CommunityAssociated MethicillinResistant Staphylococcus aureus Ruth Lynfield M D


- Slides: 22

Community-Associated Methicillin-Resistant Staphylococcus aureus Ruth Lynfield, M. D. Minnesota Department of Health
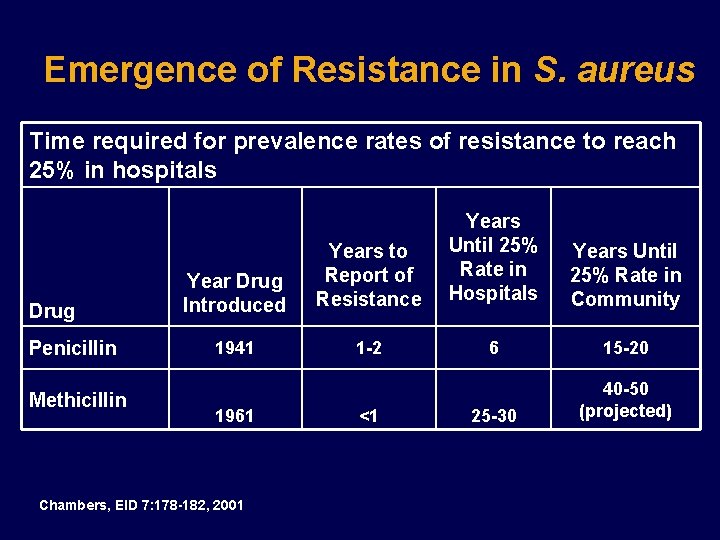
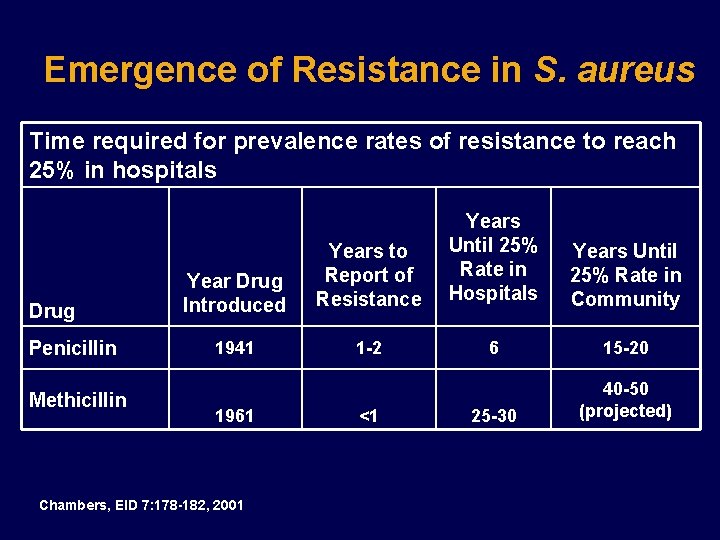
Emergence of Resistance in S. aureus Time required for prevalence rates of resistance to reach 25% in hospitals Drug Penicillin Methicillin Year Drug Introduced Years to Report of Resistance Years Until 25% Rate in Hospitals Years Until 25% Rate in Community 1941 1 -2 6 15 -20 25 -30 40 -50 (projected) 1961 Chambers, EID 7: 178 -182, 2001 <1
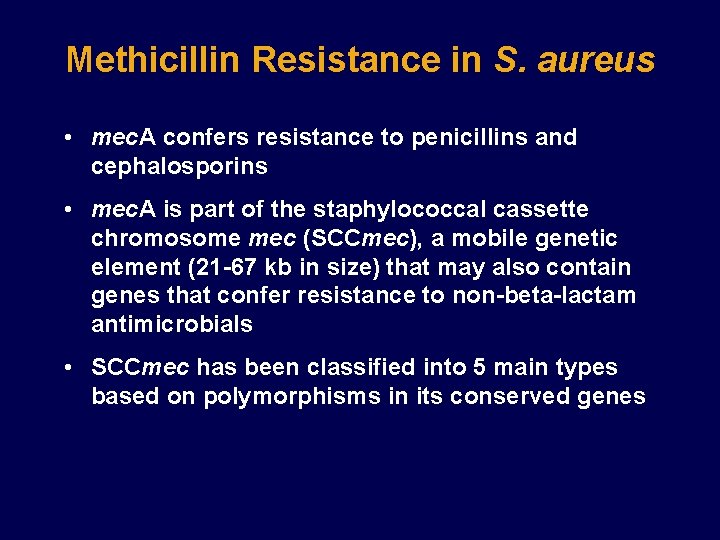
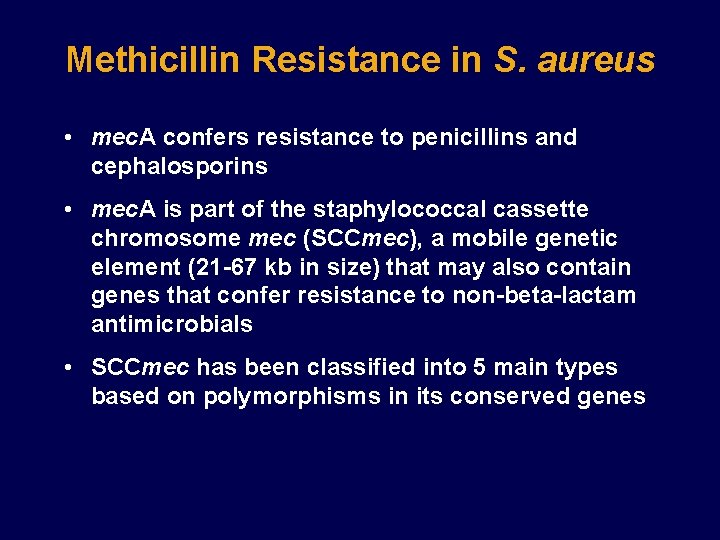
Methicillin Resistance in S. aureus • mec. A confers resistance to penicillins and cephalosporins • mec. A is part of the staphylococcal cassette chromosome mec (SCCmec), a mobile genetic element (21 -67 kb in size) that may also contain genes that confer resistance to non-beta-lactam antimicrobials • SCCmec has been classified into 5 main types based on polymorphisms in its conserved genes
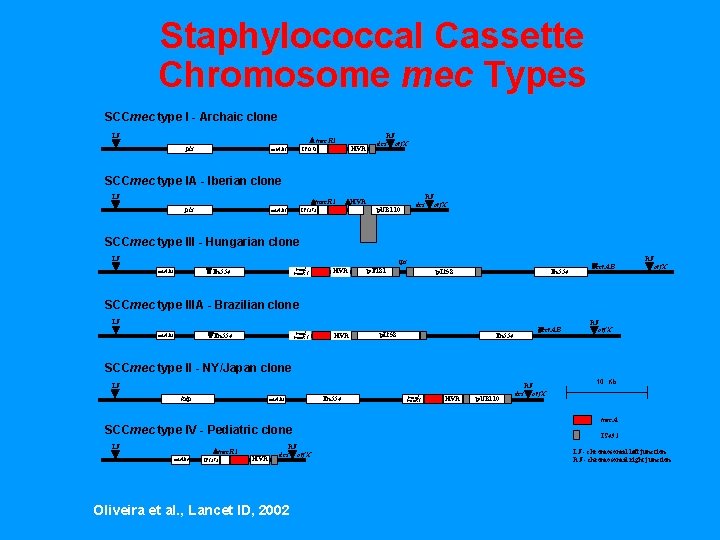
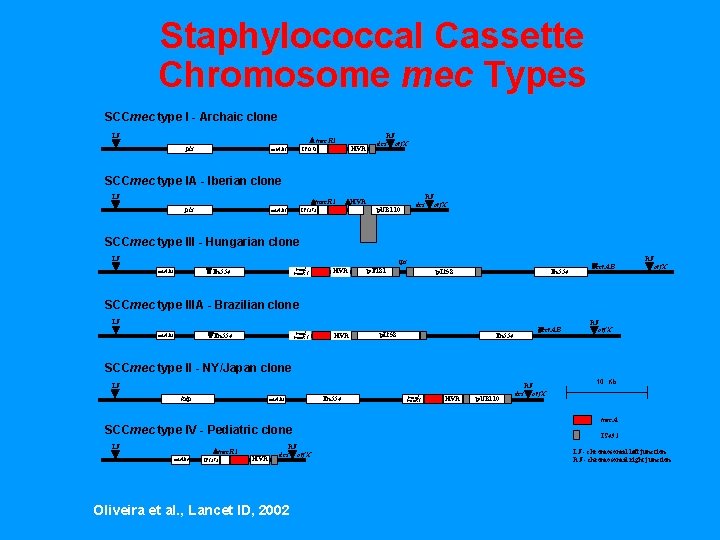
Staphylococcal Cassette Chromosome mec Types SCCmec type I - Archaic clone LJ D mec. R 1 pls ccr. AB 1 HVR IS 1272 RJ dcs orf. X SCCmec type IA - Iberian clone LJ Dmec. R 1 pls DHVR dcs p. UB 110 IS 1272 ccr. AB 1 RJ orf. X SCCmec type III - Hungarian clone LJ ips YTn 554 ccr. AB 3 mec. I mec. R 1 HVR p. T 181 p. I 258 Tn 554 Yccr. AB RJ orf. X SCCmec type IIIA - Brazilian clone LJ mec. I mec. R 1 YTn 554 ccr. AB 3 HVR p. I 258 Yccr. AB Tn 554 RJ orf. X SCCmec type II - NY/Japan clone LJ kdp ccr. AB 2 SCCmec type IV - Pediatric clone LJ Dmec. R 1 ccr. AB 4 IS 1272 HVR RJ dcs orf. X Oliveira et al. , Lancet ID, 2002 Tn 554 mec. I mec. R 1 HVR p. UB 110 dcs RJ orf. X 10 Kb mec. A IS 431 LJ - chromosomal left junction RJ - chromosomal right junction
