Benign Prostatic Hyperplasia Benign Prostatic Hyperplasia n 11242020
Benign Prostatic Hyperplasia
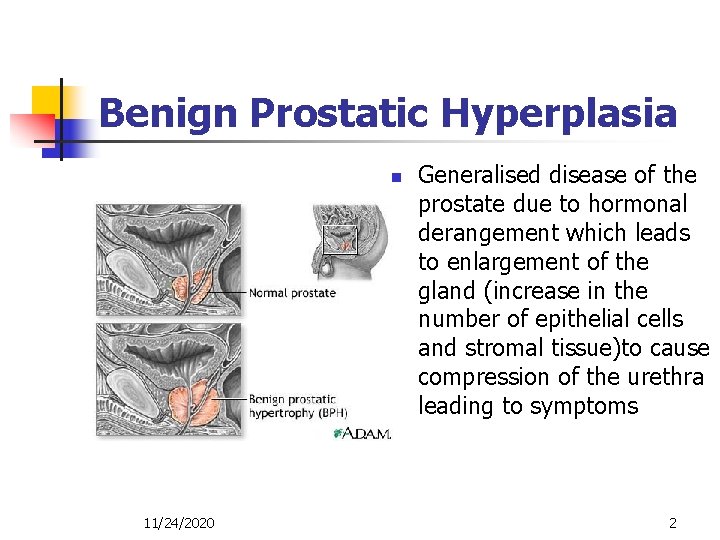
Benign Prostatic Hyperplasia n 11/24/2020 Generalised disease of the prostate due to hormonal derangement which leads to enlargement of the gland (increase in the number of epithelial cells and stromal tissue)to cause compression of the urethra leading to symptoms 2
BPH Proposed Etiologies n n n Cause not completely understood Reawakening of the urogenital sinus to proliferate Change in hormonal milieu with alterations in the testosterone/estrogen balance Induction of prostatic growth factors Increased stem cells/decreased stromal cell death Accumulation of dihydroxytestosterone, stimulation by estrogen and prostatic growth hormone actions
BPH facts n n Occurs in 50% of men over 50 and in 80% of men over 80 have BPH progresses differently in every individual Many men with BPH may have mild symptoms and may never need treatment BPH does not predispose to the development of prostate cancer 11/24/2020 4
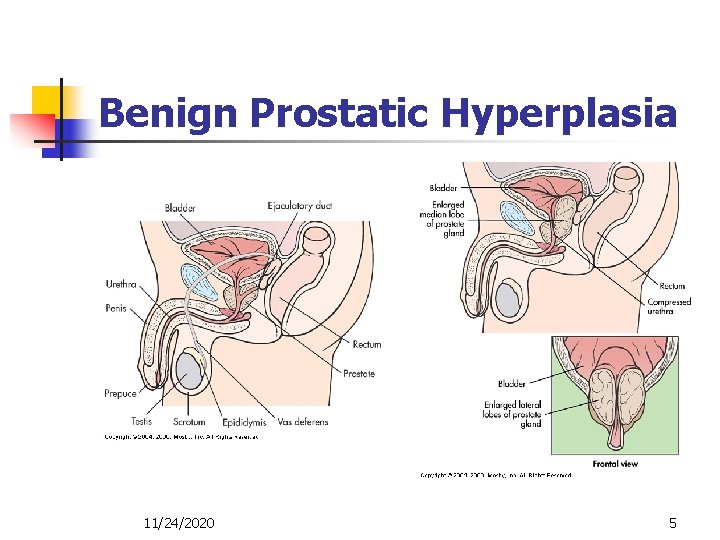
Benign Prostatic Hyperplasia 11/24/2020 5
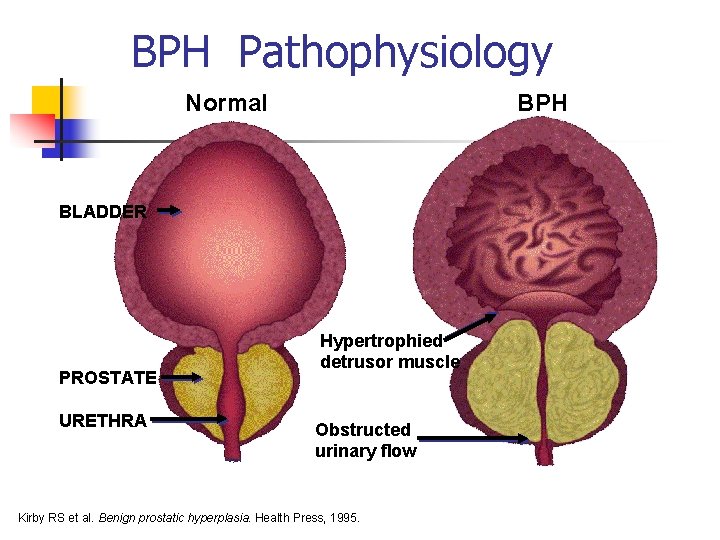
BPH Pathophysiology Normal BPH BLADDER PROSTATE URETHRA Hypertrophied detrusor muscle Obstructed urinary flow Kirby RS et al. Benign prostatic hyperplasia. Health Press, 1995.
