Drugs Used in Asthma Dr Sasan Zaeri Pharm

- Slides: 36
Drugs Used in Asthma Dr. Sasan Zaeri (Pharm. D, Ph. D) Department of Pharmacology 1
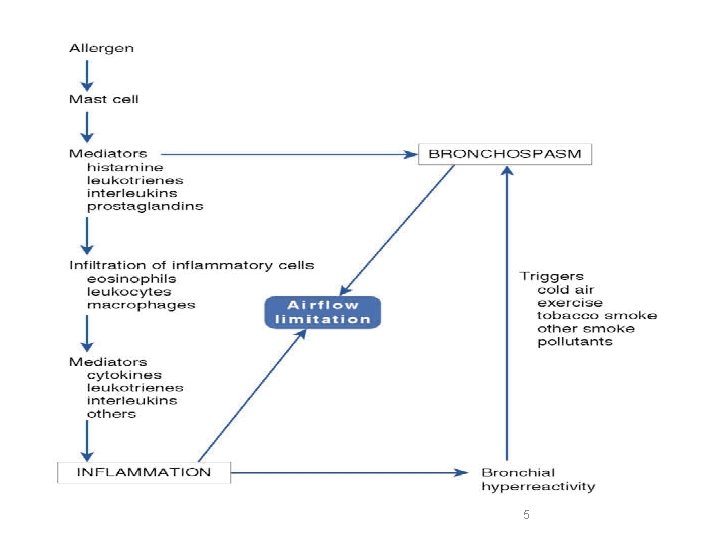
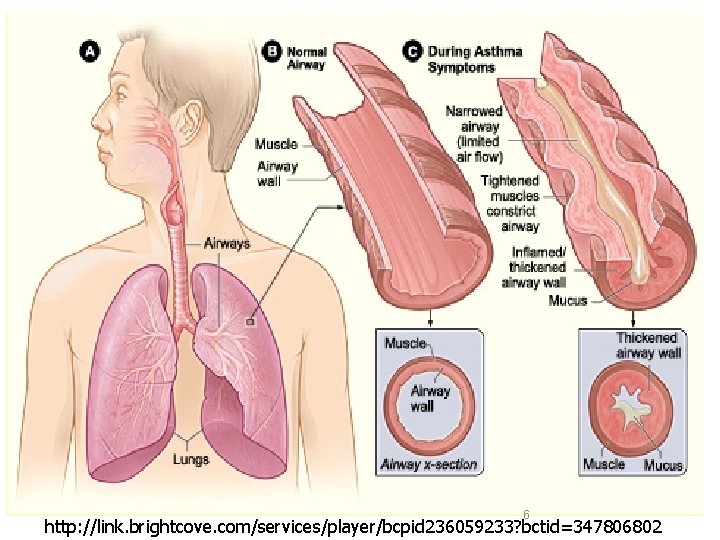
Asthma A chronic inflammatory disorder of bronchial airways that result in bronchospasm in response to external stimuli (pollen, cold air, tobacco smoke etc. ) 2
Symptoms of asthma • Asthma produces recurrent episodic attack of – Acute bronchoconstriction – Shortness of breath – Chest tightness – Wheezing – Rapid respiration – Cough 3
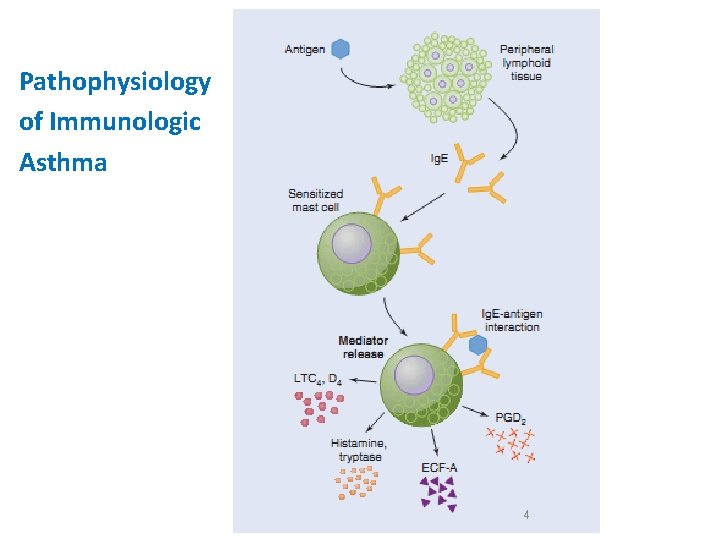
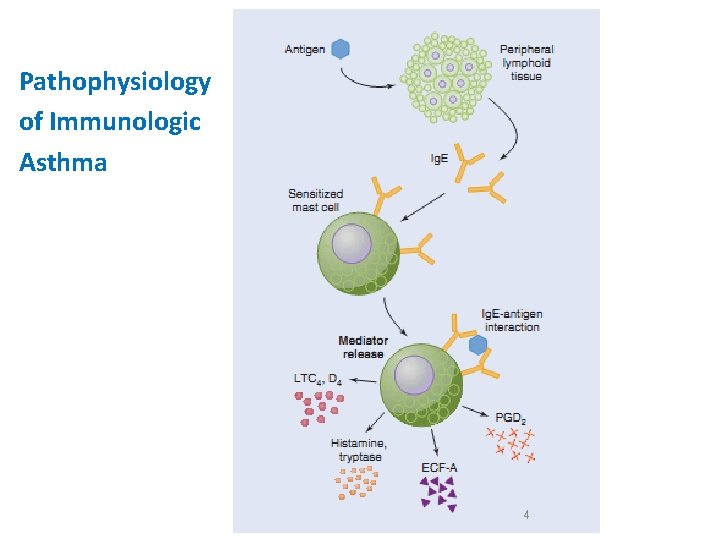
Pathophysiology of Immunologic Asthma 4
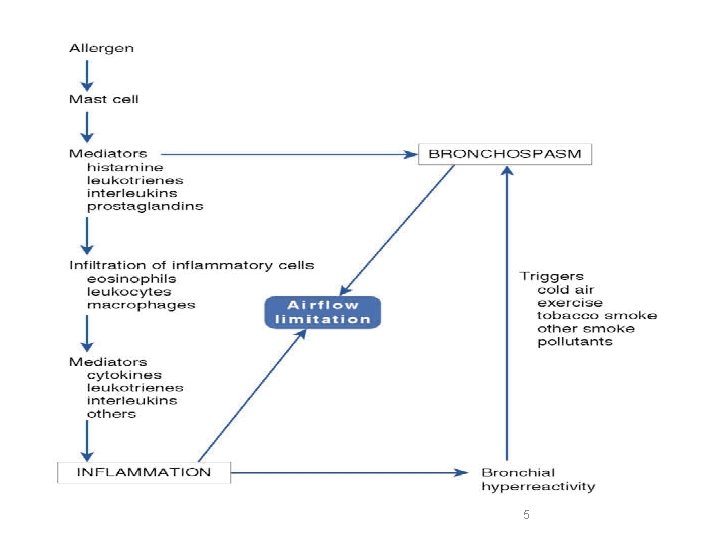
5
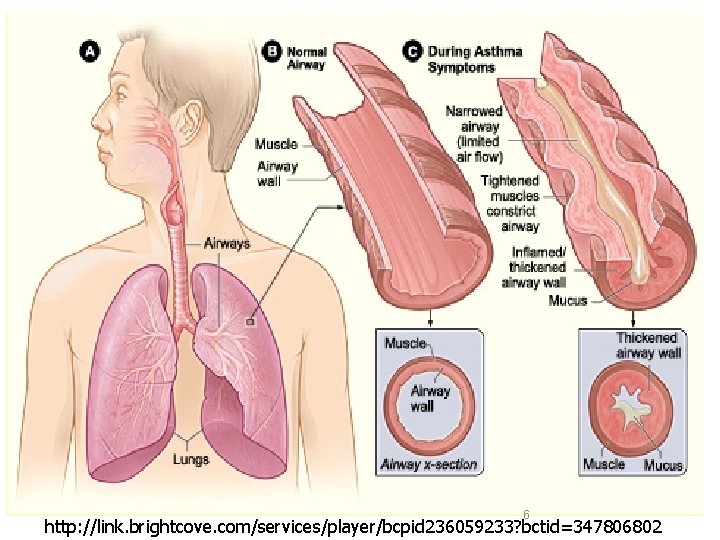
6 http: //link. brightcove. com/services/player/bcpid 236059233? bctid=347806802
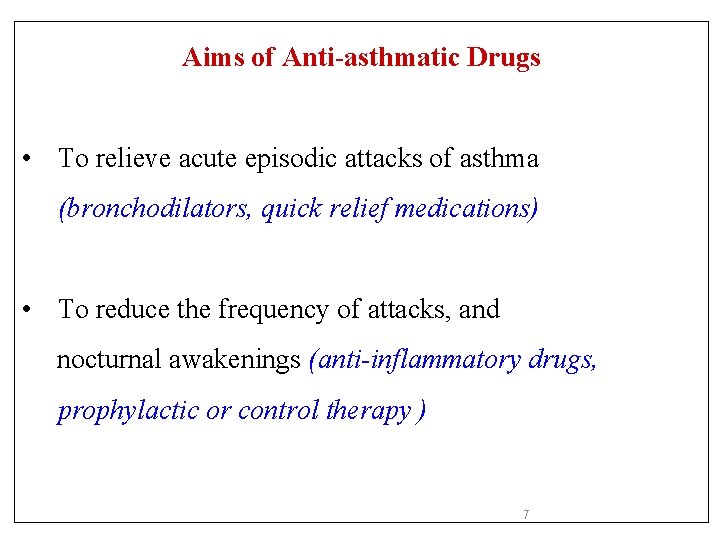
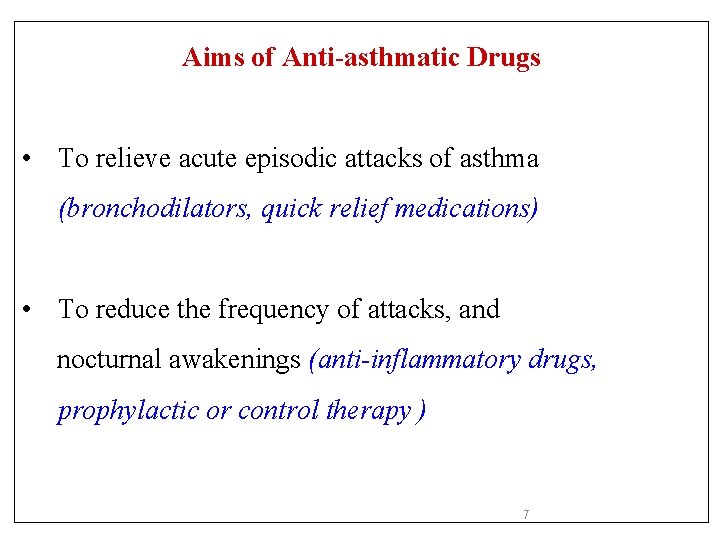
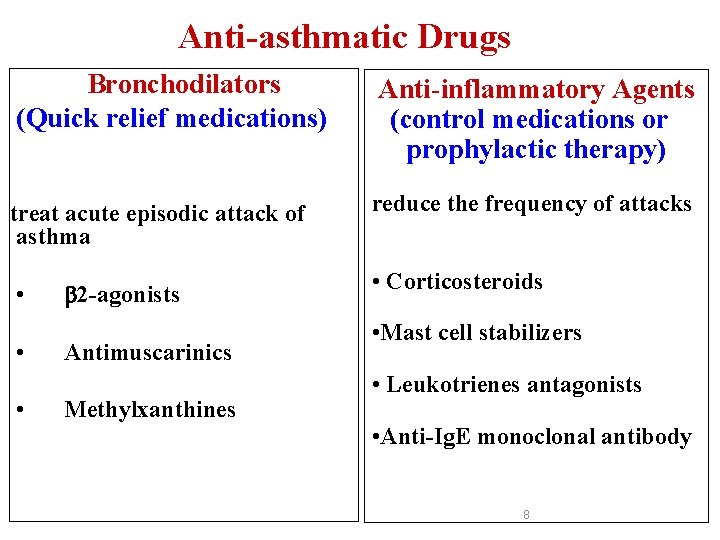
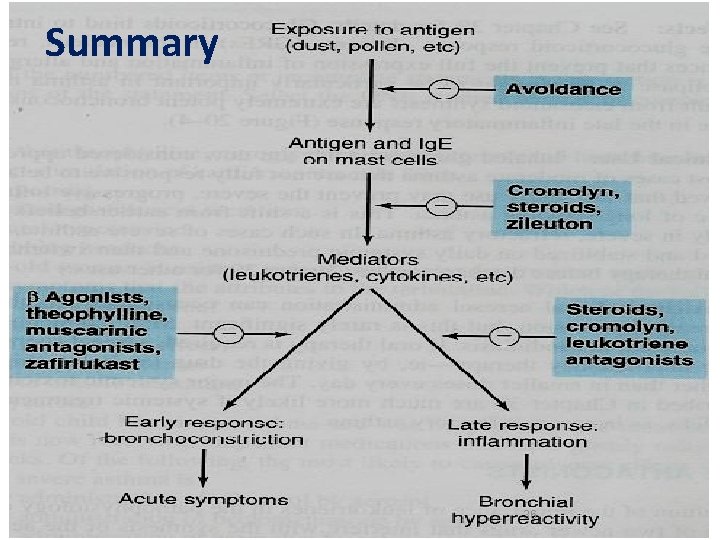
