Early and definitive treatment of pilon fractures AO





- Slides: 39
Early and definitive treatment of pilon fractures AO Trauma Advanced Principles Course
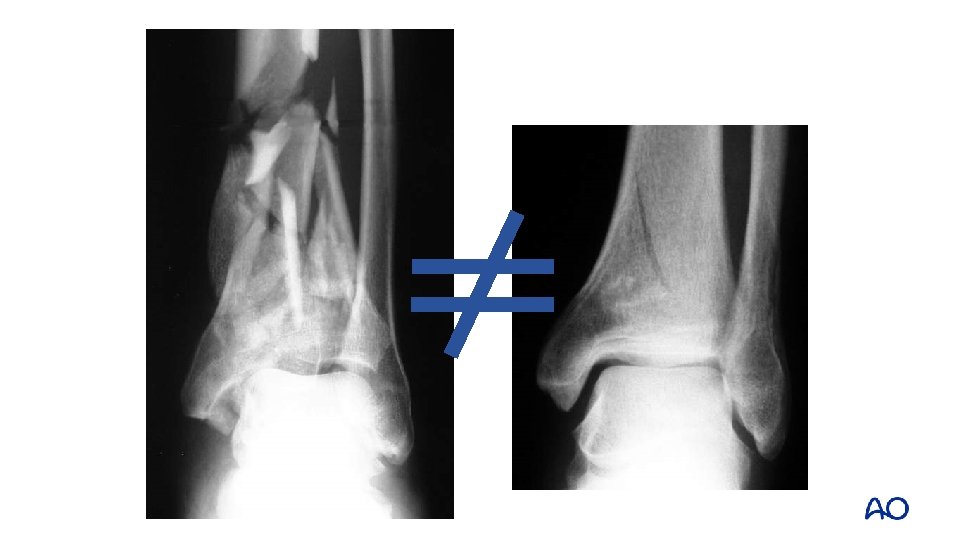
Learning objectives • Formulate a preoperative plan including rationale for imaging, choice of approach, and surgical tactics • Compare the pros/cons of conventional and locked plating and external fixator and describe reduction techniques and tools • Evaluate the role of bone graft substitutes for periarticular defects • Identify common complications • Explore key outcome publications
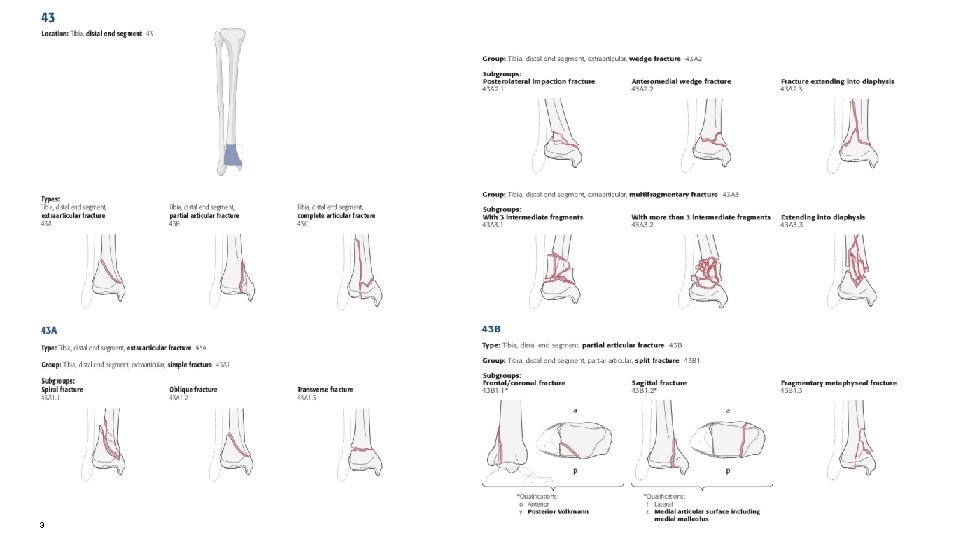
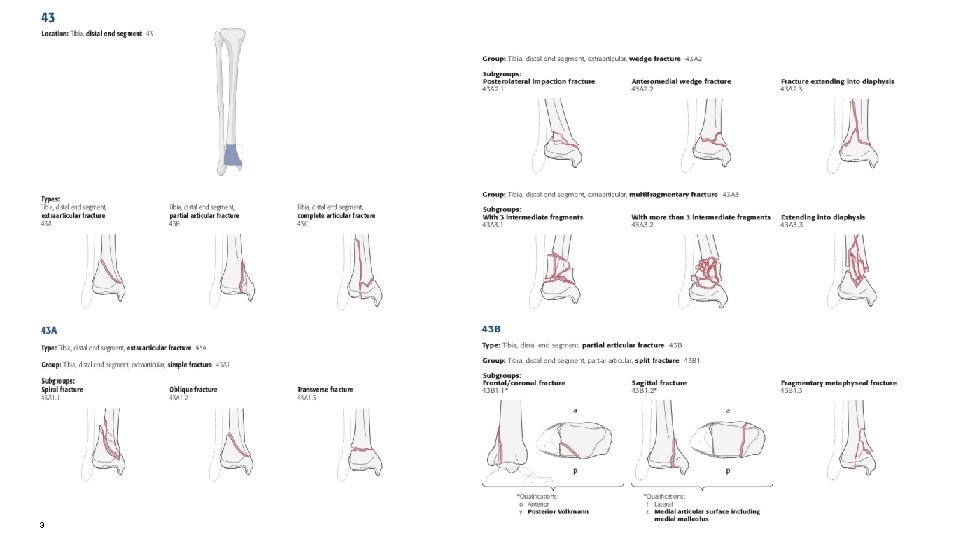
3
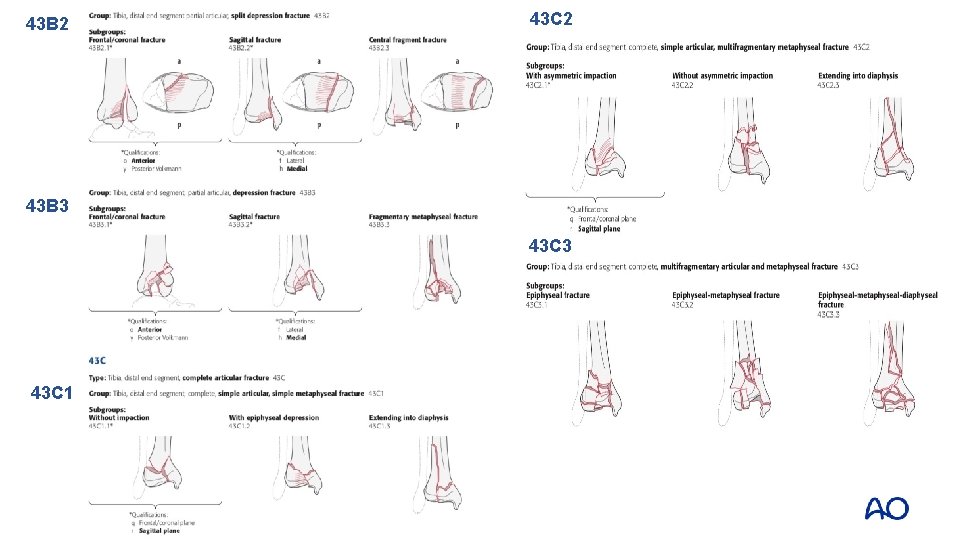
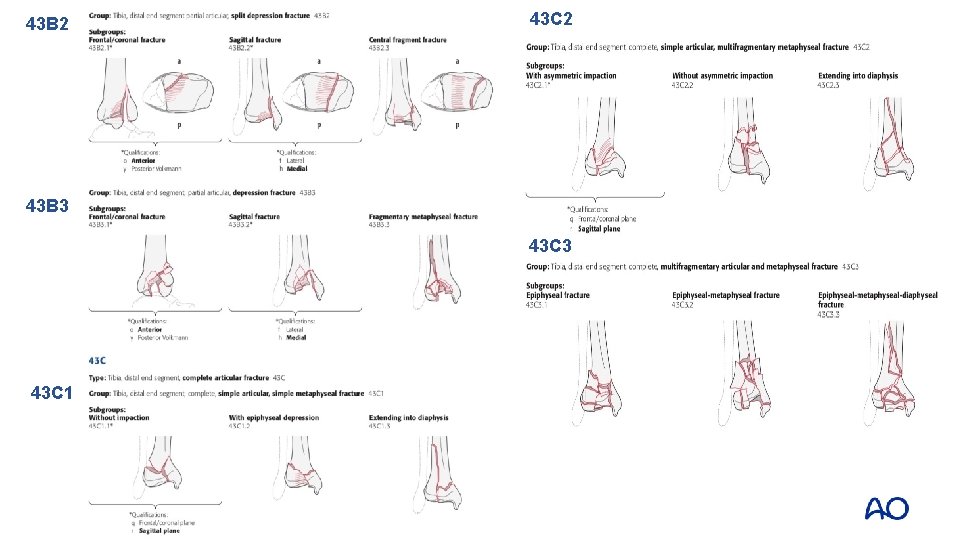
43 B 2 43 C 2 43 B 3 43 C 1
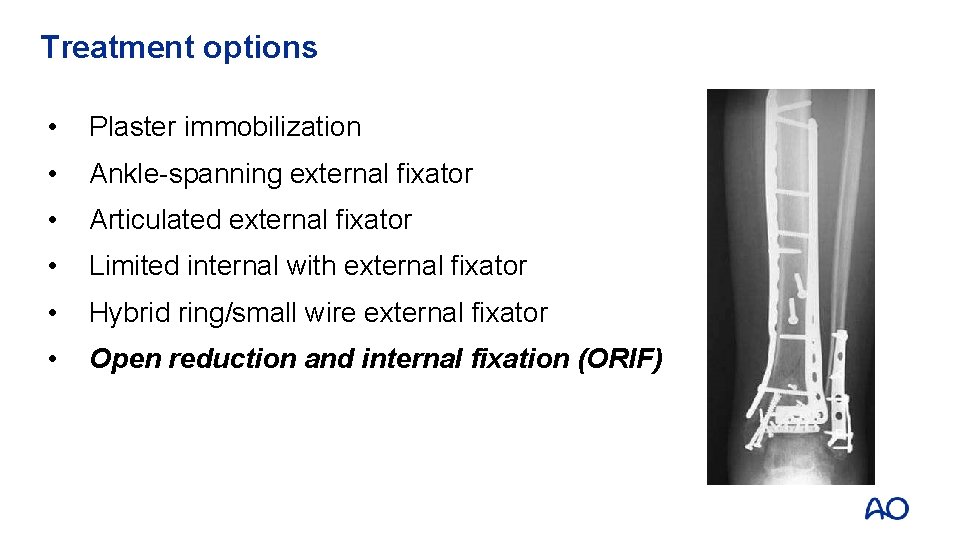
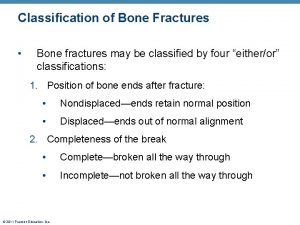
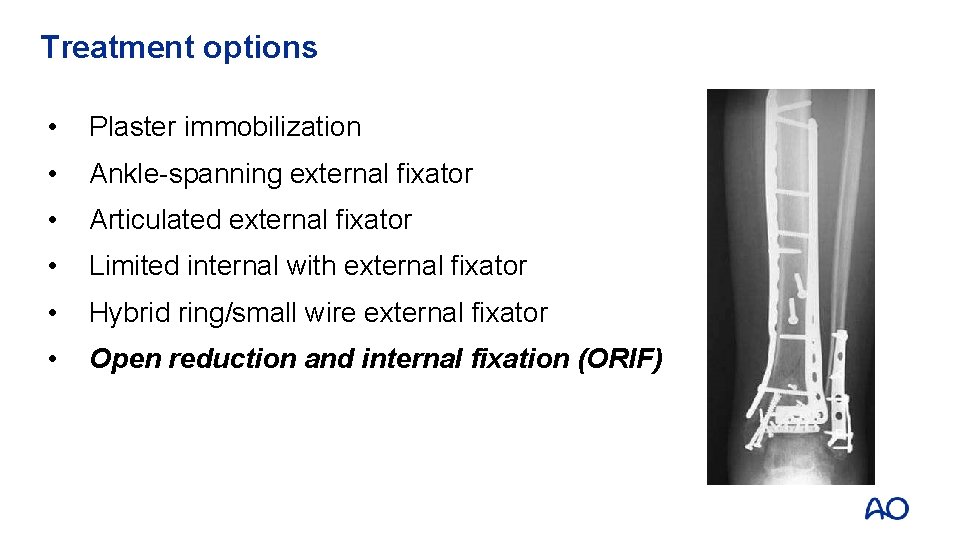
Treatment options • Plaster immobilization • Ankle-spanning external fixator • Articulated external fixator • Limited internal with external fixator • Hybrid ring/small wire external fixator • Open reduction and internal fixation (ORIF)
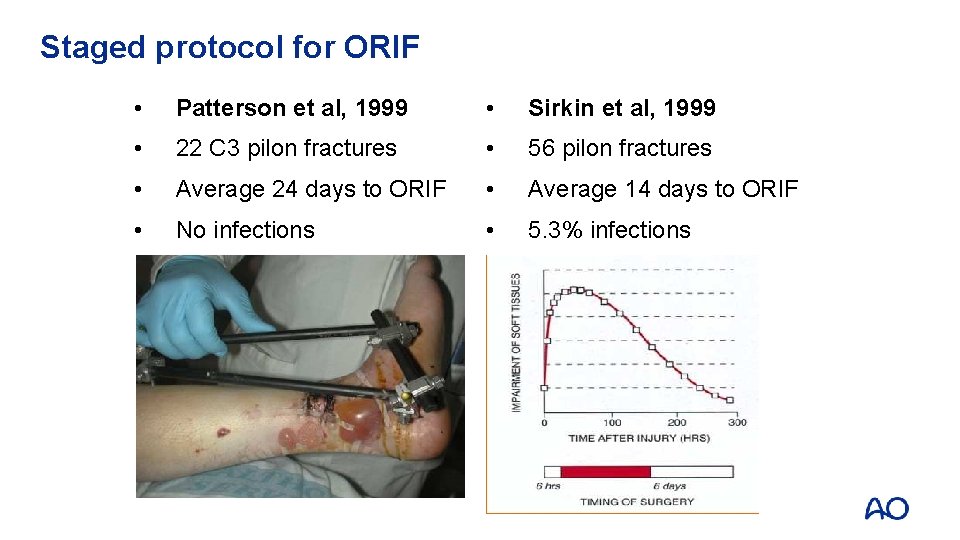
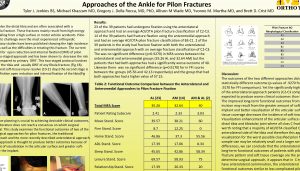
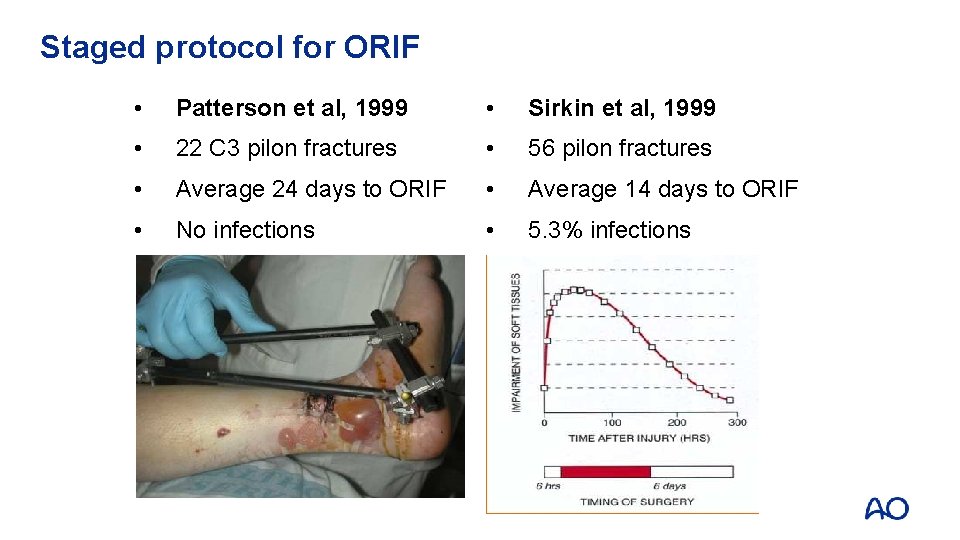
Staged protocol for ORIF • Patterson et al, 1999 • Sirkin et al, 1999 • 22 C 3 pilon fractures • 56 pilon fractures • Average 24 days to ORIF • Average 14 days to ORIF • No infections • 5. 3% infections

Timing is… Everything!
