Disorders of Electrolyte Homeostasis Potassium and Magnesium Sara
- Slides: 35
Disorders of Electrolyte Homeostasis – Potassium and Magnesium Sara E Parli, Pharm. D Assistant Professor (Adjunct) Critical Care Pharmacist Trauma/Acute Care Surgery
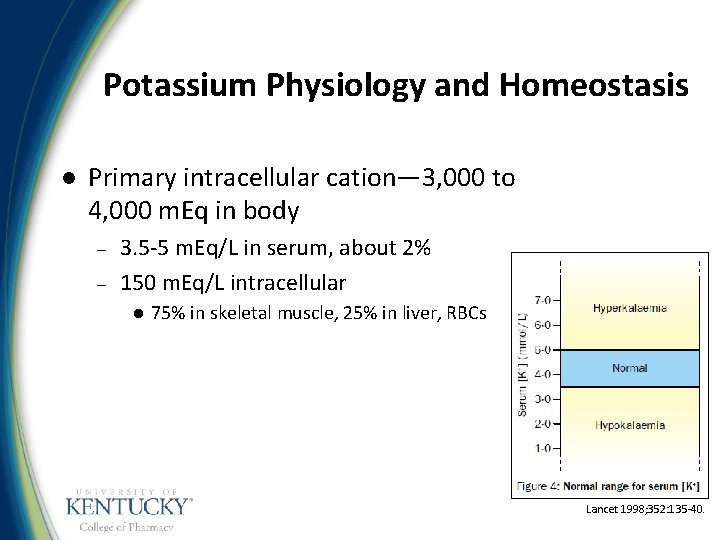
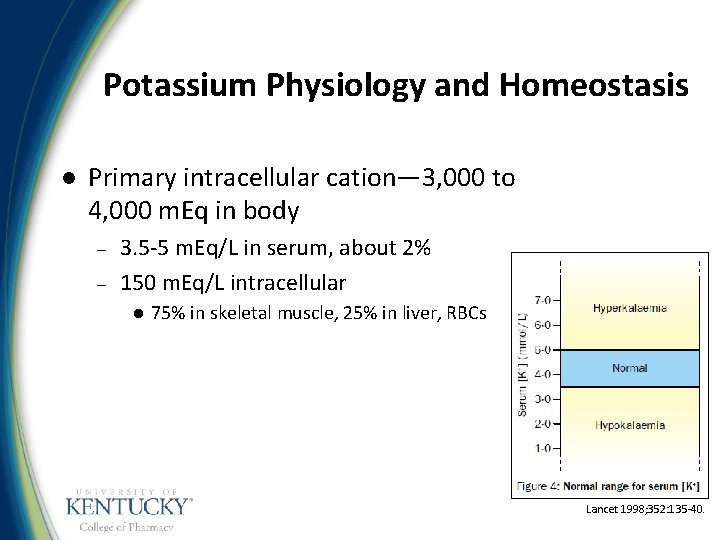
Potassium Physiology and Homeostasis l Primary intracellular cation— 3, 000 to 4, 000 m. Eq in body – – 3. 5 -5 m. Eq/L in serum, about 2% 150 m. Eq/L intracellular l 75% in skeletal muscle, 25% in liver, RBCs Lancet 1998; 352: 135 -40.
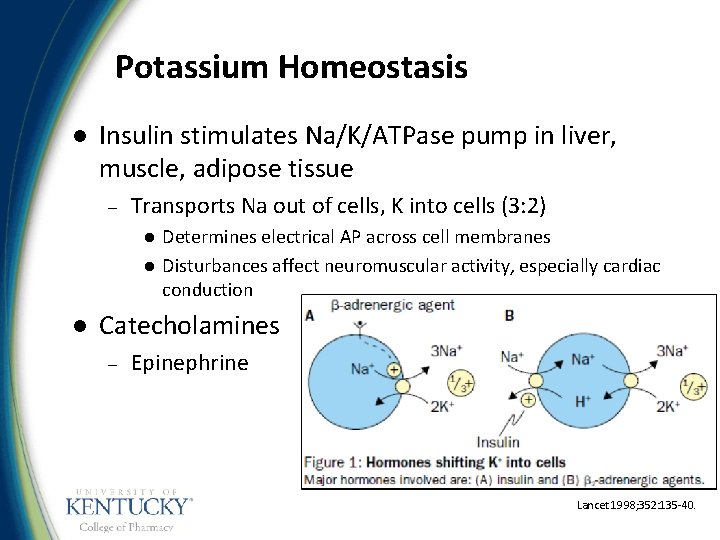
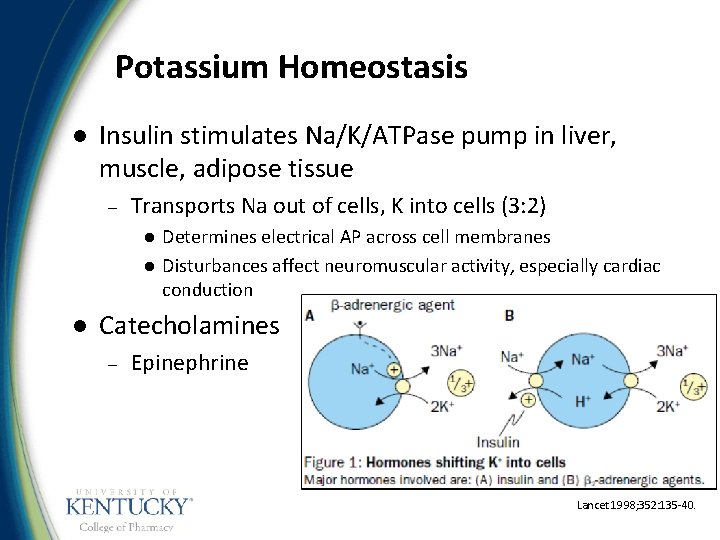
Potassium Homeostasis l Insulin stimulates Na/K/ATPase pump in liver, muscle, adipose tissue – Transports Na out of cells, K into cells (3: 2) l l l Determines electrical AP across cell membranes Disturbances affect neuromuscular activity, especially cardiac conduction Catecholamines – Epinephrine Lancet 1998; 352: 135 -40.
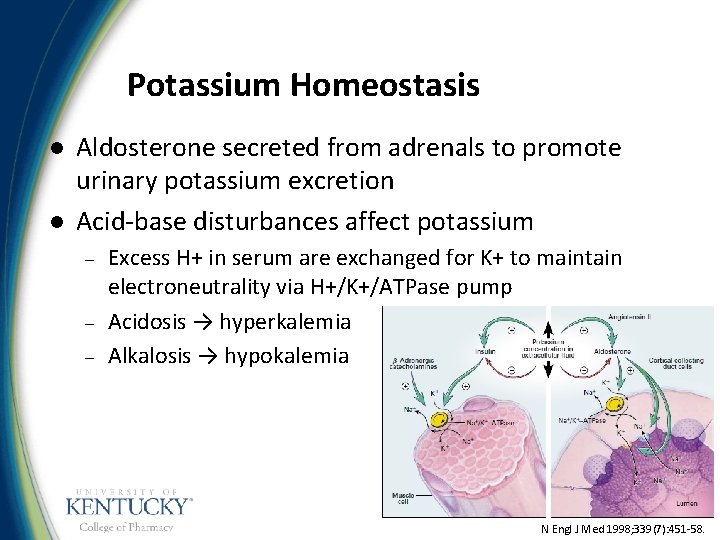
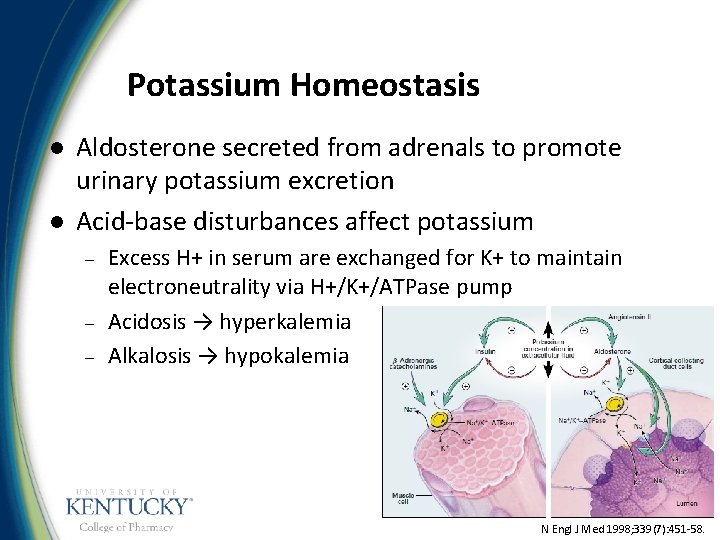
Potassium Homeostasis l l Aldosterone secreted from adrenals to promote urinary potassium excretion Acid-base disturbances affect potassium – – – Excess H+ in serum are exchanged for K+ to maintain electroneutrality via H+/K+/ATPase pump Acidosis → hyperkalemia Alkalosis → hypokalemia N Engl J Med 1998; 339(7): 451 -58.
