Diagnosis and Management of Chronic Fatigue Syndrome CFSME



- Slides: 63
Diagnosis and Management of Chronic Fatigue Syndrome (CFS/ME) Epsom GP Education Programme 13 November 2012 Dr Amolak Bansal, Consultant Immunologist Dr Yasmin Mullick, Clinical Psychologist Karen Tweed, Clinical Nurse Specialist
Sutton/St Helier Chronic Fatigue Service Clinical Team Dr Amolak Bansal - Consultant in Immunology Karen Tweed - Clinical Nurse Specialist Dr Zoe Clyde - Consultant Clinical Psychologist Dr Yasmin Mullick - Clinical Psychologist Clare Inglis - Physiotherapist (from Dec. 2012)
Outline Integrating CFS/ME Patient Care Session 1 • • Understanding CFS/ME Diagnosing CFS/ME in primary care • • Interventions for fatigue management Involving community services • Referral to St Helier/Sutton CFS/ME Service for specialist intervention Long term CFS/ME self management supported in primary care • Session 2: Session 3
Session 1 Understanding CFS/ME & Diagnosing CFS/ME in Primary Care Dr Bansal Consultant in Immunology
Fatigued Patients in Primary Care • High presentation of TATT’s • Desire for medicine to improve fatigue • Frustration of negative test results • Fear of something more sinister • Impact on occupational functioning/medical • • • cert’s Depression Impatience for recovery High incidence of healthcare appointments
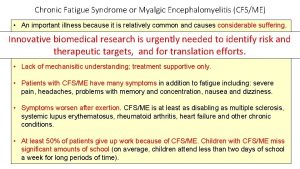
Prevalence 0. 2 – 0. 4% of the population are affected by CFS/ME (i. e. 20 - 40 patients in a G. P. practice of 10, 000)

CFS/ME Diagnostic Criteria All of the following: • Debilitating persistent or relapsing fatigue for at least 4 months, but not life-long • Not the result of ongoing exertion and not substantially alleviated by rest • Post-exertional malaise and/or fatigue, typically delayed (e. g. by at least 24 hours) with slow recovery over several days • Severe enough to cause substantial reduction in previous levels of occupational, educational, social or personal activities.
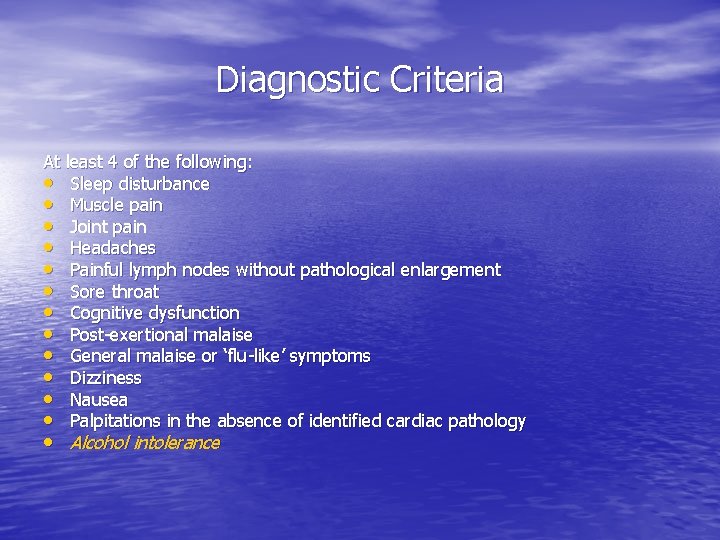
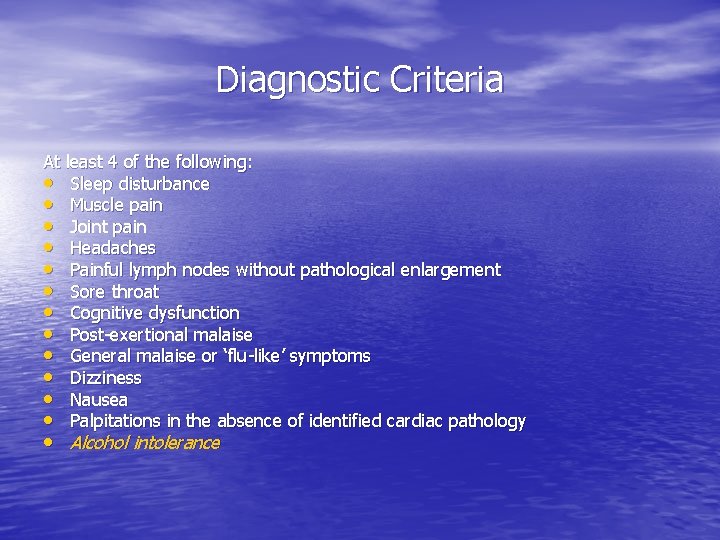
Diagnostic Criteria At least 4 of the following: • Sleep disturbance • Muscle pain • Joint pain • Headaches • Painful lymph nodes without pathological enlargement • Sore throat • Cognitive dysfunction • Post-exertional malaise • General malaise or ‘flu-like’ symptoms • Dizziness • Nausea • Palpitations in the absence of identified cardiac pathology • Alcohol intolerance
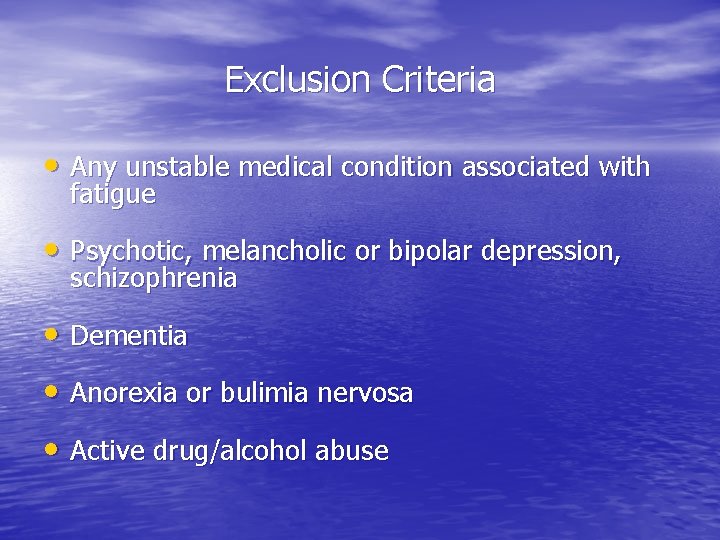
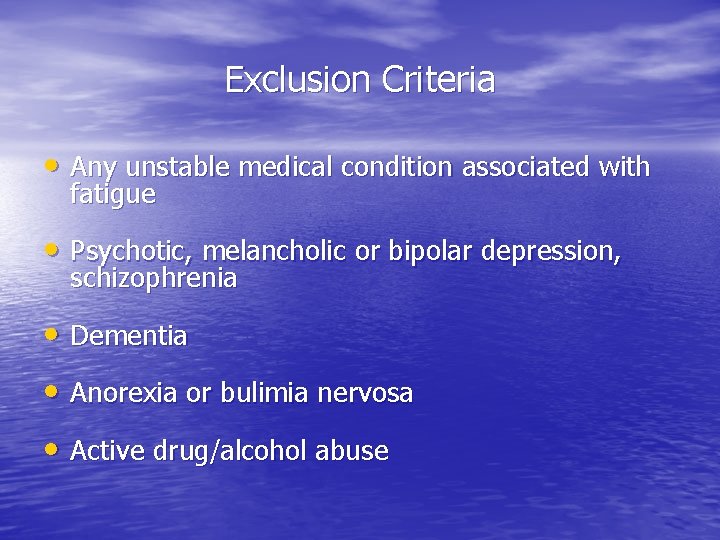
Exclusion Criteria • Any unstable medical condition associated with fatigue • Psychotic, melancholic or bipolar depression, schizophrenia • Dementia • Anorexia or bulimia nervosa • Active drug/alcohol abuse
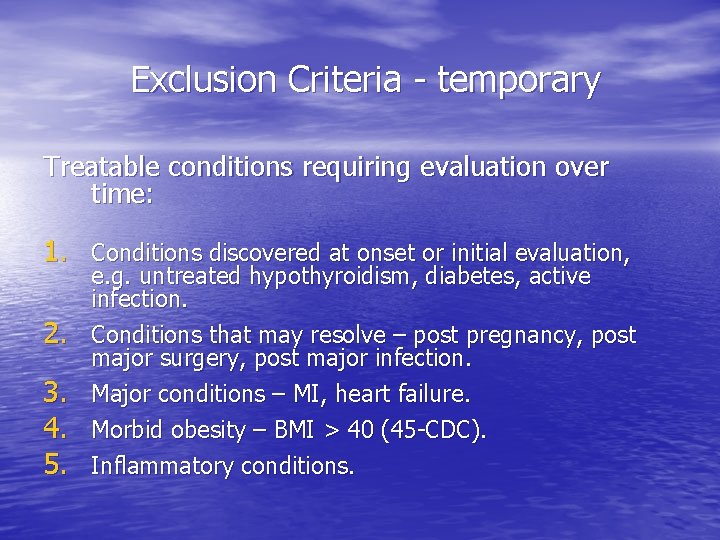
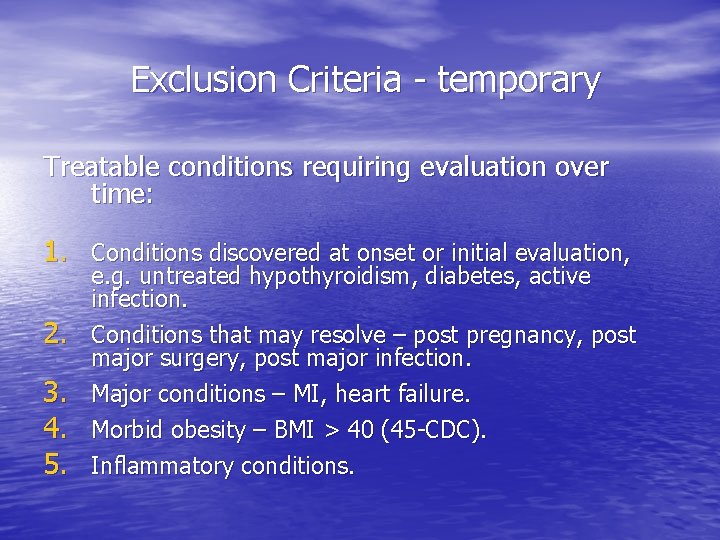
Exclusion Criteria - temporary Treatable conditions requiring evaluation over time: 1. Conditions discovered at onset or initial evaluation, 2. 3. 4. 5. e. g. untreated hypothyroidism, diabetes, active infection. Conditions that may resolve – post pregnancy, post major surgery, post major infection. Major conditions – MI, heart failure. Morbid obesity – BMI > 40 (45 -CDC). Inflammatory conditions.
