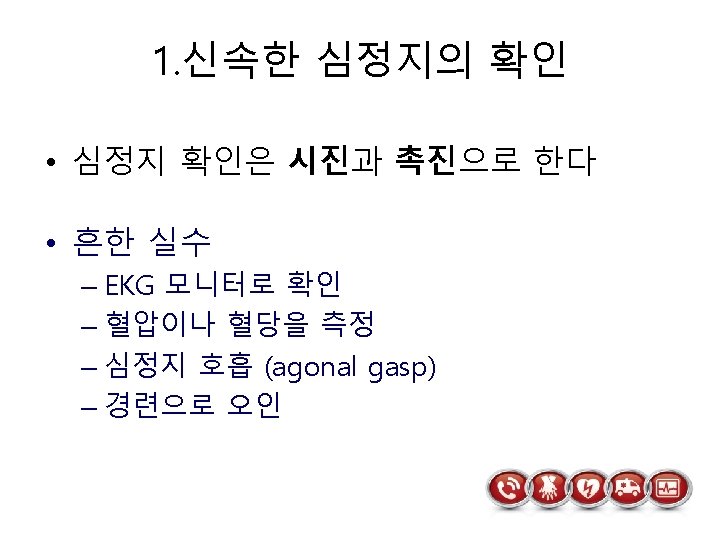
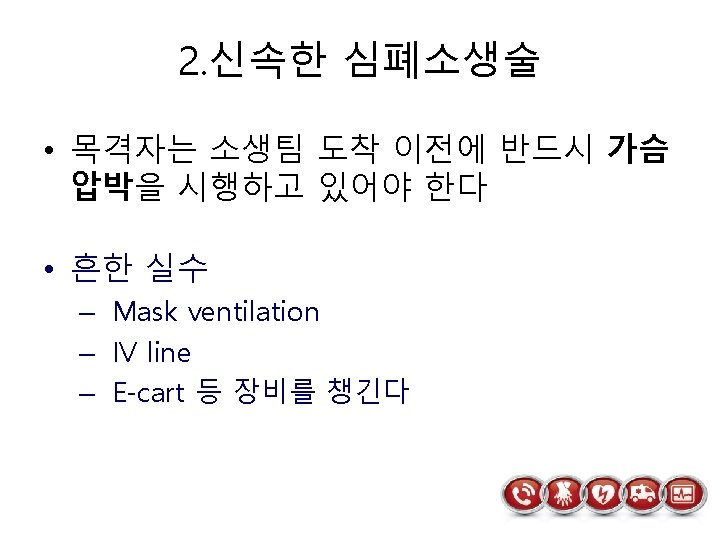
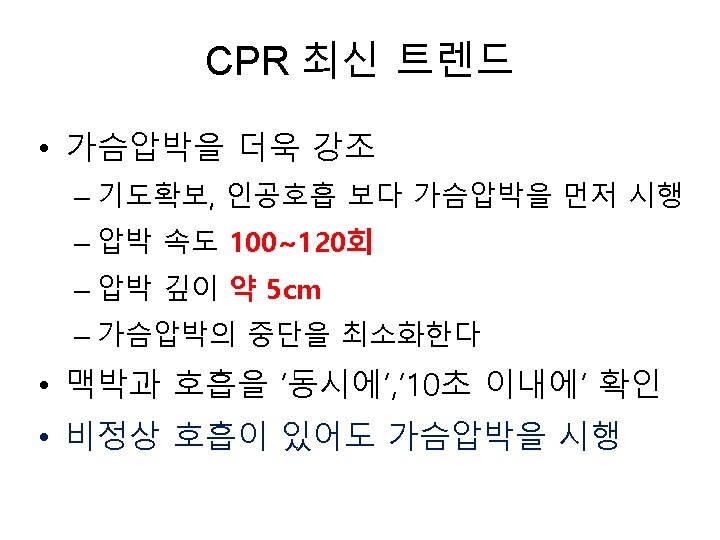
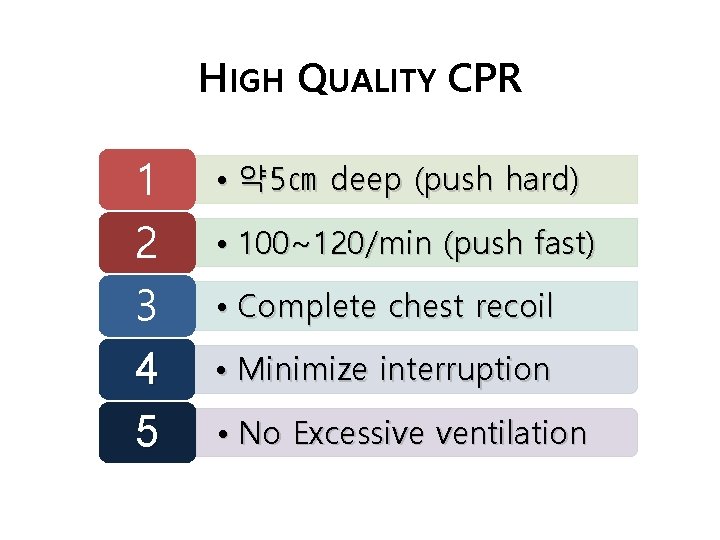
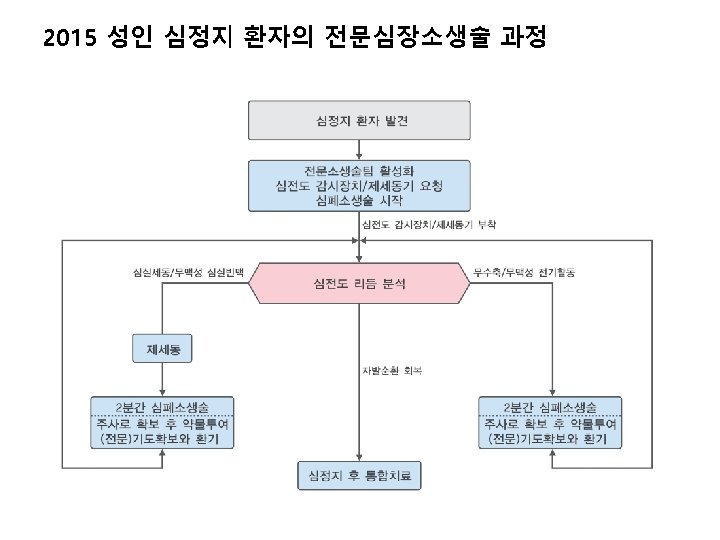
Chain of survival HIGH QUALITY CPR 1 2




- Slides: 41

Chain of survival
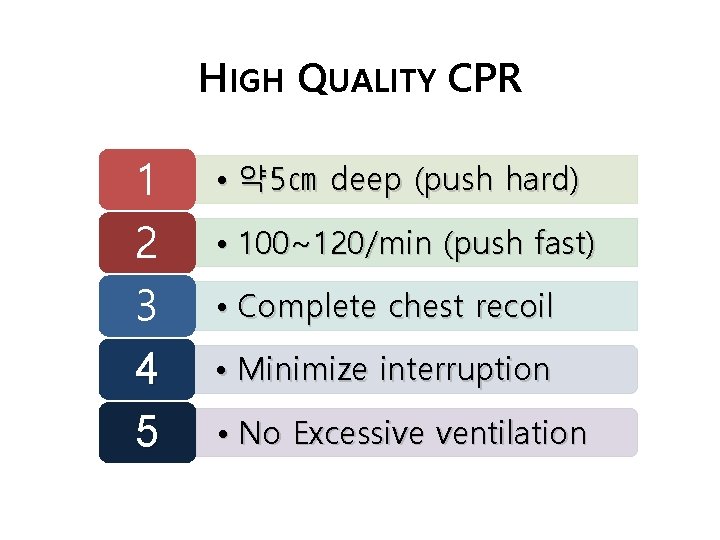
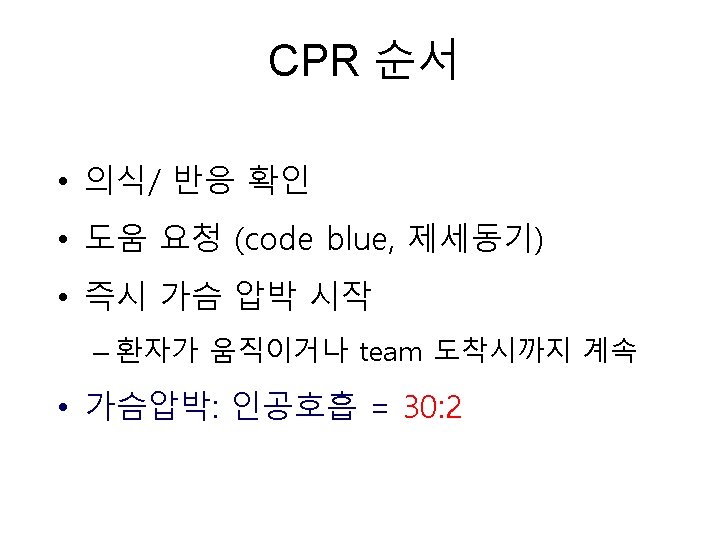
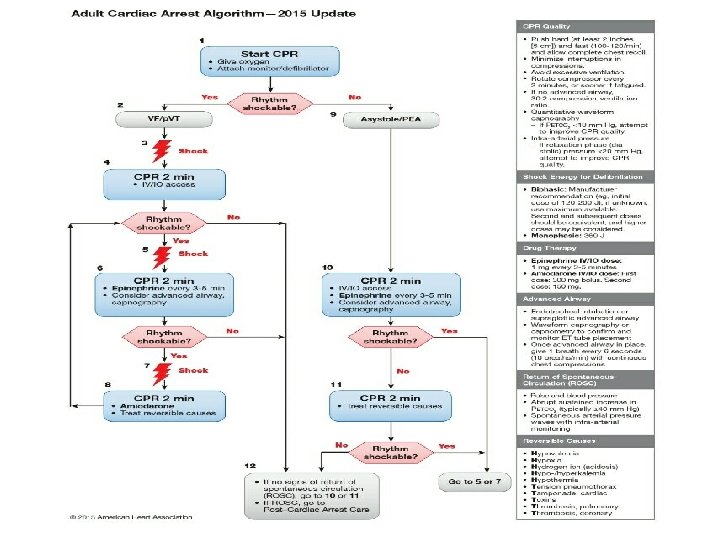
HIGH QUALITY CPR 1 2 3 4 5 • 약 5㎝ deep (push hard) • 100~120/min (push fast) • Complete chest recoil • Minimize interruption • No Excessive ventilation
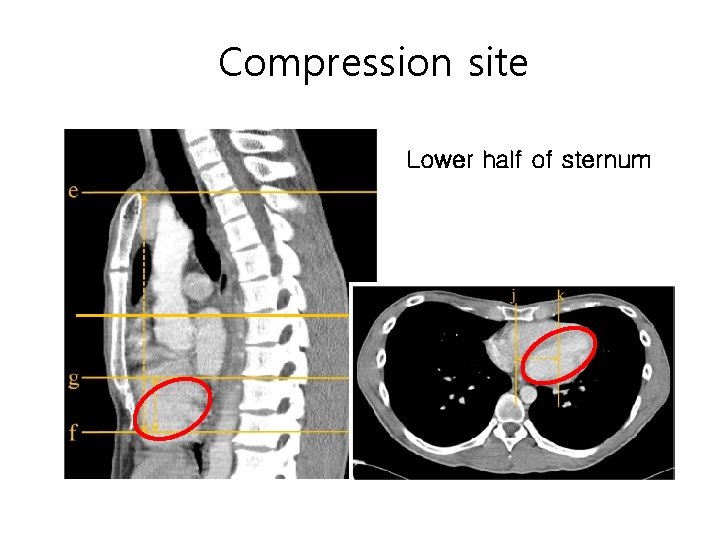
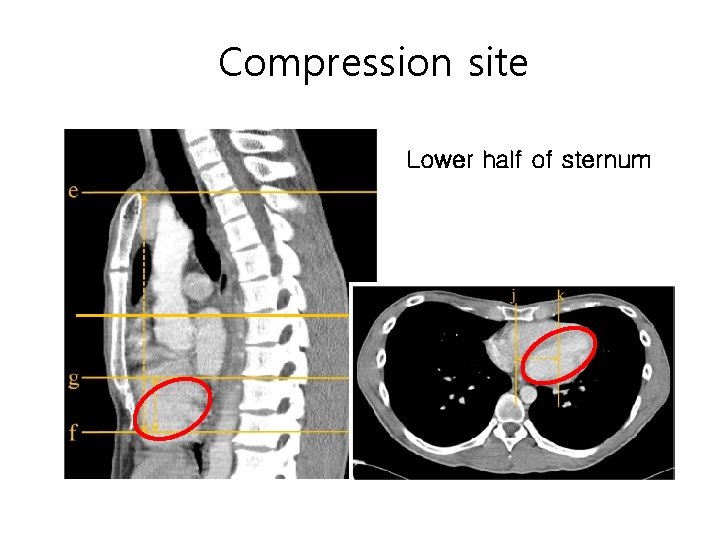
Compression site Lower half of sternum
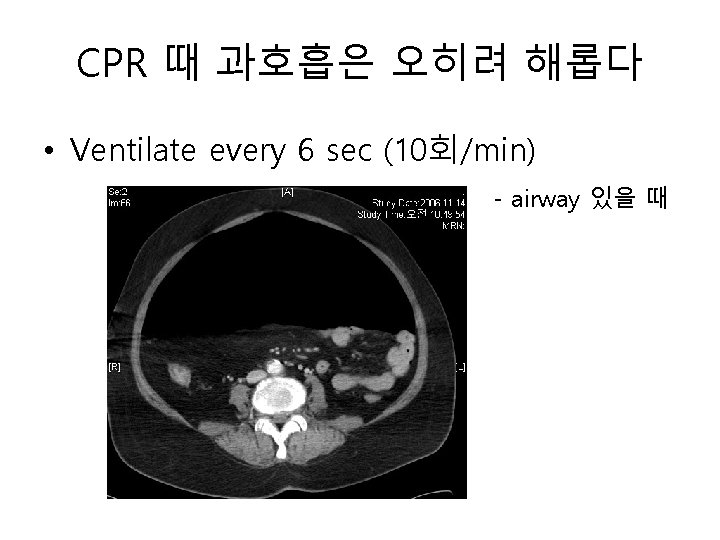
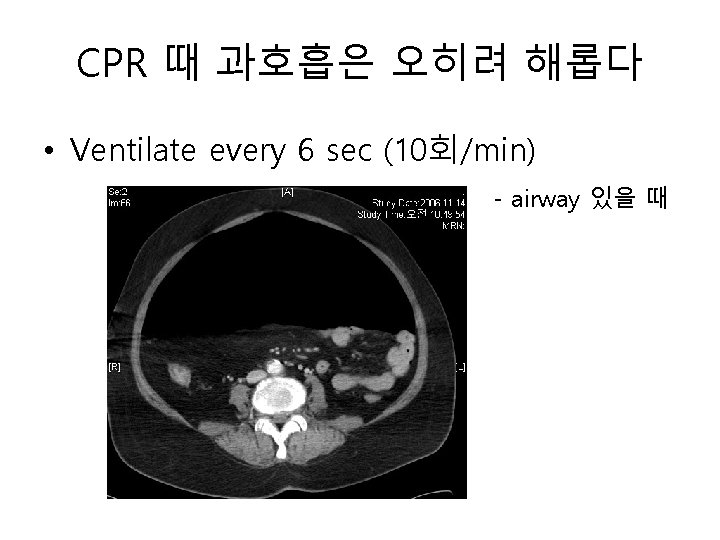
CPR 때 과호흡은 오히려 해롭다 • Ventilate every 6 sec (10회/min) - airway 있을 때

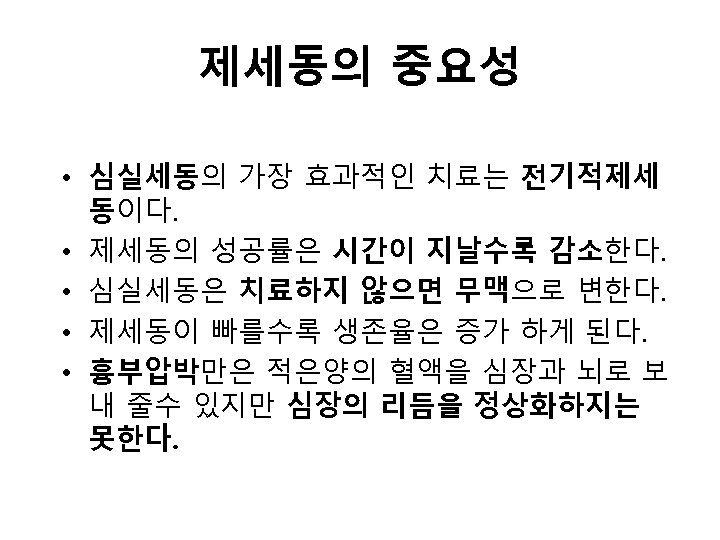
3. 신속한 제세동 0 20 Arrest Time (min)