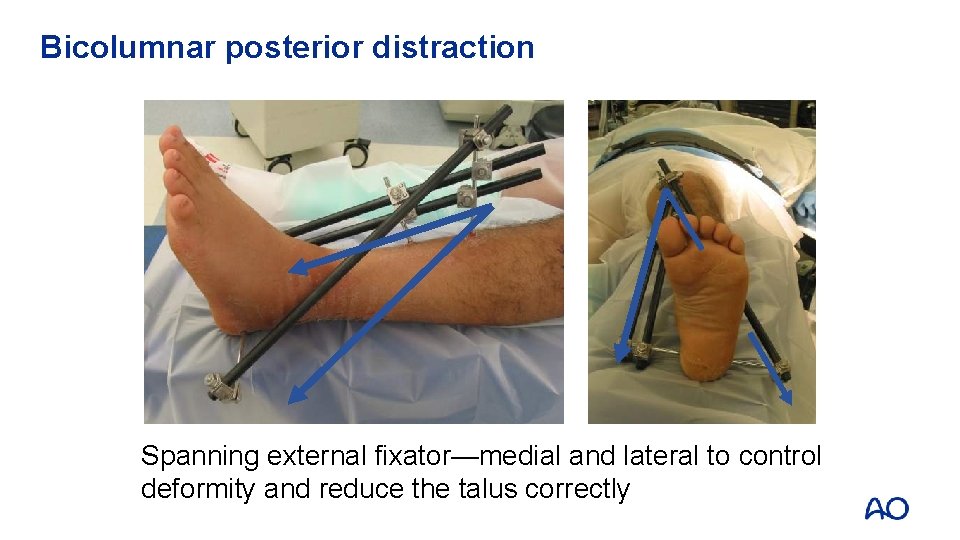
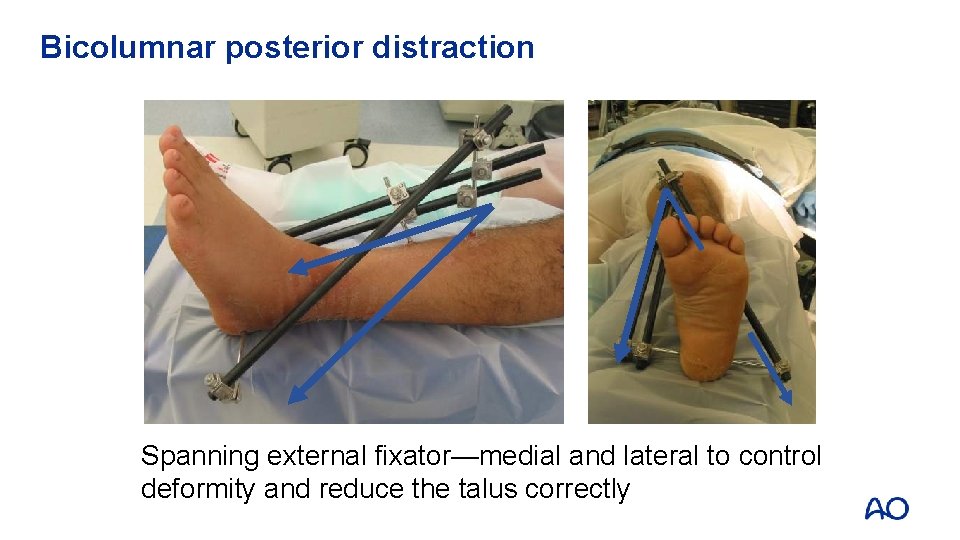
Bicolumnar posterior distraction Spanning external fixator—medial and lateral to control deformity and reduce the talus correctly
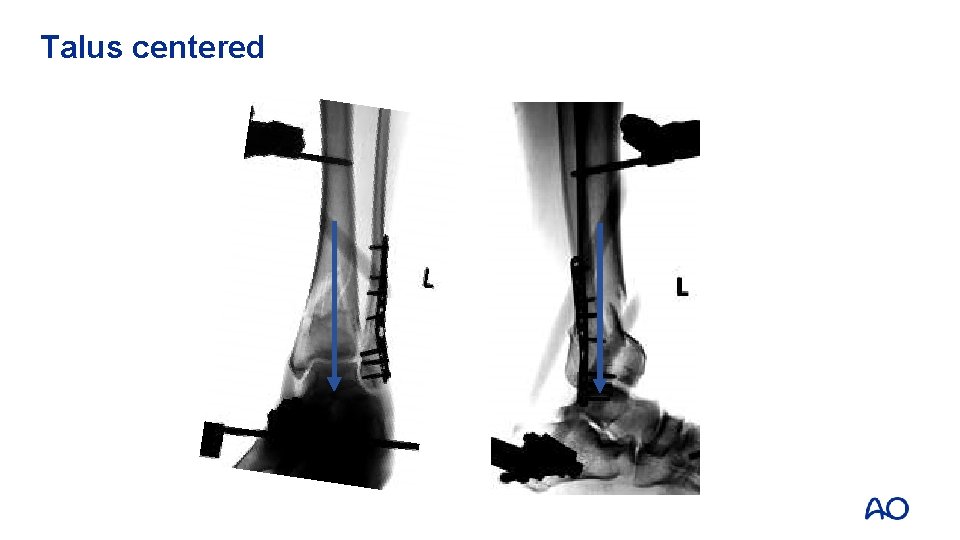
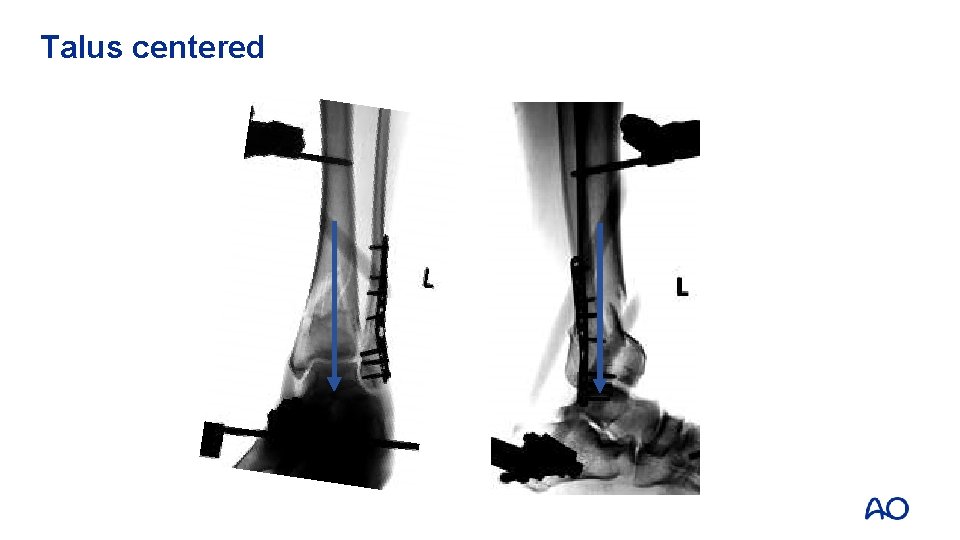
Talus centered

Tension Compression Intact Beware
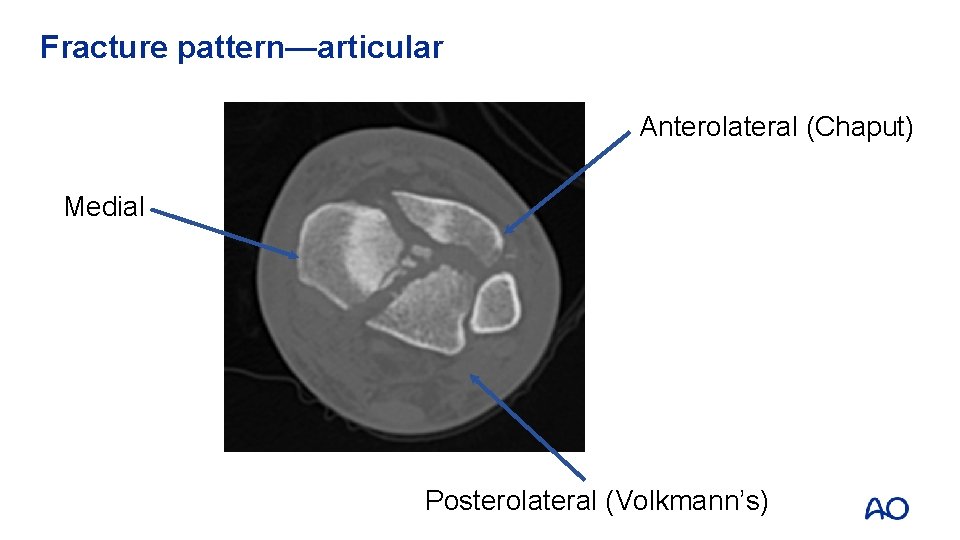
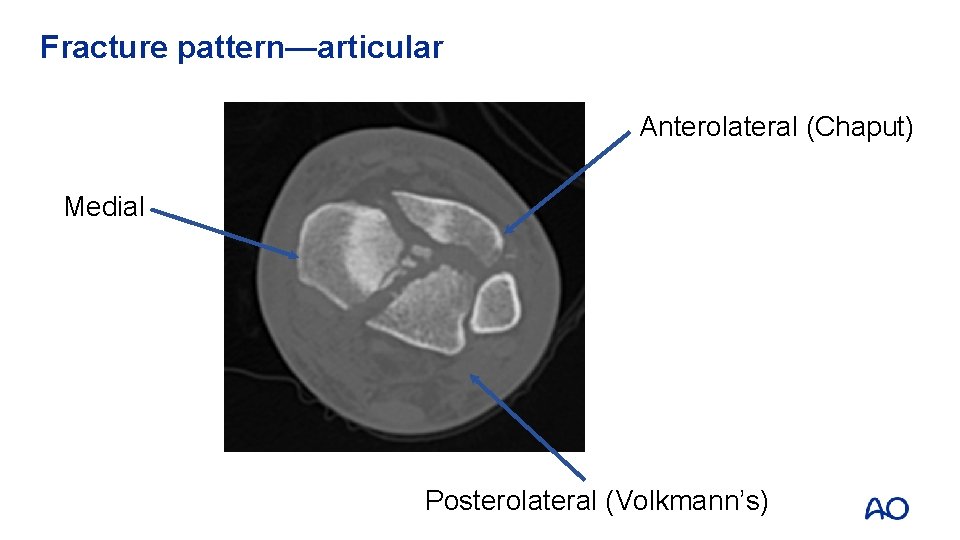
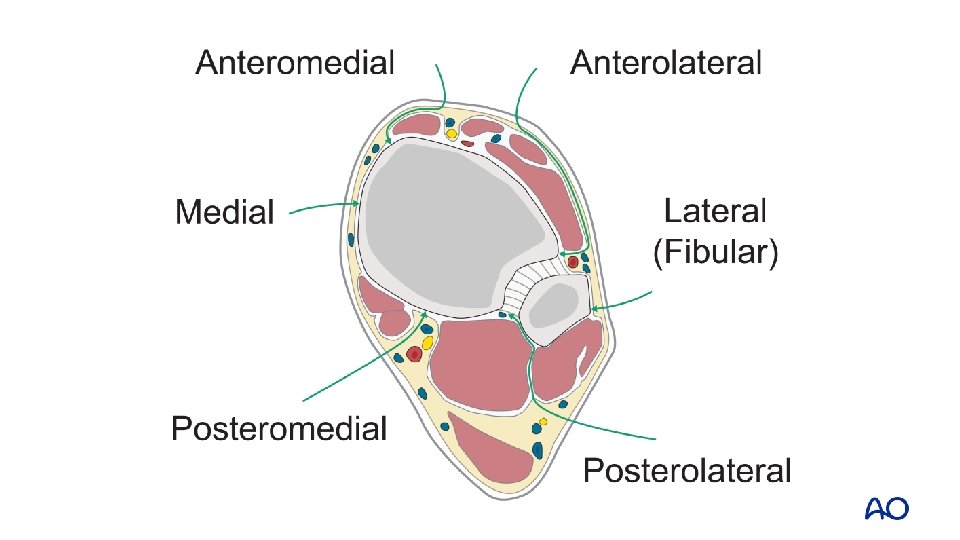
Fracture pattern—articular Anterolateral (Chaput) Medial Posterolateral (Volkmann’s)
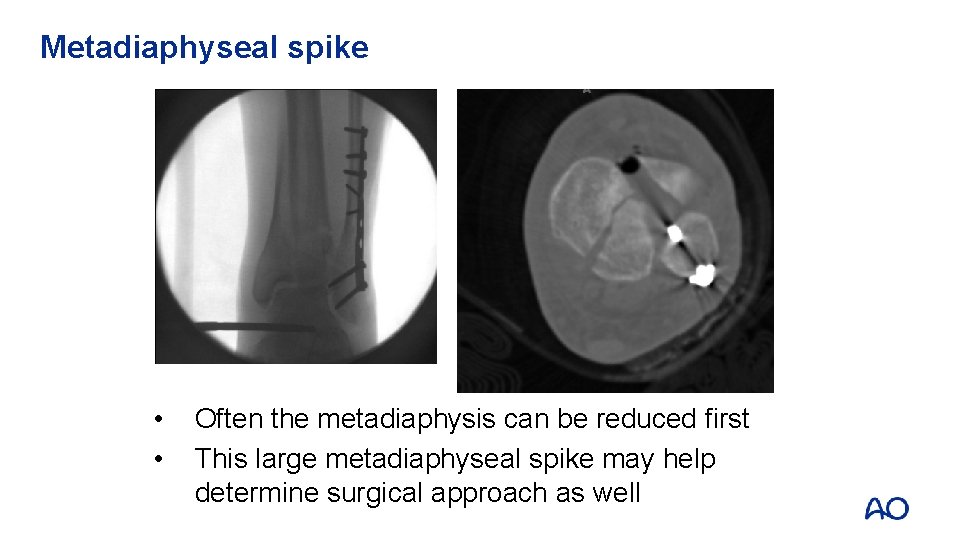
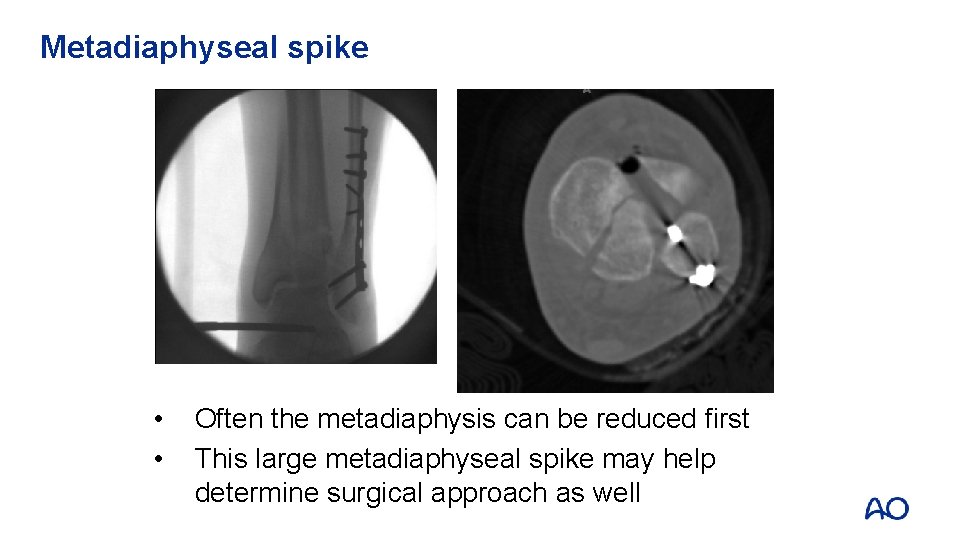
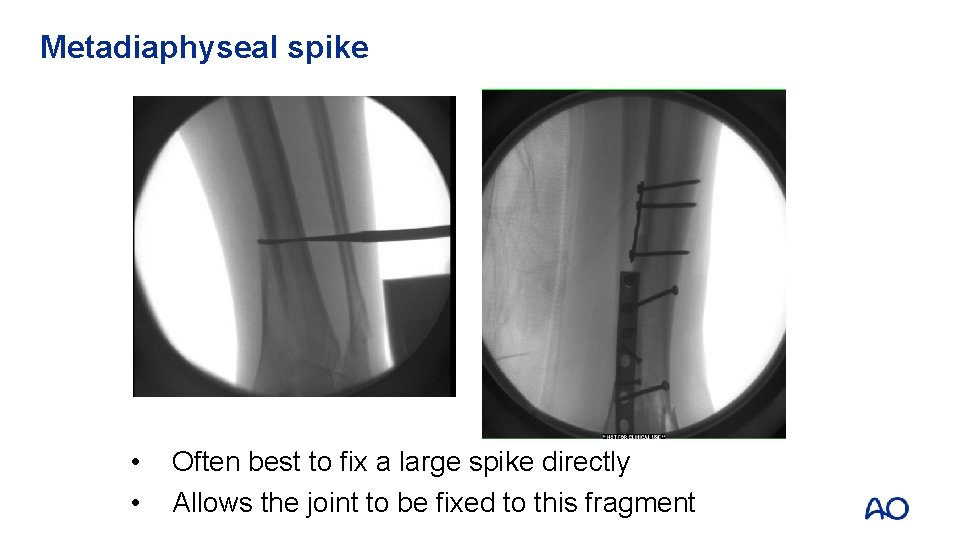
