Dr Sasan Zaeri Pharm D Ph D Department




- Slides: 46
Dr. Sasan Zaeri (Pharm. D, Ph. D) Department of Pharmacology, BPUMS
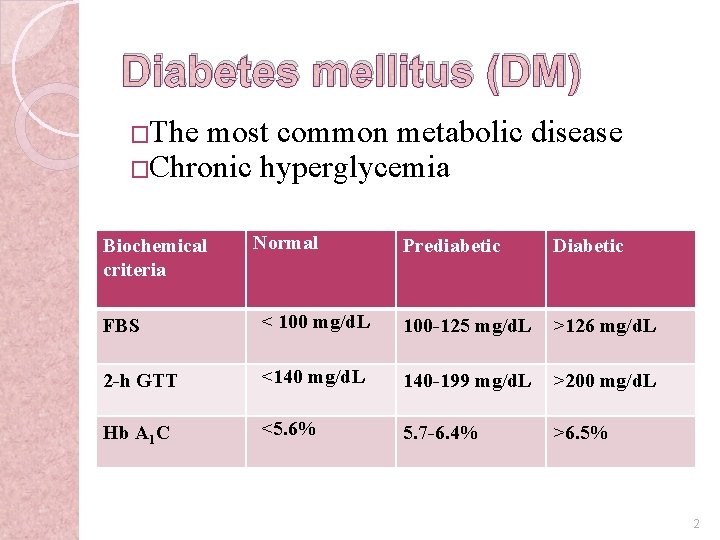
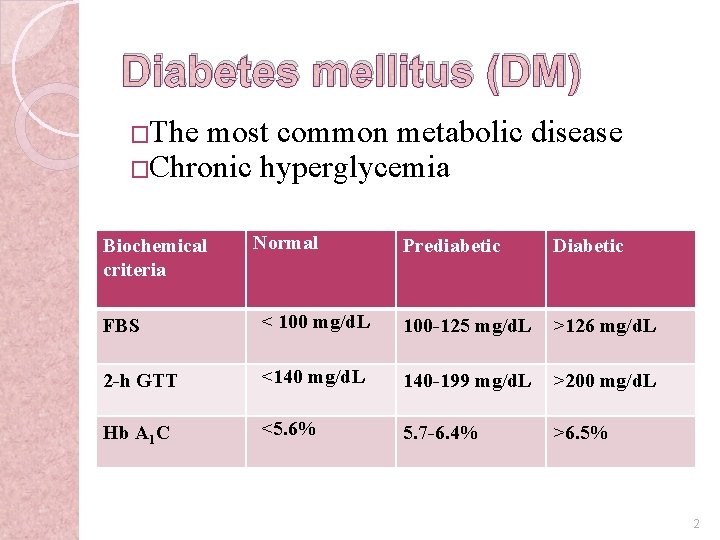
Diabetes mellitus (DM) �The most common metabolic disease �Chronic hyperglycemia Biochemical criteria Normal Prediabetic Diabetic FBS < 100 mg/d. L 100 -125 mg/d. L >126 mg/d. L 2 -h GTT <140 mg/d. L 140 -199 mg/d. L >200 mg/d. L Hb A 1 C <5. 6% 5. 7 -6. 4% >6. 5% 2
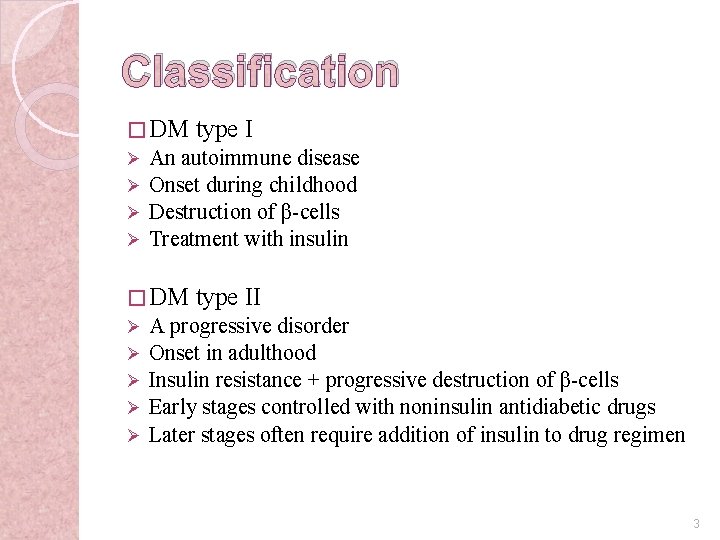
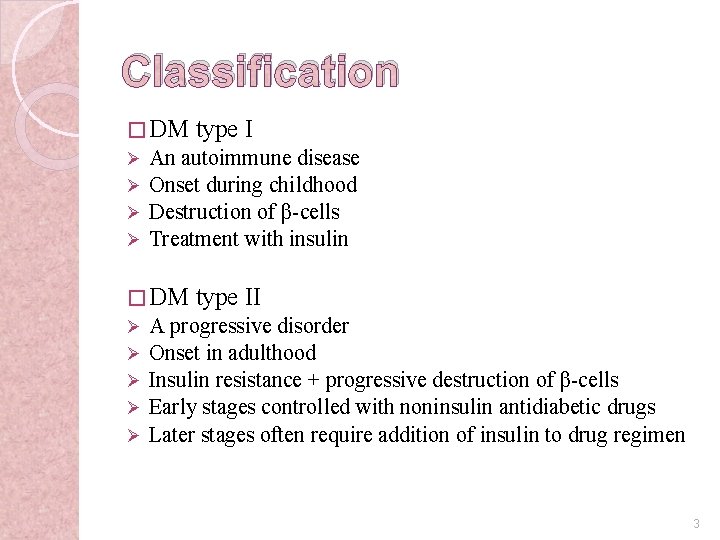
Classification � DM Ø Ø An autoimmune disease Onset during childhood Destruction of β-cells Treatment with insulin � DM Ø Ø Ø type II A progressive disorder Onset in adulthood Insulin resistance + progressive destruction of β-cells Early stages controlled with noninsulin antidiabetic drugs Later stages often require addition of insulin to drug regimen 3
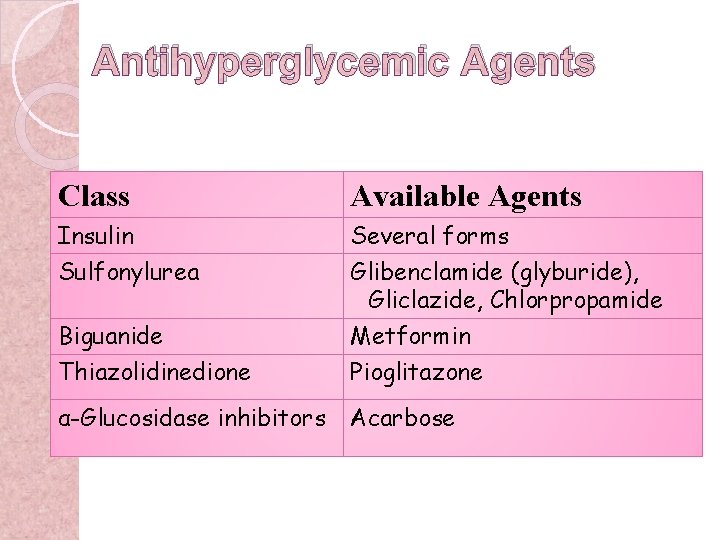
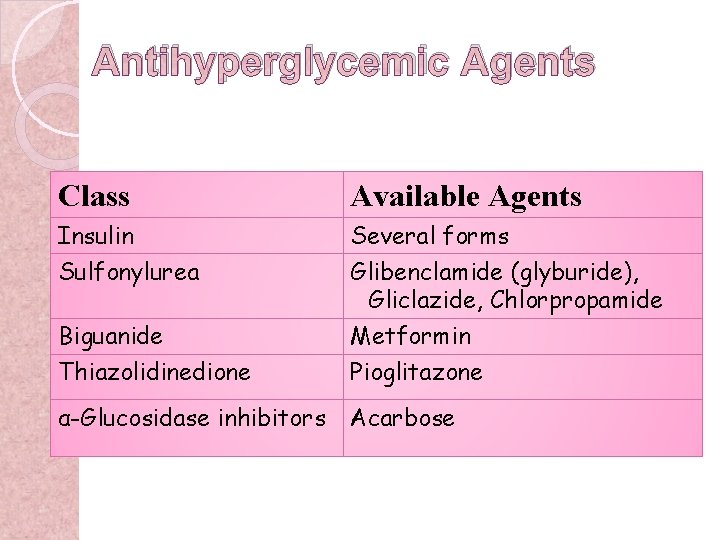