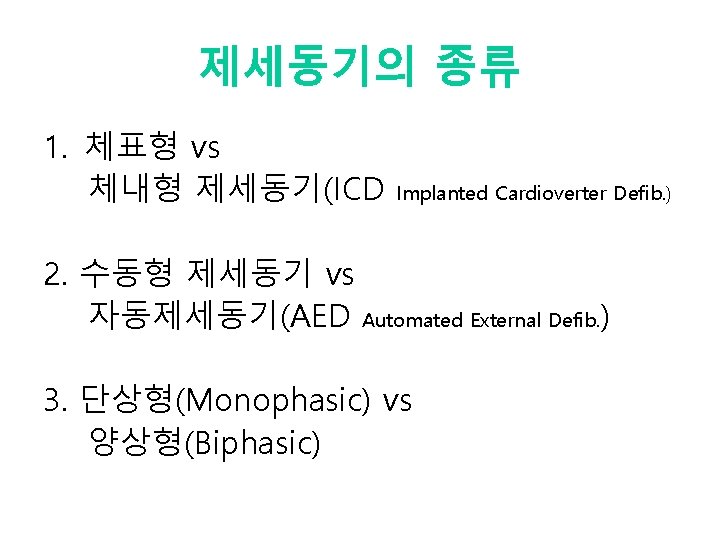
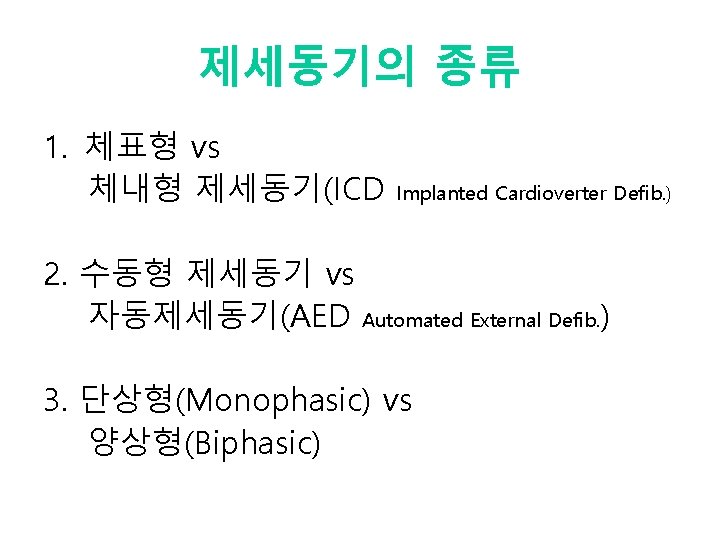
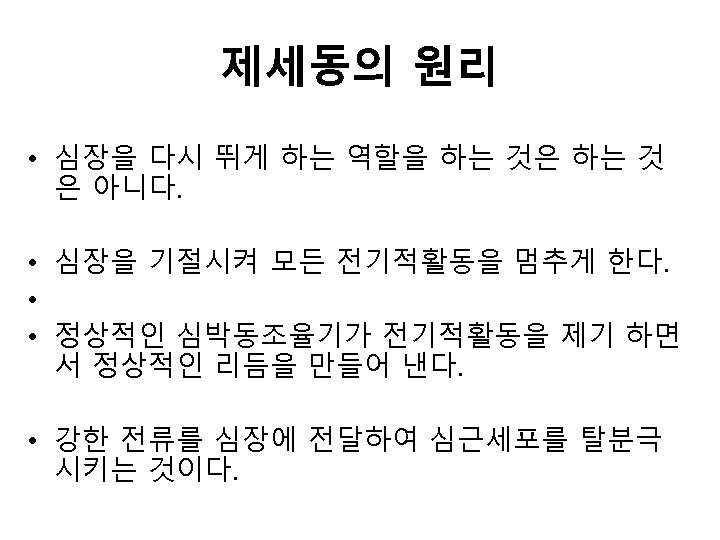
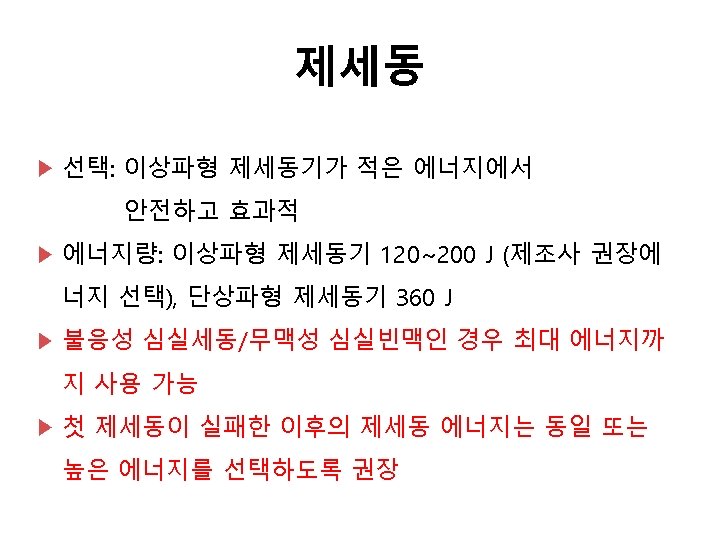
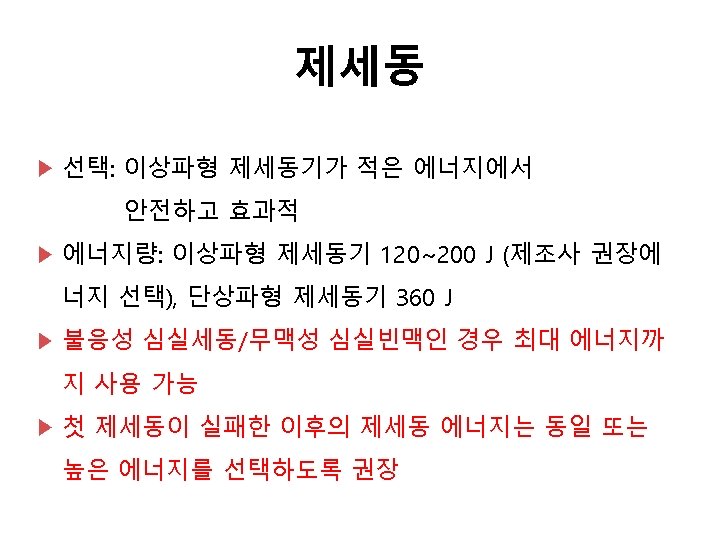
제세동기의 종류 1. 체표형 vs 체내형 제세동기(ICD Implanted Cardioverter Defib. ) 2. 수동형 제세동기 vs 자동제세동기(AED Automated External Defib. ) 3. 단상형(Monophasic) vs 양상형(Biphasic)
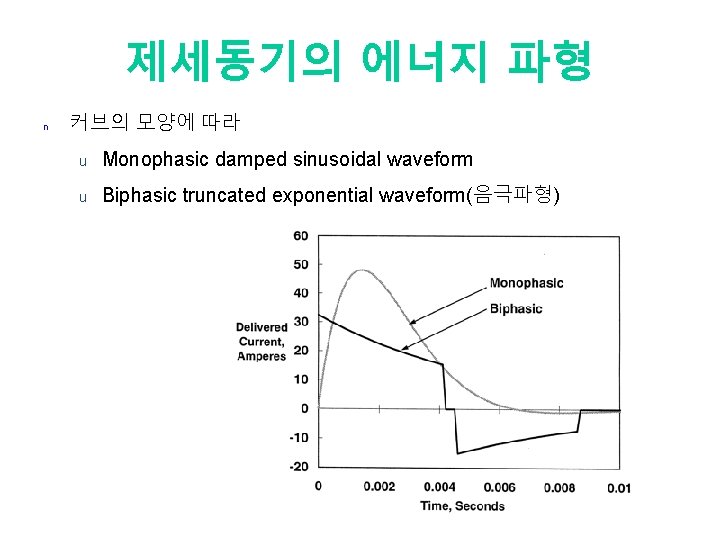
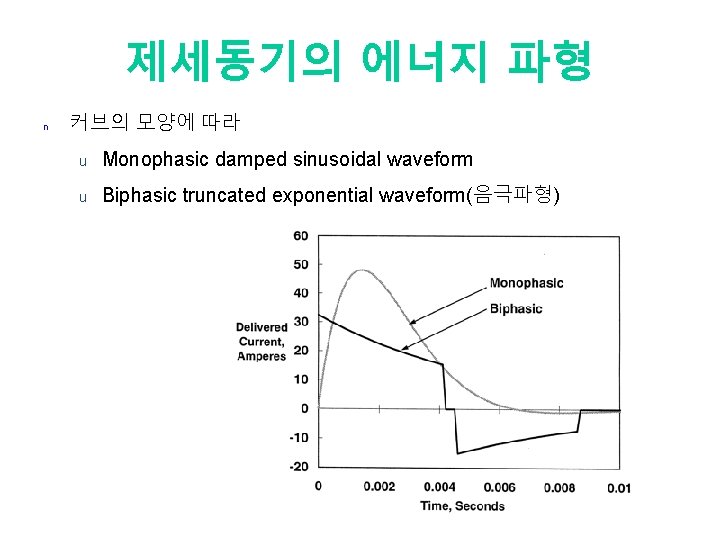
제세동기의 에너지 파형 n 커브의 모양에 따라 u Monophasic damped sinusoidal waveform u Biphasic truncated exponential waveform(음극파형)
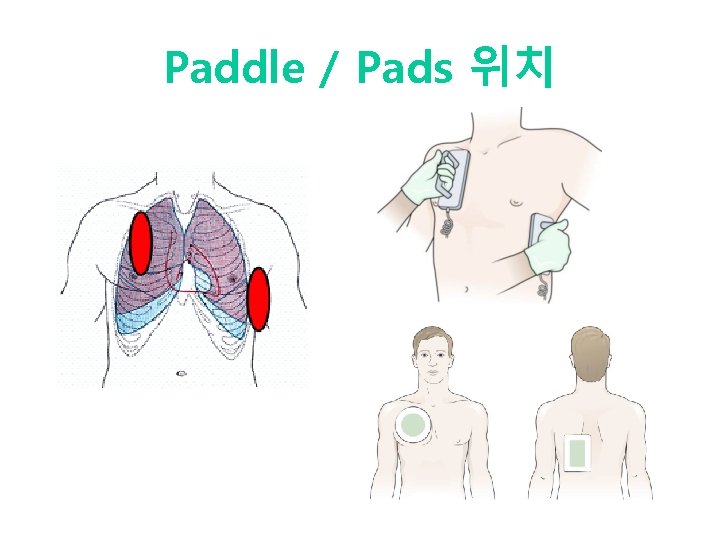
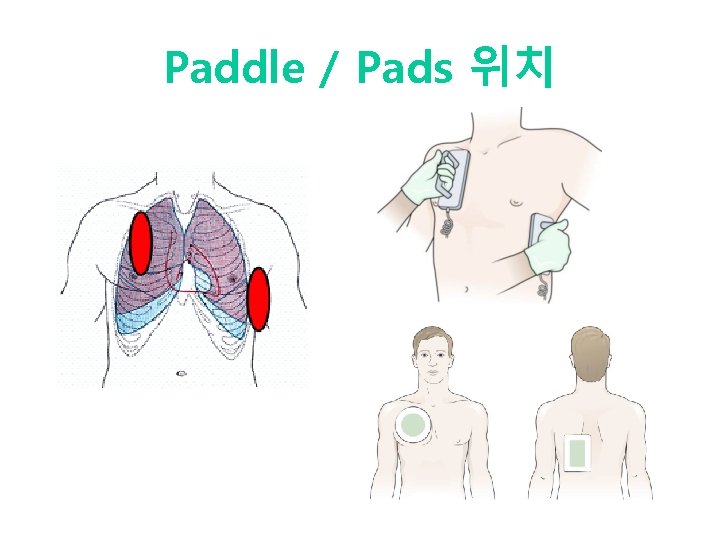
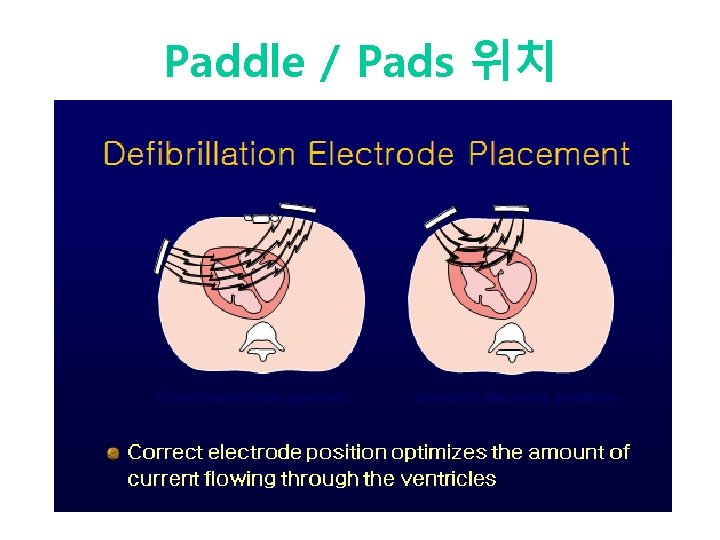
Paddle / Pads 위치
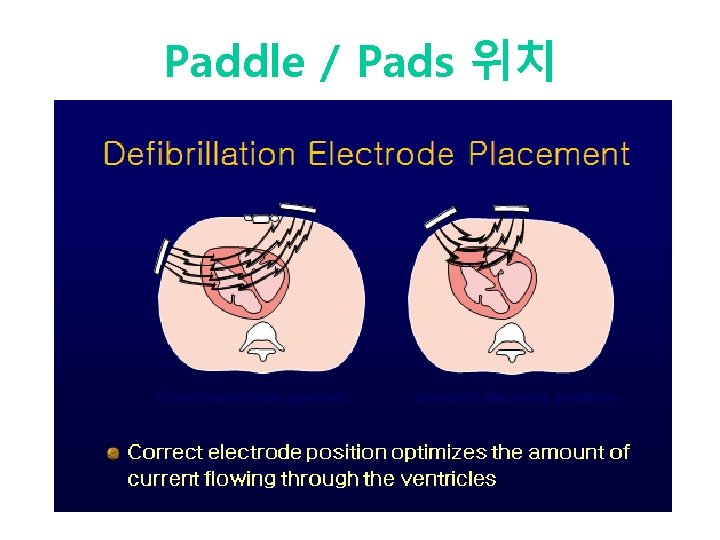
Paddle / Pads 위치
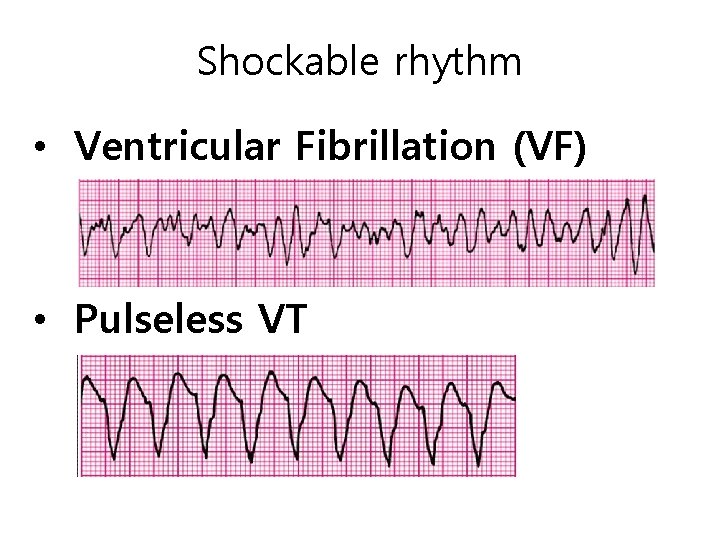
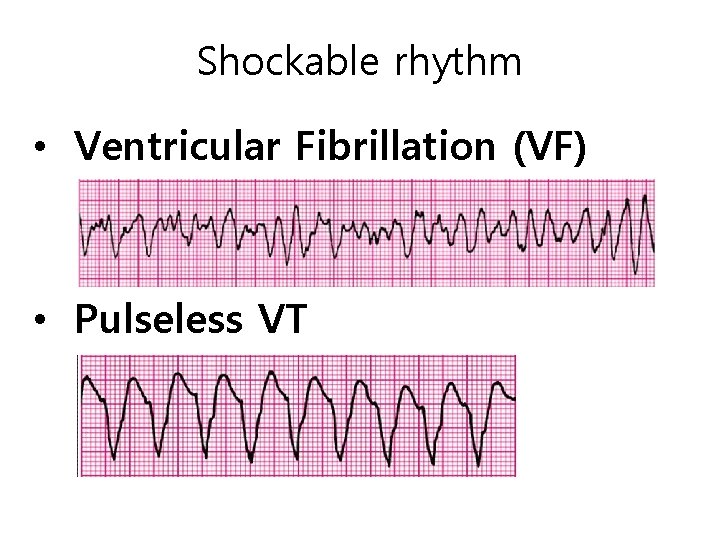
Shockable rhythm • Ventricular Fibrillation (VF) • Pulseless VT