Aims of Anti-asthmatic Drugs • To relieve acute episodic attacks of asthma (bronchodilators, quick relief medications) • To reduce the frequency of attacks, and nocturnal awakenings (anti-inflammatory drugs, prophylactic or control therapy ) 7
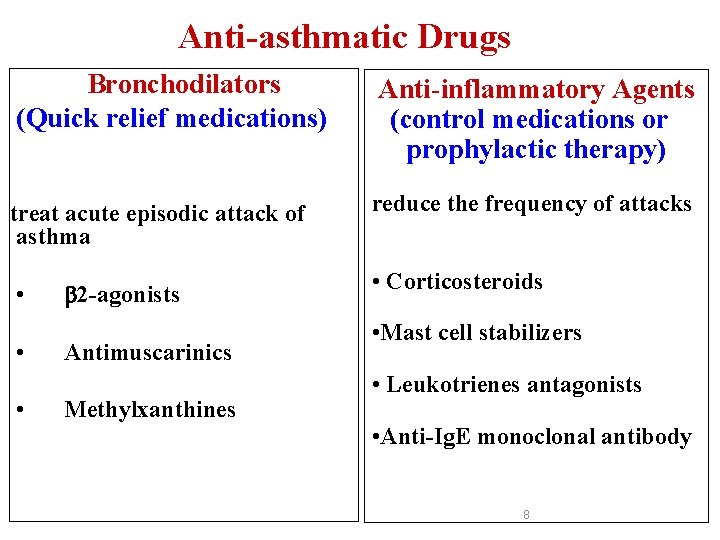
Anti-asthmatic Drugs Bronchodilators (Quick relief medications) Anti-inflammatory Agents (control medications or prophylactic therapy) treat acute episodic attack of asthma reduce the frequency of attacks • • • 2 -agonists Antimuscarinics Methylxanthines • Corticosteroids • Mast cell stabilizers • Leukotrienes antagonists • Anti-Ig. E monoclonal antibody 8
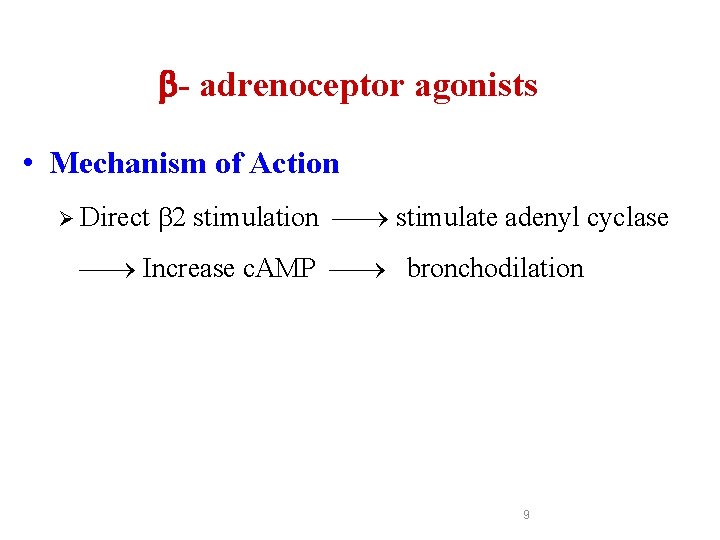
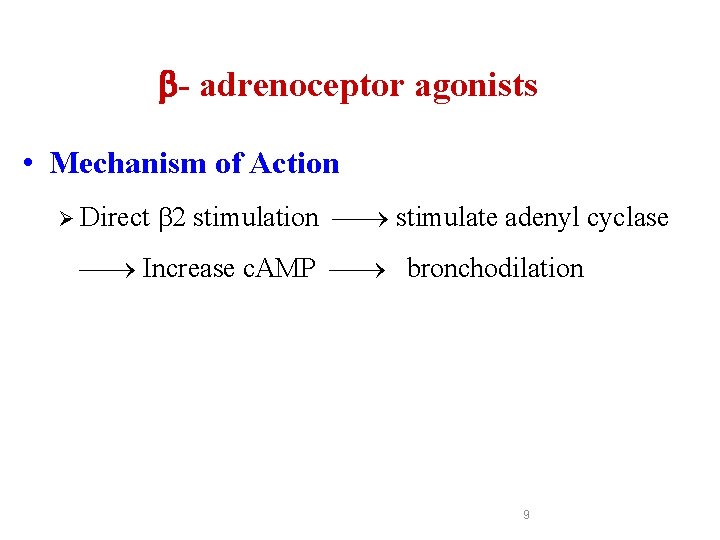
- adrenoceptor agonists • Mechanism of Action Ø Direct 2 stimulation stimulate adenyl cyclase Increase c. AMP bronchodilation 9
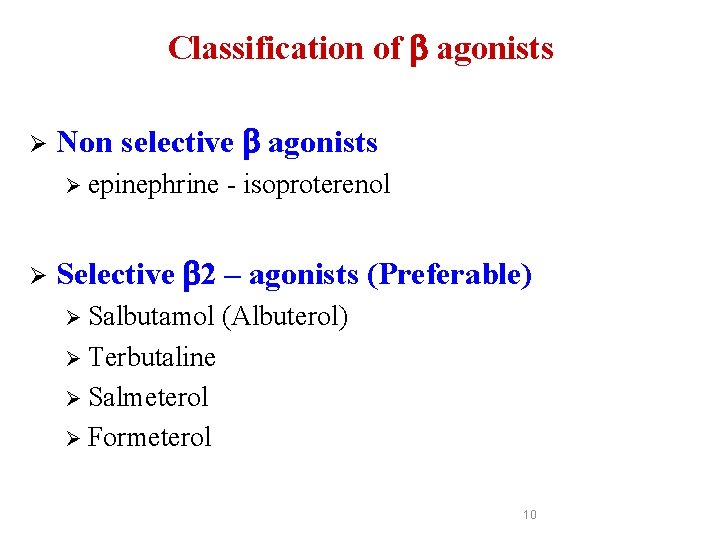
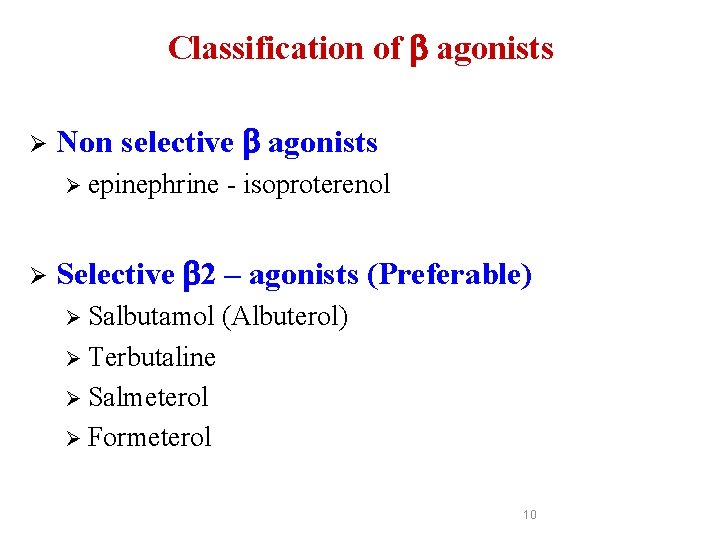
Classification of agonists Ø Non selective agonists Ø epinephrine Ø - isoproterenol Selective 2 – agonists (Preferable) Ø Salbutamol (Albuterol) Ø Terbutaline Ø Salmeterol Ø Formeterol 10

Nebulizer Inhaler 11
