Prevention and Control of HealthcareAssociated MethicillinResistant Staphylococcus aureus

- Slides: 30
Prevention and Control of Healthcare-Associated Methicillin-Resistant Staphylococcus aureus John A. Jernigan Division of Healthcare Quality Promotion Centers for Disease Control and Prevention April 29, 2008 The findings and conclusions in this presentation/report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention
Continuing Education Credits DISCLAIMER: In compliance with continuing education requirements, all presenters must disclose any financial or other relationships with the manufacturers of commercial products, suppliers of commercial services, or commercial supporters as well as any use of unlabeled product(s) or product(s) under investigational use. CDC, our planners, and the presenters for this seminar do not have financial or other relationships with the manufacturers of commercial products, suppliers of commercial services, or commercial supporters. This presentation does not involve the unlabeled use of a product or product under investigational use.
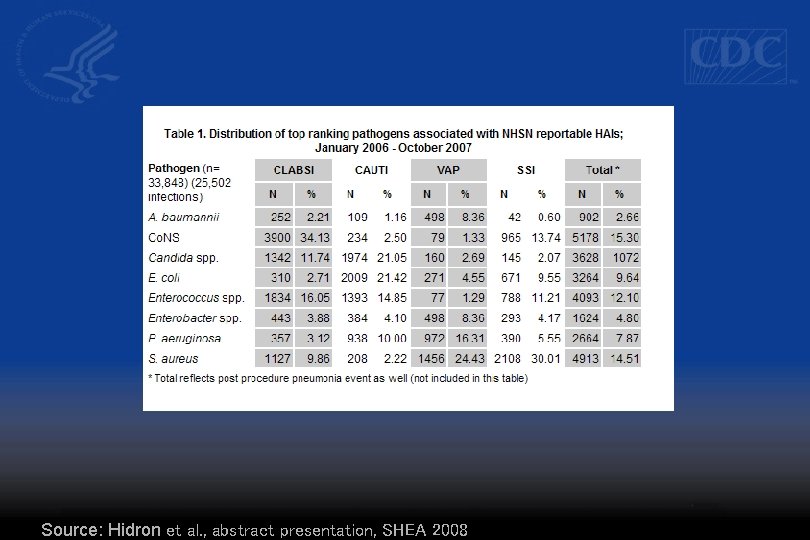
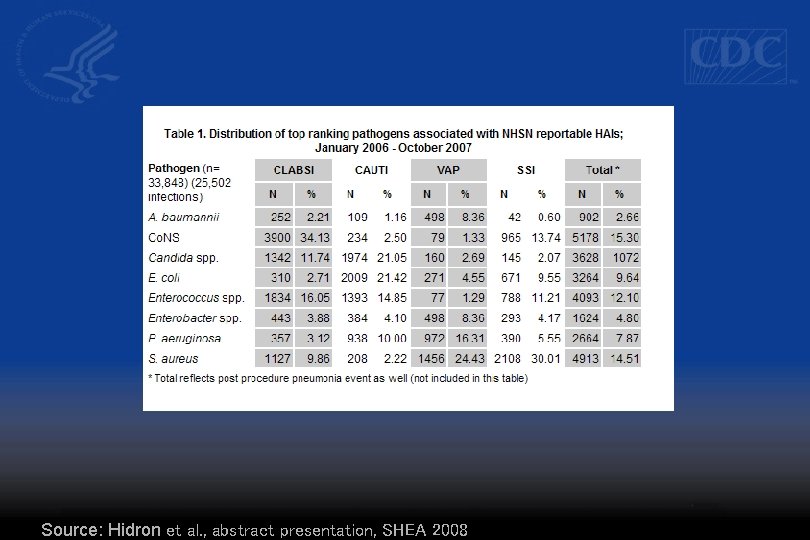
Source: Hidron et al. , abstract presentation, SHEA 2008
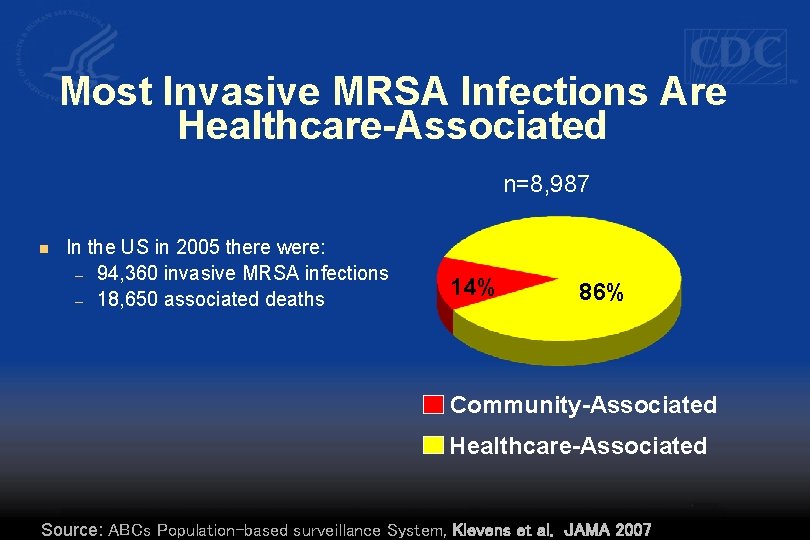
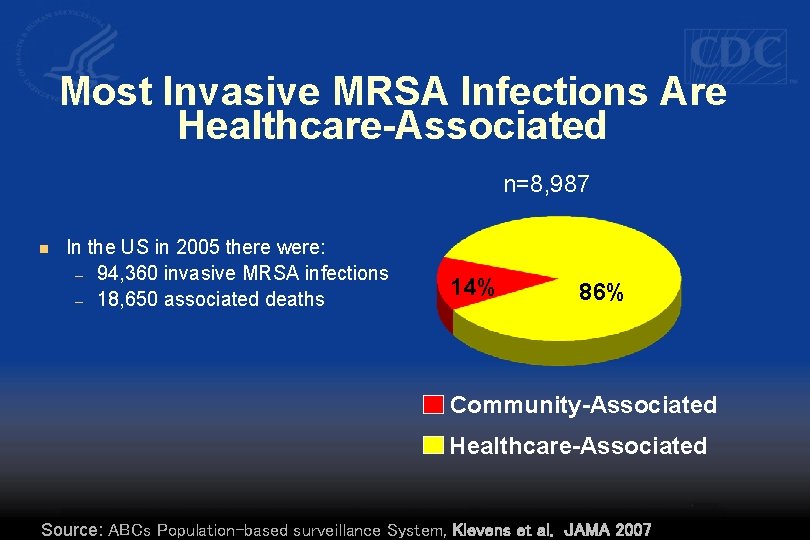
