MRSA Definition Methicillinresistant Staphylococcus aureus MRSA is a



- Slides: 13
MRSA Definition Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium responsible for difficult-to-treat infections in humans. MRSA is by definition a strain of Staphylococcus aureus that is resistant to a large group of antibiotics called the betalactams, which include the penicillins and the cephalosporins.
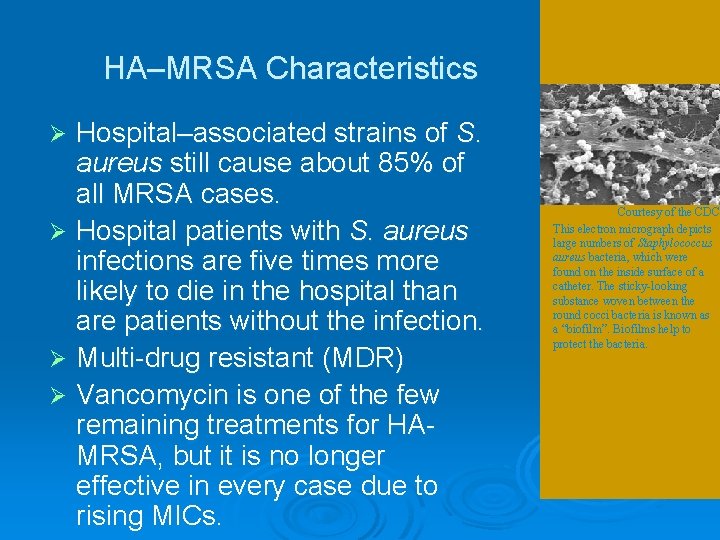
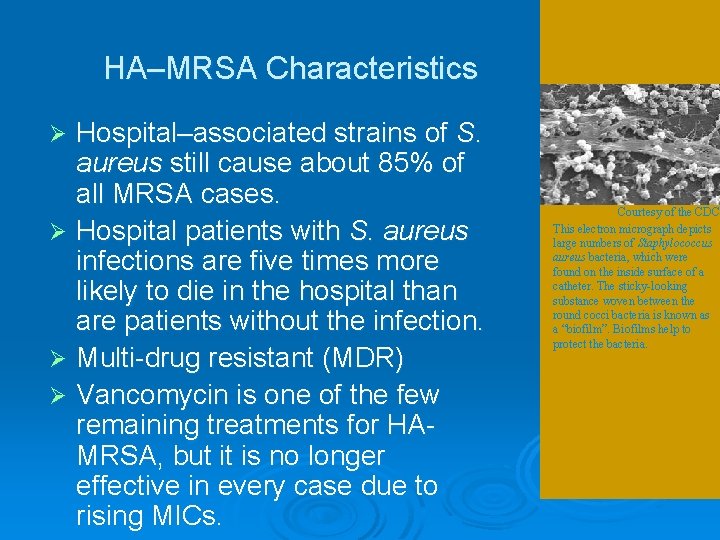
HA–MRSA Characteristics Hospital–associated strains of S. aureus still cause about 85% of all MRSA cases. Ø Hospital patients with S. aureus infections are five times more likely to die in the hospital than are patients without the infection. Ø Multi-drug resistant (MDR) Ø Vancomycin is one of the few remaining treatments for HAMRSA, but it is no longer effective in every case due to rising MICs. Ø Courtesy of the CDC This electron micrograph depicts large numbers of Staphylococcus aureus bacteria, which were found on the inside surface of a catheter. The sticky-looking substance woven between the round cocci bacteria is known as a “biofilm”. Biofilms help to protect the bacteria.