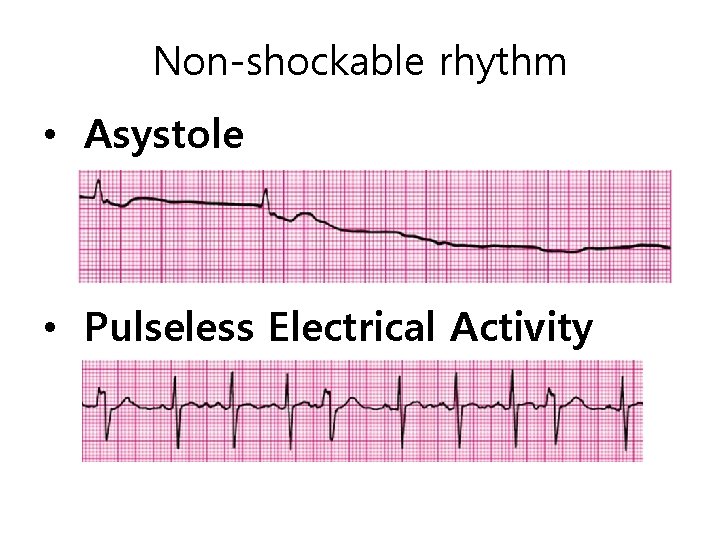
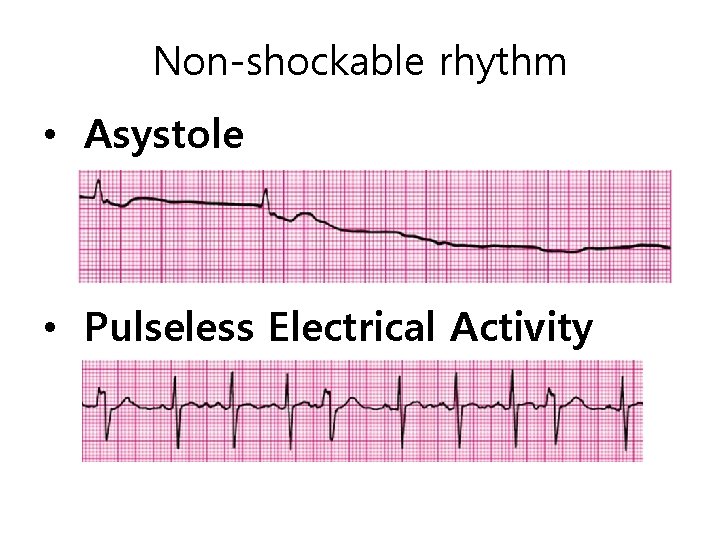
Non-shockable rhythm • Asystole • Pulseless Electrical Activity
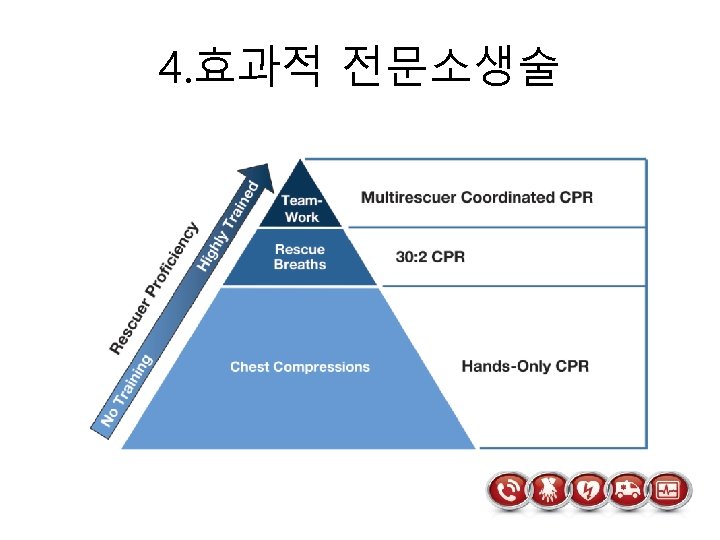

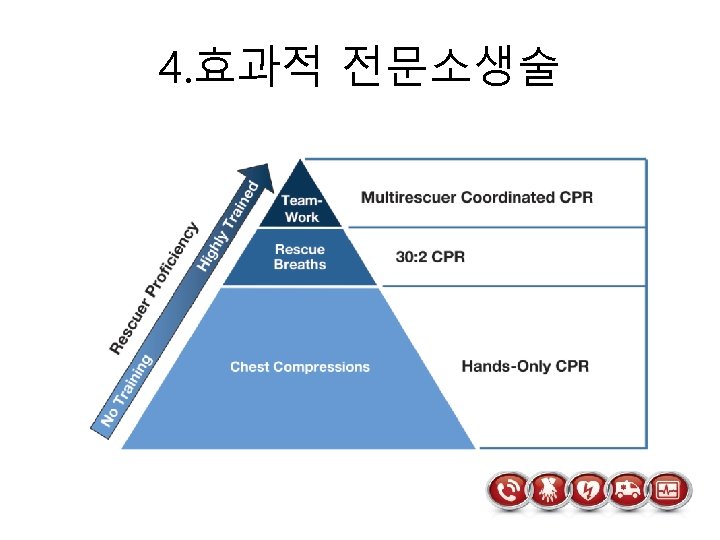
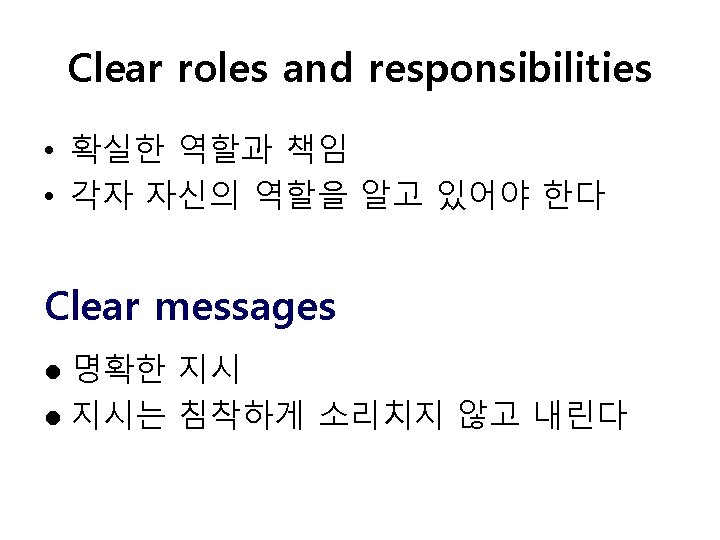
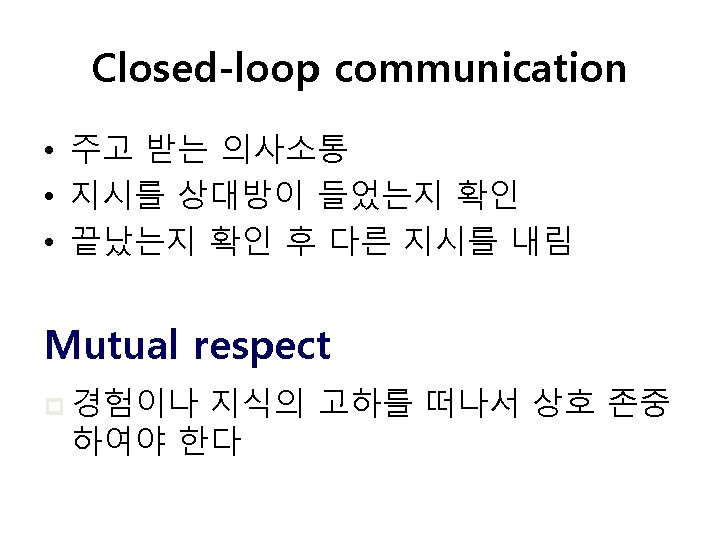
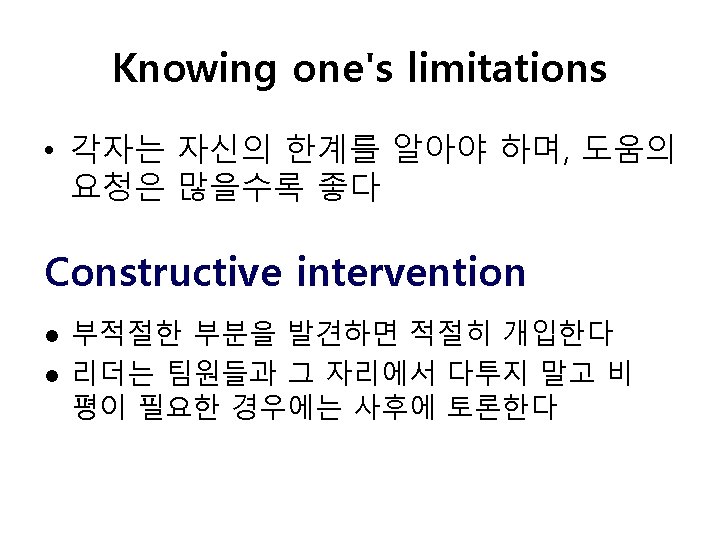
CPR is team play, not personal skill Elements of effective resuscitation team dynamics ① Closed-loop communication ② Clear messages ③ Clear roles and responsibilities ④ Knowing one’s limitations ⑤ Knowledge sharing ⑥ Constructive intervention ⑦ Reevaluation and summarizing ⑧ Mutual respect
GOOD CPR ROLE
BAD CPR ROLE
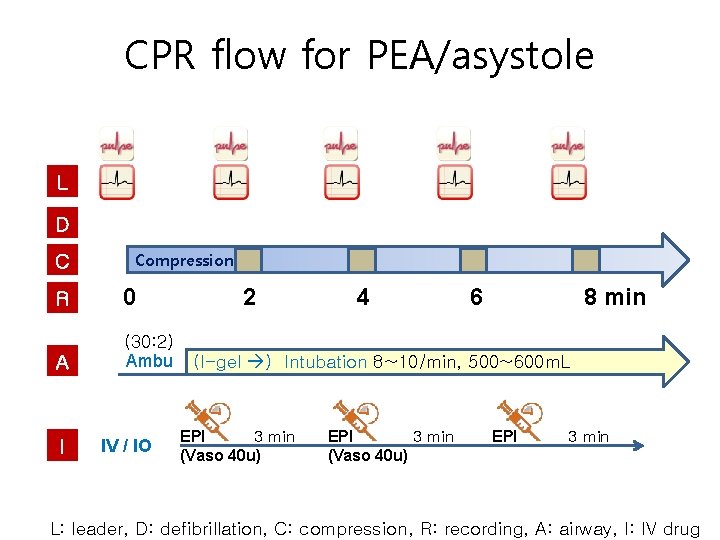
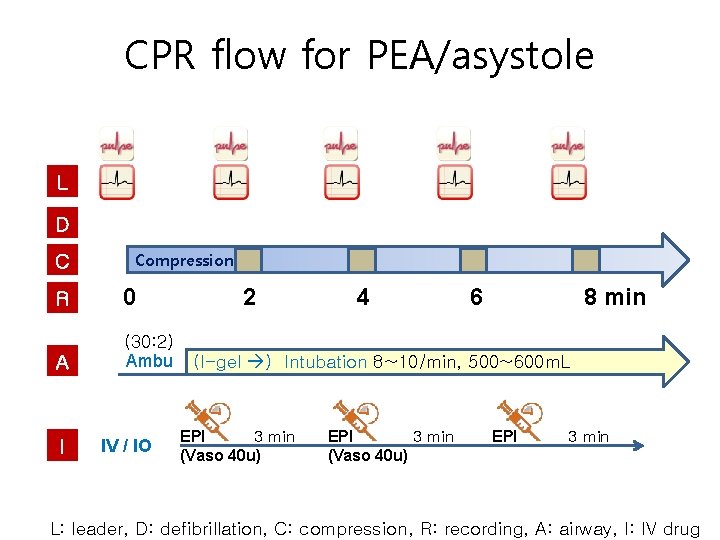
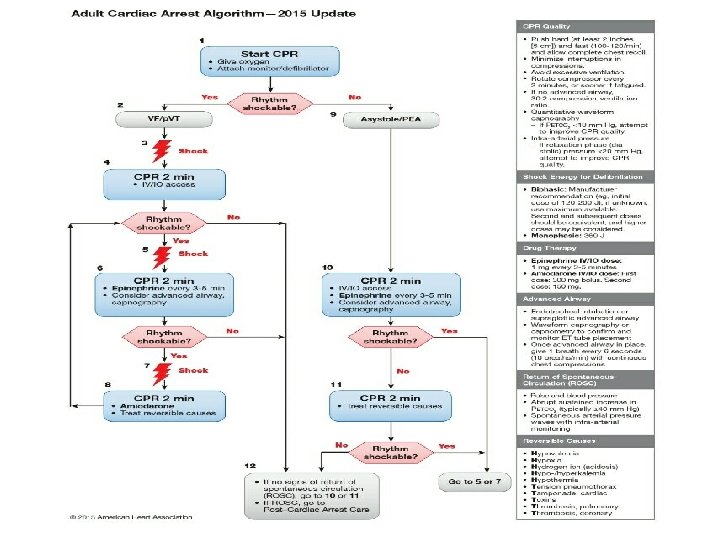
CPR flow for PEA/asystole L D C Compression R 0 A (30: 2) Ambu I IV / IO 2 4 6 8 min (I-gel ) Intubation 8~10/min, 500~600 m. L EPI 3 min (Vaso 40 u) EPI 3 min L: leader, D: defibrillation, C: compression, R: recording, A: airway, I: IV drug