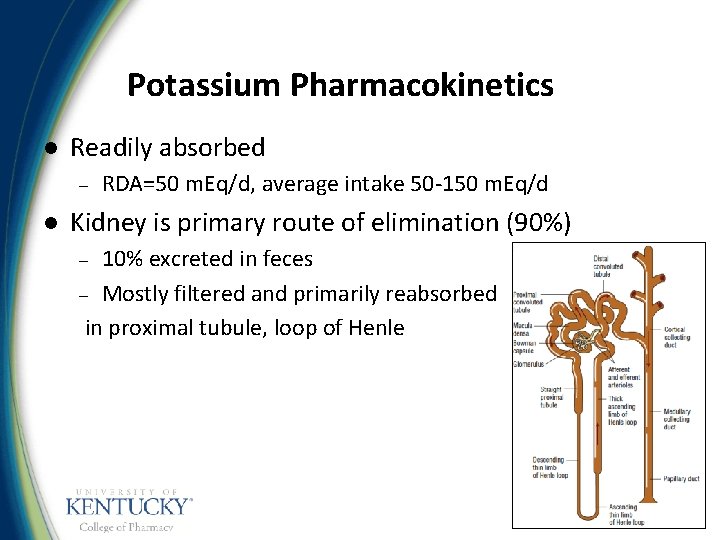
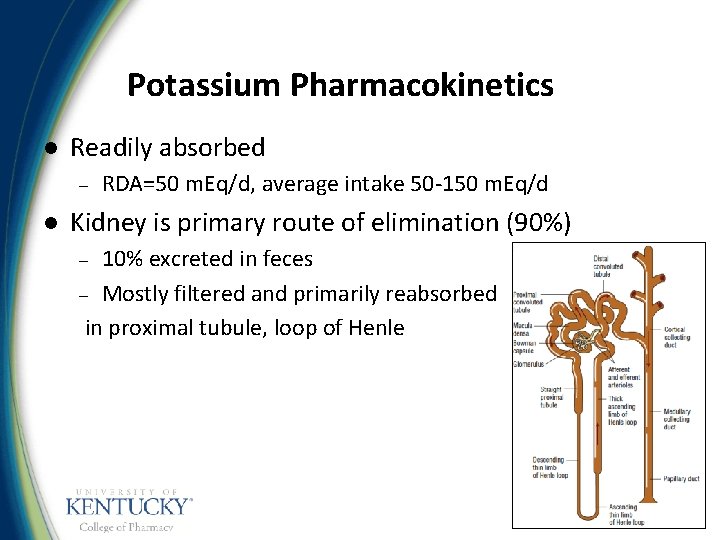
Potassium Pharmacokinetics l Readily absorbed – l RDA=50 m. Eq/d, average intake 50 -150 m. Eq/d Kidney is primary route of elimination (90%) 10% excreted in feces – Mostly filtered and primarily reabsorbed in proximal tubule, loop of Henle –
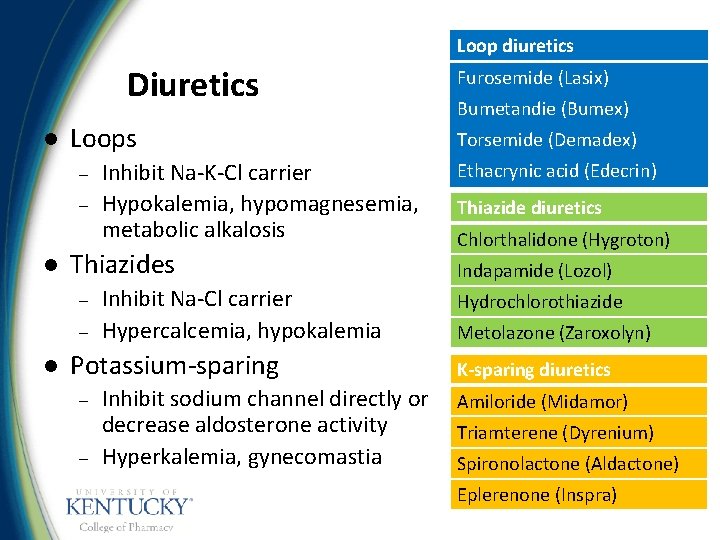
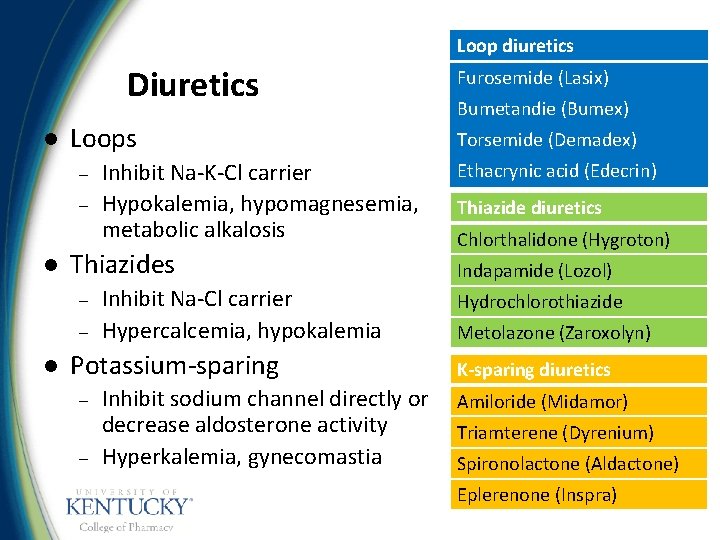
Loop diuretics Diuretics l Loops – – l Thiazides – – l Inhibit Na-K-Cl carrier Hypokalemia, hypomagnesemia, metabolic alkalosis Inhibit Na-Cl carrier Hypercalcemia, hypokalemia Potassium-sparing – – Inhibit sodium channel directly or decrease aldosterone activity Hyperkalemia, gynecomastia Furosemide (Lasix) Bumetandie (Bumex) Torsemide (Demadex) Ethacrynic acid (Edecrin) Thiazide diuretics Chlorthalidone (Hygroton) Indapamide (Lozol) Hydrochlorothiazide Metolazone (Zaroxolyn) K-sparing diuretics Amiloride (Midamor) Triamterene (Dyrenium) Spironolactone (Aldactone) Eplerenone (Inspra)
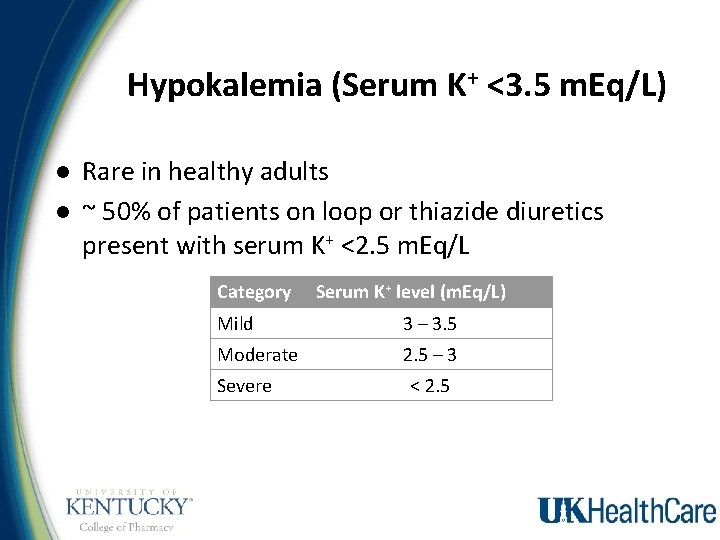
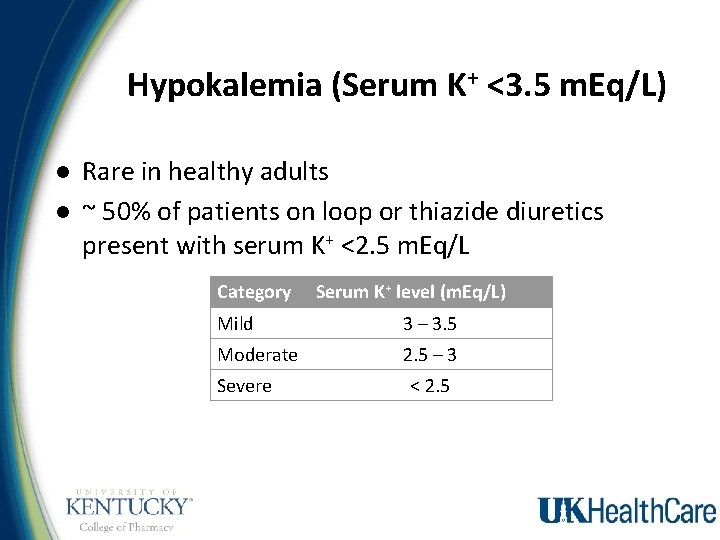
Hypokalemia (Serum K+ <3. 5 m. Eq/L) l l Rare in healthy adults ~ 50% of patients on loop or thiazide diuretics present with serum K+ <2. 5 m. Eq/L Category Serum K+ level (m. Eq/L) Mild 3 – 3. 5 Moderate 2. 5 – 3 Severe < 2. 5
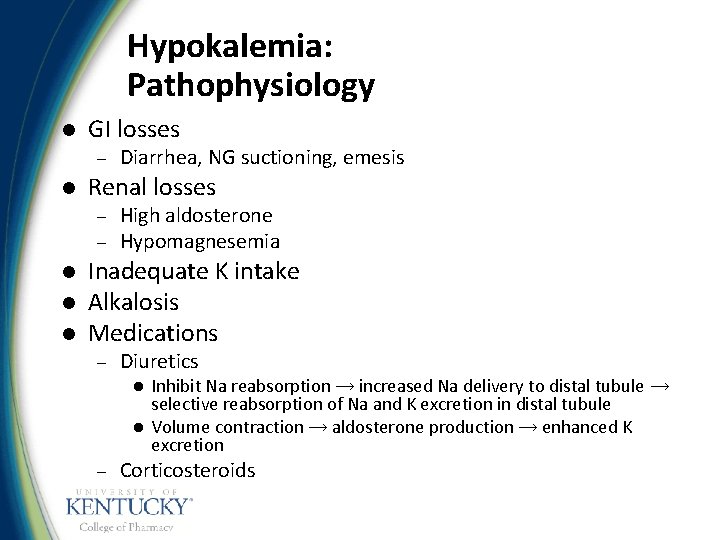
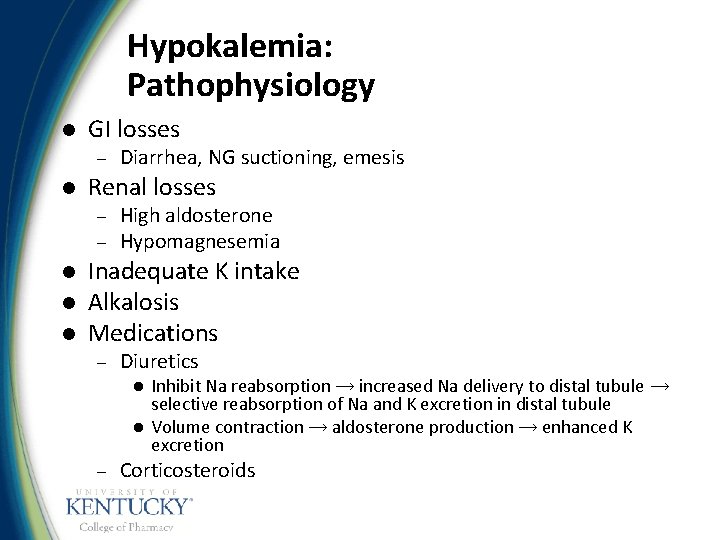