BPH Pathophysiology n n n Slow and insidious changes over time Complex interactions between prostatic urethral resistance, intravesical pressure, detrussor functionality, neurologic integrity, and general physical health. Initial hypertrophy detrussor decompensation poor tone diverticula formation increasing urine volume hydronephrosis upper tract dysfunction
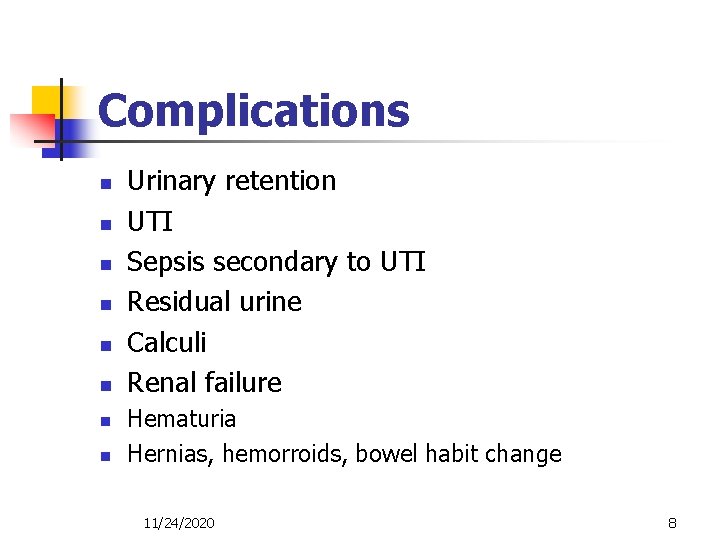
Complications n n n n Urinary retention UTI Sepsis secondary to UTI Residual urine Calculi Renal failure Hematuria Hernias, hemorroids, bowel habit change 11/24/2020 8
Clinical manifestations n Voiding symptoms n decrease in the urinary stream n Straining n Dribbling at the end of urination n Intermittency n Hesitancy n Pain or burning during urination n Feeling of incomplete bladder emptying 11/24/2020 9
Clinical manifestations n Irritative symptoms urinary frequency urgency dysuria bladder pain nocturia incontinence symptoms associated with infection 11/24/2020 10
Benign Prostatic Hyperplasia • Leading to “symptom bother” and worsened QOL
Other Relevant History n n GU History (STD, trauma, surgery) Other disorders (eg. neurologic, diabetes) Medications (anti-cholinergics) Functional Status
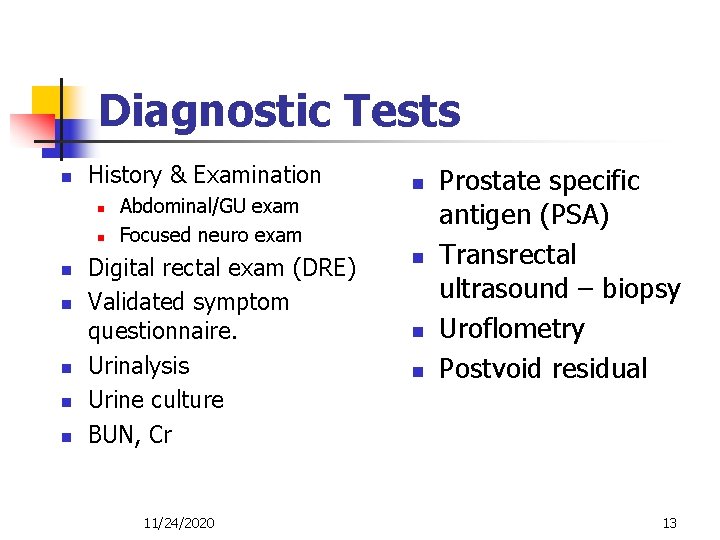
Diagnostic Tests n History & Examination n n n Abdominal/GU exam Focused neuro exam Digital rectal exam (DRE) Validated symptom questionnaire. Urinalysis Urine culture BUN, Cr 11/24/2020 n n Prostate specific antigen (PSA) Transrectal ultrasound – biopsy Uroflometry Postvoid residual 13