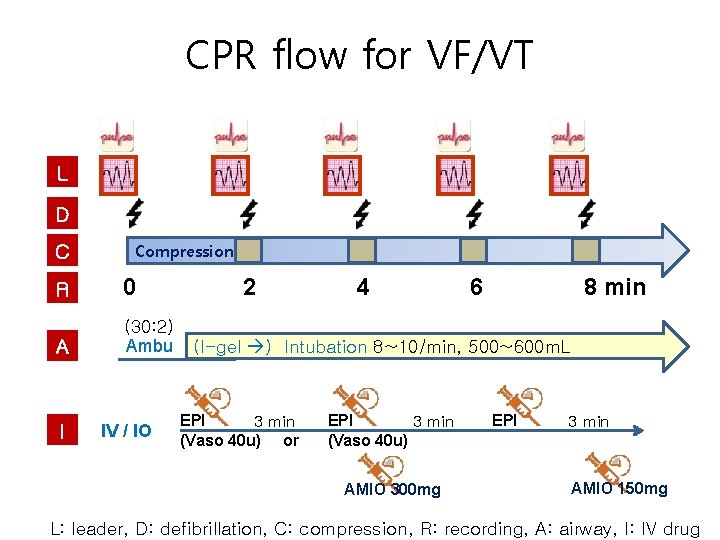
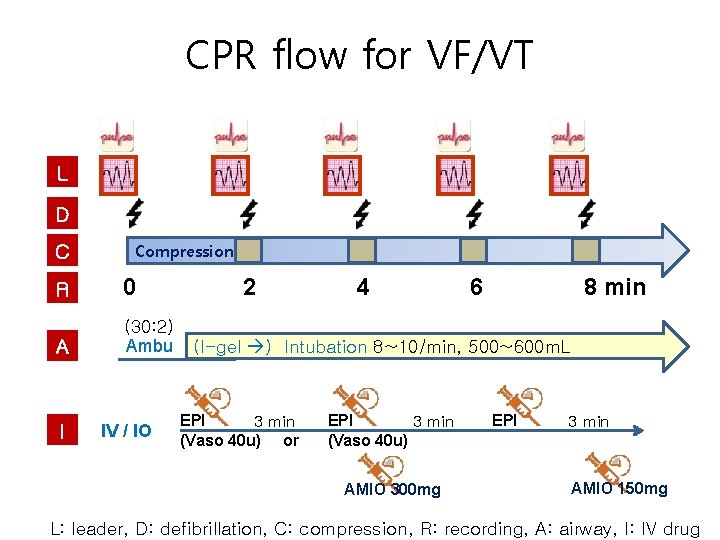
CPR flow for VF/VT L D C Compression R 0 A (30: 2) Ambu I IV / IO 2 4 6 8 min (I-gel ) Intubation 8~10/min, 500~600 m. L EPI 3 min (Vaso 40 u) or EPI 3 min (Vaso 40 u) AMIO 300 mg EPI 3 min AMIO 150 mg L: leader, D: defibrillation, C: compression, R: recording, A: airway, I: IV drug
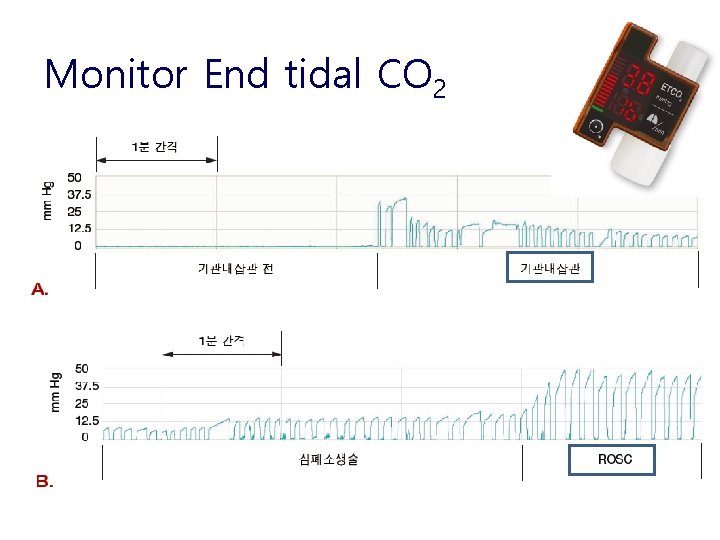
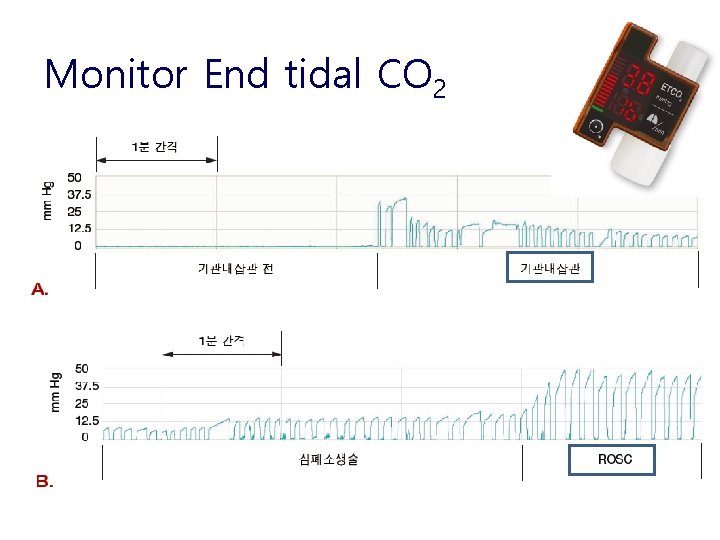
Monitor End tidal CO 2
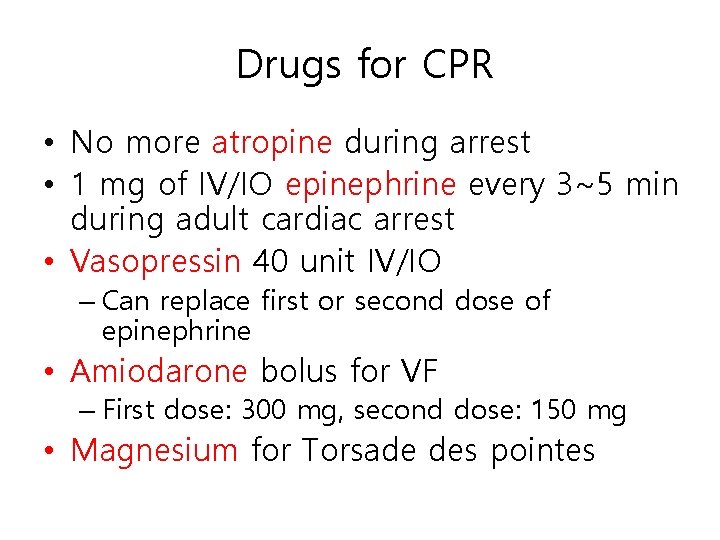
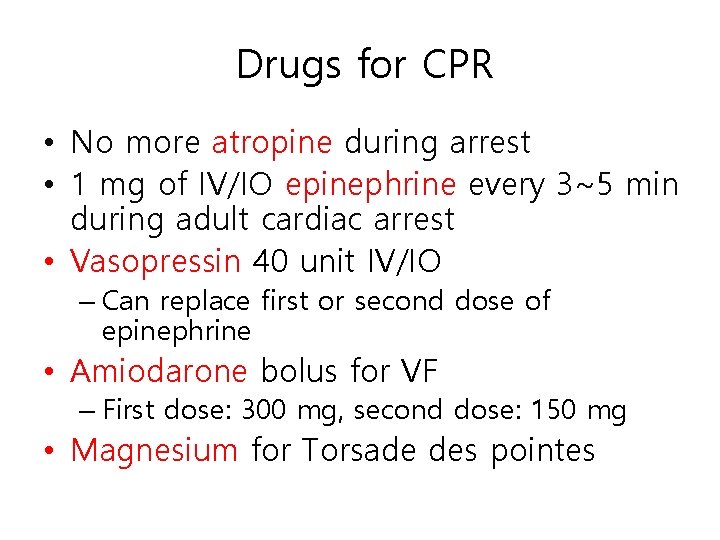
Drugs for CPR • No more atropine during arrest • 1 mg of IV/IO epinephrine every 3~5 min during adult cardiac arrest • Vasopressin 40 unit IV/IO – Can replace first or second dose of epinephrine • Amiodarone bolus for VF – First dose: 300 mg, second dose: 150 mg • Magnesium for Torsade des pointes