Hypokalemia: Pathophysiology l GI losses – l Renal losses – – l l l Diarrhea, NG suctioning, emesis High aldosterone Hypomagnesemia Inadequate K intake Alkalosis Medications – Diuretics l l – Inhibit Na reabsorption → increased Na delivery to distal tubule → selective reabsorption of Na and K excretion in distal tubule Volume contraction → aldosterone production → enhanced K excretion Corticosteroids
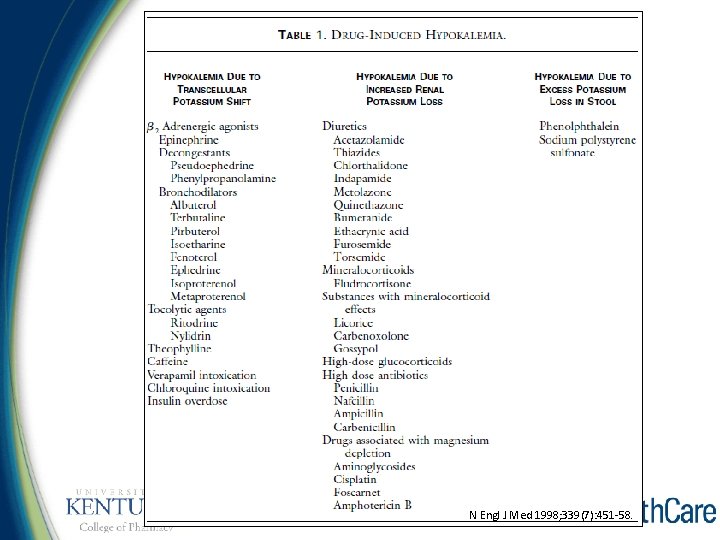
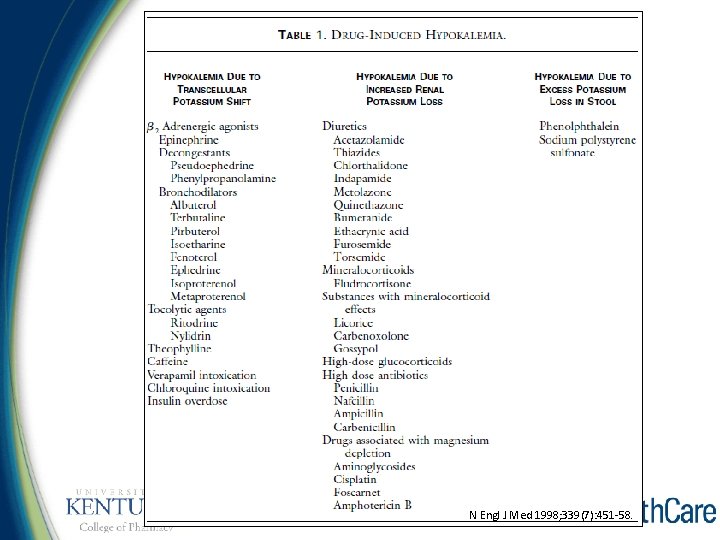
N Engl J Med 1998; 339(7): 451 -58.
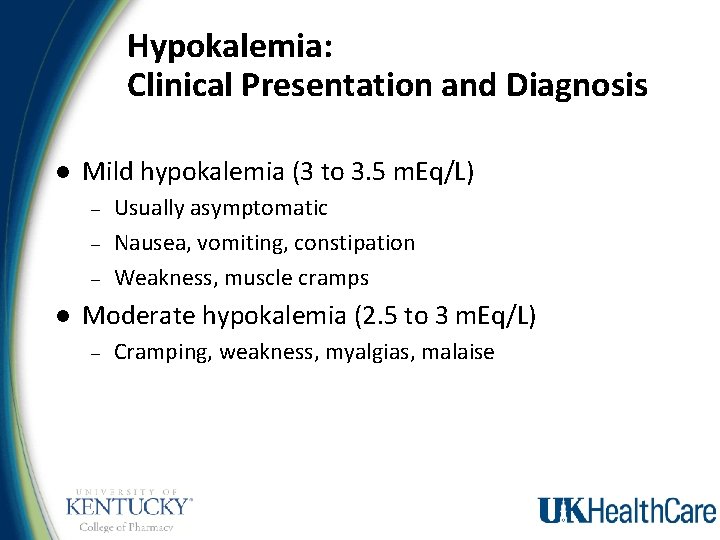
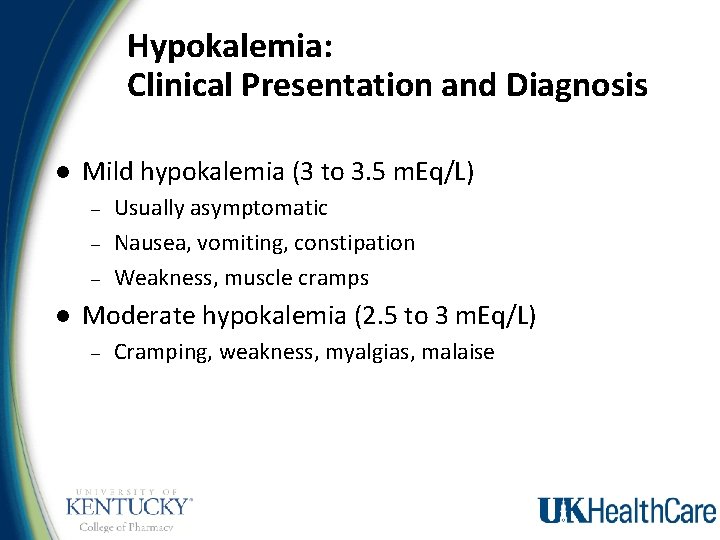
Hypokalemia: Clinical Presentation and Diagnosis l Mild hypokalemia (3 to 3. 5 m. Eq/L) – – – l Usually asymptomatic Nausea, vomiting, constipation Weakness, muscle cramps Moderate hypokalemia (2. 5 to 3 m. Eq/L) – Cramping, weakness, myalgias, malaise
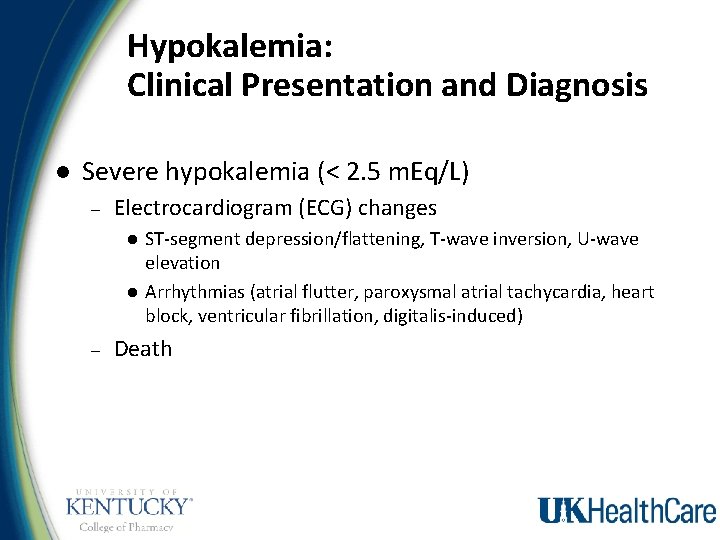
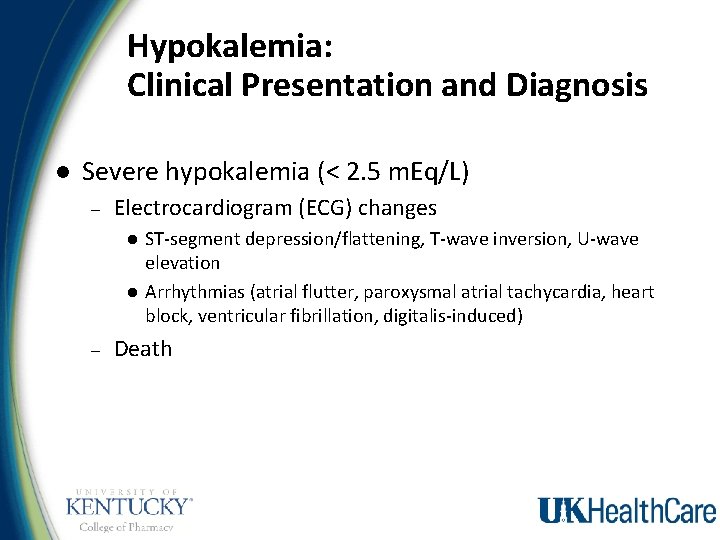
Hypokalemia: Clinical Presentation and Diagnosis l Severe hypokalemia (< 2. 5 m. Eq/L) – Electrocardiogram (ECG) changes l l – ST-segment depression/flattening, T-wave inversion, U-wave elevation Arrhythmias (atrial flutter, paroxysmal atrial tachycardia, heart block, ventricular fibrillation, digitalis-induced) Death
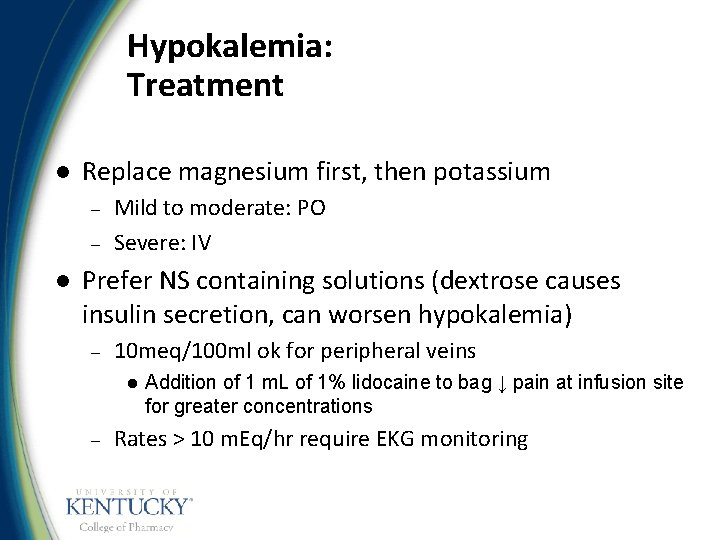
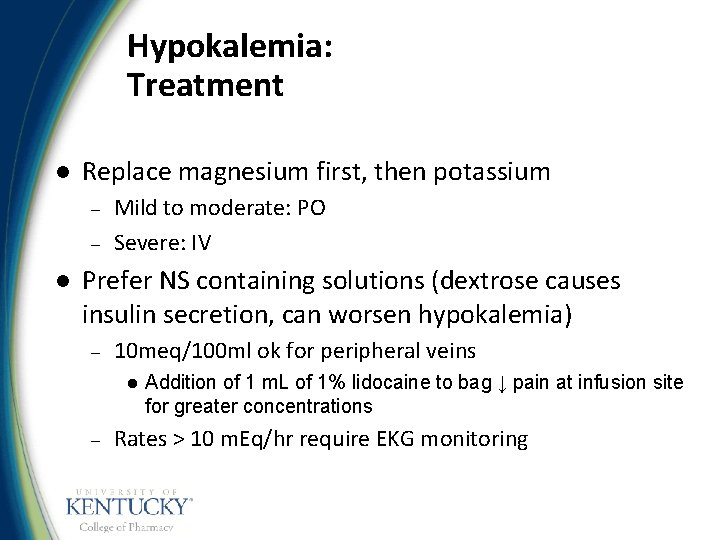
Hypokalemia: Treatment l Replace magnesium first, then potassium – – l Mild to moderate: PO Severe: IV Prefer NS containing solutions (dextrose causes insulin secretion, can worsen hypokalemia) – 10 meq/100 ml ok for peripheral veins l – Addition of 1 m. L of 1% lidocaine to bag ↓ pain at infusion site for greater concentrations Rates > 10 m. Eq/hr require EKG monitoring
