Epidemiology and Control of MethicillinResistant Staphylococcus aureus in
- Slides: 30
Epidemiology and Control of Methicillin-Resistant Staphylococcus aureus in hospitals Maria Kapi, MD Registrar of Medical Microbiology Laiko General Hospital of Athens, Greece Readings: MRSA
What are MRSA? If we want to understand what are MRSA, we should first know: 1. 2. What are Staphylococci? What is Staphylococcus aureus?
What are MRSA? 3. What are penicillin and methicillin? 4. What are PBPs? 5. What are beta-lactams and beta- lactames?
Staphylococci: Gram positive cocci ( from Greek staphyle, means bunch of grapes ) that occur singly and in pairs, short chains and irregular grape-like clusters.
Staphylococcus aureus: is the staphylococcus which has the ability to clot plasma or in other words, which is coagulase positive. More than 80% of Staphylococcous aureus strains produce beta-lactamases.
Penicillin: is the antibiotic agent that Alexander Fleming a Scottish physician discovered in 1929. In 195 only 15% of S. aureus was susceptible to penicillin. Approximately 5% of S. aureus today are sensitive to penicillin.
Methicillin: was with oxacillin the new line of penicillins in 1959, which became a new hope to the treatment of St. aureus. In 1961 the St. aureus became resistant to methicillin. Strains that are oxacillin and methicillin resistant, historically termed Methicillin-Resistant S. aureus (MRSA)
PBPs: are penicillin-binding proteins. They are responsible for the final stages of peptidoglycan synthesis of the bacterial cell wall structure. Inhibition of one or more of these essential enzymes leads to bacterial lysis.
Beta lactams: are the antibiotics that contain the beta lactam ring. These are : penicillins, cephamycins, cephalosporins, carbapenems monobactams. The ring structure is common to all beta-lactams and must be intact for antibacterial action. They are cell wall synthesis inhibitors.
Beta lactamases: are enzymes that catalyse the hydrolysis of the betalactam ring and inactivate these group of antibiotics. Genes encoding these enzymes are widespread in the bacteria.
What MRSA are doing? Methicillin Resistant Staphylococcus aureus, when its cell is exposed to βlactam antibiotics, a supernumerary βlactam-resistant PBP (PBP 2 a), takes over the biosynthetic functions of the normal PBPs. This protein is responsible for the methicillin resistance.
Heteroresistance of MRSA All the cell in the population may have the genetic information for resistance , which is encoded by the mec. A gene. Only a small number of cells can actually express the resistant phenotype under in vitro testing conditions. This phenomenon is termed heteroresistance.
Why are MRSA important? 1. 2. Hospital –acquired infections. MRSA are common nosocomial pathogens around the world. The treatment is very difficult. Vancomycin often is the only drug of choice for severe infections.
Why are MRSA important? 3. MRSA with reduced susceptibility to glycopeptides. Since 1996 has been identified in Europe, Asia and United States. That increases the possibility some strains became fully resistant to glycopeptides. 4. MRSA are easily transmissible between patients.