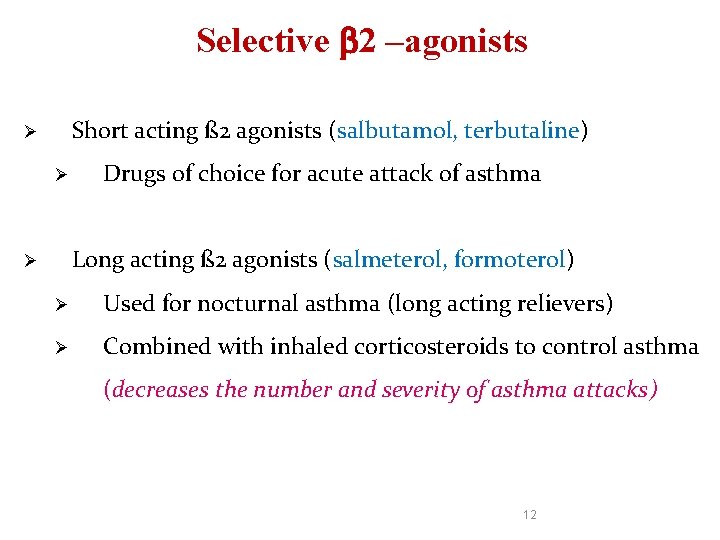
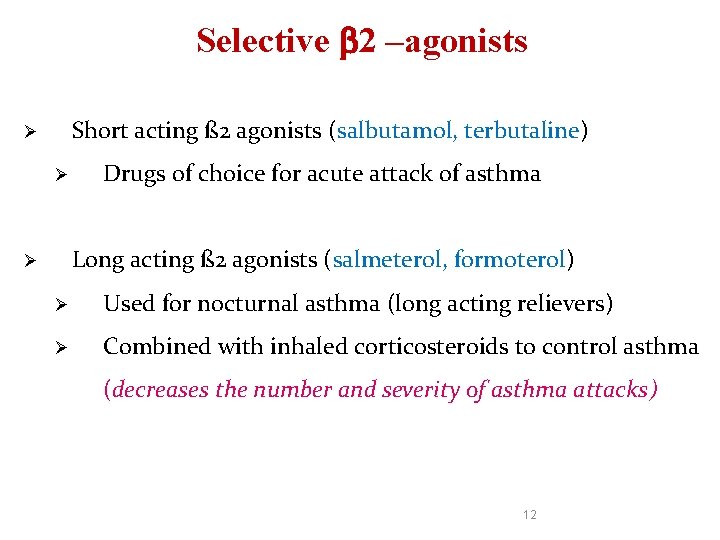
Selective 2 –agonists Short acting ß 2 agonists (salbutamol, terbutaline) Ø Ø Drugs of choice for acute attack of asthma Long acting ß 2 agonists (salmeterol, formoterol) Ø Ø Used for nocturnal asthma (long acting relievers) Ø Combined with inhaled corticosteroids to control asthma (decreases the number and severity of asthma attacks) 12
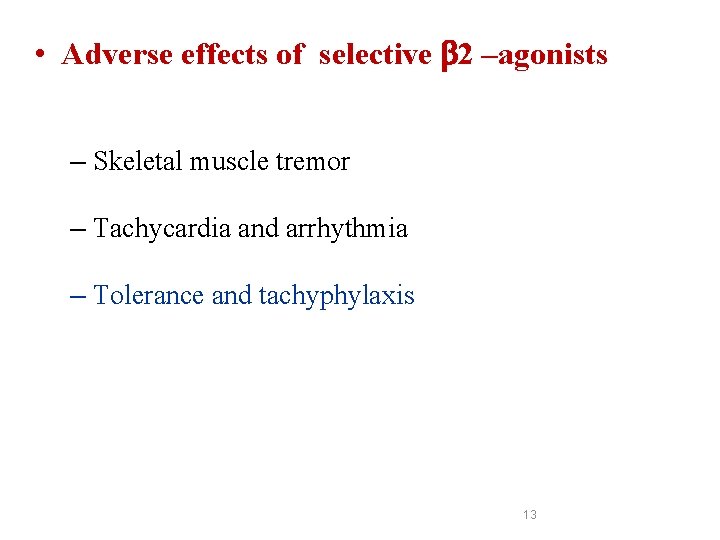
• Adverse effects of selective 2 –agonists – Skeletal muscle tremor – Tachycardia and arrhythmia – Tolerance and tachyphylaxis 13
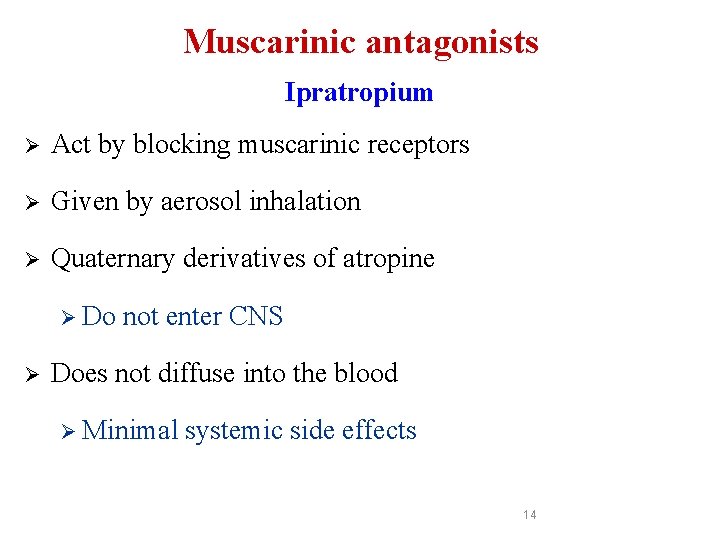
Muscarinic antagonists Ipratropium Ø Act by blocking muscarinic receptors Ø Given by aerosol inhalation Ø Quaternary derivatives of atropine Ø Do Ø not enter CNS Does not diffuse into the blood Ø Minimal systemic side effects 14
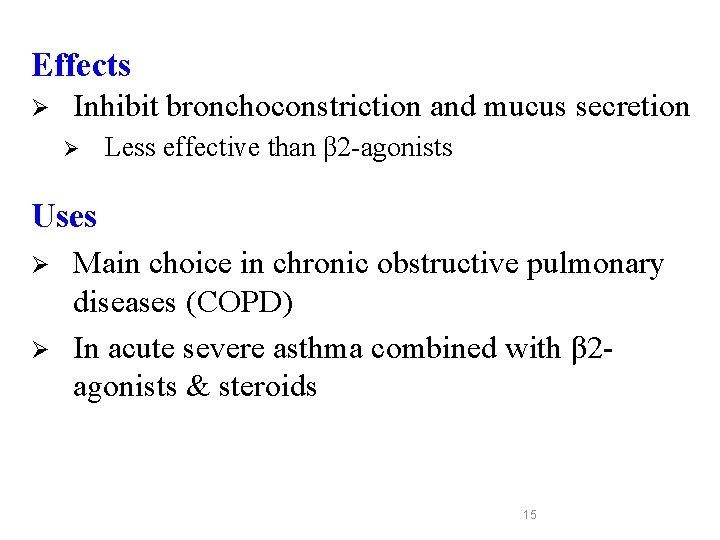
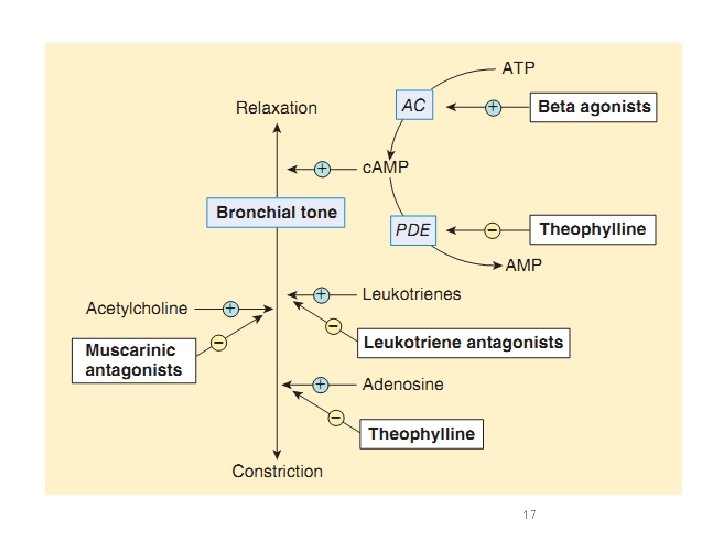
Effects Ø Inhibit bronchoconstriction and mucus secretion Ø Less effective than β 2 -agonists Uses Ø Ø Main choice in chronic obstructive pulmonary diseases (COPD) In acute severe asthma combined with β 2 agonists & steroids 15