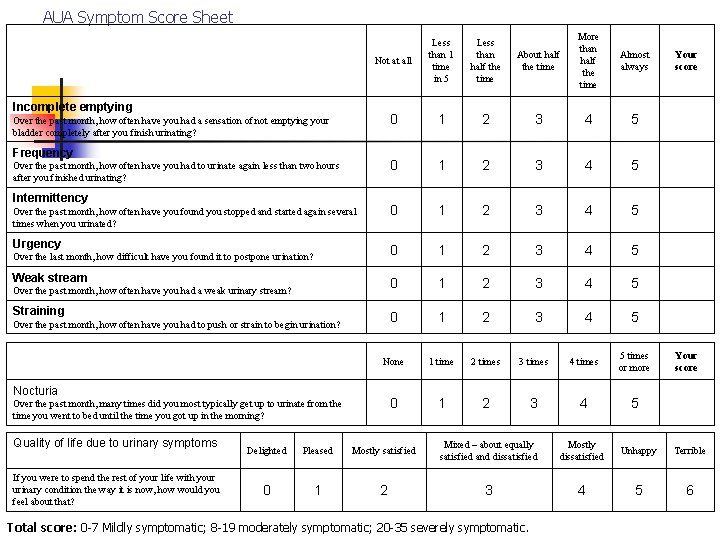
AUA Symptom Score Sheet About half the time More than half the time Almost always Your score 2 3 4 5 1 2 3 4 5 0 1 2 3 4 5 None 1 time 2 times 3 times 4 times 5 times or more Your score 0 1 2 3 4 5 Not at all Less than 1 time in 5 Less than half the time 0 1 0 Over the past month, how often have you found you stopped and started again several times when you urinated? Urgency Incomplete emptying Over the past month, how often have you had a sensation of not emptying your bladder completely after you finish urinating? Frequency Over the past month, how often have you had to urinate again less than two hours after you finished urinating? Intermittency Over the last month, how difficult have you found it to postpone urination? Weak stream Over the past month, how often have you had a weak urinary stream? Straining Over the past month, how often have you had to push or strain to begin urination? Nocturia Over the past month, many times did you most typically get up to urinate from the time you went to bed until the time you got up in the morning? Quality of life due to urinary symptoms If you were to spend the rest of your life with your urinary condition the way it is now, how would you feel about that? Delighted Pleased Mostly satisfied Mixed – about equally satisfied and dissatisfied Mostly dissatisfied Unhappy Terrible 0 1 2 3 4 5 6 Total score: 0 -7 Mildly symptomatic; 8 -19 moderately symptomatic; 20 -35 severely symptomatic.