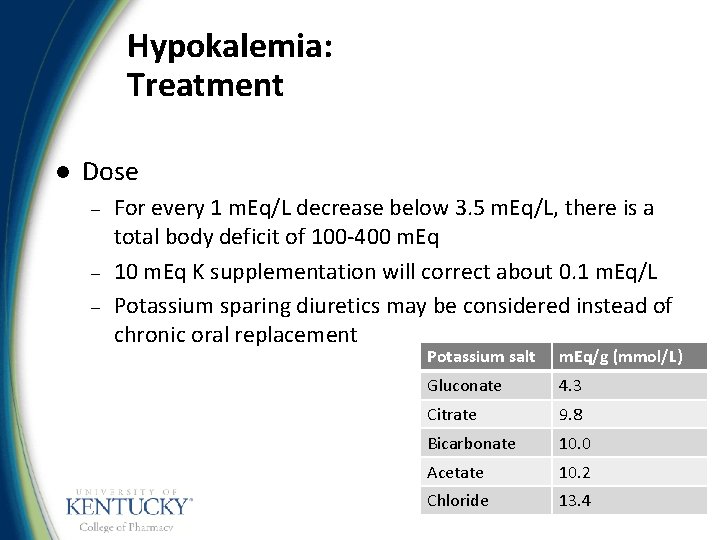
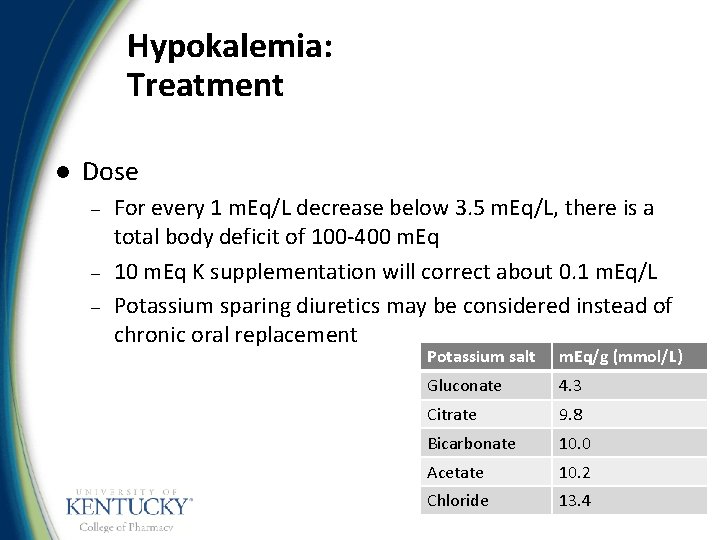
Hypokalemia: Treatment l Dose – – – For every 1 m. Eq/L decrease below 3. 5 m. Eq/L, there is a total body deficit of 100 -400 m. Eq 10 m. Eq K supplementation will correct about 0. 1 m. Eq/L Potassium sparing diuretics may be considered instead of chronic oral replacement Potassium salt m. Eq/g (mmol/L) Gluconate 4. 3 Citrate 9. 8 Bicarbonate 10. 0 Acetate 10. 2 Chloride 13. 4
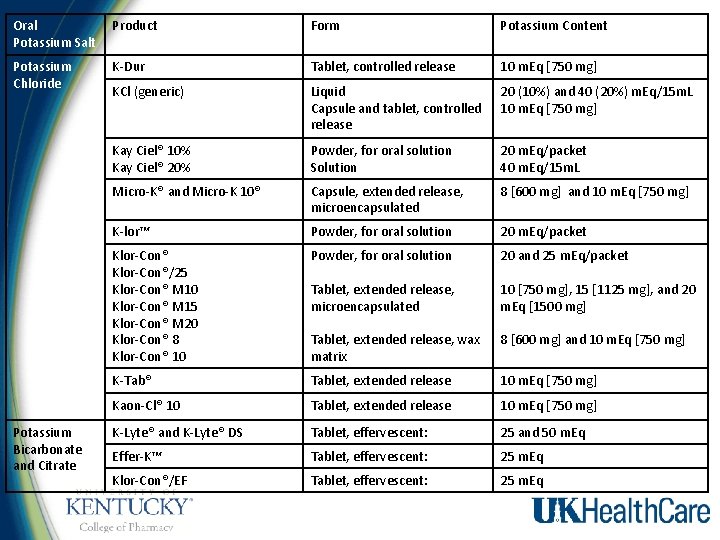
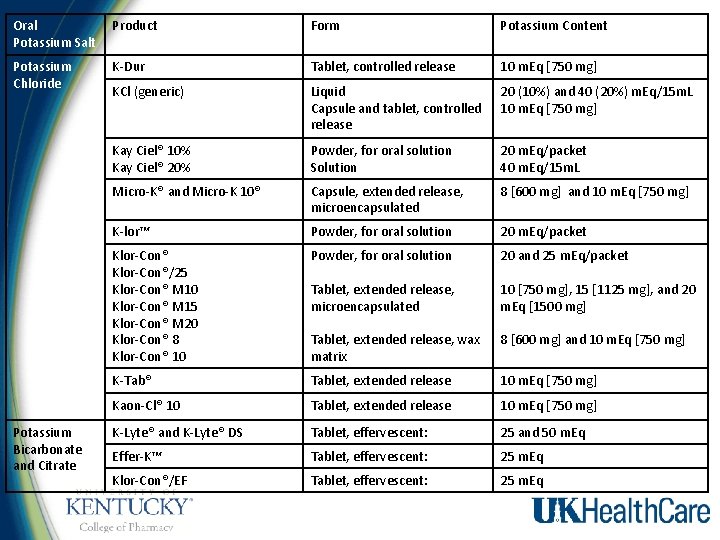
Oral Potassium Salt Product Form Potassium Content Potassium Chloride K-Dur Tablet, controlled release 10 m. Eq [750 mg] KCl (generic) Liquid Capsule and tablet, controlled release 20 (10%) and 40 (20%) m. Eq/15 m. L 10 m. Eq [750 mg] Kay Ciel® 10% Kay Ciel® 20% Powder, for oral solution Solution 20 m. Eq/packet 40 m. Eq/15 m. L Micro-K® and Micro-K 10® Capsule, extended release, microencapsulated 8 [600 mg] and 10 m. Eq [750 mg] K-lor™ Powder, for oral solution 20 m. Eq/packet Klor-Con®/25 Klor-Con® M 10 Klor-Con® M 15 Klor-Con® M 20 Klor-Con® 8 Klor-Con® 10 Powder, for oral solution 20 and 25 m. Eq/packet Tablet, extended release, microencapsulated 10 [750 mg], 15 [1125 mg], and 20 m. Eq [1500 mg] Tablet, extended release, wax matrix 8 [600 mg] and 10 m. Eq [750 