Metadiaphyseal spike • • Often the metadiaphysis can be reduced first This large metadiaphyseal spike may help determine surgical approach as well
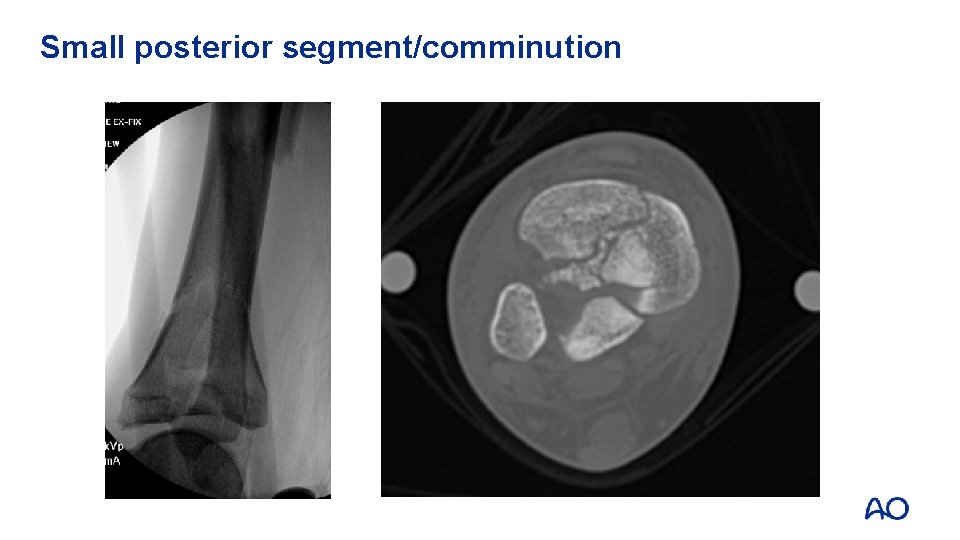
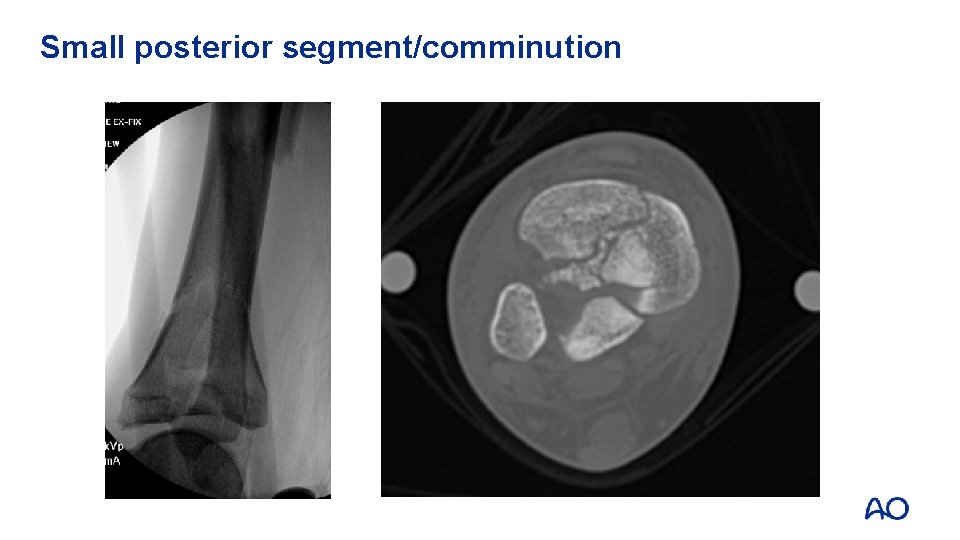
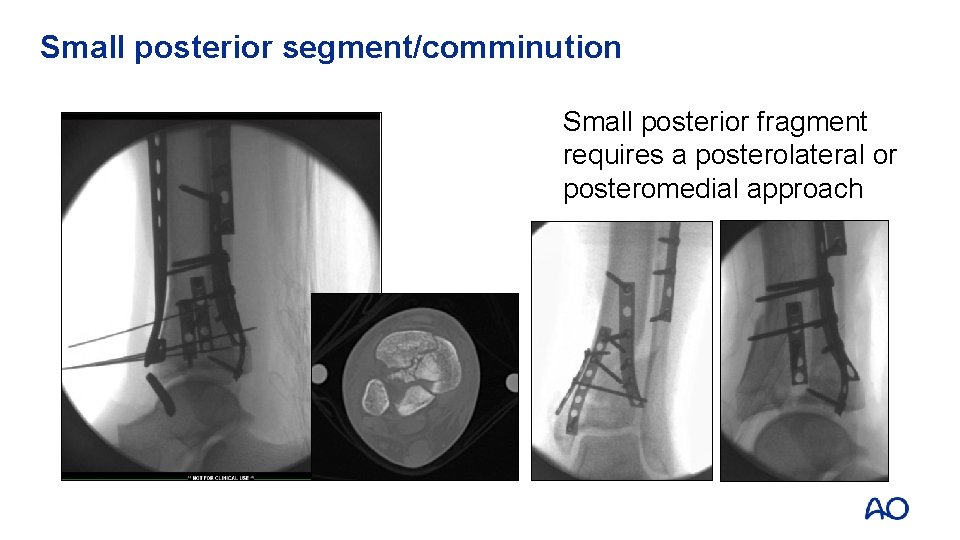
Small posterior segment/comminution
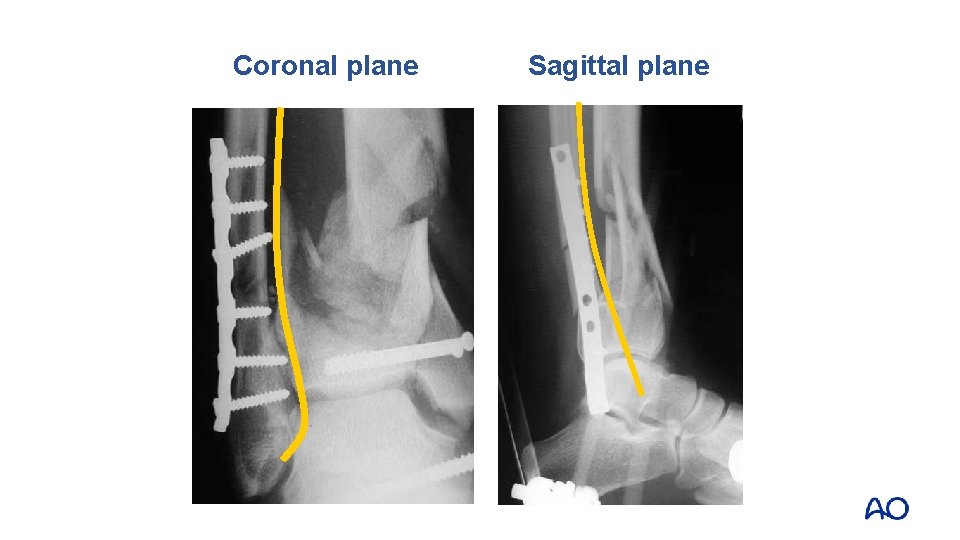
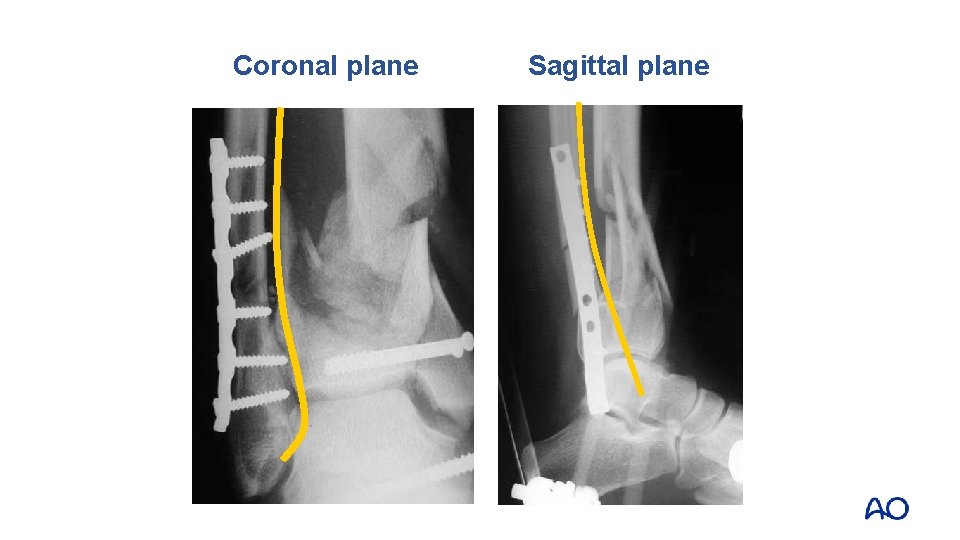
Coronal plane Sagittal plane
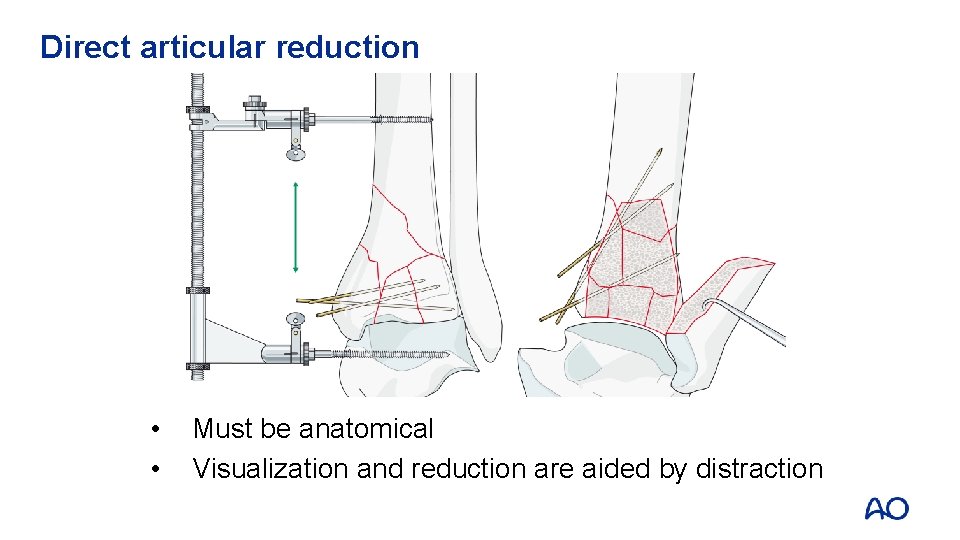
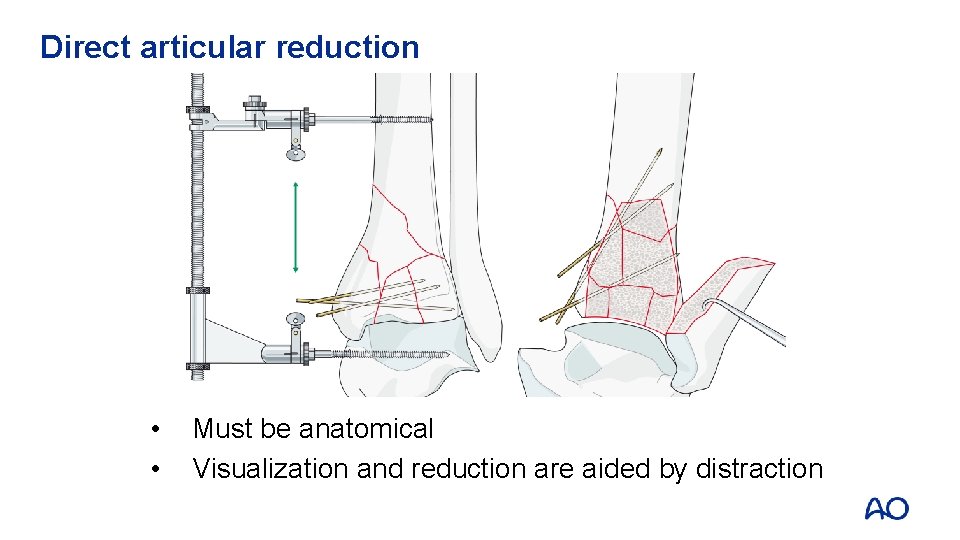
Direct articular reduction • • Must be anatomical Visualization and reduction are aided by distraction
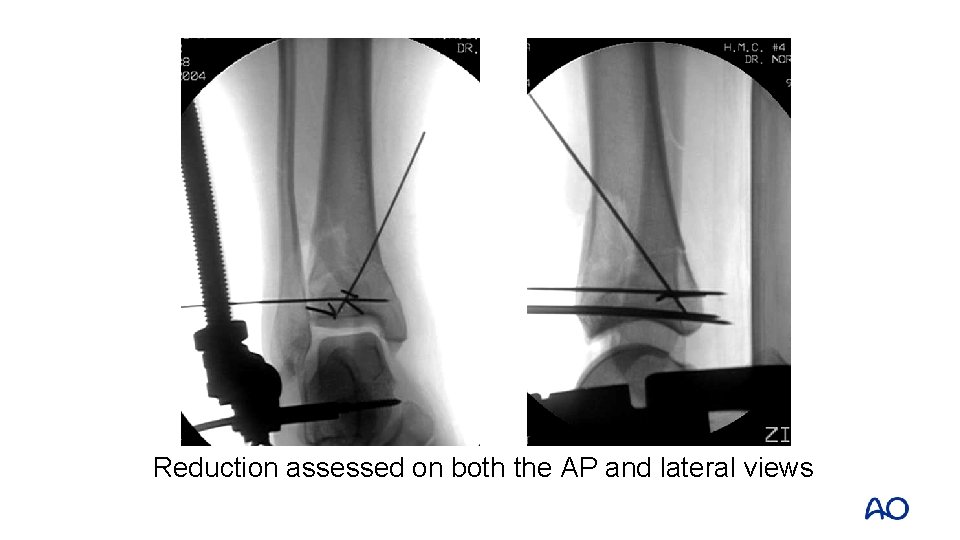
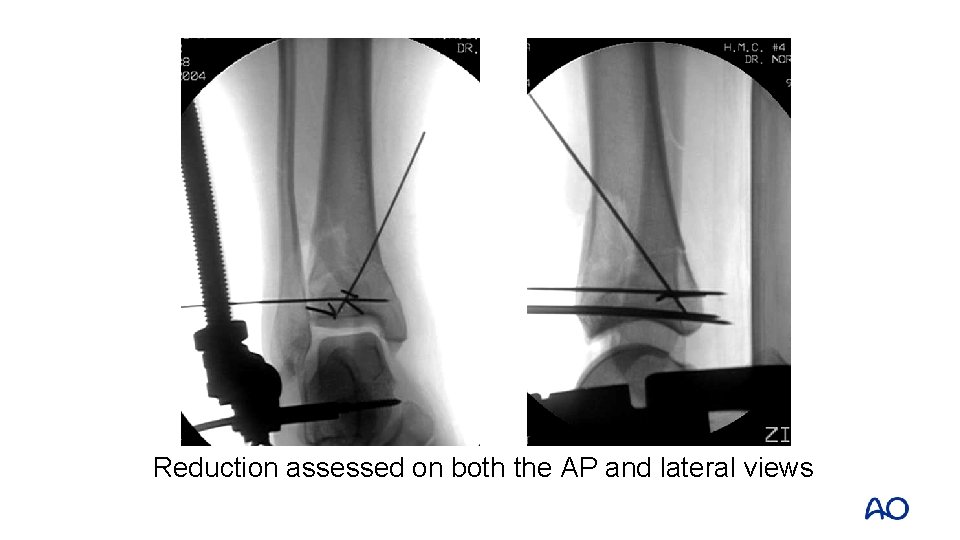
