Staphylococcus Morphology Grampositive cocci in clusters Staphylococcus Streptococcus
- Slides: 39
Staphylococcus
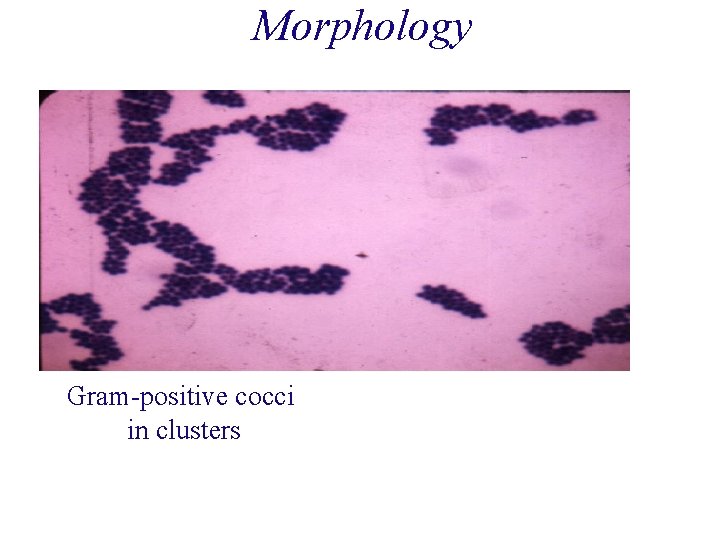
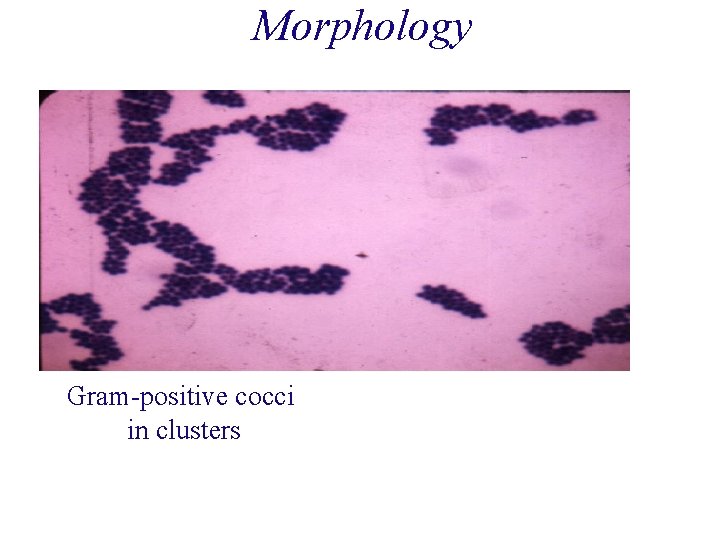
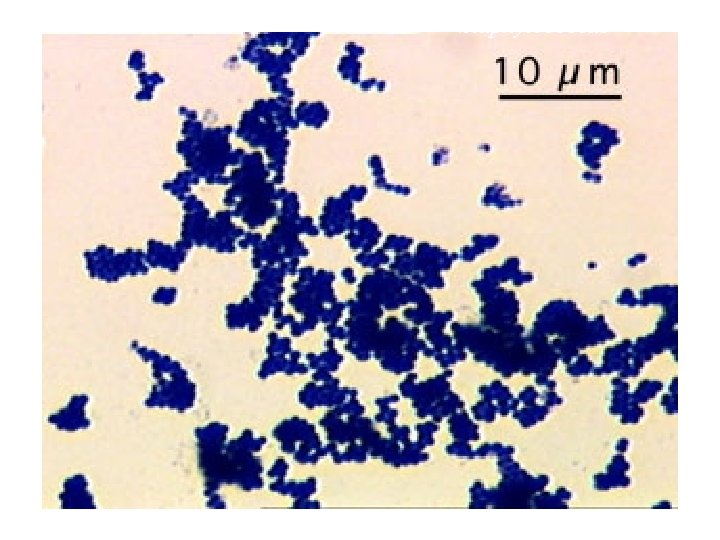
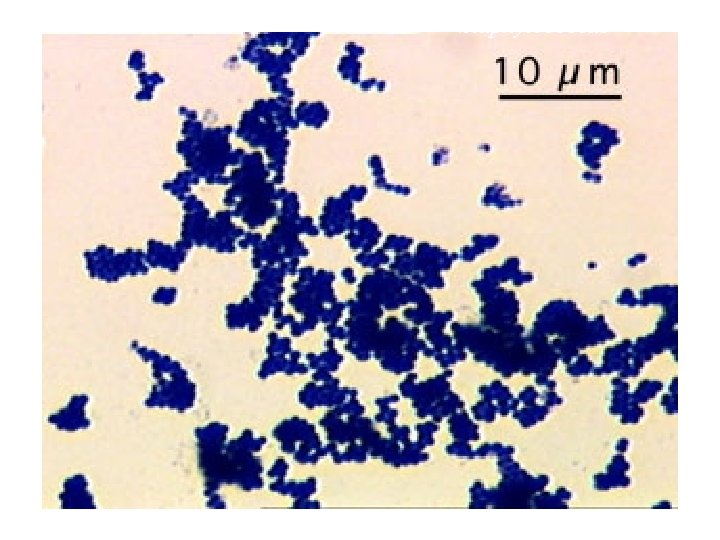
Morphology Gram-positive cocci in clusters
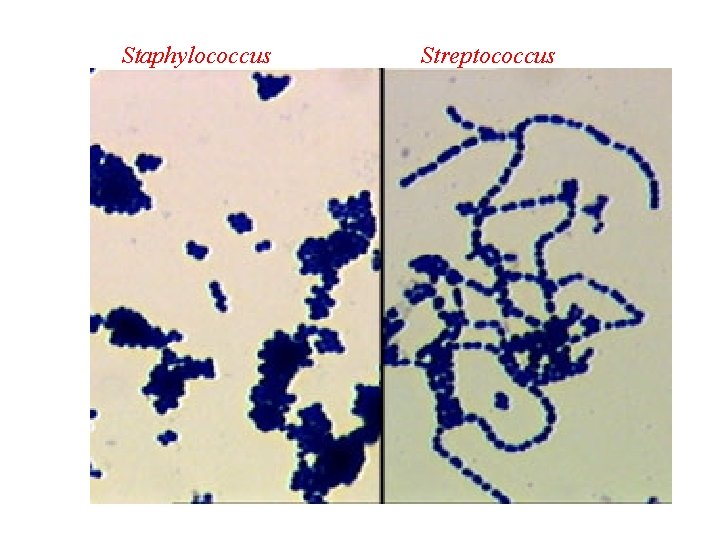
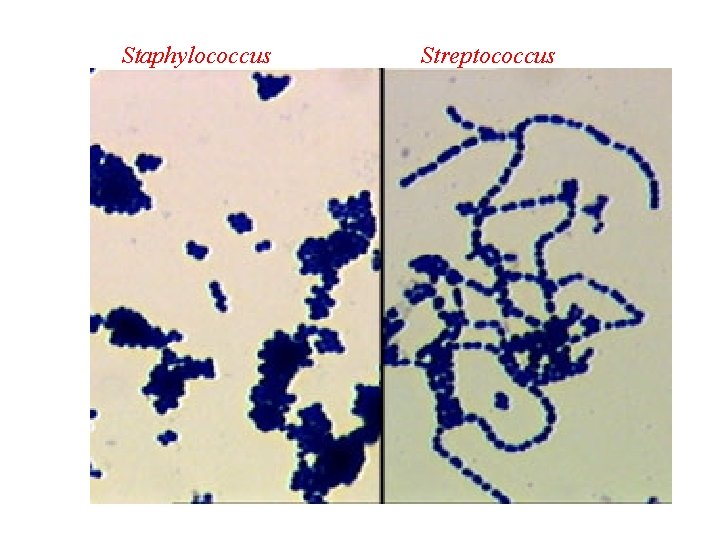
Staphylococcus Streptococcus
Staphylococcus
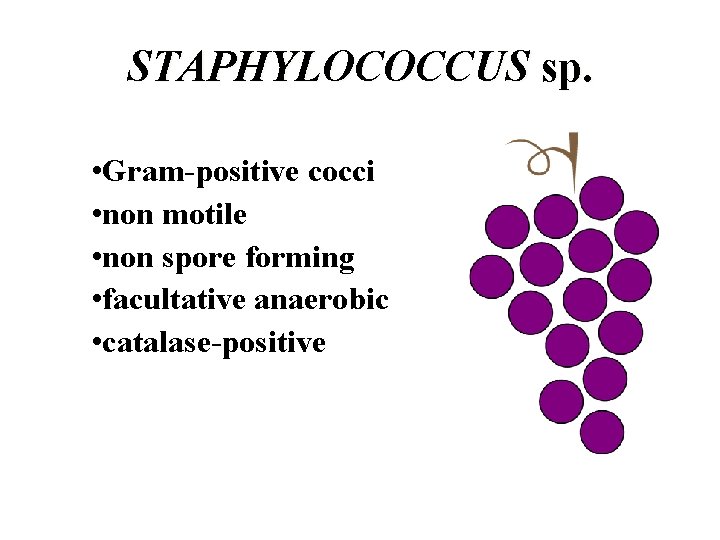
STAPHYLOCOCCUS sp. • Gram-positive cocci • non motile • non spore forming • facultative anaerobic • catalase-positive
STAPHYLOCOCCUS sp. Coagulase-positive Coagulase-negative S. aureus S. epidermidis S. Saprophyticus
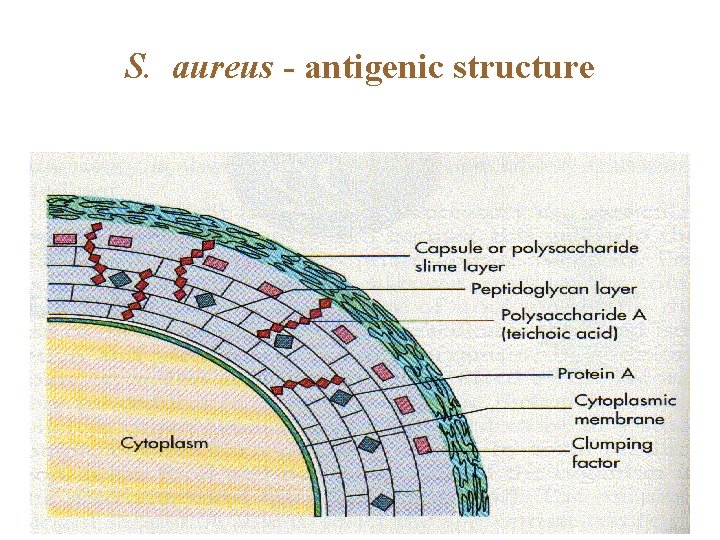
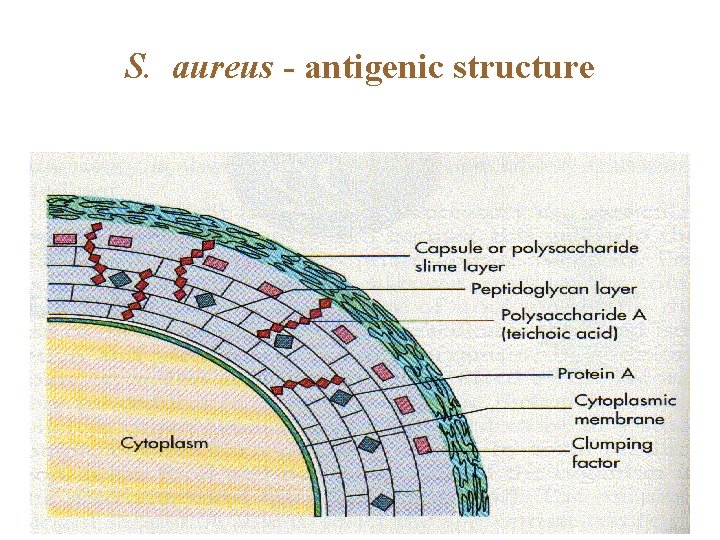
S. aureus - antigenic structure
Virulence Factors -Cell-Associated Capsule or slime layer (glycocalyx) Peptidoglycan (PG) Teichoic acid Protein A Clumping factor (bound coagulase)
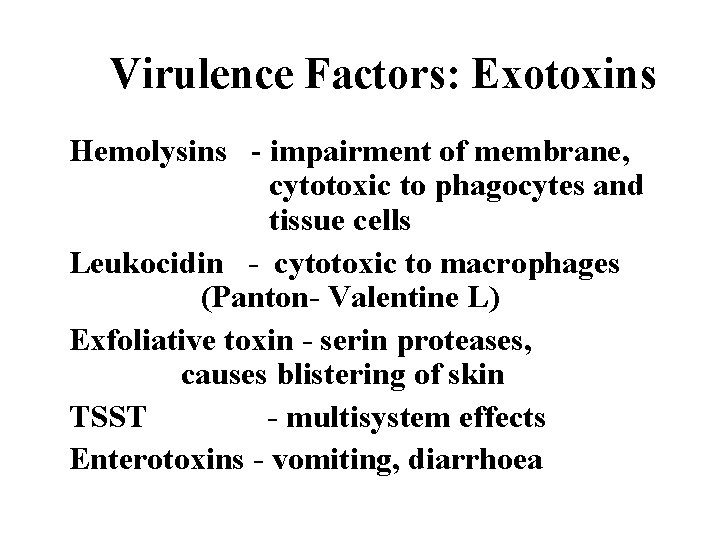
