Drugs for Epilepsy Elsevier Inc items and derived
![Phenytoin [Dilantin] • Especially effective against partial and tonic-clonic seizures • Mechanism of action: Phenytoin [Dilantin] • Especially effective against partial and tonic-clonic seizures • Mechanism of action:](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-13.jpg)
![Carbamazepine [Tegretol] • Uses: – Epilepsy – Bipolar disorder – Trigeminal and glossopharyngeal neuralgias Carbamazepine [Tegretol] • Uses: – Epilepsy – Bipolar disorder – Trigeminal and glossopharyngeal neuralgias](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-19.jpg)
![Valproic Acid [Depakene, Depakote, Depacon] • Uses – Seizure disorders – Bipolar disorder – Valproic Acid [Depakene, Depakote, Depacon] • Uses – Seizure disorders – Bipolar disorder –](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-20.jpg)
- Slides: 34
Drugs for Epilepsy Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 1
Epilepsy: new definition as of 2014 Diagnosis of epilepsy: a person is considered to have epilepsy if he or she meets any of the following conditions: • At least two unprovoked (or reflex) seizures occurring greater than 24 hours apart. • One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years. Diagnosis of an epilepsy syndrome – Epilepsy is considered to be resolved for individuals who had an age-dependent epilepsy syndrome but are now past the applicable age, or those who have remained seizure-free for the last 10 years, with no seizure medicines for the last 5 years. • Fisher RS et al. A practical clinical definition of epilepsy, Epilepsia 2014; 55: 475 -482. This definition was also adopted as a position of the International League Against Epilepsy (ILAE). 2