Reduction assessed on both the AP and lateral views
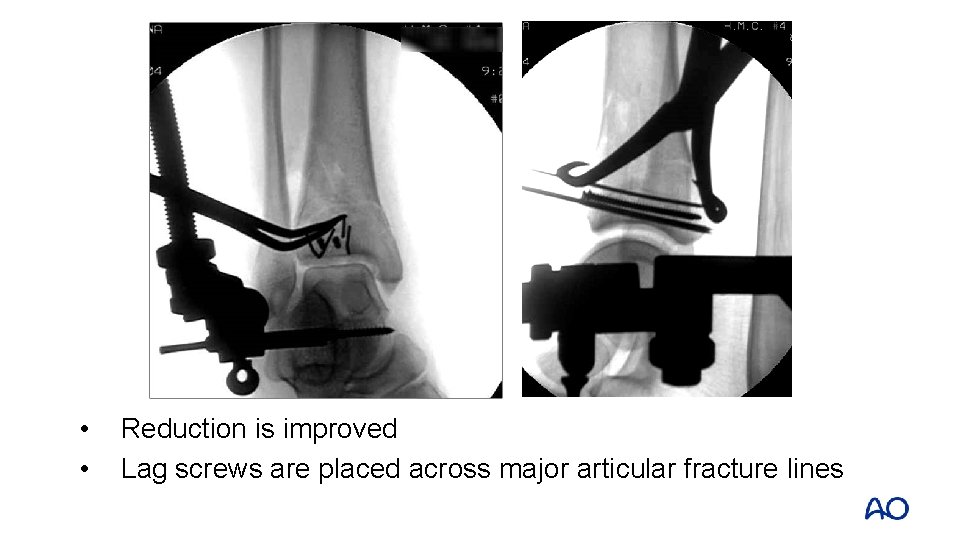
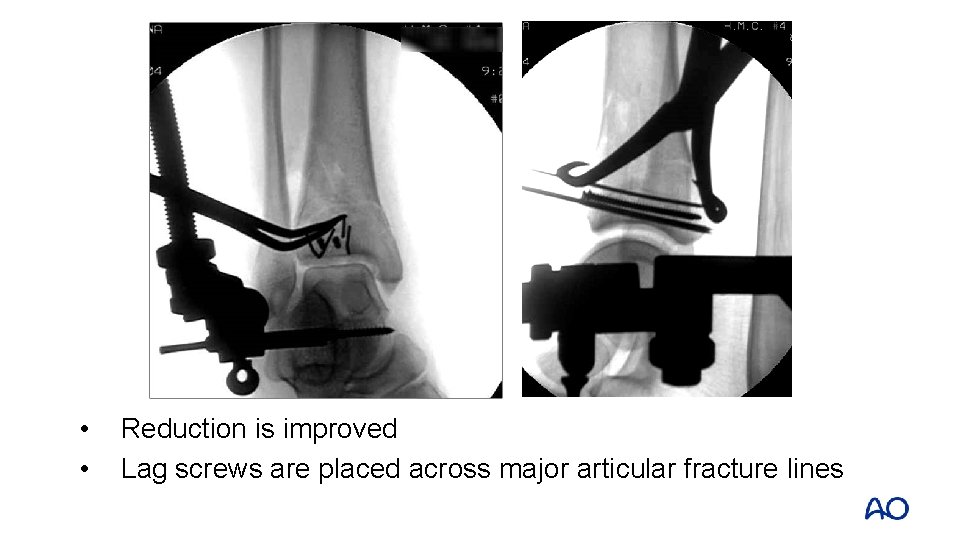
• • Reduction is improved Lag screws are placed across major articular fracture lines
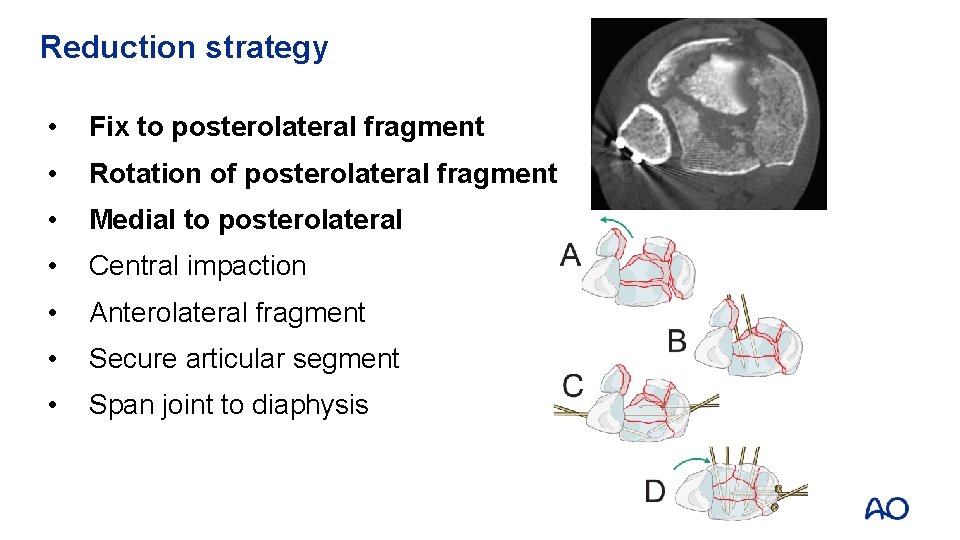
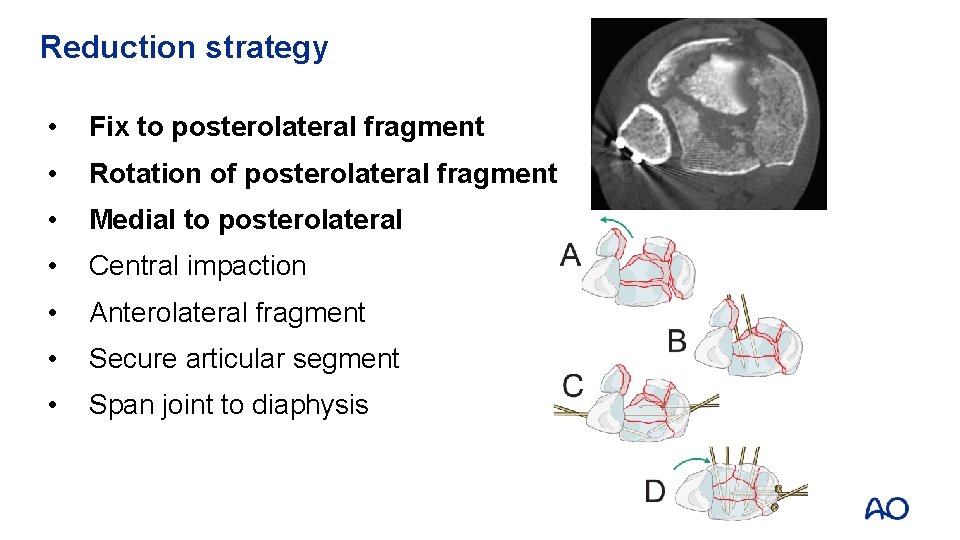
Reduction strategy • Fix to posterolateral fragment • Rotation of posterolateral fragment • Medial to posterolateral • Central impaction • Anterolateral fragment • Secure articular segment • Span joint to diaphysis
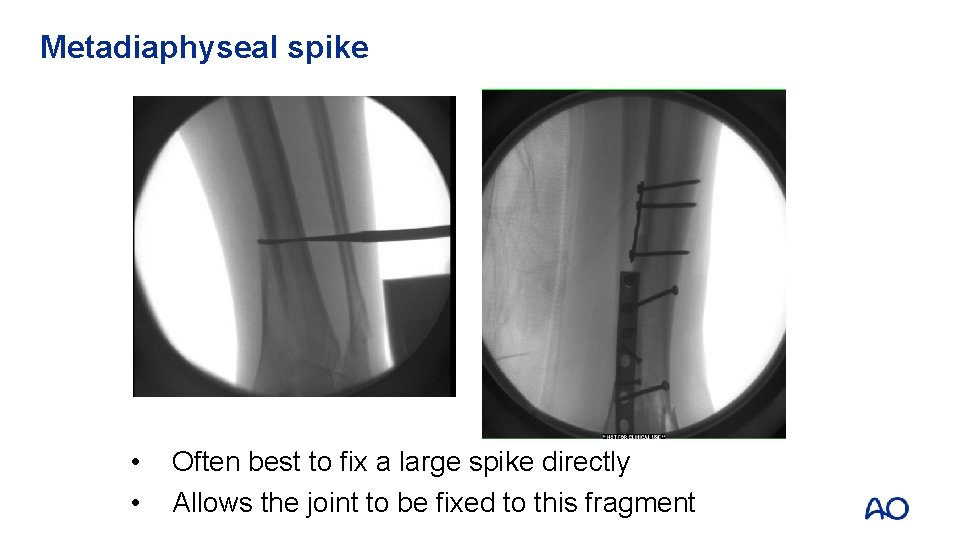
Metadiaphyseal spike • • Often best to fix a large spike directly Allows the joint to be fixed to this fragment