Virulence Factors: Exotoxins Hemolysins - impairment of membrane, cytotoxic to phagocytes and tissue cells Leukocidin - cytotoxic to macrophages (Panton- Valentine L) Exfoliative toxin - serin proteases, causes blistering of skin TSST - multisystem effects Enterotoxins - vomiting, diarrhoea
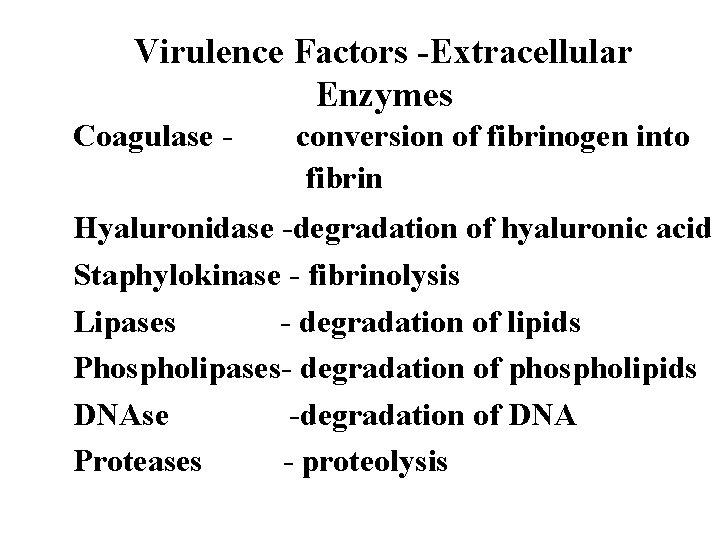
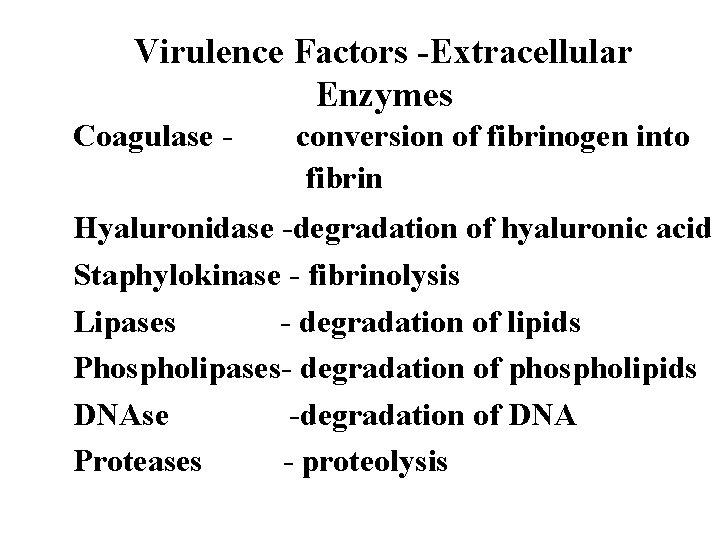
Virulence Factors -Extracellular Enzymes Coagulase - conversion of fibrinogen into fibrin Hyaluronidase -degradation of hyaluronic acid Staphylokinase - fibrinolysis Lipases - degradation of lipids Phospholipases- degradation of phospholipids DNAse -degradation of DNA Proteases - proteolysis
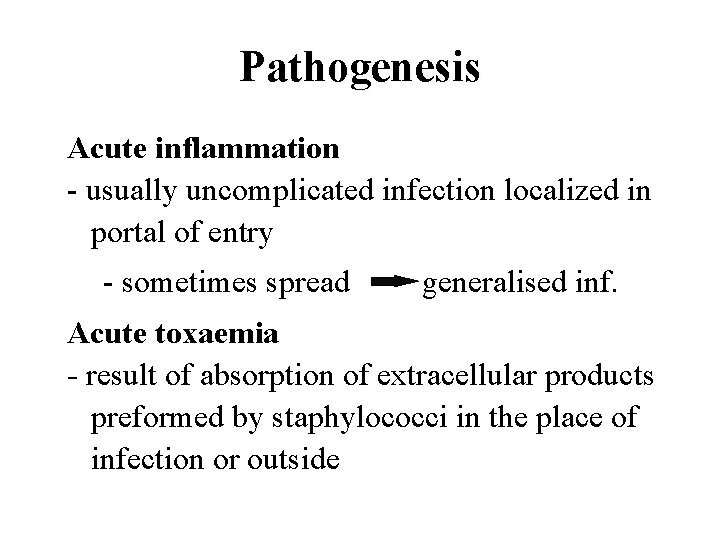
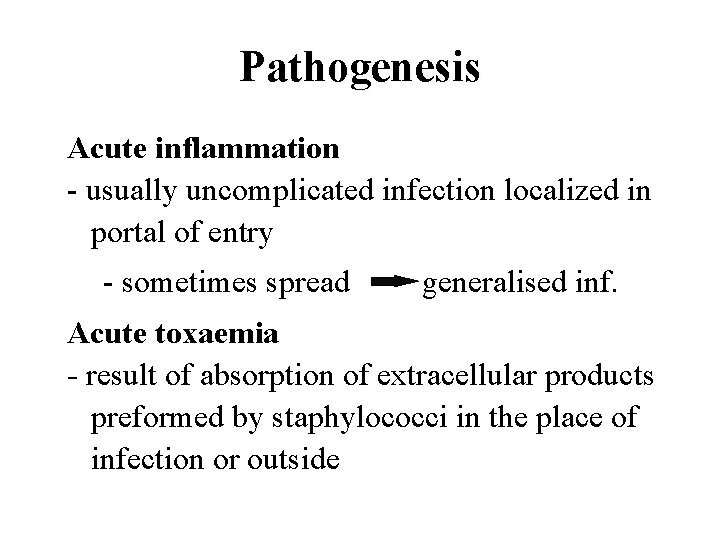
Pathogenesis Acute inflammation - usually uncomplicated infection localized in portal of entry - sometimes spread generalised inf. Acute toxaemia - result of absorption of extracellular products preformed by staphylococci in the place of infection or outside
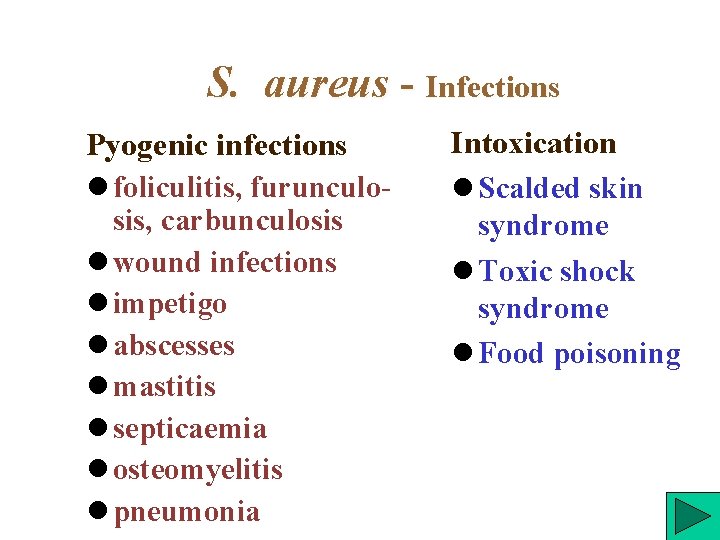
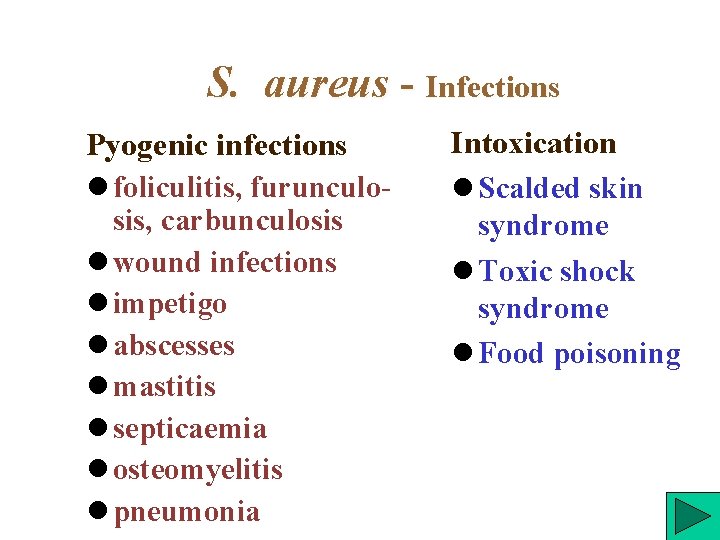
S. aureus - Infections Pyogenic infections foliculitis, furunculosis, carbunculosis wound infections impetigo abscesses mastitis septicaemia osteomyelitis pneumonia Intoxication Scalded skin syndrome Toxic shock syndrome Food poisoning