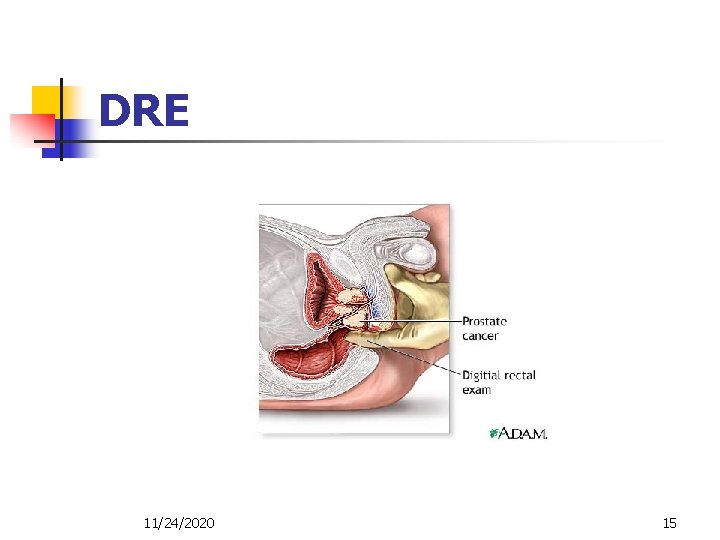
DRE 11/24/2020 15
BPH Danger Signs on DRE n n n Firm to hard nodules Irregularities, unequal lobes Induration Stony hard prostate Any palpable nodular abnormality suggests cancer and warrants investigation
Optional Evaluations and Diagnostic Tests n n Urine cytology in patients with: n Predominance of irritative voiding symptoms. n Smoking history Flow rate and post-void residual n Not necessary before medical therapy but should be considered in those undergoing invasive therapy or those with neurologic conditions Upper tract evaluation if hematuria, increased creatinine Cystoscopy

PSA n Elevated levels of PSA n 0 – 4 ng/ml n n n Prostatic pathology Correlates with tumor mass Some men with prostate cancer have normal PSA levels 11/24/2020 19
BPH SYMPTOMS Differential Diagnosis n n n n Urethral stricture Bladder neck contracture Carcinoma of the prostate Carcinoma of the bladder Bladder calculi Urinary tract infection and prostatitis Neurogenic bladder
BPH TREATMENT INDICATIONS Absolute vs Relative n n n Severe obstruction Urinary retention Signs of upper tract dilatation and renal insufficiency n n Moderate symptoms of prostatism Recurrent UTI’s Hematuria Quality of life issues
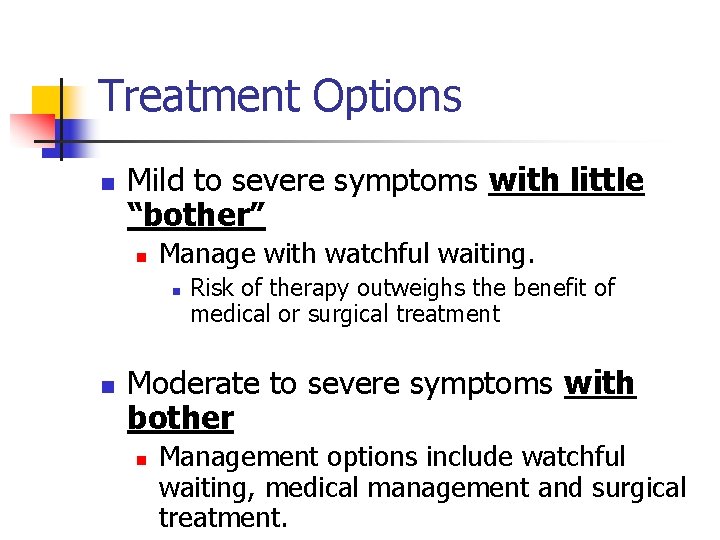
Treatment Options n Mild to severe symptoms with little “bother” n Manage with watchful waiting. n n Risk of therapy outweighs the benefit of medical or surgical treatment Moderate to severe symptoms with bother n Management options include watchful waiting, medical management and surgical treatment.
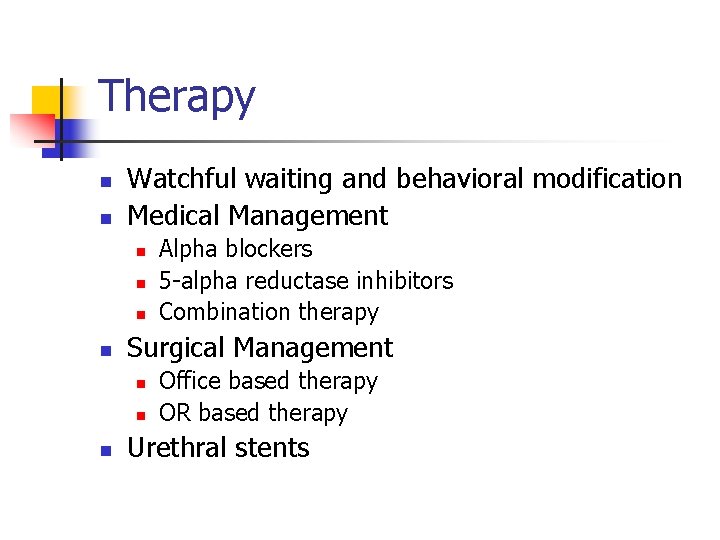
Therapy n n Watchful waiting and behavioral modification Medical Management n n Surgical Management n n n Alpha blockers 5 -alpha reductase inhibitors Combination therapy Office based therapy OR based therapy Urethral stents
Watchful Waiting and Behavioral Modification n “is the preferred management technique in patients with mild symptoms and minimal bother” n AUA score < 7, n 1/3 improve on own.
