Dr Ozra Akha Endocrinologist faculty of Mazandaran university








- Slides: 30

Dr. Ozra. Akha Endocrinologist faculty of Mazandaran university 2
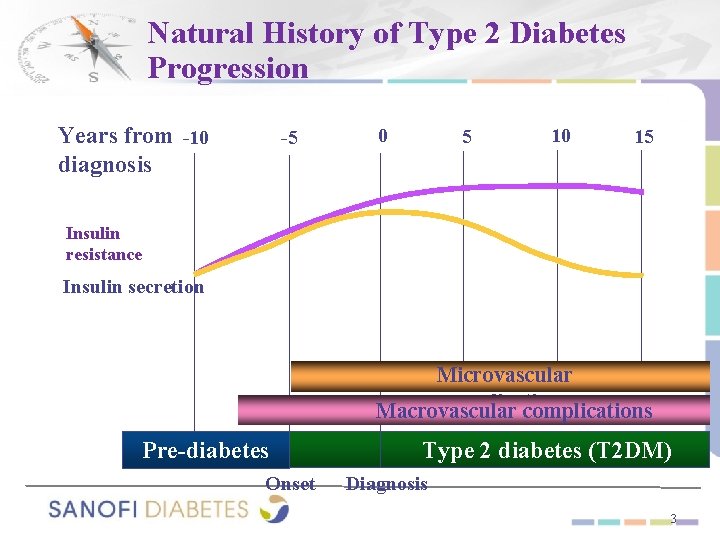
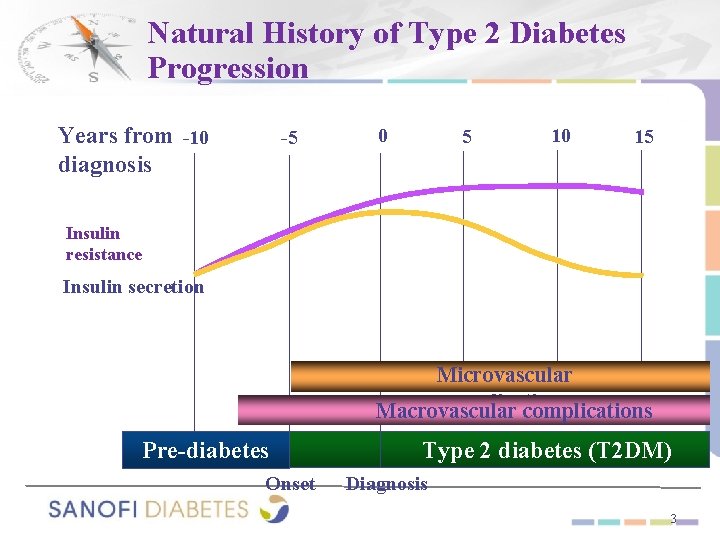
Natural History of Type 2 Diabetes Progression Years from -10 diagnosis -5 0 5 10 15 Insulin resistance Insulin secretion Microvascular complications Macrovascular complications Pre-diabetes Onset Type 2 diabetes (T 2 DM) Diagnosis 3
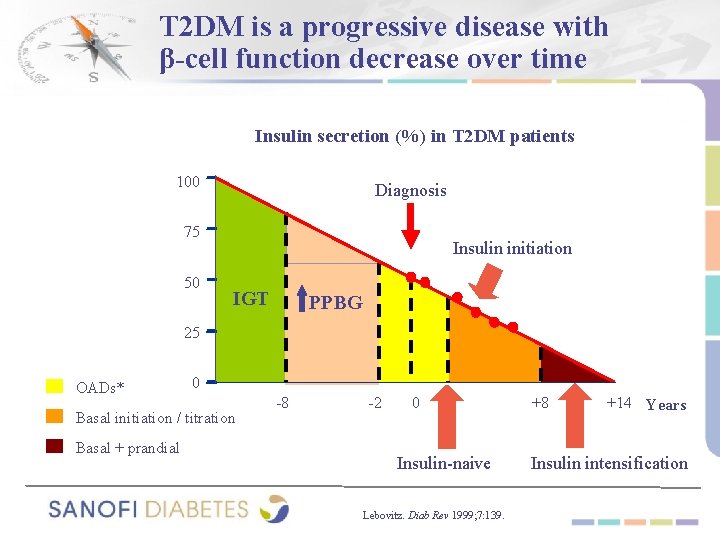
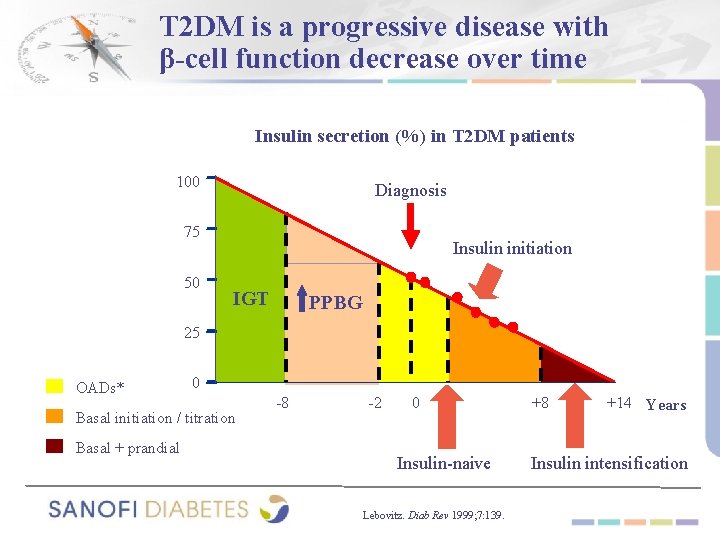
T 2 DM is a progressive disease with β-cell function decrease over time Insulin secretion (%) in T 2 DM patients 100 Diagnosis 75 50 Insulin initiation IGT PPBG 25 OADs* 0 Basal initiation / titration Basal + prandial -8 -2 0 + 2 Insulin-naive Lebovitz. Diab Rev 1999; 7: 139. +8 +14 Years Insulin intensification
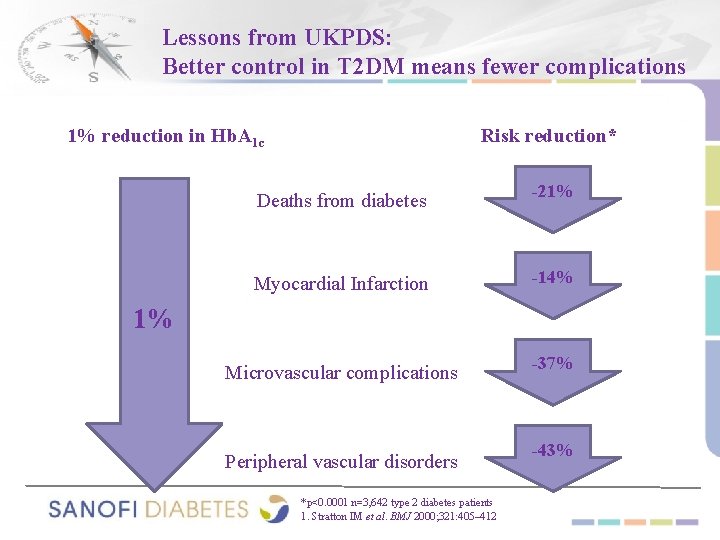
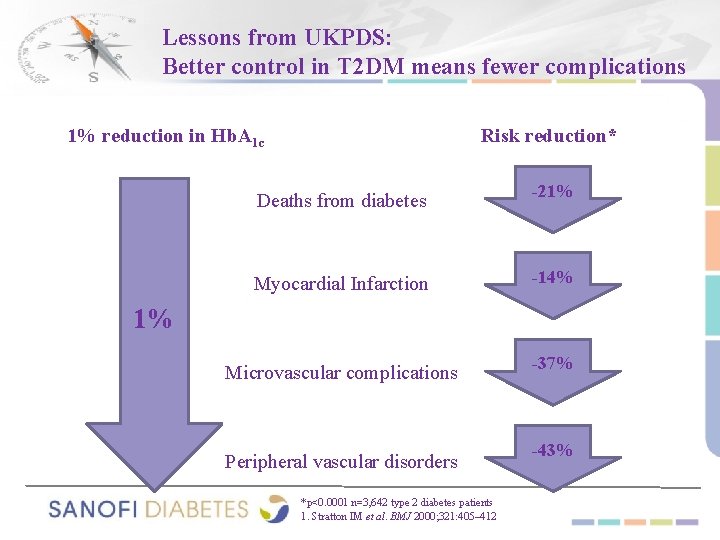