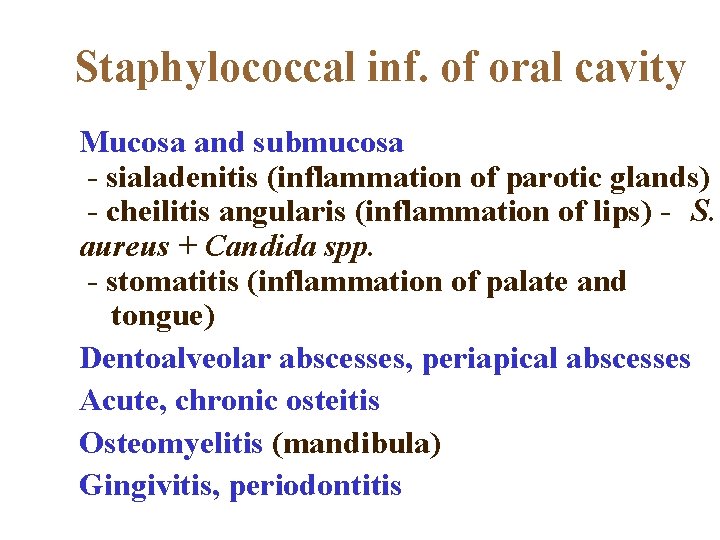
Staphylococcal inf. of oral cavity Mucosa and submucosa - sialadenitis (inflammation of parotic glands) - cheilitis angularis (inflammation of lips) - S. aureus + Candida spp. - stomatitis (inflammation of palate and tongue) Dentoalveolar abscesses, periapical abscesses Acute, chronic osteitis Osteomyelitis (mandibula) Gingivitis, periodontitis
A. Pyogenic infections Skin lesions Boils Styes Furuncles(infection of hair follicle) Carbuncles (infection of several hair follicles) Wound infections (progressive appearance of swelling and pain in a surgical wound after about 2 days from the surgery) Impetigo (skin lesion with blisters that break and become covered with crusting exudate)
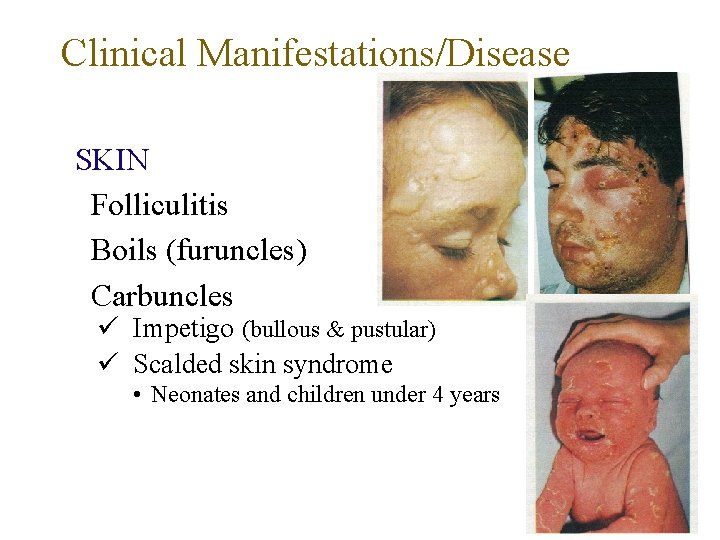
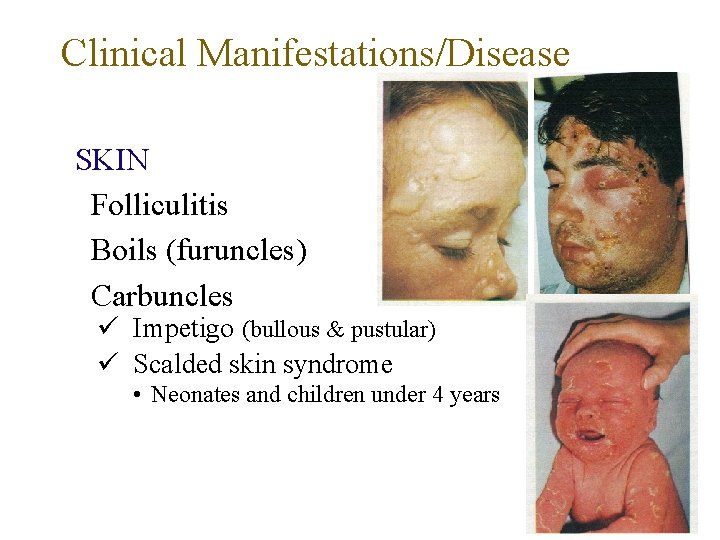
Clinical Manifestations/Disease SKIN Folliculitis Boils (furuncles) Carbuncles Impetigo (bullous & pustular) Scalded skin syndrome • Neonates and children under 4 years
