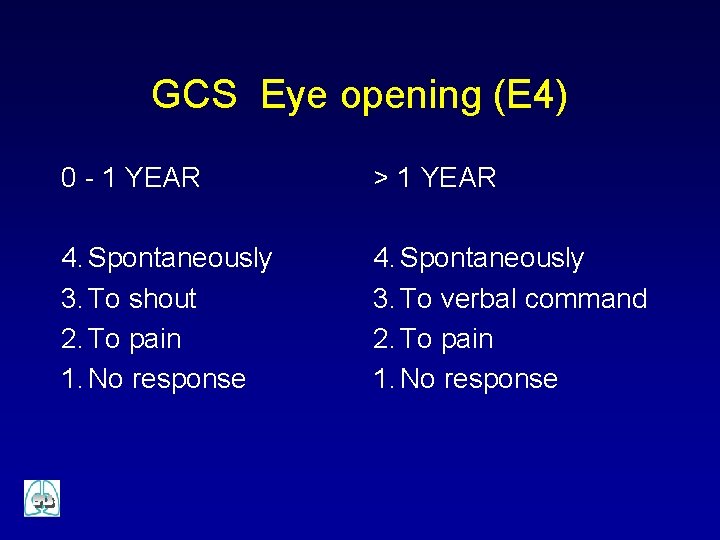
GCS Eye opening (E 4) 0 - 1 YEAR > 1 YEAR 4. Spontaneously 3. To shout 2. To pain 1. No response 4. Spontaneously 3. To verbal command 2. To pain 1. No response
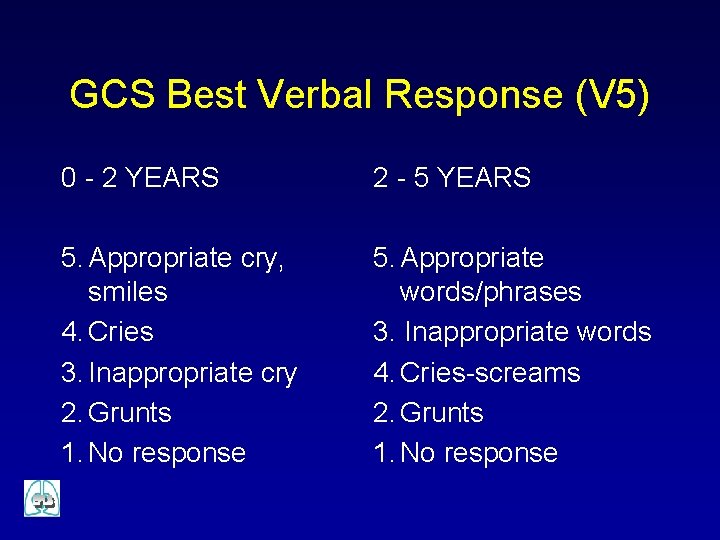
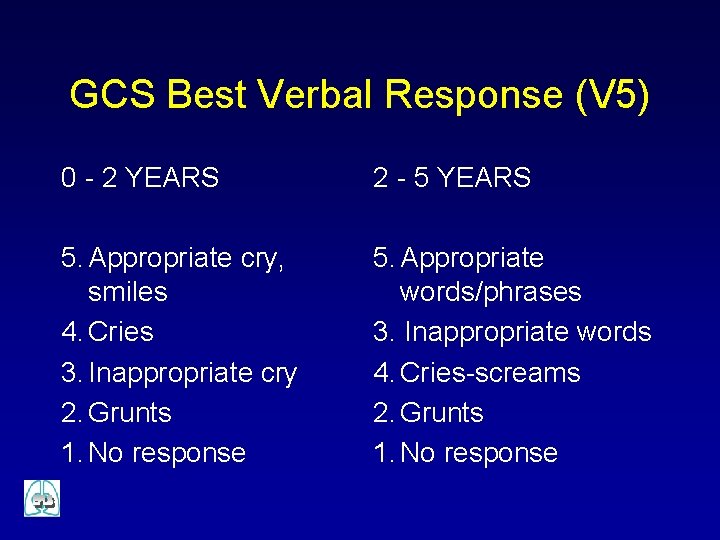
GCS Best Verbal Response (V 5) 0 - 2 YEARS 2 - 5 YEARS 5. Appropriate cry, smiles 4. Cries 3. Inappropriate cry 2. Grunts 1. No response 5. Appropriate words/phrases 3. Inappropriate words 4. Cries-screams 2. Grunts 1. No response
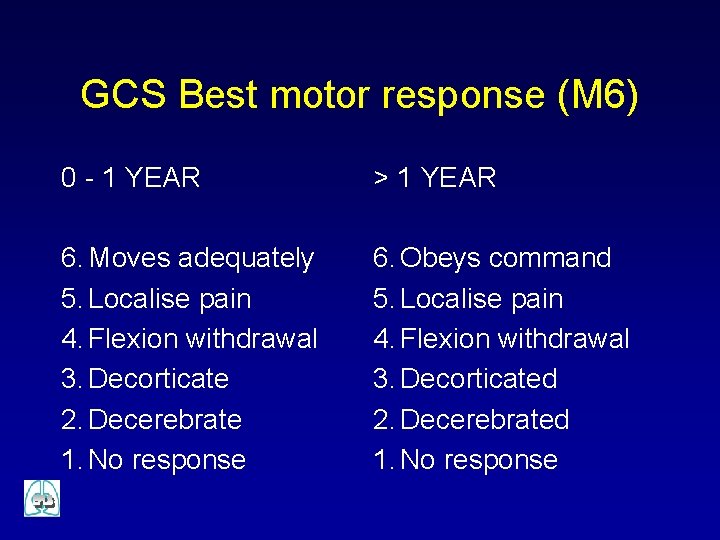
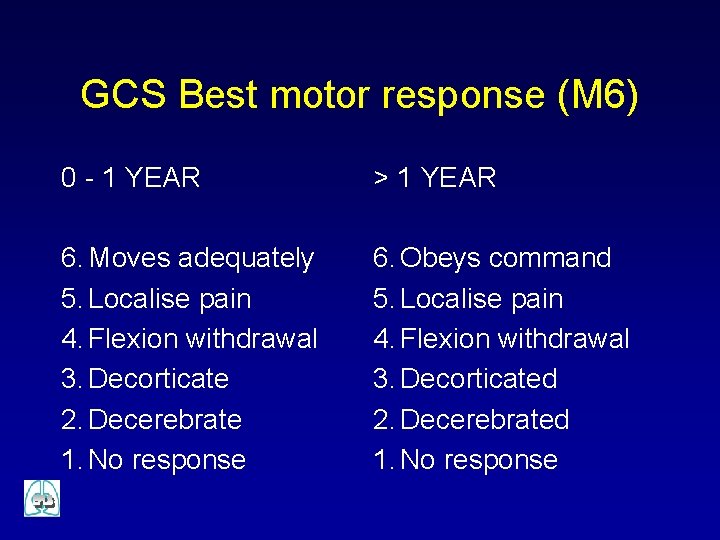
GCS Best motor response (M 6) 0 - 1 YEAR > 1 YEAR 6. Moves adequately 5. Localise pain 4. Flexion withdrawal 3. Decorticate 2. Decerebrate 1. No response 6. Obeys command 5. Localise pain 4. Flexion withdrawal 3. Decorticated 2. Decerebrated 1. No response
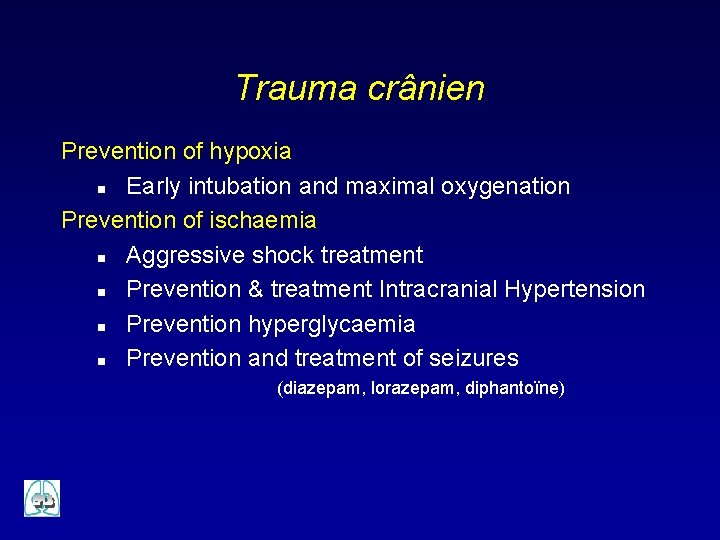