Lessons from UKPDS: Better control in T 2 DM means fewer complications 1% reduction in Hb. A 1 c Risk reduction* Deaths from diabetes -21% Myocardial Infarction -14% Microvascular complications -37% 1% Peripheral vascular disorders *p<0. 0001 n=3, 642 type 2 diabetes patients 1. Stratton IM et al. BMJ 2000; 321: 405– 412 -43%

Risk of Microvascular Complications vs. A 1 C in Type 1 Diabetes Results From the DCCT 20 Retinopathy progression Neuropathy progression Microalbuminuria progression 15 Relative risk 10 5 0 1 5 6 7 8 9 10 A 1 C (%) Skyler JS. Endocrinol Metab Clin North Am. 1996; 25: 243 -254 11 12
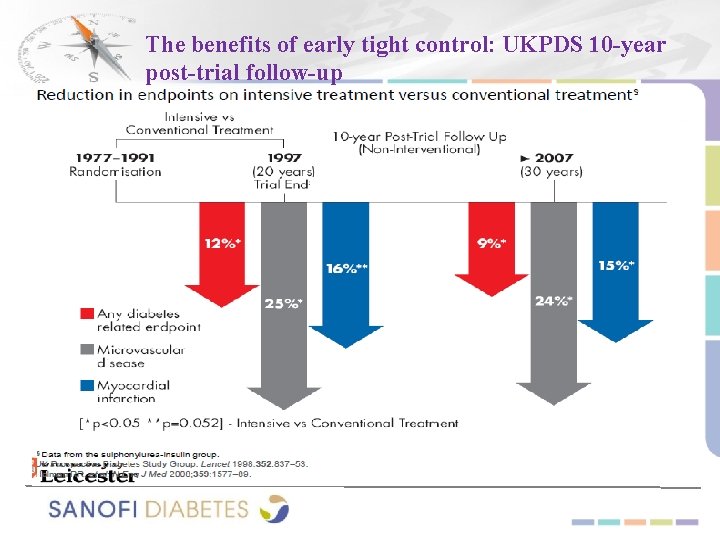
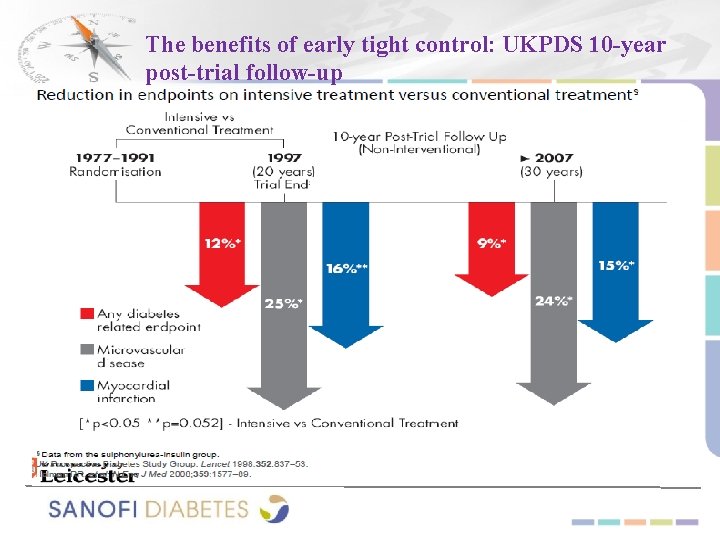
The benefits of early tight control: UKPDS 10 -year post-trial follow-up
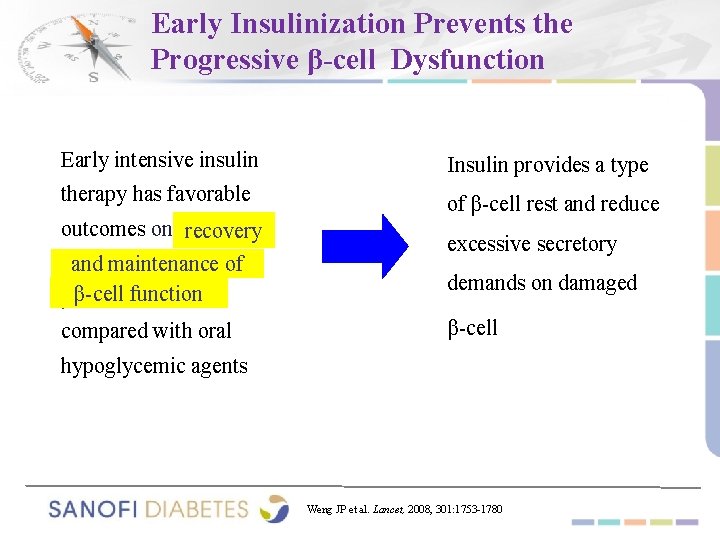
Early Insulinization Prevents the Progressive β-cell Dysfunction Early intensive insulin Insulin provides a type therapy has favorable of β-cell rest and reduce outcomes on recovery andmaintenanceofof β-cellfunction β-cell compared with oral excessive secretory demands on damaged β-cell hypoglycemic agents Weng JP et al. Lancet, 2008, 301: 1753 -1780