Evolution From HA and CA-MRSA 1961 – MRSA first described Ø Until recently, most MRSA infections started in hospitals, especially among surgery and immunocompromised patients. (HA-MRSA) Ø In the 1990 s, new strains of MRSA began to strike healthy people in community settings. (CA -MRSA) Ø These two types of MRSA are now known as hospital-associated MRSA (HA–MRSA) and community-associated MRSA (CA–MRSA). Ø
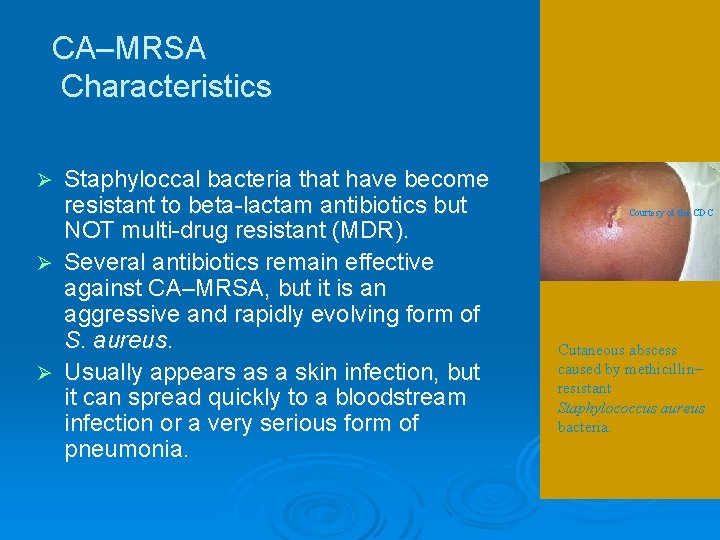
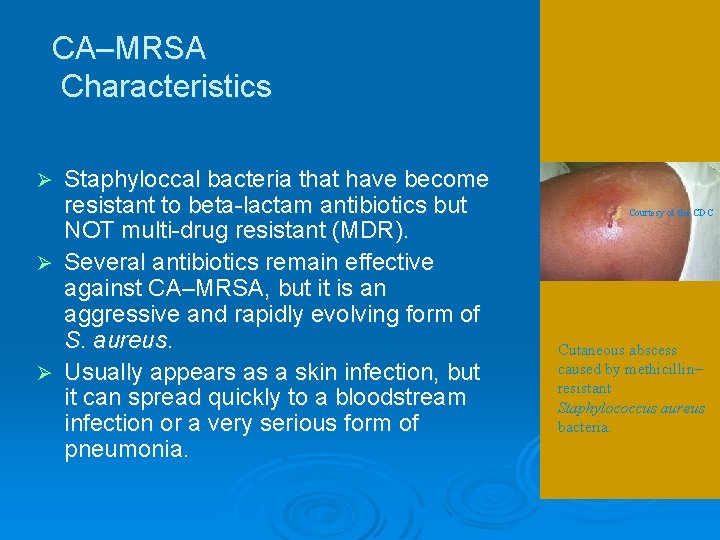
CA–MRSA Characteristics Staphyloccal bacteria that have become resistant to beta-lactam antibiotics but NOT multi-drug resistant (MDR). Ø Several antibiotics remain effective against CA–MRSA, but it is an aggressive and rapidly evolving form of S. aureus. Ø Usually appears as a