Most Invasive MRSA Infections Are Healthcare-Associated n=8, 987 n In the US in 2005 there were: – 94, 360 invasive MRSA infections – 18, 650 associated deaths 14% 86% Community-Associated Healthcare-Associated Source: ABCs Population-based surveillance System, Klevens et al. JAMA 2007
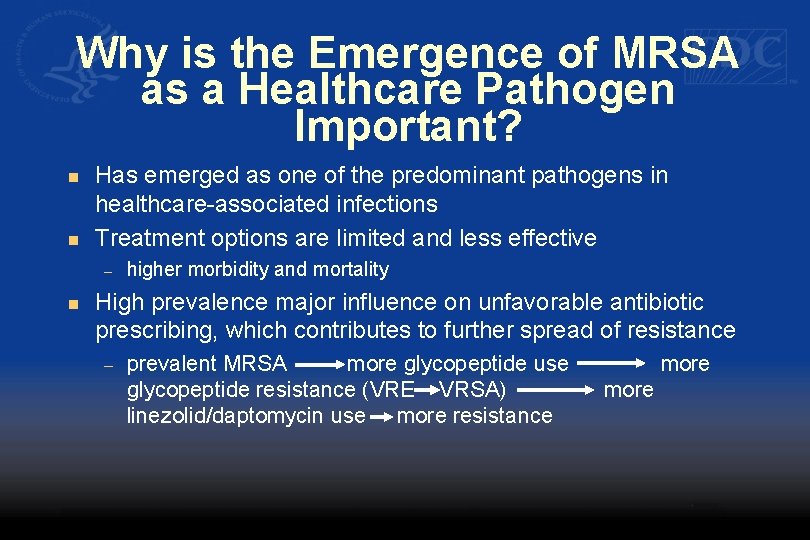
Why is the Emergence of MRSA as a Healthcare Pathogen Important? n n Has emerged as one of the predominant pathogens in healthcare-associated infections Treatment options are limited and less effective – n higher morbidity and mortality High prevalence major influence on unfavorable antibiotic prescribing, which contributes to further spread of resistance – prevalent MRSA more glycopeptide use glycopeptide resistance (VRE VRSA) linezolid/daptomycin use more resistance more
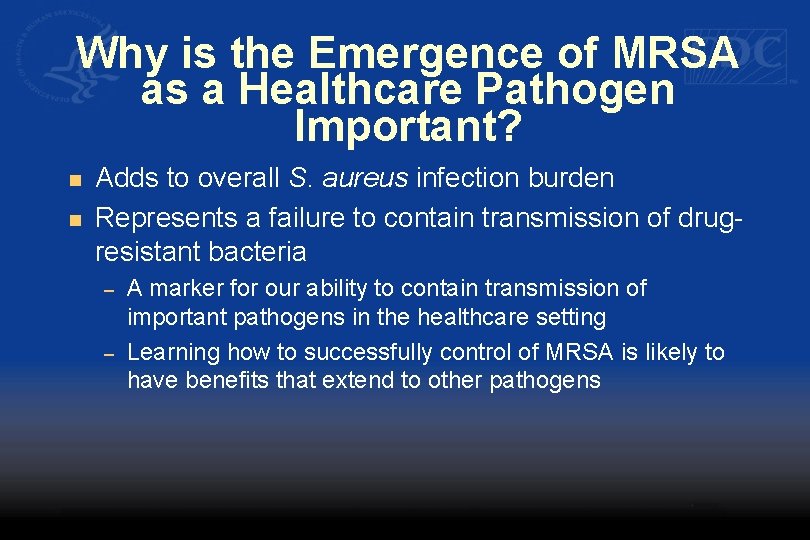
Why is the Emergence of MRSA as a Healthcare Pathogen Important? n n Adds to overall S. aureus infection burden Represents a failure to contain transmission of drugresistant bacteria – – A marker for our ability to contain transmission of important pathogens in the healthcare setting Learning how to successfully control of MRSA is likely to have benefits that extend to other pathogens
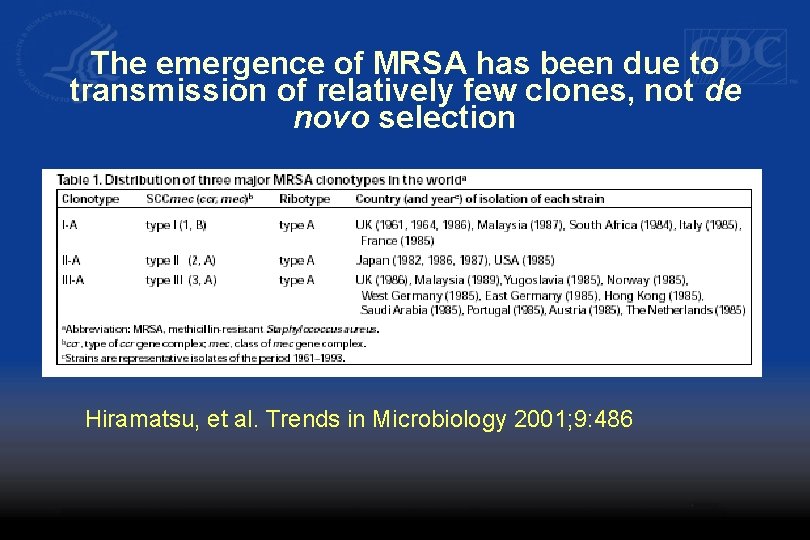
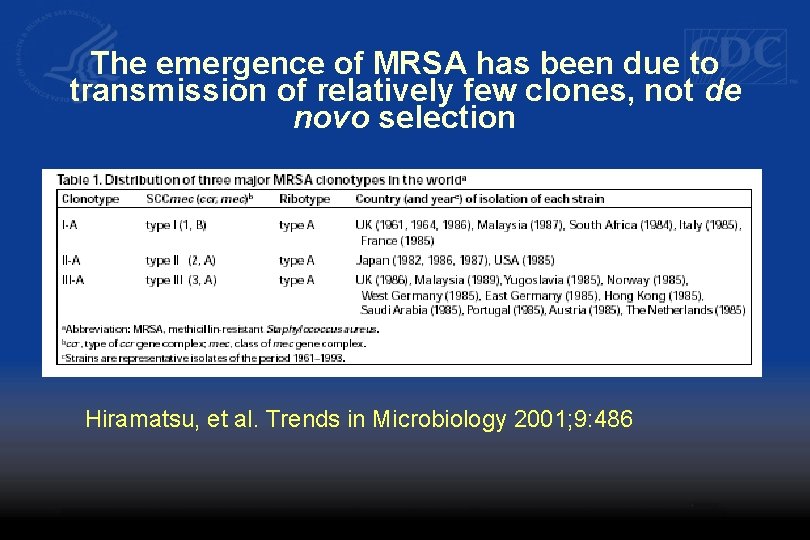
The emergence of MRSA has been due to transmission of relatively few clones, not de novo selection Hiramatsu, et al. Trends in Microbiology 2001; 9: 486