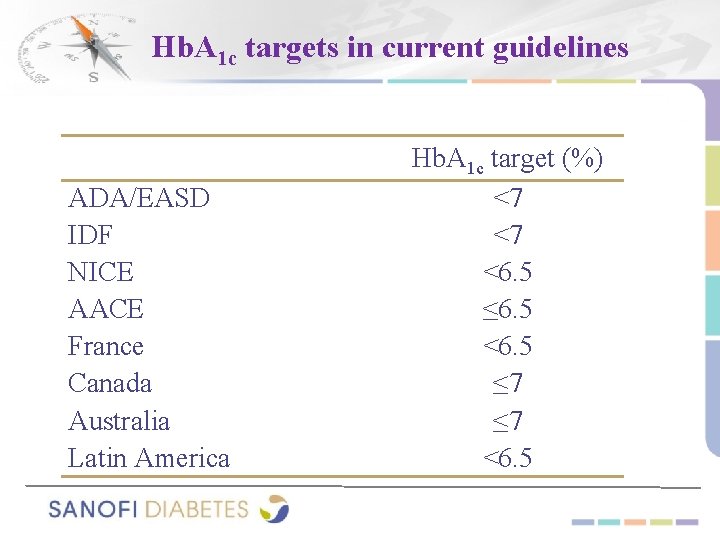
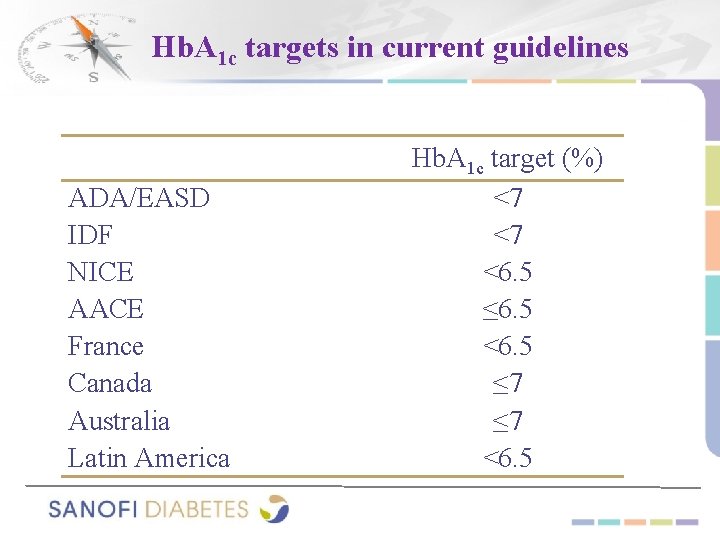
Hb. A 1 c targets in current guidelines ADA/EASD IDF NICE AACE France Canada Australia Latin America Hb. A 1 c target (%) <7 <7 <6. 5 ≤ 6. 5 <6. 5 ≤ 7 <6. 5
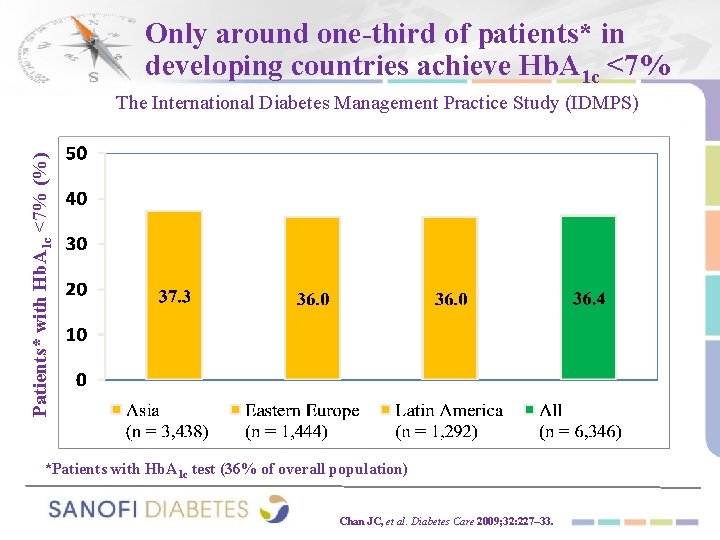
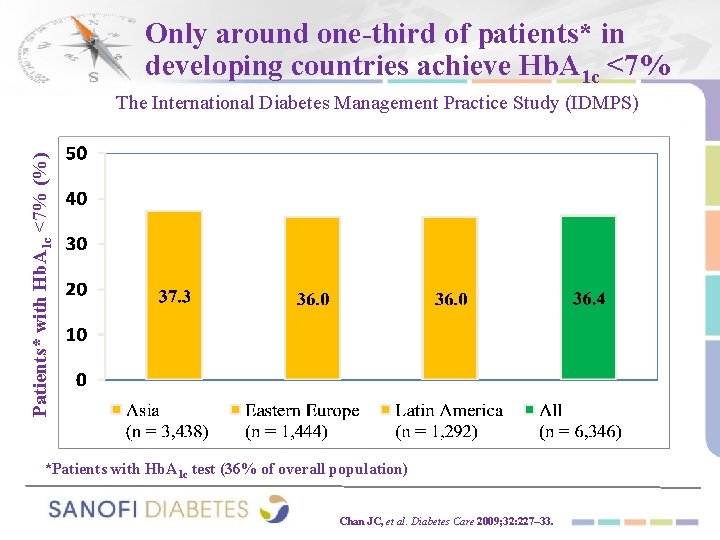
Only around one-third of patients* in developing countries achieve Hb. A 1 c <7% Patients* with Hb. A 1 c <7% (%) The International Diabetes Management Practice Study (IDMPS) *Patients with Hb. A 1 c test (36% of overall population) Chan JC, et al. Diabetes Care 2009; 32: 227– 33.
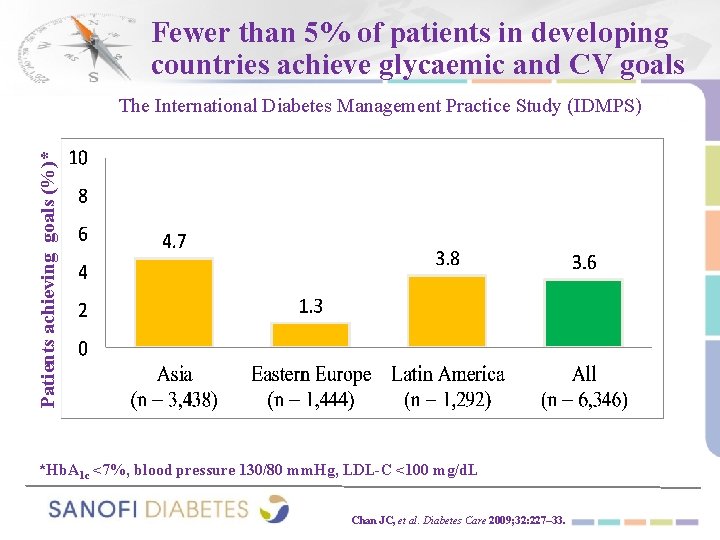
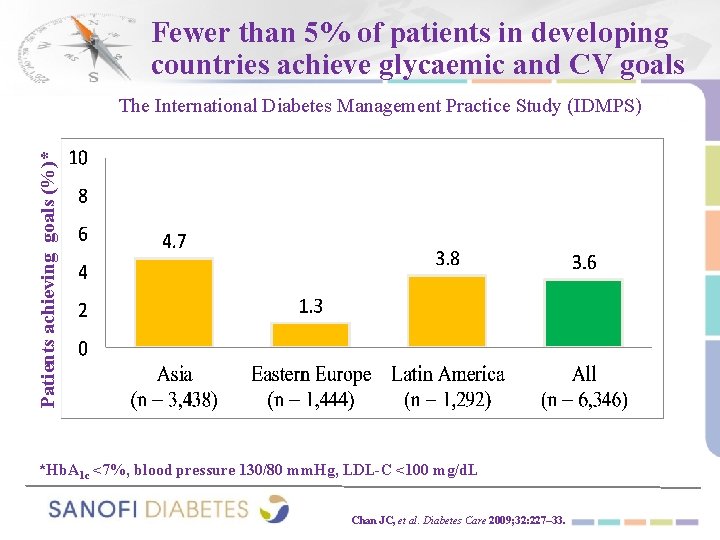
Fewer than 5% of patients in developing countries achieve glycaemic and CV goals Patients achieving goals (%)* The International Diabetes Management Practice Study (IDMPS) *Hb. A 1 c <7%, blood pressure 130/80 mm. Hg, LDL-C <100 mg/d. L Chan JC, et al. Diabetes Care 2009; 32: 227– 33.