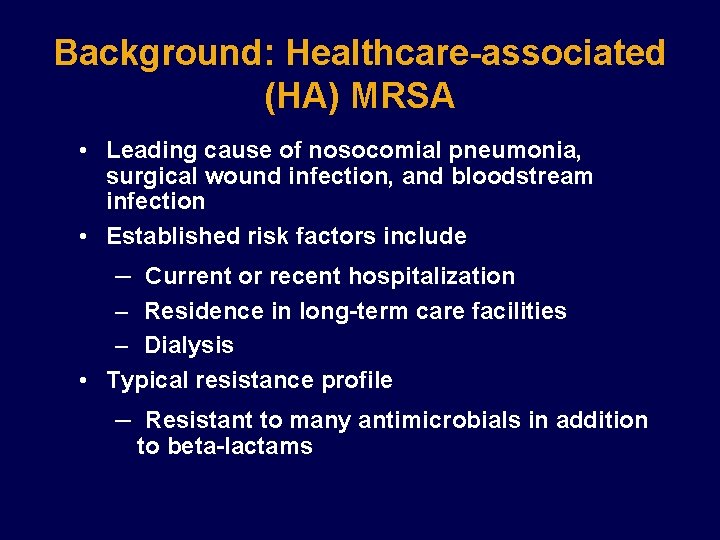
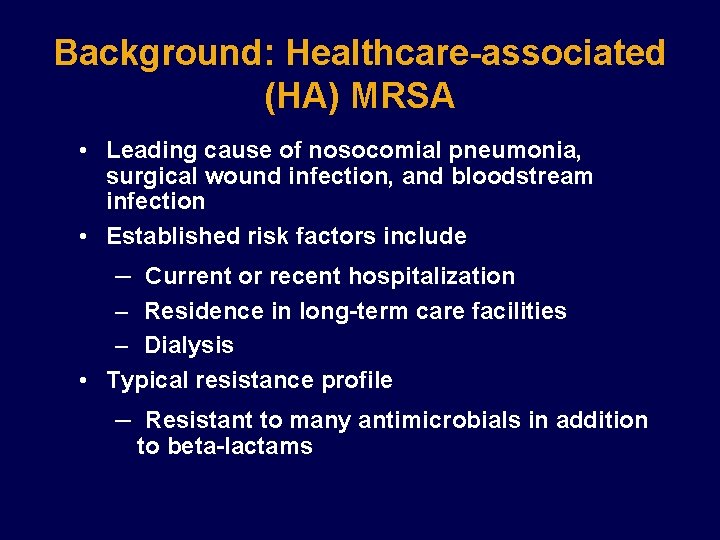
Background: Healthcare-associated (HA) MRSA • Leading cause of nosocomial pneumonia, surgical wound infection, and bloodstream infection • Established risk factors include – Current or recent hospitalization – Residence in long-term care facilities – Dialysis • Typical resistance profile – Resistant to many antimicrobials in addition to beta-lactams

Community-Associated Methicillin-Resistant Staphylococcus aureus (CA-MRSA) Reports began in 1980 s of MRSA occurring in the community in patients without established risk factors – Younger patients – Indigenous peoples and racial minorities – Skin infections common – Outbreaks: • Injection drug users • Players of close-contact sports • Prison/jail inmates • Group Homes (developmentally disabled) • Men who have sex with men
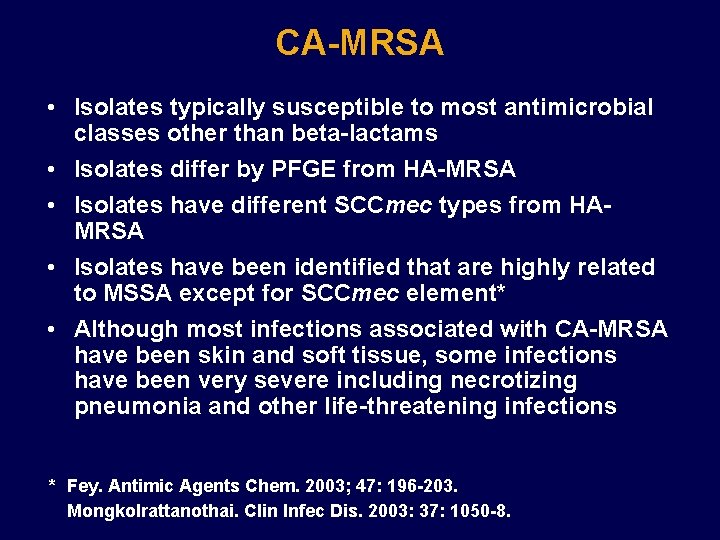
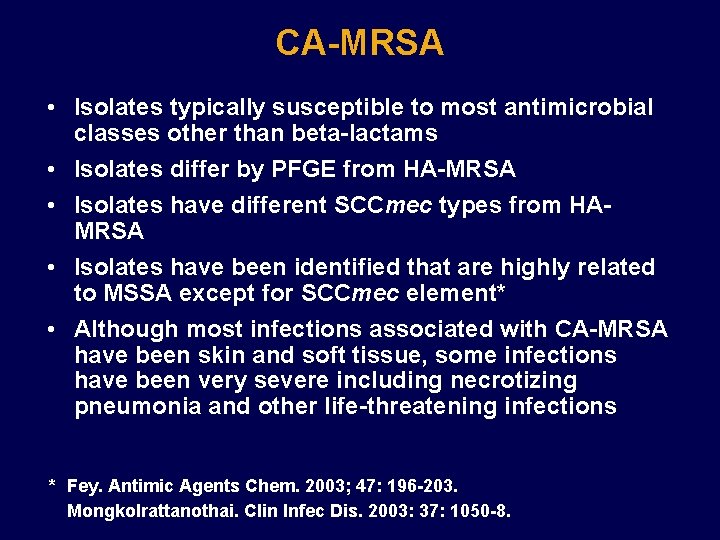
CA-MRSA • Isolates typically susceptible to most antimicrobial classes other than beta-lactams • Isolates differ by PFGE from HA-MRSA • Isolates have different SCCmec types from HAMRSA • Isolates have been identified that are highly related to MSSA except for SCCmec element* • Although most infections associated with CA-MRSA have been skin and soft tissue, some infections have been very severe including necrotizing pneumonia and other life-threatening infections * Fey. Antimic Agents Chem. 2003; 47: 196 -203. Mongkolrattanothai. Clin Infec Dis. 2003: 37: 1050 -8.
