Methicillinresistant Staphylococcus Aureus MRSA not just a healthcare




- Slides: 21
Methicillin-resistant Staphylococcus Aureus - (MRSA): not just a healthcare associated multi-drug resistant pathogen anymore Presenter: Zipporah Machuki
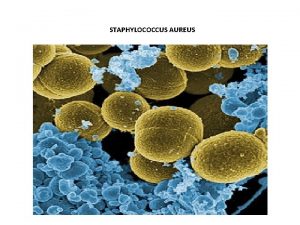
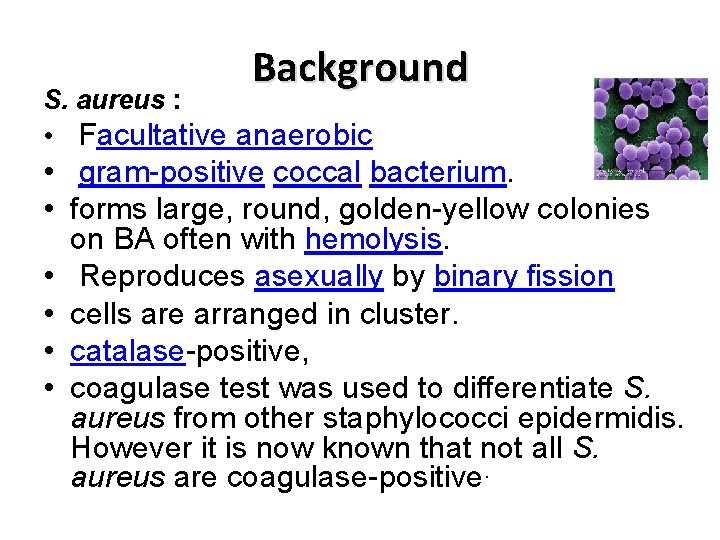
Background S. aureus : • Facultative anaerobic • gram-positive coccal bacterium. • forms large, round, golden-yellow colonies on BA often with hemolysis. • Reproduces asexually by binary fission • cells are arranged in cluster. • catalase-positive, • coagulase test was used to differentiate S. aureus from other staphylococci epidermidis. However it is now known that not all S. aureus are coagulase-positive.

• S. aureus commonly colonizes • Survives for a long time on skin or environment. • Mortality 80% prior to introduction of Penicillin. • Resistance to penicillin usually mediated by beta-lactamase,
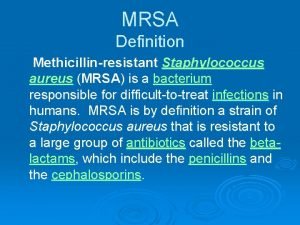
Methicillin • A penicillinase-resistant penicillin • First used in 1959 and • 2 years later S. aureus developed methicillin-resistance. • Due to acquisition of the mec. A gene. • Traditionally recognized as a nosocomial pathogen • Epidemiology has radically changed
Mode of action of methicillin • Bind to the native PBPs that are present in the S. aureus cell wall • Leads to the disruption of the synthesis of the peptidoglycan layer and therefore lysis of the S. aureus.
Methicillin Resistant S. aureus(MRSA) S. aureus(MRSA • Has a mec. A gene which is 2. 1 kb in length • mec. A gene codes for the 78 -k. Da penicillin binding protein (PBP) 2 a (or PBP 2’), • PBP 2 has decreased affinity for most beta -lactam antibiotics.
Mechanism of resistance • When PBP 2 a is produced, • the binding of the b-lactam antibiotics is hindered and • PBP 2 A (a transpeptidase), assisted by the transglycosylase domain of the native PBP 2 of S aureus, takes over the function of biosynthesis of cell-walls • Result in the growth of MRSA
staphylococcal cassette chromosome mec (SCCmec) • A mobile genomic island where mec. A gene is located. • Carries chromosome recombinances genes called ccr. A/ccr. B and ccr. C that enable excision and intergration into the host chromosome. • seven types main of SCCmec (SCCmec I to VII)
Epidemiology of MRSA • MRSA first identified in 1960 • became a common nosocomial infection in 1980. • Previously known to be only a nosocomial pathogen. • Risk factors associated with development of MRSA infections: (i) surgery, dialysis, hospitalization or residence in a long-term care facility within the prior year; (ii) indwelling percutaneous devices such as central venous catheters or feeding tubes; (iii)an MRSA infection identified more than 48 hours after hospital admission; or (iv)Had previously had. MRSA cultured
• MRSA cultured from patients with these risk factors are known as HA-MRSA. • major clones that disseminated internationally: Iberian, v Brazilian, v Hungarian, v New York/Japan, and v Paediatric clones • CA-MRSA is cultured from healthy and young individuals without any of these clinical risk factors.