skin infection, but it can spread quickly to a bloodstream infection or a very serious form of pneumonia. Ø Courtesy of the CDC Cutaneous abscess caused by methicillin– resistant Staphylococcus aureus bacteria.
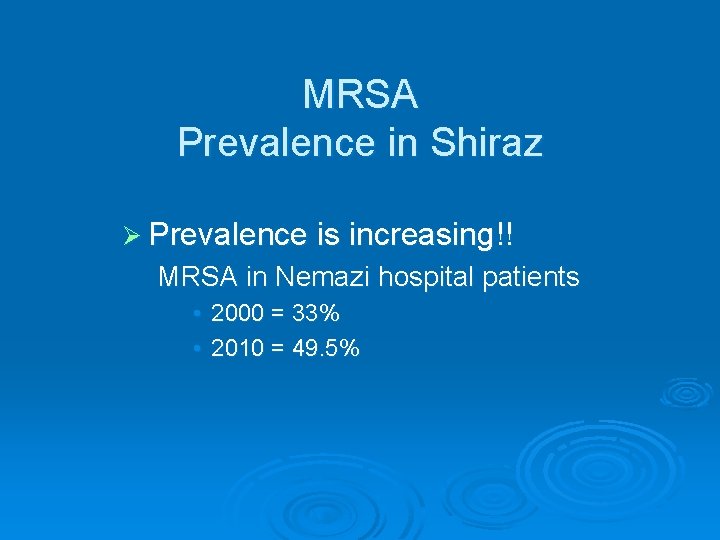
MRSA Prevalence in Shiraz Ø Prevalence is increasing!! MRSA in Nemazi hospital patients • 2000 = 33% • 2010 = 49. 5%
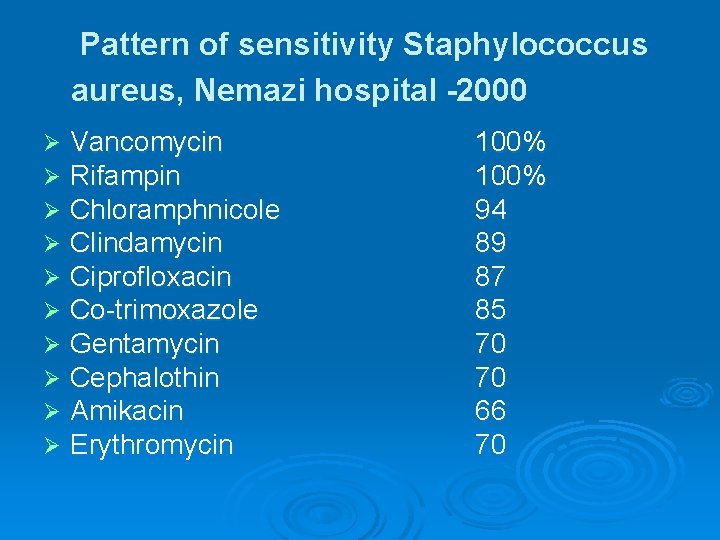
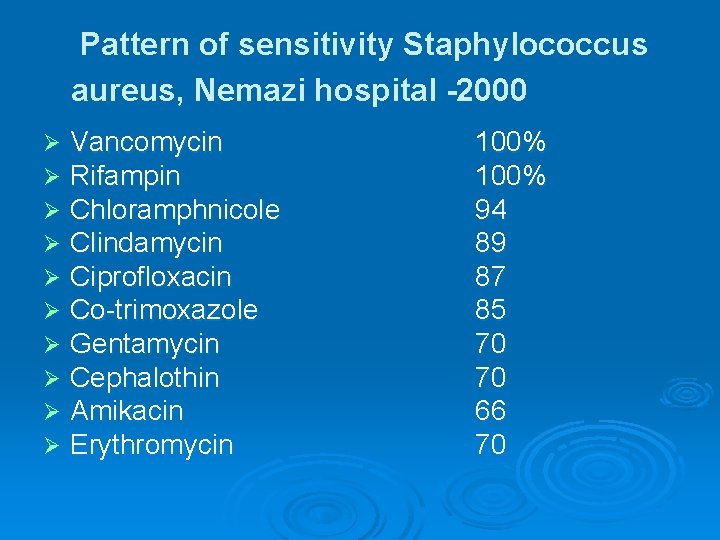
Pattern of sensitivity Staphylococcus aureus, Nemazi hospital -2000 Ø Ø Ø Ø Ø Vancomycin Rifampin Chloramphnicole Clindamycin Ciprofloxacin Co-trimoxazole Gentamycin Cephalothin Amikacin Erythromycin 100% 94 89 87 85 70 70 66 70