Deep abscesses Can be single or multiple Breast abscess can occur in 1 -3% of nursing mothers in pueperium Can produce mild to severe disease Other sites - kidney, brain from septic foci in blood
Systemic Infections 1. With obvious focus Osteomyelitis, septic arthritis 2. No obvious focus Infective endocarditis, brain abscesses 3. Associated with predisposing factors Multiple abscesses, septicaemia (IV drug users) Staphylococcal pneumonia (Post viral)
B. Toxin mediated diseases 1. Staphylococcal food poisoning Due to production of entero toxins Heat stable entero toxin acts on gut Produces severe vomiting following a very short incubation period Resolves on its own within about 24 hours
2. Toxic shock syndrome High fever, diarrhoea, shock and erythematous skin rash which desquamate Mediated via ‘toxic shock syndrome toxin’ 10% mortality rate Described in two groups of patients Associated with young women using tampons during menstruation Described in young children and men
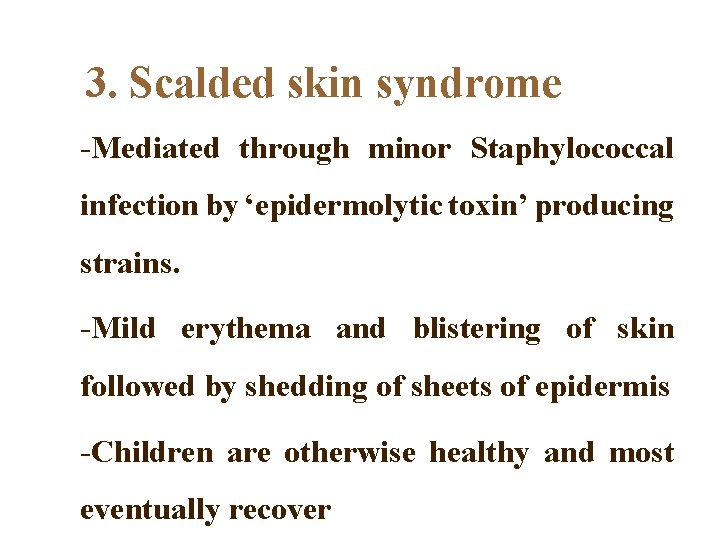
3. Scalded skin syndrome -Also known as Pemphigus neonatorum or Ritter's disease, or Localized bullous impetigo. -Disease of young children.
