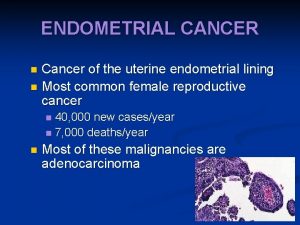
ENDOMETRIAL CANCER also endometrial polyps and endometrial hyperplasia















![HRT and hyperplasia • Do not use unopposed oestrogen in women with a uterus] HRT and hyperplasia • Do not use unopposed oestrogen in women with a uterus]](https://slidetodoc.com/presentation_image/f5f31fddde02eafe02e86730085fad07/image-16.jpg)

- Slides: 17

ENDOMETRIAL CANCER also endometrial polyps and endometrial hyperplasia Dr Jane Wilcock BSc FRCG SFHEA PGCert. Med. Ed. MAHEd. Endometrial cancer review 26: 7 193 -199 Macnab W. and Mehasseb M. K. Obstetrics, Gynaecology and Reproductive Medicine 2016 Endometrial Cancer: ESMO Clinical Practice Guidelines Ann Oncol 2013; 24 (Suppl 6): vi 33 -vi 38. N. Colombo, E. Preti, F. Landoni, S. Carinelli, A. Colombo, C. Marini, C. Sessa

The Ten Most Common Cancers in Females, Numbers of New Cases, UK, 2015 This chart excludes non-melanoma skin cancer because of known under-reporting http: //www. cancerresearchuk. org/health-professional/cancer-statistics/incidence/common-cancers-compared#heading-Two

Epidemiology/risks • In the world cervical cancer is most common cancer and endometrial second. • 50% new gynae cancers and rising incidence: increasing lifespan, obesity, less hysterectomies for benign conditions • 95%>40 years • 80% 60 -70 years old. • Lifetime risk 1 in 40 • Presents early with PMB usually

Endometrial cancer type 1 • 80%: from glandular epithelium adenocarcinoma • 50% complex atypical hyperplasia have endometrial cancer • Obesity • Nulliparity • Insulin resistance • Oestrogen (unopposed oestrogen; granulosa cell ovarian ca-5% rare, sex chord stroma derivation slow growing) • Genetic abnormalities in mismatch repair or tumour suppressor genes • Can be oestrogen and progesterone receptor positive (interact); loss of receptors occurs in carcinogenesis. Not yet useful in treatment but gaining a place in staging algorithms

Endometrial cancer type 2 • Unusual and a homogenous group of female hormone receptor negative cancers with a poorer prognosis serous endometrial cancer clear cell squamous Carcinosarcoma (malignant mixed Mullerian) Undifferentiated Endometrial stromal sarcomas ESS Not the same risk factors as type 1 Mutations of p 53 tumour suppressor gene common Often peritoneal spread ( like ovarian cancer) Metastases: lung, breast, ovary, GIT

Obesity, oestrogen and tamoxifen • • Up to 50% of endometrial cancers in developed world 2 -4 x increased risk adipocytes secrete oestrogen plus increased insulin levels due to resistance and increased insulin growth factor-1 (IGF-1) both anabolic hormones stimulating cell growth • State of play: limited evidence so far that lowering weight reduces cancer risk • Tamoxifen (selective oestrogen receptor modulator) as an adjuvant therapy in breast cancer increases endometrial pathology including cancer • State of play: no evidence that routine screening if no abnormal bleeding improves detection of endometrial cancer. Less tamoxifen being used as aromatase inhibitors have substituted (letrozole). Aromatase synthesises oestrogen in adipocytes.

Endometrial hyperplasia Endometrial atypical hyperplasia Endometrial cancer Type 1

<5% of endometrial cancer is associated with genetic inheritance • Tumour suppressor genes p 53, PTEN gene can be associated • Mismatch repair genes (MMR) • BRACA 1 and 2 not associated with endometrial cancer • Lynch II syndrome, HNPCC (hereditary non-polyposis colon cancer) is associated • Autosomal dominant with mutation DNA MMR genes • 50% F develop endometrial cancer as first cancer rather than CRC • 10% risk of other cancers • If at risk offered after completed family hysterectomy and BSO or endometrial annual imaging and biopsy

Diagnosis • Low prevalence prevents imaging as screening being practical • 90% PMB • Of women with PMB 10% will have cancer • Persistent vaginal discharge • Premenopausal women: IMB, abnormal calls at cervical screening, PCO women at increased risk Investigation History, FH, hormonal use, examination including PV and speculum to assess cervix, 2 WW referral TV USS: endometrial thickness postmenopausal has high NPV so<5 mm is reassuring; <3 mm more so