Epilepsy: overview • ‘Umbrella term’ for a group of heterogeneous disorders characterized by excessive excitability of neurons in the CNS • All seizures are caused by abnormal electrical disturbances in the brain. • Different kinds of seizures – May present with a range of symptoms from as subtle as a blank stare… to as marked as unconsciousness or convulsions • In U. S. 2. 3 million people have epilepsy • Incidence is highest during the 1 st year of life and in the elderly • Between 60 -70% of patients can be seizure-free with drug therapy. 3 Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc.
Seizures: what is the focus? • Definition. . The seizure focus is the site in the brain from which the seizure originated. • Seizures arise from many possible conditions, such as: • Congenital defects • Hypoxia at birth • Head trauma • Cancer • And more 4
Seizures: what is the focus? The symptoms of any particular seizure depend on the location in the brain of the seizure focus Where are the hyperexcitable neurons located? − More limited part of the brain partial or local seizure − Larger portion of the brain generalized seizure Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 5
Seizures: Types • Partial (focal) seizures – Simple partial – Complex partial – Secondarily generalized • Generalized seizures – Tonic-clonic (grand mal) – Absence (petit mal) – Atonic – Myoclonic – Status epilepticus (SE) – Febrile Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 6
Antiepileptic Drugs (aka AEDs, or “antiseizure medications”) • Effects: – Suppress discharge of neurons within a seizure focus – Suppress propagation of seizure activity from the focus to other areas of the brain • Mechanisms of action involving: – Sodium – Calcium – Glutamate – GABA – (potassium? ) Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 7
Therapeutic Goals • Treatment goal: seizures to an extent that allows patient to live a normal life * Balance seizure control vs. acceptability of undesired side effects • Non-drug treatment options: – Neurosurgery (best success rate) – Vagal nerve stimulation – Ketogenic diet Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 8
Therapeutic Goals, cont’d • Diagnosis and drug selection – Most AEDs selective for specific seizure disorders – Must accurately diagnose seizure & then treat with AED that treats that type of seizure * May have to try several AEDs before an effective regimen can be established Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 9
Therapeutic Goals, cont’d • Drug evaluation – Trial period – Need to determine effectiveness – Frequent dosage adjustment may be needed • Patient teaching • Monitoring plasma drug levels – Traditional AEDs vs. newer AEDs – Helpful in major convulsive disorders – Less helpful for absence seizures Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 10