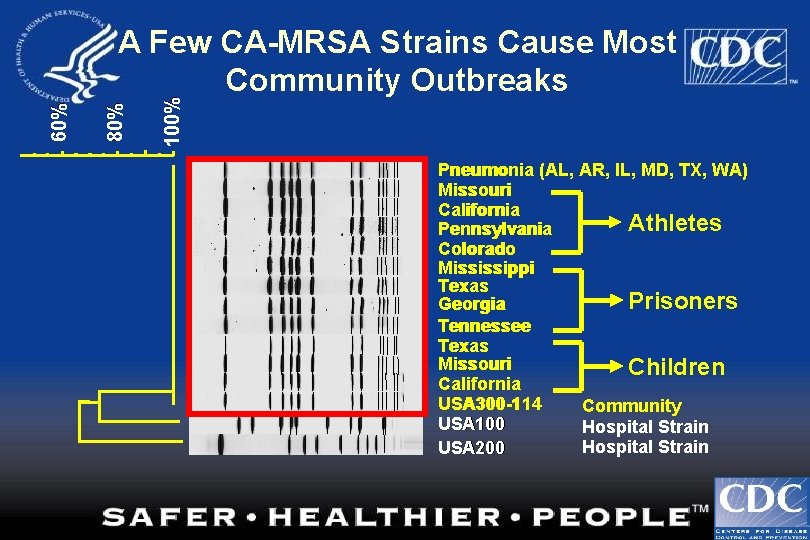
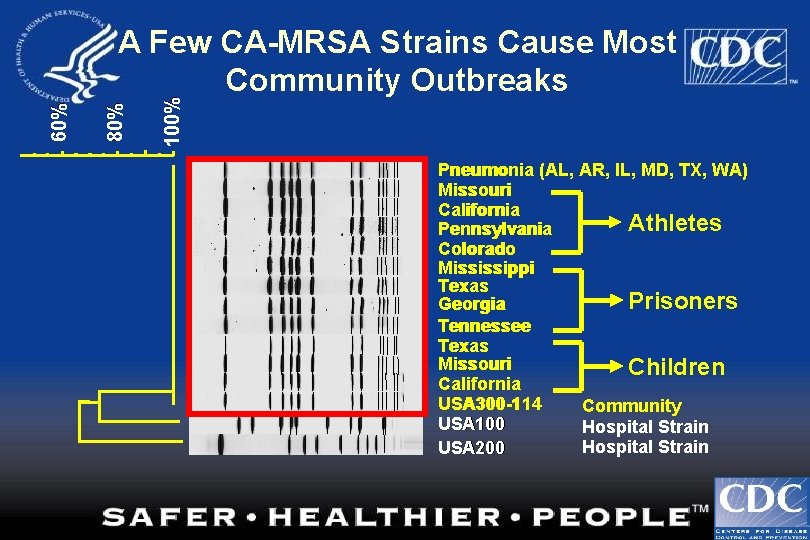
100% 80% 60% A Few CA-MRSA Strains Cause Most Community Outbreaks Pneumonia (AL, AR, IL, MD, TX, WA) Missouri California Athletes Pennsylvania Colorado Mississippi Texas Prisoners Georgia Tennessee Texas Missouri Children California USA 300 -114 Community USA 100 Hospital Strain USA 200
Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Key Prevention Strategies Clinicians hold the solution! § Prevent infection § Diagnose and treat infection effectively § Use antimicrobials wisely § Prevent transmission
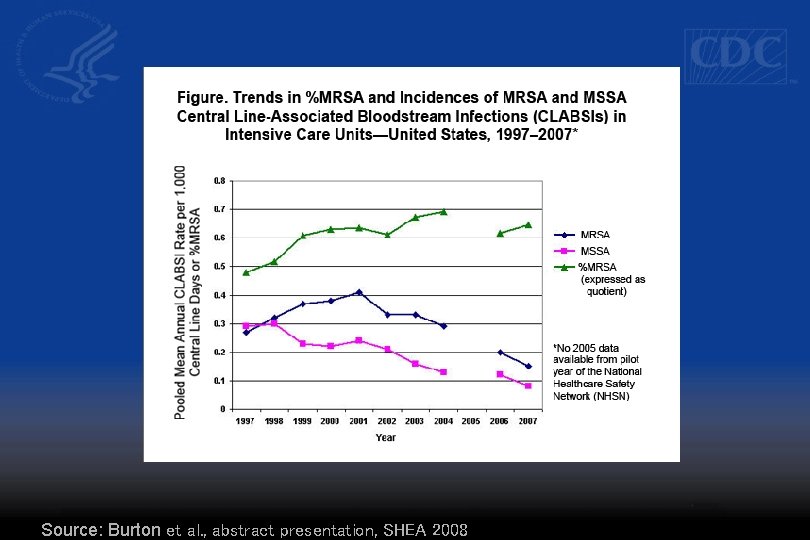
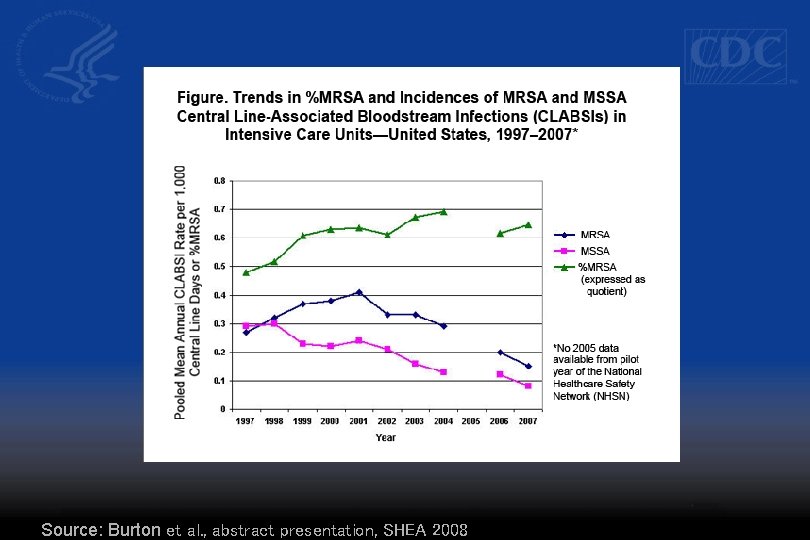
Source: Burton et al. , abstract presentation, SHEA 2008
Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Key Prevention Strategies Clinicians hold the solution! § Prevent infection § Diagnose and treat infection effectively § Use antimicrobials wisely § Prevent transmission
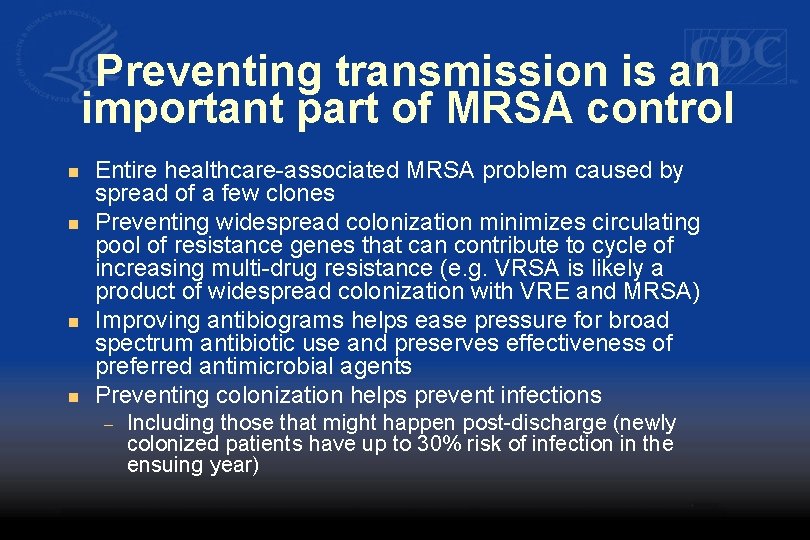
Preventing transmission is an important part of MRSA control n n Entire healthcare-associated MRSA problem caused by spread of a few clones Preventing widespread colonization minimizes circulating pool of resistance genes that can contribute to cycle of increasing multi-drug resistance (e. g. VRSA is likely a product of widespread colonization with VRE and MRSA) Improving antibiograms