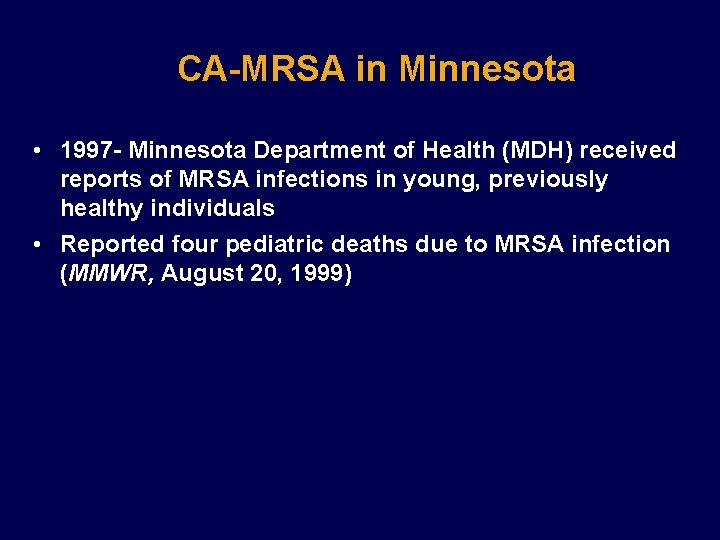
CA-MRSA in Minnesota • 1997 - Minnesota Department of Health (MDH) received reports of MRSA infections in young, previously healthy individuals • Reported four pediatric deaths due to MRSA infection (MMWR, August 20, 1999)
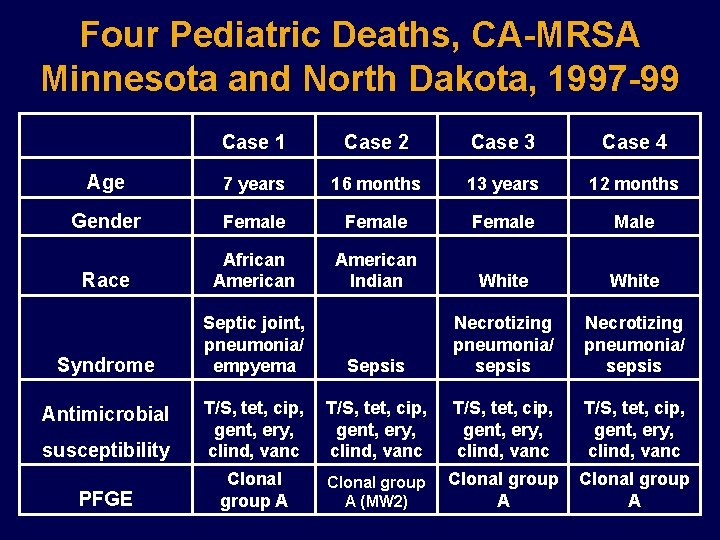
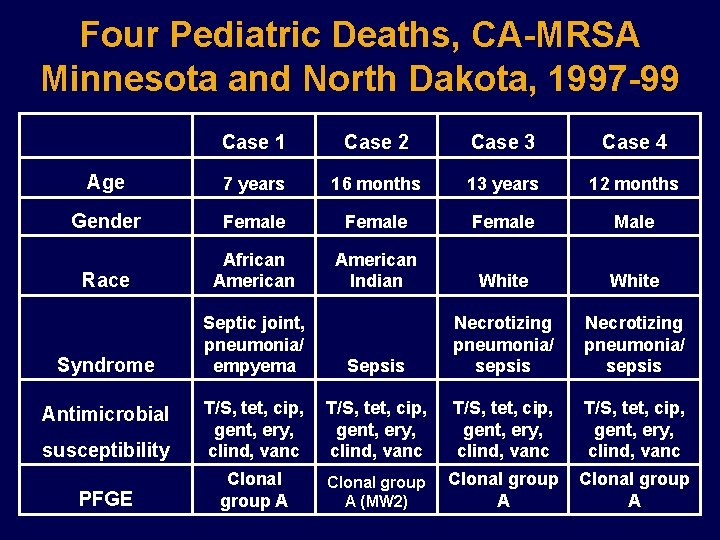
Four Pediatric Deaths, CA-MRSA Minnesota and North Dakota, 1997 -99 Case 1 Case 2 Case 3 Case 4 Age 7 years 16 months 13 years 12 months Gender Female Male Race African American Indian White Syndrome Septic joint, pneumonia/ empyema Sepsis Necrotizing pneumonia/ sepsis susceptibility T/S, tet, cip, gent, ery, clind, vanc PFGE Clonal group A (MW 2) Clonal group A Antimicrobial
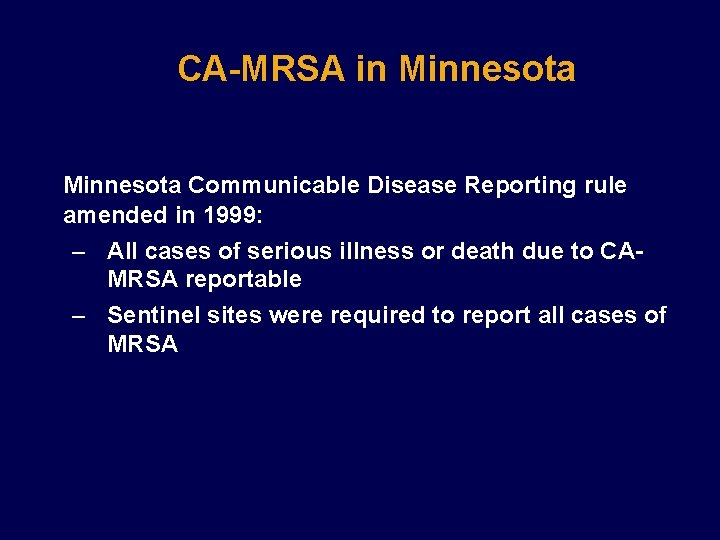
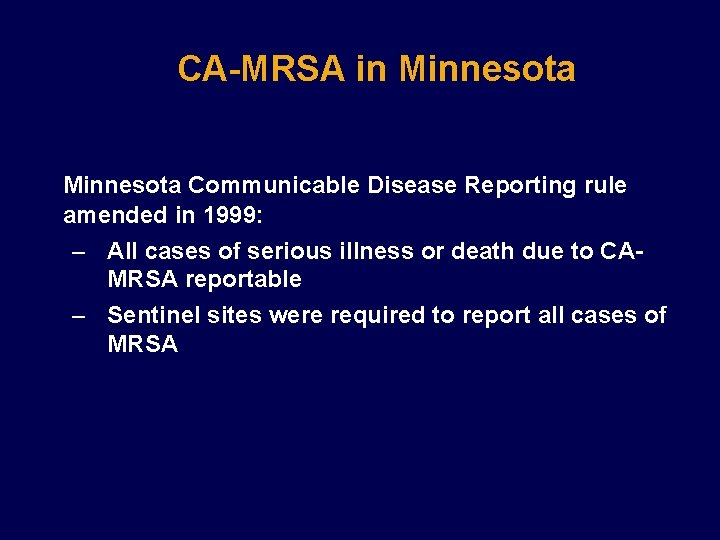
CA-MRSA in Minnesota Communicable Disease Reporting rule amended in 1999: – All cases of serious illness or death due to CAMRSA reportable – Sentinel sites were required to report all cases of MRSA