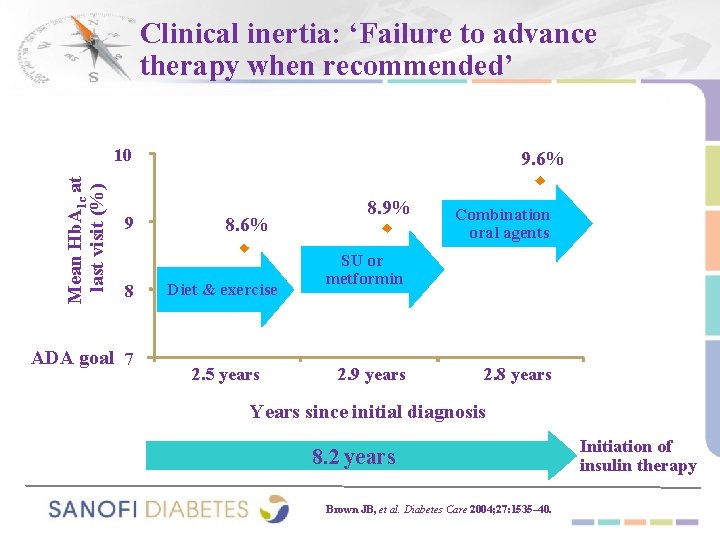
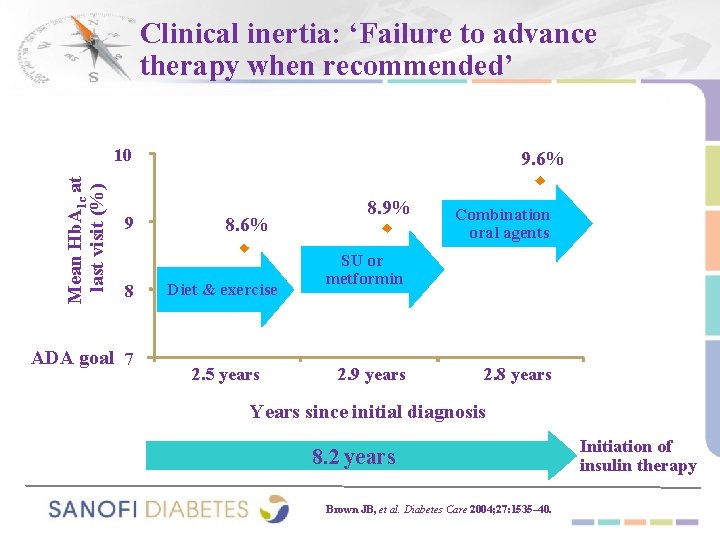
Clinical inertia: ‘Failure to advance therapy when recommended’ Mean Hb. A 1 c at last visit (%) 10 9 8 ADA goal 7 9. 6% 8. 6% Diet & exercise 2. 5 years 8. 9% Combination oral agents SU or metformin 2. 9 years 2. 8 years Years since initial diagnosis 8. 2 years Brown JB, et al. Diabetes Care 2004; 27: 1535– 40. Initiation of insulin therapy
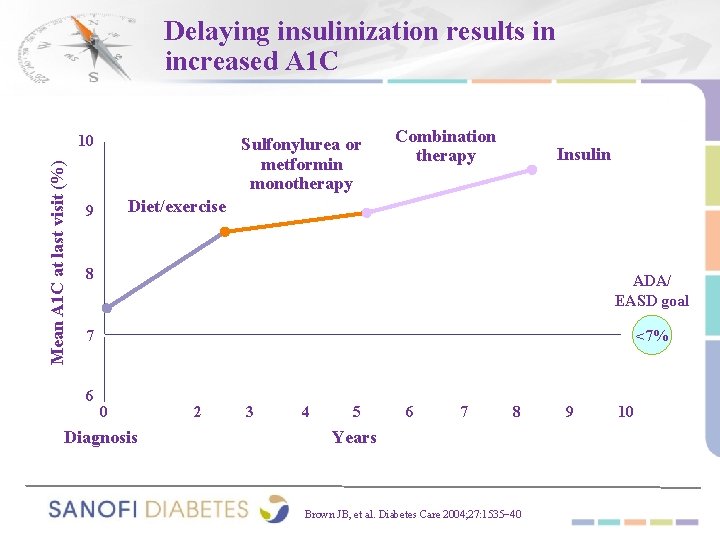
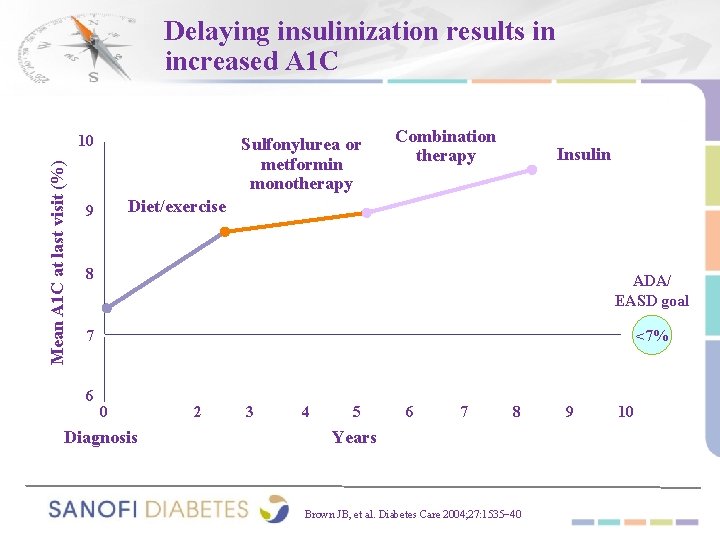
Delaying insulinization results in increased A 1 C Mean A 1 C at last visit (%) 10 Sulfonylurea or metformin monotherapy Combination therapy Insulin Diet/exercise 9 8 ADA/ EASD goal 7 <7% 6 0 Diagnosis 2 3 4 5 6 7 8 Years Brown JB, et al. Diabetes Care 2004; 27: 1535− 40 9 10
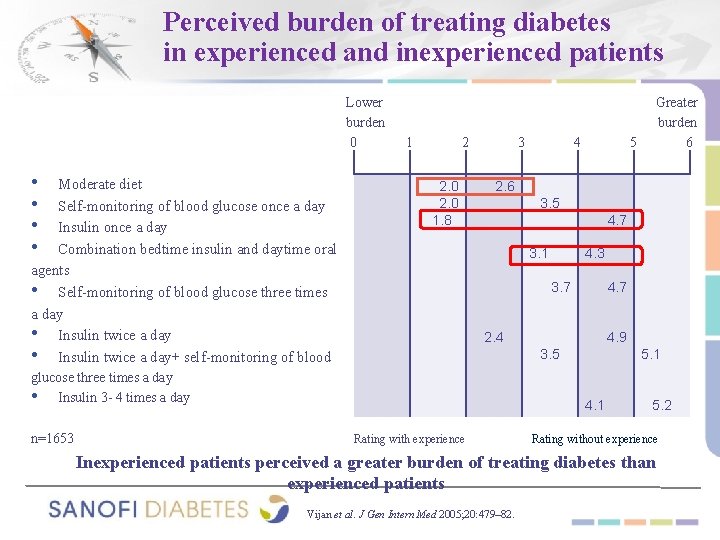
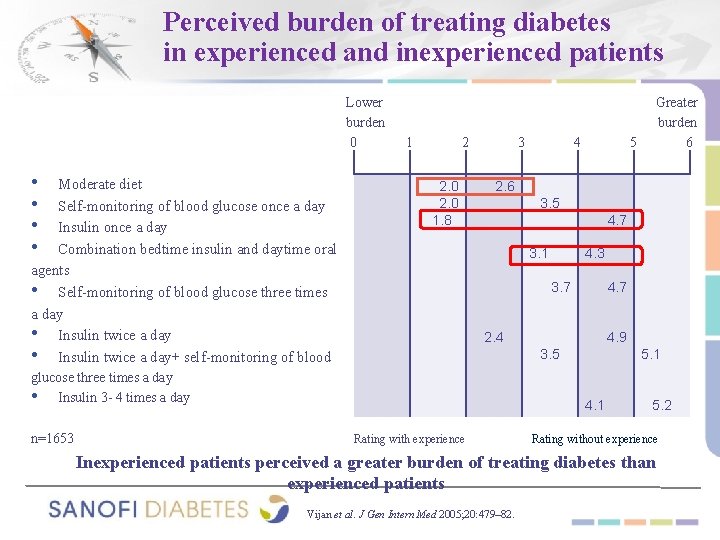
Perceived burden of treating diabetes in experienced and inexperienced patients Lower burden 0 • • Moderate diet Self-monitoring of blood glucose once a day Insulin once a day Combination bedtime insulin and daytime oral agents • Self-monitoring of blood glucose three times a day • Insulin twice a day+ self-monitoring of blood 1 2 2. 0 1. 8 3 5 2. 6 3. 5 4. 7 3. 1 4. 3 3. 7 4. 7 2. 4 4. 9 3. 5 glucose three times a day • Insulin 3 - 4 times a day n=1653 4 Greater burden 6 5. 