IR R Total Clindamycin Rifampicin 50 (53. 8) 56 (60. 2) 71 (76. 3) 1 (1. 1) 3 (3. 2) 2 (2. 2) 33 (35. 5) 84 (90. 3) 93 (100) 93 93 (100) ) 93 (100) Cefexime Erythromycin 65 44 58 (69. 9) (47. 3) (62. 4) Ciprofloxacin 93 (100) Oxacillin Cotrimoxazol Linozolid 9 93 60 (64. 5) (9. 7) (100) Vancomycin S Penicillin G Gentamicin Staphylococcus aureus antibiotic pattern in nemazi hospital -2010 27 (29) 46 33 (49. 5) (35. 5) 43 (46. 2) 37 (39. 8) 21 (22. 6) 92 (98. 9) 93 (100) 93 (100)
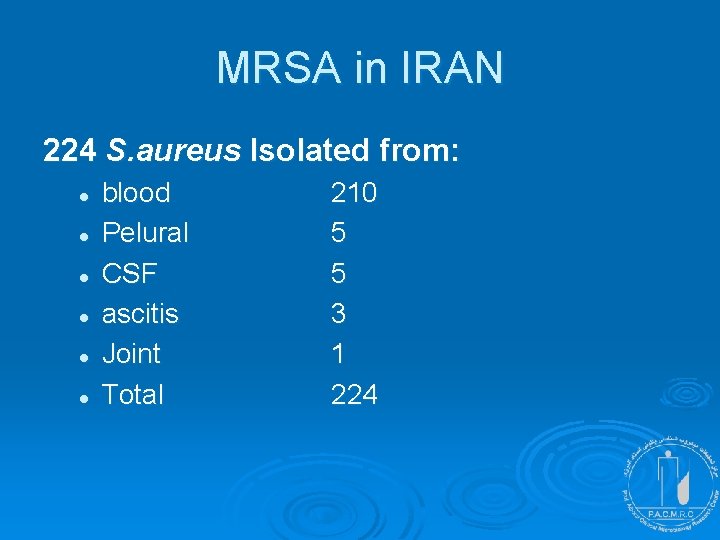
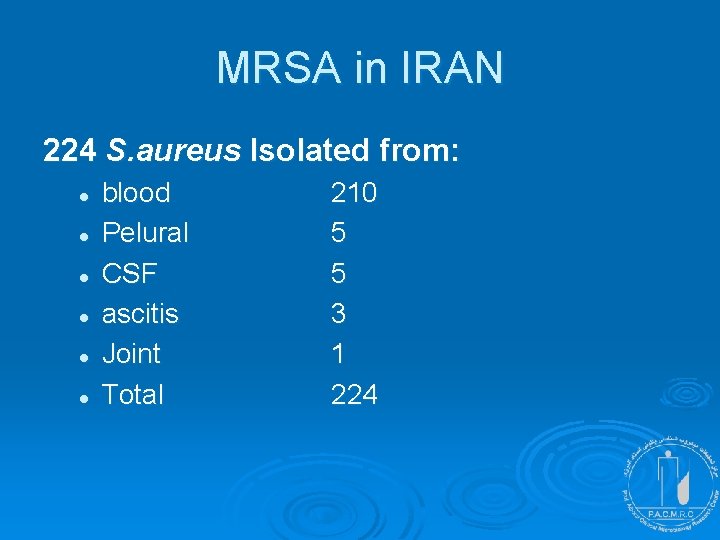
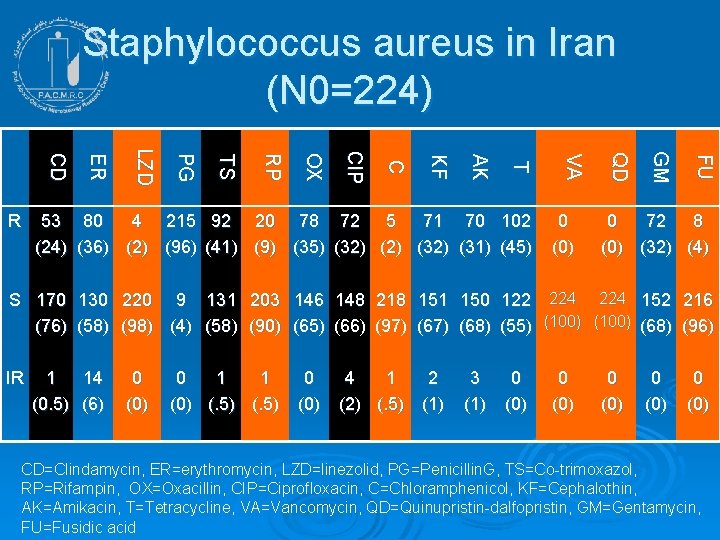
MRSA in IRAN 224 S. aureus Isolated from: l l l blood Pelural CSF ascitis Joint Total 210 5 5 3 1 224
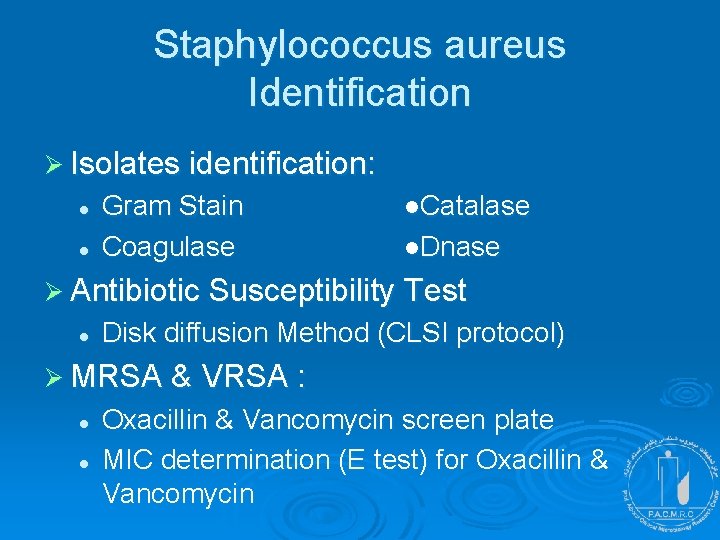
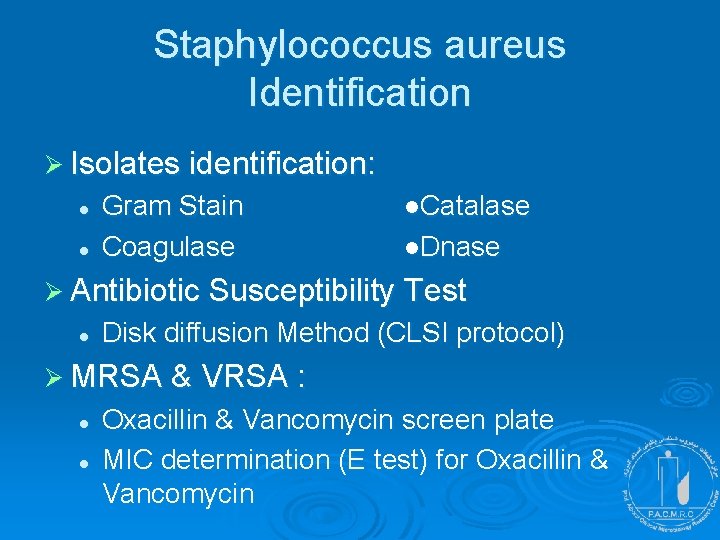