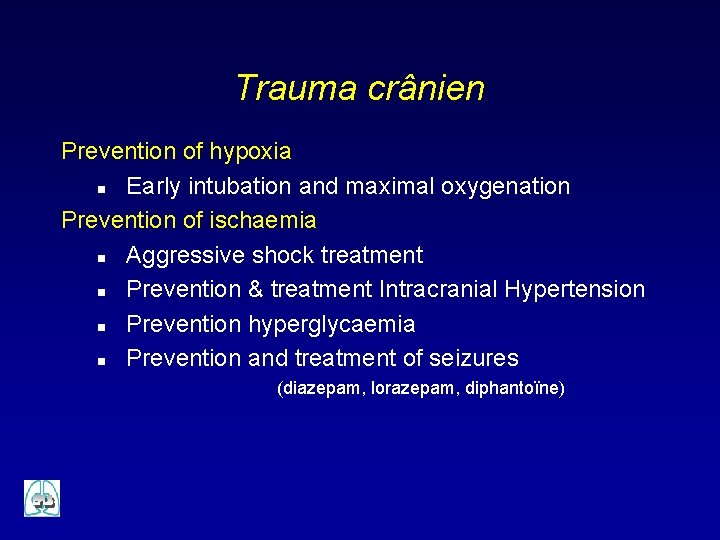
Trauma crânien Prevention of hypoxia n Early intubation and maximal oxygenation Prevention of ischaemia n Aggressive shock treatment n Prevention & treatment Intracranial Hypertension n Prevention hyperglycaemia n Prevention and treatment of seizures (diazepam, lorazepam, diphantoïne)
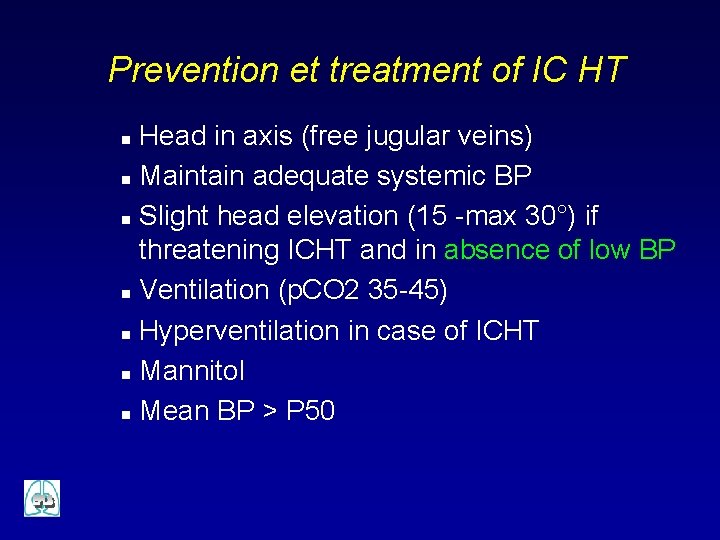
Prevention et treatment of IC HT Head in axis (free jugular veins) n Maintain adequate systemic BP n Slight head elevation (15 -max 30°) if threatening ICHT and in absence of low BP n Ventilation (p. CO 2 35 -45) n Hyperventilation in case of ICHT n Mannitol n Mean BP > P 50 n
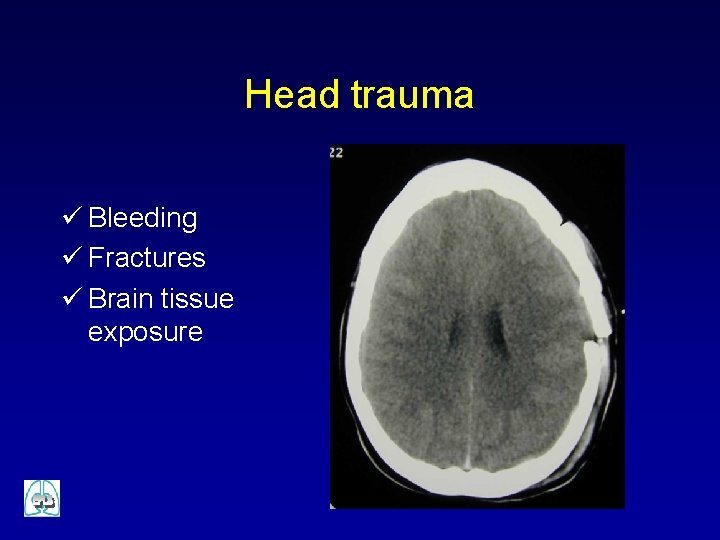
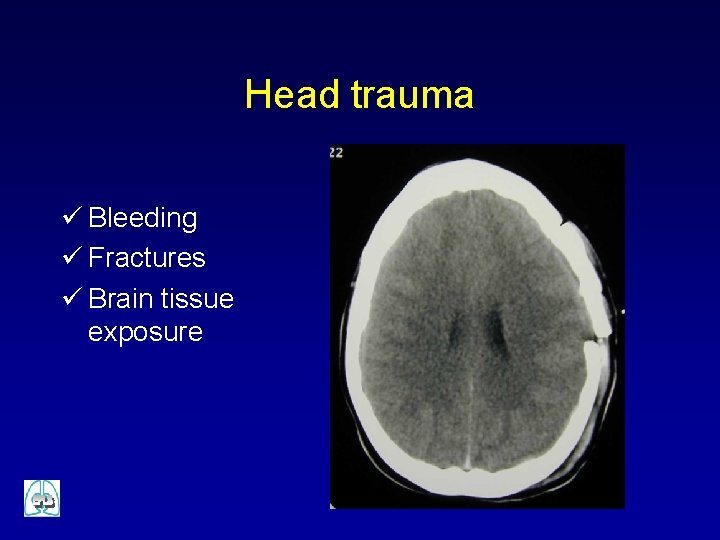
Head trauma ü Bleeding ü Fractures ü Brain tissue exposure
Emergency treatment ü Not life-threatening ü To be managed during the first hour
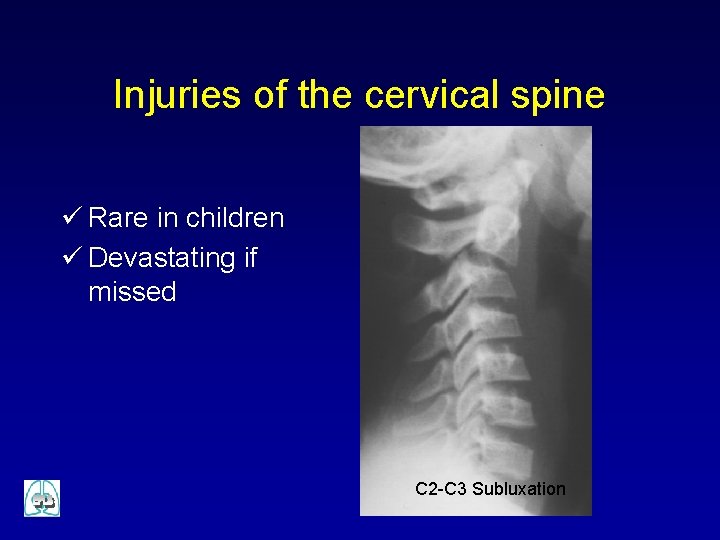