1 4. 1 Rating with experience 5. 2 Rating without experience Inexperienced patients perceived a greater burden of treating diabetes than experienced patients Vijan et al. J Gen Intern Med 2005; 20: 479– 82.

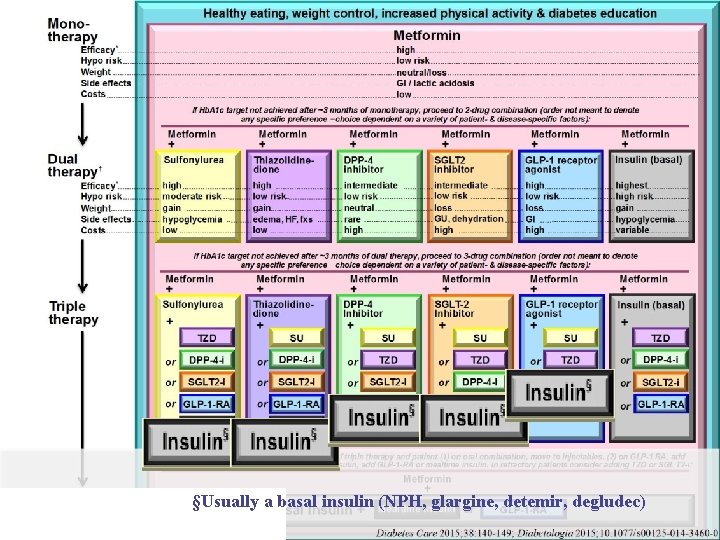
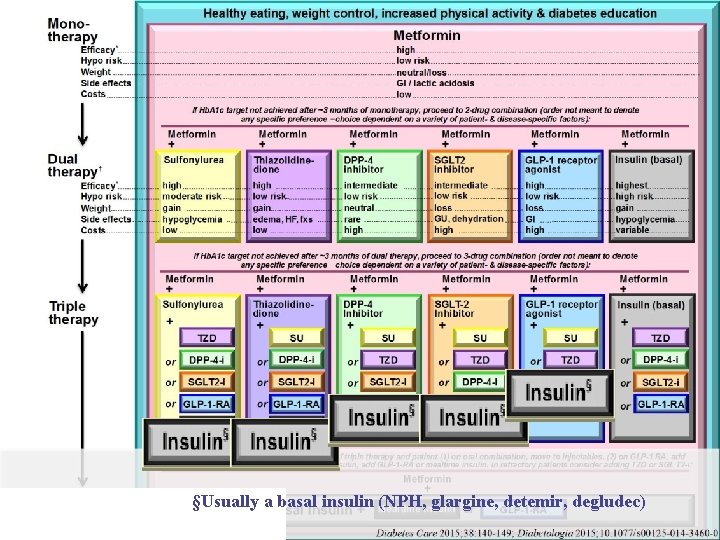
§Usually a basal insulin (NPH, glargine, detemir, degludec)
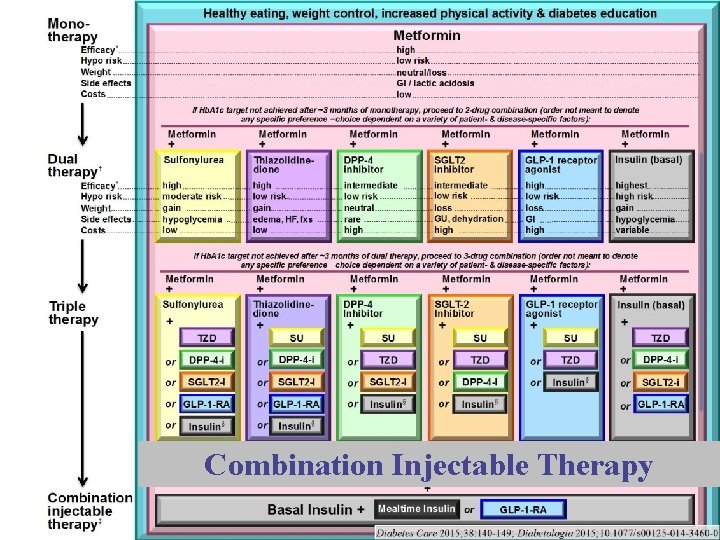
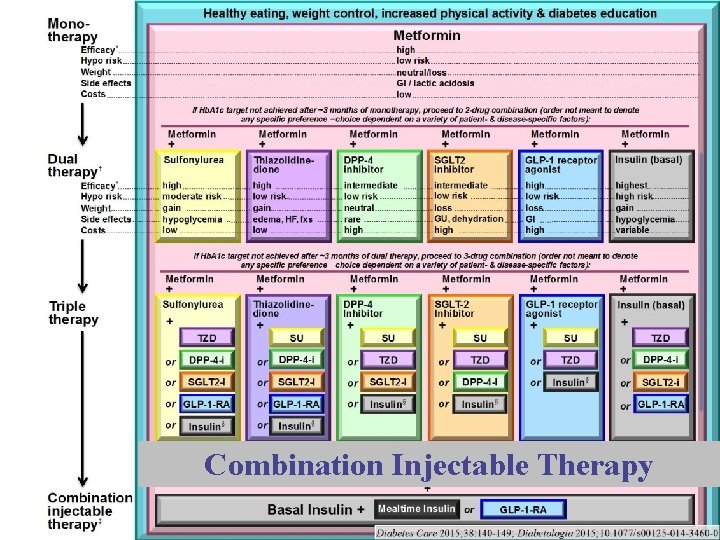
Combination Injectable Therapy

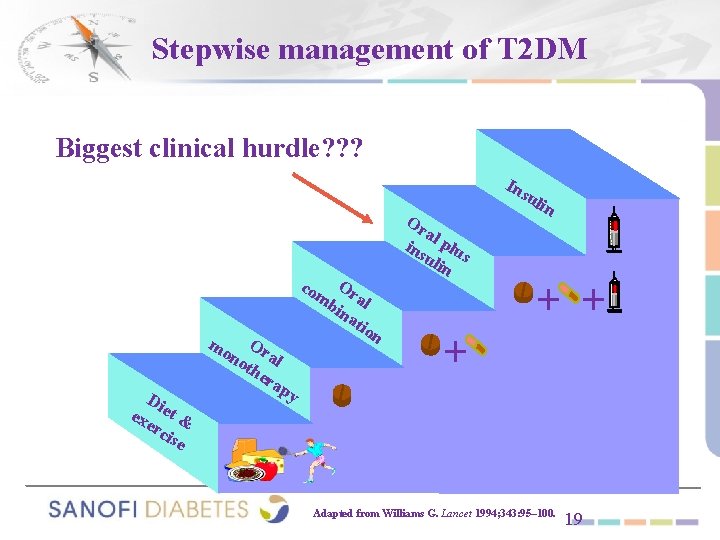
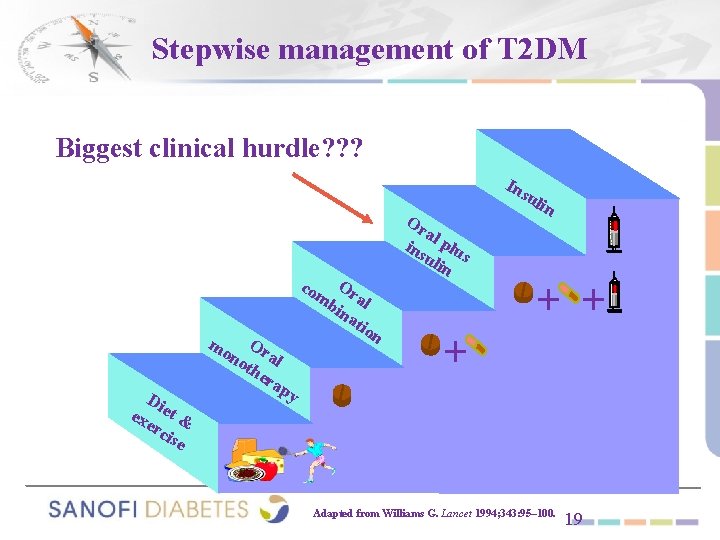
Stepwise management of T 2 DM Biggest clinical hurdle? ? ? In su O mb ral ina tio Or a ins l plu uli s n co mo Di exe et & rci se Or no al the ra py lin + + n + Adapted from Williams G. Lancet 1994; 343: 95– 100. 19
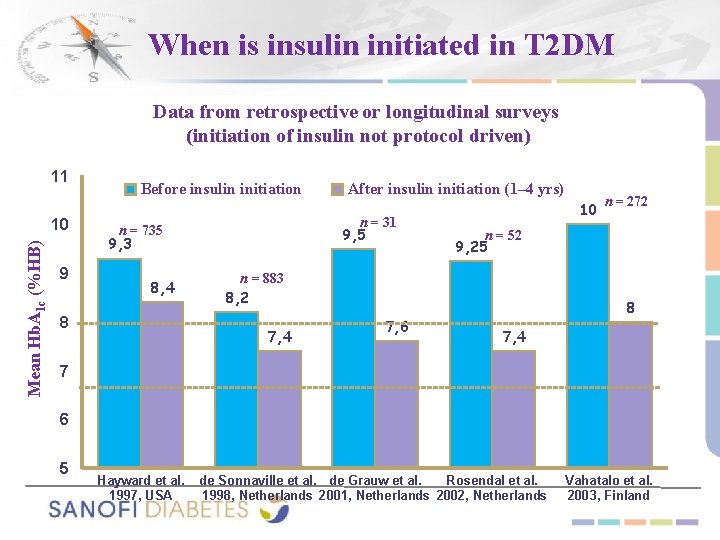
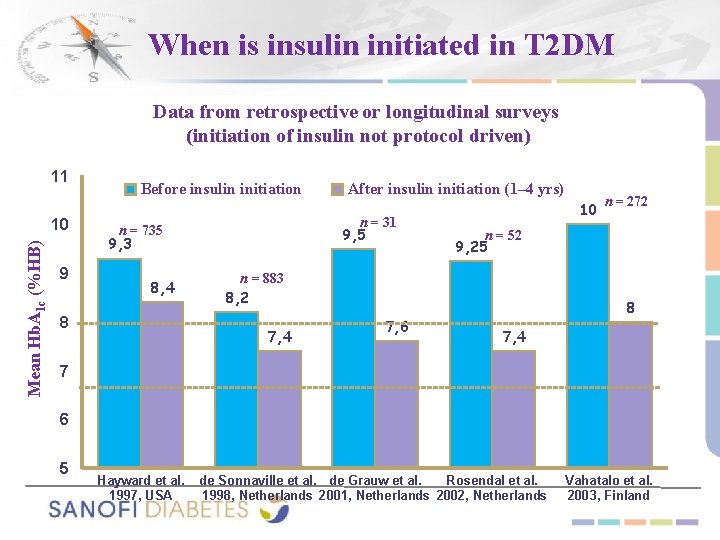
When is insulin initiated in T 2 DM Data from retrospective or longitudinal surveys (initiation of insulin not protocol driven) 11 Mean Hb. A 1 c (%HB) 10 9 Before insulin initiation n = 31 9, 5 n = 735 9, 3 8, 4 8 After insulin initiation (1– 4 yrs) 10 n = 52 9, 25 n = 883 8, 2 7, 4 7, 6 n = 272 8 7, 4 7 6 5 Hayward et al. 1997, USA de Sonnaville et al. de Grauw et al. Rosendal et al. 1998, Netherlands 2001, Netherlands 2002, Netherlands Vahatalo et al. 2003, Finland


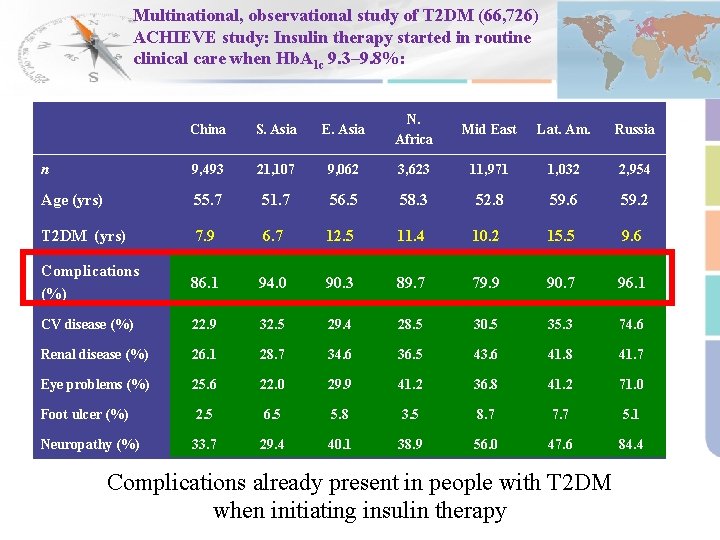