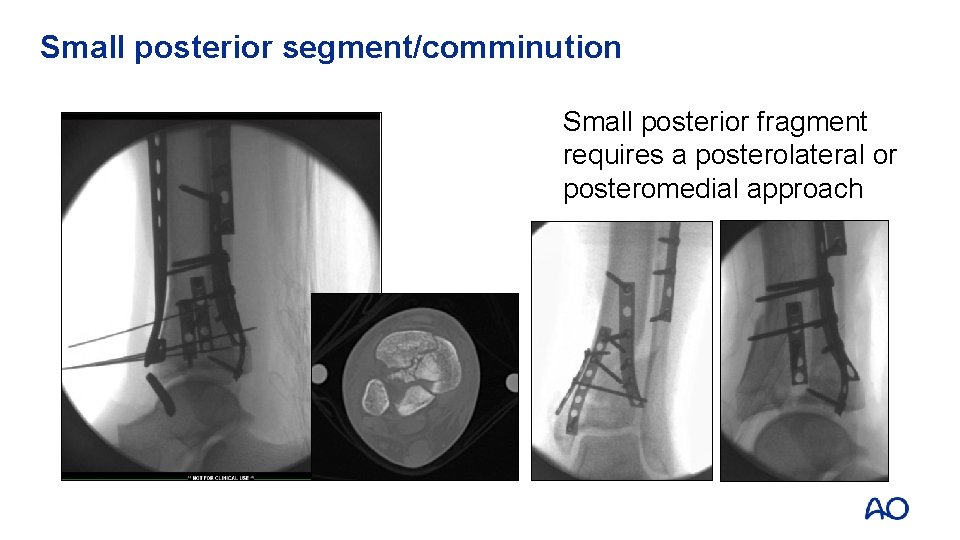
Small posterior segment/comminution Small posterior fragment requires a posterolateral or posteromedial approach

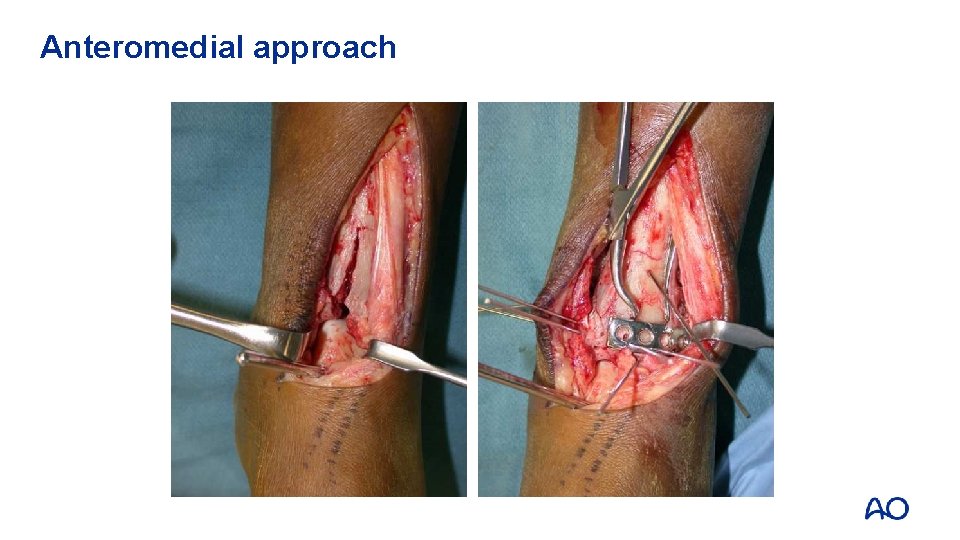
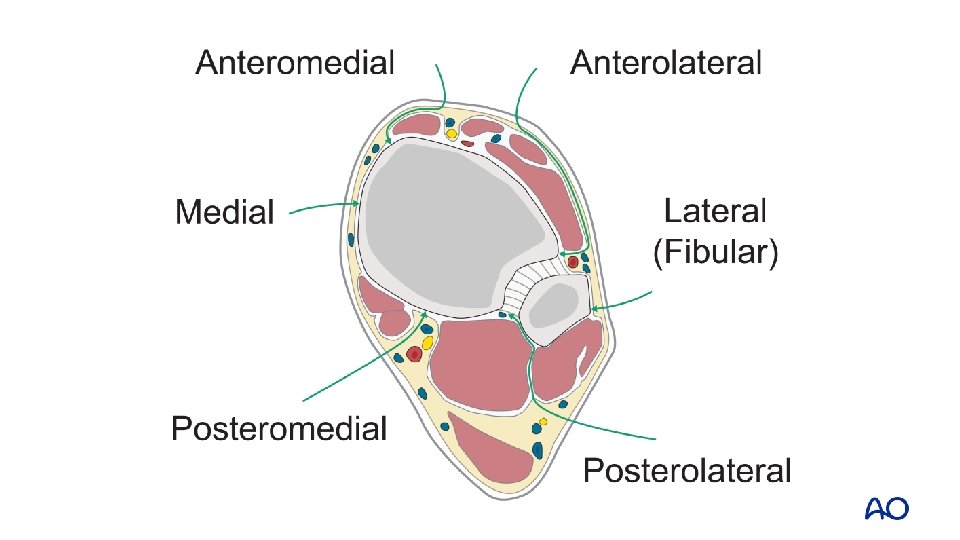
Anteromedial approach • Lateral to tibial crest • Medial to tibialis anterior • Preserve paratenon • Curve at ankle
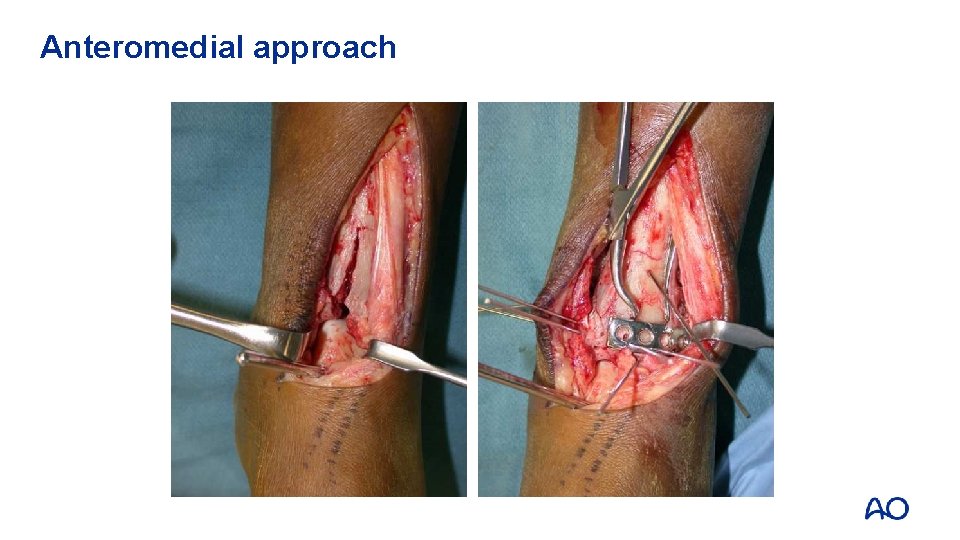
Anteromedial approach
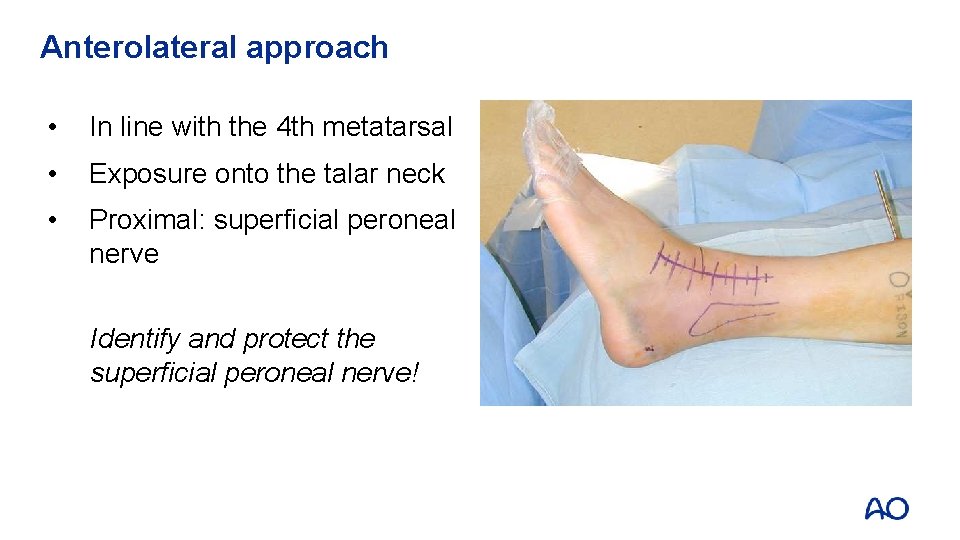
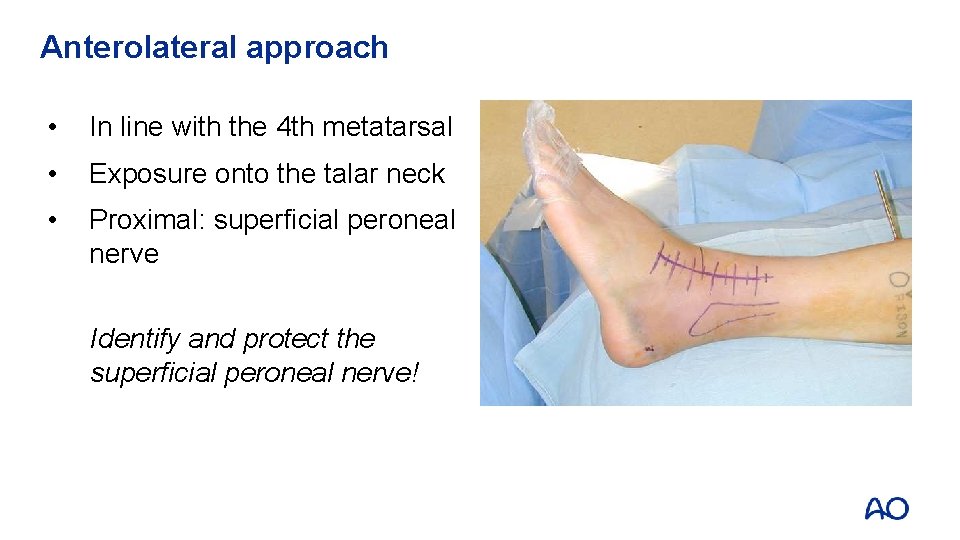
Anterolateral approach • In line with the 4 th metatarsal • Exposure onto the talar neck • Proximal: superficial peroneal nerve Identify and protect the superficial peroneal nerve!