helps ease pressure for broad spectrum antibiotic use and preserves effectiveness of preferred antimicrobial agents Preventing colonization helps prevent infections – Including those that might happen post-discharge (newly colonized patients have up to 30% risk of infection in the ensuing year)
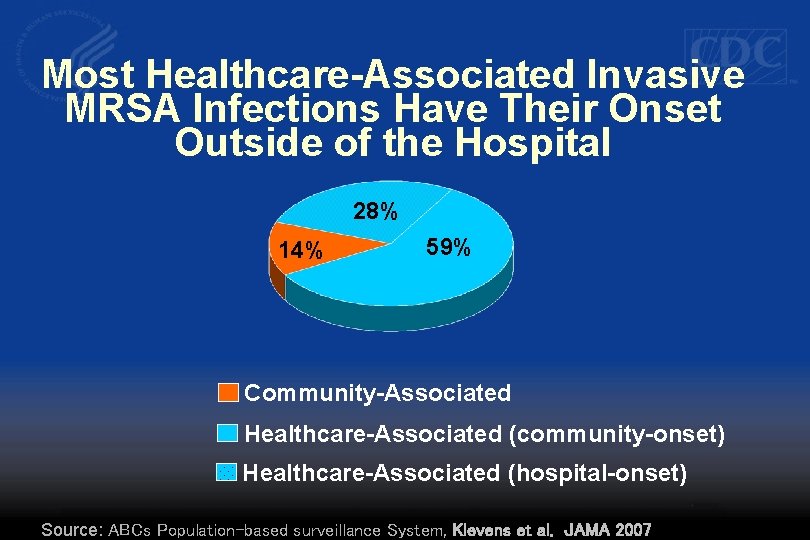
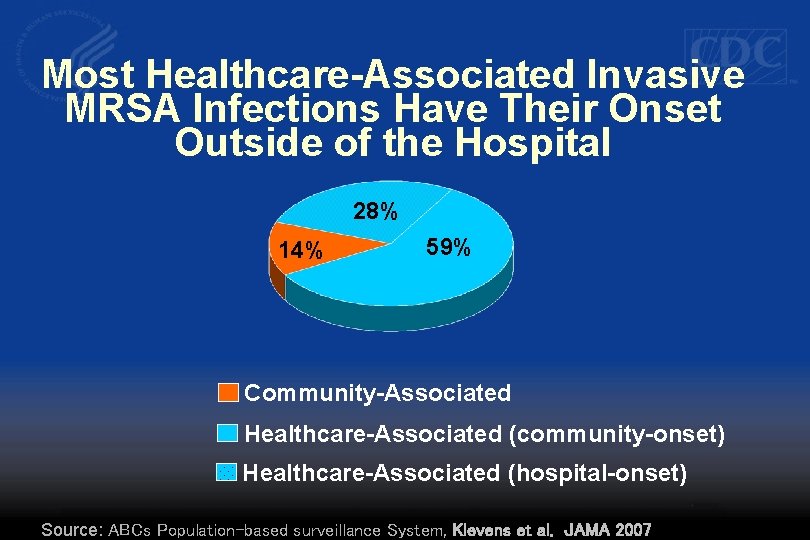
Most Healthcare-Associated Invasive MRSA Infections Have Their Onset Outside of the Hospital 28% 14% 59% Community-Associated Healthcare-Associated (community-onset) Healthcare-Associated (hospital-onset) Source: ABCs Population-based surveillance System, Klevens et al. JAMA 2007
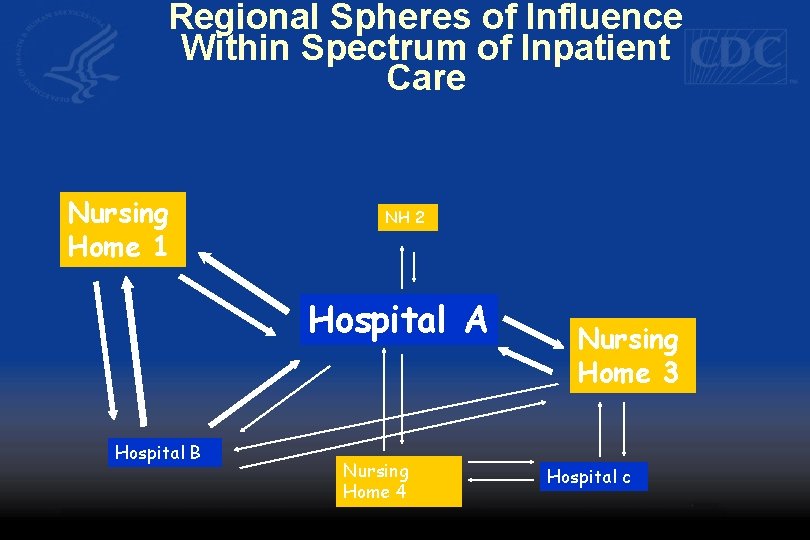
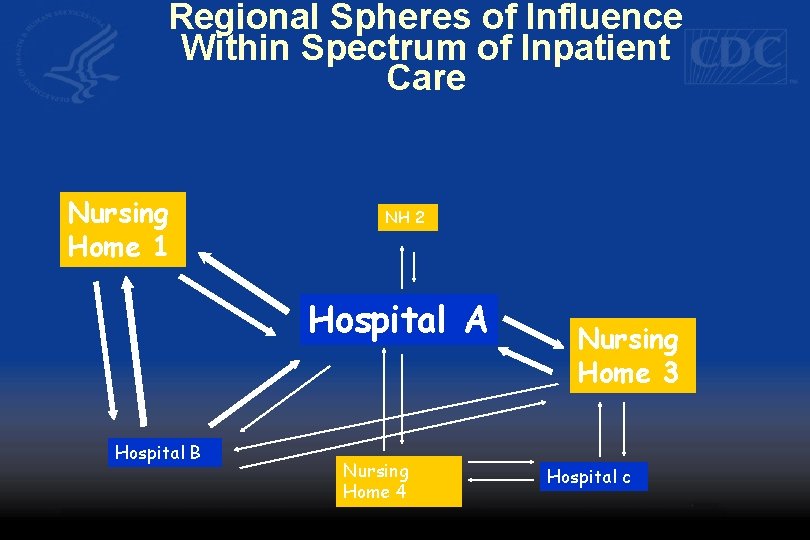
Regional Spheres of Influence Within Spectrum of Inpatient Care Nursing Home 1 NH 2 Hospital A Hospital B Nursing Home 4 Nursing Home 3 Hospital c
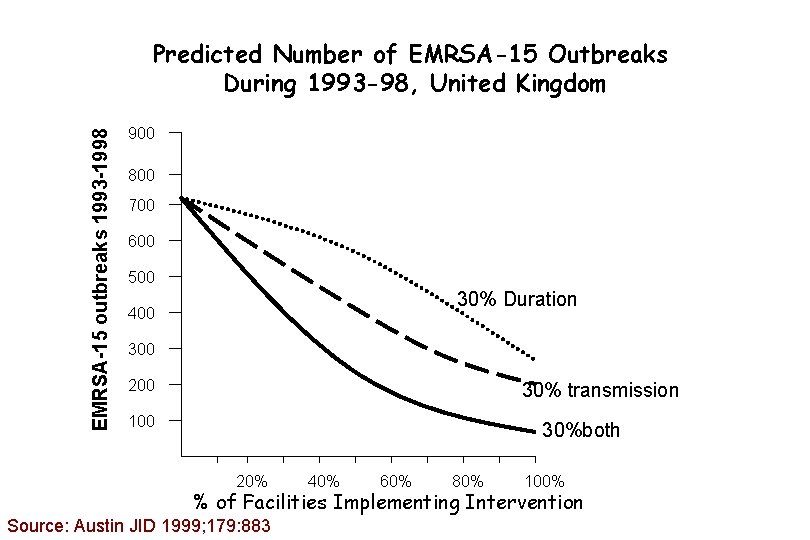
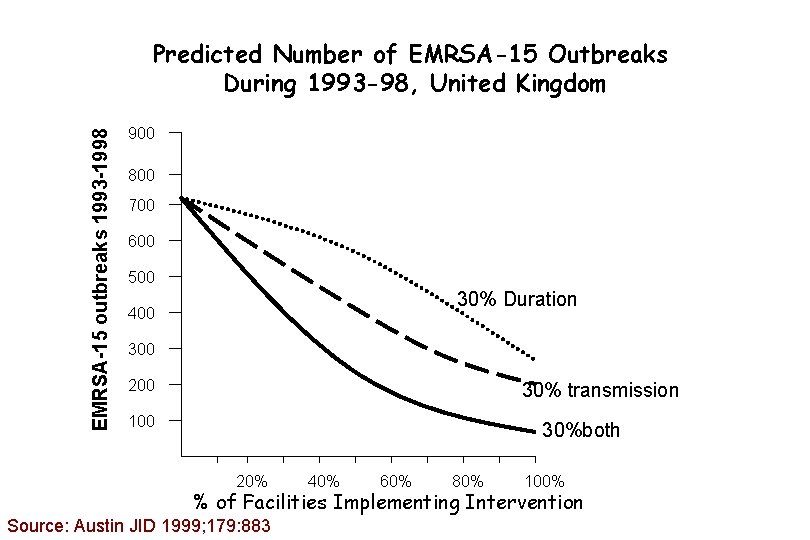
EMRSA-15 outbreaks 1993 -1998 Predicted Number of EMRSA-15 Outbreaks During 1993 -98, United Kingdom 900 800 700 600 500 30% Duration 400 300 200 30% transmission 100 30%both 20% 40% 60% 80% 100% % of Facilities Implementing Intervention Source: Austin JID 1999; 179: 883
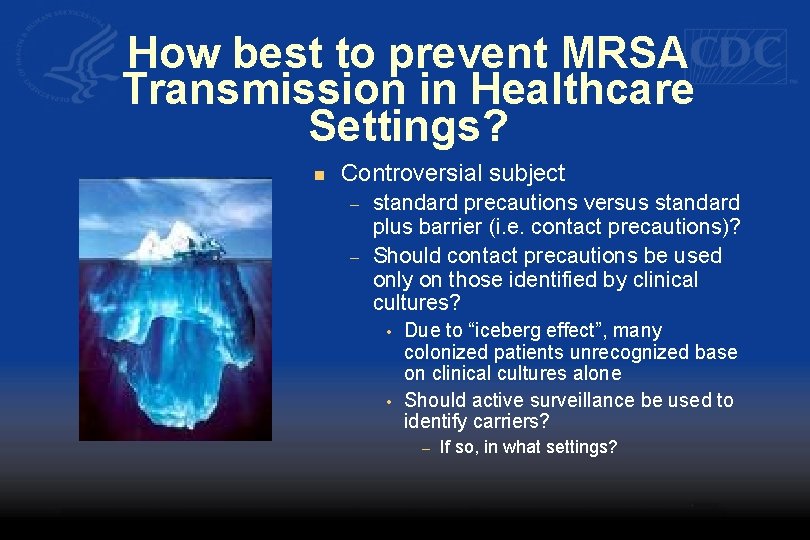
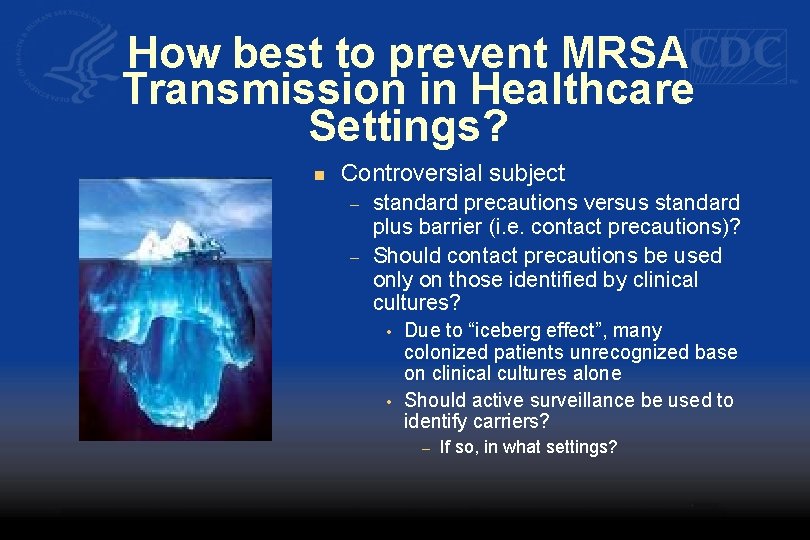