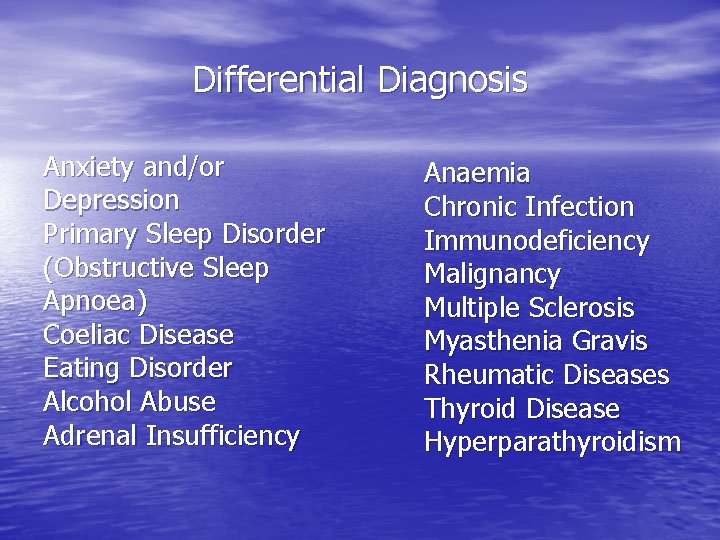
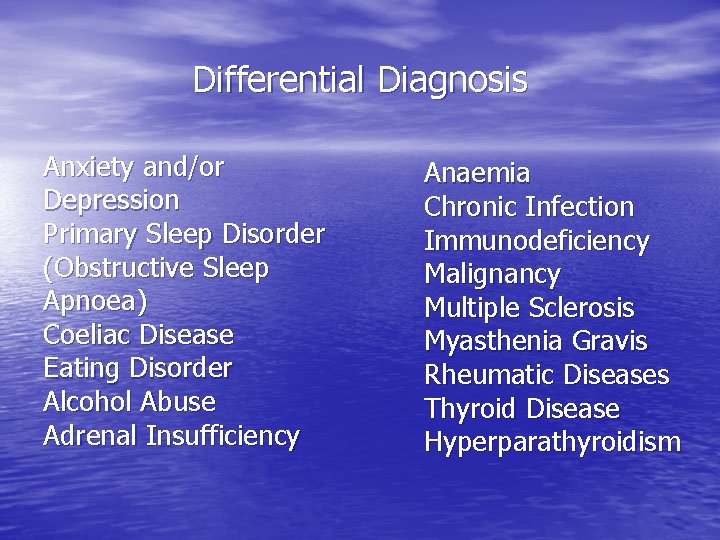
Differential Diagnosis Anxiety and/or Depression Primary Sleep Disorder (Obstructive Sleep Apnoea) Coeliac Disease Eating Disorder Alcohol Abuse Adrenal Insufficiency Anaemia Chronic Infection Immunodeficiency Malignancy Multiple Sclerosis Myasthenia Gravis Rheumatic Diseases Thyroid Disease Hyperparathyroidism
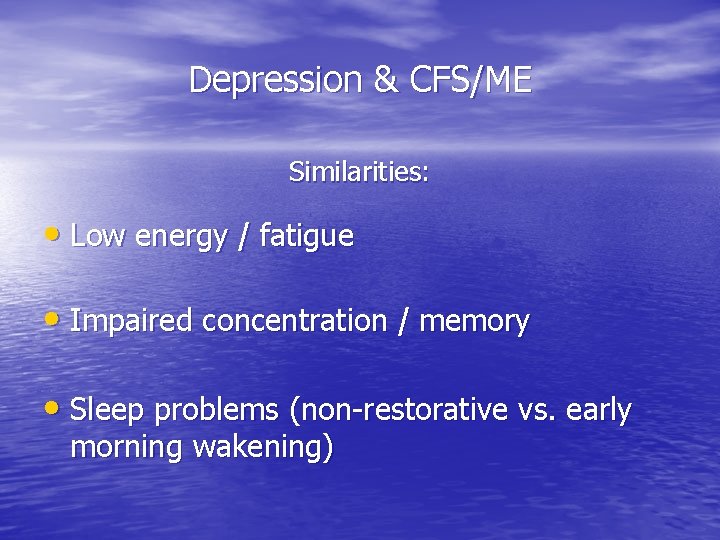
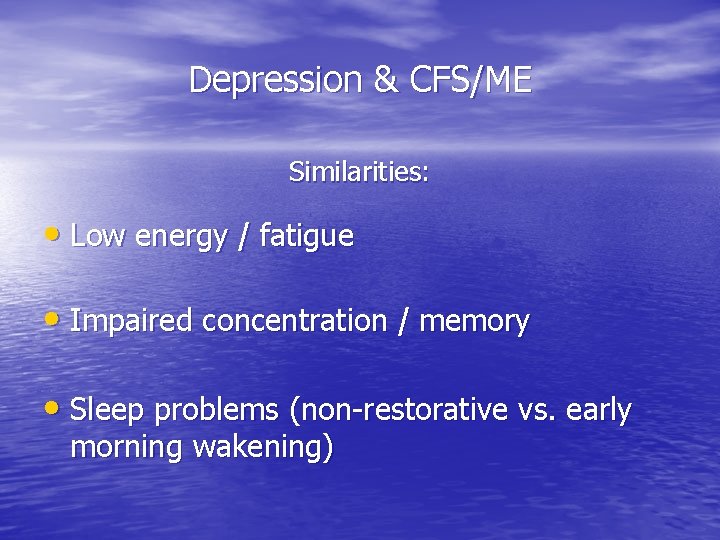
Depression & CFS/ME Similarities: • Low energy / fatigue • Impaired concentration / memory • Sleep problems (non-restorative vs. early morning wakening)
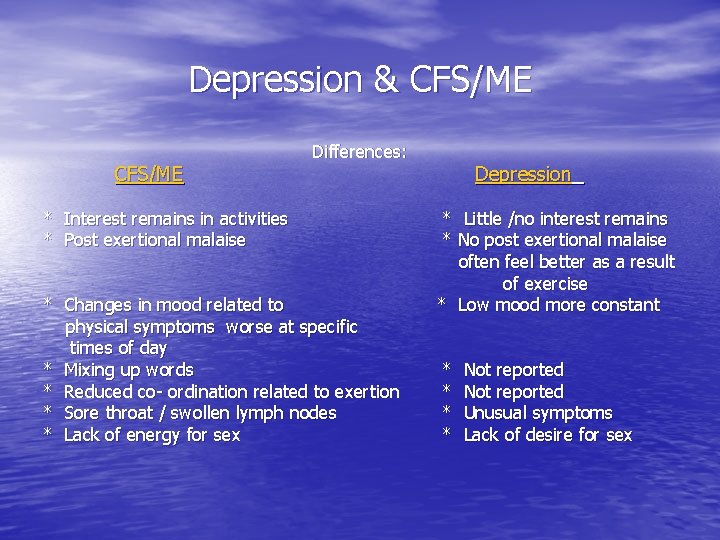
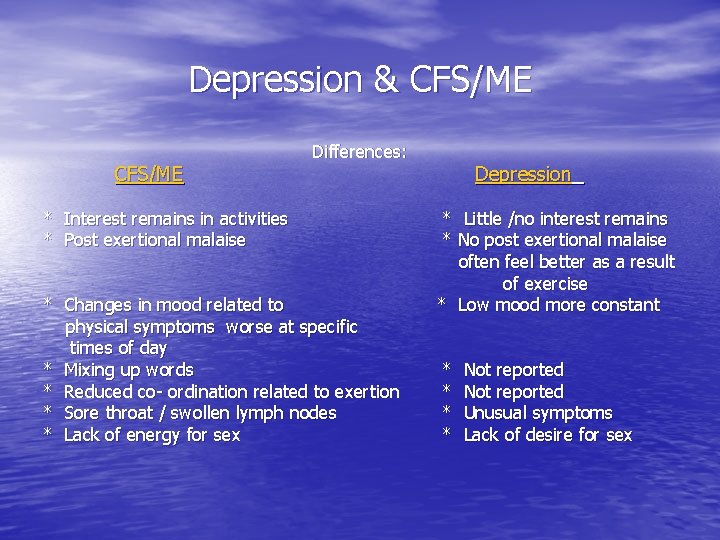
Depression & CFS/ME Differences: * Interest remains in activities * Post exertional malaise * Changes in mood related to physical symptoms worse at specific times of day * Mixing up words * Reduced co- ordination related to exertion * Sore throat / swollen lymph nodes * Lack of energy for sex Depression * Little /no interest remains * No post exertional malaise often feel better as a result of exercise * Low mood more constant * * Not reported Unusual symptoms Lack of desire for sex
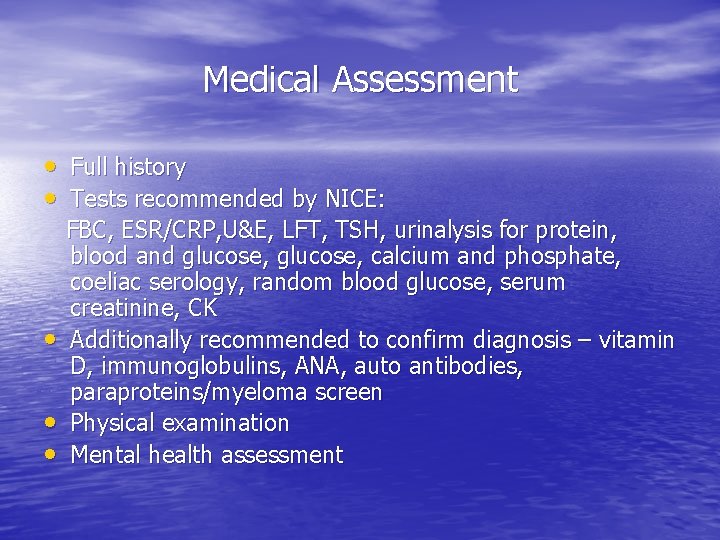
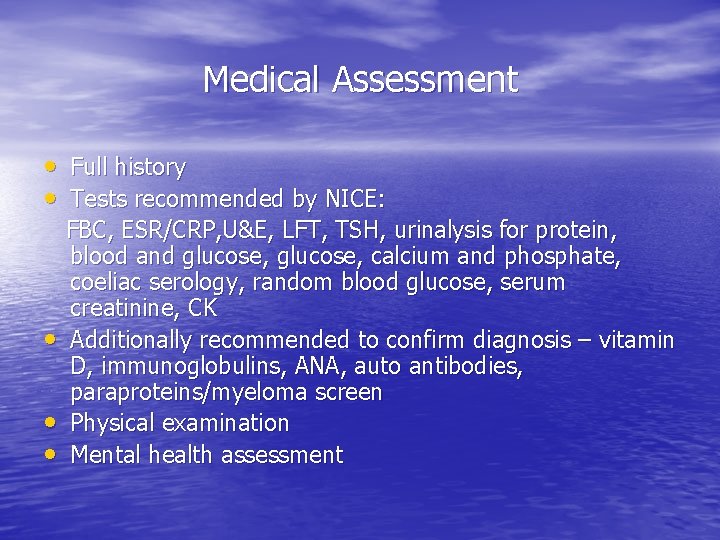
Medical Assessment • Full history • Tests recommended by NICE: • • • FBC, ESR/CRP, U&E, LFT, TSH, urinalysis for protein, blood and glucose, calcium and phosphate, coeliac serology, random blood glucose, serum creatinine, CK Additionally recommended to confirm diagnosis – vitamin D, immunoglobulins, ANA, auto antibodies, paraproteins/myeloma screen Physical examination Mental health assessment
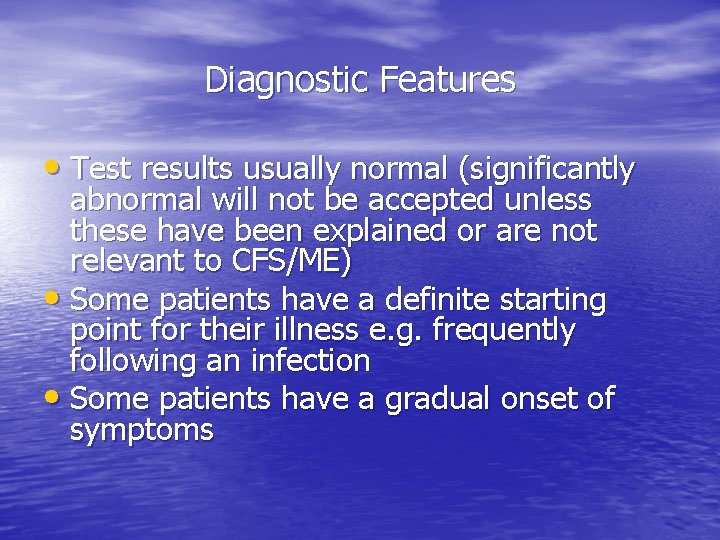