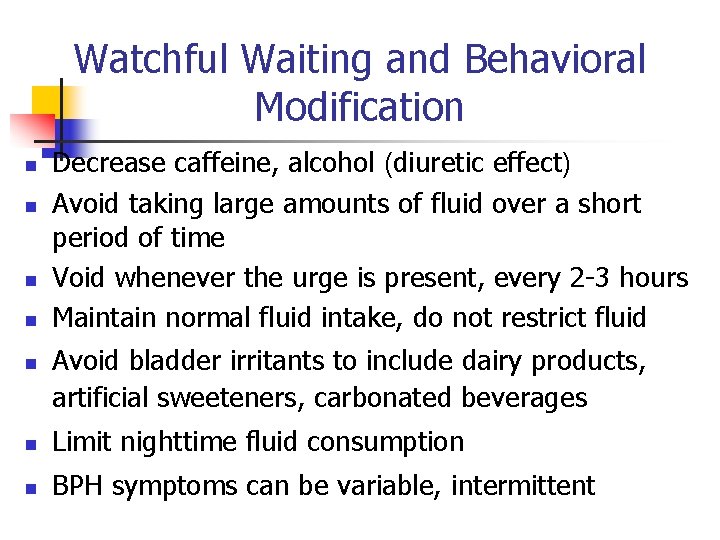
Watchful Waiting and Behavioral Modification n n Decrease caffeine, alcohol (diuretic effect) Avoid taking large amounts of fluid over a short period of time Void whenever the urge is present, every 2 -3 hours Maintain normal fluid intake, do not restrict fluid Avoid bladder irritants to include dairy products, artificial sweeteners, carbonated beverages n Limit nighttime fluid consumption n BPH symptoms can be variable, intermittent
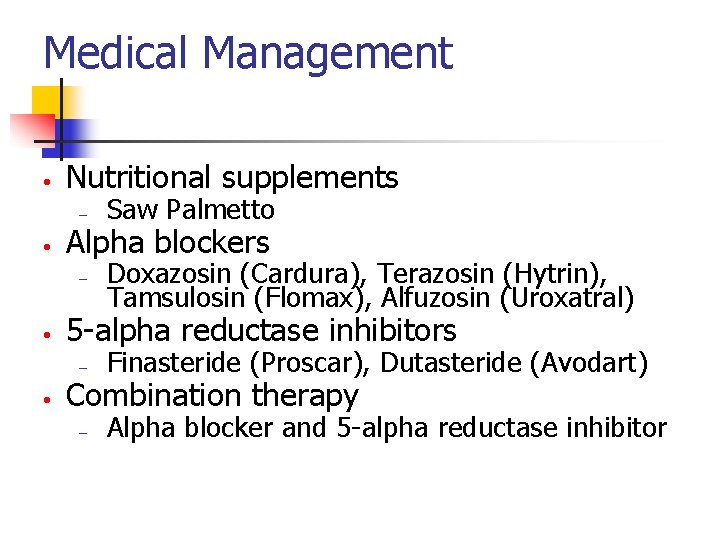
Medical Management • • Nutritional supplements – Saw Palmetto – Doxazosin (Cardura), Terazosin (Hytrin), Tamsulosin (Flomax), Alfuzosin (Uroxatral) Alpha blockers 5 -alpha reductase inhibitors – Finasteride (Proscar), Dutasteride (Avodart) – Alpha blocker and 5 -alpha reductase inhibitor Combination therapy
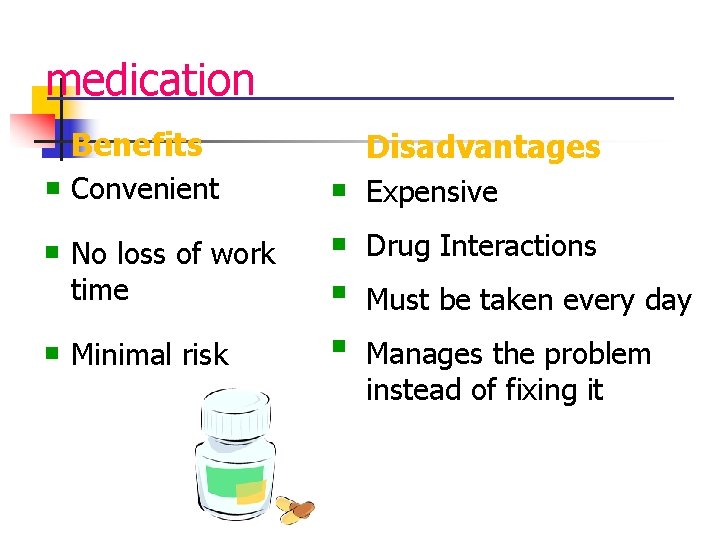
medication Benefits n n n Disadvantages Convenient n Expensive No loss of work time n Drug Interactions n Must be taken every day Minimal risk n Manages the problem instead of fixing it
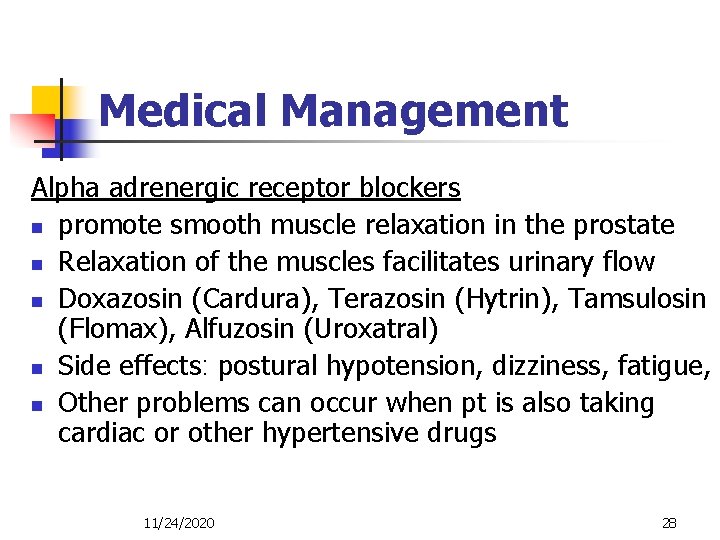