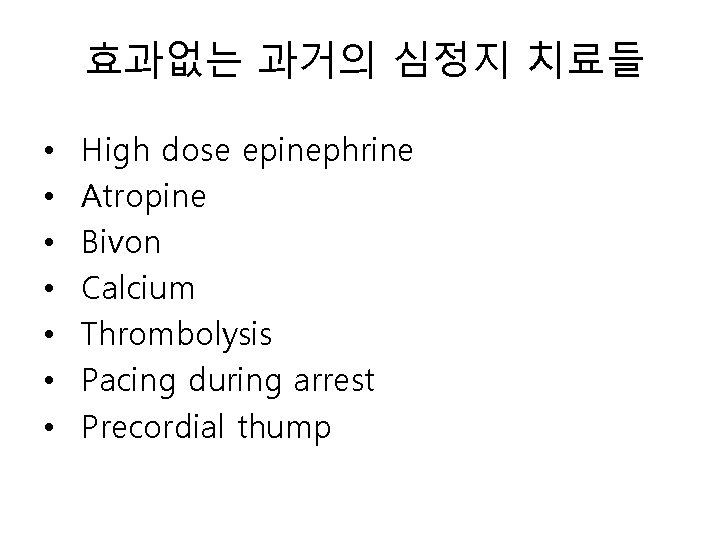
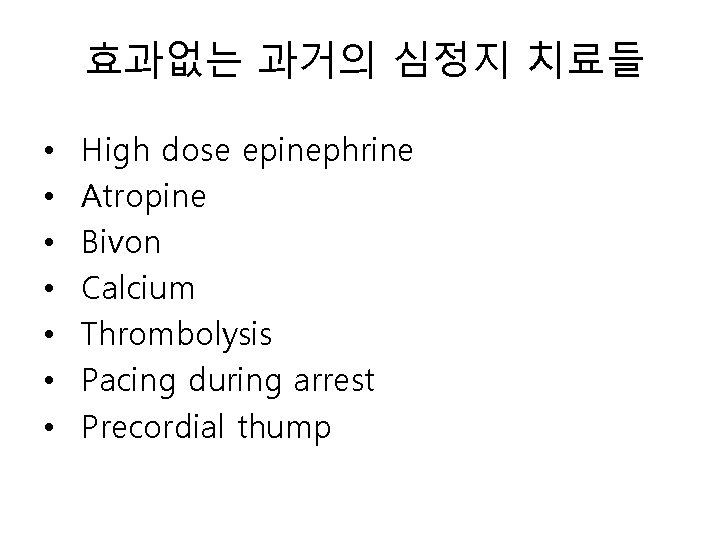
효과없는 과거의 심정지 치료들 • • High dose epinephrine Atropine Bivon Calcium Thrombolysis Pacing during arrest Precordial thump
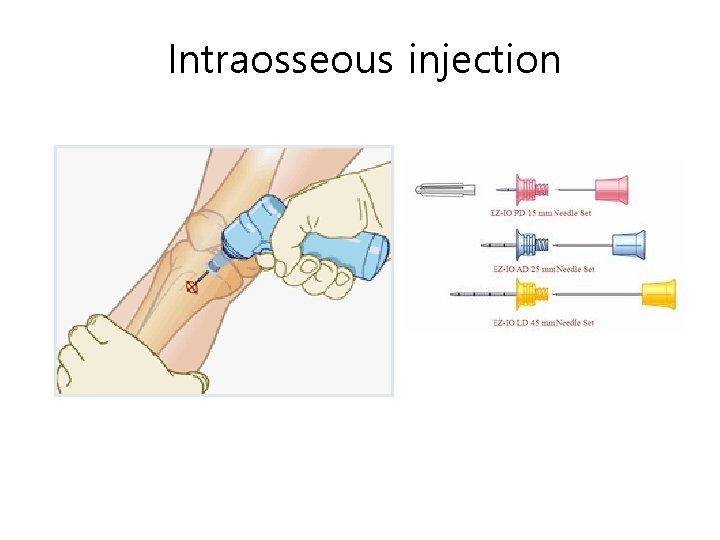
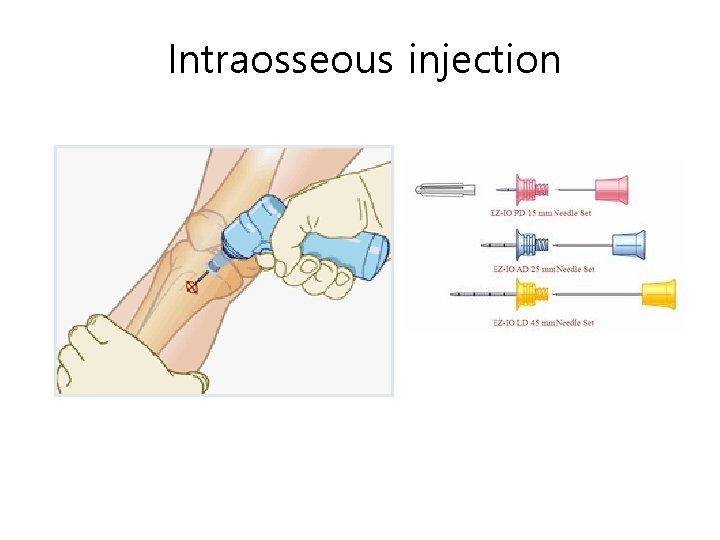
Intraosseous injection
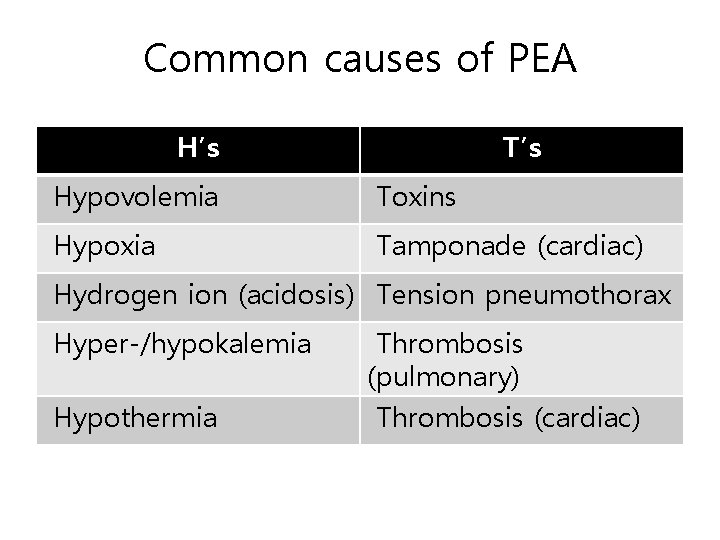
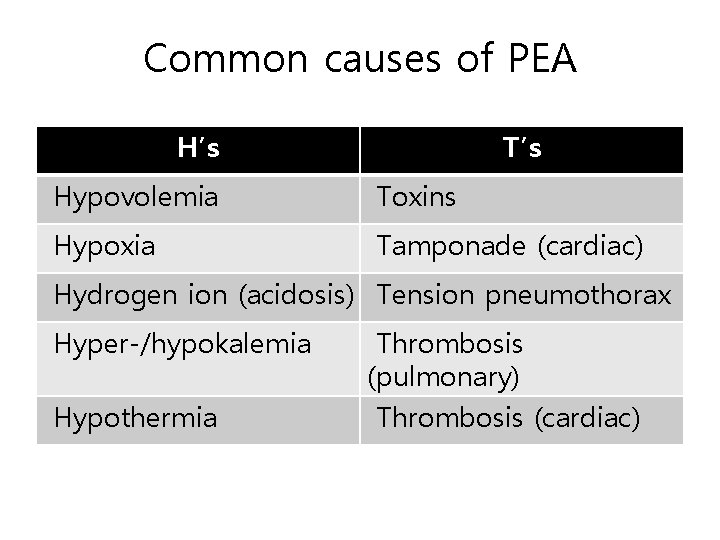
Common causes of PEA H’s T’s Hypovolemia Toxins Hypoxia Tamponade (cardiac) Hydrogen ion (acidosis) Tension pneumothorax Hyper-/hypokalemia Hypothermia Thrombosis (pulmonary) Thrombosis (cardiac)
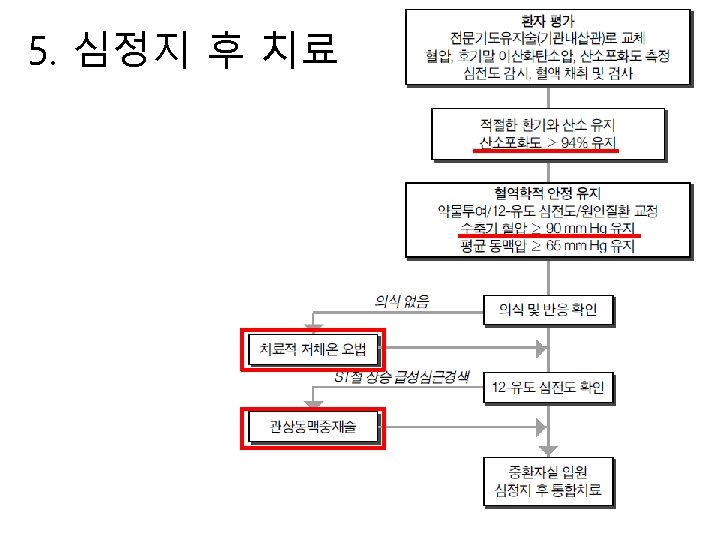
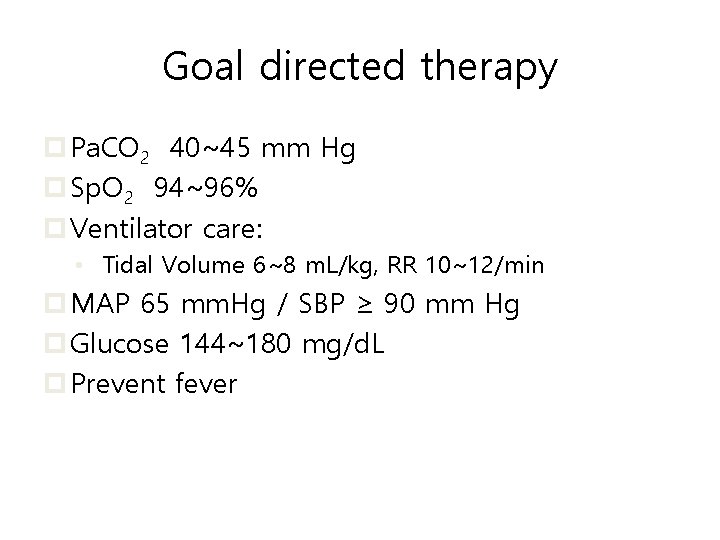
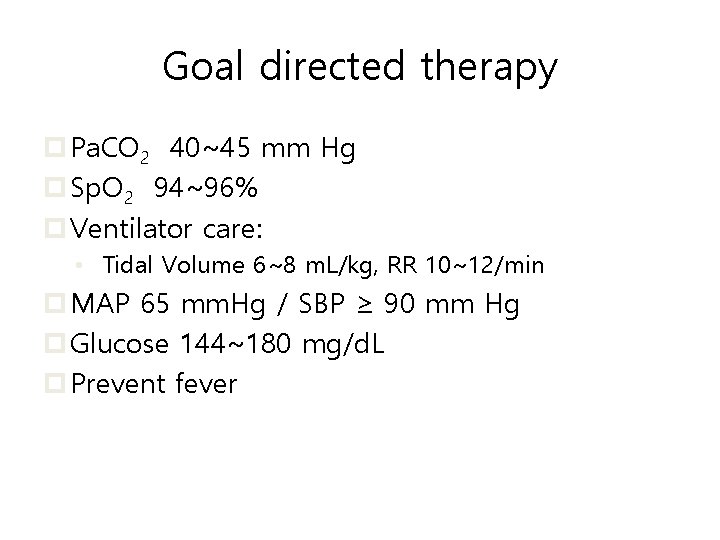
Goal directed therapy p Pa. CO 2 40~45 mm Hg p Sp. O 2 94~96% p Ventilator care: • Tidal Volume 6~8 m. L/kg, RR 10~12/min p MAP 65 mm. Hg / SBP ≥ 90 mm Hg p Glucose 144~180 mg/d. L p Prevent fever