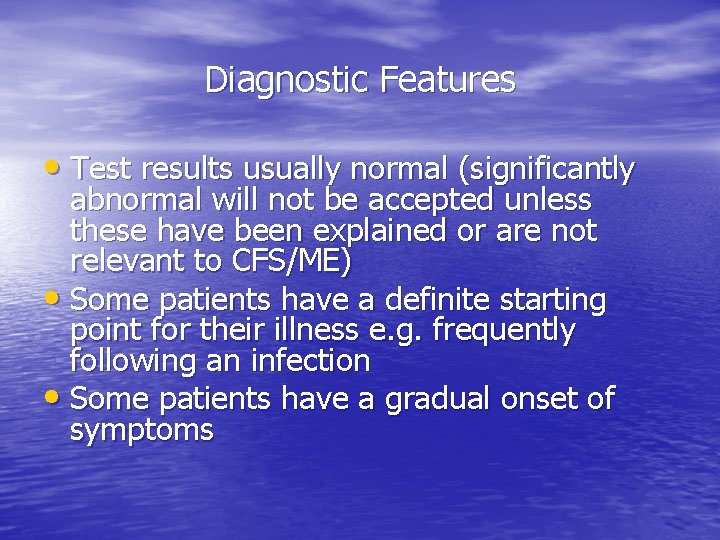
Diagnostic Features • Test results usually normal (significantly abnormal will not be accepted unless these have been explained or are not relevant to CFS/ME) • Some patients have a definite starting point for their illness e. g. frequently following an infection • Some patients have a gradual onset of symptoms

Diagnosing Levels of Severity Mild: • Mobile • Self caring • Light domestic tasks with difficulty • Working/education • Little or no leisure/social activity
Diagnosing Levels of Severity • • Moderate: Reduced mobility Restricted in ADL’s Symptoms and abilities fluctuate through peaks and troughs Frequently have stopped work
Diagnosing Levels of Severity • • Severe: Unable / very limited in carrying out activities for themselves Severe cognitive difficulties May be dependent on wheelchair for mobility Often unable to leave the house
Diagnosing Levels of Severity • • • Very severe: Bed bound Dependent for care Extreme sensitivities e. g. to light, noise etc.
Dangers of Diagnostic Labels • Patients need to have a definite diagnosis to be able to move on • Clear evidence required showing diagnostic criteria are met • Once applied, can be difficult to remove! • Label can increase anxiety – media misinformation • Danger of attribution of new symptoms to CFS/ME – new symptoms need investigating on their own merits
Precipitating Factors Infections: • Viral Infections – EBV, HHV 6, viral hepatitis, • • • influenza, enteroviruses, parvovirus. Bacterial Infections – salmonella, brucella, coxiella. Spirochetes – lyme disease. Protozoa – toxoplasmosis. Fungi – little/no evidence of candida allergy. Immunizations – rare reports only (HBV, flu).