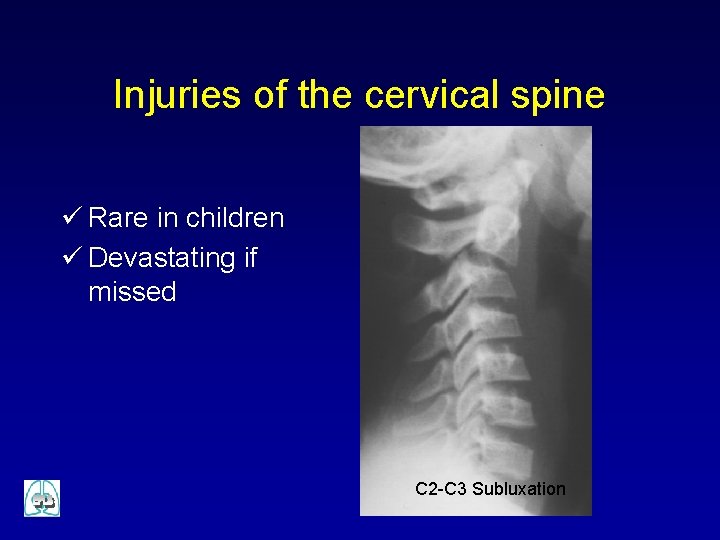
Injuries of the cervical spine ü Rare in children ü Devastating if missed C 2 -C 3 Subluxation
Immobilisation ü Collar ü Sandbags and tapes
Chest trauma IMMEDIATELY LIFE THREATENING ü Tension pneumothorax ü Massive haematopneumothorax ü Open pneumothorax ü Flail chest ü Cardiac tamponade DIAGNOSIS IS CLINICAL AND NOT RADIOLOGICAL
Tension pneumothorax SIGNS ü Hypoxaemia ü Obstructive shock ü Unilateral absence of breath sounds ü Ipsilateral hypertympanic percussion ü Asymmetric respiratory movements ü Neck veins distension ü Tracheal deviation to the opposite
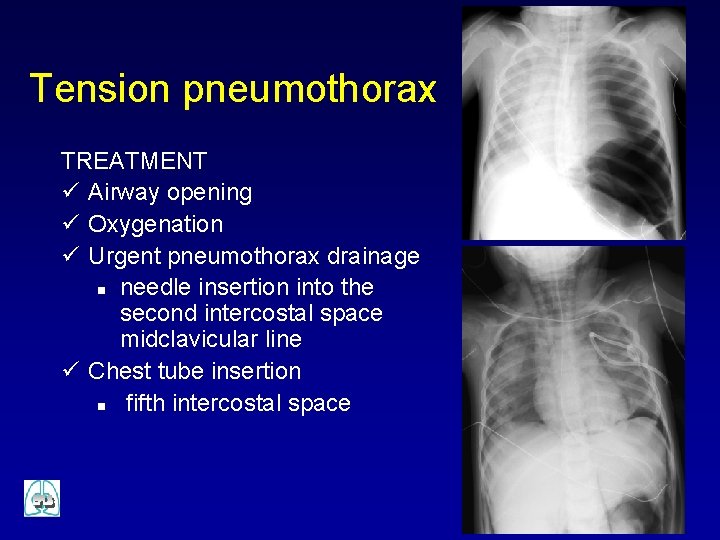
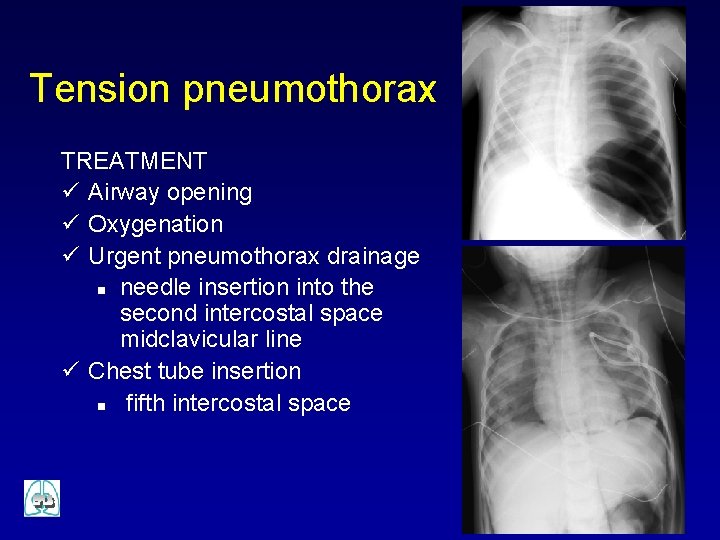
Tension pneumothorax TREATMENT ü Airway opening ü Oxygenation ü Urgent pneumothorax drainage n needle insertion into the second intercostal space midclavicular line ü Chest tube insertion n fifth intercostal space
