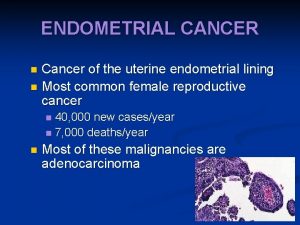
Endometrial cancer The most prevalent genital related cancer







- Slides: 22


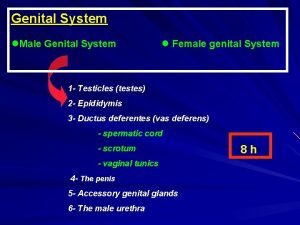
Endometrial cancer : The most prevalent genital related cancer of females and fourth most common malignancy of them. Up to 80% are endometroid type. Risk factors: long term esterogen exposure as it may increase chance of atypical endometrial hyperplasia-Aging-polycystic ovarian disease-obesity-metabolic syndrom and use of Tamoxifen. Most common symptoms: Abnormal uterine bleeding The only curable treatment : Surgical(Total hysterectomy and bilateral salpingooophorectomy-in some conditions omentectomy and retroperitoneal lymph node dissection)
Methods and materials : This study was a cross-sectional study conducted on 14 patients with low-grade endometrial cancer referred to Al-Zahra and Shahid Beheshti Hospitals in 20 I 6 -17 Inclusion criteria: 1)endometrial cancer with clinical grade I 2)stage 1 b of endometrial cancer 3) histological report of adenocarcinoma 4) patients' willing for participation in this study
Exclusion criteria : 1) hypersensitivity to technetium-99 and methylene blue 2) history of previous surgery or lymphadenectomy that has altered lymphatic drainage of the uterus (eg, myomectomy) 3) pregnancy.
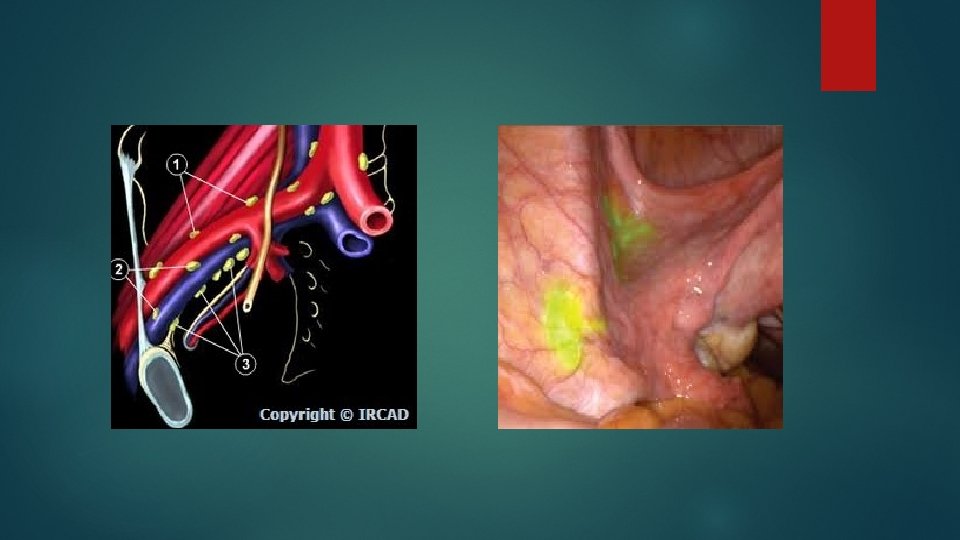
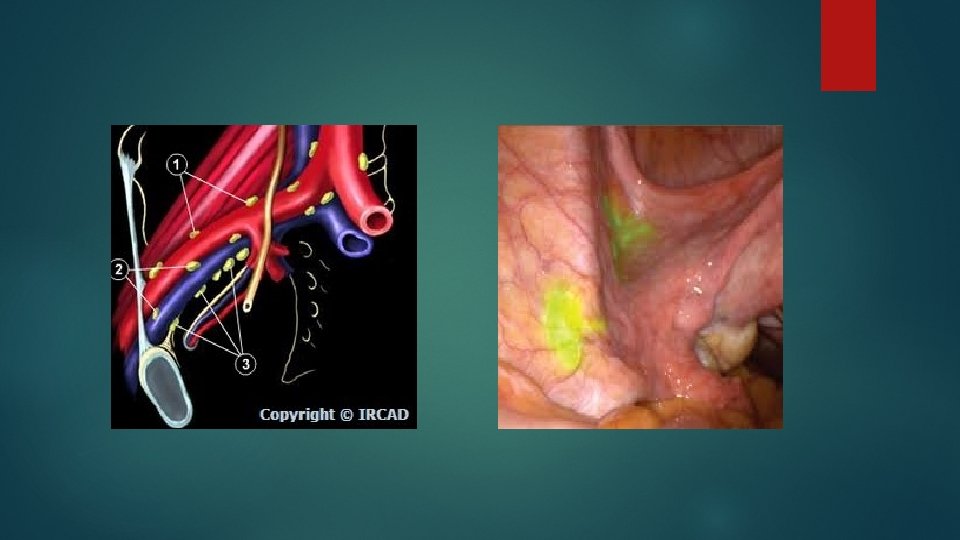
Methods & Materials : 18 -24 hours before operation, patients underwent Tc-99 injection. Injection region of Tc-99 was 3, 6, 9 and 12 o'clock regions of cervix. Each injection was done using spinal 25 gauge needle. In each region, one milliliter of Tc 99 was injected in two depth of cervical submocusal area (2 -3 mm depth) and cervical stromal region (3 -4 cm depth). In the next day, during operation tc-99 was detected was done by using manual gamma probe (Sergeoguide 2, produced by Iran) to find hot nodes. Methylene blue injection was done using spinal 25 gauge needle, injected to 3 and 6 o'clock region of cervix in operating room. Blue nodes were detected by naked eyes.
Then, in next day, all patients underwent total hysterectomy, bilateral salpingo -oophorectomy and total pelvic lymphadenectomy regardless of being detected as SLNs by methylene blue/hot nodes or not. Lymph node samples were sent for frozen section and assessment of positive/negative metastasis. Then data were analyzed with IBM SPSS 20 - United States software. Descriptive data were reported in mean ± standard deviation