Control of HA-MRSA • Screening of staff Health-care workers who are nasal carriers can serve as sources of MRSA transmission, • Isolation and barrier nursing Patients colonised or infected with MRSA • Hand hygiene Transient contamination of health-care workers’ hands • Environmental cleaning How important are contaminated environmental surfacesas a reservoir for MRSA?
Treatment of HA-MRSA • • Laptomycin, Linezolid, Tigecycline and Vancomycin Zhanel et al. 2013
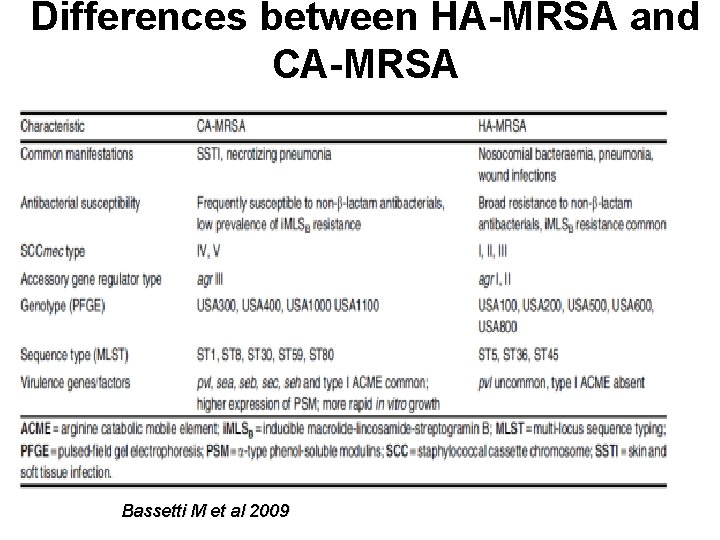
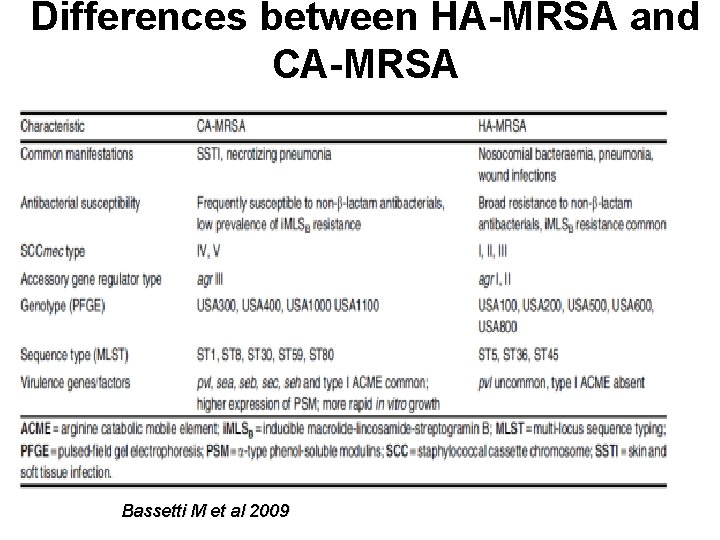
Differences between HA-MRSA and CA-MRSA Bassetti M et al 2009
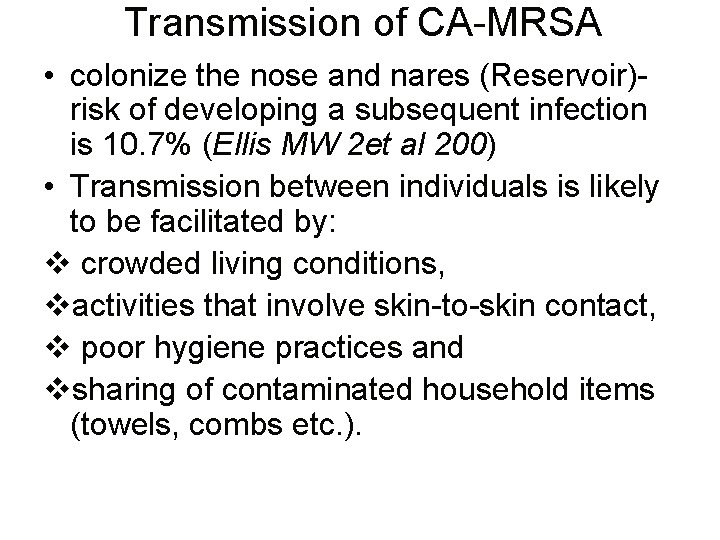
Transmission of CA-MRSA • colonize the nose and nares (Reservoir)risk of developing a subsequent infection is 10. 7% (Ellis MW 2 et al 200) • Transmission between individuals is likely to be facilitated by: v crowded living conditions, vactivities that involve skin-to-skin contact, v poor hygiene practices and vsharing of contaminated household items (towels, combs etc. ).
