Diagnosing chronic fatigue syndrome and orthostatic intolerance in


- Slides: 55
Diagnosing chronic fatigue syndrome and orthostatic intolerance in EDS Peter C. Rowe, MD Professor of Pediatrics Johns Hopkins University School of Medicine
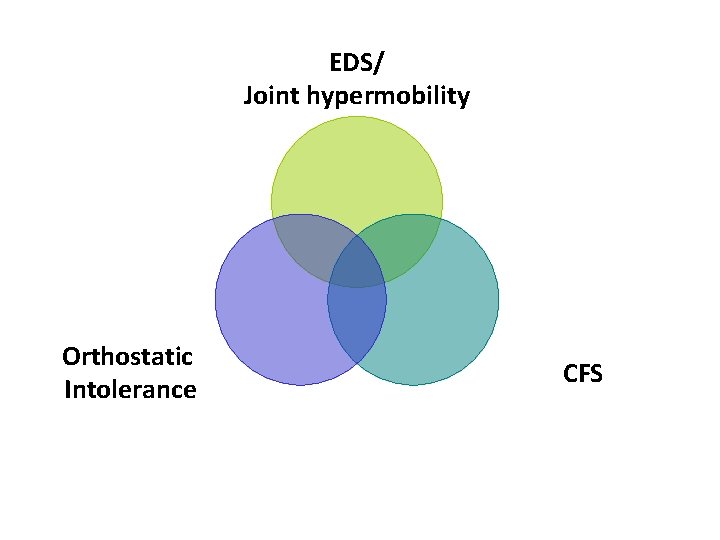
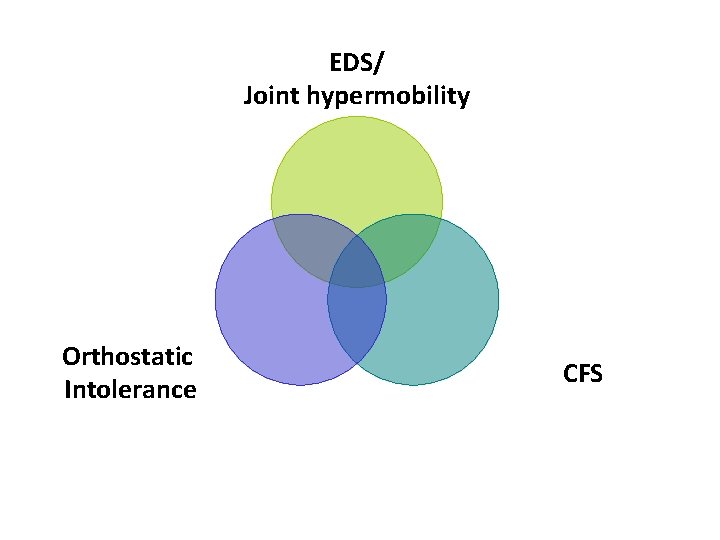
EDS/ Joint hypermobility Orthostatic Intolerance CFS
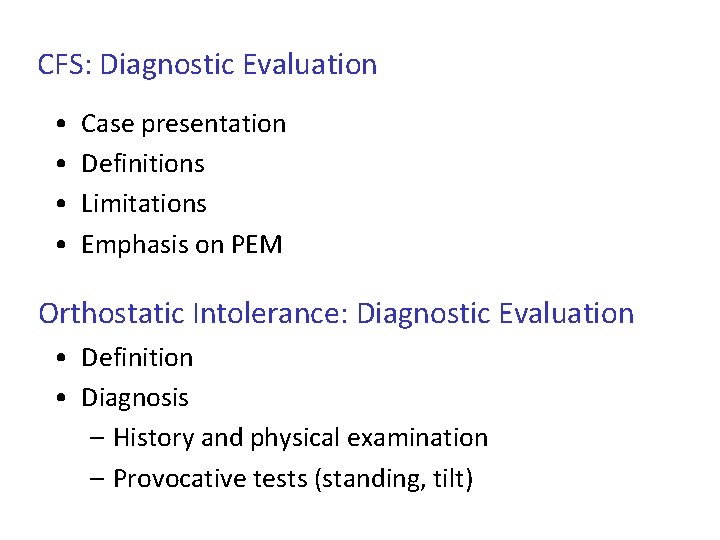
CFS: Diagnostic Evaluation • • Case presentation Definitions Limitations Emphasis on PEM Orthostatic Intolerance: Diagnostic Evaluation • Definition • Diagnosis – History and physical examination – Provocative tests (standing, tilt)
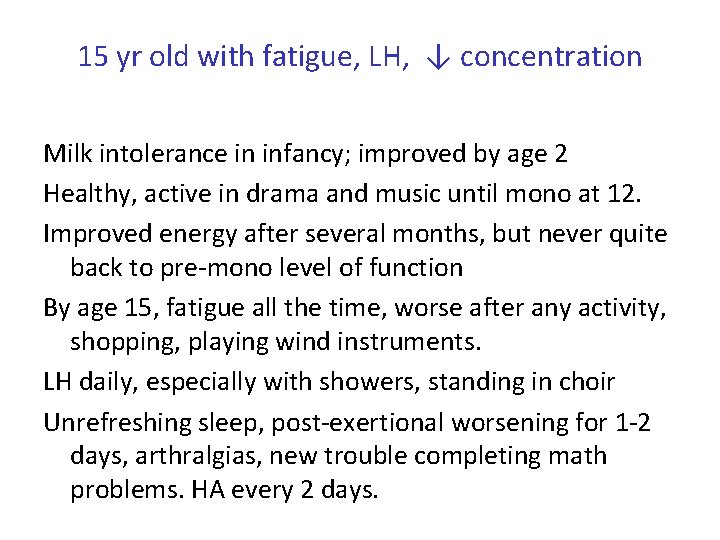
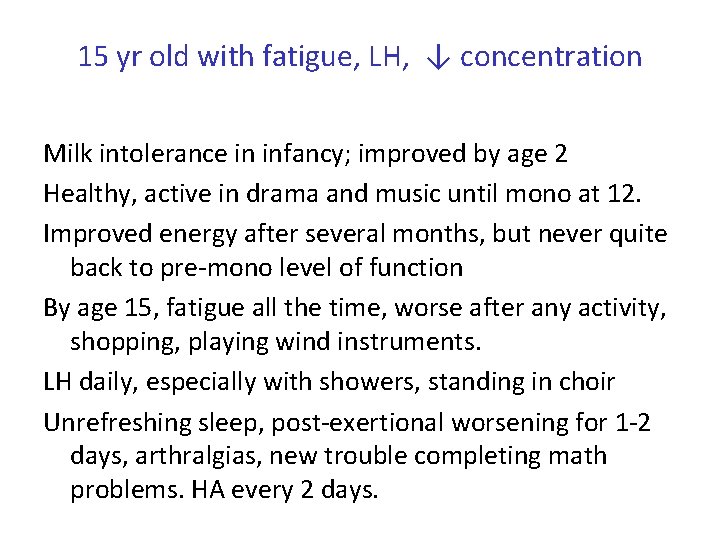
15 yr old with fatigue, LH, ↓ concentration Milk intolerance in infancy; improved by age 2 Healthy, active in drama and music until mono at 12. Improved energy after several months, but never quite back to pre-mono level of function By age 15, fatigue all the time, worse after any activity, shopping, playing wind instruments. LH daily, especially with showers, standing in choir Unrefreshing sleep, post-exertional worsening for 1 -2 days, arthralgias, new trouble completing math problems. HA every 2 days.