Antihyperglycemic Agents Class Available Agents Insulin Sulfonylurea Several forms Glibenclamide (glyburide), Gliclazide, Chlorpropamide Biguanide Thiazolidinedione Metformin Pioglitazone α-Glucosidase inhibitors Acarbose
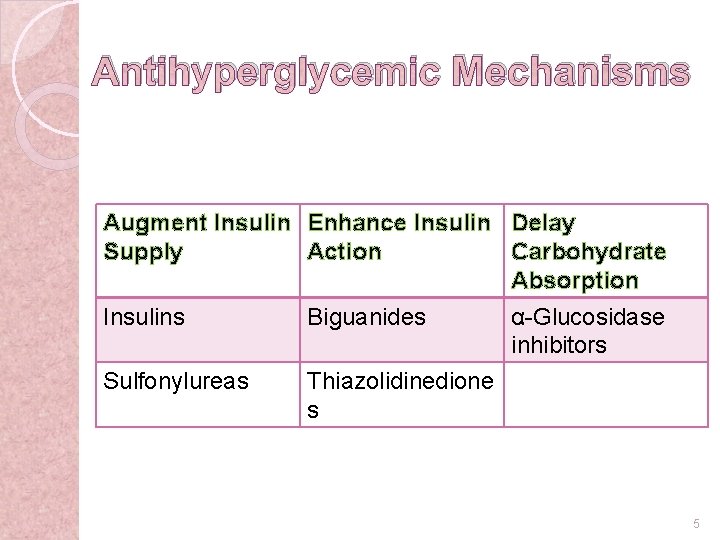
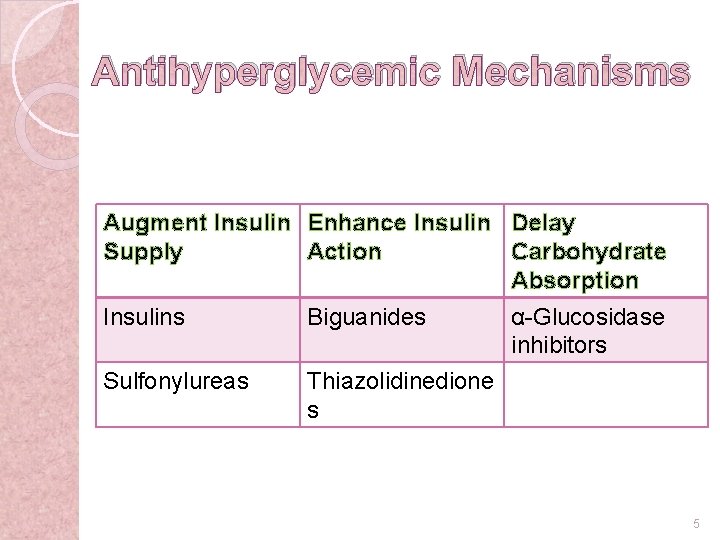
Antihyperglycemic Mechanisms Augment Insulin Enhance Insulin Delay Supply Action Carbohydrate Absorption Insulins Biguanides α-Glucosidase inhibitors Sulfonylureas Thiazolidinedione s 5
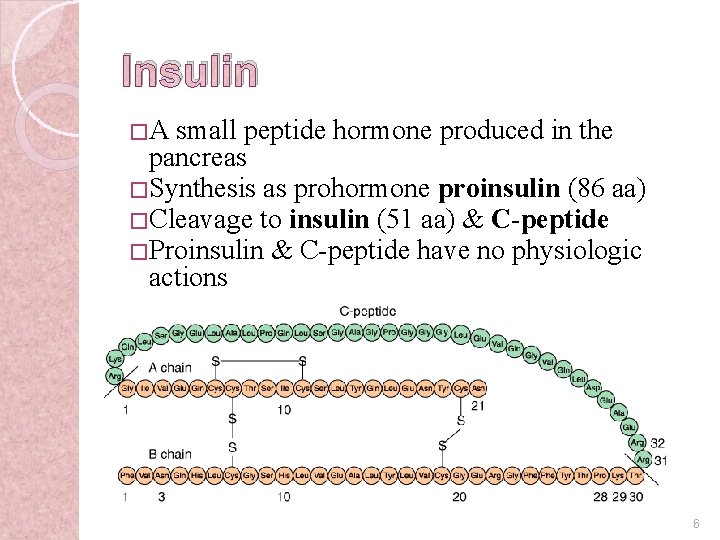
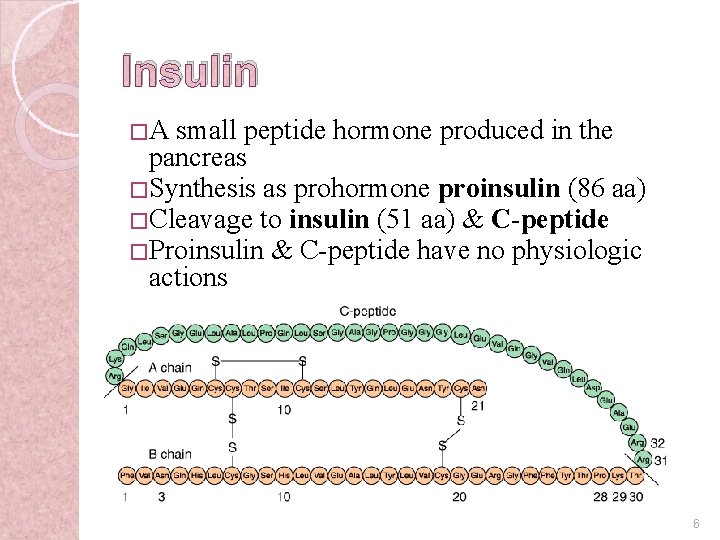
Insulin �A small peptide hormone produced in the pancreas � Synthesis as prohormone proinsulin (86 aa) � Cleavage to insulin (51 aa) & C-peptide � Proinsulin & C-peptide have no physiologic actions 6
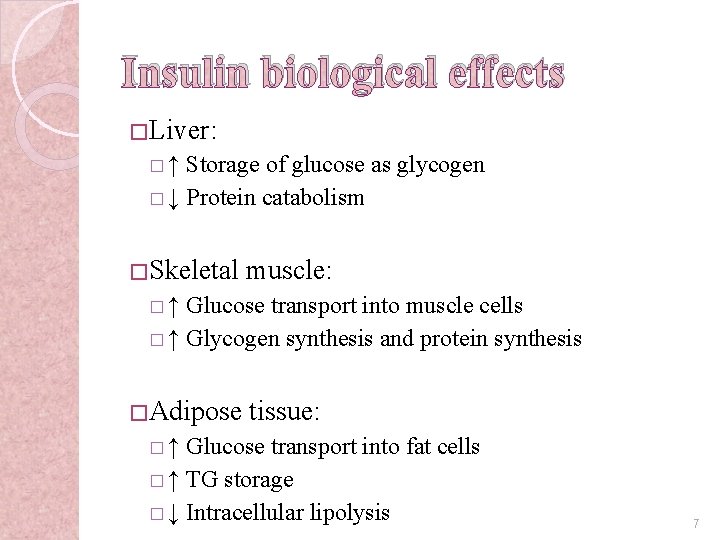
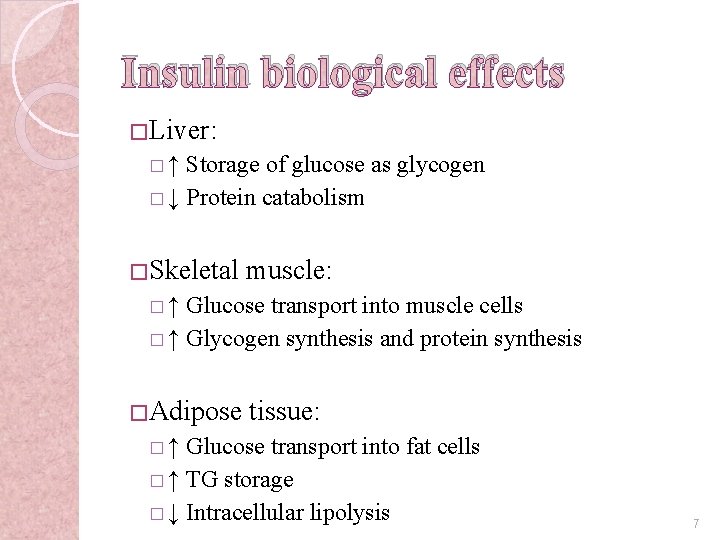
Insulin biological effects � Liver: �↑ Storage of glucose as glycogen � ↓ Protein catabolism � Skeletal muscle: �↑ Glucose transport into muscle cells � ↑ Glycogen synthesis and protein synthesis � Adipose tissue: �↑ Glucose transport into fat cells � ↑ TG storage � ↓ Intracellular lipolysis 7