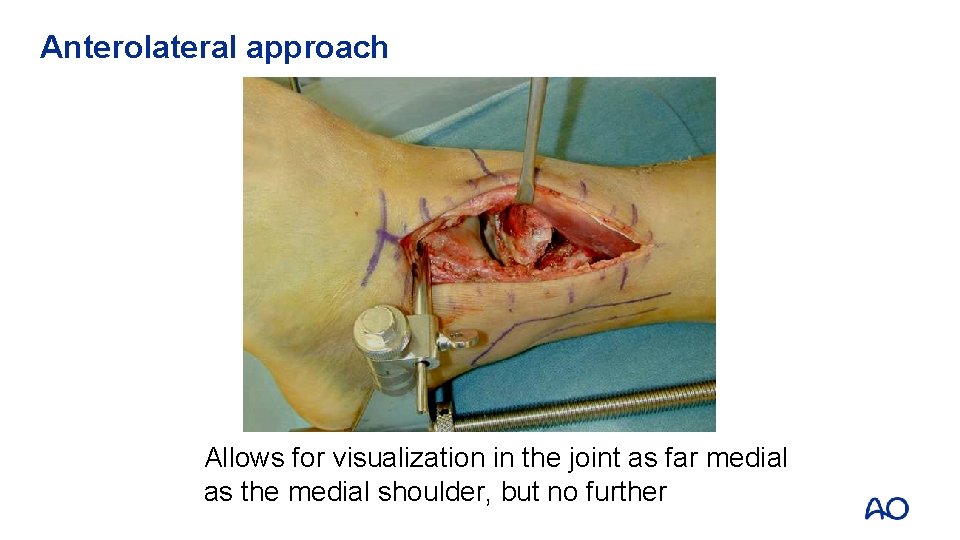
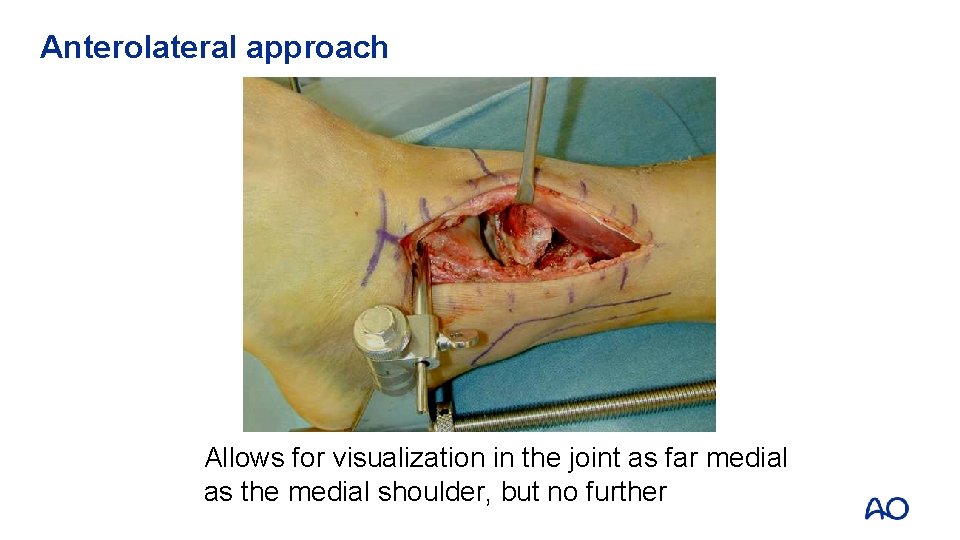
Anterolateral approach Allows for visualization in the joint as far medial as the medial shoulder, but no further
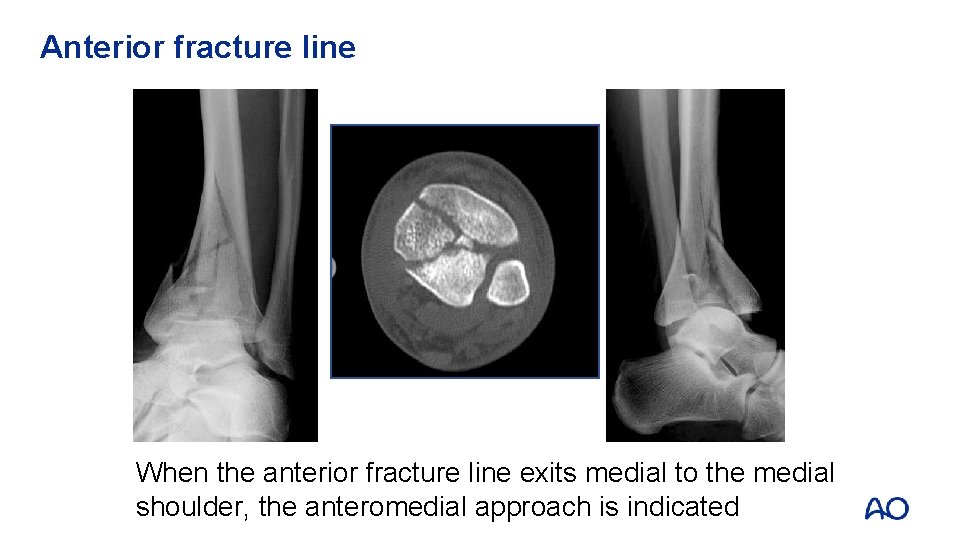
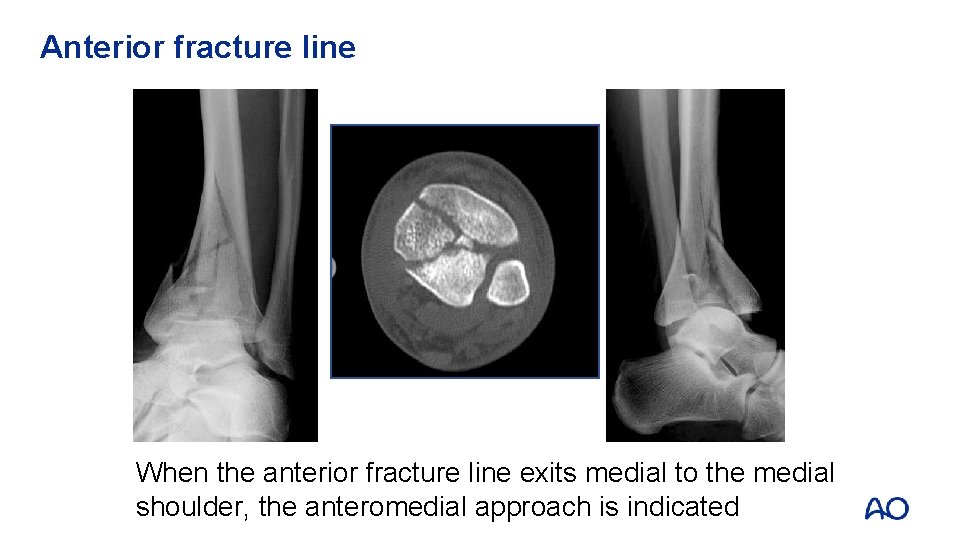
Anterior fracture line When the anterior fracture line exits medial to the medial shoulder, the anteromedial approach is indicated
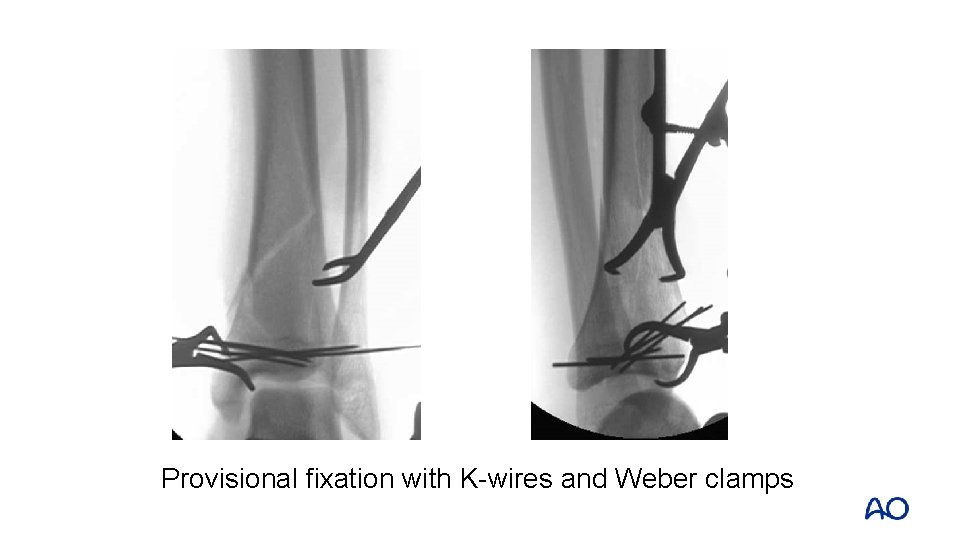
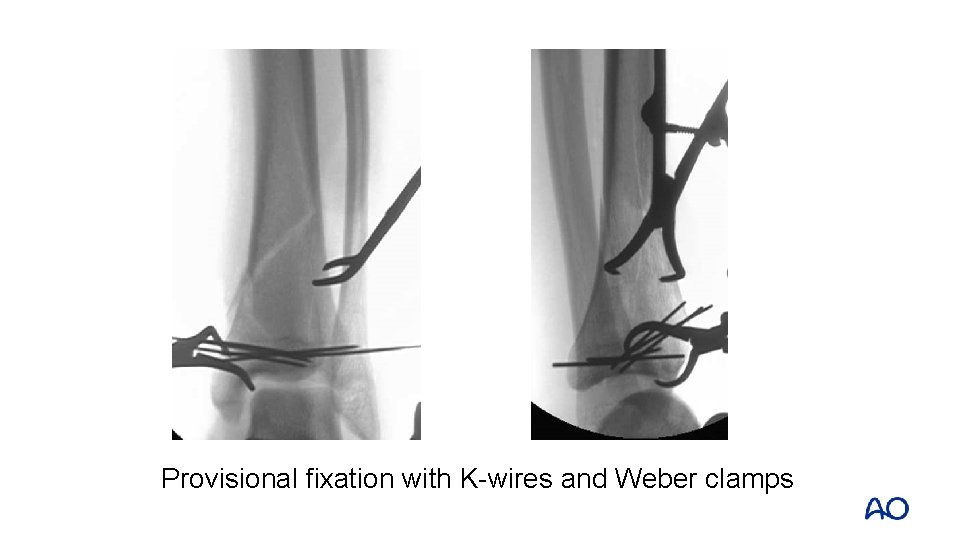
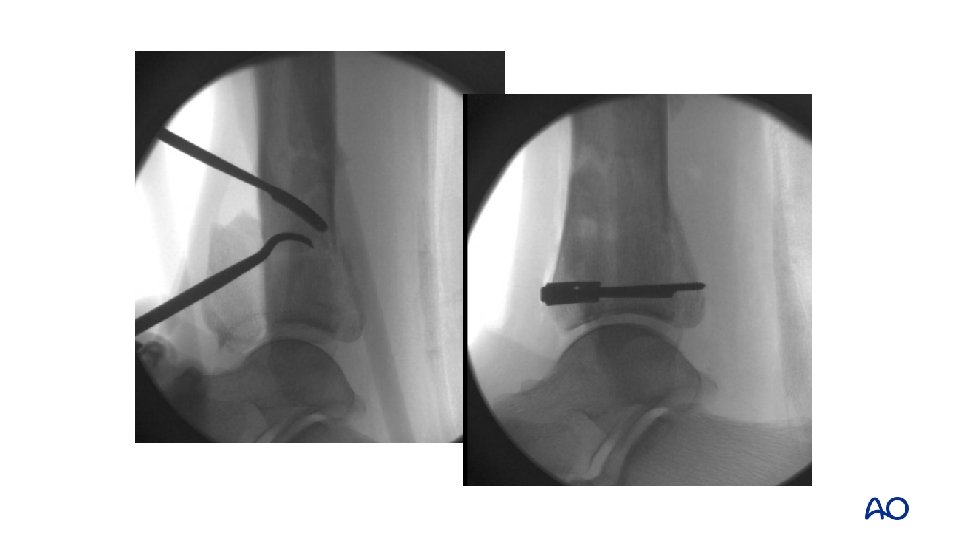
Provisional fixation with K-wires and Weber clamps
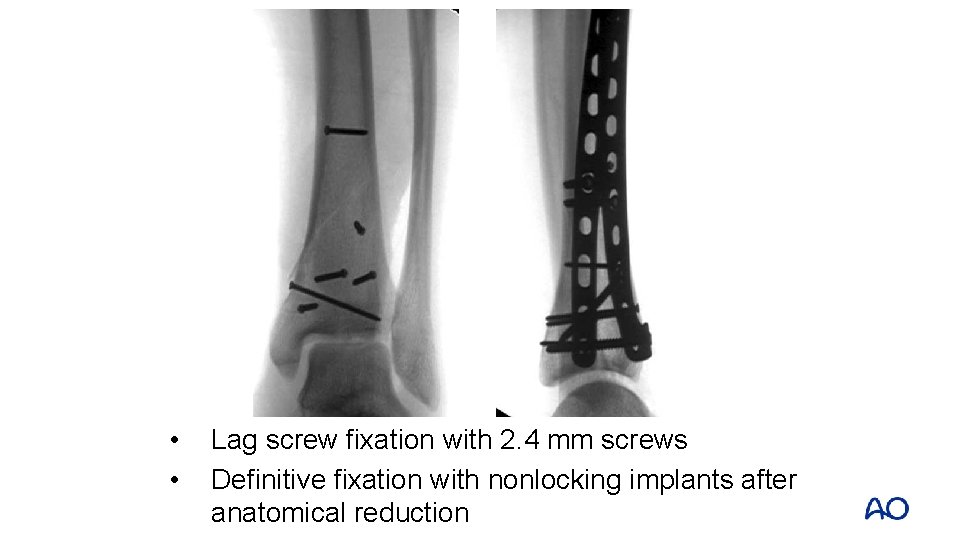
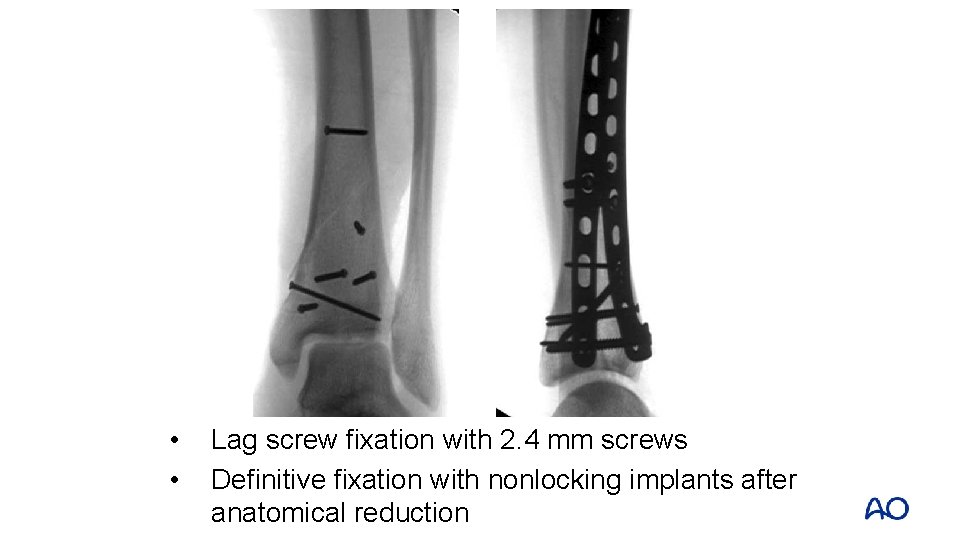
• • Lag screw fixation with 2. 4 mm screws Definitive fixation with nonlocking implants after anatomical reduction
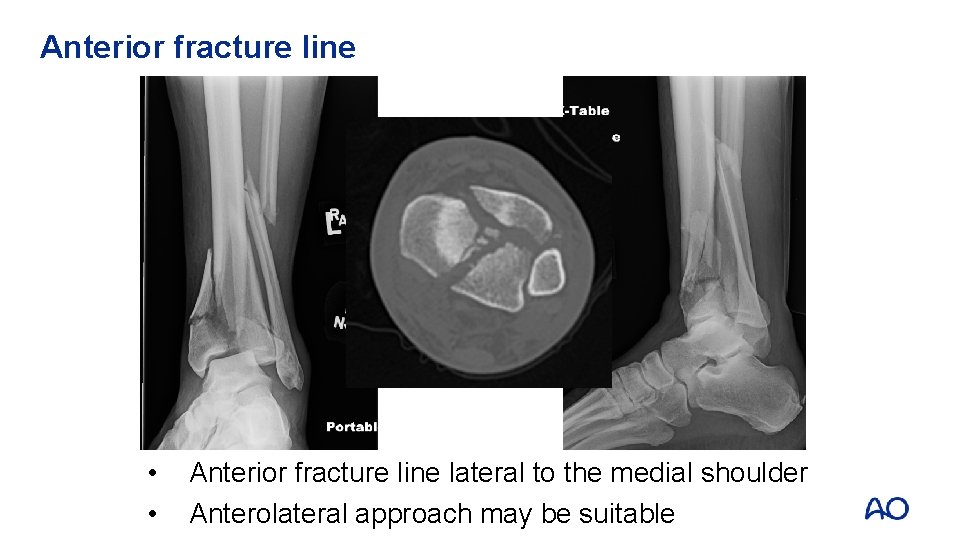
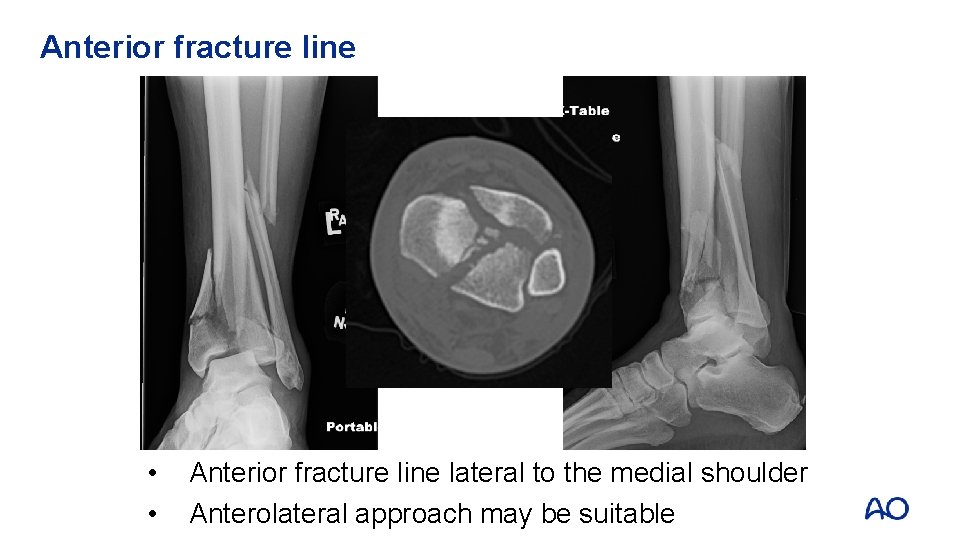
Anterior fracture line • • Anterior fracture line lateral to the medial shoulder Anterolateral approach may be suitable
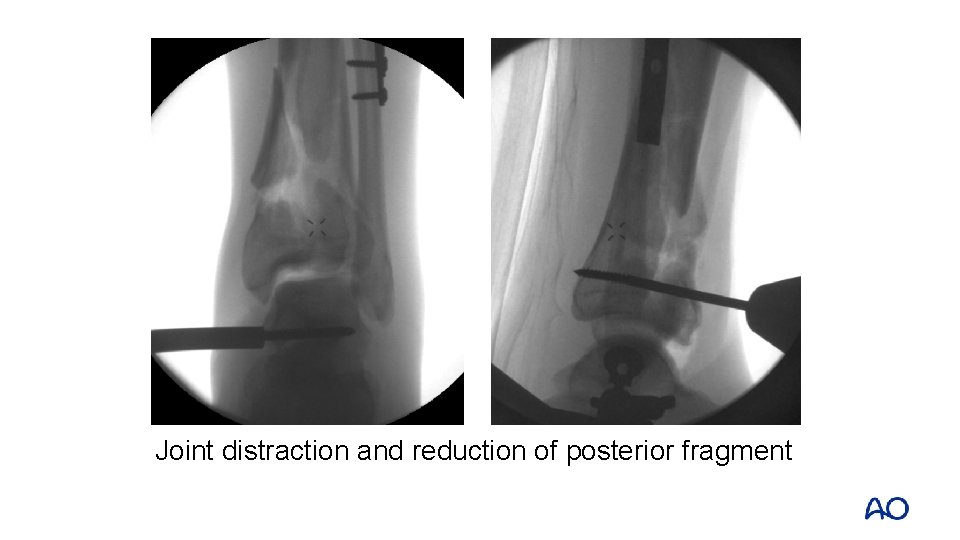
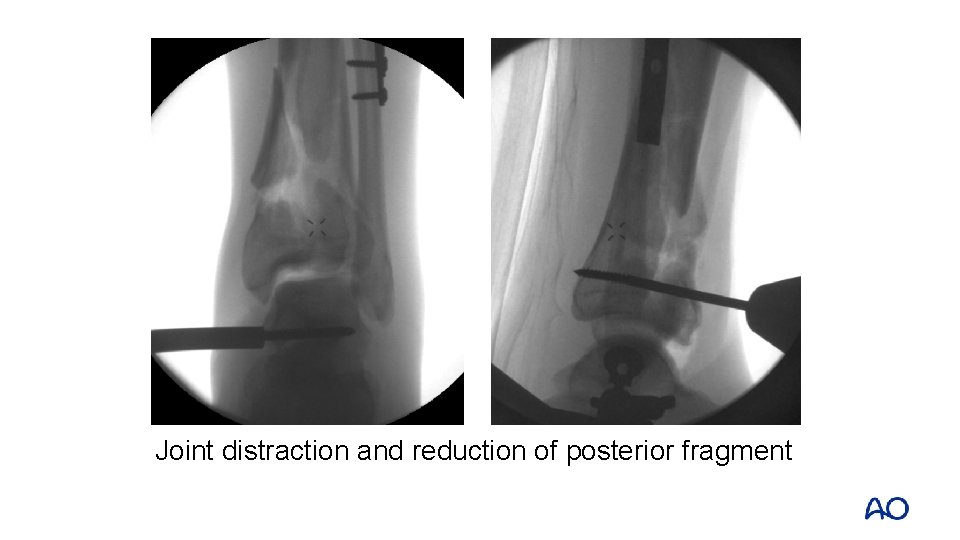
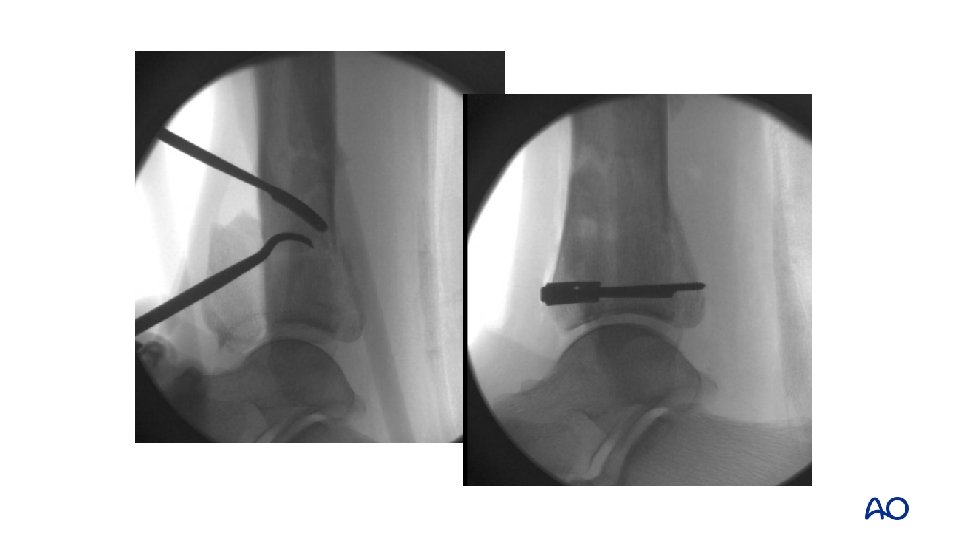
Joint distraction and reduction of posterior fragment
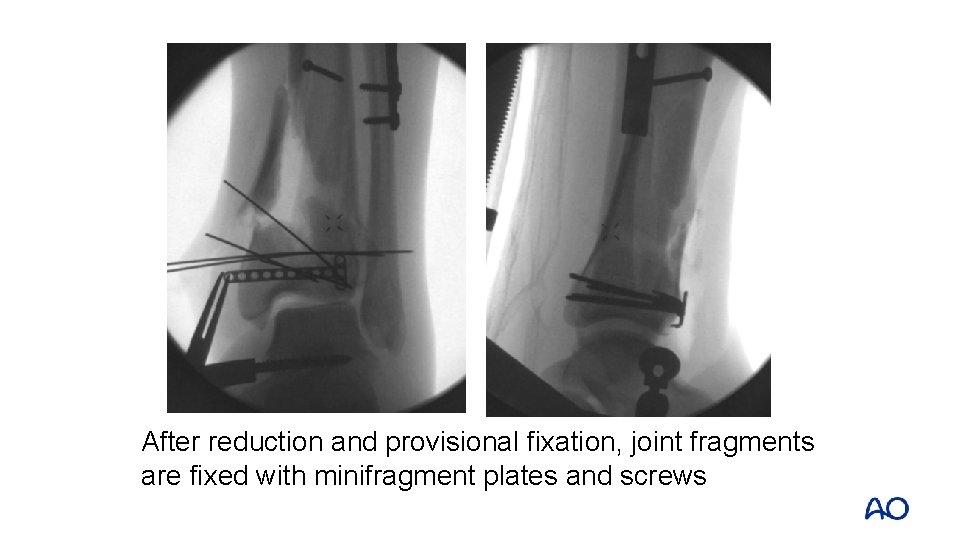
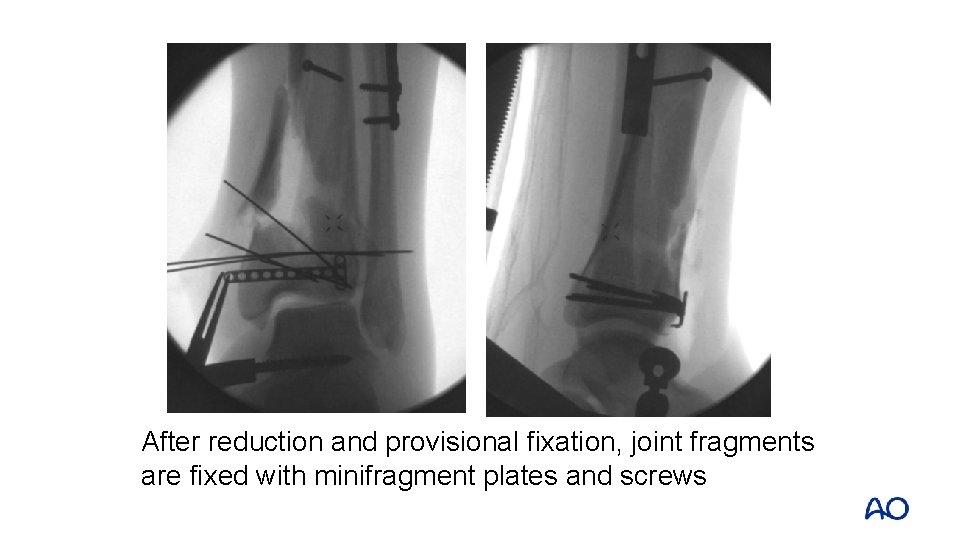
After reduction and provisional fixation, joint fragments are fixed with minifragment plates and screws

Soft-tissue limitation
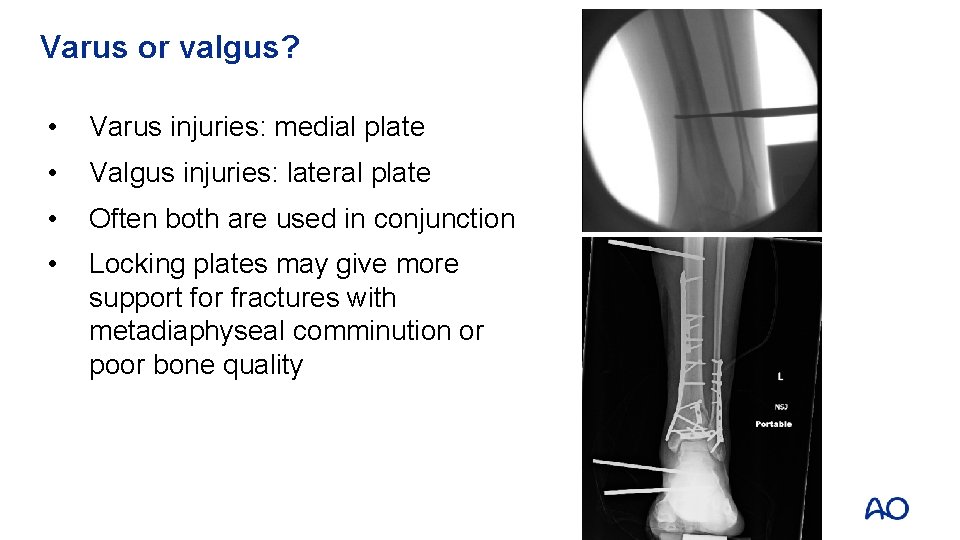
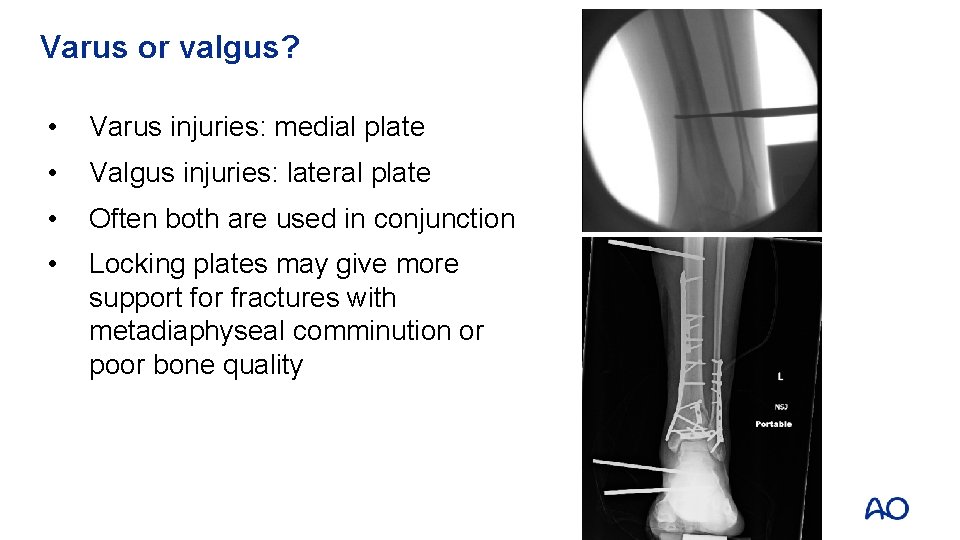