Does she meet criteria for CFS?
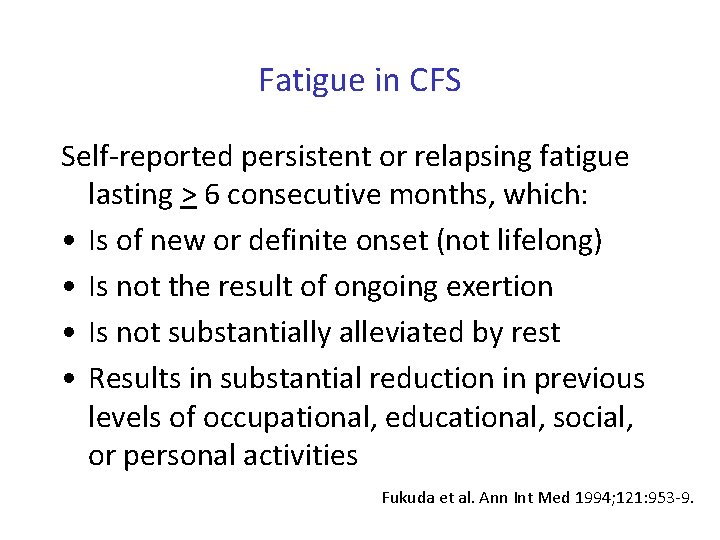
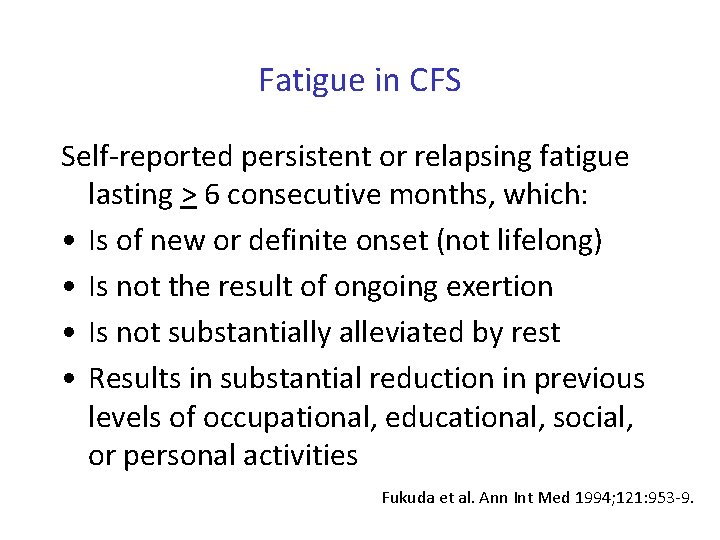
Fatigue in CFS Self-reported persistent or relapsing fatigue lasting > 6 consecutive months, which: • Is of new or definite onset (not lifelong) • Is not the result of ongoing exertion • Is not substantially alleviated by rest • Results in substantial reduction in previous levels of occupational, educational, social, or personal activities Fukuda et al. Ann Int Med 1994; 121: 953 -9.
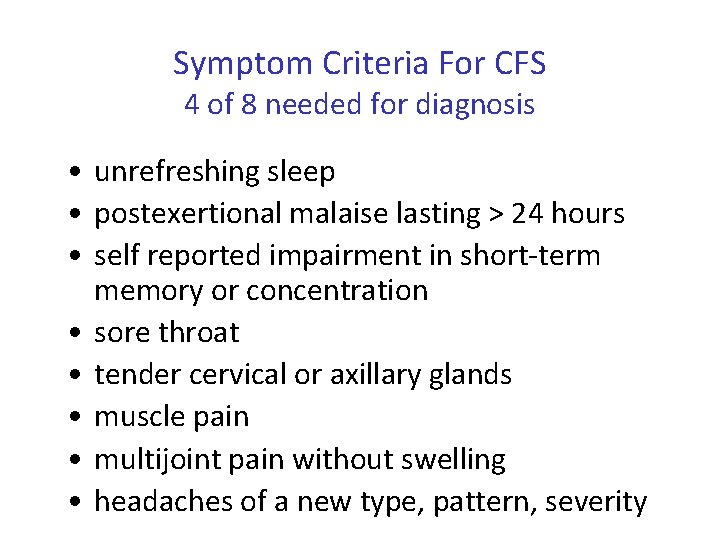
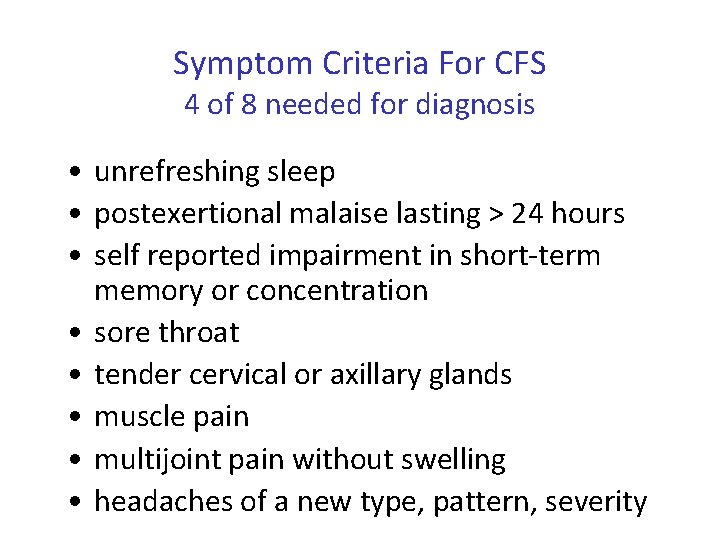
Symptom Criteria For CFS 4 of 8 needed for diagnosis • unrefreshing sleep • postexertional malaise lasting > 24 hours • self reported impairment in short-term memory or concentration • sore throat • tender cervical or axillary glands • muscle pain • multijoint pain without swelling • headaches of a new type, pattern, severity
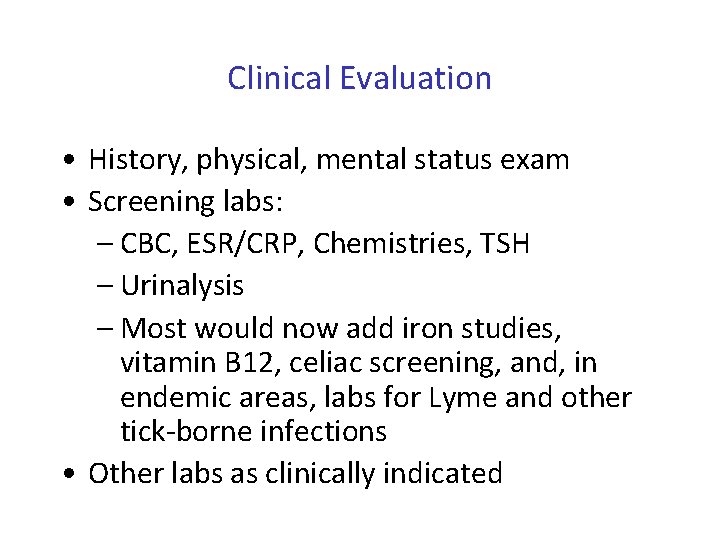
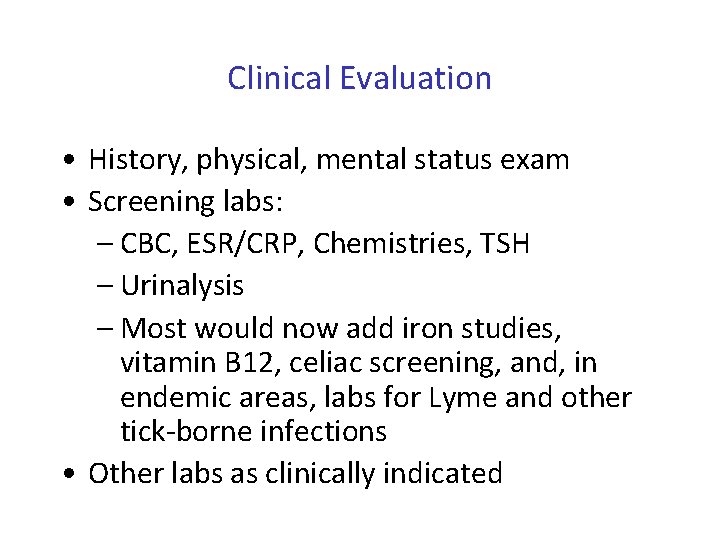
Clinical Evaluation • History, physical, mental status exam • Screening labs: – CBC, ESR/CRP, Chemistries, TSH – Urinalysis – Most would now add iron studies, vitamin B 12, celiac screening, and, in endemic areas, labs for Lyme and other tick-borne infections • Other labs as clinically indicated