How best to prevent MRSA Transmission in Healthcare Settings? n Controversial subject – – standard precautions versus standard plus barrier (i. e. contact precautions)? Should contact precautions be used only on those identified by clinical cultures? • • Due to “iceberg effect”, many colonized patients unrecognized base on clinical cultures alone Should active surveillance be used to identify carriers? – If so, in what settings?
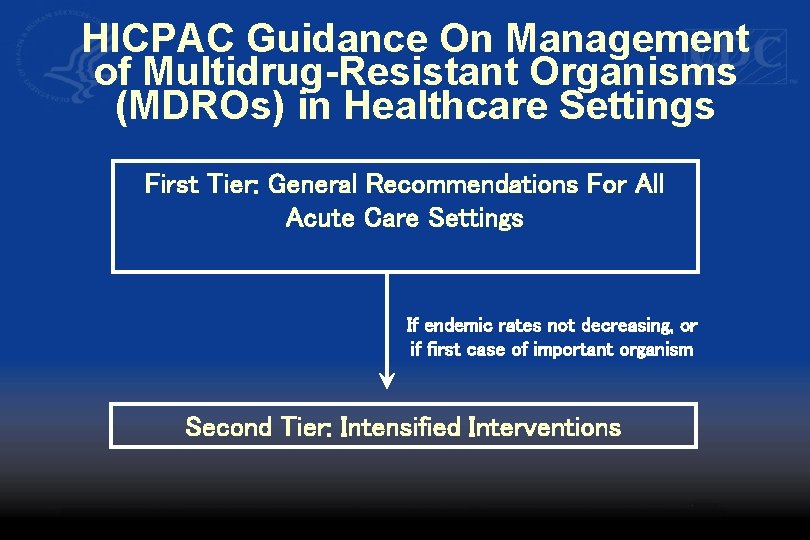
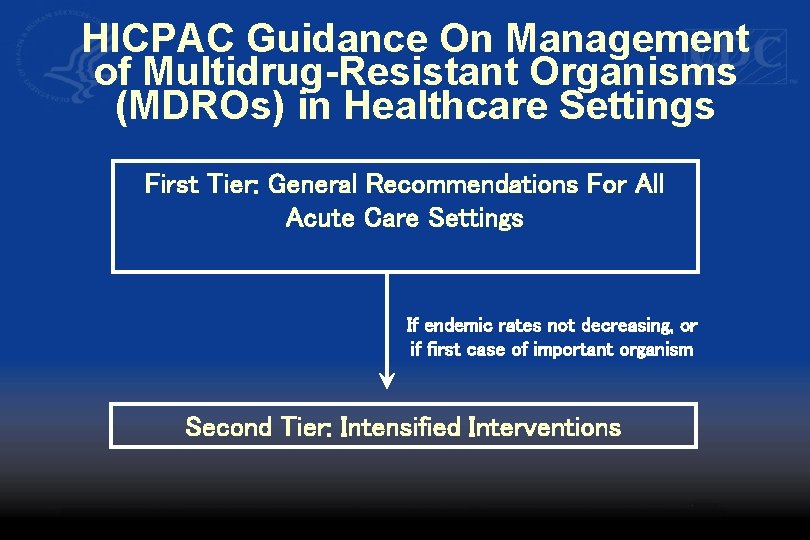
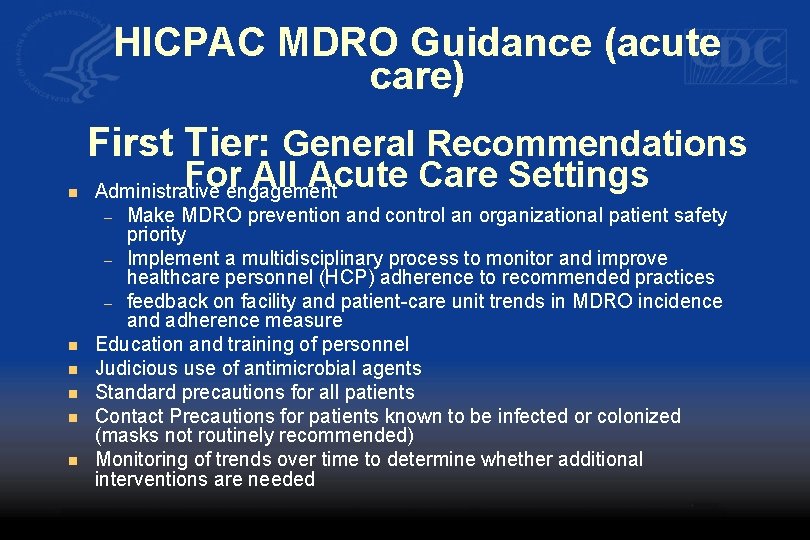
HICPAC Guidance On Management of Multidrug-Resistant Organisms (MDROs) in Healthcare Settings First Tier: General Recommendations For All Acute Care Settings If endemic rates not decreasing, or if first case of important organism Second Tier: Intensified Interventions
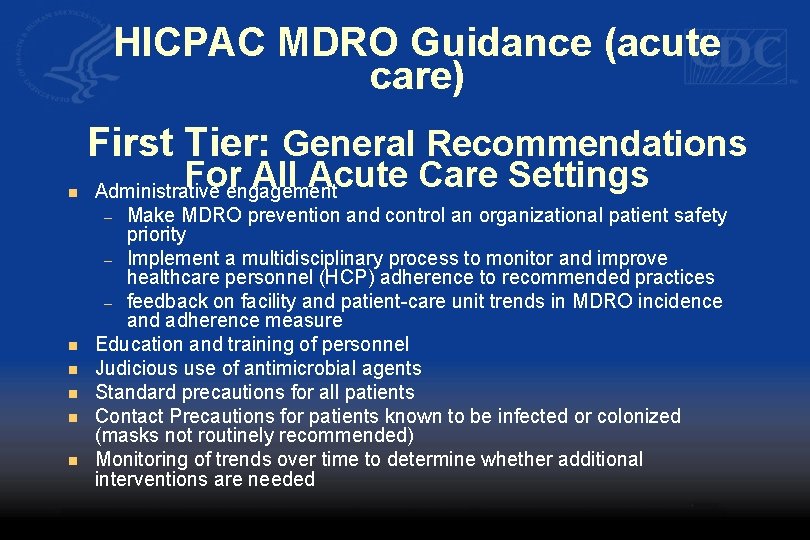
HICPAC MDRO Guidance (acute care) First Tier: General Recommendations n n n For All Acute Care Settings Administrative engagement – Make MDRO prevention and control an organizational patient safety priority – Implement a multidisciplinary process to monitor and improve healthcare personnel (HCP) adherence to recommended practices – feedback on facility and patient-care unit trends in MDRO incidence and adherence measure Education and training of personnel Judicious use of antimicrobial agents Standard precautions for all patients Contact Precautions for patients known to be infected or colonized (masks not routinely recommended) Monitoring of trends over time to determine whether additional interventions are needed