Insulin indications �DM II �DM emergencies �Diabetic pregnant women 8
Insulin Preparations �Different ◦ ◦ capacity to lower blood glucose. Rapid acting Short acting Intermediate acting Long acting 9
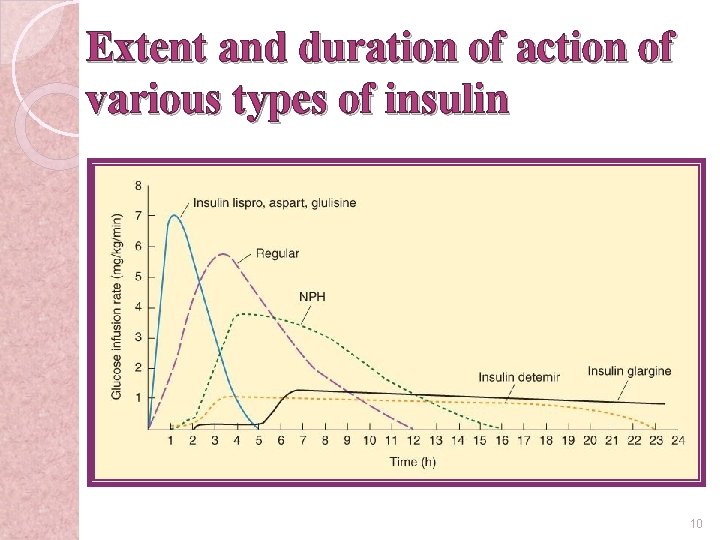
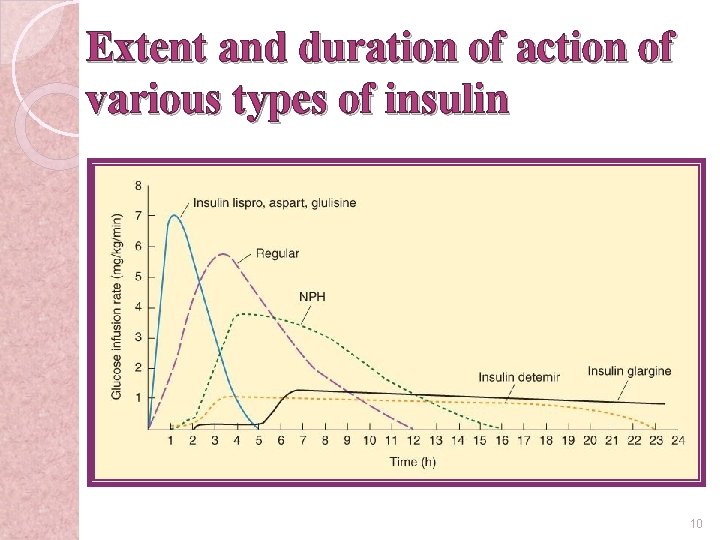
Extent and duration of action of various types of insulin 10
Rapid-acting insulin �Lispro, aspart, glulisine �Onset: <15 min �Duration: 3 -4 h �rapid onsets and early peaks of activity 11
Rapid-acting insulin �Lispro, aspart, glulisine �Indications: ◦ control of postprandial glucose (immediately before a meal ) ◦ emergency treatment of uncomplicated diabetic ketoacidosis 12
Short-acting insulin �Regular �Onset: 0. 5 -1 h �Duration: 4 -6 h 13
Short-acting insulin �Regular �Indications: ◦ emergencies of hyperglycemia (IV) ◦ ordinary maintenance regimens (SC) �alone or mixed with intermediate preparations 14