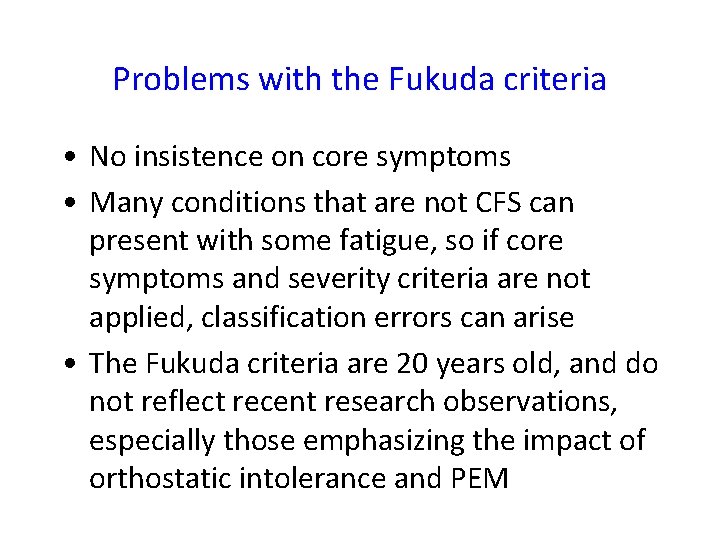
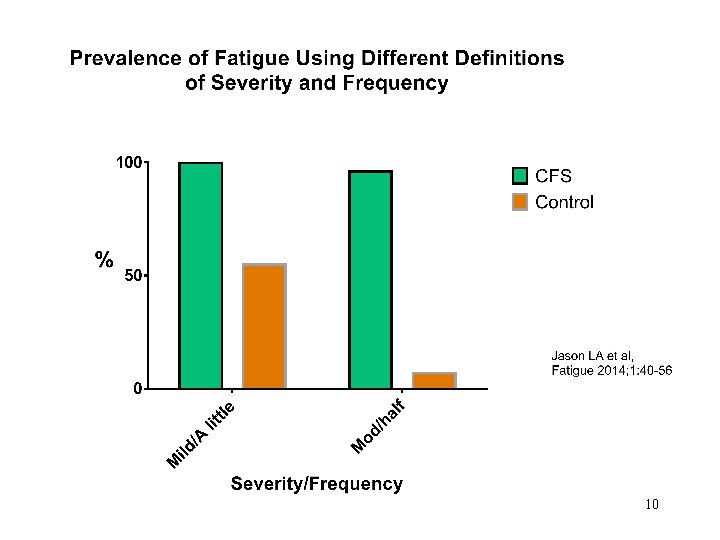
Problems with the Fukuda criteria • No insistence on core symptoms • Many conditions that are not CFS can present with some fatigue, so if core symptoms and severity criteria are not applied, classification errors can arise • The Fukuda criteria are 20 years old, and do not reflect recent research observations, especially those emphasizing the impact of orthostatic intolerance and PEM
10
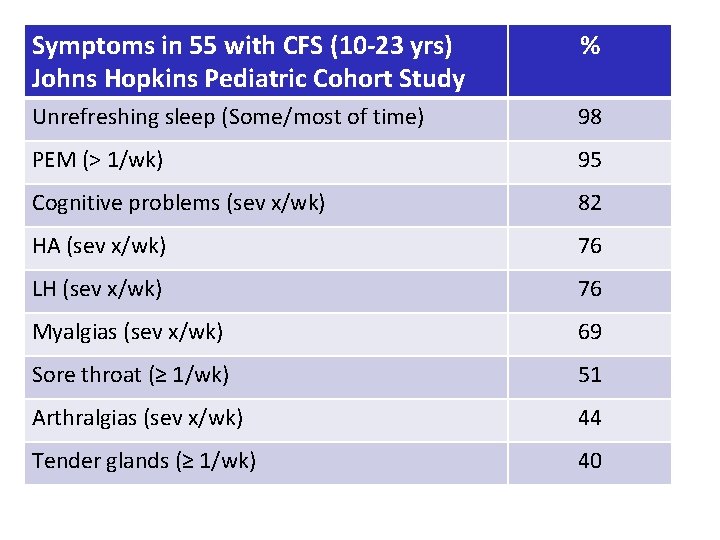
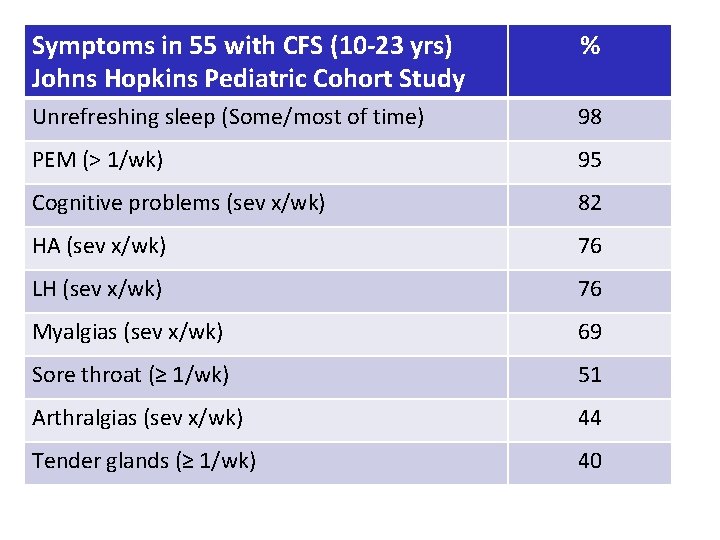
Symptoms in 55 with CFS (10 -23 yrs) Johns Hopkins Pediatric Cohort Study % Unrefreshing sleep (Some/most of time) 98 PEM (> 1/wk) 95 Cognitive problems (sev x/wk) 82 HA (sev x/wk) 76 LH (sev x/wk) 76 Myalgias (sev x/wk) 69 Sore throat (≥ 1/wk) 51 Arthralgias (sev x/wk) 44 Tender glands (≥ 1/wk) 40
Impact of CFS: helpful clinical questions • What happens when you try to do normal activities that you used to tolerate? (e. g. , reading, studying, walking 20 min, exercising) • What activities have you had to limit since you got sick? (school, after-school activities, shopping) • How often do you get out of the house? • How many chores can you manage in a day, or on consecutive days? If you do more, what are the consequences?