Other Precipitating Factors • Life Events – Significant negative events are more likely to trigger mood disorder. Stress at the time of a triggering event may increase the chance of CFS/ME. • Physical Injuries – Are more likely to trigger Fibromyalgia but CFS/ME has been reported after physical or operative trauma. • Environmental Toxins
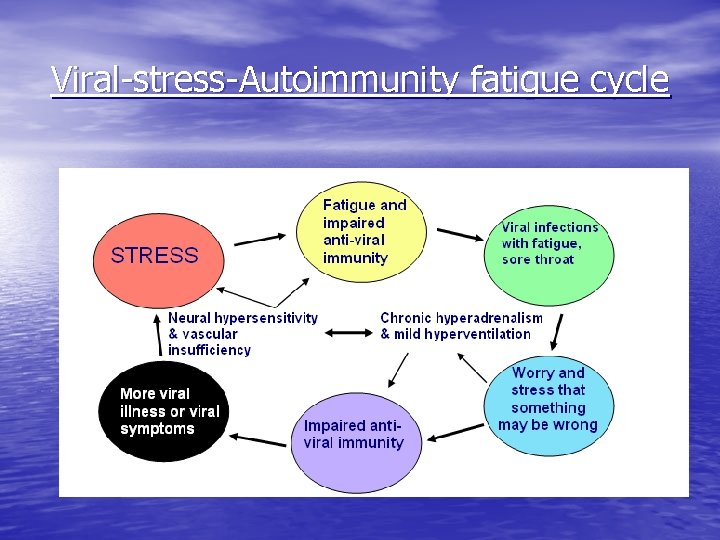
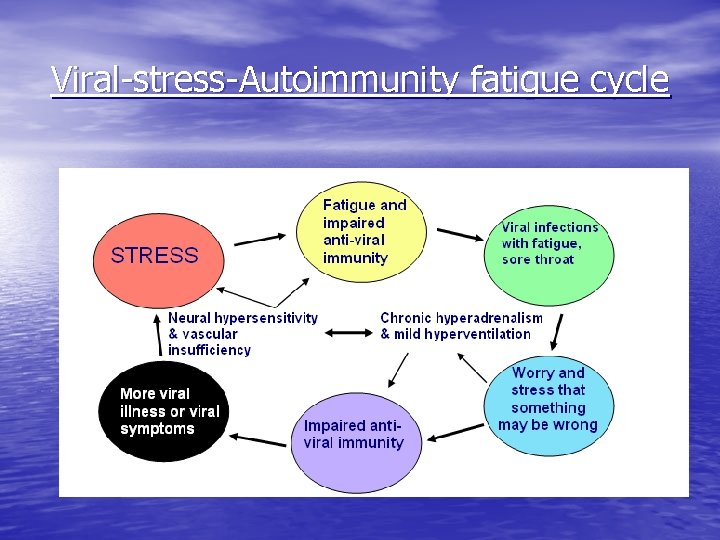
Viral-stress-Autoimmunity fatigue cycle
Current thinking about CFS • Viral infection – unlikely a retorvirus • PACE trial – benefits of CBT and GET • Benefits of Rituximab – B cell depletion • Autoimmunity – Ig. M rather than Ig. G • Immune deficiency – cellular > humoral • Muscle dysfunction – impaired energy • Post exertional malaise – PME XS
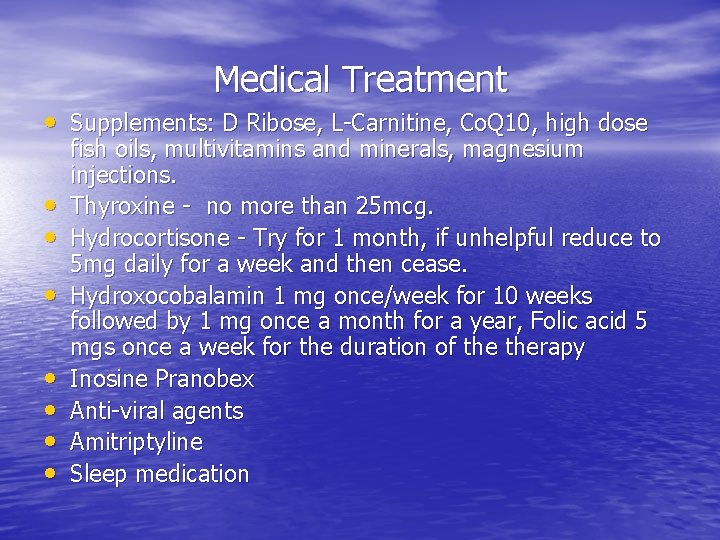
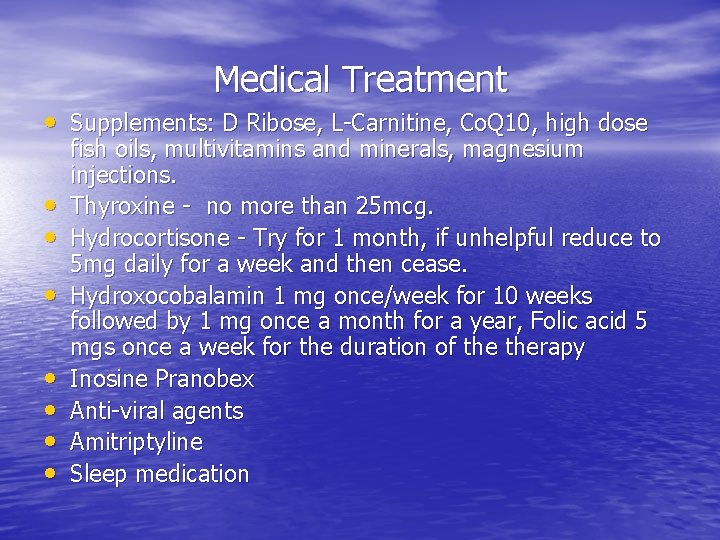
Medical Treatment • Supplements: D Ribose, L-Carnitine, Co. Q 10, high dose • • fish oils, multivitamins and minerals, magnesium injections. Thyroxine - no more than 25 mcg. Hydrocortisone - Try for 1 month, if unhelpful reduce to 5 mg daily for a week and then cease. Hydroxocobalamin 1 mg once/week for 10 weeks followed by 1 mg once a month for a year, Folic acid 5 mgs once a week for the duration of therapy Inosine Pranobex Anti-viral agents Amitriptyline Sleep medication
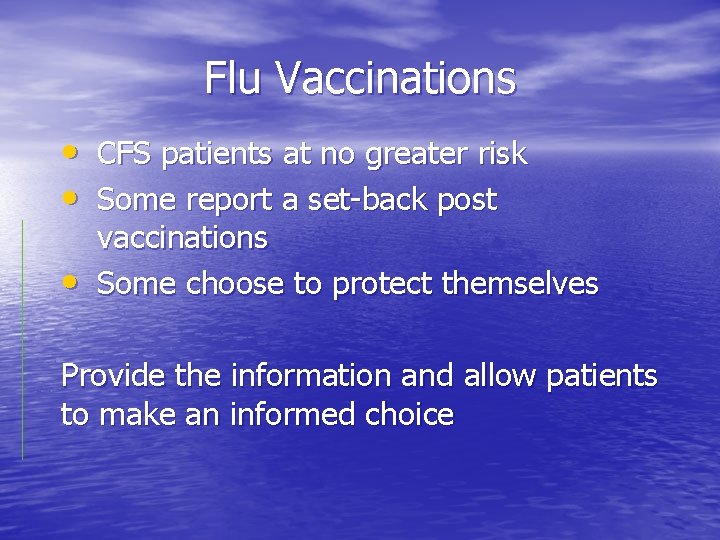
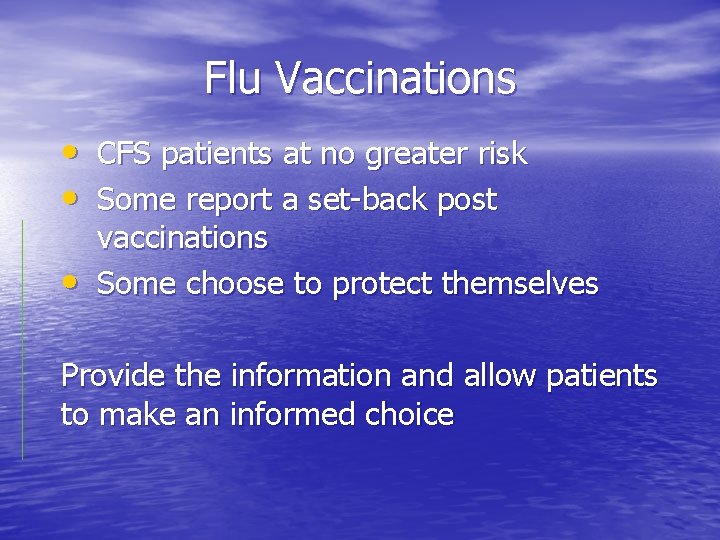