Intermediate-acting insulin �Lente, Neutral Protamine Hagedorn (NPH) �Onset: 1 -4 h �Duration : 10 -16 h 15
Intermediate-acting insulin �NPH insulin: exhibits a delayed onset and peak of action �NPH insulin is often combined with regular and rapid-acting insulins 16
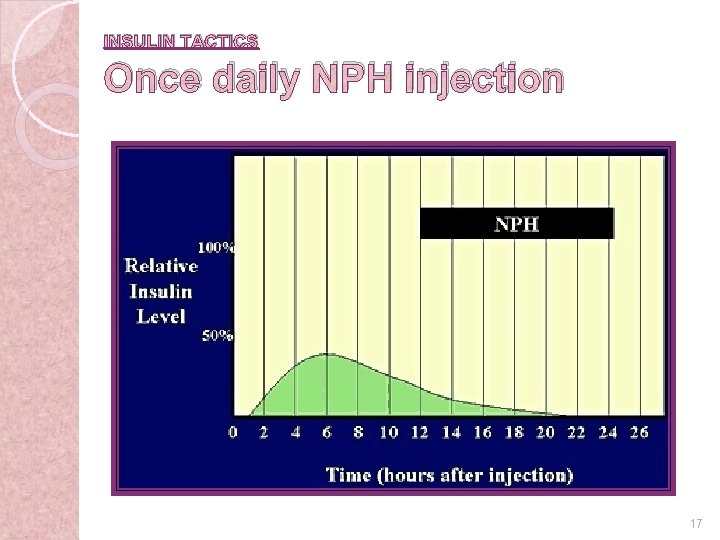
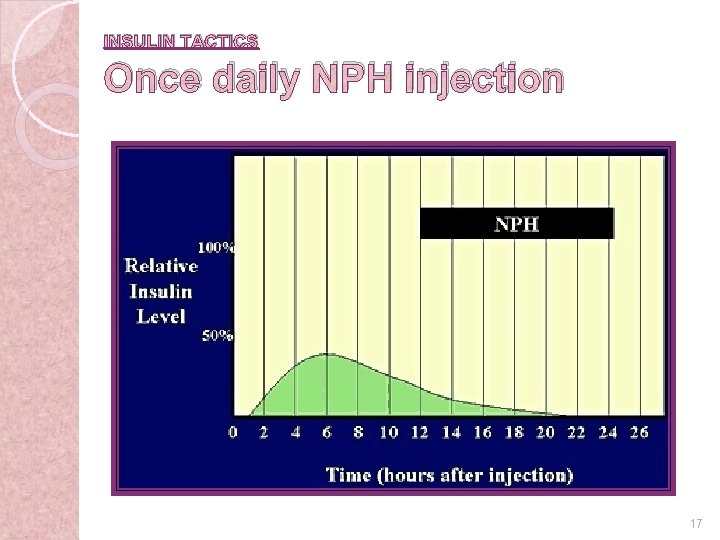
INSULIN TACTICS Once daily NPH injection 17 6 -23
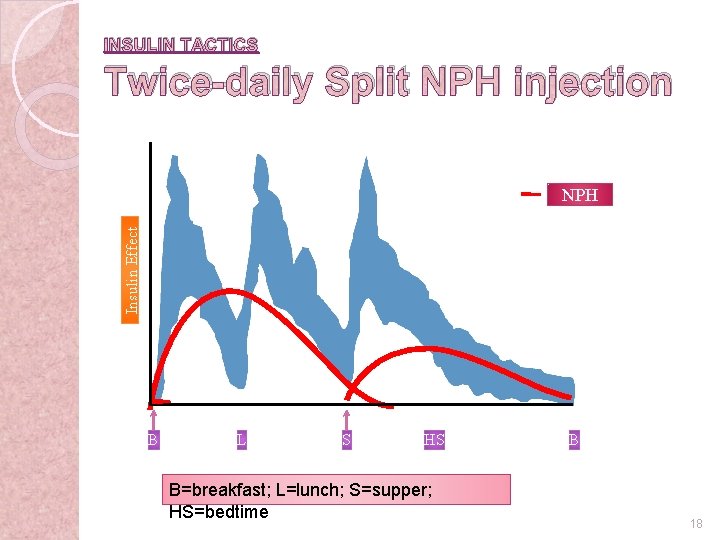
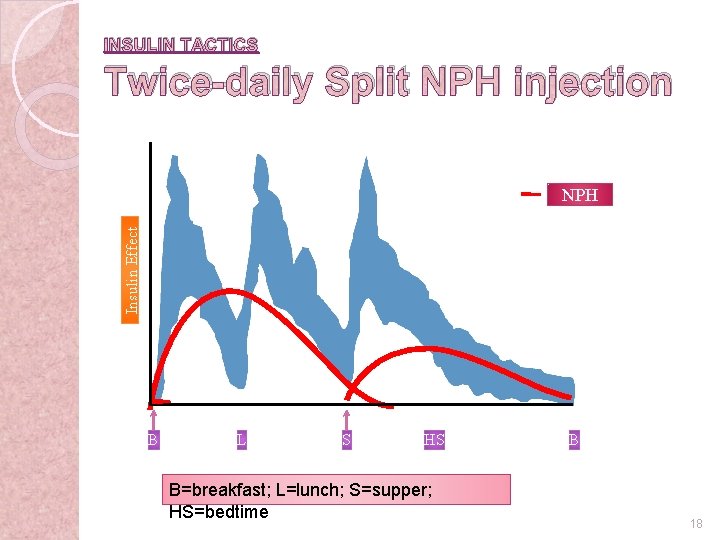
INSULIN TACTICS Twice-daily Split NPH injection Insulin Effect NPH B L S HS B=breakfast; L=lunch; S=supper; HS=bedtime B 18 6 -23
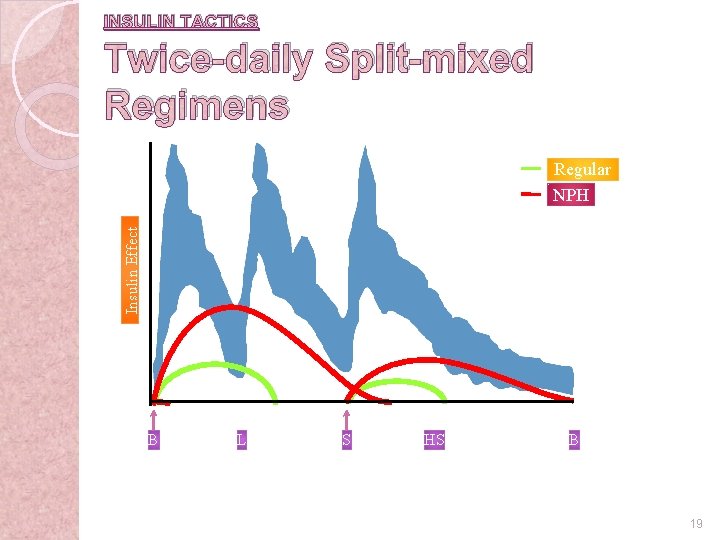
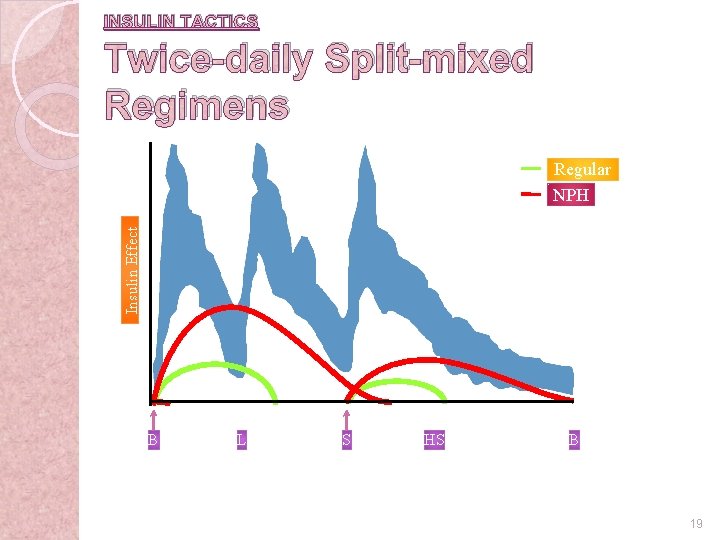
INSULIN TACTICS Twice-daily Split-mixed Regimens Insulin Effect Regular NPH B L S HS B 19 6 -23
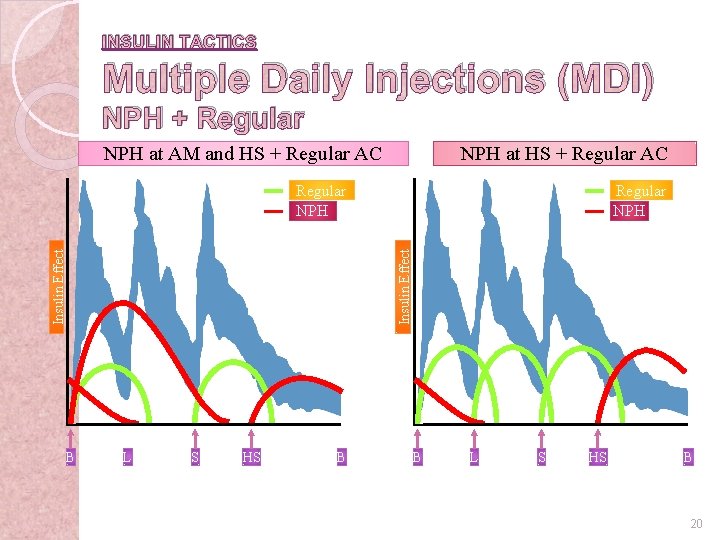
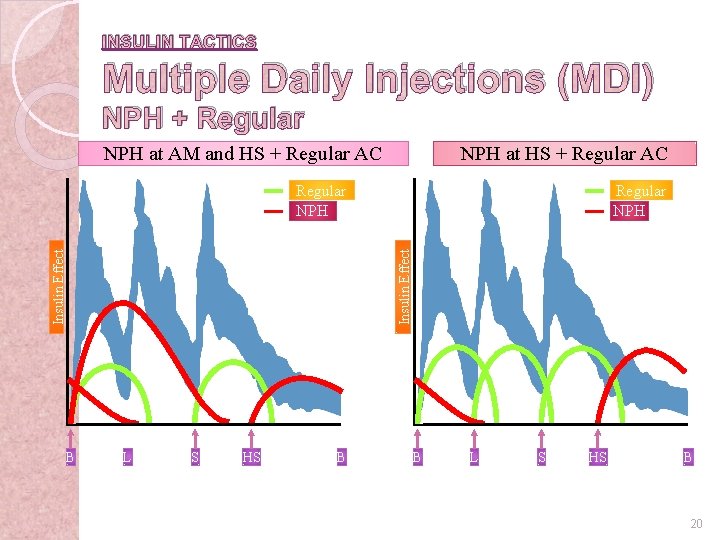
INSULIN TACTICS Multiple Daily Injections (MDI) NPH + Regular NPH at AM and HS + Regular AC NPH at HS + Regular AC Regular NPH Insulin Effect Regular NPH B L S HS B 20 6 -24