3. Scalded skin syndrome -Mediated through minor Staphylococcal infection by ‘epidermolytic toxin’ producing strains. -Mild erythema and blistering of skin followed by shedding of sheets of epidermis -Children are otherwise healthy and most eventually recover
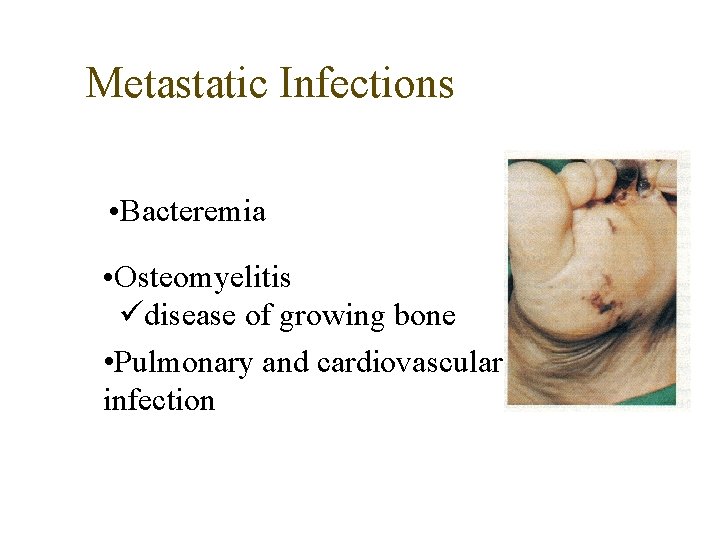
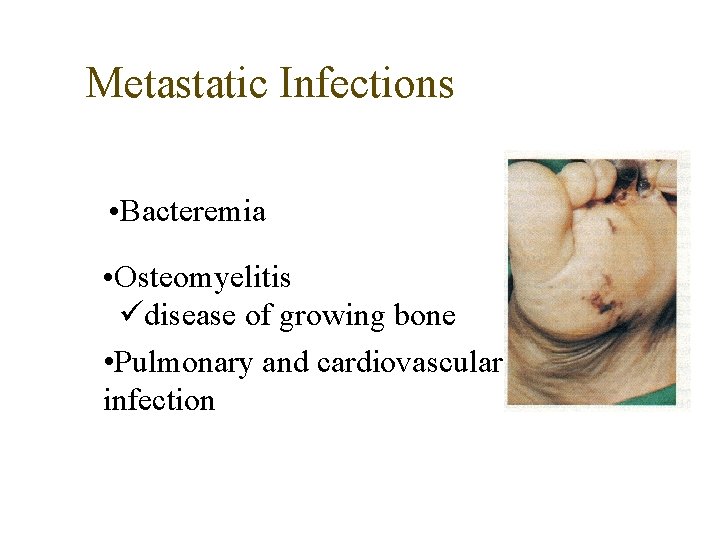
Metastatic Infections • Bacteremia • Osteomyelitis disease of growing bone • Pulmonary and cardiovascular infection
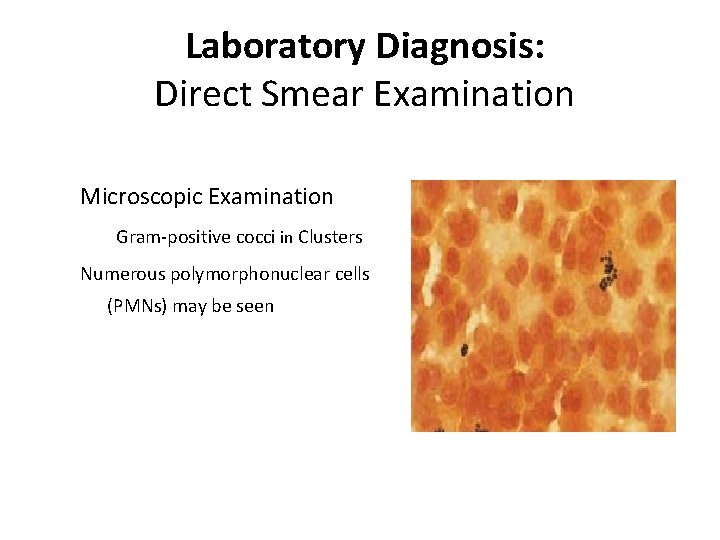
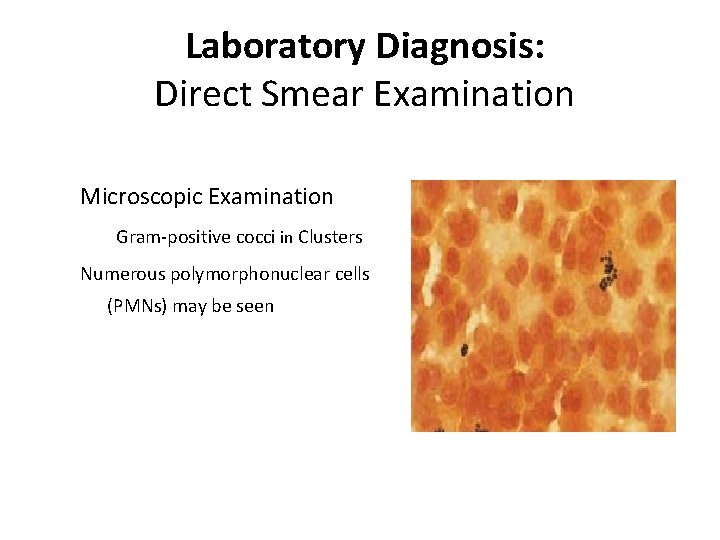
Laboratory Diagnosis: Direct Smear Examination Microscopic Examination Gram-positive cocci in Clusters Numerous polymorphonuclear cells (PMNs) may be seen Insert Figure 10 -1
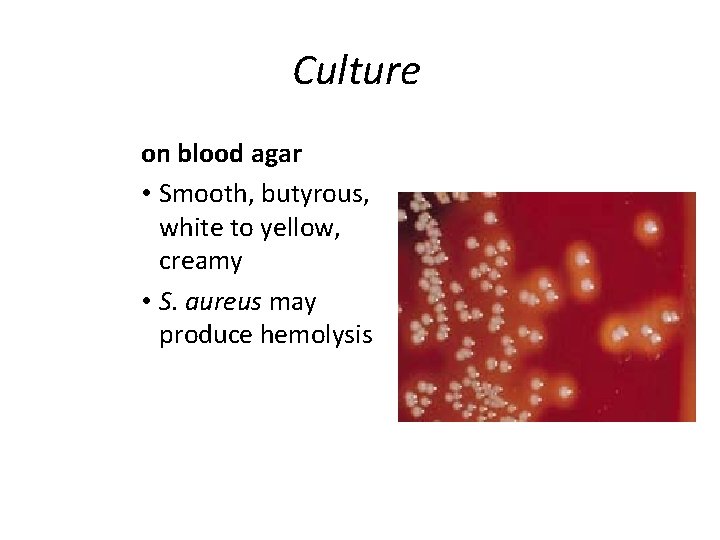
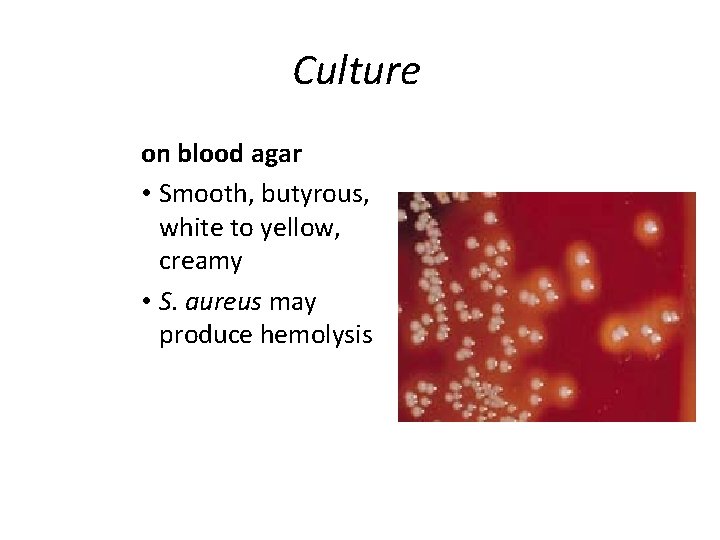
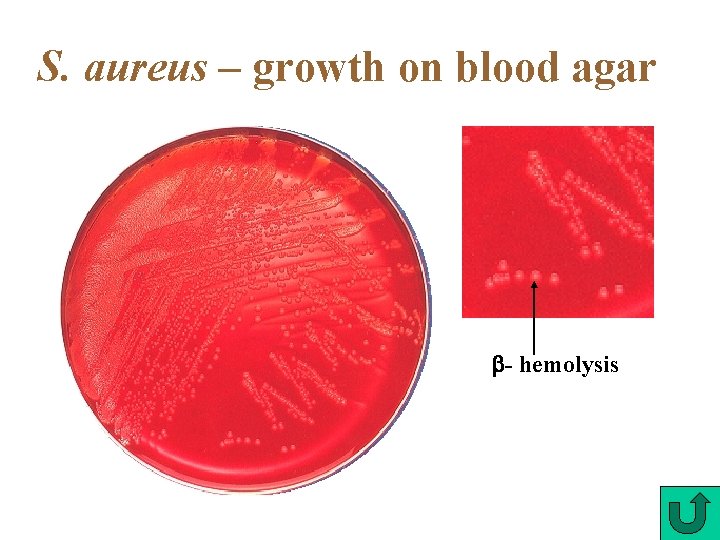
Culture on blood agar • Smooth, butyrous, white to yellow, creamy • S. aureus may produce hemolysis S. aureus
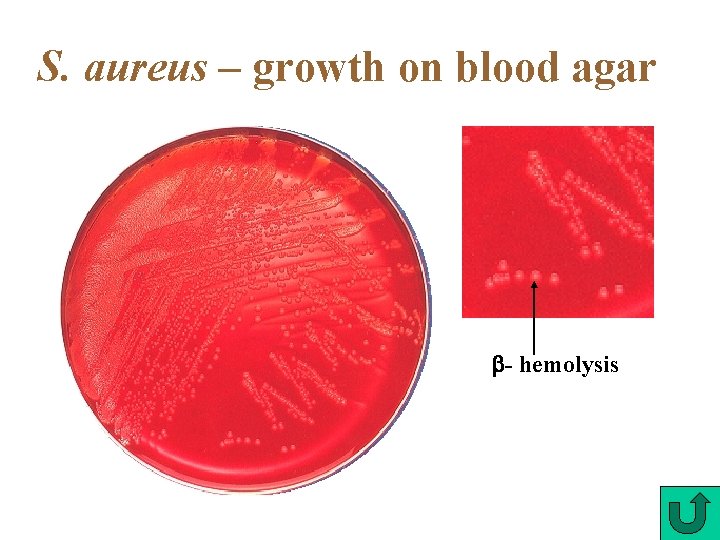
S. aureus – growth on blood agar - hemolysis
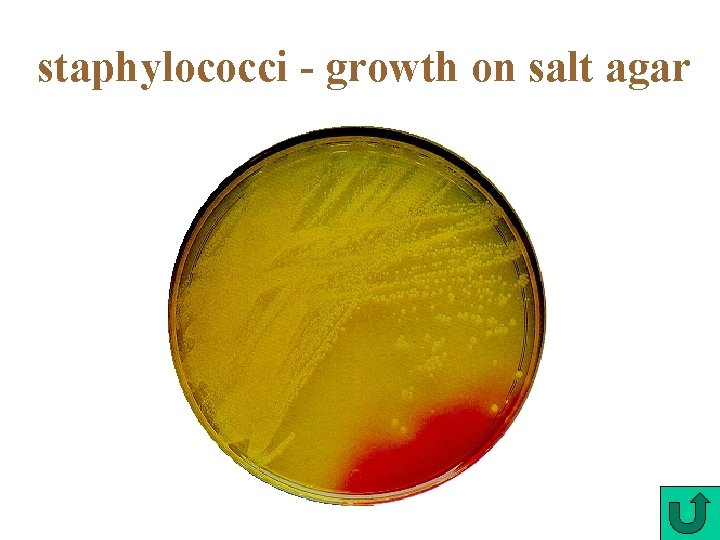
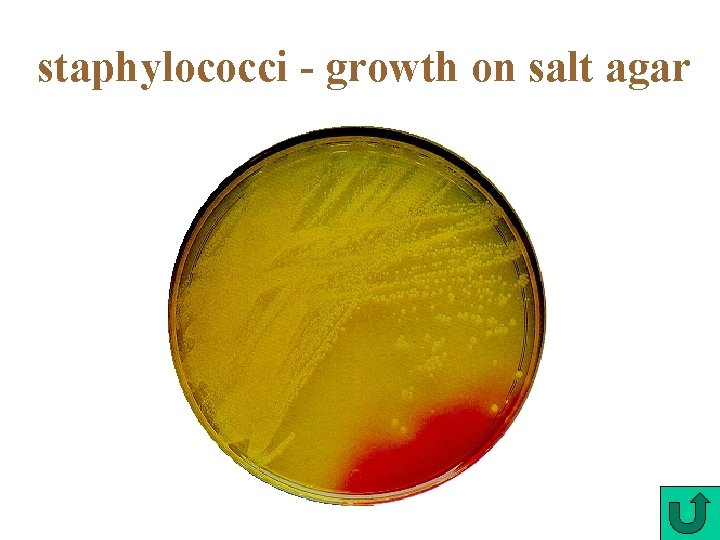