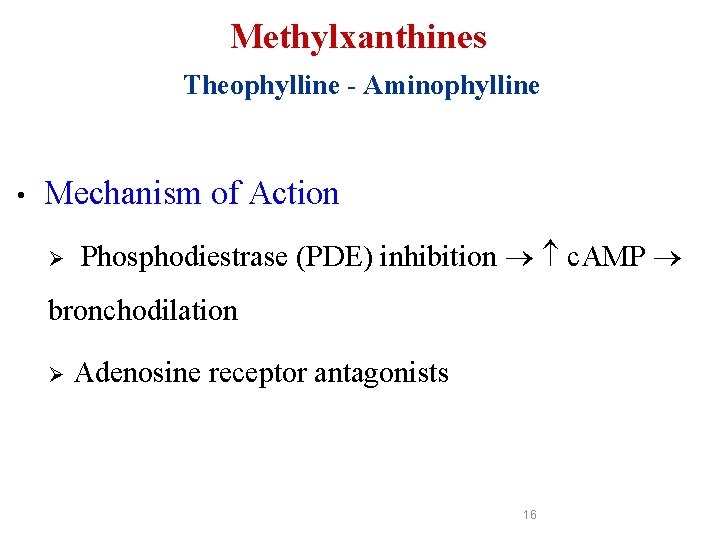
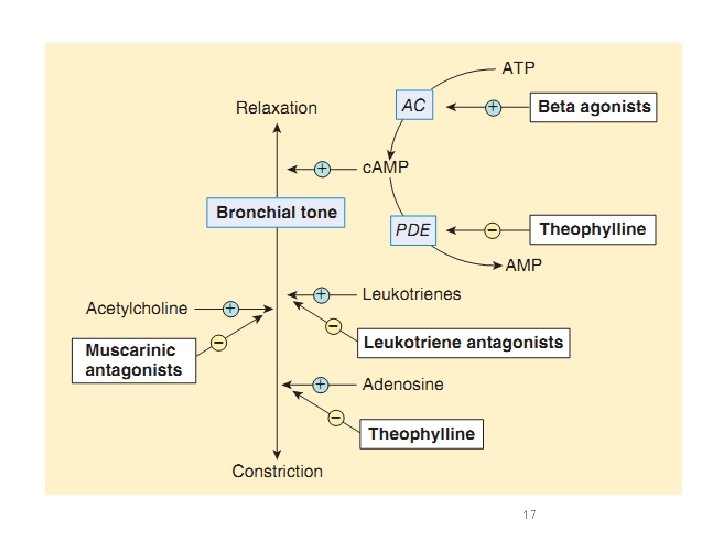
Methylxanthines Theophylline - Aminophylline • Mechanism of Action Ø Phosphodiestrase (PDE) inhibition c. AMP bronchodilation Ø Adenosine receptor antagonists 16
17
• Uses Ø Second line drug in asthma (theophylline in nocturnal asthma) Ø For status asthmatics (aminophylline is given as slow infusion) 18
• Side Effects Ø CVS: arrhythmia Ø GI: nausea & vomiting, ↑ gastric acid secretion Ø CNS: tremors, nervousness, insomnia, convulsion Ø Kidney: ↑renal blood flow, weak diuretic action 19
• Drug interactions Ø Metabolized by Cyp P 450 enzymes in liver Ø Enzyme inducers e. g. phenobarbital, rifampin, tobaco smoke → ↑metabolism of theophylline Ø Enzyme inhibitors e. g. erythromycin→ ↓ metabolism of theophylline 20
Anti - inflammatory Agents (control medications / prophylactic therapy) By reducing inflammation, they reduce bronchial hyper-reactivity and bronchospasm 21