Medical Management Alpha adrenergic receptor blockers n promote smooth muscle relaxation in the prostate n Relaxation of the muscles facilitates urinary flow n Doxazosin (Cardura), Terazosin (Hytrin), Tamsulosin (Flomax), Alfuzosin (Uroxatral) n Side effects: postural hypotension, dizziness, fatigue, n Other problems can occur when pt is also taking cardiac or other hypertensive drugs 11/24/2020 28
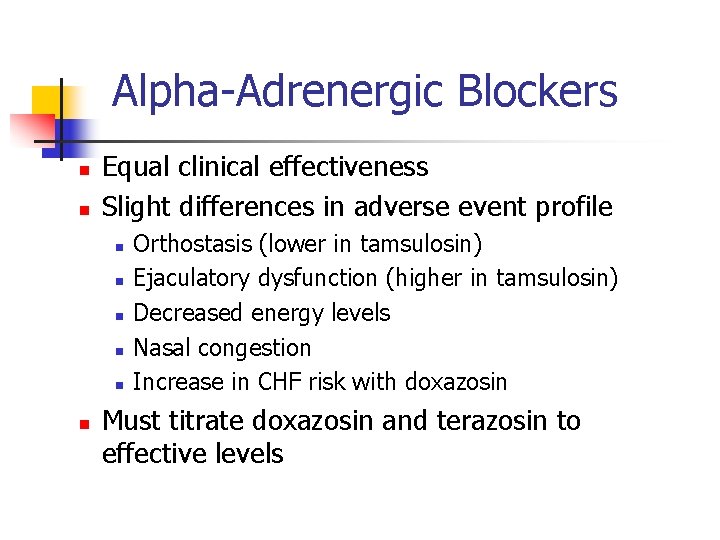
Alpha-Adrenergic Blockers n n Equal clinical effectiveness Slight differences in adverse event profile n n n Orthostasis (lower in tamsulosin) Ejaculatory dysfunction (higher in tamsulosin) Decreased energy levels Nasal congestion Increase in CHF risk with doxazosin Must titrate doxazosin and terazosin to effective levels
Medical Management 5 alpha reductase inhibitor (finasteride : Proscar) n Reduce size of prostate gland by up to 30 % n Blocks the enzyme of 5 alpha reductase which is nec, for the conversion of testosterone to dihydroxytestostersone n Regression of hyperplastic growth n Don’t work immediately n Small effect on symptom score and flow rates 11/24/2020 30
5 -Alpha Reductase Inhibitors n Agents are effective and appropriate treatment for patients with lower urinary tract symptoms and demonstrable enlargement of the prostate. n Average prostate size is 30 cc’s. Original studies showed benefit only in men with prostate sizes greater than 50 cc’s.