Flu Vaccinations • CFS patients at no greater risk • Some report a set-back post • vaccinations Some choose to protect themselves Provide the information and allow patients to make an informed choice
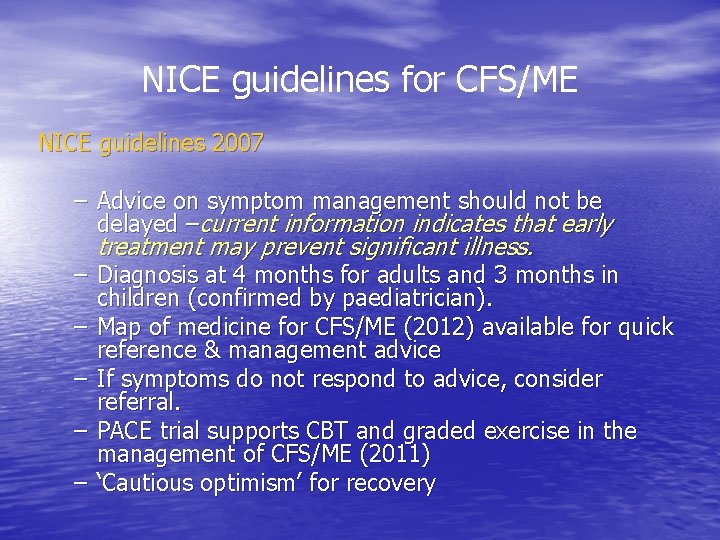
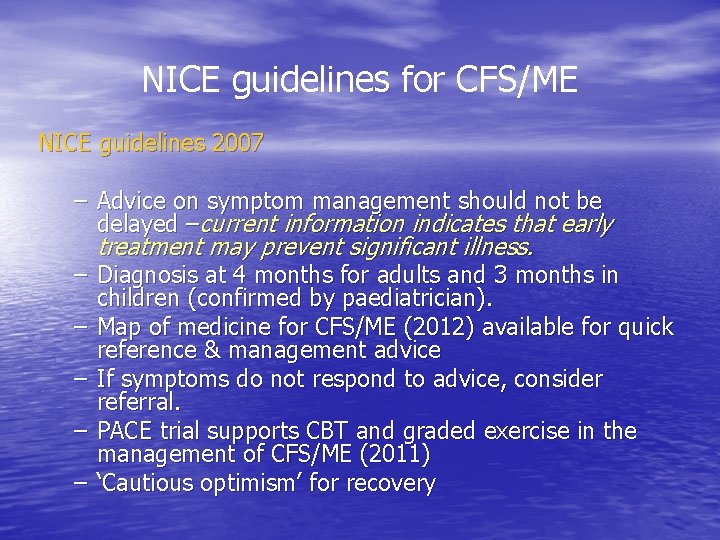
NICE guidelines for CFS/ME NICE guidelines 2007 – Advice on symptom management should not be delayed –current information indicates that early treatment may prevent significant illness. – Diagnosis at 4 months for adults and 3 months in children (confirmed by paediatrician). – Map of medicine for CFS/ME (2012) available for quick reference & management advice – If symptoms do not respond to advice, consider referral. – PACE trial supports CBT and graded exercise in the management of CFS/ME (2011) – ‘Cautious optimism’ for recovery
Questions?
Session 2 Interventions for fatigue management & Involving community services Dr Yasmin Mullick Clinical Psychologist
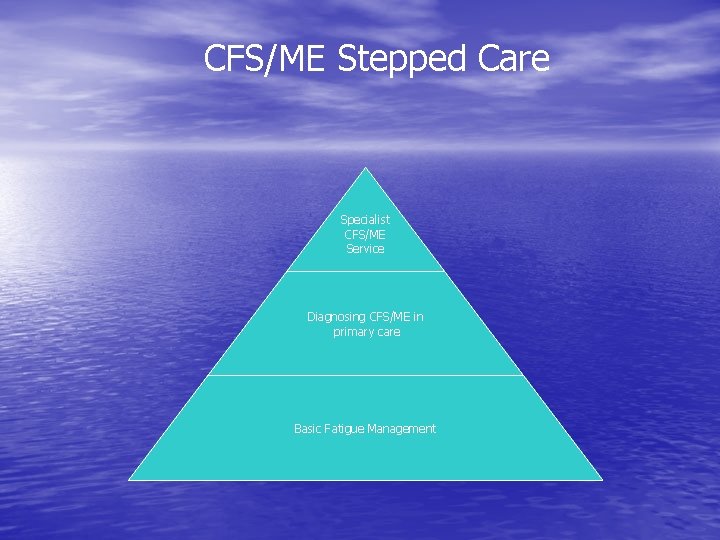
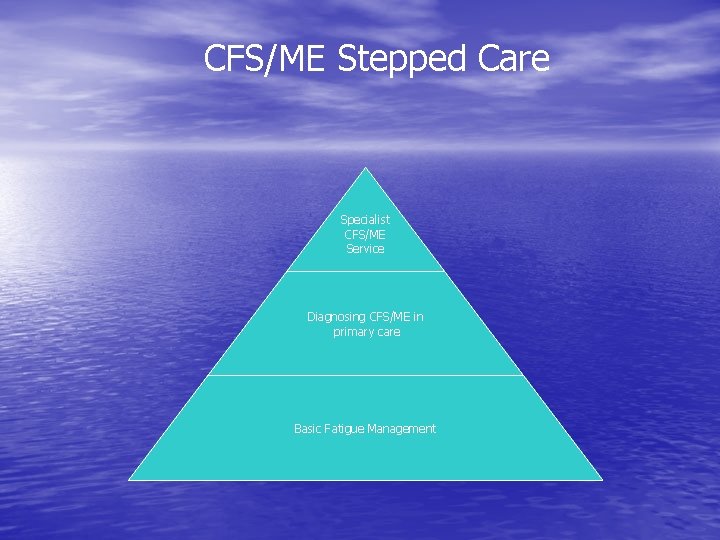
CFS/ME Stepped Care Specialist CFS/ME Service Diagnosing CFS/ME in primary care Basic Fatigue Management
Recovery Goal CFS/ME symptom management & Sustaining a good quality of life
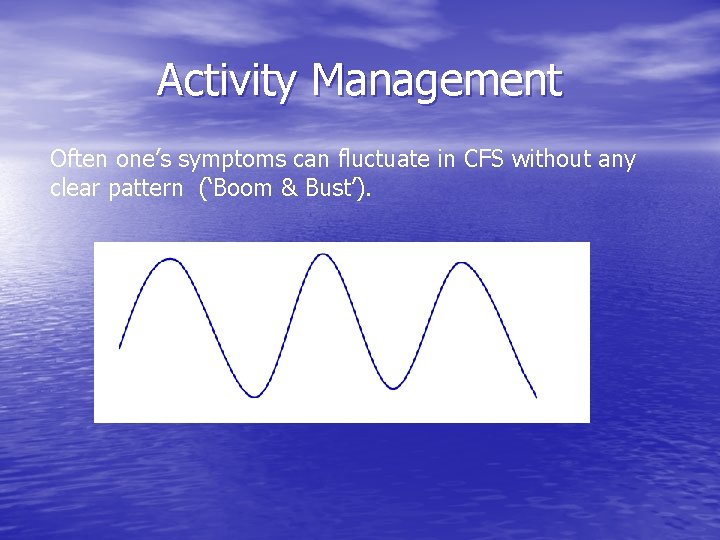
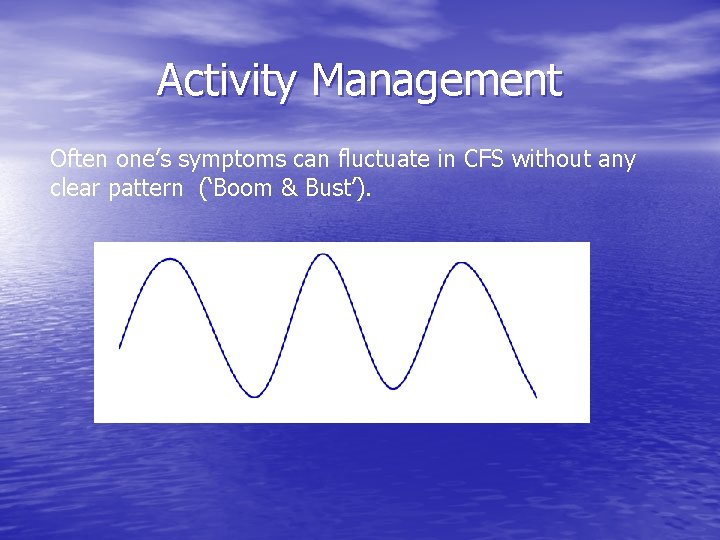
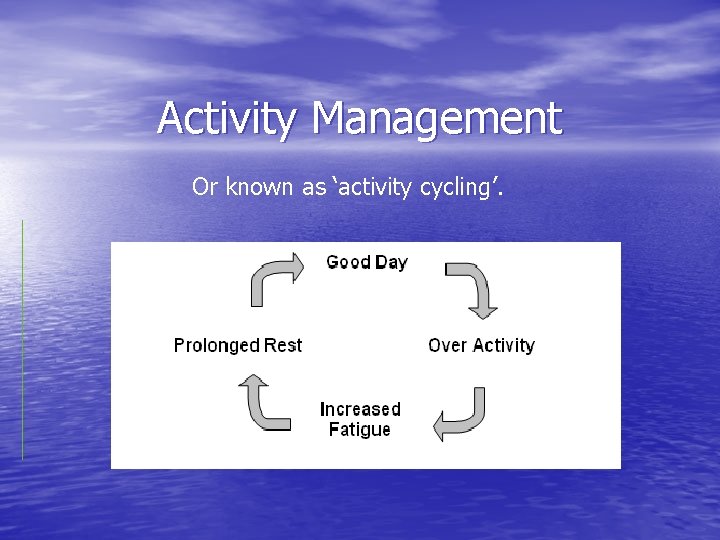
Activity Management Often one’s symptoms can fluctuate in CFS without any clear pattern (‘Boom & Bust’).