staphylococci - growth on salt agar
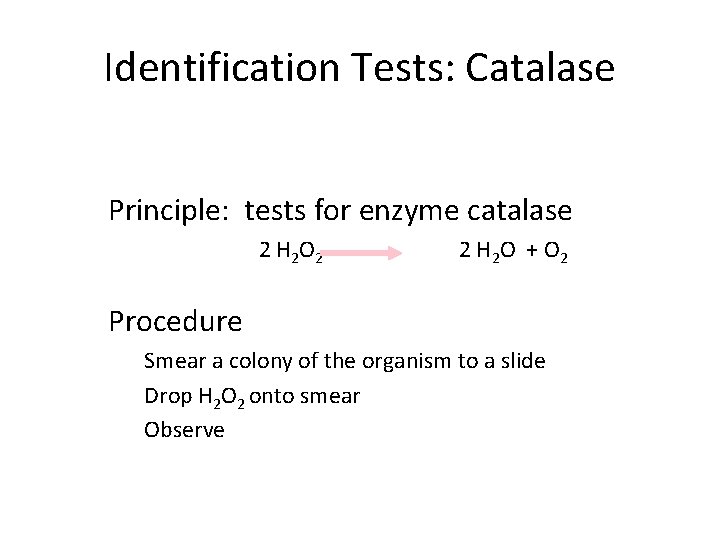
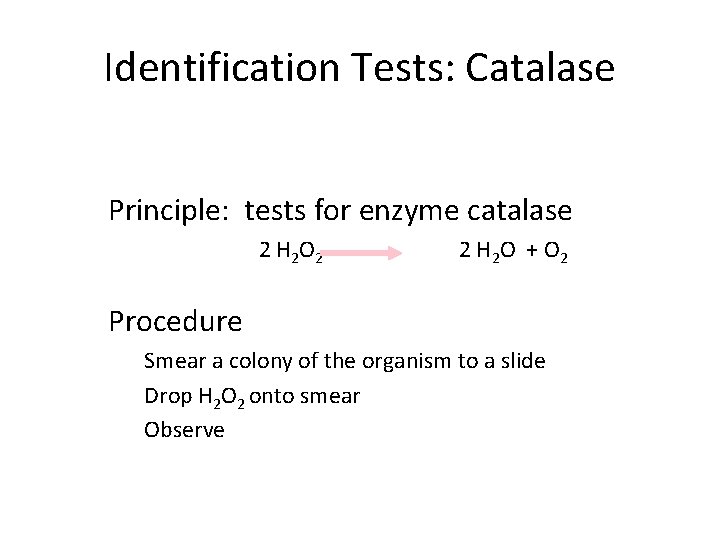
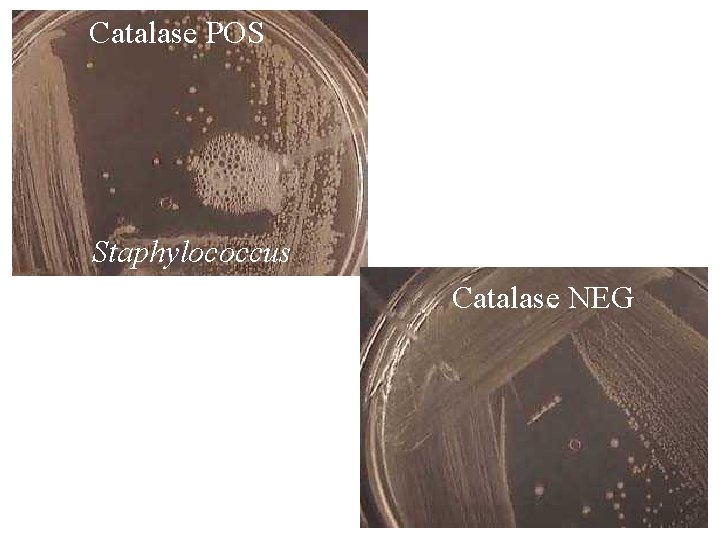
Identification Tests: Catalase Principle: tests for enzyme catalase 2 H 2 O 2 2 H 2 O + O 2 Procedure Smear a colony of the organism to a slide Drop H 2 O 2 onto smear Observe
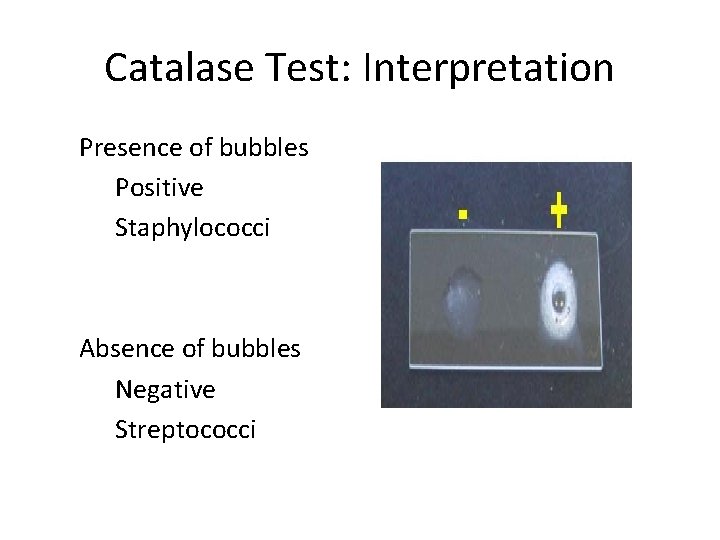
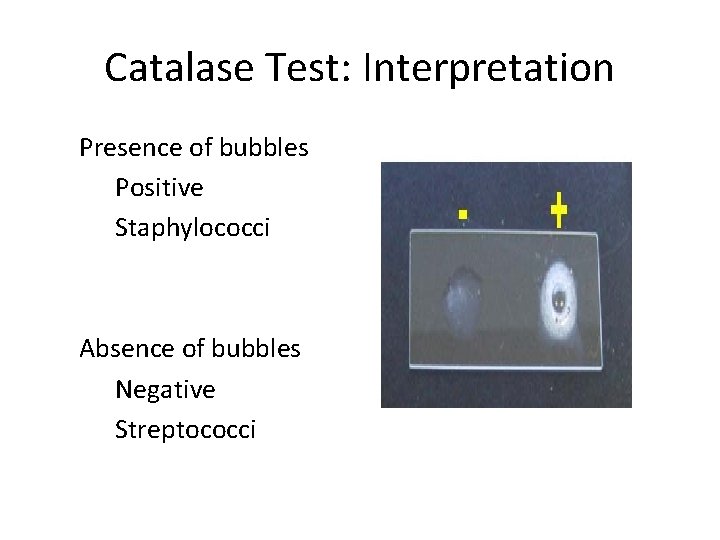
Catalase Test: Interpretation Presence of bubbles Positive Staphylococci Absence of bubbles Negative Streptococci
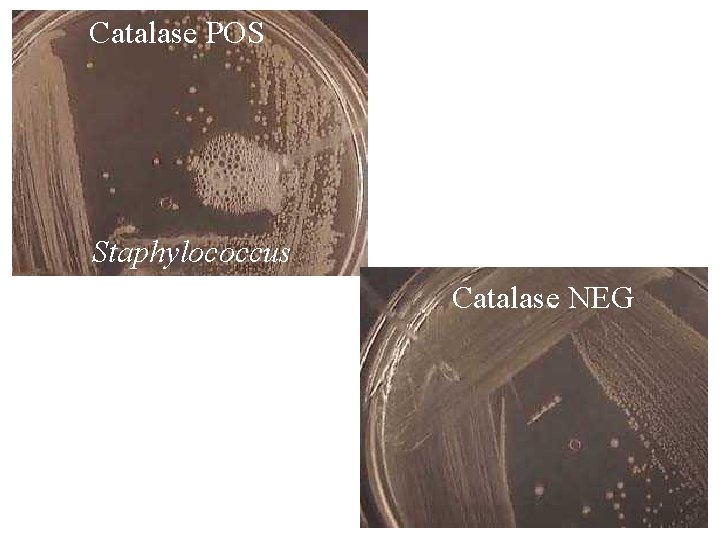
Catalase POS Staphylococcus Catalase NEG
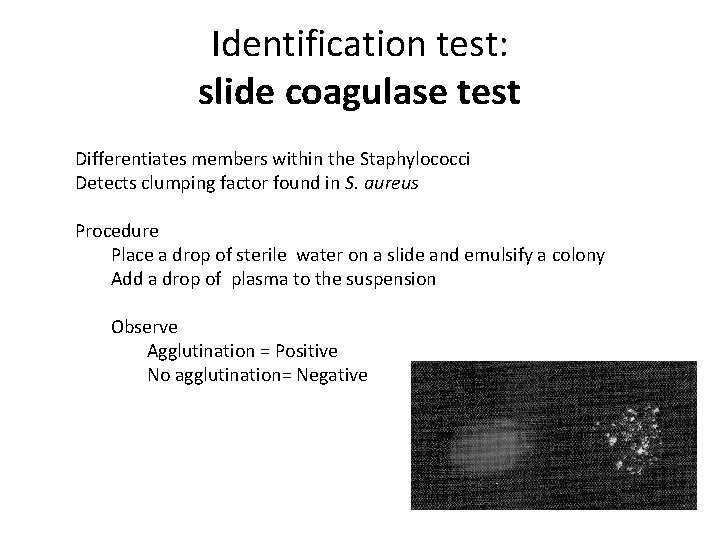
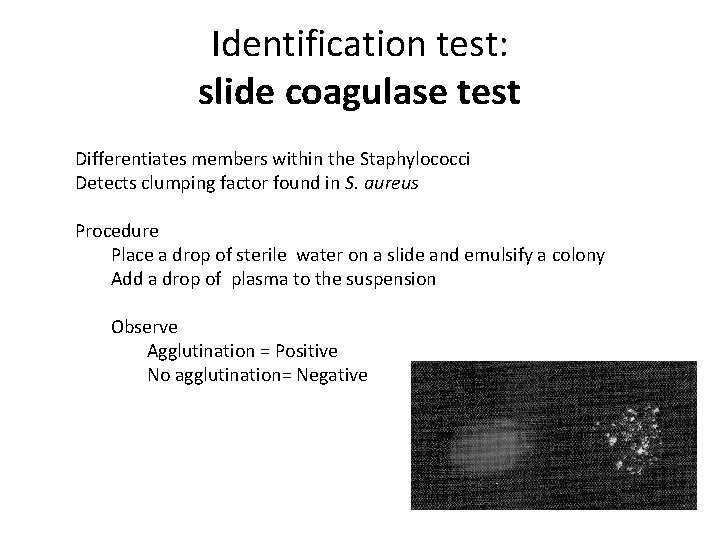
Identification test: slide coagulase test Differentiates members within the Staphylococci Detects clumping factor found in S. aureus Procedure Place a drop of sterile water on a slide and emulsify a colony Add a drop of plasma to the suspension Observe Agglutination = Positive No agglutination= Negative
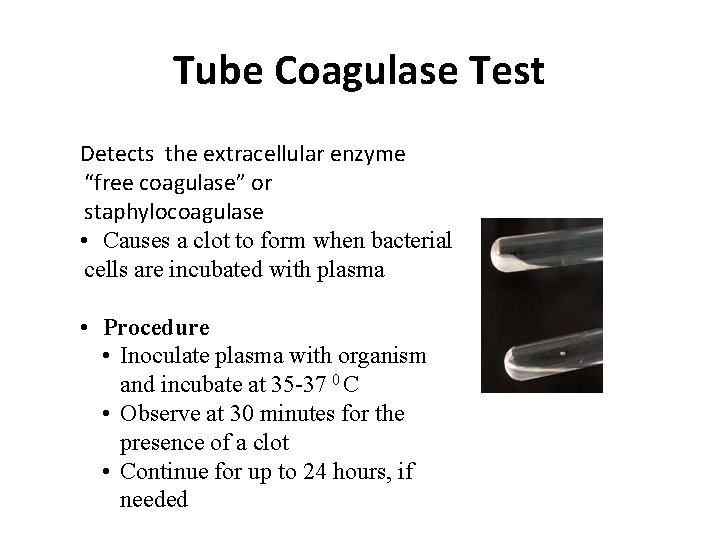
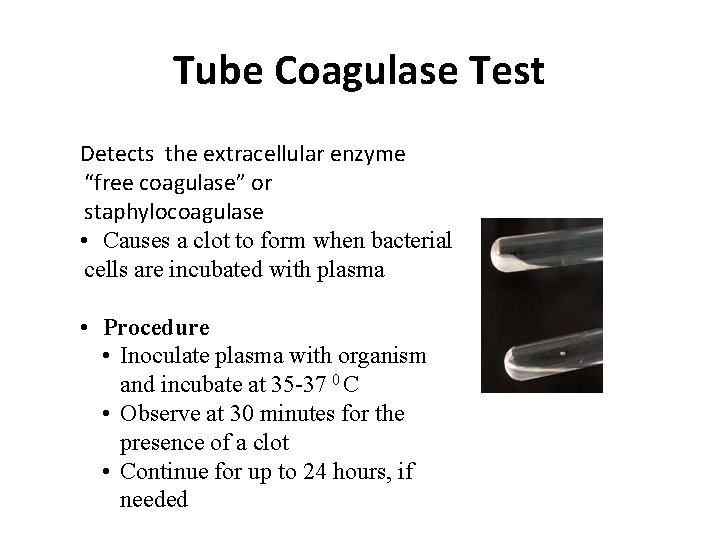