Chronic Fatigue syndrome: Diagnostic Evaluation • • Case presentation Definitions Limitations Emphasis on PEM
14
Study design • 25 females with CFS (Fukuda definition) • 23 sedentary controls • Maximal cardiopulmonary exercise test (duration 5 -15 minutes) • Daily written responses to questions about how they felt and duration of symptoms 15
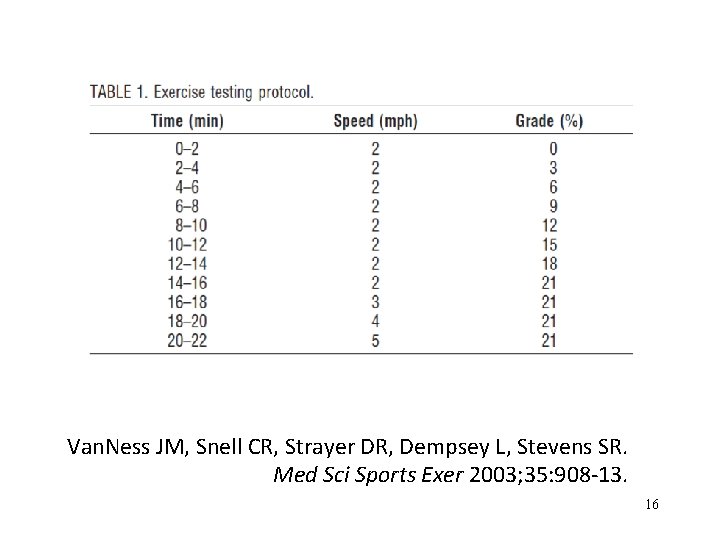
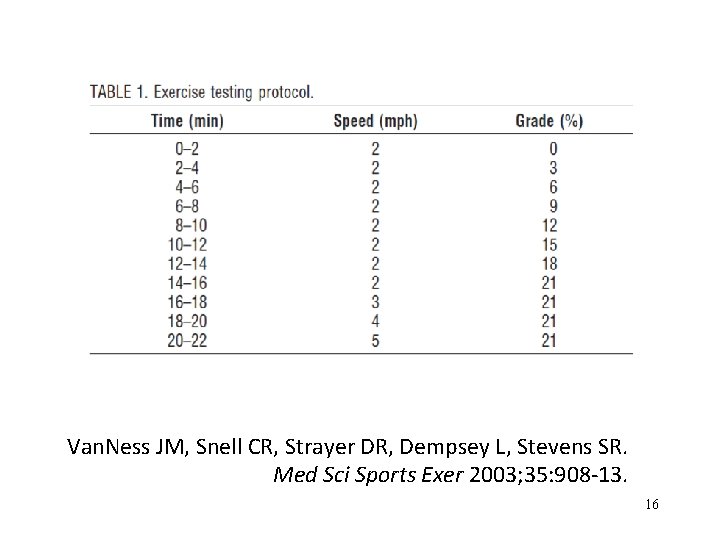
Van. Ness JM, Snell CR, Strayer DR, Dempsey L, Stevens SR. Med Sci Sports Exer 2003; 35: 908 -13. 16
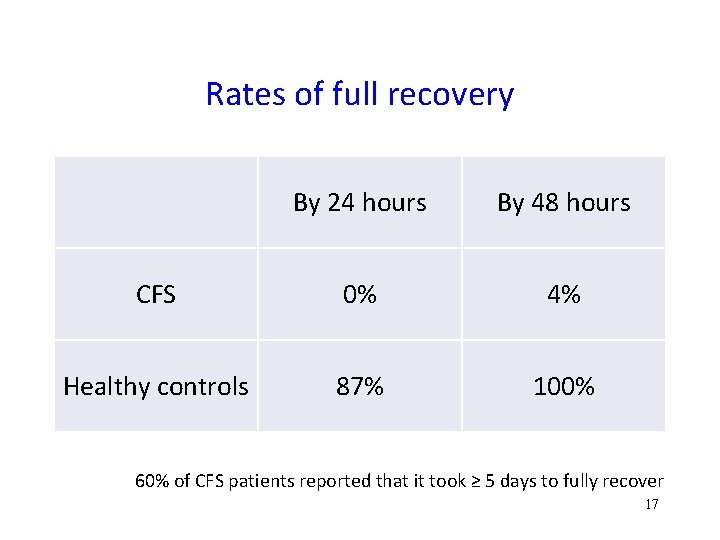
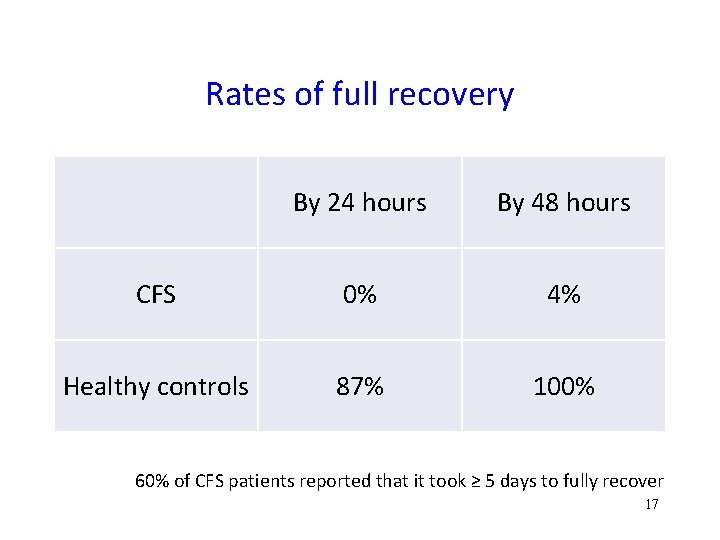
Rates of full recovery By 24 hours By 48 hours CFS 0% 4% Healthy controls 87% 100% 60% of CFS patients reported that it took ≥ 5 days to fully recover 17