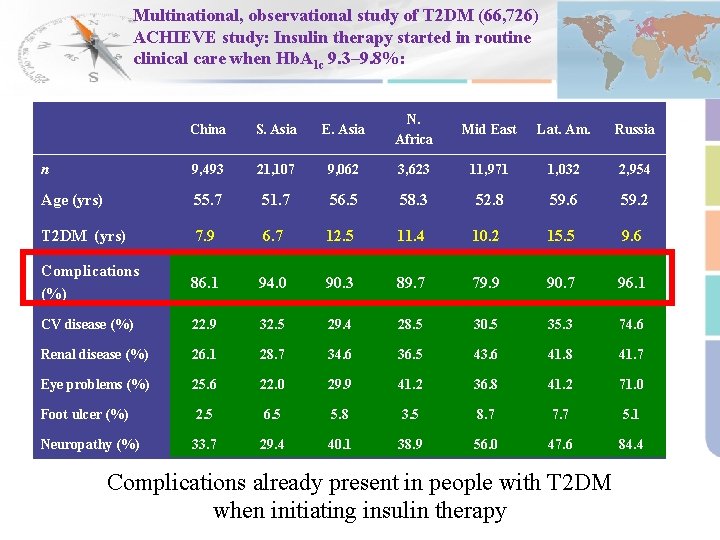
Multinational, observational study of T 2 DM (66, 726) ACHIEVE study: Insulin therapy started in routine clinical care when Hb. A 1 c 9. 3– 9. 8%: China S. Asia E. Asia N. Africa Mid East Lat. Am. Russia n 9, 493 21, 107 9, 062 3, 623 11, 971 1, 032 2, 954 Age (yrs) 55. 7 51. 7 56. 5 58. 3 52. 8 59. 6 59. 2 T 2 DM (yrs) 7. 9 6. 7 12. 5 11. 4 10. 2 15. 5 9. 6 Complications (%) 86. 1 94. 0 90. 3 89. 7 79. 9 90. 7 96. 1 CV disease (%) 22. 9 32. 5 29. 4 28. 5 30. 5 35. 3 74. 6 Renal disease (%) 26. 1 28. 7 34. 6 36. 5 43. 6 41. 8 41. 7 Eye problems (%) 25. 6 22. 0 29. 9 41. 2 36. 8 41. 2 71. 0 Foot ulcer (%) 2. 5 6. 5 5. 8 3. 5 8. 7 7. 7 5. 1 Neuropathy (%) 33. 7 29. 4 40. 1 38. 9 56. 0 47. 6 84. 4 Adjusted for age at diagnosis; Complications (%) predicted from a logistic model Zilov AV, et al. Diabetes 2011; 60(Suppl. 1): 2485. Complications already present in people with T 2 DM when initiating insulin therapy
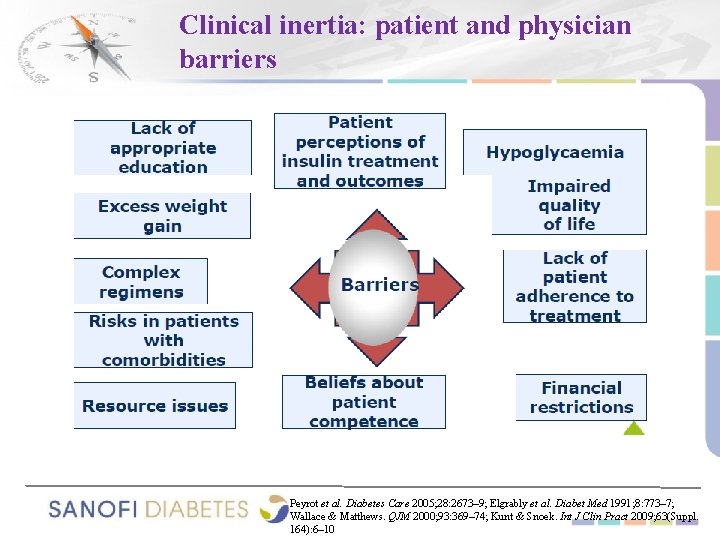
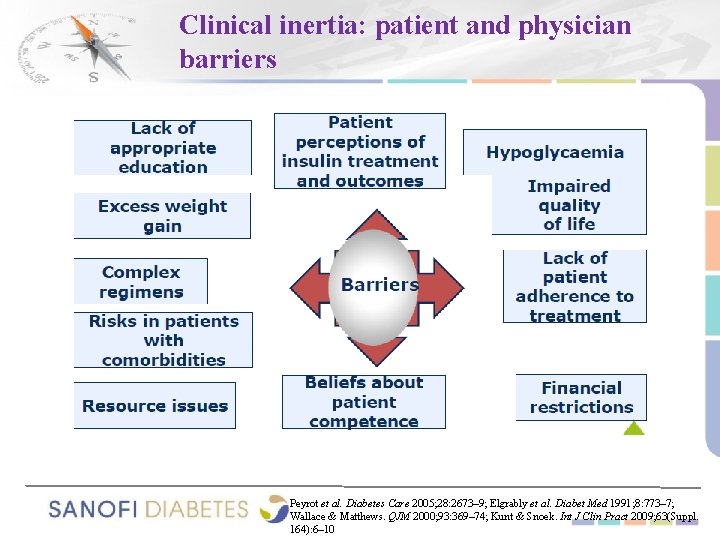
Clinical inertia: patient and physician barriers Peyrot et al. Diabetes Care 2005; 28: 2673– 9; Elgrably et al. Diabet Med 1991; 8: 773– 7; Wallace & Matthews. QJM 2000; 93: 369– 74; Kunt & Snoek. Int J Clin Pract 2009; 63(Suppl. 164): 6– 10

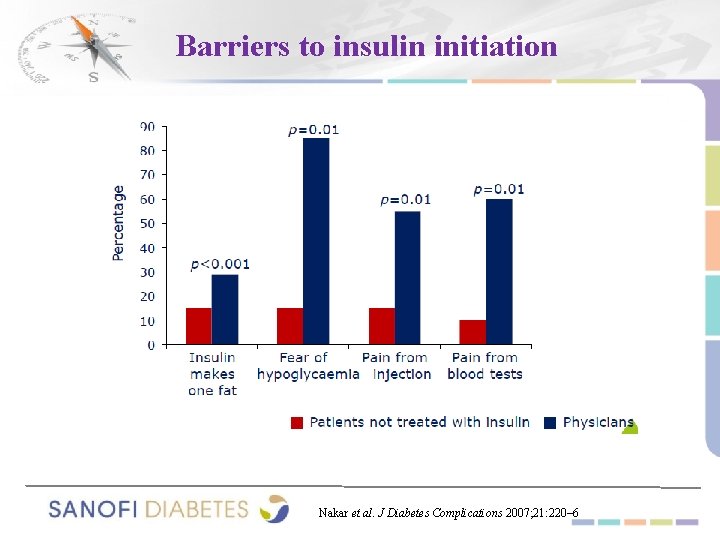