Anti-inflammatory Agents Ø Glucocorticoids Ø Leukotrienes antagonists Ø Mast cell stabilizers Ø Anti-Ig. E monoclonal antibody (Omalizumab) 22
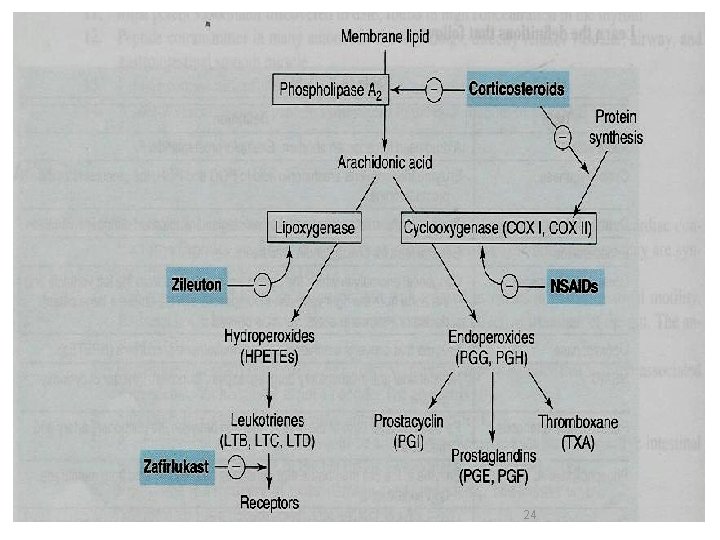
Glucocorticoids • Mechanism of action – Inhibition of phospholipase A 2 → ↓ prostaglandin and leukotrienes – Mast cell stabilization →↓ histamine release – Upregulation of β 2 receptors 23
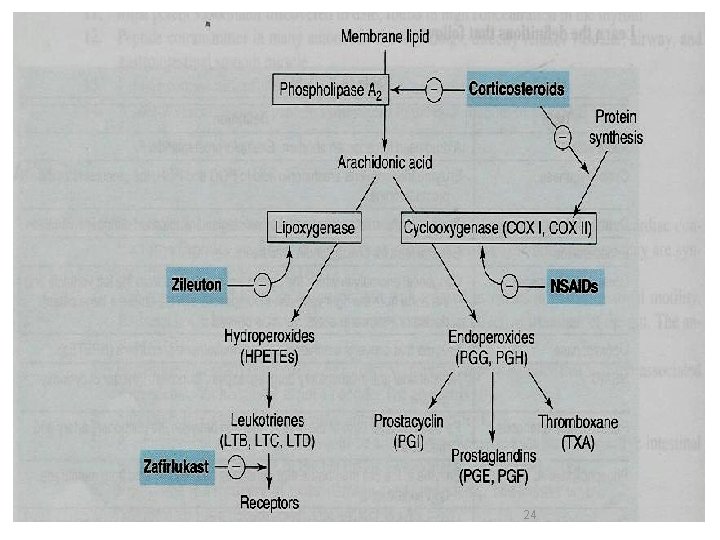
24
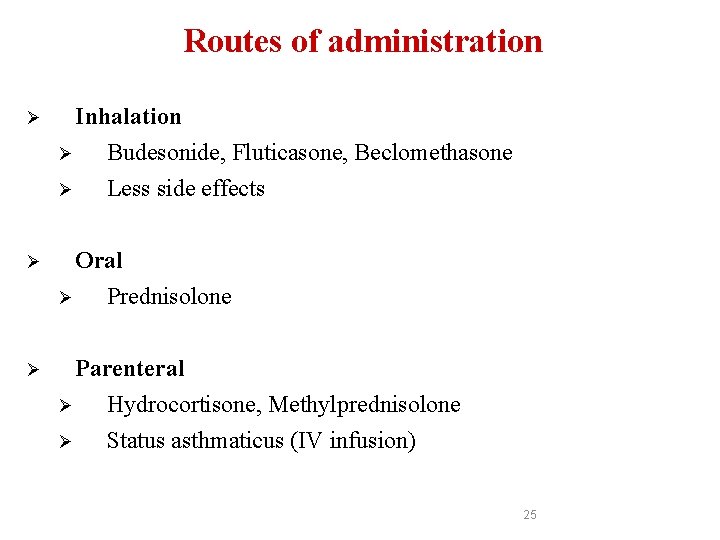
Routes of administration Ø Inhalation Ø Budesonide, Fluticasone, Beclomethasone Ø Less side effects Oral Ø Ø Ø Prednisolone Parenteral Ø Hydrocortisone, Methylprednisolone Ø Status asthmaticus (IV infusion) 25
Glucocorticoids § Are not bronchodilators § Given as prophylactic medications, used alone or combined with beta-agonists 26
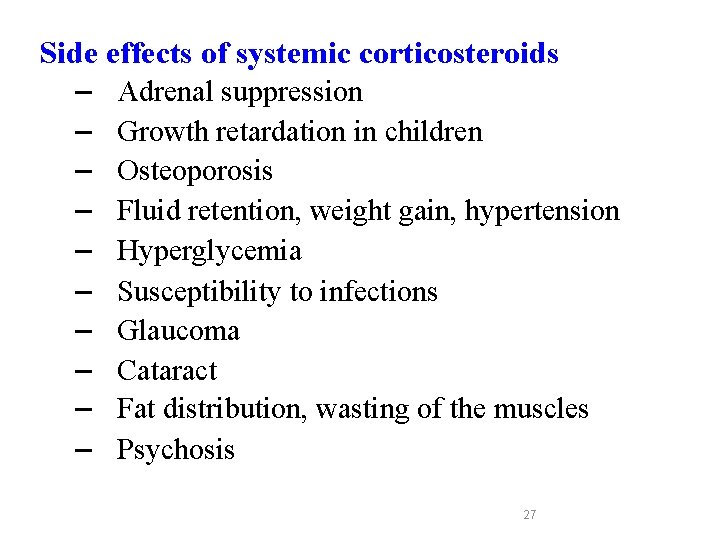
Side effects of systemic corticosteroids – Adrenal suppression – Growth retardation in children – Osteoporosis – Fluid retention, weight gain, hypertension – Hyperglycemia – Susceptibility to infections – Glaucoma – Cataract – Fat distribution, wasting of the muscles – Psychosis 27