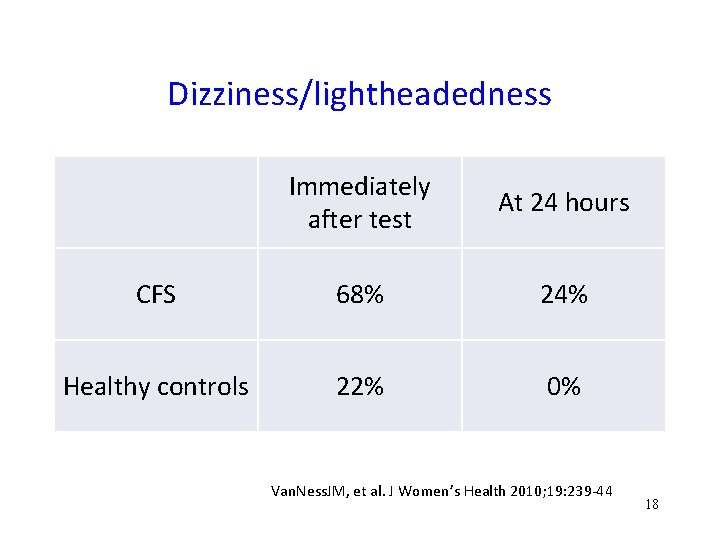
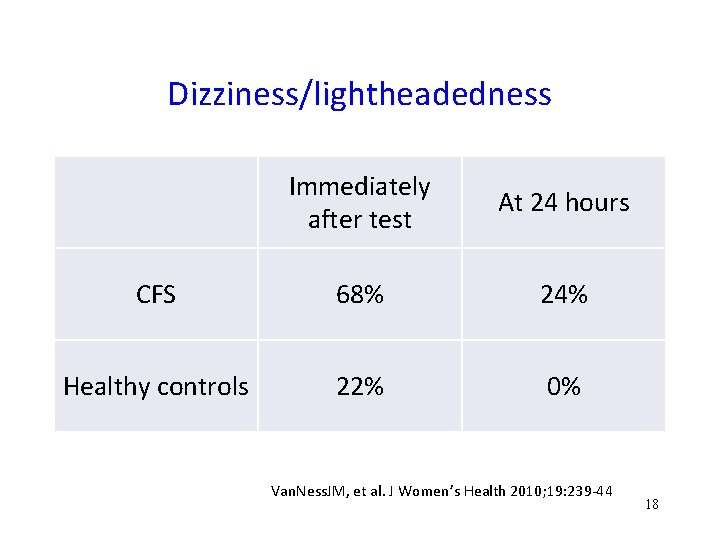
Dizziness/lightheadedness Immediately after test At 24 hours CFS 68% 24% Healthy controls 22% 0% Van. Ness. JM, et al. J Women’s Health 2010; 19: 239 -44 18
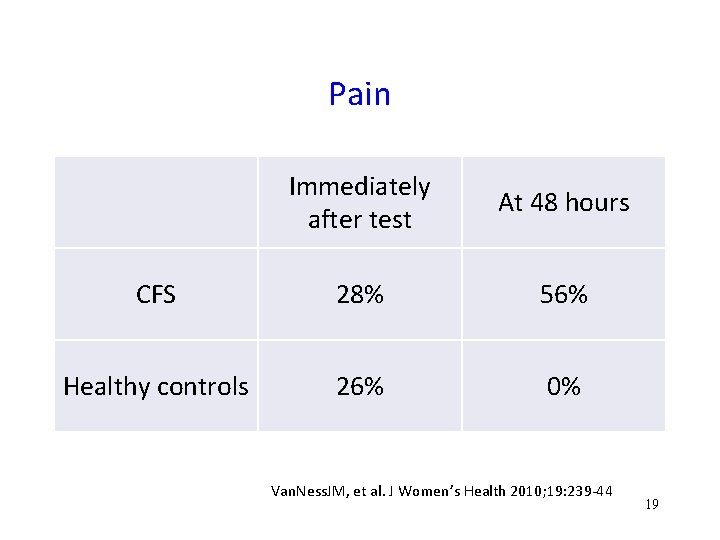
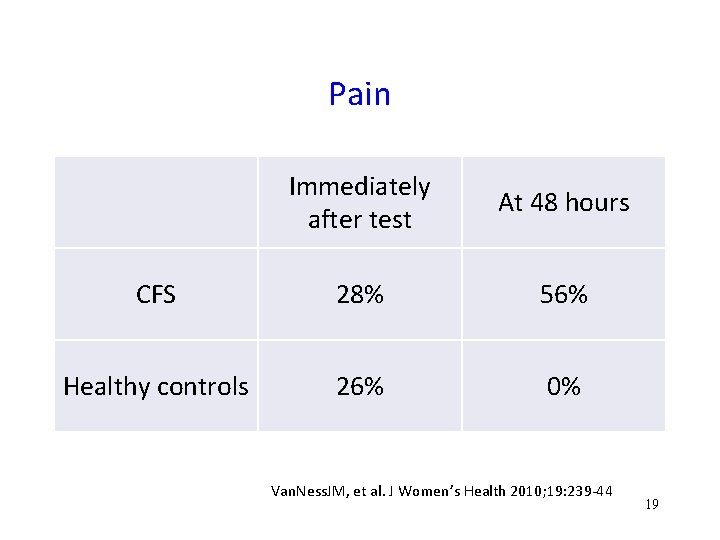
Pain Immediately after test At 48 hours CFS 28% 56% Healthy controls 26% 0% Van. Ness. JM, et al. J Women’s Health 2010; 19: 239 -44 19
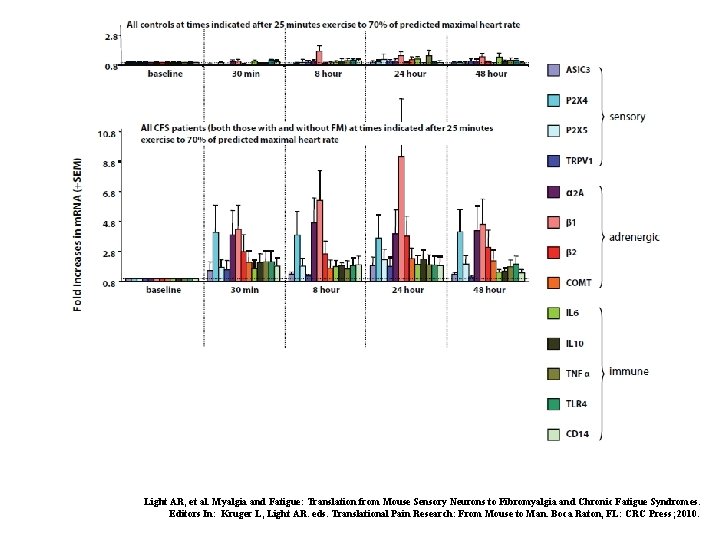
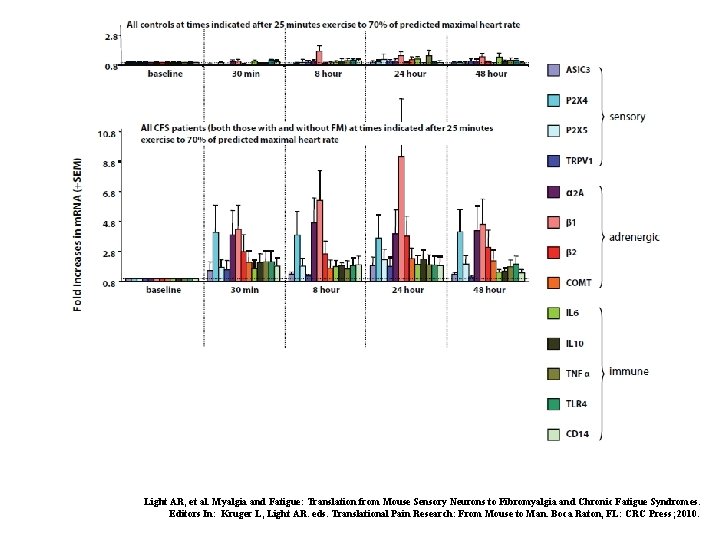
Light AR, et al. Myalgia and Fatigue: Translation from Mouse Sensory Neurons to Fibromyalgia and Chronic Fatigue Syndromes. Editors In: Kruger L, Light AR. eds. Translational Pain Research: From Mouse to Man. Boca Raton, FL: CRC Press; 2010.