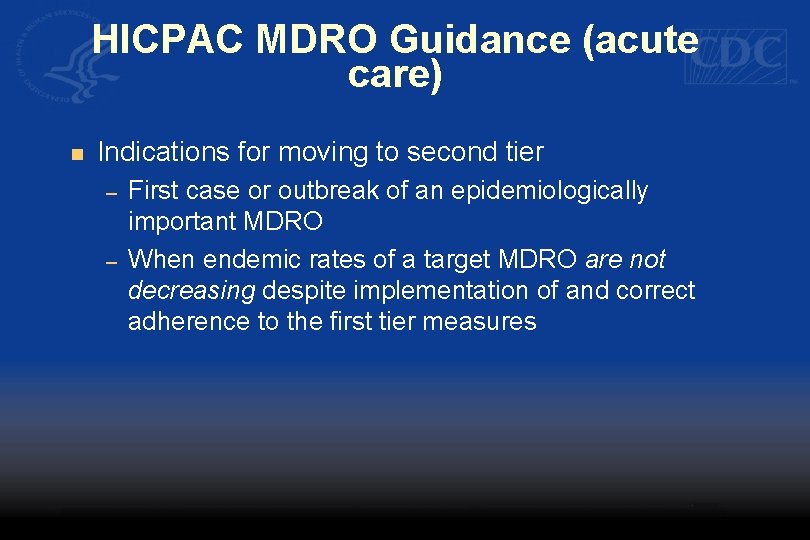
HICPAC MDRO Guidance (acute care) n Indications for moving to second tier – – First case or outbreak of an epidemiologically important MDRO When endemic rates of a target MDRO are not decreasing despite implementation of and correct adherence to the first tier measures
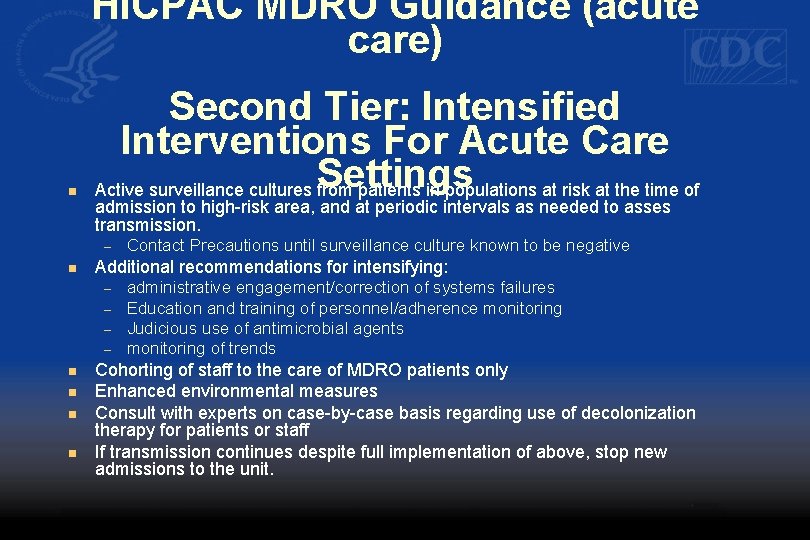
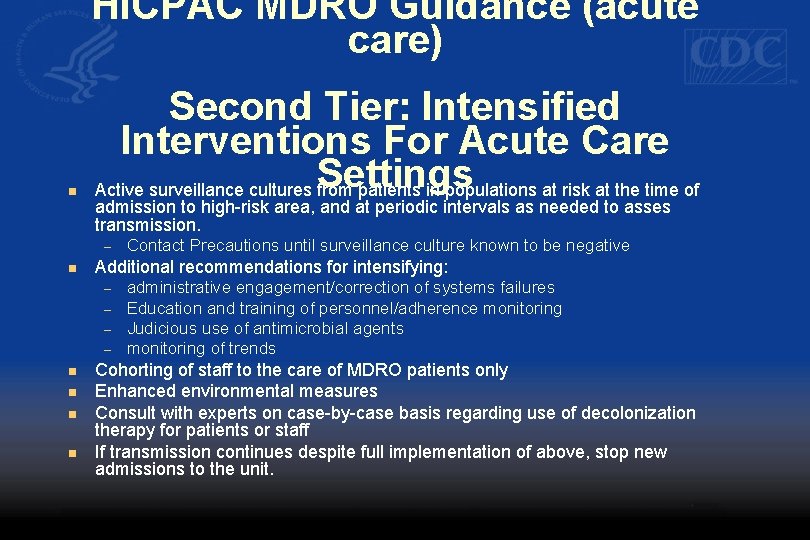
HICPAC MDRO Guidance (acute care) n Second Tier: Intensified Interventions For Acute Care Active surveillance cultures Settings from patients in populations at risk at the time of admission to high-risk area, and at periodic intervals as needed to asses transmission. – n Additional recommendations for intensifying: – – n n Contact Precautions until surveillance culture known to be negative administrative engagement/correction of systems failures Education and training of personnel/adherence monitoring Judicious use of antimicrobial agents monitoring of trends Cohorting of staff to the care of MDRO patients only Enhanced environmental measures Consult with experts on case-by-case basis regarding use of decolonization therapy for patients or staff If transmission continues despite full implementation of above, stop new admissions to the unit.