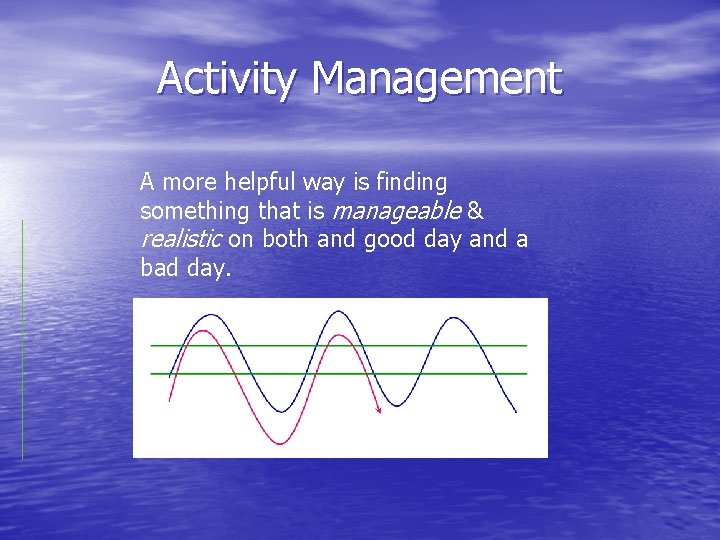
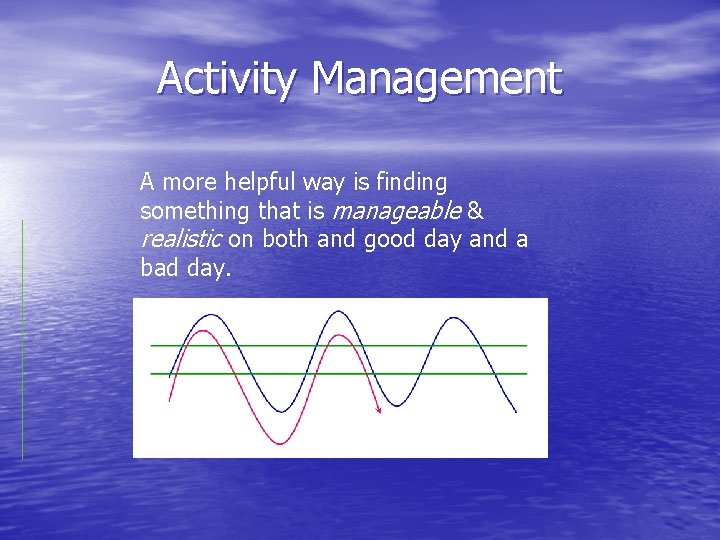
Activity Management A more helpful way is finding something that is manageable & realistic on both and good day and a bad day.
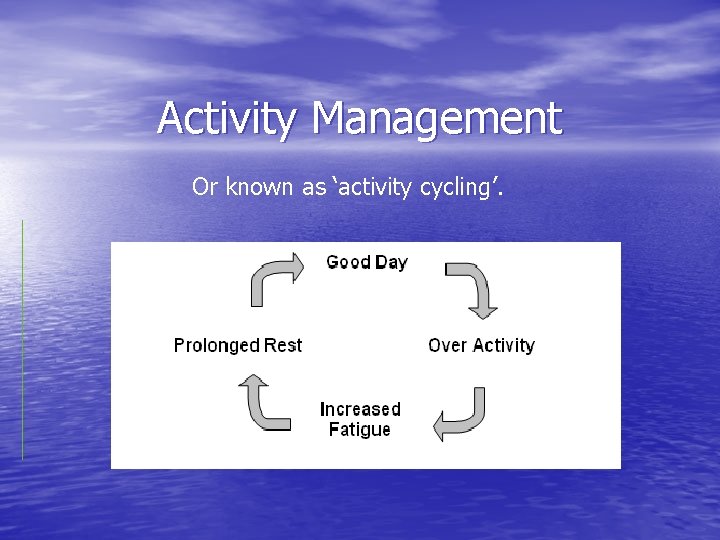
Activity Management Or known as ‘activity cycling’.
Basic Fatigue Management Remember RAISE to aid recovery • R – Rest/relaxation • A – Activity management • I – Information • S – Sleep • E - Exercise
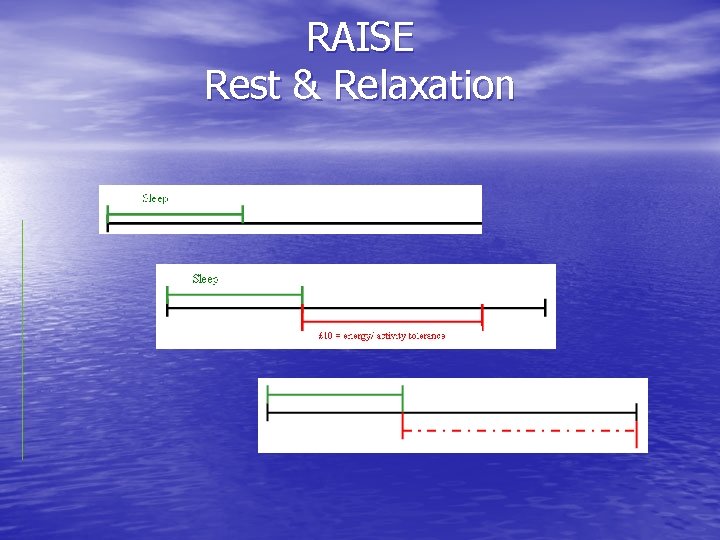
RAISE • • R – Rest & relaxation Use regular rest breaks to manage activity and energy Utilise breathing exercises Practise daily formal relaxation Prolonged rest not necessary
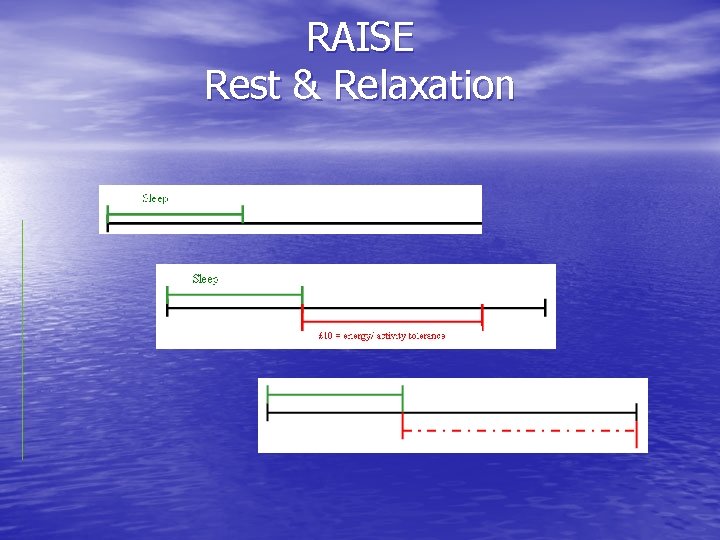
RAISE Rest & Relaxation
RAISE • • A – Activity Management Avoid boom and bust cycle Find sustainable level of activity and gradually increase Physical, mental and emotional activity all use energy Encourage balance – engage in necessary and enjoyable activities
RAISE I – Information • Dispel myths e. g. mortality fears, media images, progressive illness • Reduce uncertainty and stigma • Validate condition (NICE 2007) • Enable individuals to make informed choices about treatment • Support individuals making lifestyle changes
RAISE S - Sleep • Promote good sleep hygiene • Address sleep problems • Discourage oversleeping • Original sleep hours apply • Consider medication if appropriate
RAISE E - Exercise • Prevention of deconditioning • Prevention of reduced stamina and fitness • Important to find sustainable level depending on severity of symptoms and increase gradually.