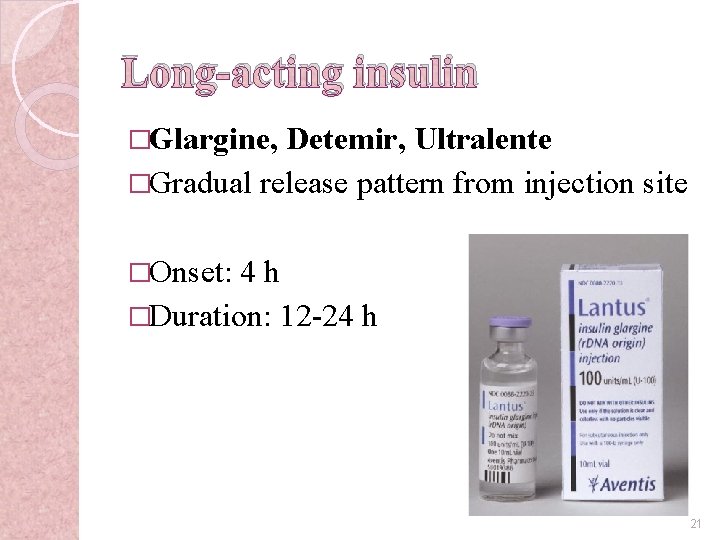
Long-acting insulin �Glargine, Detemir, Ultralente �Gradual release pattern from injection site �Onset: 4 h �Duration: 12 -24 h 21
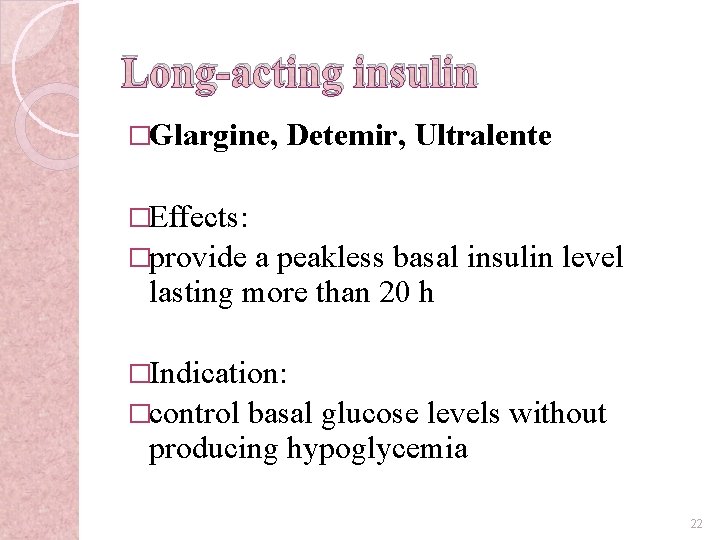
Long-acting insulin �Glargine, Detemir, Ultralente �Effects: �provide a peakless basal insulin level lasting more than 20 h �Indication: �control basal glucose levels without producing hypoglycemia 22
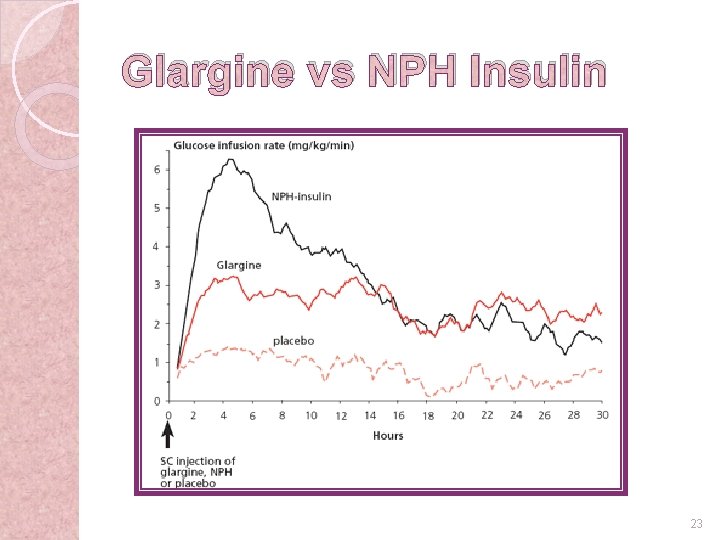
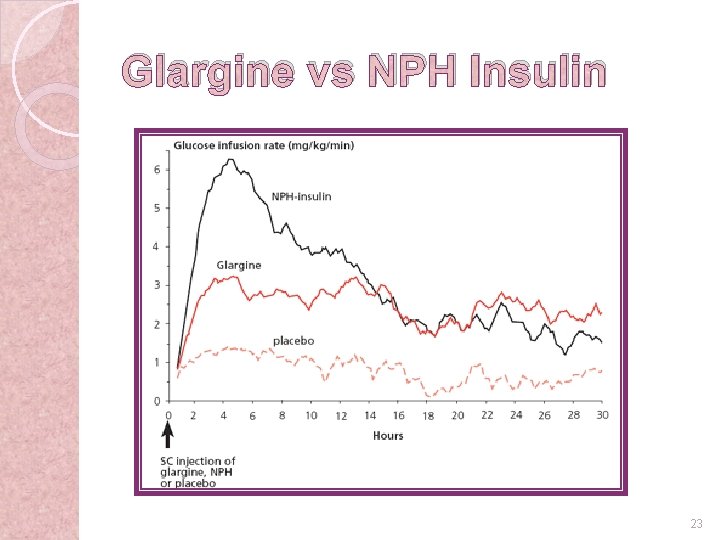
Glargine vs NPH Insulin 23 6 -34
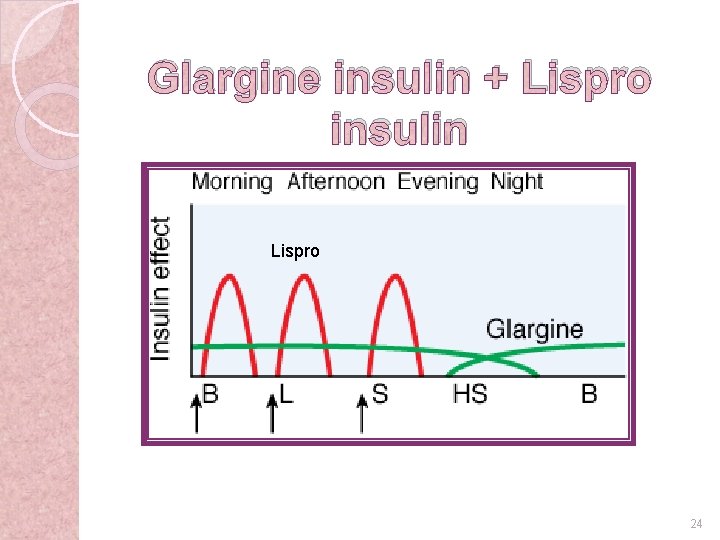
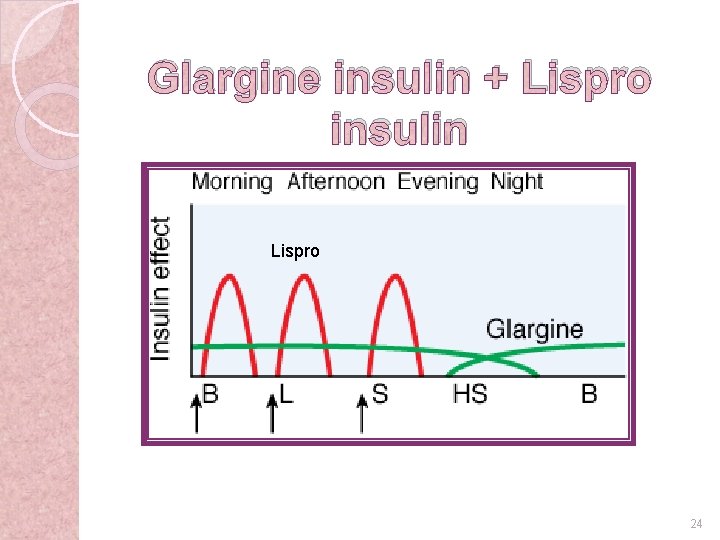
Glargine insulin + Lispro insulin Lispro 24
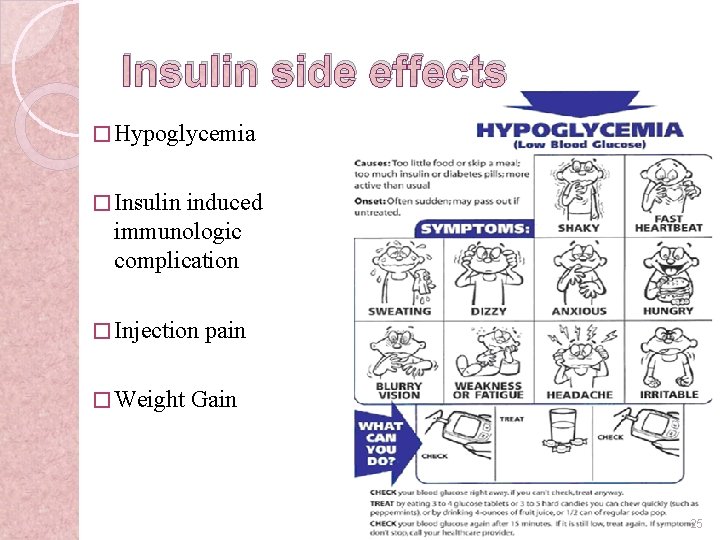
Insulin side effects � Hypoglycemia � Insulin induced immunologic complication � Injection � Weight pain Gain 25
26
Oral antidiabetic drugs �Insulin secretagogues (sulfonylureas) �Biguanide (metformin) �Thiazolidinediones (pioglitazone) �α-glucosidase inhibitors (acarbose) �Most commonly for TM II treatment 27