mg] K-Tab® Tablet, extended release 10 m. Eq [750 mg] Kaon-Cl® 10 Tablet, extended release 10 m. Eq [750 mg] K-Lyte® and K-Lyte® DS Tablet, effervescent: 25 and 50 m. Eq Effer-K™ Tablet, effervescent: 25 m. Eq Klor-Con®/EF Tablet, effervescent: 25 m. Eq Potassium Bicarbonate and Citrate
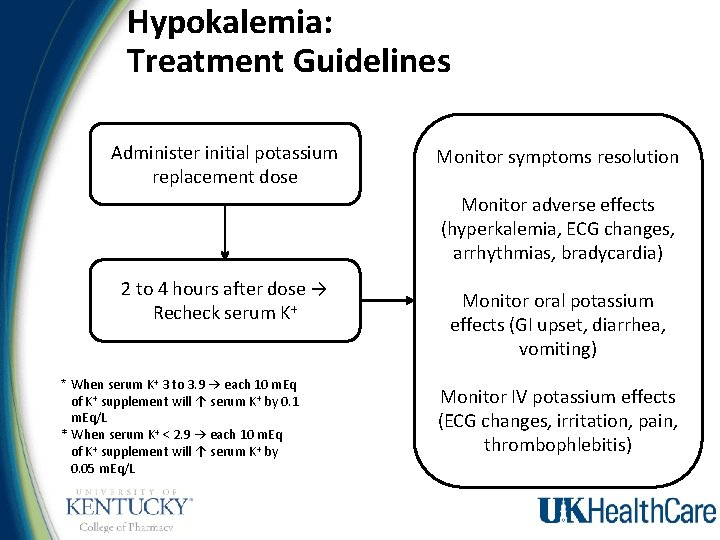
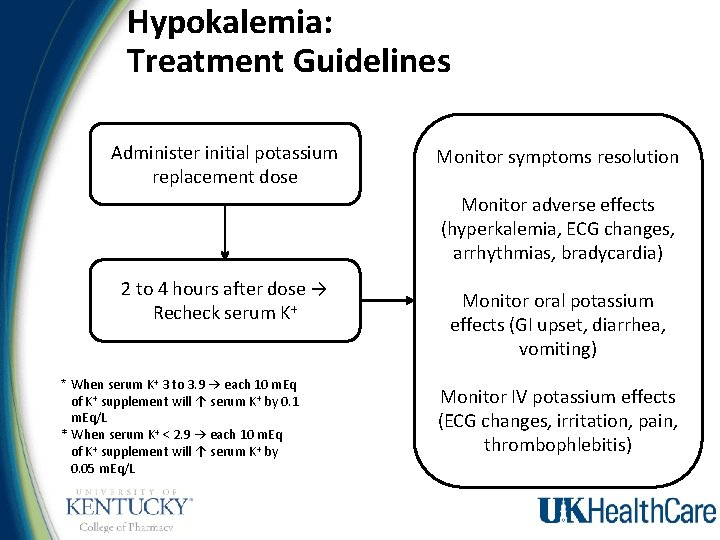
Hypokalemia: Treatment Guidelines Administer initial potassium replacement dose Monitor symptoms resolution Monitor adverse effects (hyperkalemia, ECG changes, arrhythmias, bradycardia) 2 to 4 hours after dose → Recheck serum K+ * When serum K+ 3 to 3. 9 → each 10 m. Eq of K+ supplement will ↑ serum K+ by 0. 1 m. Eq/L * When serum K+ < 2. 9 → each 10 m. Eq of K+ supplement will ↑ serum K+ by 0. 05 m. Eq/L Monitor oral potassium effects (GI upset, diarrhea, vomiting) Monitor IV potassium effects (ECG changes, irritation, pain, thrombophlebitis)
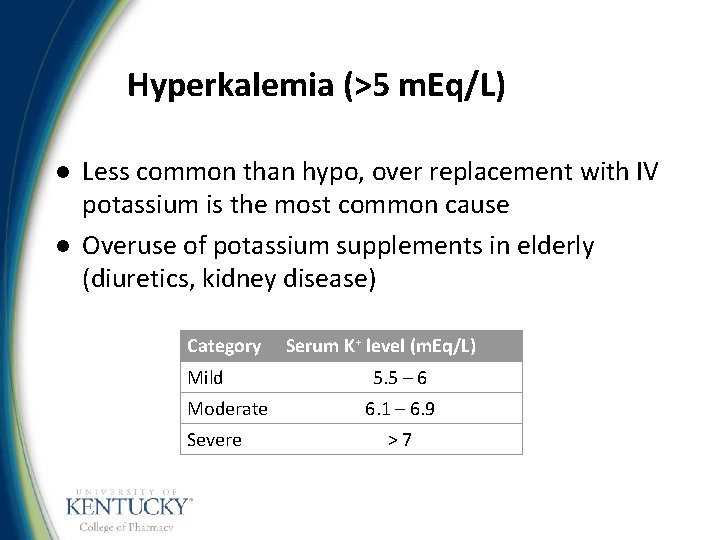
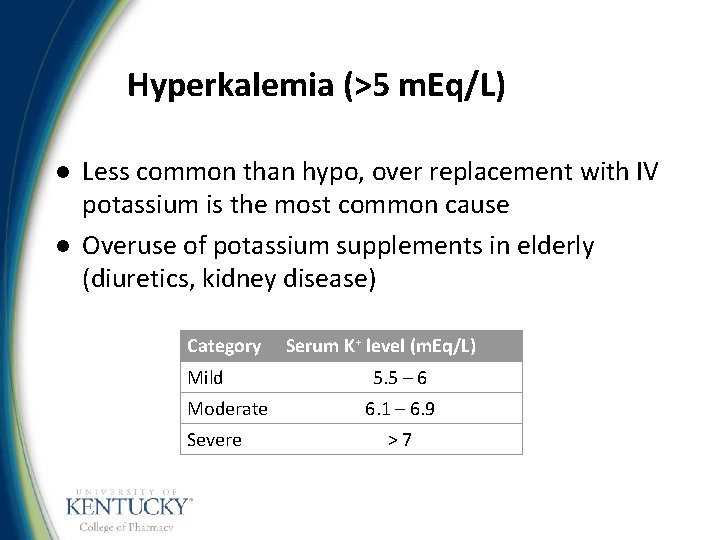
Hyperkalemia (>5 m. Eq/L) l l Less common than hypo, over replacement with IV potassium is the most common cause Overuse of potassium supplements in elderly (diuretics, kidney disease) Category Mild Moderate Severe Serum K+ level (m. Eq/L) 5. 5 – 6 6. 1 – 6. 9 >7
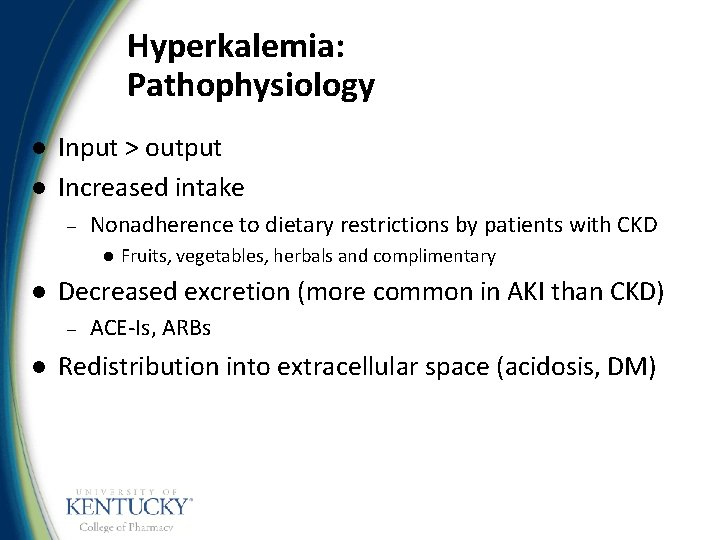
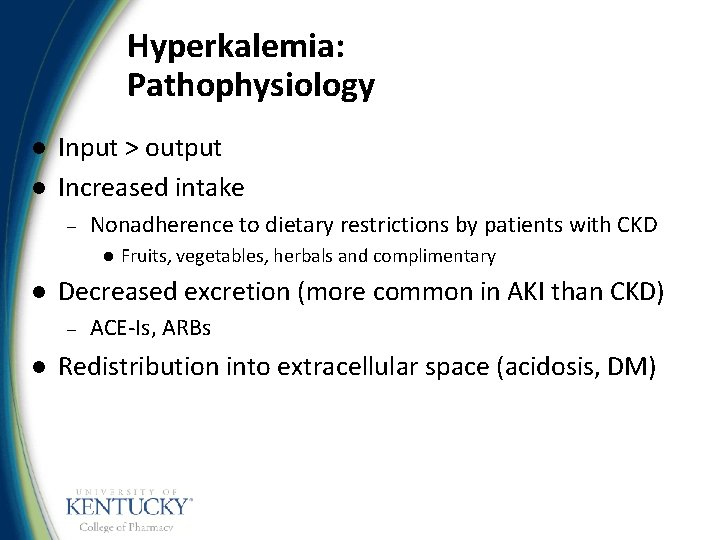