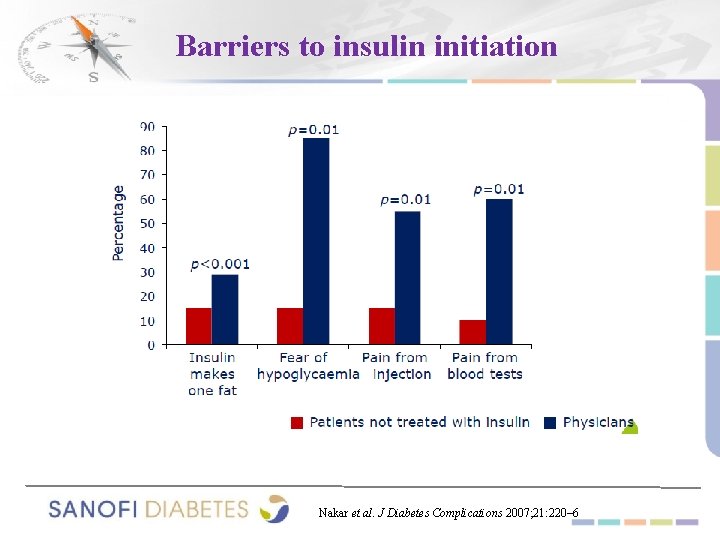
Barriers to insulin initiation Nakar et al. J Diabetes Complications 2007; 21: 220– 6
Do not forget! ● The beneficial effects of early insulin therapy in T 2 DM on beta-cell function, micro/macrovascular morbidity and mortality, and total mortality.
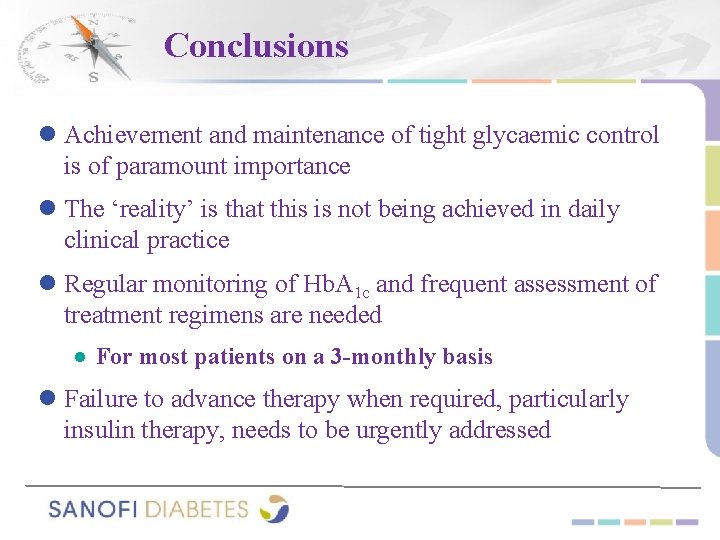
Conclusions ● Achievement and maintenance of tight glycaemic control is of paramount importance ● The ‘reality’ is that this is not being achieved in daily clinical practice ● Regular monitoring of Hb. A 1 c and frequent assessment of treatment regimens are needed ● For most patients on a 3 -monthly basis ● Failure to advance therapy when required, particularly insulin therapy, needs to be urgently addressed
So, why not to do! Start Insulin At The Right Time! Adjust & Follow! | 29

Thank You! | 30
 University of science and technology of mazandaran
University of science and technology of mazandaran Dr pang endocrinologist
Dr pang endocrinologist Endocrinologist in parbhani
Endocrinologist in parbhani Dr durkan
Dr durkan Dr swade endocrinologist
Dr swade endocrinologist Dimitrios thomas endocrinologist
Dimitrios thomas endocrinologist Dr suri endocrinologist
Dr suri endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Dr. alireza amirbaigloo, md, endocrinologist
Dr. alireza amirbaigloo, md, endocrinologist Endocrinologist lifestyle
Endocrinologist lifestyle Endocrinologist newcastle
Endocrinologist newcastle Stephen ponder md
Stephen ponder md Cushing syndrome most common cause
Cushing syndrome most common cause Masaryk university medical faculty
Masaryk university medical faculty Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Slidetodoc.com
Slidetodoc.com Chulalongkorn university faculty of arts
Chulalongkorn university faculty of arts Faculty of education york university
Faculty of education york university University of cologne faculty of management
University of cologne faculty of management Faculty of law of the university of zagreb
Faculty of law of the university of zagreb Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Faculty of mechanical engineering thammasat university
Faculty of mechanical engineering thammasat university Auricle of heart vs atrium
Auricle of heart vs atrium Feup university of porto
Feup university of porto Semmelweis
Semmelweis Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Elearningunideb
Elearningunideb Leading university tuition fees
Leading university tuition fees University of montenegro faculty of law
University of montenegro faculty of law Singularity executive program
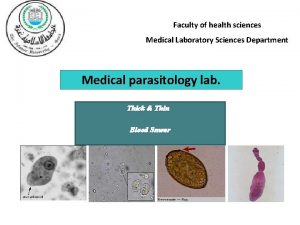
Singularity executive program Thin and thick smear
Thin and thick smear