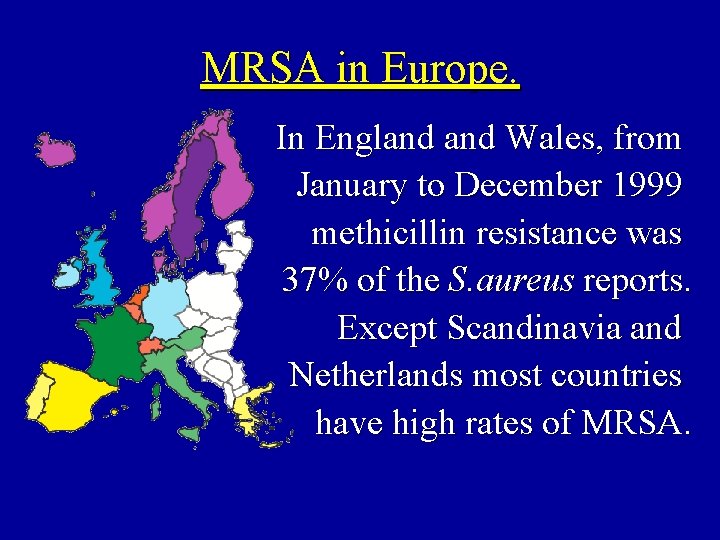
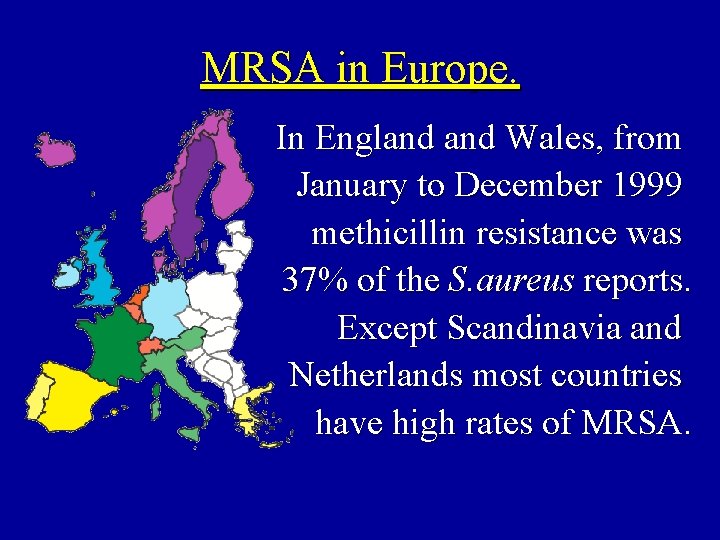
MRSA in Europe. In England Wales, from January to December 1999 methicillin resistance was 37% of the S. aureus reports. Except Scandinavia and Netherlands most countries have high rates of MRSA.
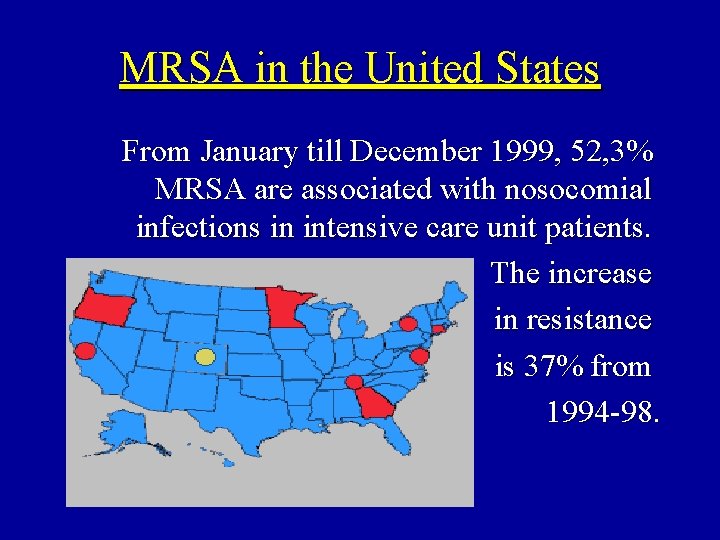
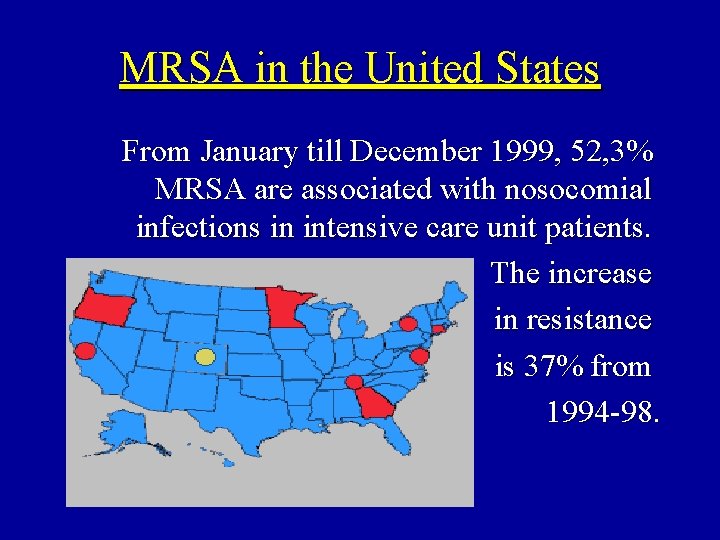
MRSA in the United States From January till December 1999, 52, 3% MRSA are associated with nosocomial infections in intensive care unit patients. The increase in resistance is 37% from 1994 -98.