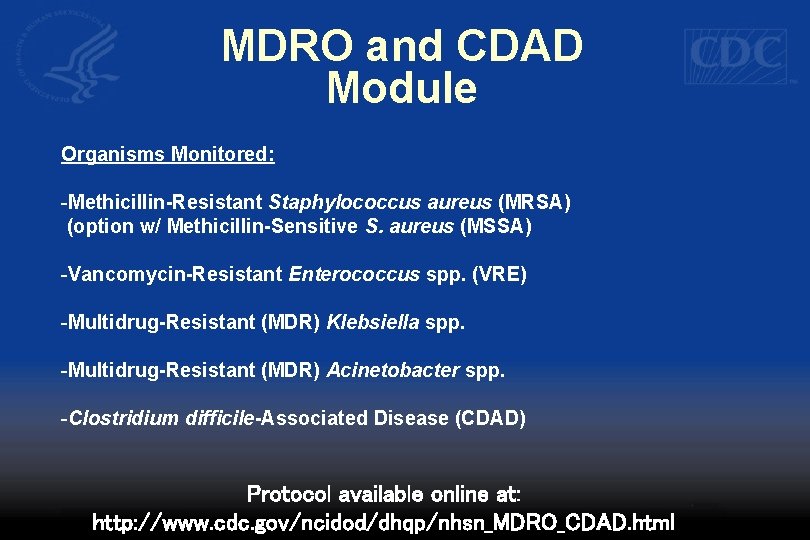
MDRO and CDAD Module Multidrug-Resistant Organism (MDRO) and Clostridium difficile-Associated Disease (CDAD) Module
MDRO and CDAD Module Organisms Monitored: -Methicillin-Resistant Staphylococcus aureus (MRSA) (option w/ Methicillin-Sensitive S. aureus (MSSA) -Vancomycin-Resistant Enterococcus spp. (VRE) -Multidrug-Resistant (MDR) Klebsiella spp. -Multidrug-Resistant (MDR) Acinetobacter spp. -Clostridium difficile-Associated Disease (CDAD) Protocol available online at: http: //www. cdc. gov/ncidod/dhqp/nhsn_MDRO_CDAD. html
Goal of the MDRO and CDAD Module n Provide a mechanism for healthcare facilities to report and analyze data that will inform infection control staff of the impact of targeted prevention efforts
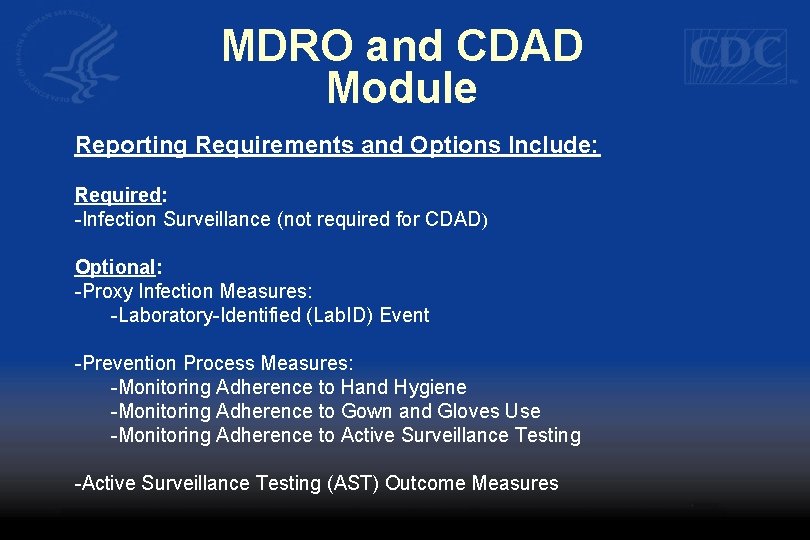
MDRO and CDAD Module Reporting Requirements and Options Include: Required: -Infection Surveillance (not required for CDAD) Optional: -Proxy Infection Measures: -Laboratory-Identified (Lab. ID) Event -Prevention Process Measures: -Monitoring Adherence to Hand Hygiene -Monitoring Adherence to Gown and Gloves Use -Monitoring Adherence to Active Surveillance Testing -Active Surveillance Testing (AST) Outcome Measures
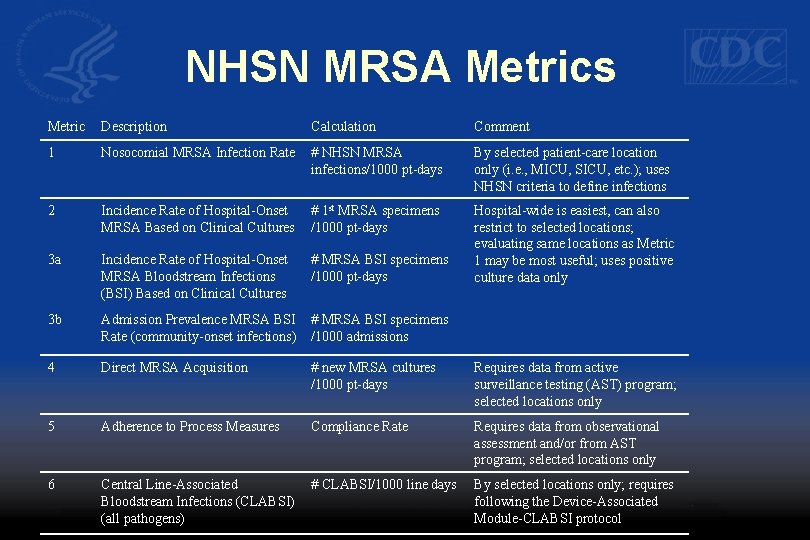
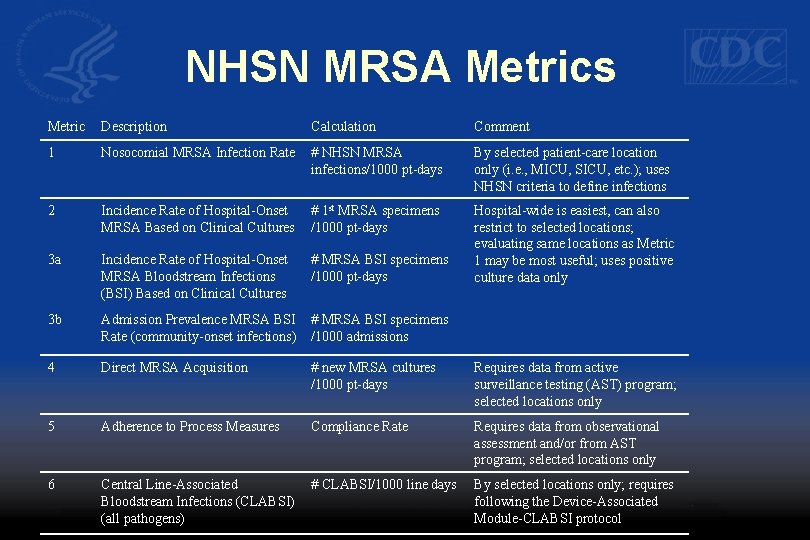
NHSN MRSA Metrics Metric Description Calculation Comment 1 Nosocomial MRSA Infection Rate # NHSN MRSA infections/1000 pt-days By selected patient-care location only (i. e. , MICU, SICU, etc. ); uses NHSN criteria to define infections 2 Incidence Rate of Hospital-Onset MRSA Based on Clinical Cultures # 1 st MRSA specimens /1000 pt-days 3 a Incidence Rate of Hospital-Onset MRSA Bloodstream Infections (BSI) Based on Clinical Cultures # MRSA BSI specimens /1000 pt-days Hospital-wide is easiest, can also restrict to selected locations; evaluating same locations as Metric 1 may be most useful; uses positive culture data only 3 b Admission Prevalence MRSA BSI Rate (community-onset infections) # MRSA BSI specimens /1000 admissions 4 Direct MRSA Acquisition # new MRSA cultures /1000 pt-days Requires data from active surveillance testing (AST) program; selected locations only 5 Adherence to Process Measures Compliance Rate Requires data from observational assessment and/or from AST program; selected locations only 6 Central Line-Associated Bloodstream Infections (CLABSI) (all pathogens) # CLABSI/1000 line days By selected locations only; requires following the Device-Associated Module-CLABSI protocol
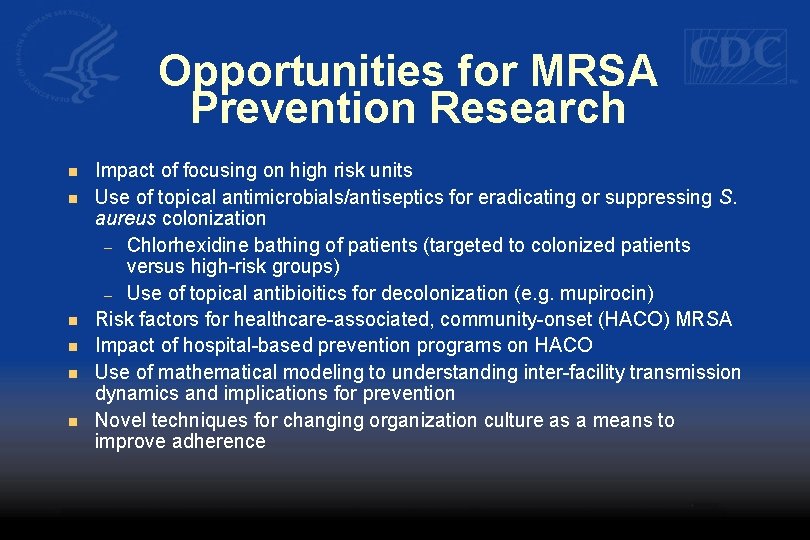
Opportunities for MRSA Prevention Research n n n Impact of focusing on high risk units Use of topical antimicrobials/antiseptics for eradicating or suppressing S. aureus colonization – Chlorhexidine bathing of patients (targeted to colonized patients versus high-risk groups) – Use of topical antibioitics for decolonization (e. g. mupirocin) Risk factors for healthcare-associated, community-onset (HACO) MRSA Impact of hospital-based prevention programs on HACO Use of mathematical modeling to understanding inter-facility transmission dynamics and implications for prevention Novel techniques for changing organization culture as a means to improve adherence
Conclusions n The burden of MRSA remains high in US healthcare settings n Community-associated MRSA (CA-MRSA) infections are emerging rapidly in many areas, but population-based estimates suggest that most MRSA infections are healthcare-associated n Epidemic strains of MRSA originally associated with the community have emerged as important causes of hospital-acquired infections n MRSA infections and transmission can be prevented, even in endemic settings in the US n Effective control programs must be multifaceted, and broad institutional commitment, including measurement of impact, is required for successful implementation