Therapeutic Considerations • Promoting patient adherence *Seizure control dependent on patient compliance • Withdrawing antiepileptic drugs – Spontaneous remission – Withdraw slowly over a period of 6 weeks to several months Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 11
Classifications of Antiepileptic Drugs Two major categories: Both equally effective – neither group superior • Traditional antiepileptic drugs (AEDs) – phenytoin – carbamazepine – valproic acid – and others • Newer AEDs – oxcarbazepine – Lamotrigine – Levetiracetam – and others Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 12
![Phenytoin Dilantin Especially effective against partial and tonicclonic seizures Mechanism of action Phenytoin [Dilantin] • Especially effective against partial and tonic-clonic seizures • Mechanism of action:](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-13.jpg)
Phenytoin [Dilantin] • Especially effective against partial and tonic-clonic seizures • Mechanism of action: selective inhibition of sodium channels • Varied oral absorption • Half-life: 8 to 60 hours • Dosage is highly individualized Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 13
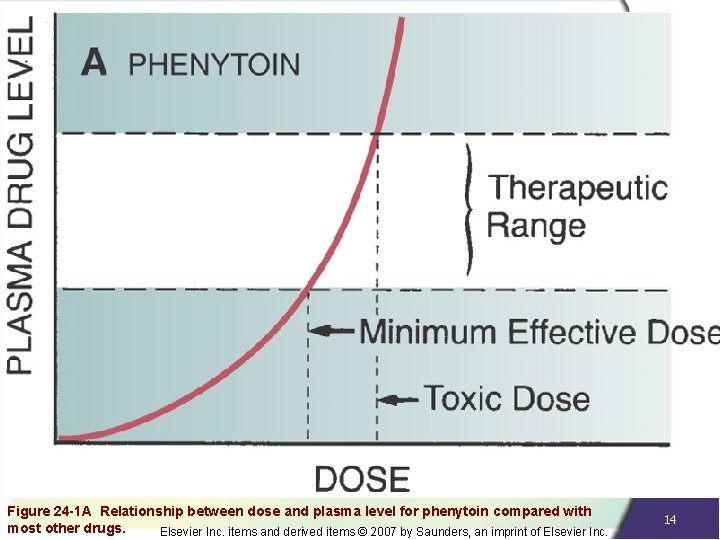
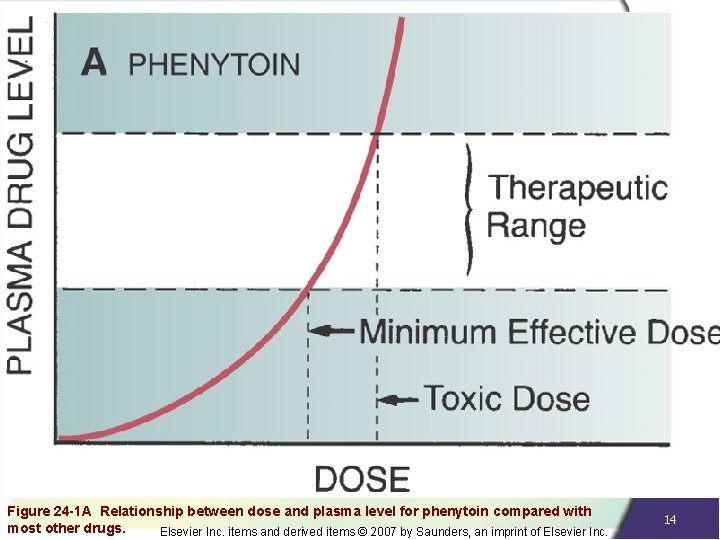
Figure 24 -1 A Relationship between dose and plasma level for phenytoin compared with most other drugs. Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 14
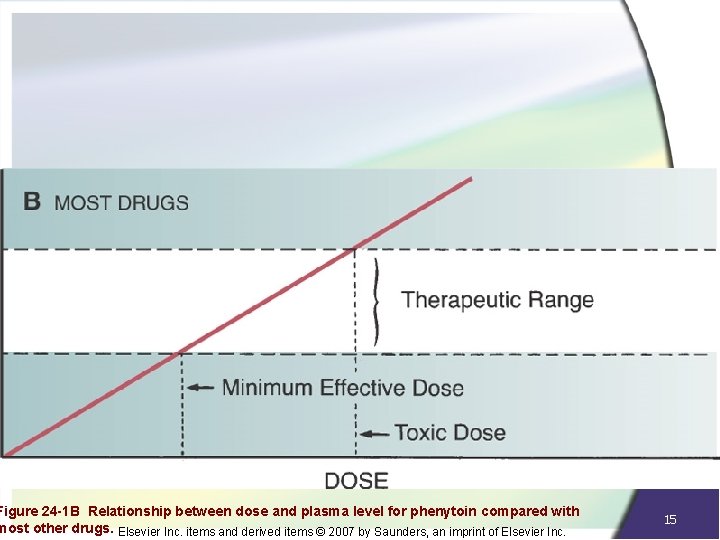