Beyond Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome Redefining an Illness Committee on Diagnostic Criteria for ME/CFS February 10 th, 2015
Recommendations New diagnostic criteria—more focused on the core symptoms of ME/CFS than many other definitions—are warranted: 1. Impaired function 2. Post-exertional malaise 3. Unrefreshing sleep 4. Cognitive impairment or orthostatic intolerance
15 yr old with fatigue, LH, ↓ concentration Milk intolerance in infancy; improved by age 2 Healthy, active in drama and music until mono at 12. Improved energy after several months, but never quite back to pre-mono level of function By age 15, fatigue all the time, worse after any activity, shopping, playing wind instruments. LH daily, especially with showers, standing in choir Unrefreshing sleep, post-exertional worsening for 1 -2 days, arthralgias, new trouble completing math problems. HA every 2 days.
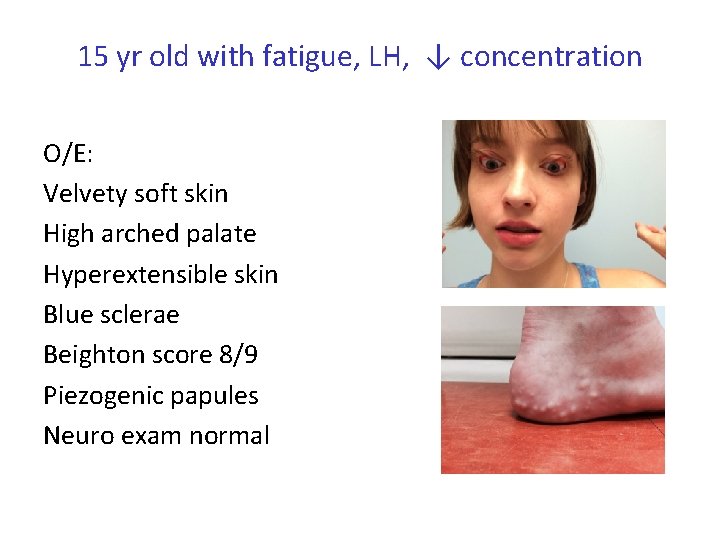
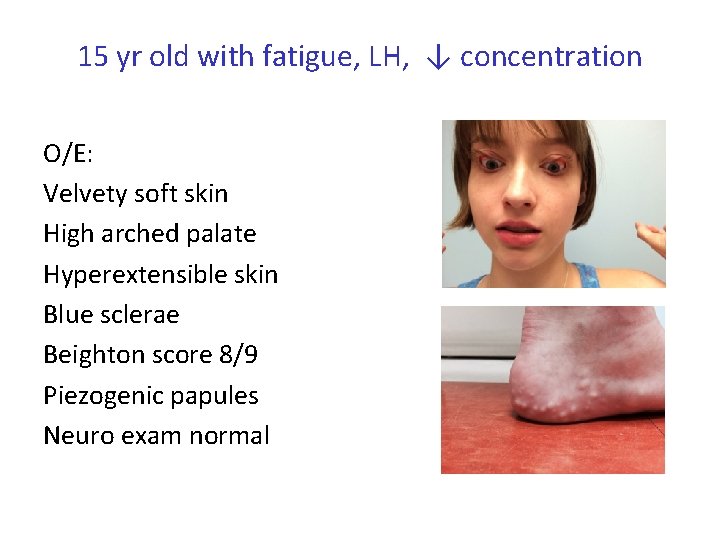
15 yr old with fatigue, LH, ↓ concentration O/E: Velvety soft skin High arched palate Hyperextensible skin Blue sclerae Beighton score 8/9 Piezogenic papules Neuro exam normal
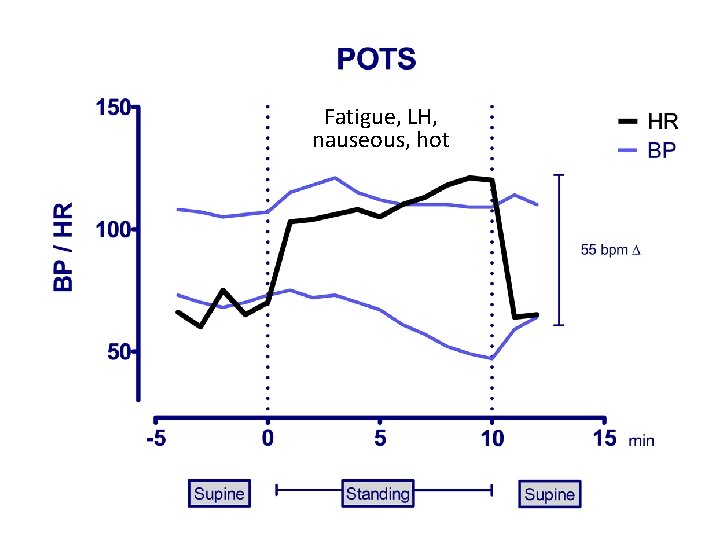
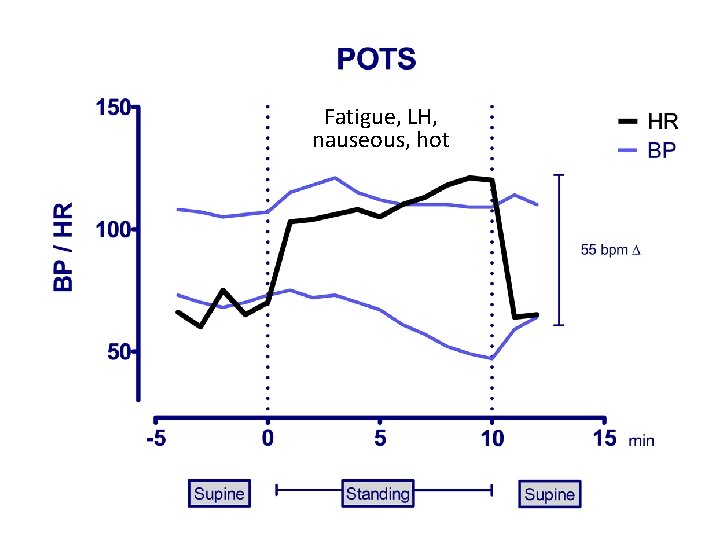
Fatigue, LH, nauseous, hot
Orthostatic Intolerance: Diagnostic Evaluation • Definition • Diagnosis – History – Physical examination – Provocative tests (standing, tilt) – Other testing in Appendix
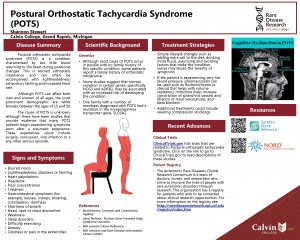
Orthostatic Intolerance The term “orthostatic intolerance” refers to a group of clinical conditions in which symptoms worsen with quiet upright posture and are ameliorated (although not necessarily abolished) by recumbency. Modified from: Low PA, Sandroni P, Joyner M, Shen WK. Postural tachycardia syndrome (POTS). J Cardiovasc Electrophysiol 2009; 20: 352 -8.