Massive haemothorax SIGNS ü Hypoxaemia ü Hypovolaemic shock ü Ipsilateraly decreased breath sounds and respiratory movements ü Ipsilateral dullness to percussion TREATMENT ü Oxygenation ü Vascular access and fluid infusion ü Drainage ü Transfusion
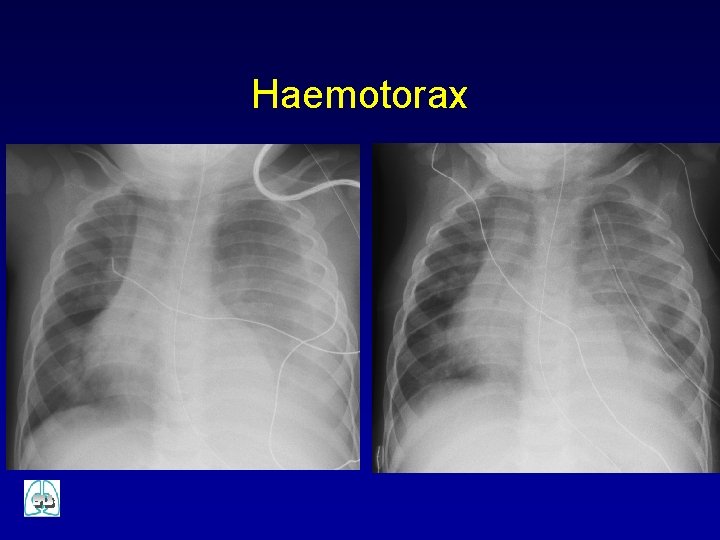
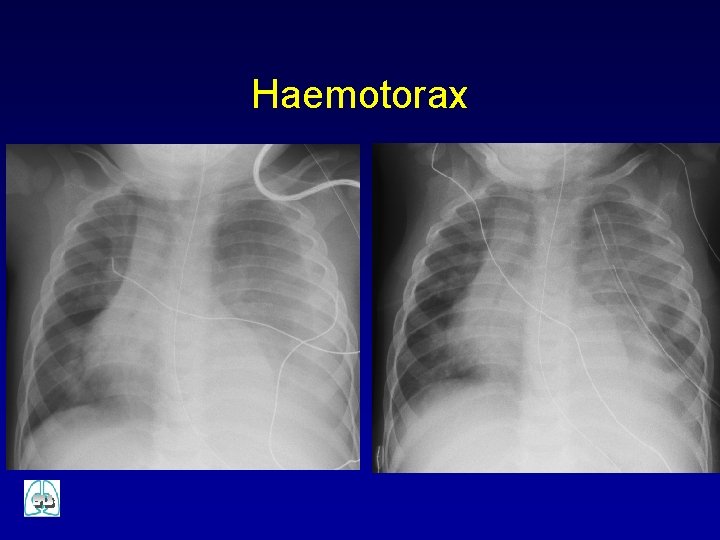
Haemotorax
Cardiac tamponade SIGNS ü Obstructive shock ü Muffled heart tones respiratory movements ü Distended neck veins TREATMENT ü Oxygenation ü Vascular access and fluid infusion ü Pericardiocentesis ü Urgent surgical repair
Thorax and abdomen ü Penetrating injury ü Vascular injury ü Suspicion of bowl perforation ü Refractory shock of abdominal or thoracic origin
Skeletal trauma ü Crush injuries of the abdomen and pelvis ü Traumatic amputation of an extremity n n Partial Total ü Massive open long-bone fractures

Definitive care ü Referral ü Safe transport
 European resuscitation council