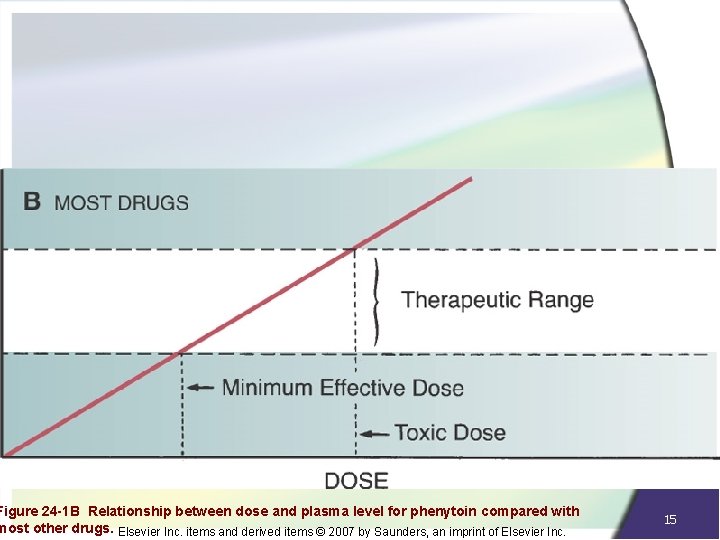
Figure 24 -1 B Relationship between dose and plasma level for phenytoin compared with most other drugs. Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 15
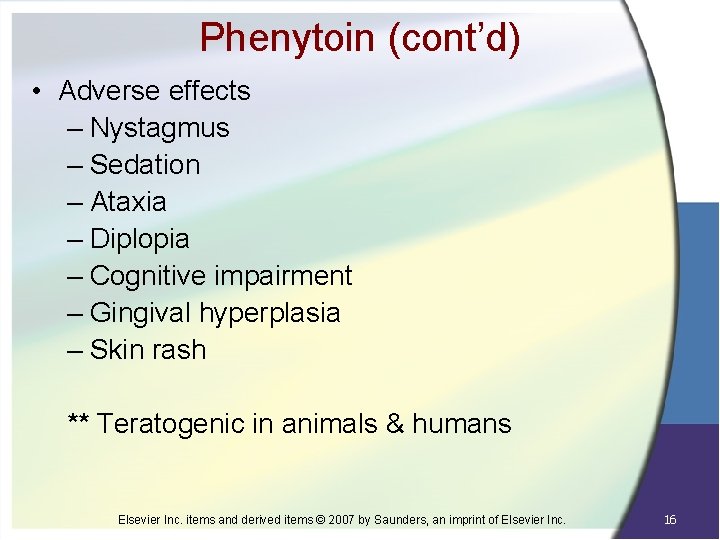
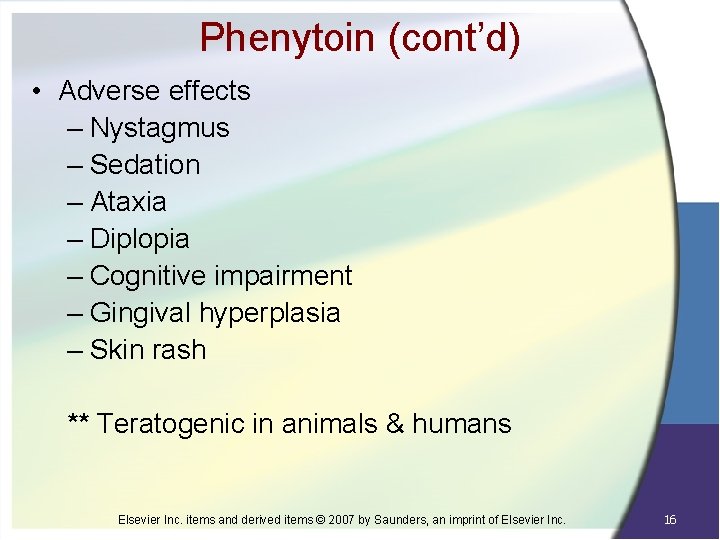
Phenytoin (cont’d) • Adverse effects – Nystagmus – Sedation – Ataxia – Diplopia – Cognitive impairment – Gingival hyperplasia – Skin rash ** Teratogenic in animals & humans Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 16
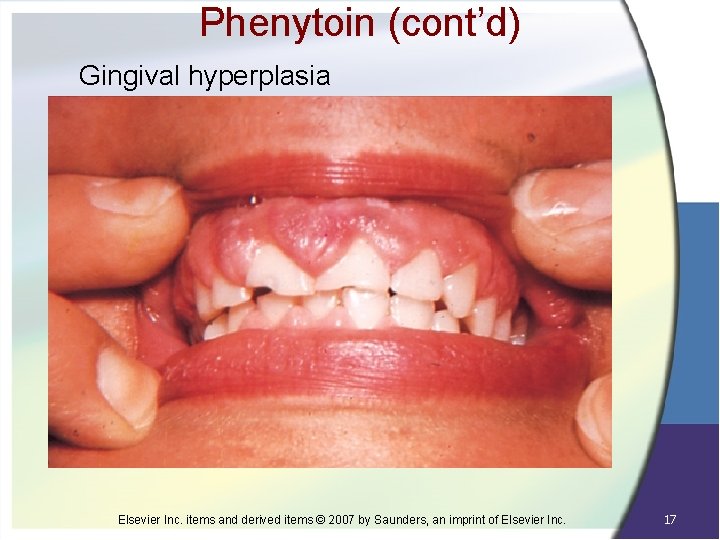
Phenytoin (cont’d) Gingival hyperplasia Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 17
Phenytoin (cont’d) • Drug interactions – Decreases the effects of oral contraceptives, warfarin, and glucocorticoids – Increases levels of diazepam, isoniazid, cimetidine, alcohol, valproic acid Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 18
![Carbamazepine Tegretol Uses Epilepsy Bipolar disorder Trigeminal and glossopharyngeal neuralgias Carbamazepine [Tegretol] • Uses: – Epilepsy – Bipolar disorder – Trigeminal and glossopharyngeal neuralgias](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-19.jpg)
Carbamazepine [Tegretol] • Uses: – Epilepsy – Bipolar disorder – Trigeminal and glossopharyngeal neuralgias • Mechanism of action • Adverse effects – Neurologic effects: nystagmus, ataxia – Hematologic effects: leukopenia, anemia, thrombocytopenia – Dermatologic effects: rash, photosensitivity reactions Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 19