Hyperkalemia: Pathophysiology l l Input > output Increased intake – Nonadherence to dietary restrictions by patients with CKD l l Decreased excretion (more common in AKI than CKD) – l Fruits, vegetables, herbals and complimentary ACE-Is, ARBs Redistribution into extracellular space (acidosis, DM)
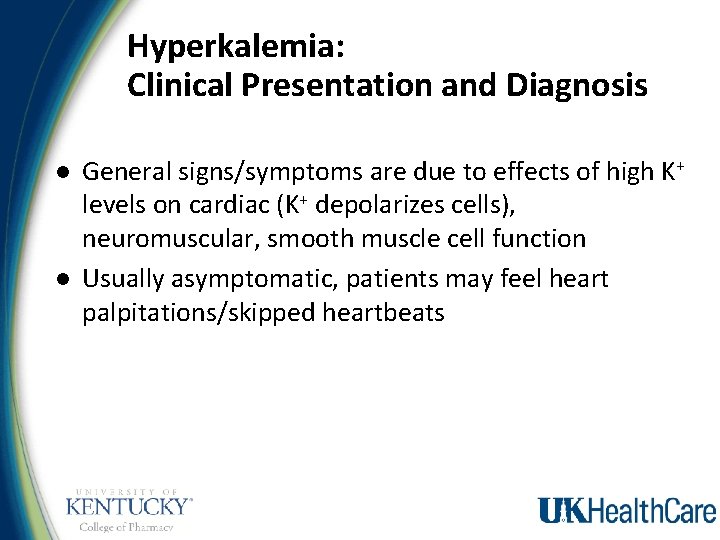
Hyperkalemia: Clinical Presentation and Diagnosis l l General signs/symptoms are due to effects of high K+ levels on cardiac (K+ depolarizes cells), neuromuscular, smooth muscle cell function Usually asymptomatic, patients may feel heart palpitations/skipped heartbeats
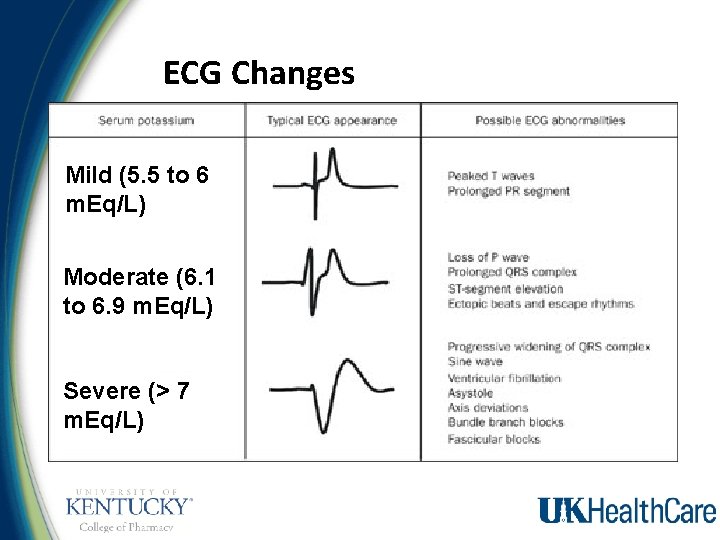
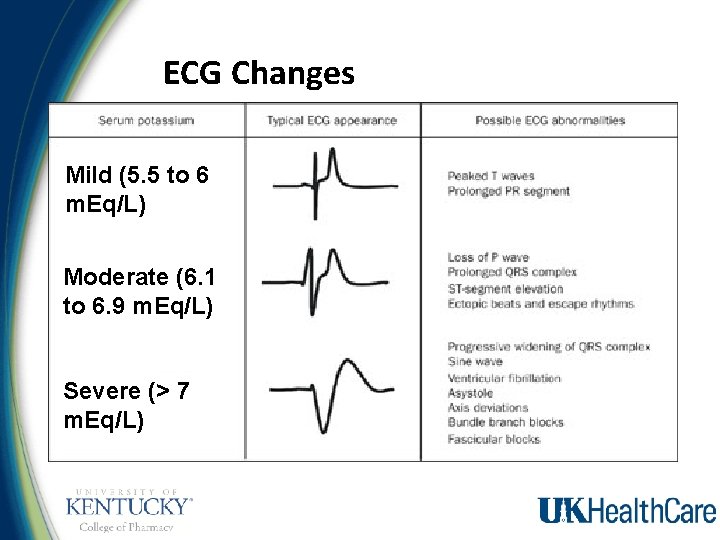
ECG Changes Mild (5. 5 to 6 m. Eq/L) Moderate (6. 1 to 6. 9 m. Eq/L) Severe (> 7 m. Eq/L)
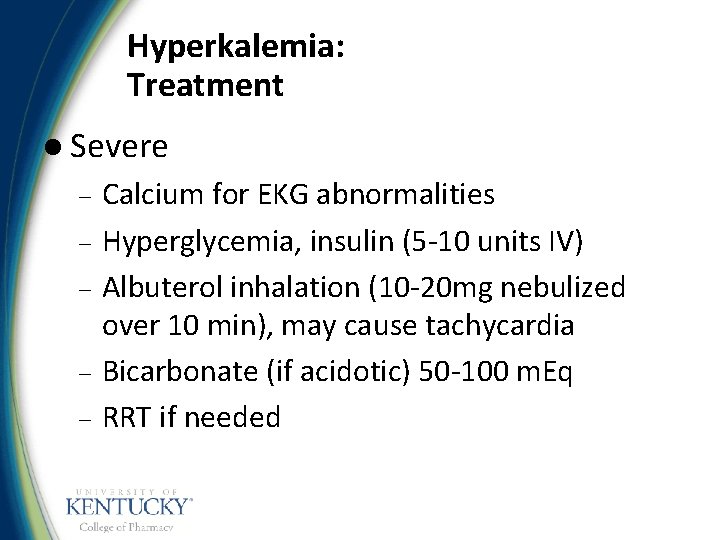
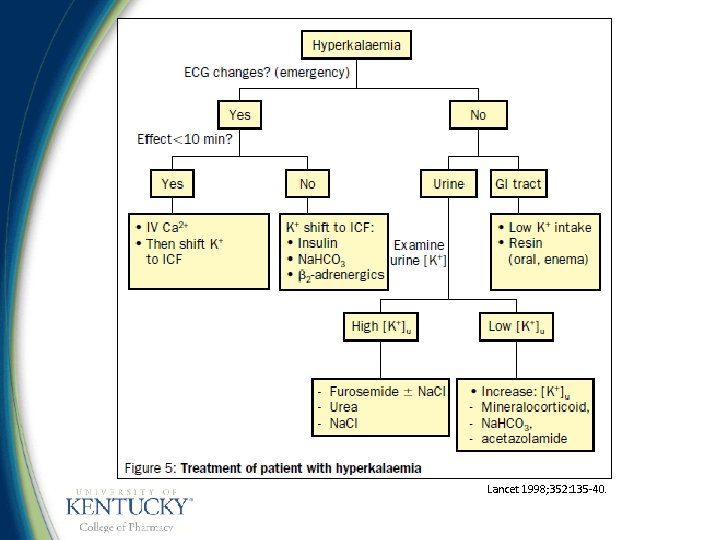
Hyperkalemia: Treatment l Severe – – – Calcium for EKG abnormalities Hyperglycemia, insulin (5 -10 units IV) Albuterol inhalation (10 -20 mg nebulized over 10 min), may cause tachycardia Bicarbonate (if acidotic) 50 -100 m. Eq RRT if needed
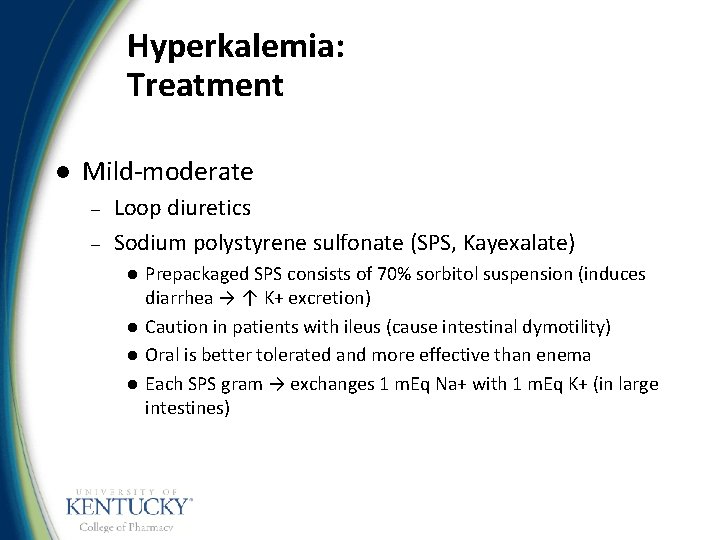
Hyperkalemia: Treatment l Mild-moderate – – Loop diuretics Sodium polystyrene sulfonate (SPS, Kayexalate) l l Prepackaged SPS consists of 70% sorbitol suspension (induces diarrhea → ↑ K+ excretion) Caution in patients with ileus (cause intestinal dymotility) Oral is better tolerated and more effective than enema Each SPS gram → exchanges 1 m. Eq Na+ with 1 m. Eq K+ (in large intestines)
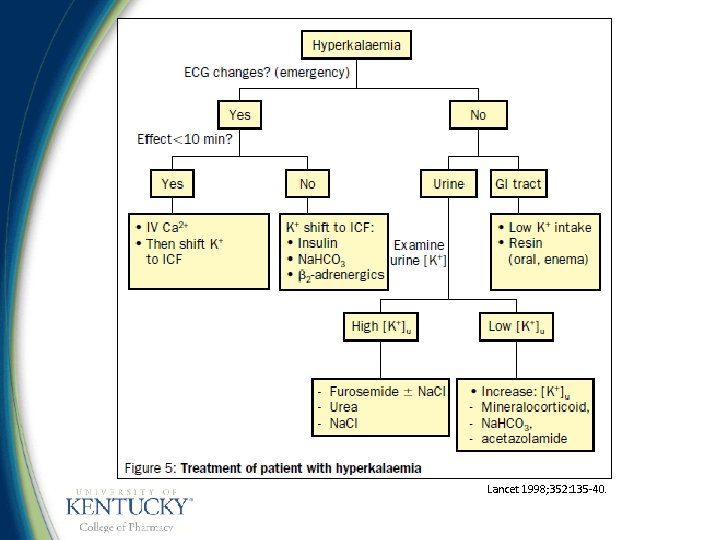
Lancet 1998; 352: 135 -40.