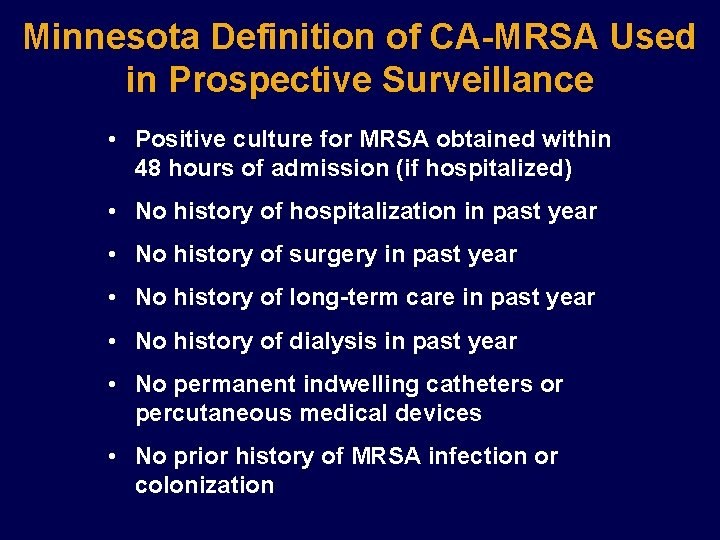
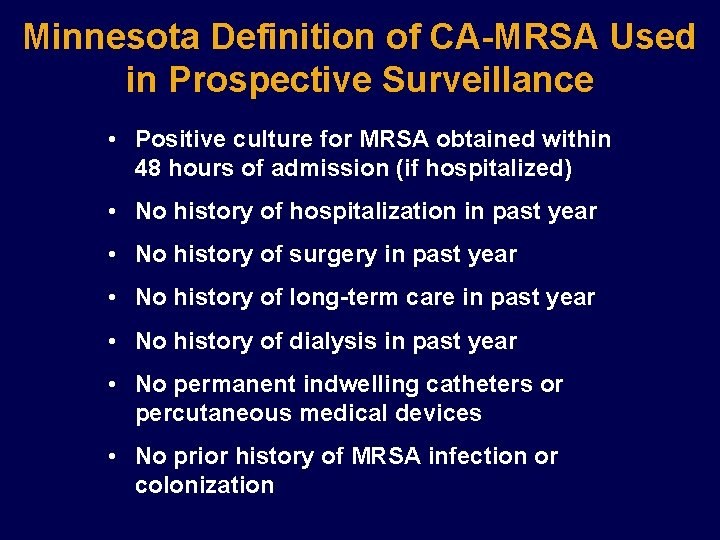
Minnesota Definition of CA-MRSA Used in Prospective Surveillance • Positive culture for MRSA obtained within 48 hours of admission (if hospitalized) • No history of hospitalization in past year • No history of surgery in past year • No history of long-term care in past year • No history of dialysis in past year • No permanent indwelling catheters or percutaneous medical devices • No prior history of MRSA infection or colonization
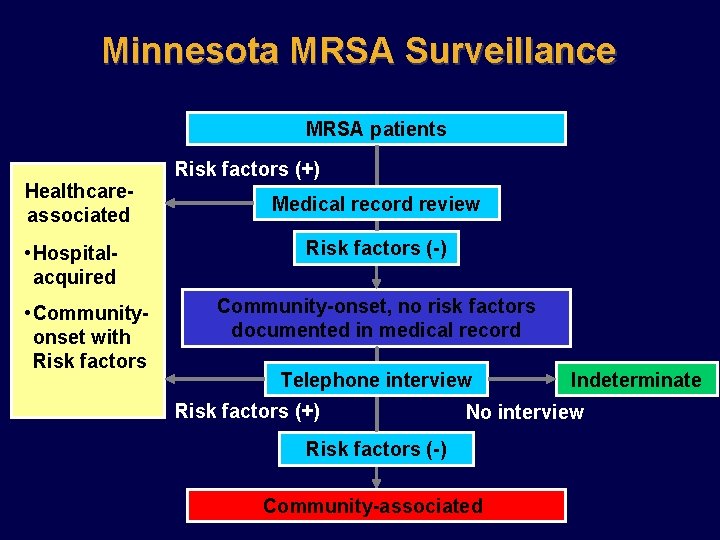
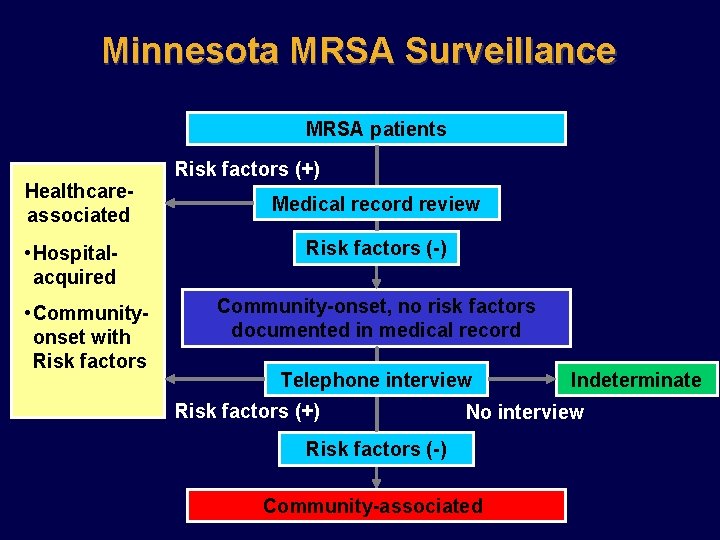
Minnesota MRSA Surveillance MRSA patients Healthcareassociated • Hospitalacquired • Communityonset with Risk factors (+) Medical record review Risk factors (-) Community-onset, no risk factors documented in medical record Telephone interview Risk factors (+) Indeterminate No interview Risk factors (-) Community-associated