Management of severely affected • Use advice for basic fatigue management • Monitor general physical well being - pressure • • • areas, deconditioning, nutrition (e. g. Vit D) Treat symptomatically Refer to community services, e. g. physiotherapy, occupational therapy, social services (equipment) Refer to specialist service when patient physically able to attend appointments
Diagnosing CFS/ME in primary care • Diagnose CFS/ME where possible • Medical treatment options for CFS/ME symptom • • management Basic fatigue management advice (RAISE) Advice for employers www. nhsplus. nhs. uk Local M. E. support groups IAPT – CBT for anxiety and depression
Questions?
Session 3 Referral to St Helier/Sutton CFS/ME for specialist intervention & Long term self management of CFS/ME in primary care Karen Tweed Clinical Nurse Specialist
Patient hopes and expectations of a specialist CFS/ME Service • GP referral to a specialist service highly valued by • • the participants Information about CFS/ME during early stages of illness important to help manage uncertainty Suggests a need for more reassurance and positive advice during the waiting period Patients hopes and expectations of a specialist chronic fatigue syndrome/ME service: a qualitative study. Fam Pract. 2011 Oct; 28(5): 572 -8. Epub 2011 May 9. Mc. Dermott C, Lynch J, Leydon GM.

Specialist CFS/ME Service • • CFS/ME First Steps Seminar CFS/ME Lifestyle Management Programme CBT for CFS/ME G. E. T. Medical support Activity management Liaison & consultation
First Steps Seminar After GP’s confirm CFS/ME diagnosis, patients are invited to attend our First Steps Seminar: • 1 ½ hour seminar • MDT led • Capacity 20 • 2 x month
First Steps Seminar What is CFS? Viral/stress/fatigue cycle Biopsychosocial model Activity Management Treatment Options at Sutton / St Helier CFS Service Getting Started Opting in Appointment sent 6 -8 weeks
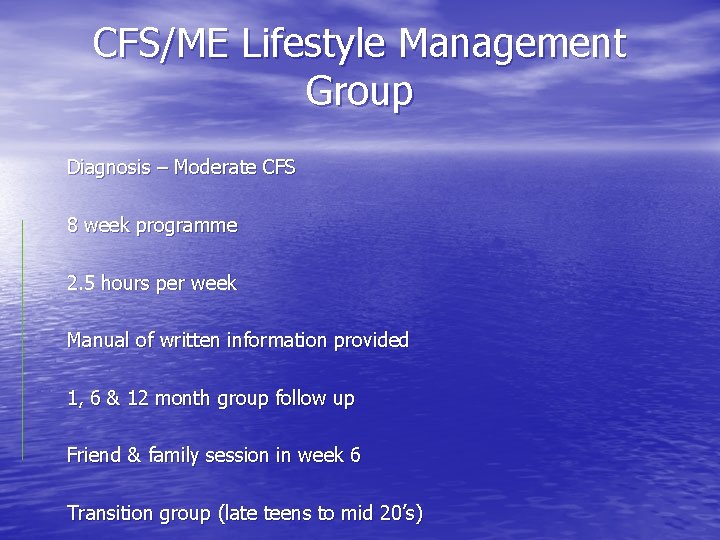
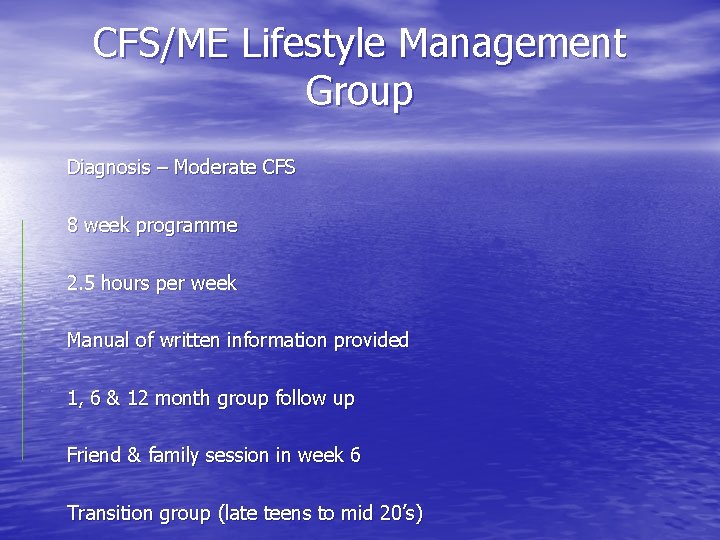
CFS/ME Lifestyle Management Group Diagnosis – Moderate CFS 8 week programme 2. 5 hours per week Manual of written information provided 1, 6 & 12 month group follow up Friend & family session in week 6 Transition group (late teens to mid 20’s)
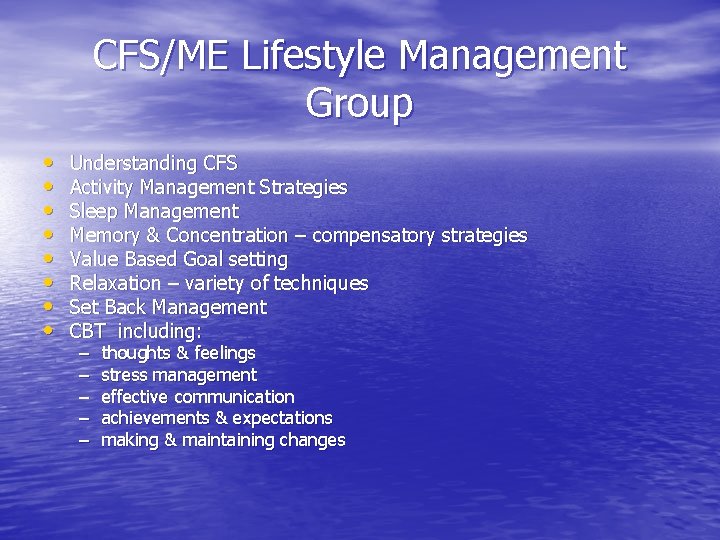
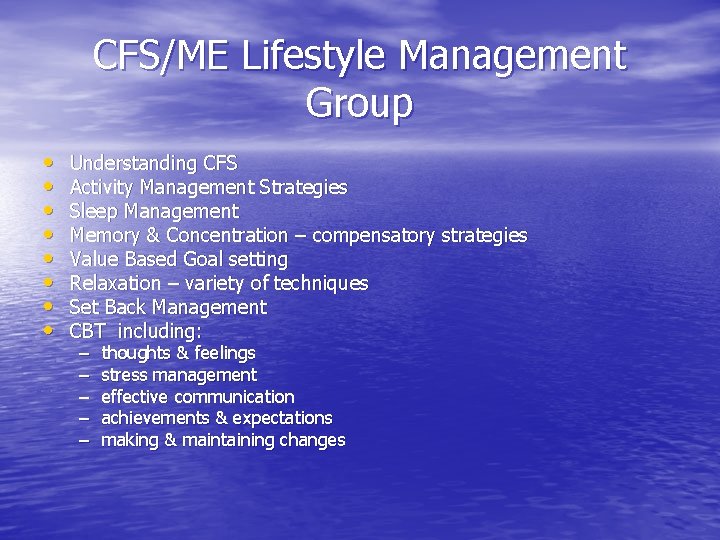
CFS/ME Lifestyle Management Group • • Understanding CFS Activity Management Strategies Sleep Management Memory & Concentration – compensatory strategies Value Based Goal setting Relaxation – variety of techniques Set Back Management CBT including: – – – thoughts & feelings stress management effective communication achievements & expectations making & maintaining changes
Specialist CFS/ME Interventions • CBT for CFS/ME • G. E. T
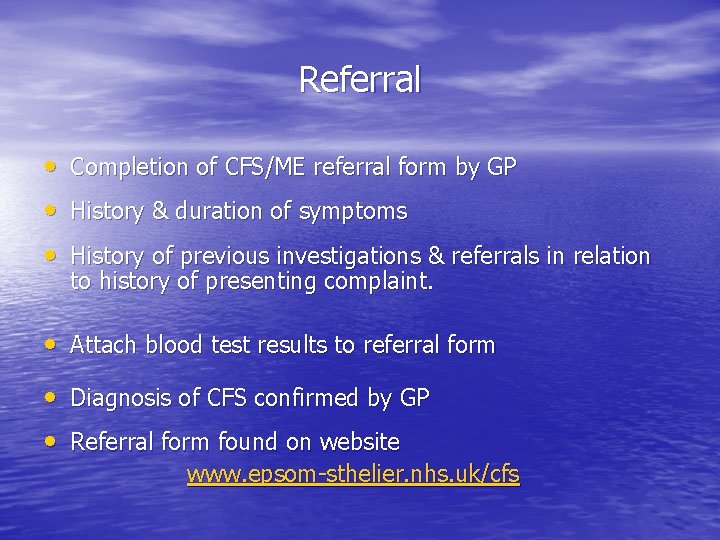
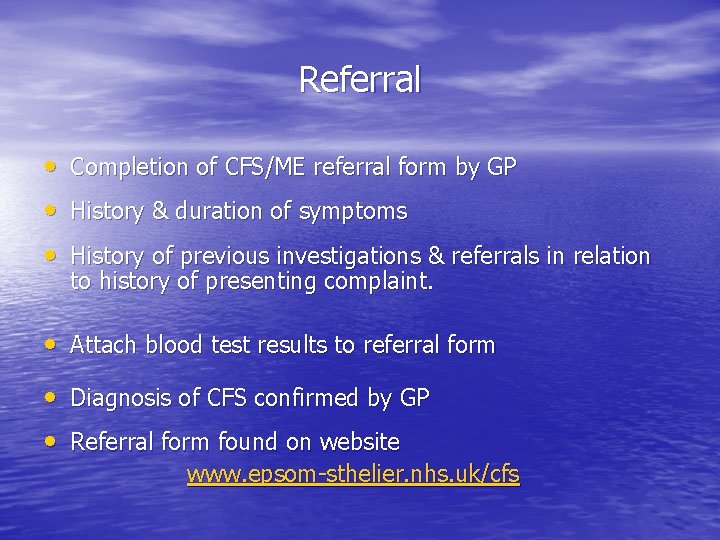
Referral • Completion of CFS/ME referral form by GP • History & duration of symptoms • History of previous investigations & referrals in relation to history of presenting complaint. • Attach blood test results to referral form • Diagnosis of CFS confirmed by GP • Referral form found on website www. epsom-sthelier. nhs. uk/cfs
Triage of Referrals • Completed by Consultant/ CNS • Confirmation of diagnosis & completed blood tests – booked into First Steps Seminar • Unclear diagnosis or additional medical complications – booked into to see Consultant or Clinical Nurse specialist • Severe CFS/ME patients – domically service on hold. CFS team to liaise/ consult with local MDT’s where appropriate
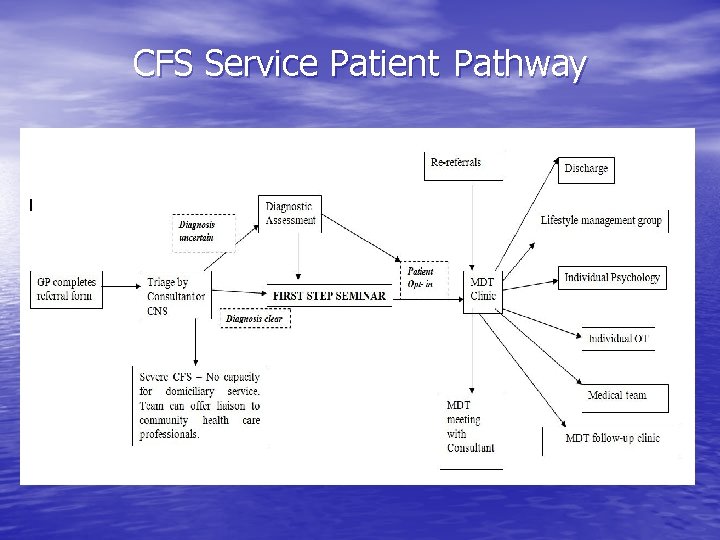
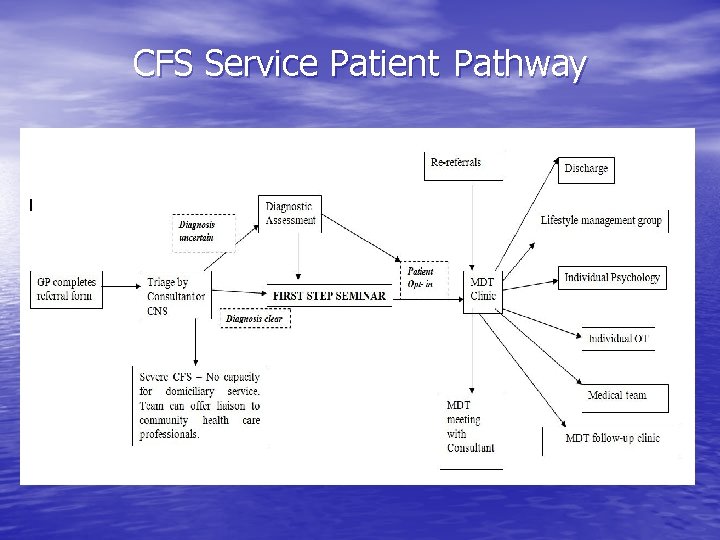
CFS Service Patient Pathway
CFS/ME Setback Management • Don’t panic • Identify possible triggers • No new advice • Increase rest and relaxation • Monitor activity – may stay the same or reduce • Involve support where appropriate • Recognise distressing thoughts. • Symptom control during acute episode
CFS Service • Aim is to offer information, advice and support • • to facilitate long-term self management of CFS/ME based on NICE guidelines Patients discharged for non attendance/nonengagement Service unable to support patients long term Re-referrals assessed on case by case basis Cautious optimism for recovery (NICE).