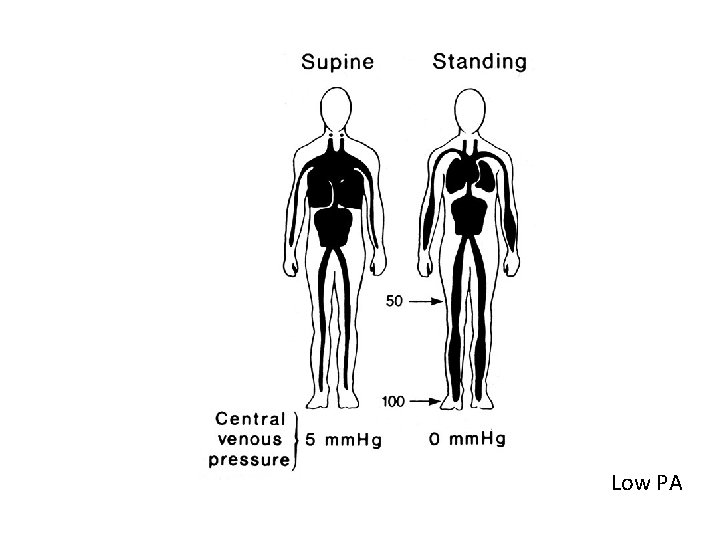
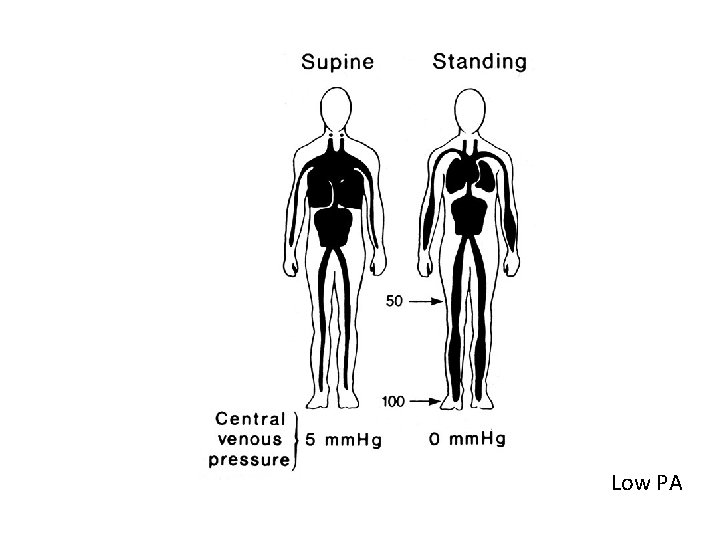
Low PA
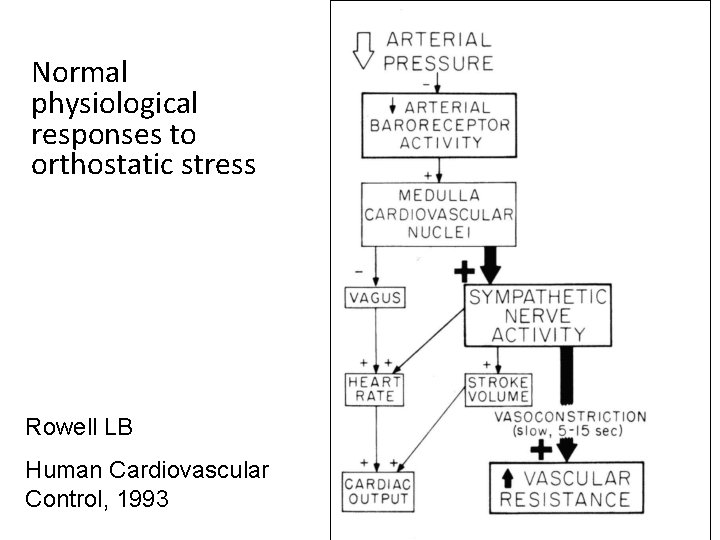
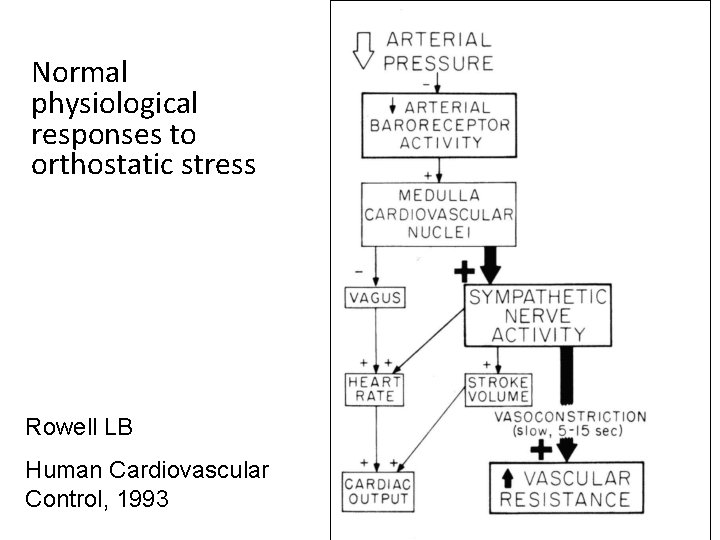
Normal physiological responses to orthostatic stress Rowell LB Human Cardiovascular Control, 1993
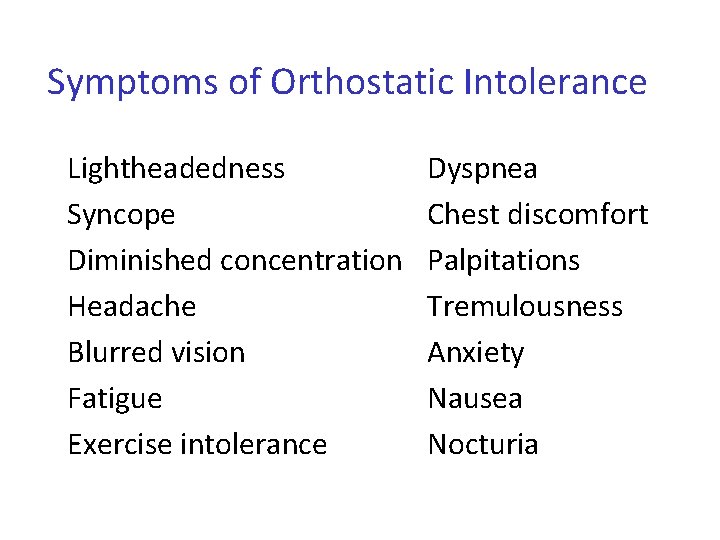
Symptoms of Orthostatic Intolerance Lightheadedness Syncope Diminished concentration Headache Blurred vision Fatigue Exercise intolerance Dyspnea Chest discomfort Palpitations Tremulousness Anxiety Nausea Nocturia
Common forms of OI in EDS (in relative order of frequency) • • Orthostatic intolerance POTS NMH OH
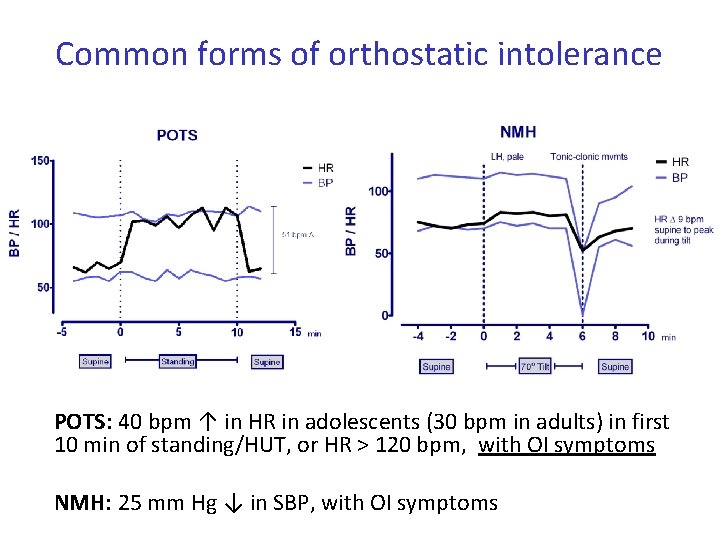
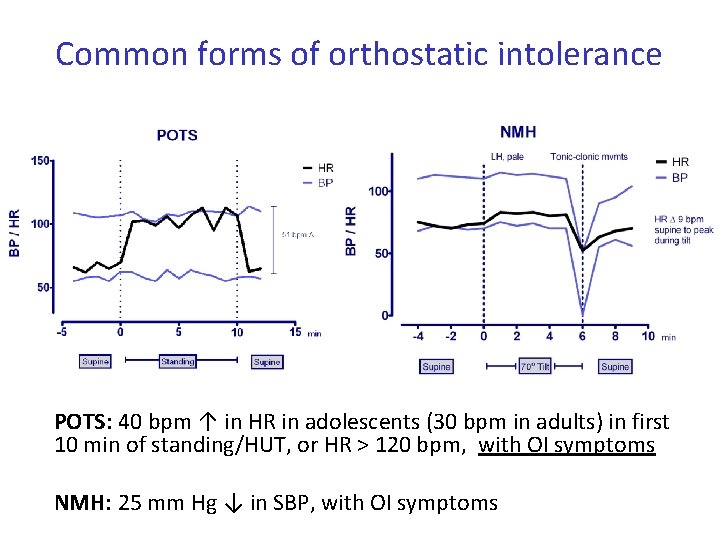
Common forms of orthostatic intolerance POTS: 40 bpm ↑ in HR in adolescents (30 bpm in adults) in first 10 min of standing/HUT, or HR > 120 bpm, with OI symptoms NMH: 25 mm Hg ↓ in SBP, with OI symptoms
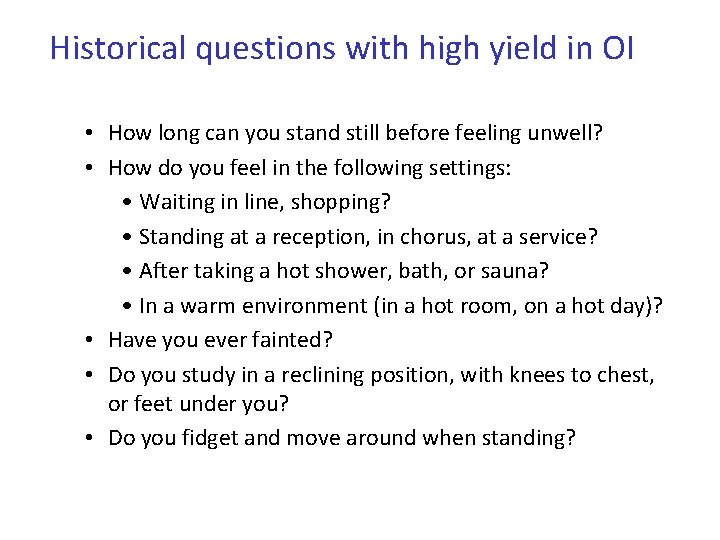
Historical questions with high yield in OI • How long can you stand still before feeling unwell? • How do you feel in the following settings: • Waiting in line, shopping? • Standing at a reception, in chorus, at a service? • After taking a hot shower, bath, or sauna? • In a warm environment (in a hot room, on a hot day)? • Have you ever fainted? • Do you study in a reclining position, with knees to chest, or feet under you? • Do you fidget and move around when standing?
Orthostatic Intolerance: Diagnostic Evaluation • Definition • Diagnosis – History – Physical examination – Provocative tests (standing, tilt) – Other testing in Appendix