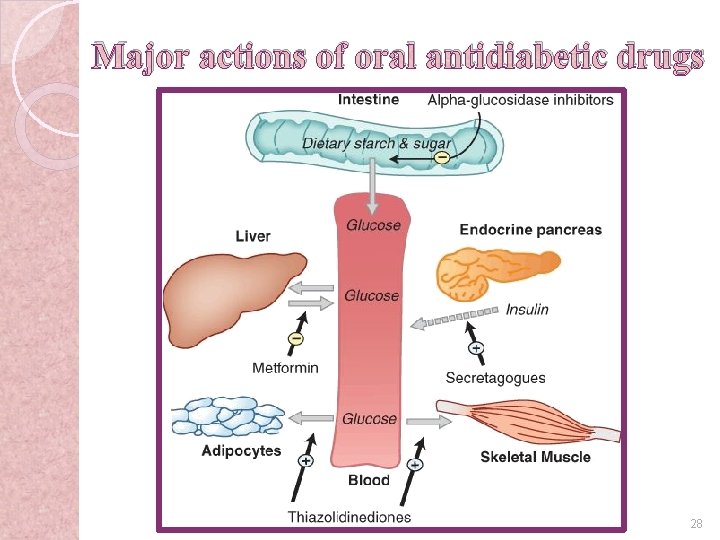
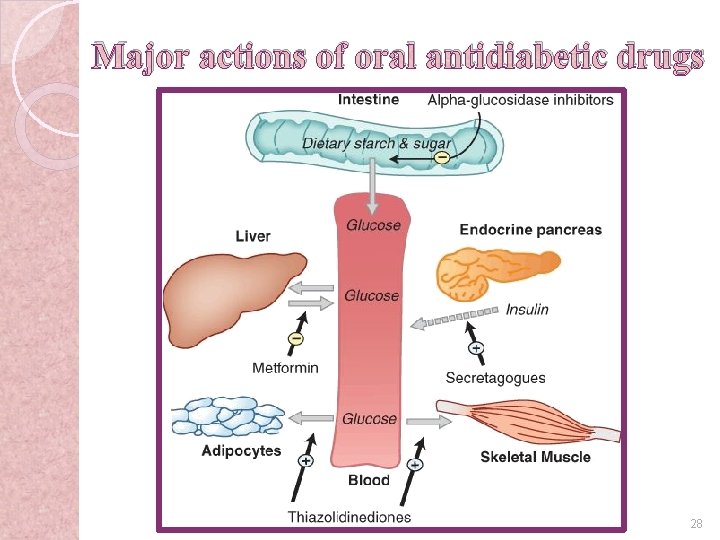
Major actions of oral antidiabetic drugs 28
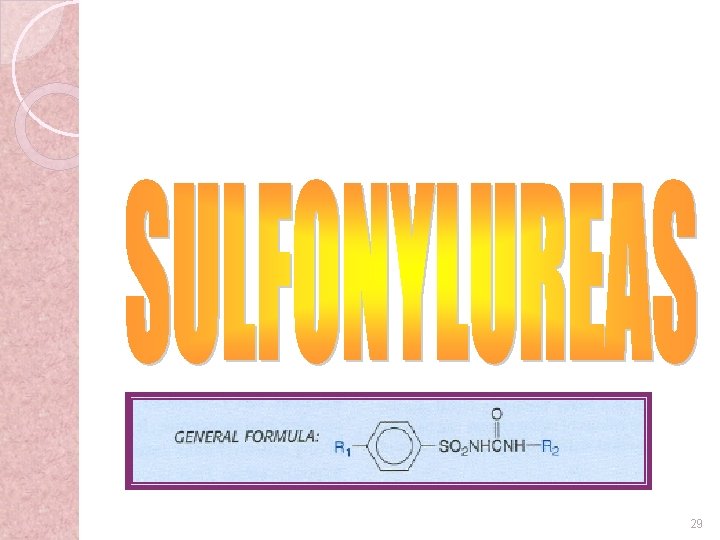
29
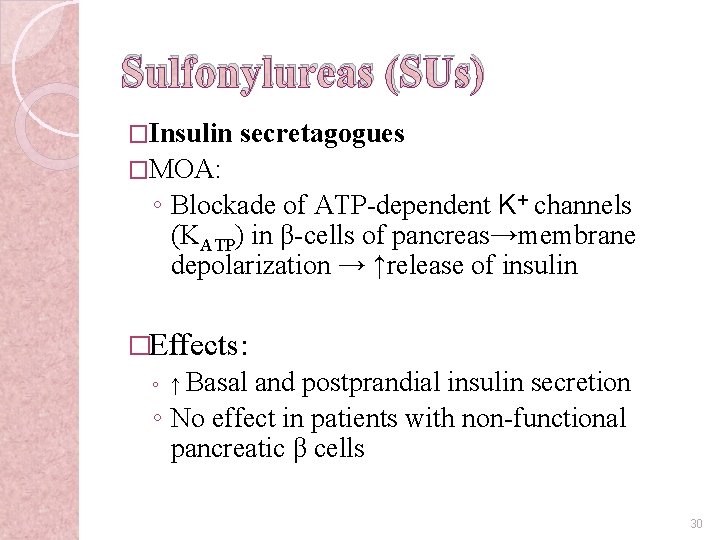
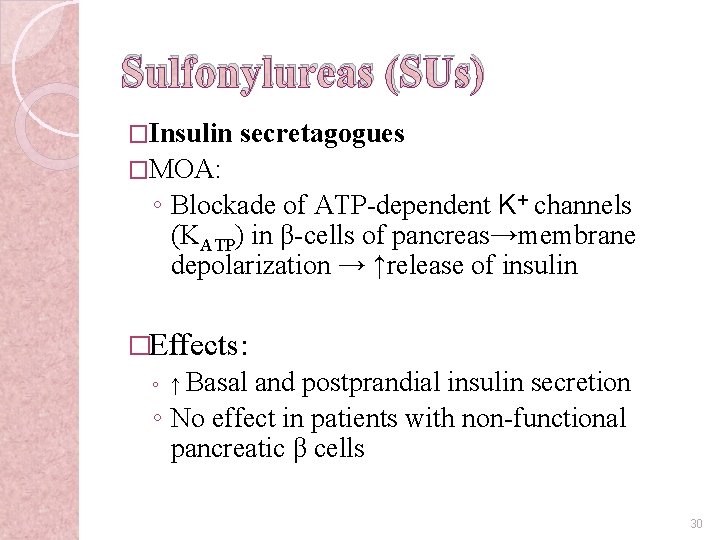
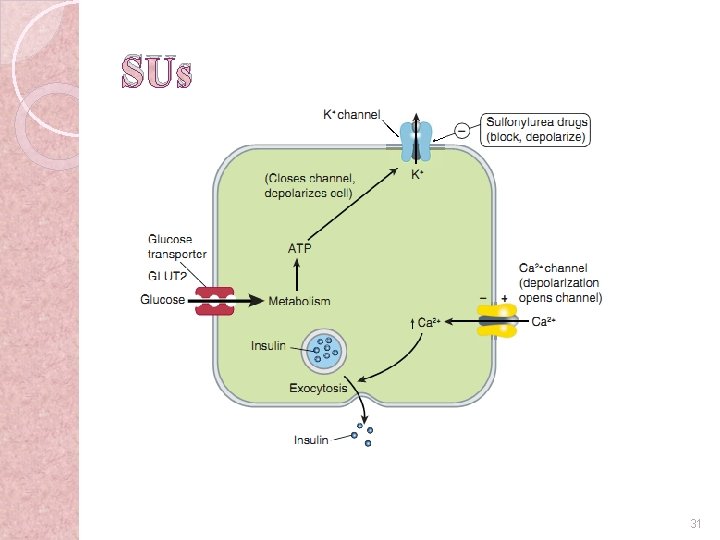
Sulfonylureas (SUs) �Insulin secretagogues �MOA: ◦ Blockade of ATP-dependent K+ channels (KATP) in β-cells of pancreas→membrane depolarization → ↑release of insulin �Effects: ◦ ↑ Basal and postprandial insulin secretion ◦ No effect in patients with non-functional pancreatic β cells 30
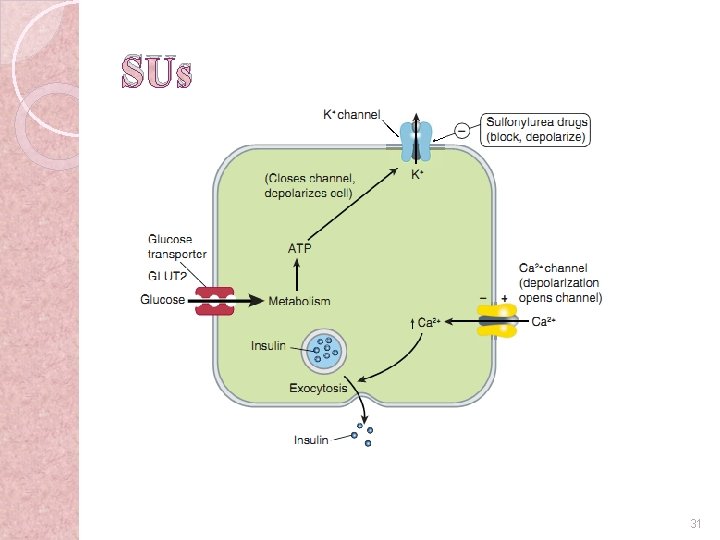
SUs 31
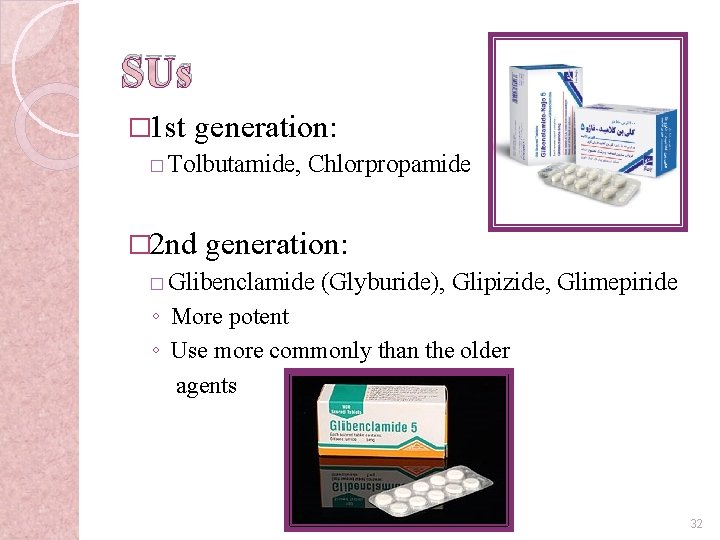
SUs � 1 st generation: � Tolbutamide, Chlorpropamide � 2 nd generation: � Glibenclamide (Glyburide), Glipizide, Glimepiride ◦ More potent ◦ Use more commonly than the older agents 32
SUs �Indication: �Dosing: �Side DM II Once or twice daily effects: ◦ Hypoglycemia ◦ Weight gain 33
34