![Valproic Acid Depakene Depakote Depacon Uses Seizure disorders Bipolar disorder Valproic Acid [Depakene, Depakote, Depacon] • Uses – Seizure disorders – Bipolar disorder –](https://slidetodoc.com/presentation_image_h/1f4b352d82d02709fd861fb85185a1a6/image-20.jpg)
Valproic Acid [Depakene, Depakote, Depacon] • Uses – Seizure disorders – Bipolar disorder – Migraine • MOA • Adverse effects – GI effects – Hepatotoxicity: liver failure – Pancreatitis Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 20
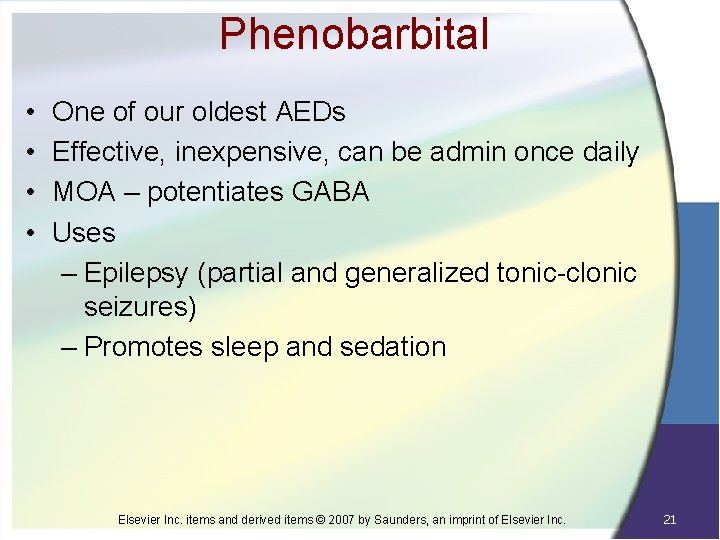
Phenobarbital • • One of our oldest AEDs Effective, inexpensive, can be admin once daily MOA – potentiates GABA Uses – Epilepsy (partial and generalized tonic-clonic seizures) – Promotes sleep and sedation Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 21
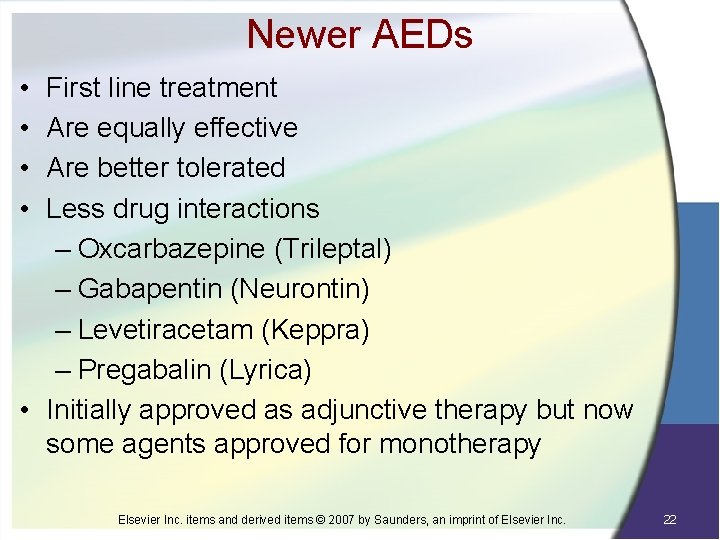
Newer AEDs • • First line treatment Are equally effective Are better tolerated Less drug interactions – Oxcarbazepine (Trileptal) – Gabapentin (Neurontin) – Levetiracetam (Keppra) – Pregabalin (Lyrica) • Initially approved as adjunctive therapy but now some agents approved for monotherapy Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 22
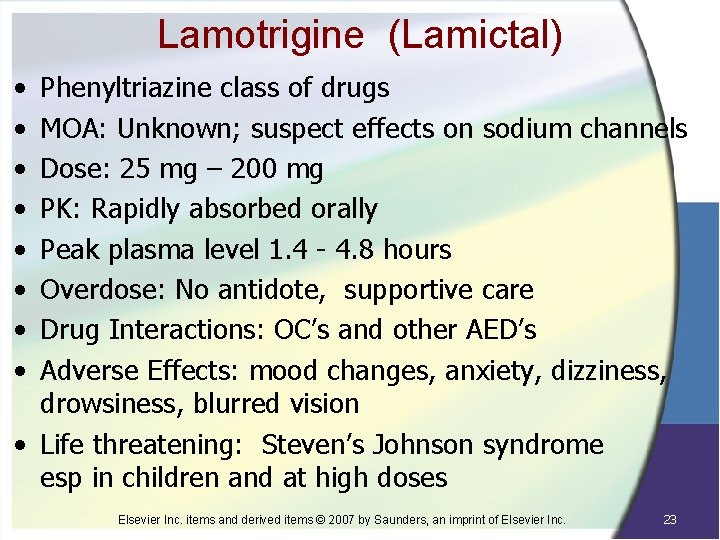
Lamotrigine (Lamictal) • • Phenyltriazine class of drugs MOA: Unknown; suspect effects on sodium channels Dose: 25 mg – 200 mg PK: Rapidly absorbed orally Peak plasma level 1. 4 - 4. 