5 -Alpha Reductase Inhibitors n Finasteride (Proscar) and Dutasteride (Avodart) n Less effective for relief of BPH symptoms than alpha blockers n Adverse events include n Decreased libido n Worsened sexual function (erectile dysfunction) n decrease volume of ejaculation n Breast enlargement and tenderness n Reduces risk of urinary retention by 3%/year. n PSA must be doubled if screening for prostate cancer
Combination Therapy n Concomitant use of alpha blockers and 5 -alpha reductase inhibitors n Should be reserved for patients who are at significant risk of progression and adverse outcome n n n Poor surgical candidate Patient wants to avoid surgery Significant cost associated with dual medications
Medical Management n n Herbal therapy – saw palmetto fruit – use to improve urinary symptoms and urinary flow Problem with herbal therapy – long term effectiveness 11/24/2020 34

surgical treatment
Surgical Management n Office based therapies: n n Transurethral microwave therapy (TUMT) Transurethral needle ablation (TUNA) n Therapies are effective or partially effective for relieving the symptoms of BPH n Significant side effects/complications associated with these treatments have prompted a FDA warning
Surgical Management n OR based therapies n n n Open simple prostatectomy TURP Transurethral incision of the prostate Laser photoselective vaporization of the prostate (green light laser PVP) Laser Prostatectomy
Surgical Management n n n Patients may select surgical treatment as initial therapy if moderate or severe bother is present. Patients who have developed complications of BPH (i. e urinary retention, renal insufficiency, recurrent UTI) are best treated surgically. New surgical treatment have not demonstrated better outcomes than TURP to date.
BPH TREATMENT Surgical n n Indicated for AUA score >16 Transurethral Prostatectomy(TURP): 18% morbidity with. 2% mortality. 80 -90% improvement at 1 year but 60 -75% at 5 years and 5% require repeat TURP. Transurethral Incision of Prostate (TUIP): less morbidity with similar efficacy indicated for smaller prostates. Open Prostatectomy: indicated for glands > 60 grams or when additional procedure needed for suprapubic/retropubic approaches
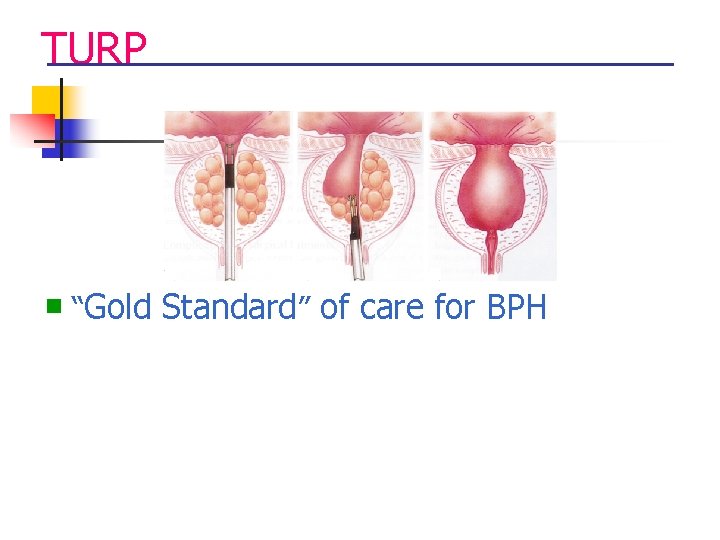
TURP n “Gold Standard” of care for BPH
the “gold standard”- TURP Disadvantages Benefits n Widely available n Effective n Long lasting n Greater risk of side effects and complications n 1 -4 days hospital stay n 1 -3 days catheter n 4 -6 week recovery
possible side effects of n TURP Greater than 5% risk of: n n n Irritative voiding symptoms Bladder neck contracture UTI Risk of incontinence 1% n. Decline in erectile function n 65% of retrograde ejaculation n. TUR syndrome (acute hyponatremia from free water absorption) n. Hemorrhage n. Bladder spasms n