Biguanides �Metformin �MOA: ◦ ◦ ↓hepatic glucose release ↓gluconeogenesis Enhance peripheral glucose uptake & utilization ↑peripheral tissue sensitivity to insulin �Effects: Enhancement of insulin action, decrease weight �Depends upon: Presence of insulin �Metformin is a euglycemic agent �Slower action 35
Metformin �Indications: ◦ DM II �Dosing: �Side Two to three times daily effects: � Nausea � ↓appetite & weight loss ◦ Lactic acidosis ◦ diarrhea 36

37
α-glucosidase inhibitors �MOA: ◦ Carbohydrate analogs → α-glucosidase inhibition within the intestine → ↓glucose liberation → ↓intestinal glucose absorption → ↓(mild) blood glucose �Acarbose & Miglitol 38

α-glucosidase inhibitors �Effects: ◦ Delays carbohydrate absorption ◦ ↓Postprandial hyperglycemia ◦ No effect on fasting blood sugar and insulin release 39
α-glucosidase inhibitors indications �DM II �Prevent DM II in prediabetics �Must be taken just before a meal �Can be combined with other oral hypoglycemic agents �Dosing: Three times daily (with each meal) 40
α-glucosidase inhibitors side effects �Flatulence � Diarrhea � Abdominal pain 41