Varus or valgus? • Varus injuries: medial plate • Valgus injuries: lateral plate • Often both are used in conjunction • Locking plates may give more support for fractures with metadiaphyseal comminution or poor bone quality
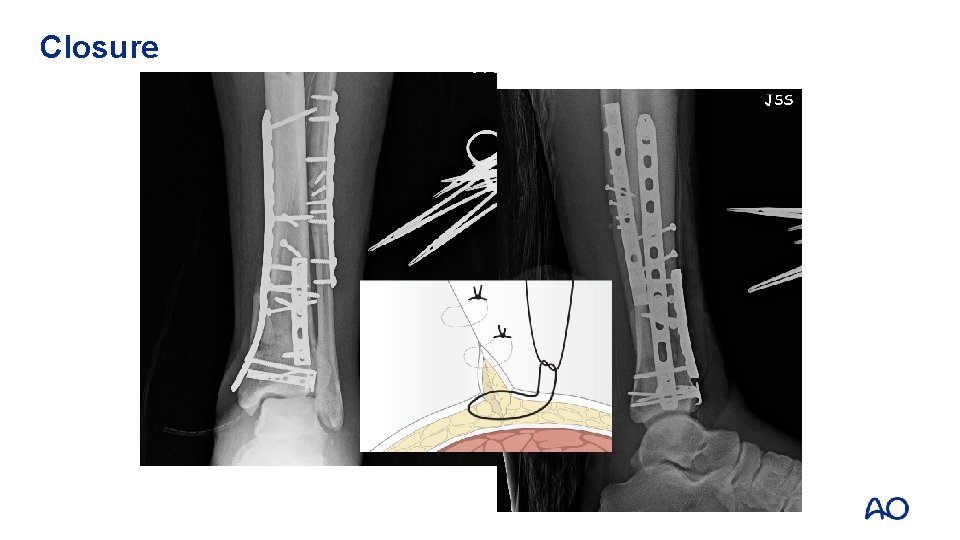
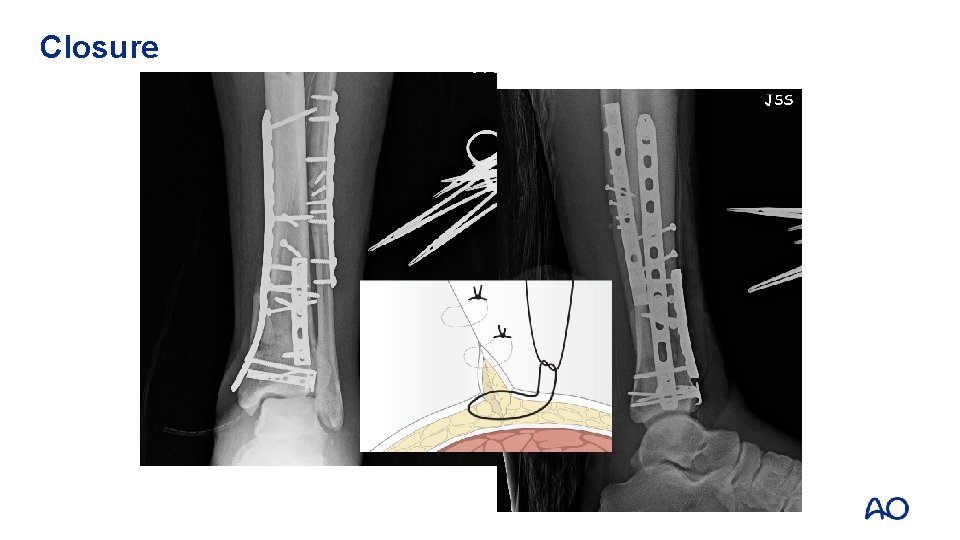
Closure

Closure
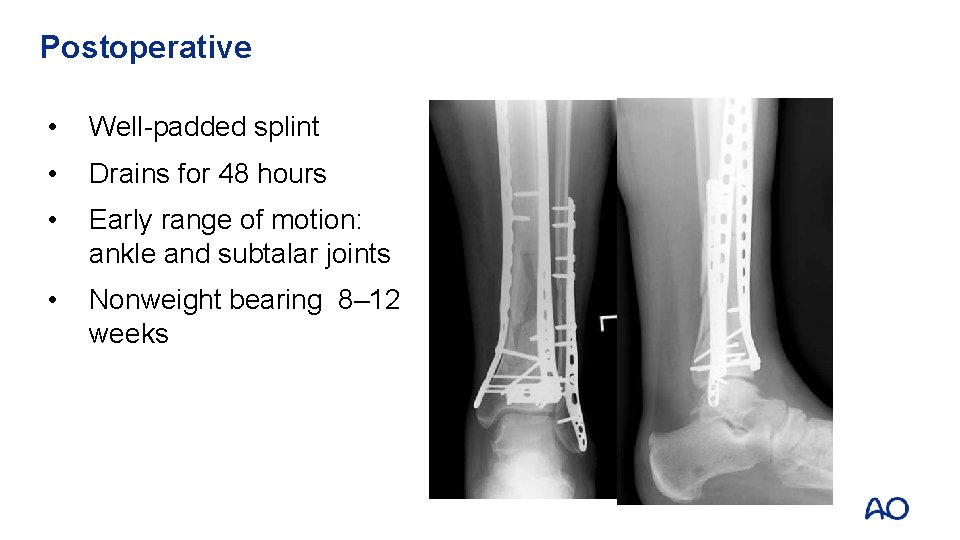
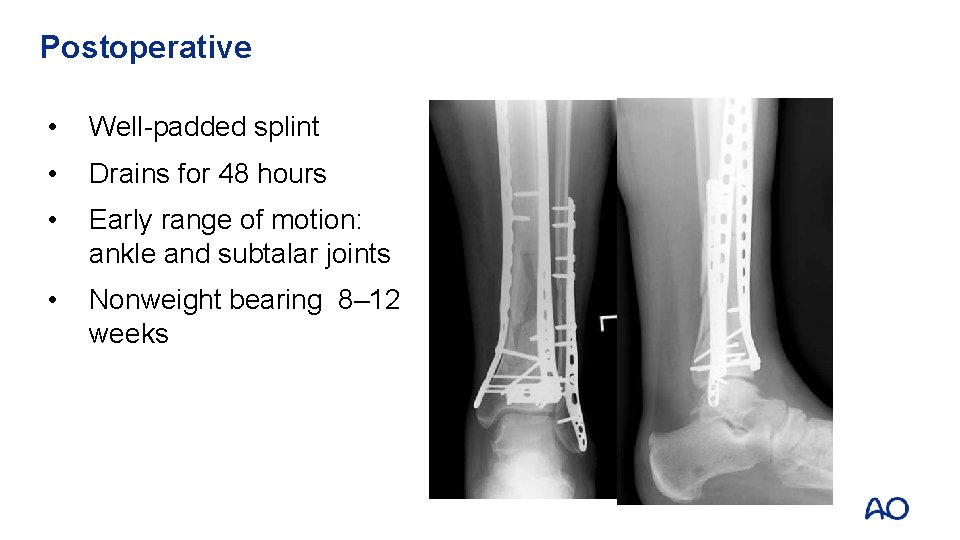
Postoperative • Well-padded splint • Drains for 48 hours • Early range of motion: ankle and subtalar joints • Nonweight bearing 8– 12 weeks
Take-home messages • Understand the fracture • Choose approach(es) • Direct articular reduction • Soft tissue friendly and effective plate application • (You can and will) avoid complications
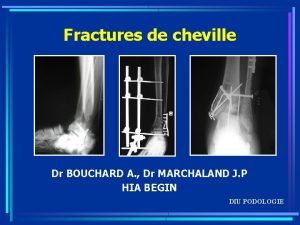
 Plafond tibial
Plafond tibial Test de skinner
Test de skinner First stage of god's revelation
First stage of god's revelation Concentric fracture in glass
Concentric fracture in glass Activity 14-1 glass fracture patterns
Activity 14-1 glass fracture patterns Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Expectant stakeholders
Expectant stakeholders Osseous surgery ppt
Osseous surgery ppt He undertook the first definitive study of fingerprints.
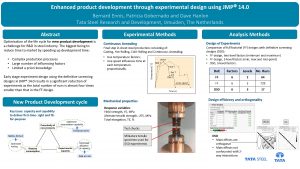
He undertook the first definitive study of fingerprints. Definitive screening design jmp
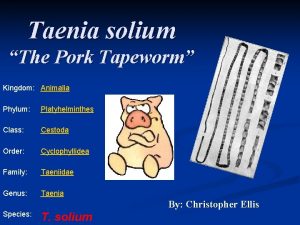
Definitive screening design jmp Dipylidium caninum definitive host
Dipylidium caninum definitive host Work breakdown structure for birthday party