8 hours Overdose: No antidote, supportive care Drug Interactions: OC’s and other AED’s Adverse Effects: mood changes, anxiety, dizziness, drowsiness, blurred vision • Life threatening: Steven’s Johnson syndrome esp in children and at high doses Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 23
Alzheimer’s Disease 24
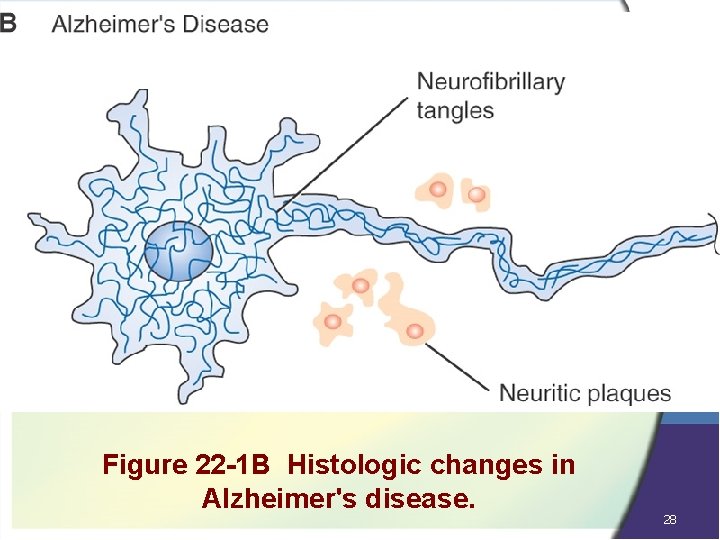
Alzheimer’s Disease Pathophysiology • Degeneration of neurons – Role of hippocampus → Important role in memory – Role of cerebral cortex → Speech, perception, reasoning, higher functioning • Reduced cholinergic transmission – In advanced disease, levels of ACh are 90% below normal • Beta-amyloid and neuritic plaques – Form outside of neurons esp. hippocampus and cortex causing neuronal injury 25
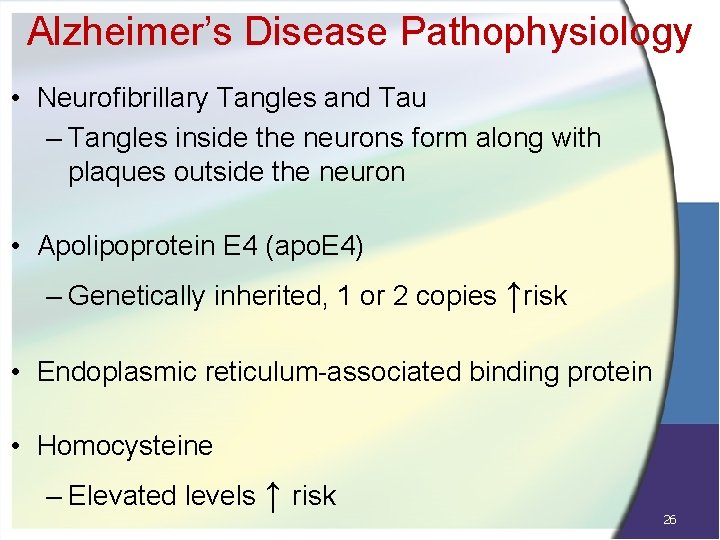
Alzheimer’s Disease Pathophysiology • Neurofibrillary Tangles and Tau – Tangles inside the neurons form along with plaques outside the neuron • Apolipoprotein E 4 (apo. E 4) – Genetically inherited, 1 or 2 copies ↑risk • Endoplasmic reticulum-associated binding protein • Homocysteine – Elevated levels ↑ risk 26
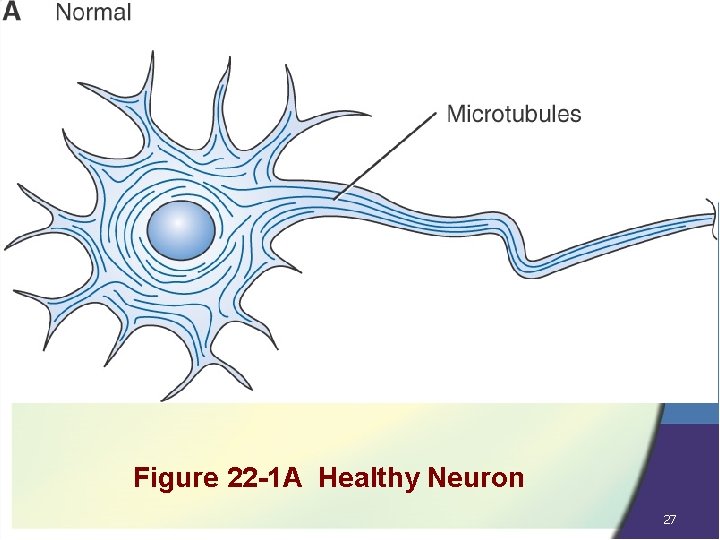
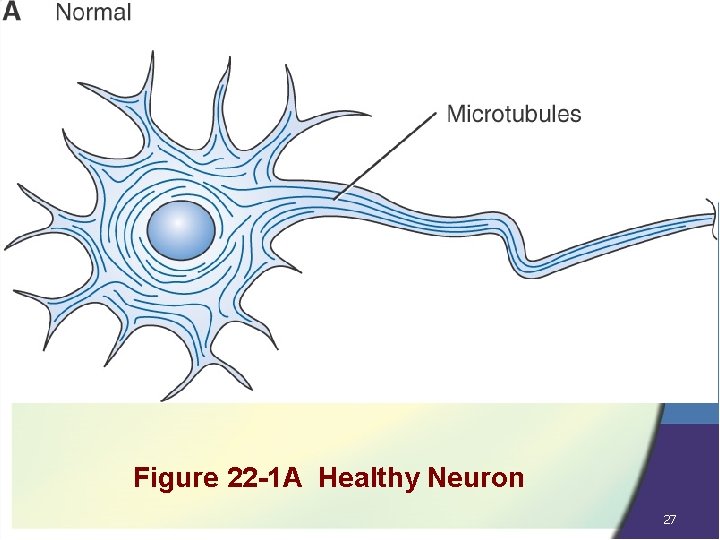
Figure 22 -1 A Healthy Neuron 27
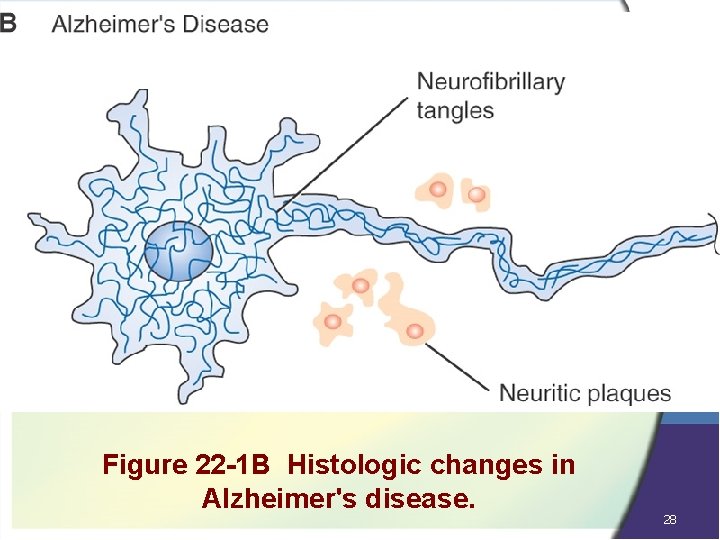
Figure 22 -1 B Histologic changes in Alzheimer's disease. 28
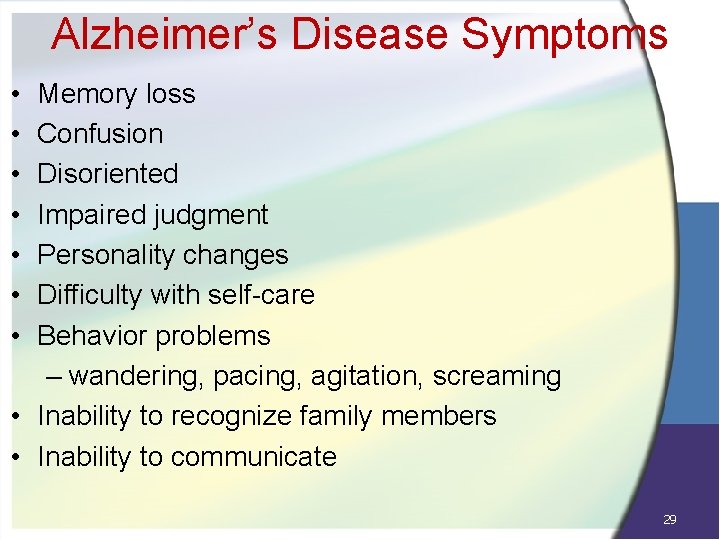
Alzheimer’s Disease Symptoms • • Memory loss Confusion Disoriented Impaired judgment Personality changes Difficulty with self-care Behavior problems – wandering, pacing, agitation, screaming • Inability to recognize family members • Inability to communicate 29