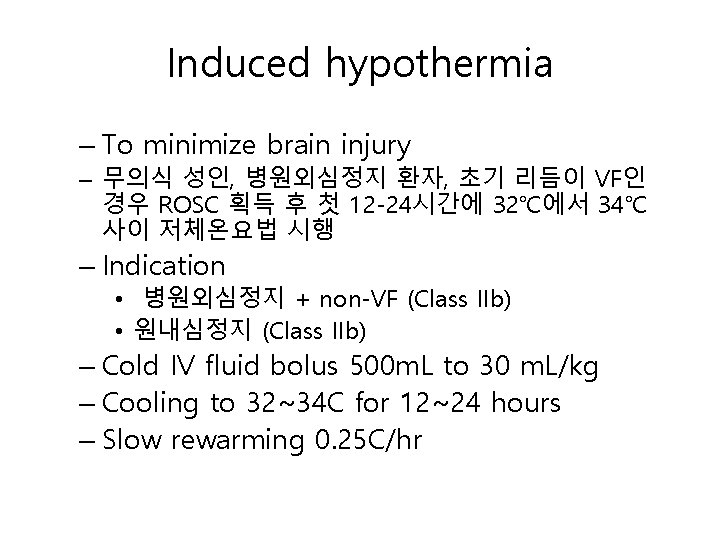
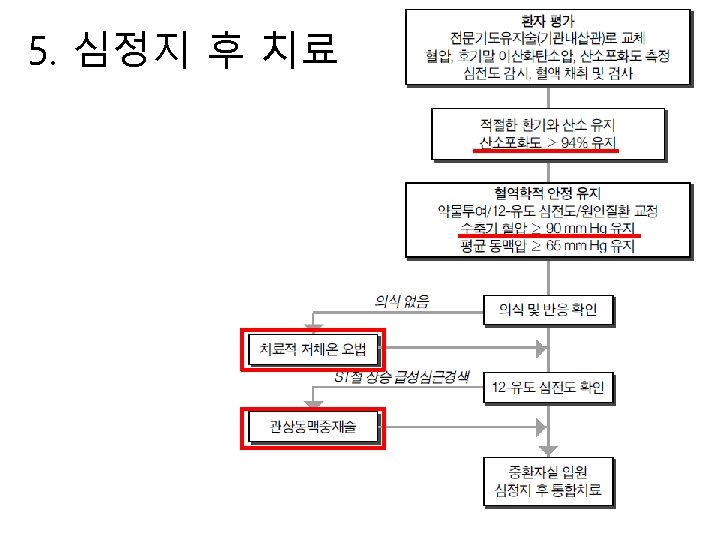
Induced hypothermia – To minimize brain injury – 무의식 성인, 병원외심정지 환자, 초기 리듬이 VF인 경우 ROSC 획득 후 첫 12 -24시간에 32℃에서 34℃ 사이 저체온요법 시행 – Indication • 병원외심정지 + non-VF (Class IIb) • 원내심정지 (Class IIb) – Cold IV fluid bolus 500 m. L to 30 m. L/kg – Cooling to 32~34 C for 12~24 hours – Slow rewarming 0. 25 C/hr
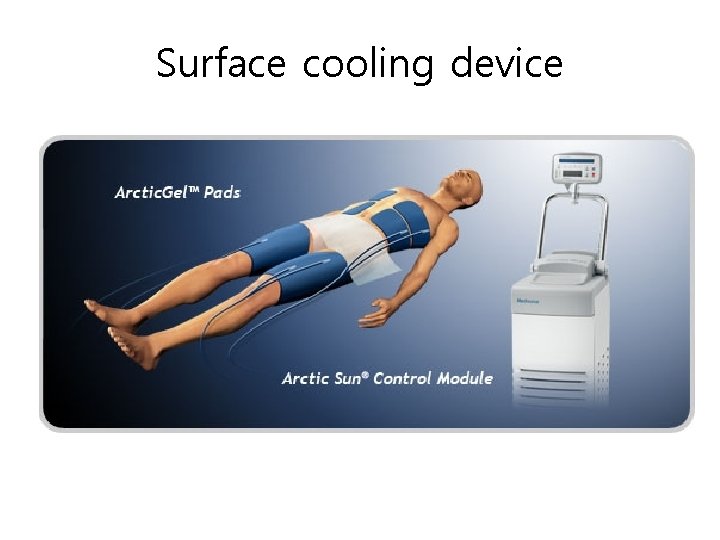
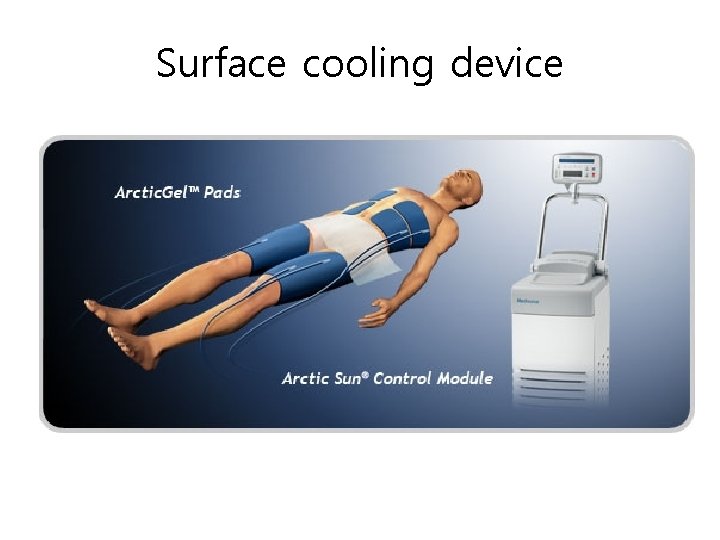
Surface cooling device

 High quality cpr infant
High quality cpr infant Push hard push fast fully recoil
Push hard push fast fully recoil Coronary perfusion pressure
Coronary perfusion pressure Ekg vf
Ekg vf State of survival survival of the fittest tweak
State of survival survival of the fittest tweak State of survival survival of the fittest stages
State of survival survival of the fittest stages Eltonian pyramid