Disorders of Potassium Homeostasis l l Primary intracellular cation, normal K= 3. 5– 5 m. Eq/L Tightly regulated by Na/K/ATPase pump – l l Determines electrical action potential across myocardium Hypokalemia is common with diuretics and GI losses – l Insulin, catecholamines, acid/base Replace IV or PO depending on severity Hyperkalemia can be due to over-correction with IV potassium – Treat symptoms, promote excretion
Magnesium Homeostasis l l Primarily distributed in ICF (67% in bone, 20% in muscle) Serum = 1. 7 -2. 3 mg/dl (1% of total body in ECF) 30 -40% ingested is absorbed in small intestine Renal elimination – Majority of Mg 2+ is reabsorbed in loop of Henle
Factors Affecting Magnesium Loop Reabsorption l Serum Mg++ levels – l Intraluminal Na+ and ECF volume status – – l ↑ serum Mg++ → ↓ Mg++ reabsorption ↓ ECF volume → ↑ Mg++ reabsorption (due to ↓ luminal flow and ↑ Na+ reabsorption (Na+ - K+ - 2 Cl- -ATPase cotransport pump) Low Na+ diet → ↑ Mg++ reabsorption Parathyroid hormone (PTH) ↑ Mg++ reabsorption
Magnesium Physiology l l l Central role → cellular function, and cofactor in numerous biochemical reactions (especially systems depending on adenosine triphosphate (ATP)) and enzymes Mitochondrial and cell membrane function Protein synthesis PTH secretion Nerve conduction, membrane stabilization Inhibits calcium channels
Hypomagnesemia (<1. 5 mg/d. L) l l More common in ICU GI losses – l Renal losses – – l Decreased absorption/intake (alcoholism), increased loss Most common with loops, thiazides Also with other drugs-foscarnet, aminoglycosides, amphotericin, etc. Commonly associated with hypocalcemia
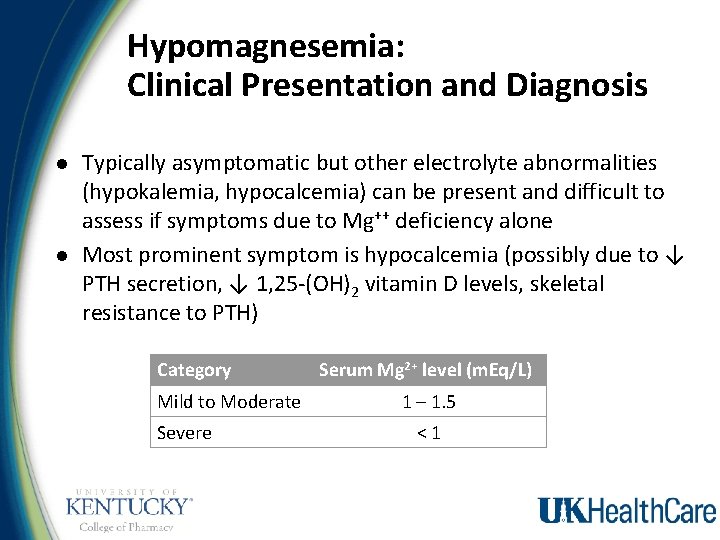
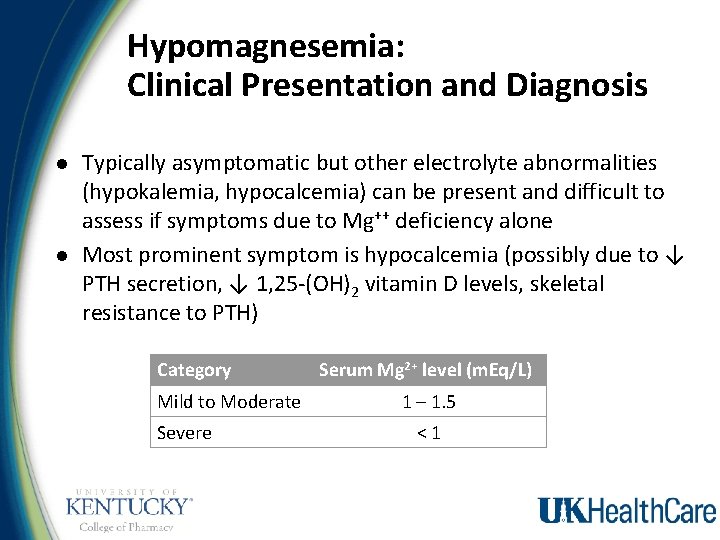
Hypomagnesemia: Clinical Presentation and Diagnosis l l Typically asymptomatic but other electrolyte abnormalities (hypokalemia, hypocalcemia) can be present and difficult to assess if symptoms due to Mg++ deficiency alone Most prominent symptom is hypocalcemia (possibly due to ↓ PTH secretion, ↓ 1, 25 -(OH)2 vitamin D levels, skeletal resistance to PTH) Category Mild to Moderate Severe Serum Mg 2+ level (m. Eq/L) 1 – 1. 5 <1
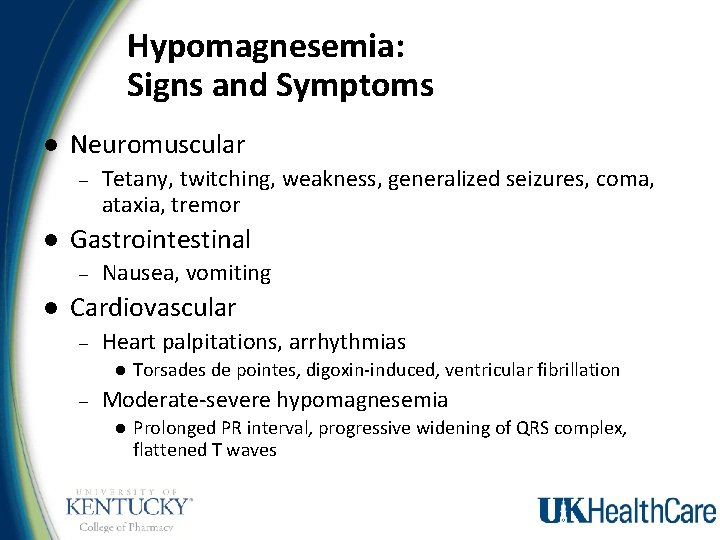
Hypomagnesemia: Signs and Symptoms l Neuromuscular – l Gastrointestinal – l Tetany, twitching, weakness, generalized seizures, coma, ataxia, tremor Nausea, vomiting Cardiovascular – Heart palpitations, arrhythmias l – Torsades de pointes, digoxin-induced, ventricular fibrillation Moderate-severe hypomagnesemia l Prolonged PR interval, progressive widening of QRS complex, flattened T waves
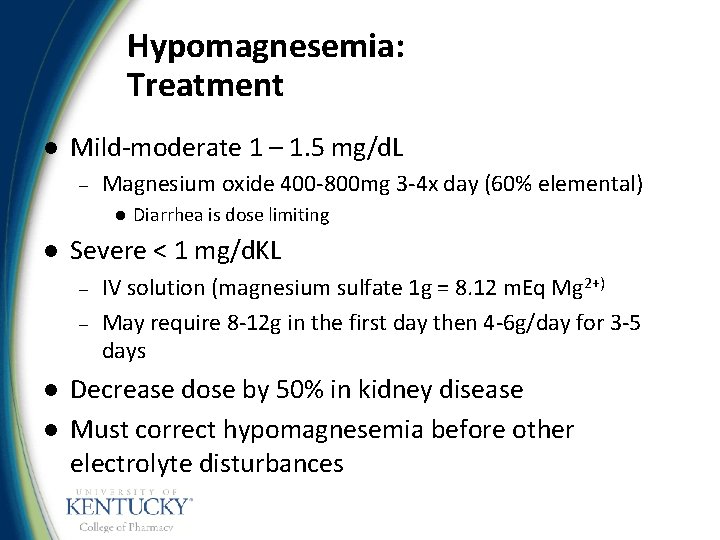
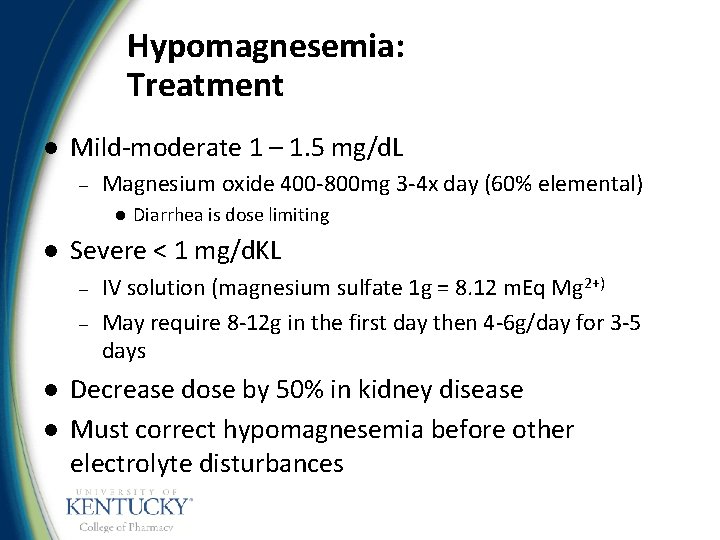
Hypomagnesemia: Treatment l Mild-moderate 1 – 1. 5 mg/d. L – Magnesium oxide 400 -800 mg 3 -4 x day (60% elemental) l l Severe < 1 mg/d. KL – – l l Diarrhea is dose limiting IV solution (magnesium sulfate 1 g = 8. 12 m. Eq Mg 2+) May require 8 -12 g in the first day then 4 -6 g/day for 3 -5 days Decrease dose by 50% in kidney disease Must correct hypomagnesemia before other electrolyte disturbances
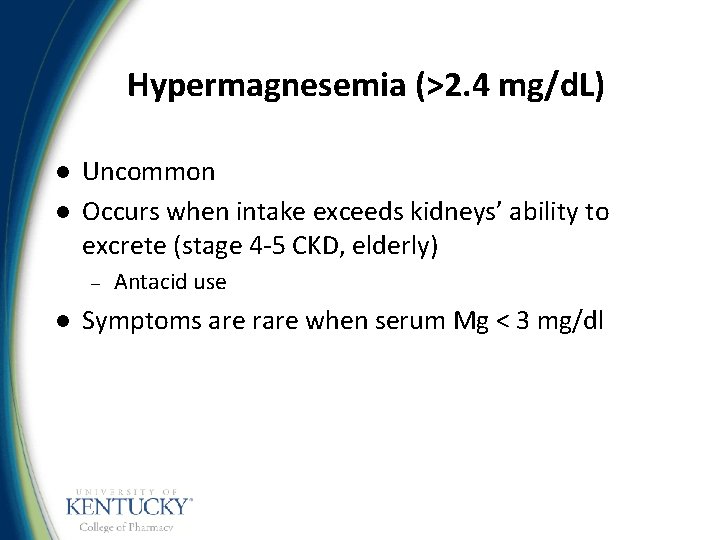
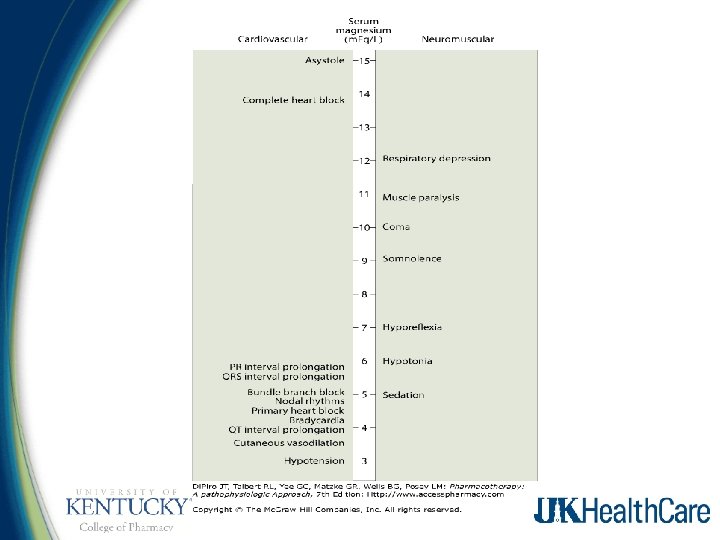
Hypermagnesemia (>2. 4 mg/d. L) l l Uncommon Occurs when intake exceeds kidneys’ ability to excrete (stage 4 -5 CKD, elderly) – l Antacid use Symptoms are rare when serum Mg < 3 mg/dl
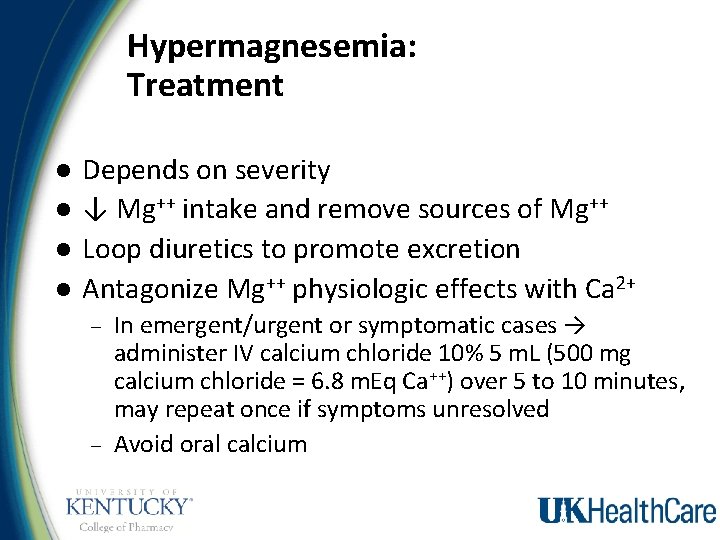