Tube Coagulase Test Detects the extracellular enzyme “free coagulase” or staphylocoagulase • Causes a clot to form when bacterial cells are incubated with plasma • Procedure • Inoculate plasma with organism and incubate at 35 -37 0 C • Observe at 30 minutes for the presence of a clot • Continue for up to 24 hours, if needed
Treatment Drain infected area Deep/metastatic infections semi-synthetic penicllins cephalosporins erythromycin clindamycin Endocarditis semi-synthetic penicillin + an aminoglycoside
Antimicrobial Susceptibility For non–beta-lactamase producing S. aureus • Use penicillin • Penicillinase-resistant synthetic penicillins (methicillin, nafcillin, oxacillin, dicloxacillin) Beta-lactamase producers break down the betalactam ring of penicillin so it inactivates antibiotic before it acts on bacterial cells
Beta lactamase production – plasmid mediated Has made S. aureus resistant to penicillin group of antibiotics - 90% of S. aureus B lactamase stable penicillins (cloxacillin, methicillin) are used
Alteration of penicillin binding proteins (Chromosomal mediated) Has made S. aureus resistant to B lactamase stable penicillins 10 -20% S. aureus resistant to all Penicillins and Cephalasporins) Vancomycin is the drug of choice
Prevention Carrier status prevents complete control Proper hygiene, segregation of carrier from highly susceptible individuals Good aseptic techniques when handling surgical instruments Control of nosocomial infections
Coagulase-Negative Staphylococci: Staphylococcus epidermidis Predominantly hospital acquired infections Skin flora gets introduced by catheters, heart valves, CSF shunts Produces a slime layer that helps adherence to prosthetics and avoidance of phagocytosis UTIs are a common result
Coagulase-Negative Staphylococci: Staphylococcus saprophyticus UTIs in young sexually active women Due in part to increased adherence to epithelial cells lining the urogenital tract Rarely present in other skin areas or mucous membranes Urine cultures If present in low amounts, it is still considered significant
Coagulase-Negative Staphylococci: Staphylococcus haemolyticus Habitat: skin and mucous membranes Rarely implicated in infections Associated with wound infections, bacteremia, and endocarditis