42
Thiazolidinediones (glitazones) � Pioglitazone, Rosiglitazone 43
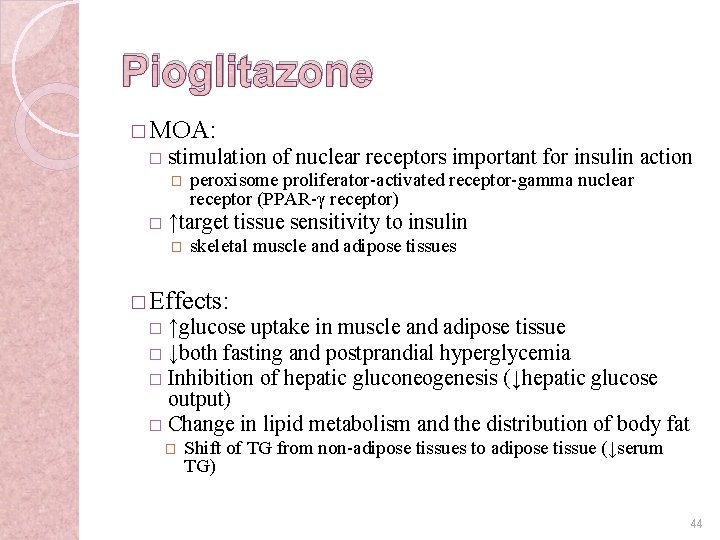
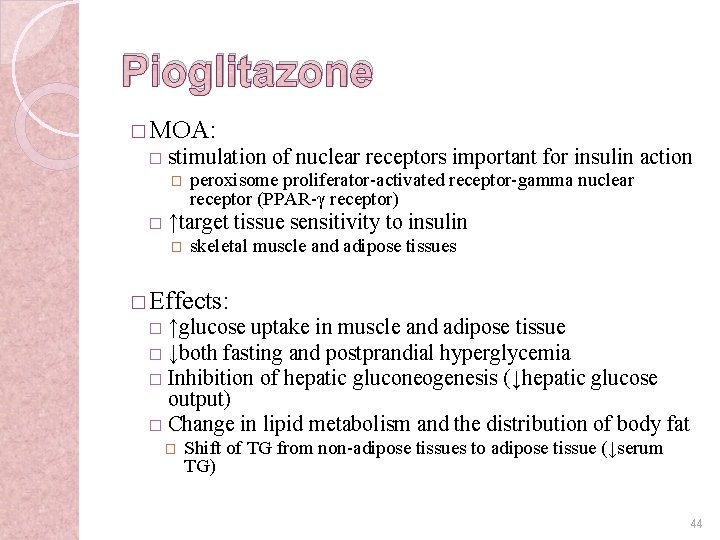
Pioglitazone � MOA: � stimulation of nuclear receptors important for insulin action � � peroxisome proliferator-activated receptor-gamma nuclear receptor (PPAR-γ receptor) ↑target tissue sensitivity to insulin � skeletal muscle and adipose tissues � Effects: ↑glucose uptake in muscle and adipose tissue � ↓both fasting and postprandial hyperglycemia � Inhibition of hepatic gluconeogenesis (↓hepatic glucose output) � Change in lipid metabolism and the distribution of body fat � � Shift of TG from non-adipose tissues to adipose tissue (↓serum TG) 44
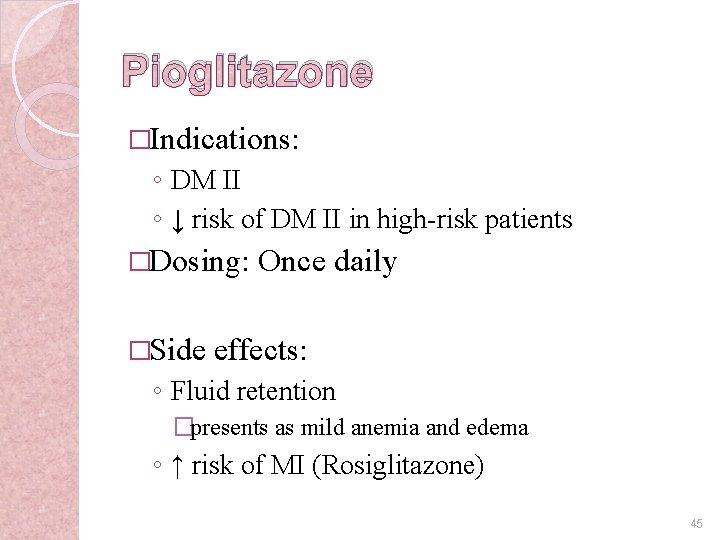
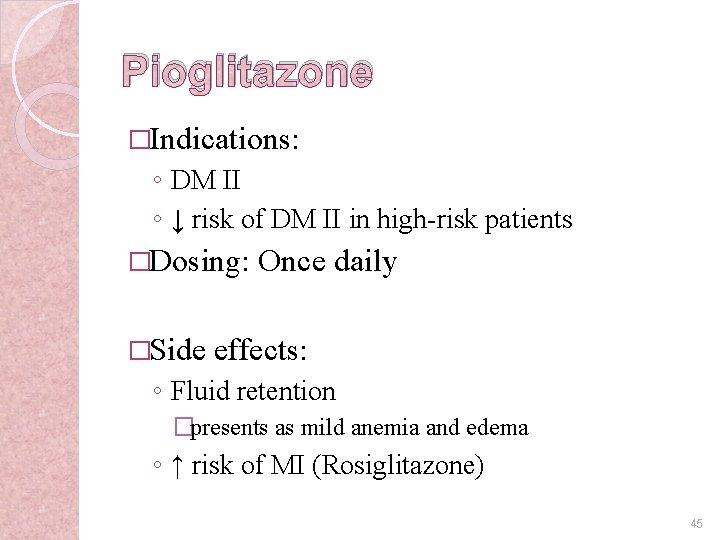
Pioglitazone �Indications: ◦ DM II ◦ ↓ risk of DM II in high-risk patients �Dosing: �Side Once daily effects: ◦ Fluid retention �presents as mild anemia and edema ◦ ↑ risk of MI (Rosiglitazone) 45

Any question? 46