Work breakdown structure for birthday party Definitive estimate range
Definitive estimate range Definite vs definitive
Definite vs definitive Vat definitive system
Vat definitive system Definitive screening design
Definitive screening design Information technology cost management
Information technology cost management Definitive articles in spanish
Definitive articles in spanish Widows peak periodontics
Widows peak periodontics Definitive rechtsöffnung
Definitive rechtsöffnung Definitive airway
Definitive airway Sustantivos definidos
Sustantivos definidos Definitive money
Definitive money Definitive host
Definitive host Definitive host vs intermediate host
Definitive host vs intermediate host A definitive host harbors which stage of a parasite
A definitive host harbors which stage of a parasite Definitive article
Definitive article Irving tennis elbow
Irving tennis elbow Gustilo anderson classification antibiotics
Gustilo anderson classification antibiotics Fracture supracondylienne classification
Fracture supracondylienne classification Classification tile bassin
Classification tile bassin Water seal suction chest tube
Water seal suction chest tube Primary bone vs secondary bone
Primary bone vs secondary bone Panfacial fractures sequencing
Panfacial fractures sequencing Daniel tibia
Daniel tibia Dr sukhpal singh
Dr sukhpal singh Open fracture treatment
Open fracture treatment Lisa kasman
Lisa kasman Farhad fazel
Farhad fazel Types of fractures with pictures
Types of fractures with pictures