Acknowledgments n n n n Rachel Gorwitz Kate Ellingson n David Kleinbaum Val Gebski Jonathan Edwards Pei-Jean Chang Alexander Kallen Scott Fridkin n Monina Klevens Jeff Hageman Fred Tenover Melissa Morrison Teresa Horan n n Robert Muder Rajiv Jain The Active Bacterial Core Surveillance Investigators/Teams Dawn Sievert Deron Burton Alicia Hidron Dan Pollock
n Continuing Education guidelines require that the attendance of all who participate in COCA Conference Calls be properly documented. ALL Continuing Education credits (CME, CNE, CEU and CHES) for COCA Conference Calls are issued online through the CDC Training & Continuing Education Online system http: //www 2 a. cdc. gov/TCEOnline/. n Those who participate in the COCA Conference Calls and who wish to receive CE credit and will complete the online evaluation by April 26, 2008 will use the course code EC 1265. Those who wish to receive CE credit and will complete the online evaluation between April 27, 2008 and March 27, 2009 will use course code WD 1265. CE certificates can be printed immediately upon completion of your online evaluation. A cumulative transcript of all CDC/ATSDR CE’s obtained through the CDC Training & Continuing Education Online System will be maintained for each user.
CME: CDC is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. CDC designates this educational activity for a maximum of 1 Category 1 credit toward the AMA Physician's Recognition Award. Physicians should only claim credit commensurate with the extent of their participation in the activity. CNE: This activity for 1. 0 contact hours is provided by CDC, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditations. CEU: CDC has been reviewed and approved as an authorized provider by the International Association for Continuing Education and Training (IACET), 8405 Greensboro Drive, Suite 800, Mc. Lean, VA 22102. CDC has awarded 0. 1 CEU to participants who successfully complete this program. CHEC: CDC is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is a designated event for the CHES to receive 1 Category I Contact Hour(s) in health education. CDC provider number GA 0082.
 Confirmatory test for staphylococcus aureus
Confirmatory test for staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus Staphylocoque mrs1
Staphylocoque mrs1 Fastidious bacteria
Fastidious bacteria Micrococcaceae family
Micrococcaceae family Etiolgia
Etiolgia Catalase
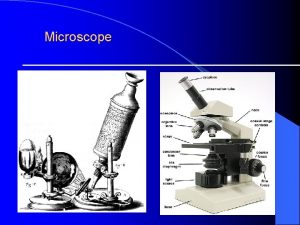
Catalase Microbiology
Microbiology Staphylococcus aureus?
Staphylococcus aureus? Three domains of life
Three domains of life Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Staphylococcus aureus
Staphylococcus aureus Staphylococcus aureus
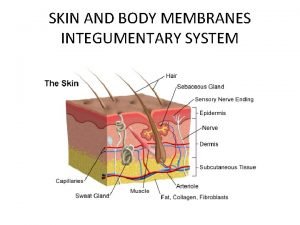
Staphylococcus aureus Staphylococcus aureus bacteria structure
Staphylococcus aureus bacteria structure Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli Enzymes of staphylococcus aureus
Enzymes of staphylococcus aureus Prokaryotic cells
Prokaryotic cells Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Staph aureus morphology
Staph aureus morphology Antibiogram
Antibiogram Difference selective and differential media
Difference selective and differential media Streptococcus aureus
Streptococcus aureus Streptococcus aureus
Streptococcus aureus Spcc template
Spcc template Colorado jprs
Colorado jprs Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control European centre for disease prevention and control
European centre for disease prevention and control Chapter 16 infection prevention and control
Chapter 16 infection prevention and control Prevention and control of poliomyelitis
Prevention and control of poliomyelitis Poliomyelitis slideshare
Poliomyelitis slideshare Catalase test
Catalase test