Staphylococcus aureus Identification Ø Isolates identification: l l Gram Stain Coagulase ●Catalase ●Dnase Ø Antibiotic Susceptibility Test l Disk diffusion Method (CLSI protocol) Ø MRSA & VRSA : l l Oxacillin & Vancomycin screen plate MIC determination (E test) for Oxacillin & Vancomycin
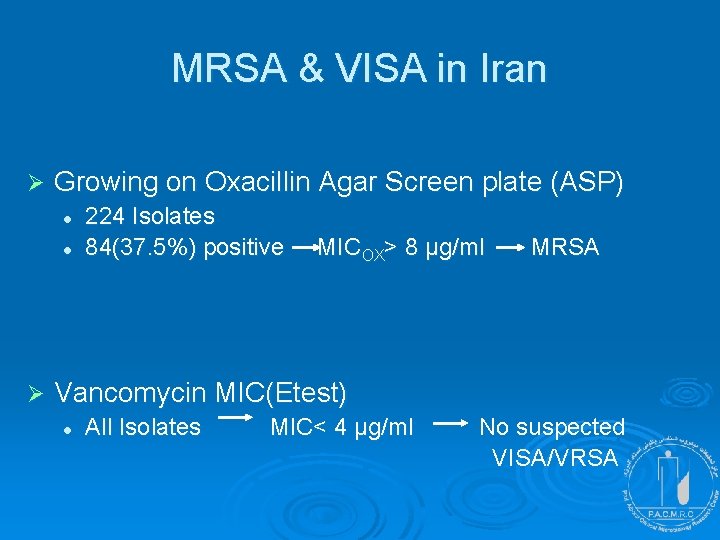
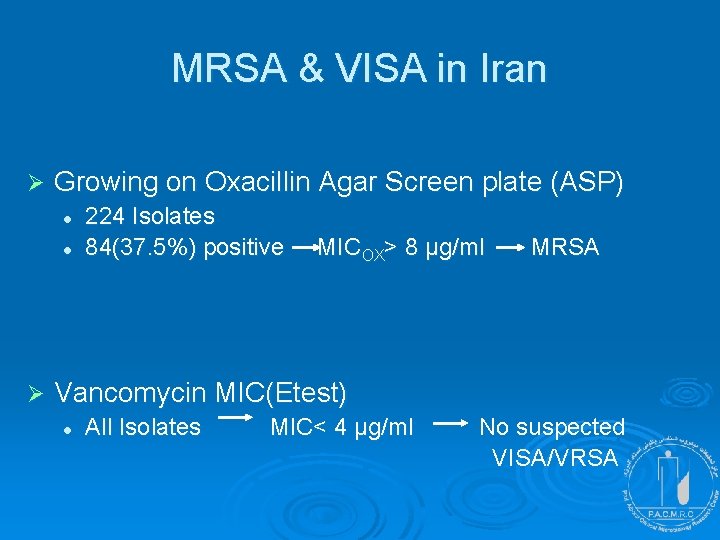
MRSA & VISA in Iran Ø Growing on Oxacillin Agar Screen plate (ASP) l l Ø 224 Isolates 84(37. 5%) positive MICOX> 8 μg/ml MRSA Vancomycin MIC(Etest) l All Isolates MIC< 4 μg/ml No suspected VISA/VRSA
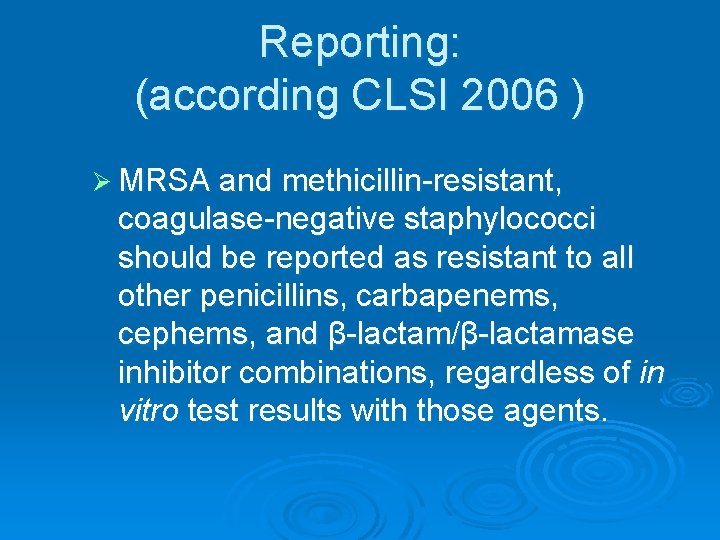
Reporting: (according CLSI 2006 ) Ø MRSA and methicillin-resistant, coagulase-negative staphylococci should be reported as resistant to all other penicillins, carbapenems, cephems, and β-lactam/β-lactamase inhibitor combinations, regardless of in vitro test results with those agents.