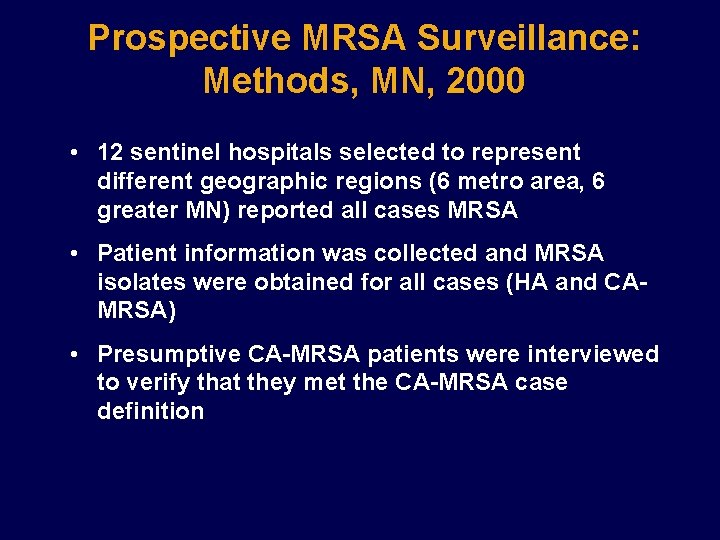
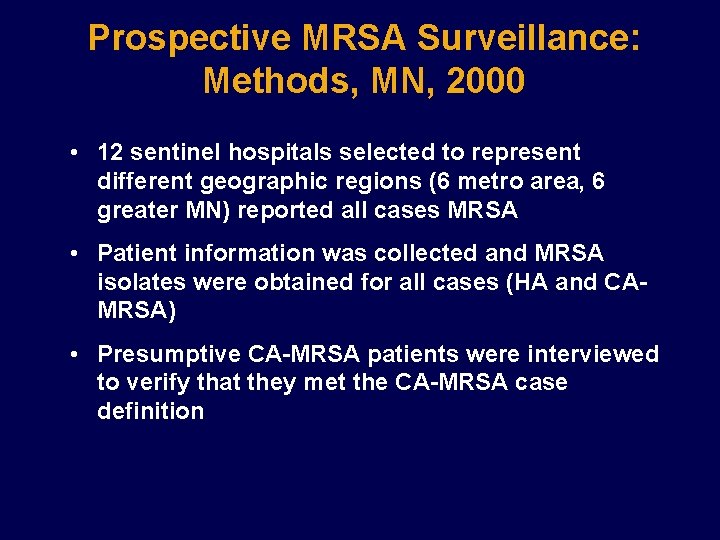
Prospective MRSA Surveillance: Methods, MN, 2000 • 12 sentinel hospitals selected to represent different geographic regions (6 metro area, 6 greater MN) reported all cases MRSA • Patient information was collected and MRSA isolates were obtained for all cases (HA and CAMRSA) • Presumptive CA-MRSA patients were interviewed to verify that they met the CA-MRSA case definition
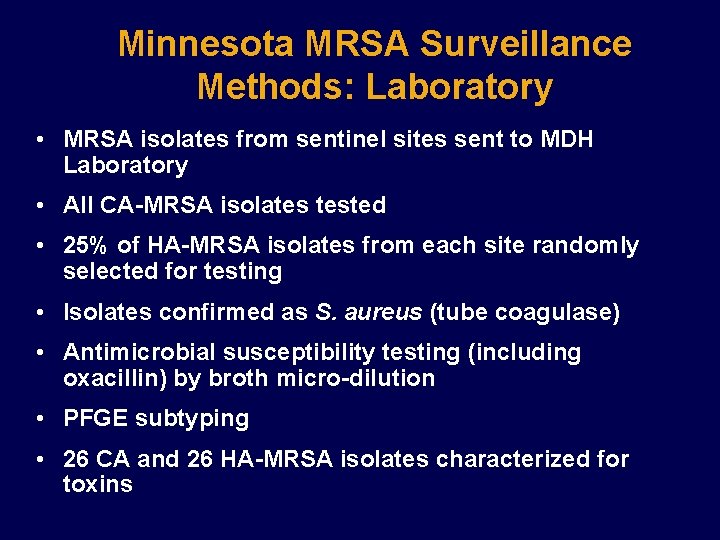
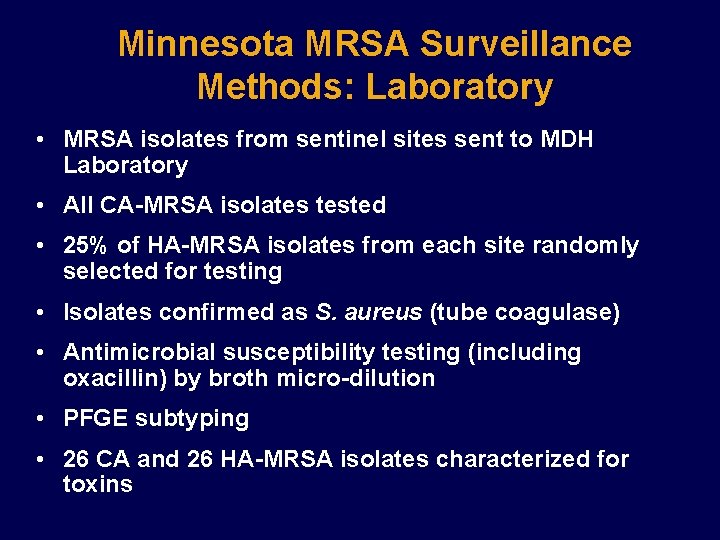
Minnesota MRSA Surveillance Methods: Laboratory • MRSA isolates from sentinel sites sent to MDH Laboratory • All CA-MRSA isolates tested • 25% of HA-MRSA isolates from each site randomly selected for testing • Isolates confirmed as S. aureus (tube coagulase) • Antimicrobial susceptibility testing (including oxacillin) by broth micro-dilution • PFGE subtyping • 26 CA and 26 HA-MRSA isolates characterized for toxins