European resuscitation council European resuscitation council
European resuscitation council European resuscitation council
European resuscitation council Prevalence calculation formula
Prevalence calculation formula Incidence vs incidence rate
Incidence vs incidence rate Singapore first aid council
Singapore first aid council Ace test score interpretation pdf
Ace test score interpretation pdf Childhood trauma discussion questions
Childhood trauma discussion questions Gabriela zapata alma
Gabriela zapata alma Early childhood adolescence
Early childhood adolescence European cruise council
European cruise council Erec european renewable energy council
Erec european renewable energy council Coordinating european council
Coordinating european council European language council
European language council European council role
European council role Neonatal resuscitation
Neonatal resuscitation Cardioprotection resuscitation
Cardioprotection resuscitation Endpoint of resuscitation
Endpoint of resuscitation Chapter 17 providing first aid
Chapter 17 providing first aid Dope neonatal resuscitation
Dope neonatal resuscitation Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Resuscitation triangle roles
Resuscitation triangle roles Pediatric color coding
Pediatric color coding Cpr tutorial
Cpr tutorial Bronze baby syndrome
Bronze baby syndrome Apgar score meaning
Apgar score meaning Fluid resuscitation formula
Fluid resuscitation formula Principles of resuscitation
Principles of resuscitation Difference between resuscitation and resurrection
Difference between resuscitation and resurrection Dr sneha sood
Dr sneha sood Amber care bundle nice
Amber care bundle nice Resuscitation cpr
Resuscitation cpr Acute resuscitation plan form
Acute resuscitation plan form Infiltration épaule
Infiltration épaule