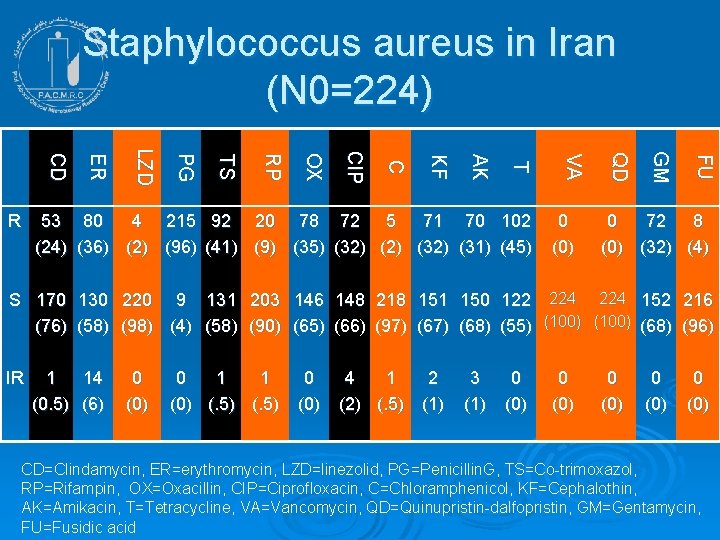
Staphylococcus aureus in Iran (N 0=224) FU GM 0 (0) QD 53 80 4 215 92 20 78 72 5 71 70 102 (24) (36) (2) (96) (41) (9) (35) (32) (31) (45) VA T AK KF C CI P OX RP TS PG LZ D ER CD R 0 72 8 (0) (32) (4) S 170 130 220 9 131 203 146 148 218 151 150 122 224 152 216 (76) (58) (98) (4) (58) (90) (65) (66) (97) (68) (55) (100) (68) (96) IR 1 14 (0. 5) (6) 0 (0) 0 1 1 (0) (. 5) 0 (0) 4 1 2 (2) (. 5) (1) 3 (1) 0 (0) 0 (0) CD=Clindamycin, ER=erythromycin, LZD=linezolid, PG=Penicillin. G, TS=Co-trimoxazol, RP=Rifampin, OX=Oxacillin, CIP=Ciprofloxacin, C=Chloramphenicol, KF=Cephalothin, AK=Amikacin, T=Tetracycline, VA=Vancomycin, QD=Quinupristin-dalfopristin, GM=Gentamycin, FU=Fusidic acid