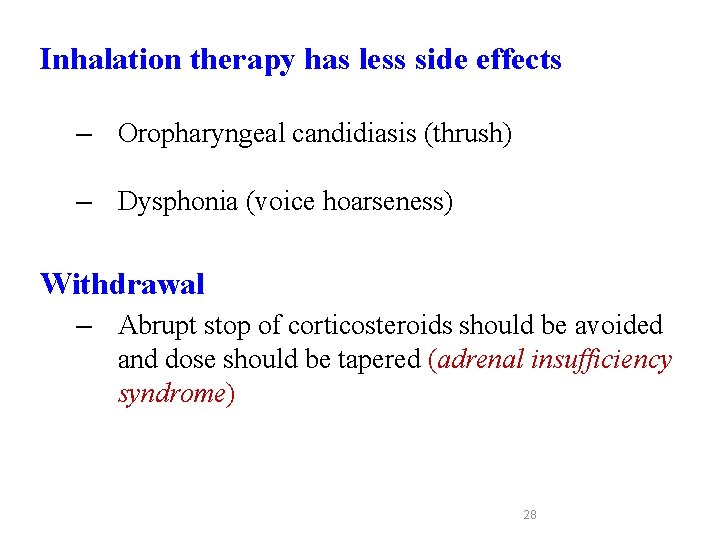
Inhalation therapy has less side effects – Oropharyngeal candidiasis (thrush) – Dysphonia (voice hoarseness) Withdrawal – Abrupt stop of corticosteroids should be avoided and dose should be tapered (adrenal insufficiency syndrome) 28
Mast cell stabilizers Cromolyn - Nedocromil Ø Act by stabilization of mast cell membrane Ø Have poor oral absorption Ø Given by inhalation 29
Mast cell stabilizers §Not bronchodilators §Not effective in acute attack of asthma §Prophylactic anti-inflammatory drugs §Children respond better than adults 30
Uses Ø Prophylactic therapy in asthma especially in children Ø Allergic rhinitis Ø Conjunctivitis Side effects Ø Bitter taste Ø minor upper respiratory tract irritation (burning sensation) 31
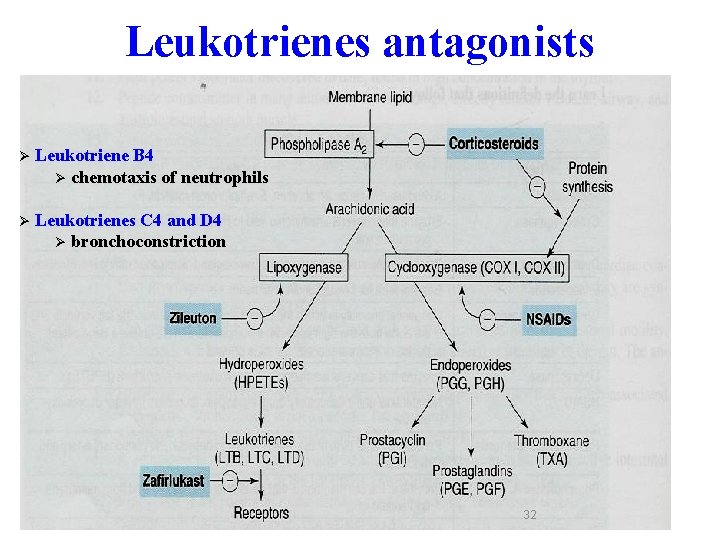
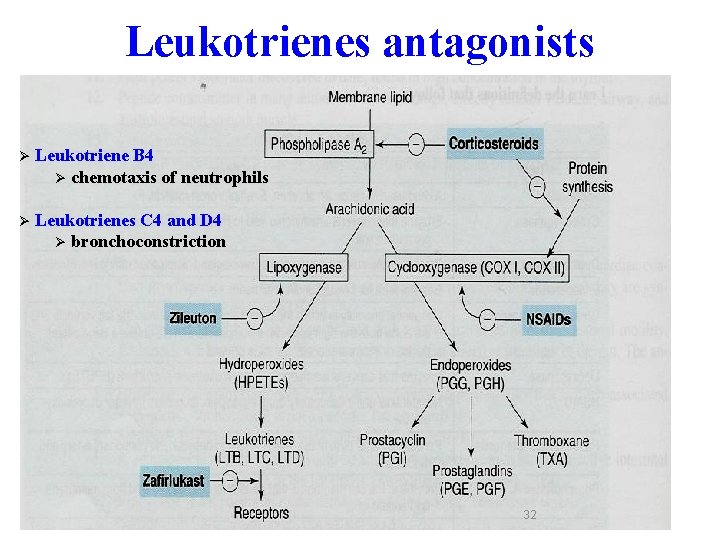
Leukotrienes antagonists Ø Leukotriene B 4 Ø chemotaxis of neutrophils Ø Leukotrienes C 4 and D 4 Ø bronchoconstriction 32
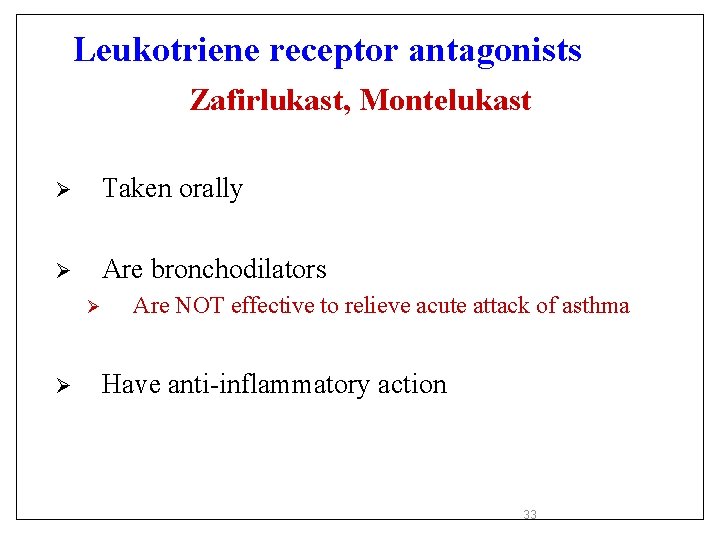