Hypermagnesemia: Treatment l l Depends on severity ↓ Mg++ intake and remove sources of Mg++ Loop diuretics to promote excretion Antagonize Mg++ physiologic effects with Ca 2+ – – In emergent/urgent or symptomatic cases → administer IV calcium chloride 10% 5 m. L (500 mg calcium chloride = 6. 8 m. Eq Ca++) over 5 to 10 minutes, may repeat once if symptoms unresolved Avoid oral calcium
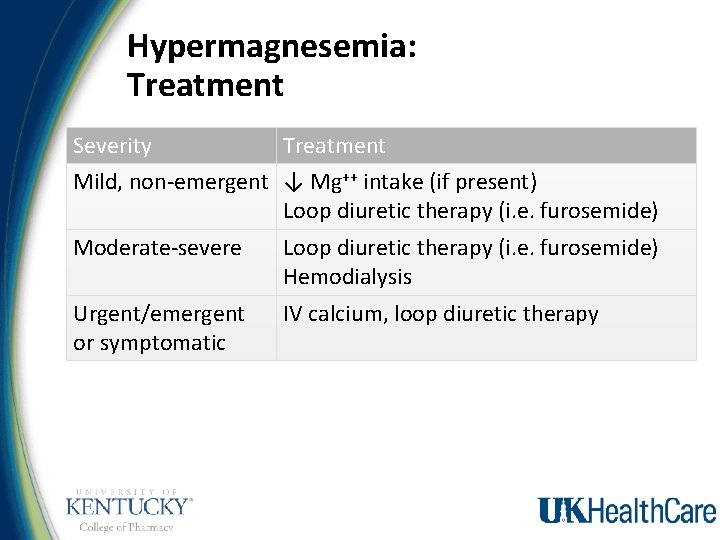
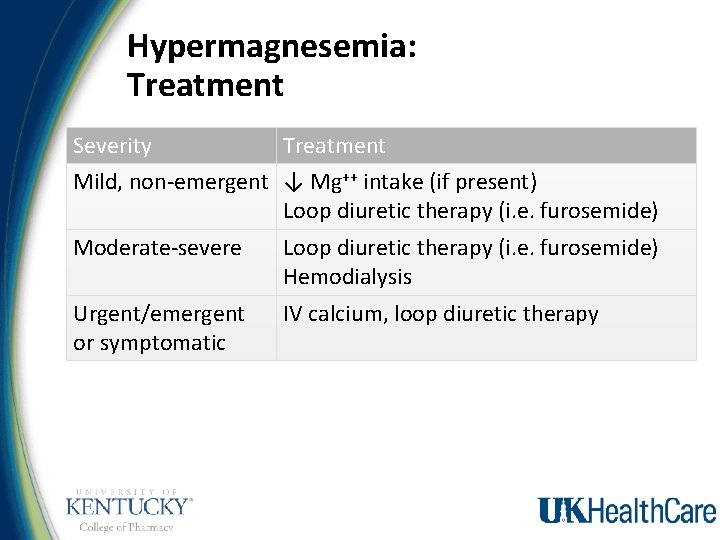
Hypermagnesemia: Treatment Severity Treatment Mild, non-emergent ↓ Mg++ intake (if present) Loop diuretic therapy (i. e. furosemide) Moderate-severe Loop diuretic therapy (i. e. furosemide) Hemodialysis Urgent/emergent or symptomatic IV calcium, loop diuretic therapy
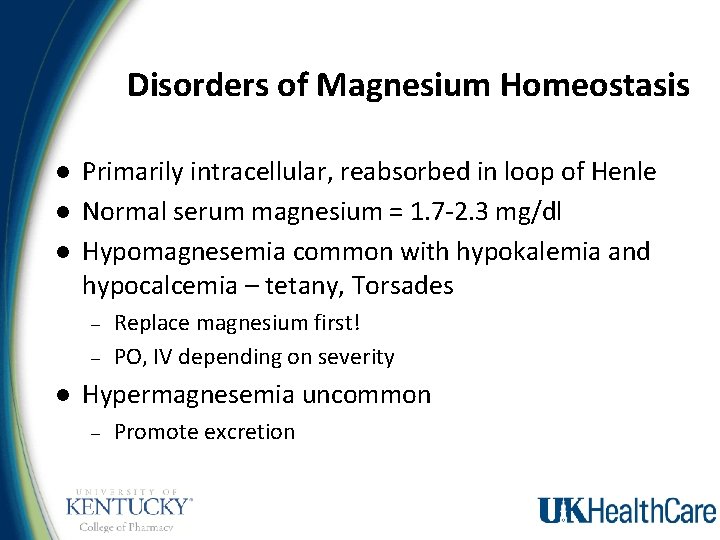
Disorders of Magnesium Homeostasis l l l Primarily intracellular, reabsorbed in loop of Henle Normal serum magnesium = 1. 7 -2. 3 mg/dl Hypomagnesemia common with hypokalemia and hypocalcemia – tetany, Torsades – – l Replace magnesium first! PO, IV depending on severity Hypermagnesemia uncommon – Promote excretion
 Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Bioflix activity homeostasis hormones and homeostasis
Bioflix activity homeostasis hormones and homeostasis Blood chemistry
Blood chemistry Role of lungs and kidneys in acid base balance
Role of lungs and kidneys in acid base balance Fluid calculation formula
Fluid calculation formula An atypical accumulation of fluid in the interstitial space
An atypical accumulation of fluid in the interstitial space Anp
Anp Normal electrolytes values
Normal electrolytes values Water electrolyte imbalance
Water electrolyte imbalance Weak electrolytes examples
Weak electrolytes examples Hf electrolyte
Hf electrolyte Freddy santoso
Freddy santoso Signs hyperkalemia
Signs hyperkalemia Spintek anthracite
Spintek anthracite Degree of dissociation of electrolyte depends on
Degree of dissociation of electrolyte depends on What is electrolyte
What is electrolyte Electrolyte replacement therapy
Electrolyte replacement therapy Chapter 28 human systems and homeostasis
Chapter 28 human systems and homeostasis The term homeostasis literally means
The term homeostasis literally means Osmoregulation in plants
Osmoregulation in plants Body organization and homeostasis
Body organization and homeostasis Homeostasis and cell transport
Homeostasis and cell transport Copper oxide and hydrogen reaction
Copper oxide and hydrogen reaction How does a positive ion form
How does a positive ion form Mass of kclo3
Mass of kclo3 React with water
React with water Magnesium and beryllium
Magnesium and beryllium Acute fulminating preeclampsia
Acute fulminating preeclampsia Solubility rules table
Solubility rules table Preparation and standardization of potassium permanganate
Preparation and standardization of potassium permanganate Valence electrons of potassium
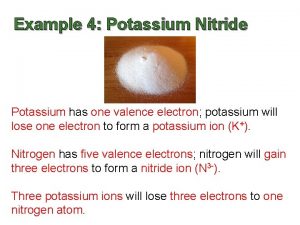
Valence electrons of potassium Potassium bromine and krypton
Potassium bromine and krypton Silver nitrate and potassium chloride
Silver nitrate and potassium chloride Chlorine gas and potassium bromide
Chlorine gas and potassium bromide Halogen family
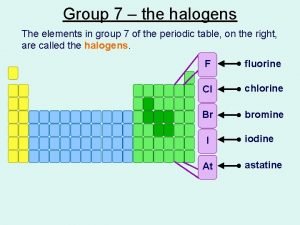
Halogen family Copper sulfate and potassium iodide precipitate
Copper sulfate and potassium iodide precipitate