Eltonian pyramid Adult chain of survival
Adult chain of survival Adult chain of survival
Adult chain of survival Adult chain of survival
Adult chain of survival Stemi chain of survival
Stemi chain of survival Ihca chain of survival exercise
Ihca chain of survival exercise Perform quality assurance
Perform quality assurance Quality management pmp
Quality management pmp What are quality standards in project management
What are quality standards in project management Quality improvement vs quality assurance
Quality improvement vs quality assurance Quality improvement vs quality assurance
Quality improvement vs quality assurance Quality control basics
Quality control basics American quality gurus
American quality gurus Crosby quality is free
Crosby quality is free What is tqm
What is tqm Contemporary management practices
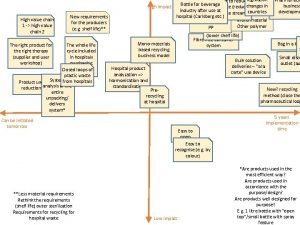
Contemporary management practices Value chain and supply chain difference
Value chain and supply chain difference Okc ckc
Okc ckc Extracorporeal cpr
Extracorporeal cpr 3 prinsip sebelum cpr
3 prinsip sebelum cpr Perbedaan cpr dan mpr
Perbedaan cpr dan mpr Bls algorithm
Bls algorithm Objectives of cpr
Objectives of cpr What is the secondary survey in first aid
What is the secondary survey in first aid Cpr infant breaths
Cpr infant breaths For adult
For adult Emotional cpr pdf
Emotional cpr pdf Cpr hand placement sternum
Cpr hand placement sternum What are the three c's of cpr
What are the three c's of cpr American heart association recommends child cpr for:
American heart association recommends child cpr for: Pulse check in child cpr
Pulse check in child cpr Cpr e 281
Cpr e 281 Dyrektywa cpr
Dyrektywa cpr Head tilt
Head tilt Cpr compression rate
Cpr compression rate When to stop cpr
When to stop cpr