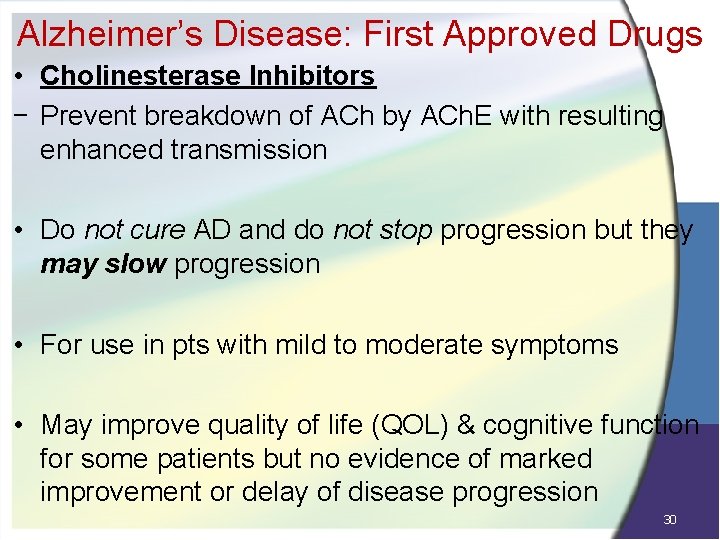
Alzheimer’s Disease: First Approved Drugs • Cholinesterase Inhibitors − Prevent breakdown of ACh by ACh. E with resulting enhanced transmission • Do not cure AD and do not stop progression but they may slow progression • For use in pts with mild to moderate symptoms • May improve quality of life (QOL) & cognitive function for some patients but no evidence of marked improvement or delay of disease progression 30
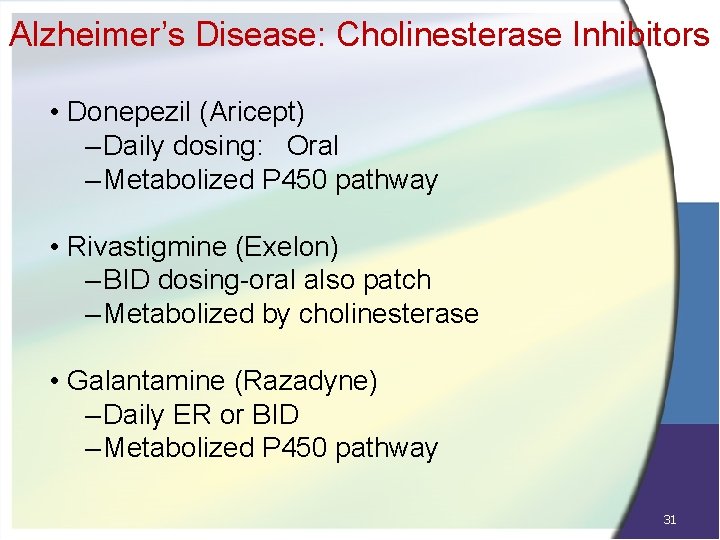
Alzheimer’s Disease: Cholinesterase Inhibitors • Donepezil (Aricept) – Daily dosing: Oral – Metabolized P 450 pathway • Rivastigmine (Exelon) – BID dosing-oral also patch – Metabolized by cholinesterase • Galantamine (Razadyne) – Daily ER or BID – Metabolized P 450 pathway 31
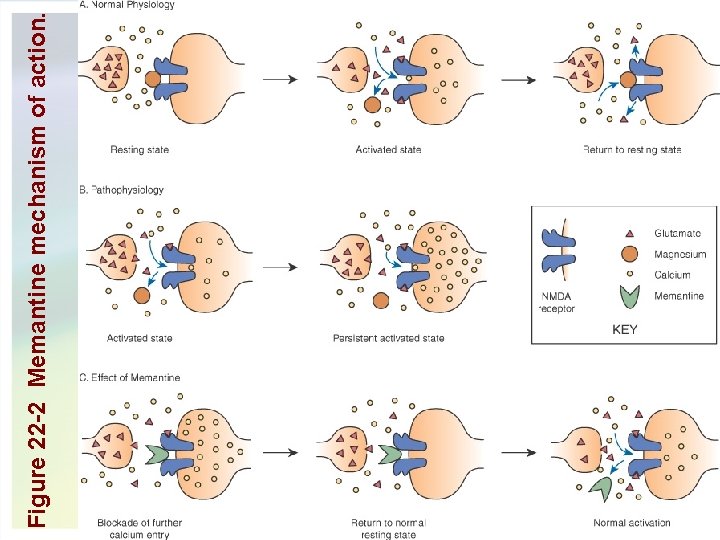
Alzheimer’s Disease: NMDA Antagonist • NMDA receptor antagonists (N-methyl-D-aspartate) • MOA: Modulates glutamate at NMDA receptors promoting calcium influx, thereby increasing signaling • NMDA receptors believed to play a critical role in learning and memory • Memantine (Namenda) – Indicated for moderate to severe AD – Half life 60 -80 hours – Dizziness, Headache, Confusion – Dose 5 - 21 mg depending on formulation 32
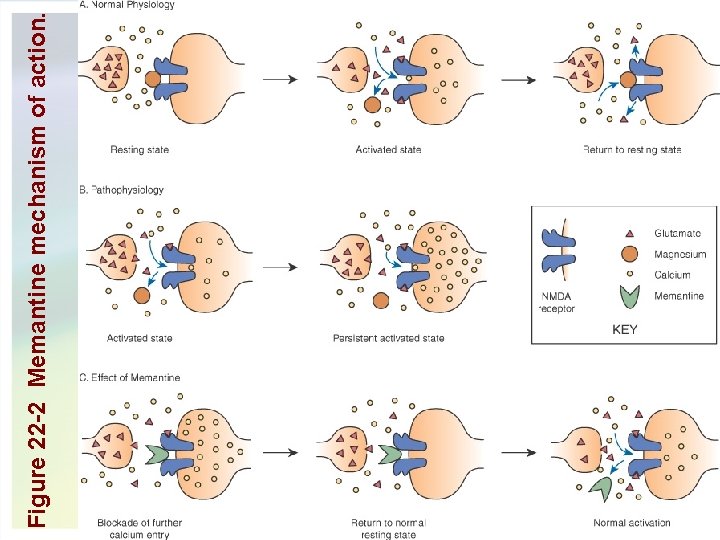
Figure 22 -2 Memantine mechanism of action. 33
Questions? Elsevier Inc. items and derived items © 2007 by Saunders, an imprint of Elsevier Inc. 34