Preoperative Goals n n n Restoration of urinary drainage Treatment of any urinary tract infection Understanding of procedure, implications for sexual functioning and urinary control 11/24/2020 43
Preoperative care n n n Antibiotics Allow pt to discuss concerns about surgery on sexual functioning Prostatic surgery may result in retrograde ejaculation 11/24/2020 44
Postoperative Goals n n No complications Restoration of urinary control Complete bladder emptying Satisfying sexual expression 11/24/2020 45
Postoperative Care n n Monitoring Continuous irrigation & maintain catheter patency Blood clots and hematuria are expected for the first 24 -36 hours After catheter is removed – check for urinary retention and urinary stream 11/24/2020 46
TURP n n n Sphincter tone may be poor after catheter is removed. Kegal exercise pelvic muscle floor technique is encouraged. Starting and stopping the urinary stream is helpful. Stool softeners to avoid straining Sitting and walking for long periods should be avoided 11/24/2020 47
Discharge planning n n n n Catheter care Managing urinary incontinence Oral fluid intake – 2, 000 -3, 000 cc per day Observe for s/s of urinary tract infection Prevent constipation Avoid lifting No driving or intercourse after surgery 11/24/2020 48
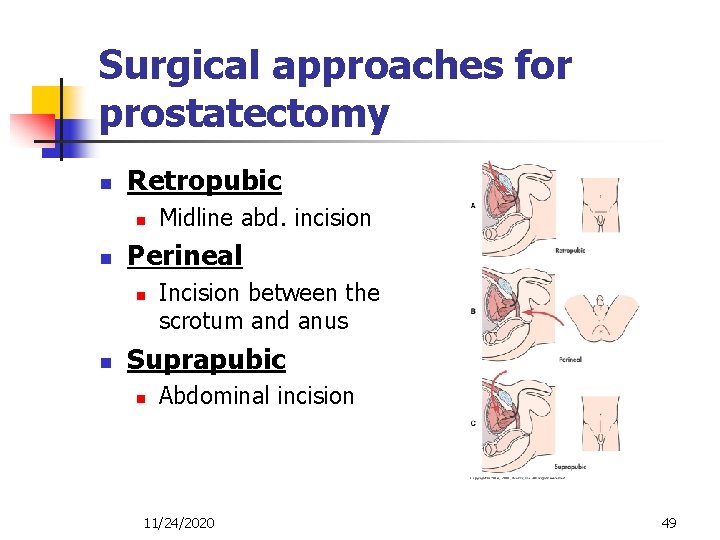
Surgical approaches for prostatectomy n Retropubic n n Perineal n n Midline abd. incision Incision between the scrotum and anus Suprapubic n Abdominal incision 11/24/2020 49
Prostatectomy n Complications: n n Bleeding Postoperative pain Risk for infection Erectile dysfunction 11/24/2020 50
BPH TREATMENT New Modalities n n n Minimally invasive: (Prostatic Stents, TUNA, TUMT, HIFU, Waterinduced Thermotherapy) Laser prostatectomy (VLAP, ILC, CLAP, TULIP, Ho. LRP) Electrovaporization (TUVP, TVRP)
heat therapies n Destroy prostate tissue with heat n Tissue is left in the body and is expelled over time (called sloughing) n Transurethral Microwave Therapy (TUMT) n Transurethral Needle Ablation (TUNA®) n Interstitial Laser Coagulation (ILC) n Water Induced Thermotherapy (WIT)
heat therapies n n n Benefits Office treatments Local anesthesia Minimally invasive n Reduced risk of complications as compared to invasive surgical “TURP” Disadvantages n n n Some symptoms will persist for up to 3 months Cannot predict who will respond May require prolonged catheterization
possible side effects of heat therapies n Urinary Tract Infection n Impotence n Incontinence
Laser Photoselective Vaporization of the Prostate (Laser PVP) n n n TURP-equivalent 7 year improvement in symptom score and urination parameters Decreased risk of bleeding and TUR syndrome, otherwise similar adverse effect profile May be done on anti-coagulated patients
- Slides: 55