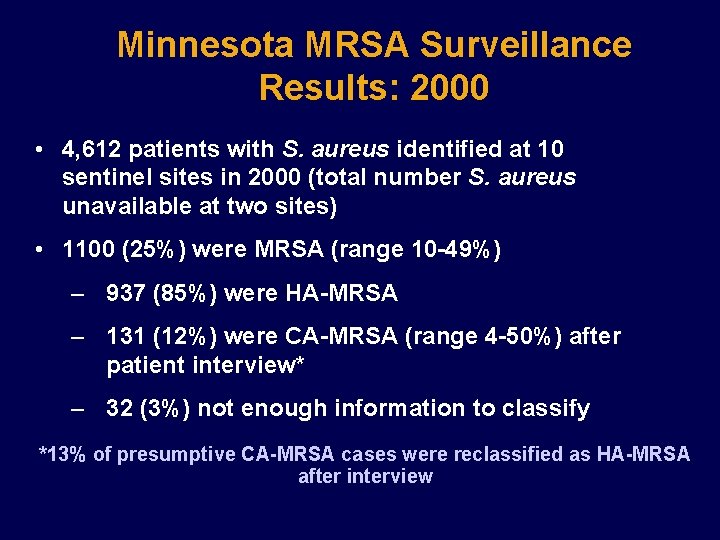
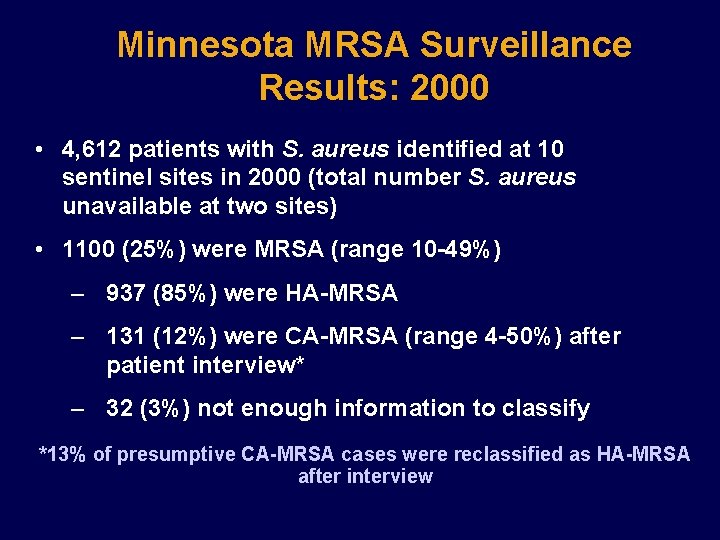
Minnesota MRSA Surveillance Results: 2000 • 4, 612 patients with S. aureus identified at 10 sentinel sites in 2000 (total number S. aureus unavailable at two sites) • 1100 (25%) were MRSA (range 10 -49%) – 937 (85%) were HA-MRSA – 131 (12%) were CA-MRSA (range 4 -50%) after patient interview* – 32 (3%) not enough information to classify *13% of presumptive CA-MRSA cases were reclassified as HA-MRSA after interview
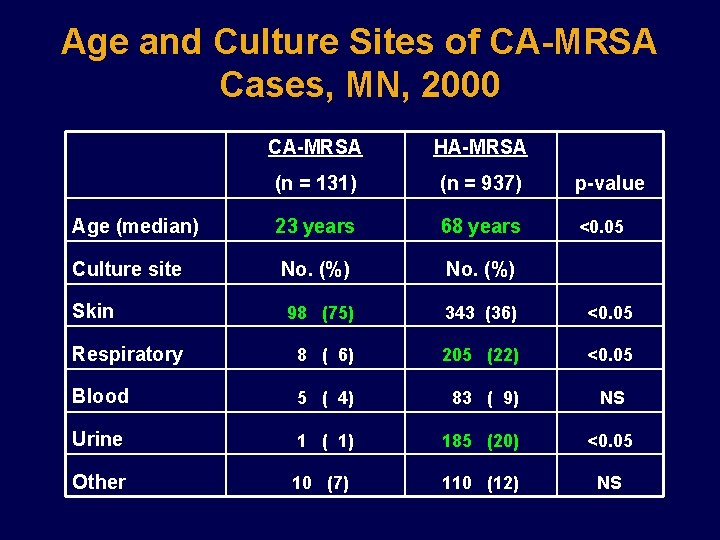
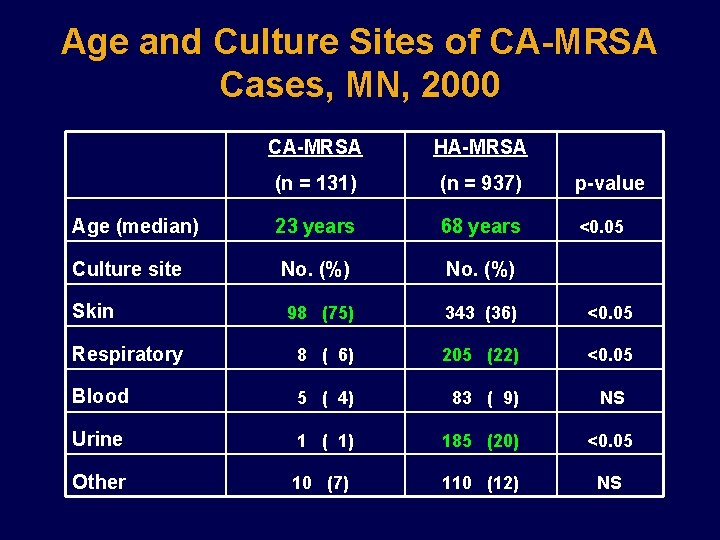
Age and Culture Sites of CA-MRSA Cases, MN, 2000 CA-MRSA HA-MRSA (n = 131) (n = 937) p-value Age (median) 23 years 68 years <0. 05 Culture site No. (%) 98 (75) 343 (36) <0. 05 Respiratory 8 ( 6) 205 (22) <0. 05 Blood 5 ( 4) 83 ( 9) NS Urine 1 ( 1) 185 (20) <0. 05 Other 10 (7) 110 (12) NS Skin