Service strengths • High level of patient satisfaction • Good group outcomes • Offer individual care pathway • Contributing to National Outcome Database - BACME • Links with local support groups • Teaching and training events • Research
Service Limitations • Small team (2. 9 wte) covering wide area (6 PCT’s) • Currently focused on those able to attend clinic, i. e. Mild/moderate CFS/ME • No service in area for children and young people currently
Summary • Aim to increase understanding of diagnosis and management of CFS • Aim to increase awareness of the CFS service and consider how we can work better together to support people with CFS/ME.
Recovery “If you have had to prove you are ill, it is very difficult to get well”. Dr Brian Marien (Barts & The London)
Any questions? How can we work better together? What would you like from us? www. epsom-sthelier. nhs. uk/cfs
 Fibromyalgia vs chronic fatigue
Fibromyalgia vs chronic fatigue Classification of antianginal drugs
Classification of antianginal drugs 3 part nursing diagnosis examples
3 part nursing diagnosis examples Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnosis
Types of nursing diagnosis Nursing process objectives
Nursing process objectives Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Toolbox talk fatigue
Toolbox talk fatigue Drivers fatigue management test
Drivers fatigue management test Fatigue risk assessment matrix
Fatigue risk assessment matrix Nephrotic syndrome differential diagnosis
Nephrotic syndrome differential diagnosis Differential diagnosis of articular syndrome
Differential diagnosis of articular syndrome Carpal tunnel differential diagnosis
Carpal tunnel differential diagnosis Nursing diagnosis for nephrotic syndrome slideshare
Nursing diagnosis for nephrotic syndrome slideshare Rash-freudian-latex
Rash-freudian-latex Flinders model of care
Flinders model of care Kate lorig stanford
Kate lorig stanford Developed by ed
Developed by ed Stage 3 liver cirrhosis
Stage 3 liver cirrhosis Pancreatitis nursing diagnosis
Pancreatitis nursing diagnosis Chronic pain management irwin
Chronic pain management irwin Energy expenditure and fatigue
Energy expenditure and fatigue Age fatigue inattentiveness eyesight and footwear are
Age fatigue inattentiveness eyesight and footwear are Go placidly
Go placidly Crashworthiness course
Crashworthiness course Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Compassion fatigue signs
Compassion fatigue signs Compassion fatigue vs burnout
Compassion fatigue vs burnout Fatigue assessment tool
Fatigue assessment tool Beach marks
Beach marks What is the cause of fatigue for the alactacid system
What is the cause of fatigue for the alactacid system Ted talk compassion fatigue
Ted talk compassion fatigue Gerber equation fatigue
Gerber equation fatigue Steinberg fatigue
Steinberg fatigue Employee fatigue training
Employee fatigue training Alarm fatigue definition
Alarm fatigue definition Est-ce que tu es fatigué
Est-ce que tu es fatigué 30m sprint fatigue test
30m sprint fatigue test Fatigue analysis
Fatigue analysis System shock fatigue
System shock fatigue Fatigue toolbox talk
Fatigue toolbox talk Composite fatigue
Composite fatigue Fatigue test
Fatigue test Muscle fatigue
Muscle fatigue Slides fatigue test
Slides fatigue test Asthénie amaigrissement anorexie
Asthénie amaigrissement anorexie Fatigue
Fatigue Fatigue
Fatigue Icao doc 9966
Icao doc 9966 On-site manager fatigue workshop
On-site manager fatigue workshop Abs fatigue
Abs fatigue Vulnerability fatigue
Vulnerability fatigue Fatigue template
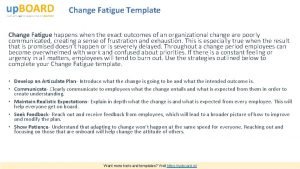
Fatigue template Ansys fatigue tool
Ansys fatigue tool Thermo-mechanical fatigue
Thermo-mechanical fatigue Adrenal fatigue symptoms
Adrenal fatigue symptoms Defination of fatigue
Defination of fatigue Compassion fatigue definition
Compassion fatigue definition Corrections fatigue
Corrections fatigue Fatigue crack
Fatigue crack Guthrie behaviorism
Guthrie behaviorism Warrantee definition
Warrantee definition Fatigue
Fatigue 10 cfr part 26
10 cfr part 26