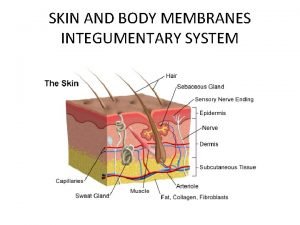
Epidemiology of MRSA Mode of Transmission. Is transmitted by contact with a person who has MRSA infection or is colonized with the organism. Hands of the health care workers is the most common mode of transmission from patient to patient.
Epidemiology of MRSA Reservoirs. Colonized and infected patients are the major reservoir of MRSA. Although has been isolated from environmental surfaces, these are not the most likely source of spread.
Epidemiology of MRSA. Risk factors. The factors that have been identified as increasing the risk of MRSA infection are: n Increased length of hospital stay n Multiple hospitalizations n Wounds
Epidemiology of MRSA. Risk factors Invasive procedures n Greater than 65 years old n Severe underlying disease. Administration of broad-spectrum antibiotics. n n
Costs of MRSA Directly attributable costs: n “ hotel costs” of extended lengths of stay n the cost of diagnostic procedures, n morbidity and mortality that can follow infection n glycopeptides are more expensive than other antibiotics e. t. c
Costs of MRSA Costs of control: n costs of involvement of the infection control team. n temporary closure of wards or theatres. n re-deployment of staff.
Control of MRSA in Hospitals General Principles: n Prevention of acquisition and spread of infection by patients and staff n Priorities are high risk units, such as intensive care units and patients who are susceptible to infection.
Control of MRSA in Hospitals n Handwashing. Health care workers should wash their hands before and after contact with all patients, even when gloves are worn. A written protocol detailing proper hand wash technique should be available for reference.
Control of MRSA in Hospitals n Gloves should be worn when in contact with any body substance. Gloves should be changed and hands washed immediately after contact with each resident. n Appropriate use of antimicrobials. Monitoring and auditing of drug use.
Control of MRSA in Hospitals n Isolation is necessary for infected patients and possible carriers in a single room or preferably in an isolation unit with designated staff. Isolation reduce staphylococcal crossinfection.
Control of MRSA in Hospitals n Ward Closure should be considered when new patients become infected with MRSA. The presence of strains of MRSA causing invasive infection is another indication. n Screening of patients for MRSA at the nose, throat and perineum.
Control of MRSA in Hospitals n Carriage of MRSA by health care workers. During outbreaks staff should be reminded of the handwashing and transient carriage of MRSA. Staff with infected or colonized lesions should not be at work especially in critical areas, as intensive care units, cardiothoracic words e. t. c.
Control of MRSA in Hospitals n Treatment of carriers. Nasal carriage is treated topical with mupirocin. n Systemic treatment of infections The glycopeptide antibiotics are currently the agents of choice for treatment. n Microbiological characterization of MRSA.
Antimicrobial resistance: is a major threat to public health. Bacterial resistance to multiple antibiotics characterises the present decade. Finding organisms resistant to over 10 different antibiotics is not unusual. Globally we need to look at how antibiotics are used and reduce their inappropriate use.
 Confirmatory test for staphylococcus aureus
Confirmatory test for staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus Portage staphylococcus aureus
Portage staphylococcus aureus Differential vs selective media
Differential vs selective media Micrococcaceae family
Micrococcaceae family Etiolgia
Etiolgia Blood agar
Blood agar Microbiology
Microbiology Staphylococcus aureus?
Staphylococcus aureus? Three domains of life
Three domains of life Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Site:slidetodoc.com
Site:slidetodoc.com Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus bacteria structure
Staphylococcus aureus bacteria structure Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Prokaryotic cells
Prokaryotic cells Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Cocci
Cocci White
White Enterobacter aerogenes gram positive or negative
Enterobacter aerogenes gram positive or negative Streptococcus aureus
Streptococcus aureus Streptococcus aureus
Streptococcus aureus Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Define nutritional epidemiology
Define nutritional epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Incidence and prevalence meaning
Incidence and prevalence meaning Epidemiology person place time
Epidemiology person place time Agar
Agar Coagulaza
Coagulaza Coagulase negative staphylococcus
Coagulase negative staphylococcus