• • • Investigation Hysteroscopy and endometrial sampling 80% F in OPC Pipelle: detects ca postmenopausal women 99. 6% and pre-menopause 91% Endometrial hyperplasia 81% sensitive (identify cases correctly) and specificity 98% (identify those without hyperplasia correctly) MDT: CXR, CT scan, MRI for cervix and myometrial invasion Spread is to LNs, trans-tubal to ovaries and peritoneum, lungs Treatment is hysterectomy and BSO, can be laparoscopic and robotic Adjuvant or later stage radiotherapy: external or brachytherapy Controversies about lymph node dissection study on carboplatin and paclitaxel ongoing Progesterone therapy no a cure all: 40% recurrence after initial response in younger women wanting to retain their uterus

survival • 5 year survival 80%; most recurrences in first 3 years post op • Stage 1 disease 85 -90% • Future therapy: • PTEN is a protein produced in oestrogen high environments and regulates cell growth. Mutations of PTEN occur in many endometrial cancer type 1 and if PTEN errors then signalling pathways (m. TOR) are stimulates to cell division and growth. Temsirolinus inhibits m. TOR and has a 26% response rate and 63% disease stabilisation rate • Trials on Bevacizumab (Avastin), recombinant monocloncal antibody against vascular endothelial growth factor (VEGF) • Epidermal growth factor (EGFR) inhibitors (erlotinib, tyrosine kinase inhibitor TKI) not helpful so far but some tumours have high EGFR levels

Endometrial polyps: a study Human Reproduction, Vol. 32, No. 2 pp. 340– 345, 2017 The natural history of endometrial polyps M. Wong, B. Crnobrnja, V. Liberale, K. Dharmarajah, M. Widschwendter, and D. Jurkovic at UCL, Slovenia and Italy • 1997 -2005 case note review of women(112) treated expectantly≥ 6 months with endometrial cancer • all adults. All had 2 x USS and growth rate of polyps ascertained • exclusion: anyone on hormones or hormone modulators • Results: mean 22. 5 months range 6 -136 months • 11/75 =15% women with no abnormal bleeding developed abnormal bleeding • Growth rate did not associate with abnormal bleeding • 7/11= 6. 3% had complete spontaneous polyp regression • Those that had surgery (9%) were confirmed as benign • Findings: women should be told that the growth pattern of a polyp cannot be accurately predicated

Endometrial hyperplasia Management of Endometrial Hyperplasia Green-top Guideline No. 67 RCOG/BSGE Joint Guideline | February 2016 Presents as abnormal bleeding, HMB, irregular bleeding, IMB, PMB, unscheduled bleeding on HRT Risks: obesity, PCO syndrome, oestrogen secreting tumours, drug induced oestrogen stimulation, possible immunosuppression If endometrial thickness is<3 -4 mm then risk of endometrial cancer is <1% 2014 World Health Organization (WHO) classification separates endometrial hyperplasia into 1. hyperplasia without atypia; endometrial cancer is < 5% over 20 years and majority of cases regress spontaneously during follow-up 2. atypical hyperplasia

hyperplasia without atypia • endometrial cancer risk is < 5% over 20 years and most regress spontaneously during follow-up. Followed up in gynae. OPC 6 monthly, before if abnormal bleeding • Lose weight if obese, review (stop HRT) • Both continuous oral and local intrauterine (levonorgestrel-releasing intrauterine system [LNG-IUS]) progestogens are effective in achieving regression. • The LNG-IUS is first-line medical treatment as compared with oral progestogens it has a higher regression rate, more favourable bleeding profile and fewer adverse effects. Try to keep in for 5 years as reduces relapse rates • Continuous progestogens should be used (medroxyprogesterone 10– 20 mg/day or norethisterone 10– 15 mg/day) for women who decline the LNG-IUS. • Endometrial ablation not recommended • Can have hysterectomy (BSO in postmenopausal women) but not first line

Hyperplasia with atypia • Treatment is hysterectomy, laparoscopic if possible and possibly with BSO( individualise in pre-menopausal women) • If patients want fertility and refuse surgery then LNG-IUS or second line progesterone continuously with monitoring should be started and 3 monthly surveillance
![HRT and hyperplasia Do not use unopposed oestrogen in women with a uterus HRT and hyperplasia • Do not use unopposed oestrogen in women with a uterus]](https://slidetodoc.com/presentation_image/f5f31fddde02eafe02e86730085fad07/image-16.jpg)
HRT and hyperplasia • Do not use unopposed oestrogen in women with a uterus] • Report unscheduled bleeding on HRT (3 months as in FSRH hormonal contraception advice? ) • If hyperplasia occurs on sequential HRT change to continuous progesterone as LNG-IUS or with continuous combined HRT preparation (Kliovance) under specialist advice

Thankyou for listening
 Projektov�� mana����r
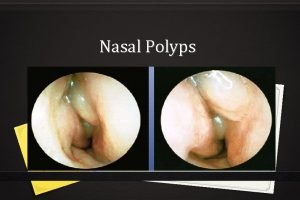
Projektov�� mana����r Unilateral nasal obstruction
Unilateral nasal obstruction Cnidaria
Cnidaria Endometrial cancer
Endometrial cancer Endometrial cancer
Endometrial cancer Hyperplasia and hypertrophy difference
Hyperplasia and hypertrophy difference Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics 17 hydroxyprogesterone levels
17 hydroxyprogesterone levels Virilisation in females
Virilisation in females Sebaceous hyperplasia
Sebaceous hyperplasia Fundus mirigy hyperplasia
Fundus mirigy hyperplasia Vaginal agensis
Vaginal agensis Intimal hyperplasia
Intimal hyperplasia Seminal vesicle
Seminal vesicle Intimal hyperplasia
Intimal hyperplasia Intimal hyperplasia
Intimal hyperplasia Gingival hyperplasia
Gingival hyperplasia