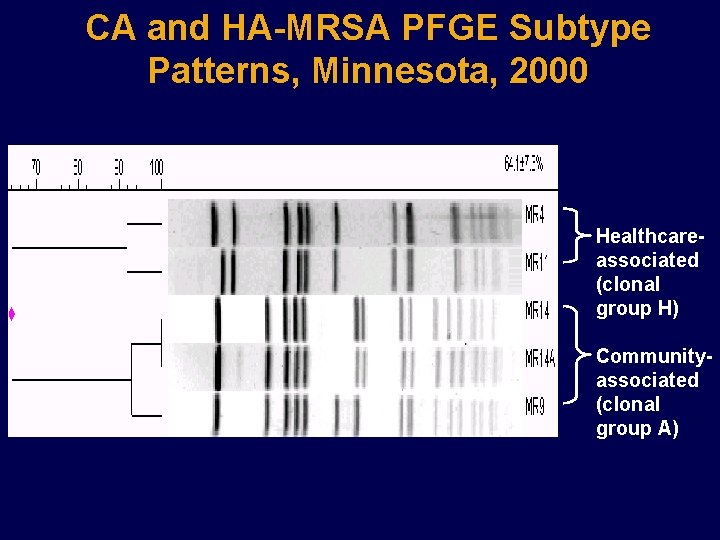
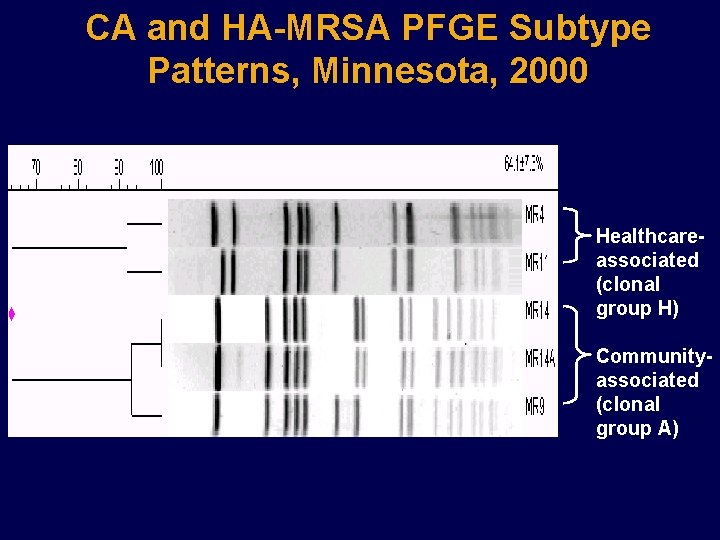
CA and HA-MRSA PFGE Subtype Patterns, Minnesota, 2000 Healthcareassociated (clonal group H) Communityassociated (clonal group A)
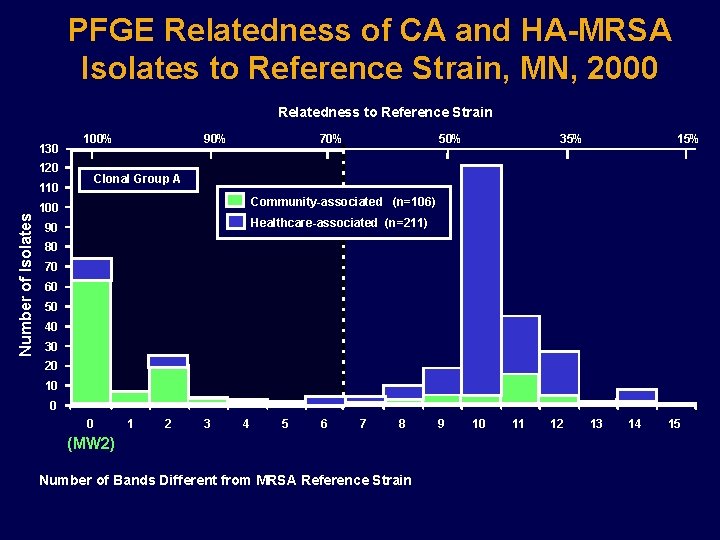
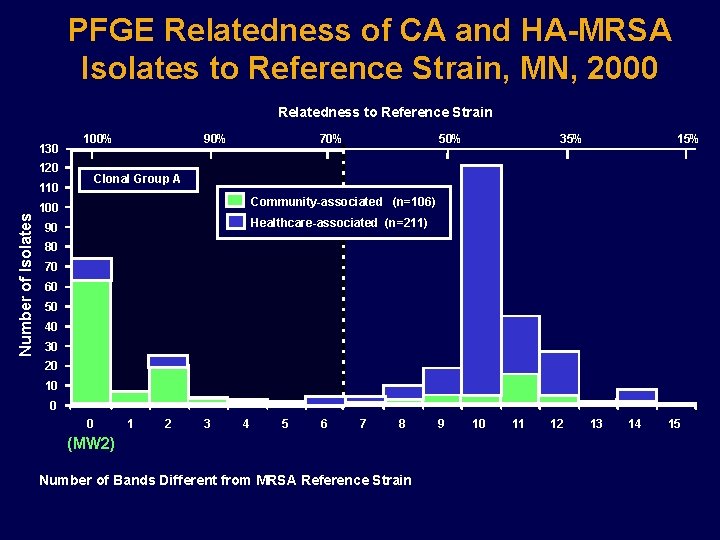
PFGE Relatedness of CA and HA-MRSA Isolates to Reference Strain, MN, 2000 Relatedness to Reference Strain 130 100% 120 70% 50% 35% 15% Clonal Group A 110 Number of Isolates 90% Community-associated (n=106) 100 Healthcare-associated (n=211) 90 80 70 60 50 40 30 20 10 0 0 1 2 3 4 5 6 7 8 (MW 2) Number of Bands Different from MRSA Reference Strain 9 10 11 12 13 14 15
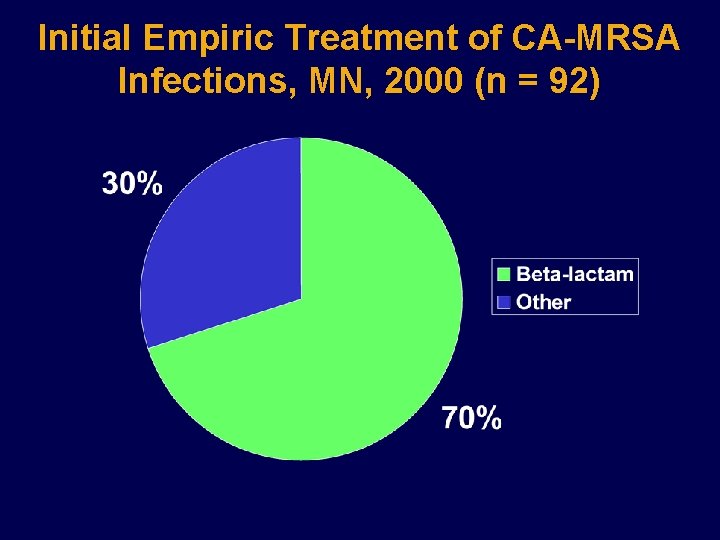
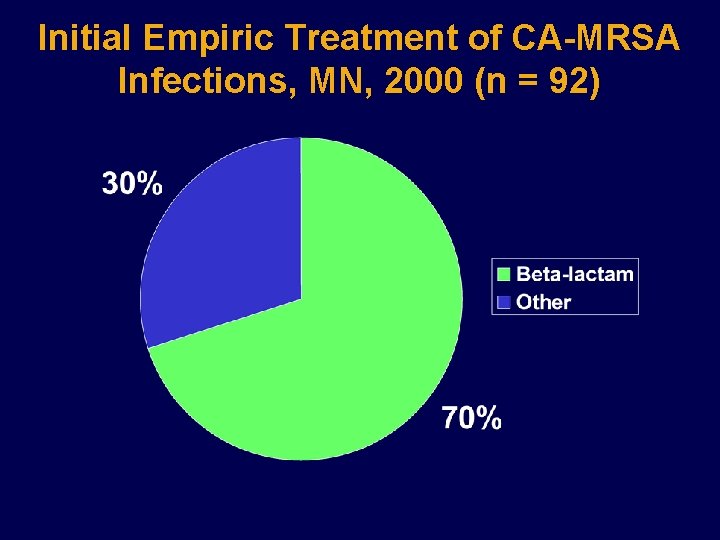
Initial Empiric Treatment of CA-MRSA Infections, MN, 2000 (n = 92)
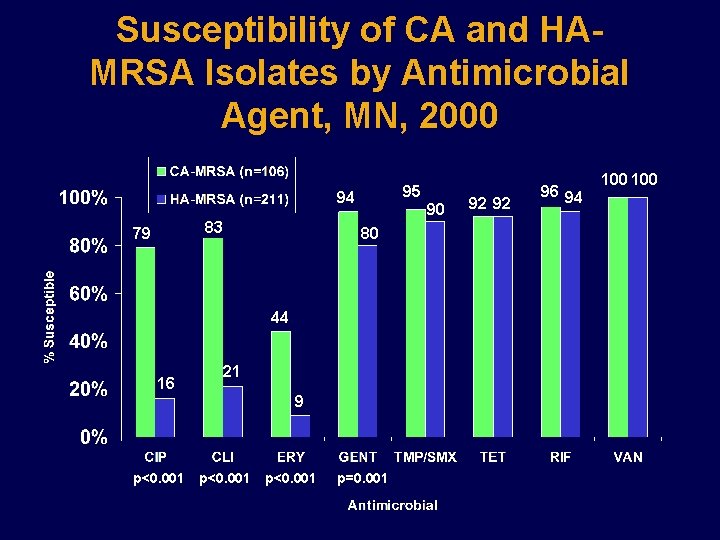
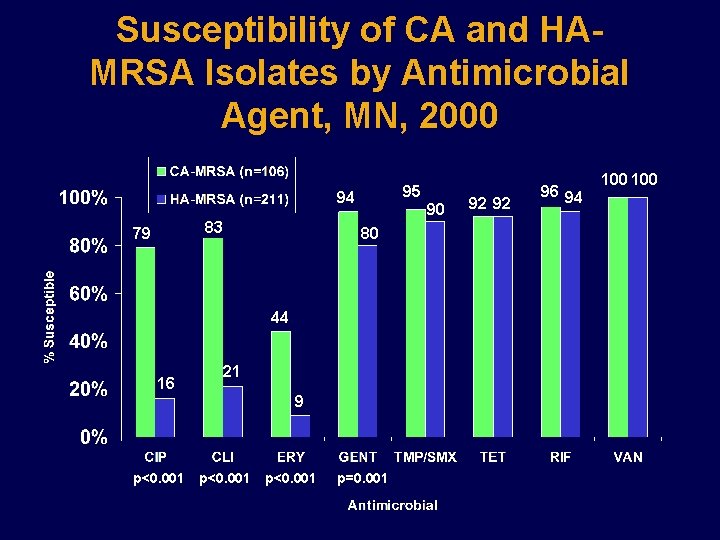