Age (mean±std) 60. 64± 9. 18 Methylene blue (Number of diagnosed SLNs) 15/80 (18. 8%) TC-99 (Number of diagnosed SLNs) 10/80 (12. 5%) Methylene blue + TC-99 (Number of diagnosed SLNs) 5/80 (6. 3%) Lymphovascular invasion (lymph node) Present Absent 2 (14. 3%) 12(85. 7%) Table-1. Characteristics of study population Lymph node location (N) 27 (33. 8%) Right internal iliac Left internal iliac Right external iliac 14 (17. 5%) 3 (3. 8%) Left external iliac 9 (11. 3%) Right common iliac 6 (7. 5%) Left common iliac 8 (10%) Right obturator 8 (10%) Left obturator 5 (6. 3%) Table 2. Location of sentinel lymph nodes

Methylene blue TC-99 Methylene blue + TC-99 Detection rate 100% Sensitivity 100% Negative predictive value False negative 100% 0% Table-3. Detection rate. Sensitivity, negative predictive value and false negative of different tests
Other studies : Lymphatic mapping and sentinel node biopsy in endometrial cancer—a feasibility study using cervical injection of radiotracer and blue dye kadkhodayan S. shirvani Z. Hasanzadeh M – 2014 Result: studied patients with high grade endometrial cancer and reported 87% intra operative detection of SLN.
Study 2: Establishing a sentinel lymph node mapping algorithm for the treatment of early endometrial cancer Cormier B, Diaz JP, Shih K, Sampson RM, Sonoda Y, Park KJ, et 2016 Result : total of 21% of SLN s were detected using both blue dye & TC-99
Study 3: Sentinel lymph node mapping in early stage of endometrial and cervical cancer Allameh T, Hashemi V, Mohammadizadeh F, Behnamfar F. 2015 Result : detection rate of metastatic disease : 80% NPV: 100% false negative : 0 sensitivity : 100%

Discussion : Metastatic involvement : 2/14 (14. 3%) = consistent with other studies all dissected SLN regardless of intra operative method : 25% is similar to study of Beatrice cormier and opposite of kadkhodayan et al studies and Niikura et al studies (because their patient with high grade endometrial carcinoma) site of injection: cervical- fundal & sub-endometrial = consistent with other studies Location of lyph node: most common: internal iliac – no para aortic = consistent with other studies
SLN found by each test(methylene blue-Tc 99 -combination of methylene blue and Tc-99) = opposite of other studies Detection rate-sensitivity-NPV-False negative = similar to other studies Adverse effect : No = similar to other studies Although lymph node dissection in low grade endometrial cancer is contra versial but it is possible to have diverse diagnosis based on dilation and curettage in comparison to pathology. It means that pathological diagnosis maybe high garde tumor. Thus sentinel node detection can provide diagnosis of metastatic nodes and help prevent more tumor invasion.
Conclusion: Our study found that methylene blue, tc 99 and combination of them had acceptable rate of SLNs detection due to low probability of metastasis in low grade endometrial cancers with detection rate of 100%. sensitivity of 100%. negative predictive value of 100% and false negative of 0%. Further studies with larger population for pre-operative SLNs detection in low grade endometrial cancers are recommended.

 Difference between animal and human hair
Difference between animal and human hair Endometrial cancer
Endometrial cancer Endometrial cancer
Endometrial cancer Why computer incidents are so prevalent
Why computer incidents are so prevalent Pablo cubillos
Pablo cubillos Postmenopausal endometrial thickness
Postmenopausal endometrial thickness Bipartite uterus
Bipartite uterus Endometrial polyp gross
Endometrial polyp gross Endometrial histology menstrual cycle
Endometrial histology menstrual cycle Endometrial cells
Endometrial cells Shirodkar cerclage
Shirodkar cerclage Adenohipofisis
Adenohipofisis It projektov�� mana����r
It projektov�� mana����r What is this organ
What is this organ Tamaño normal del endometrio
Tamaño normal del endometrio Progesterone breakthrough bleeding
Progesterone breakthrough bleeding Two types of physical fitness
Two types of physical fitness Health related skill
Health related skill What is reproductive system
What is reproductive system Erkek genital sistem histolojisi
Erkek genital sistem histolojisi Internal genital organs female
Internal genital organs female Taenia saginata
Taenia saginata Síndrome de bubão genital
Síndrome de bubão genital