Leukotriene receptor antagonists Zafirlukast, Montelukast Ø Taken orally Ø Are bronchodilators Ø Ø Are NOT effective to relieve acute attack of asthma Have anti-inflammatory action 33
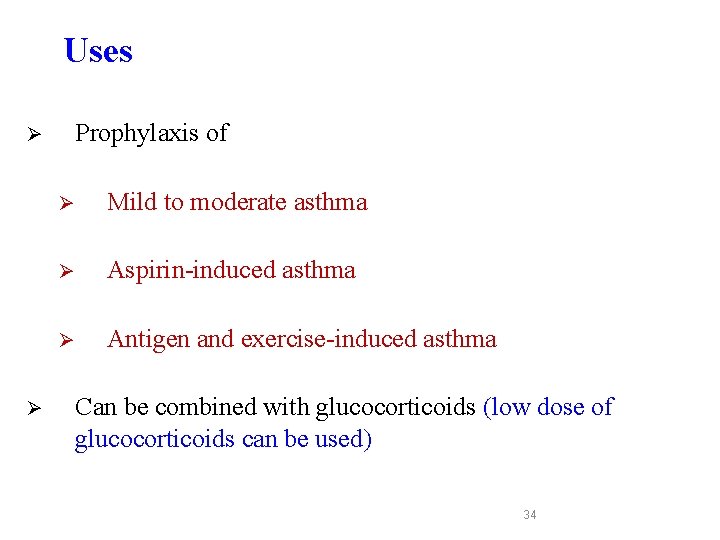
Uses Prophylaxis of Ø Ø Ø Mild to moderate asthma Ø Aspirin-induced asthma Ø Antigen and exercise-induced asthma Can be combined with glucocorticoids (low dose of glucocorticoids can be used) 34
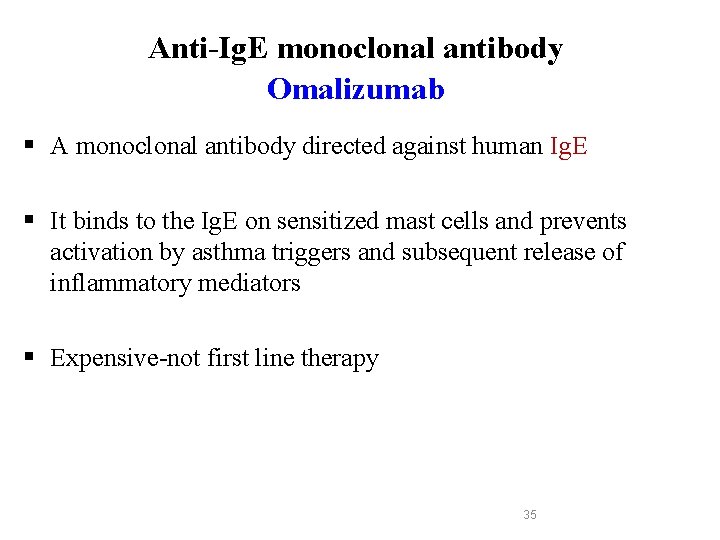
Anti-Ig. E monoclonal antibody Omalizumab § A monoclonal antibody directed against human Ig. E § It binds to the Ig. E on sensitized mast cells and prevents activation by asthma triggers and subsequent release of inflammatory mediators § Expensive-not first line therapy 35
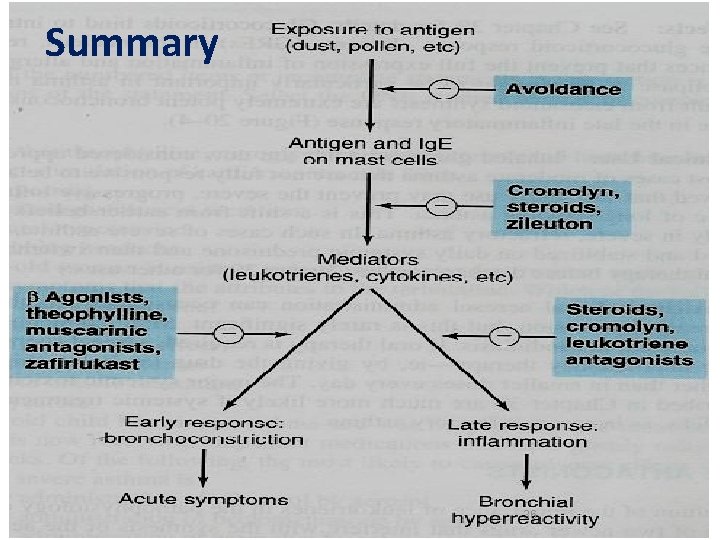
Summary 36
 بیمارستان مدرس
بیمارستان مدرس Pathophysiology definition
Pathophysiology definition English for pharmacist
English for pharmacist Pharm d means
Pharm d means Ambio pharm
Ambio pharm Pharm gkb
Pharm gkb Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Pharm
Pharm Pharm 406
Pharm 406 Secur pharm
Secur pharm Library.med.utah.edu/kw/pharm/hyper heart.html
Library.med.utah.edu/kw/pharm/hyper heart.html Solid blender
Solid blender Klucel exf
Klucel exf Bc bio-pharm
Bc bio-pharm Nicole noel purdue
Nicole noel purdue Outfield pharm
Outfield pharm Pharm id
Pharm id Media pharm
Media pharm Mva/eva tray
Mva/eva tray Drugs used in pregnancy
Drugs used in pregnancy Specific objectives of asthma
Specific objectives of asthma X ray of asthma patient
X ray of asthma patient Asthma clinical pathway
Asthma clinical pathway Amas faa drugs
Amas faa drugs Abcde assessment asthma
Abcde assessment asthma Nwts asthma
Nwts asthma Asthma diagnosis criteria
Asthma diagnosis criteria Pediatric asthma care near santa rosa
Pediatric asthma care near santa rosa Asthma pathophysiology
Asthma pathophysiology American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Asthma progression
Asthma progression Gold asthma
Gold asthma Copd vs asthma
Copd vs asthma Global initiative for asthma
Global initiative for asthma Spirometry
Spirometry Asthma bronx
Asthma bronx Unmet needs in severe asthma
Unmet needs in severe asthma