Susceptibility of CA and HAMRSA Isolates by Antimicrobial Agent, MN, 2000 95 94 83 79 90 80 44 16 21 9 p<0. 001 p=0. 001 92 92 96 94 100
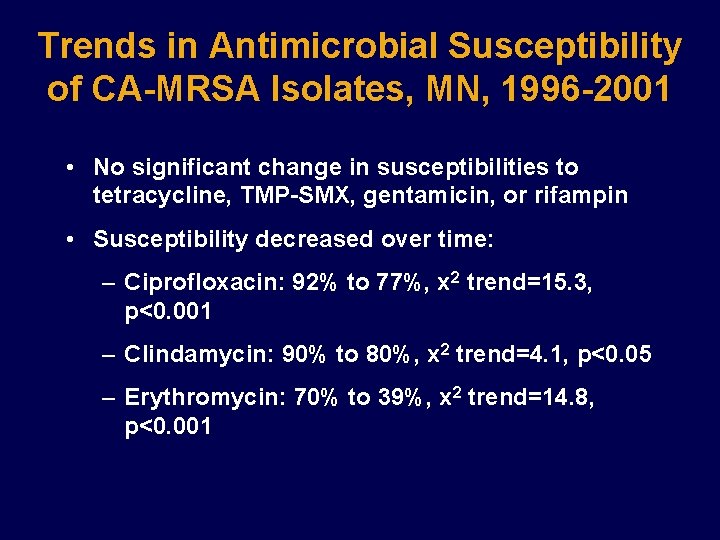
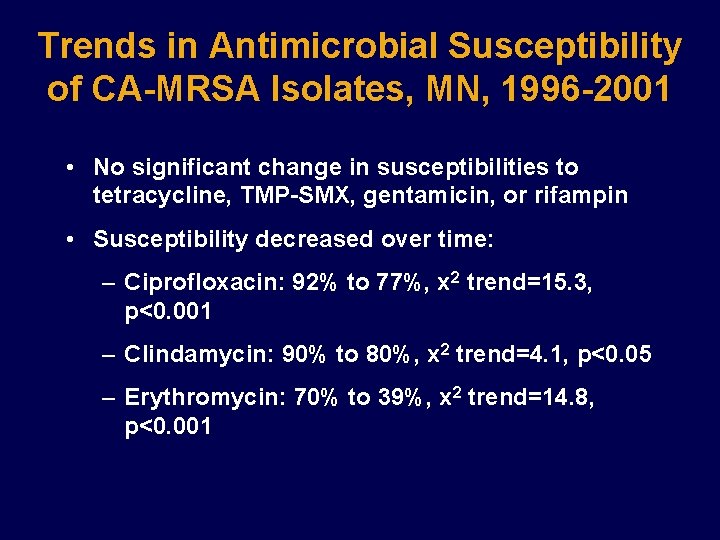
Trends in Antimicrobial Susceptibility of CA-MRSA Isolates, MN, 1996 -2001 • No significant change in susceptibilities to tetracycline, TMP-SMX, gentamicin, or rifampin • Susceptibility decreased over time: – Ciprofloxacin: 92% to 77%, x 2 trend=15. 3, p<0. 001 – Clindamycin: 90% to 80%, x 2 trend=4. 1, p<0. 05 – Erythromycin: 70% to 39%, x 2 trend=14. 8, p<0. 001
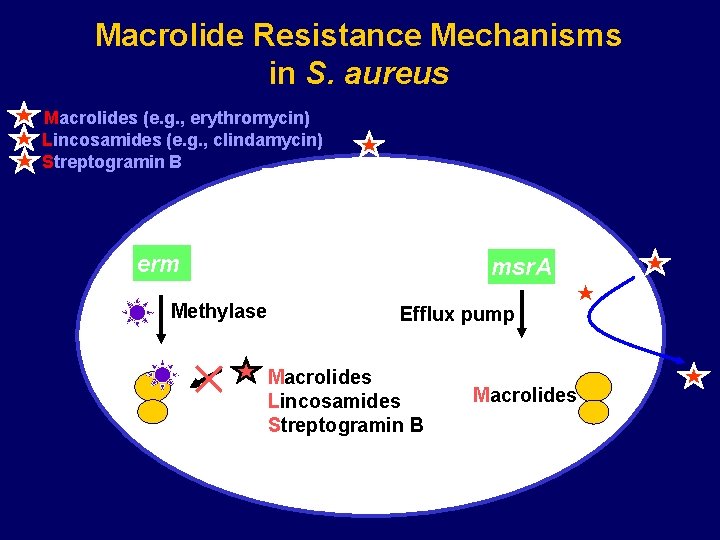
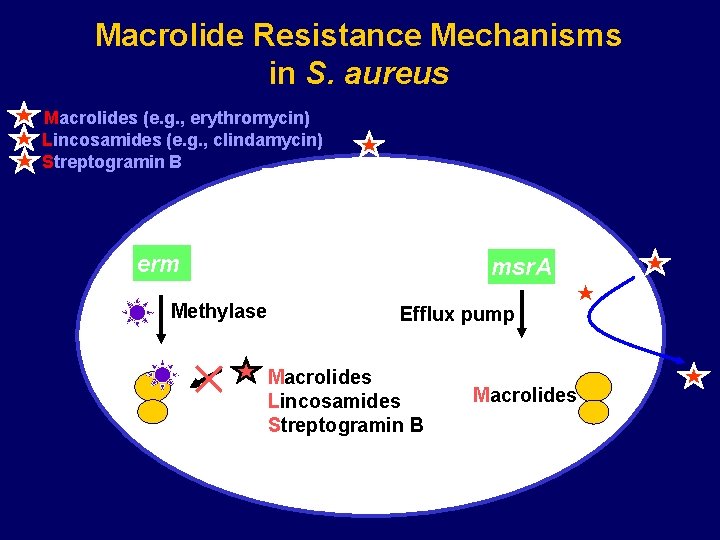
Macrolide Resistance Mechanisms in S. aureus Macrolides (e. g. , erythromycin) Lincosamides (e. g. , clindamycin) Streptogramin B Protein synthesis erm Methylase Ribosome msr. A Efflux pump Macrolides Lincosamides Streptogramin B Macrolides