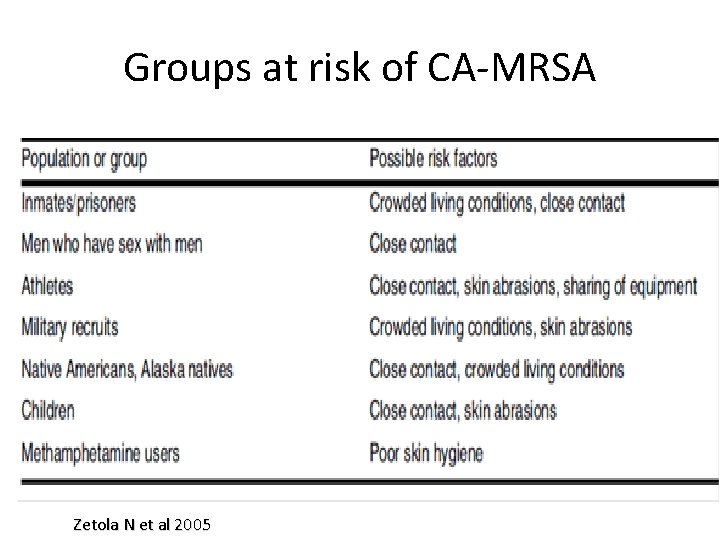
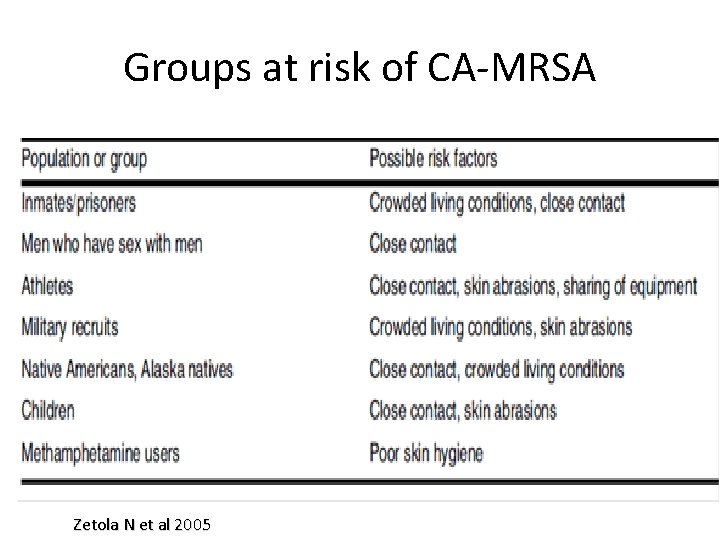
Groups at risk of CA-MRSA Zetola N et al 2005
CA-MRSA causes: • skin and soft tissue infections and • invasive disease such as vsepsis and vnecrotizing pneumonia
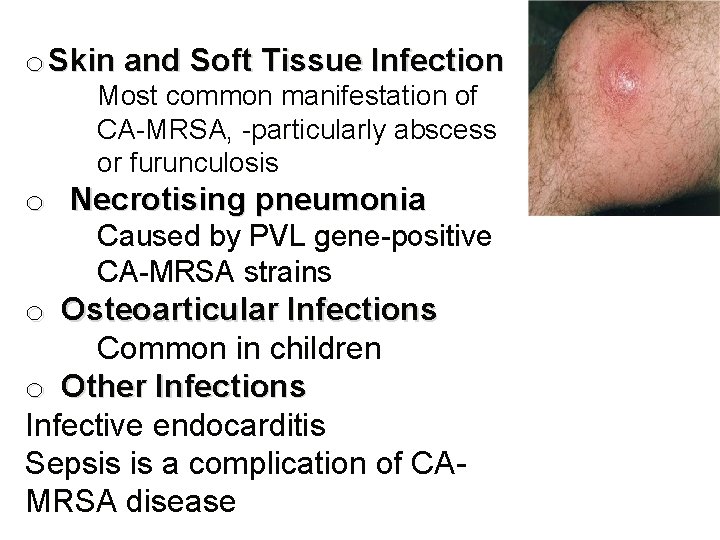
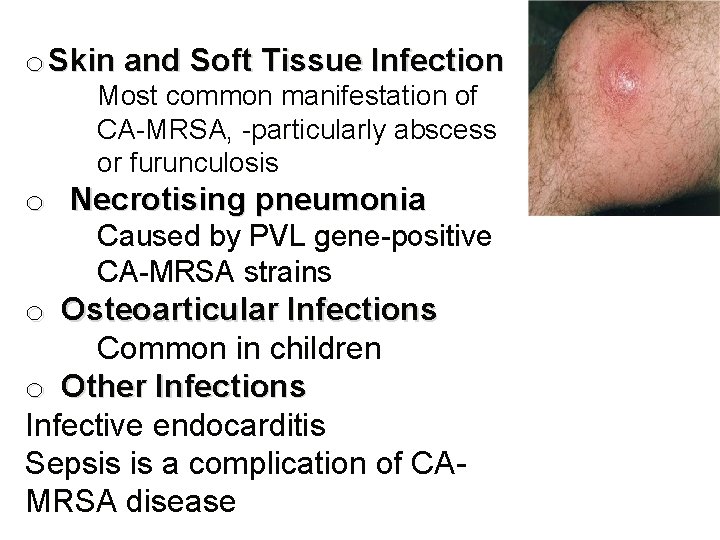
o Skin and Soft Tissue Infection Most common manifestation of CA-MRSA, -particularly abscess or furunculosis o Necrotising pneumonia Caused by PVL gene-positive CA-MRSA strains o Osteoarticular Infections Common in children o Other Infections Infective endocarditis Sepsis is a complication of CAMRSA disease
Treatment of CA-MRSA Infections • There is no defined optimum management of CA-MRSA infections. • Current strategies include a combination of pharmacological and nonpharmacological intervention eg In patients with recurrent infections, attempts to decolonize CA-MRSA

Commonly used antibiotic Agent comment Ceflobiprole Not yet widely availabel Clindamycin i. MLSβ resistance my reduce activity Daptomycin 6 mg/kg IV indicated for bacteraemia; do not use to treat pneumonia Linezolid Not recommended to treat bacteraemia Quinupristin/dalfopristin i. MLSβ resistance my reduce activity Tigecycline Tlow serum concentration so not recommended for bacteraemia treatment Cotrimoxazole Activity against GAS is unknown; Not for use in infants aged <2 mo or during 3 rd trimester of pregnance. Vanomycin Requires monitoring concentration when treating serious infections

 Micrococcaceae staphylococcus
Micrococcaceae staphylococcus Prokaryotic cells vs eukaryotic cells
Prokaryotic cells vs eukaryotic cells Staphylococcus aureus?
Staphylococcus aureus? Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus kingdom
Staphylococcus aureus kingdom Staphylocoque mrs1
Staphylocoque mrs1 Conjugation reproduction
Conjugation reproduction Epidermidis
Epidermidis Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Selective and differential media
Selective and differential media Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli Nitrate reduction test staphylococcus aureus
Nitrate reduction test staphylococcus aureus Confirmation test for staphylococcus aureus
Confirmation test for staphylococcus aureus Site:slidetodoc.com
Site:slidetodoc.com Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine meaning
Sports medicine meaning Not too big not too small just right
Not too big not too small just right Streptococcus aureus
Streptococcus aureus Staph aureus morphology
Staph aureus morphology