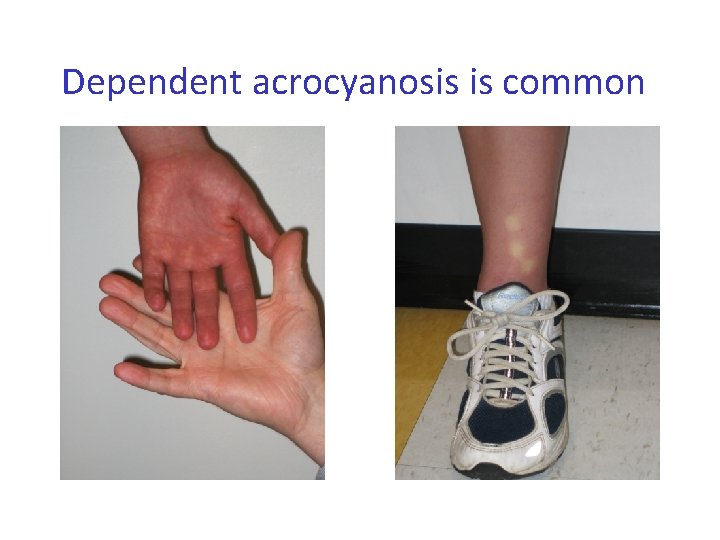
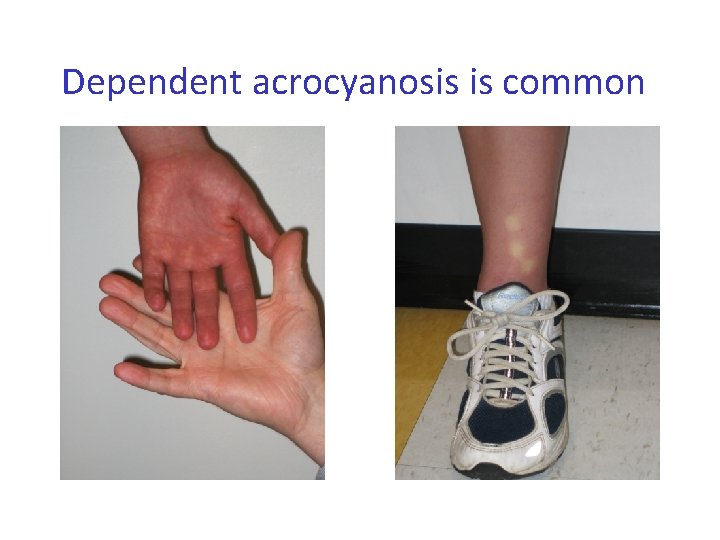
Dependent acrocyanosis is common
Orthostatic Intolerance: Diagnostic Evaluation • Definition of Orthostatic Intolerance • Diagnosis – History – Physical examination – Provocative tests (standing, tilt)
Provocative testing • Orthostatic vital signs—HR and BP measured supine, sitting, and standing— often measured over < 2 minutes: insufficient to identify most forms of chronic orthostatic intolerance. • 10 min. upright needed to document POTS • NMH usually will be missed unless testing is prolonged (10 -45 minutes)
Passive Stand Test Supine: 5 min with BP and HR every minute Standing: 10 -15 min with feet positioned 6 inches apart, 6 inches from a wall, leaning slightly backwards against the wall. HR & BP measured each minute Symptoms recorded every 1 -2 minutes Hyatt KH, Jacobson LB, Schneider VS. Comparison of 70° tilt, LBNP, and passive standing as measures of orthostatic tolerance. Aviat Space Environ Med 1975; 46: 801 -8.
Active Stand Test V 1: Supine: 30 min with BP and HR every minute Standing: up to 60 min while standing at the bedside, arm with BP cuff resting on a support table at the 2 nd intercostal space. Streeten DHP, et al. The roles of orthostatic hypotension, orthostatic tachycardia, and subnormal erythrocyte volume in the pathogenesis of the CFS. Am J Med Sci 2000; 320: 1 -8. V 2: Supine: at least 1 h, many for the entire night. Standing: Patients discouraged from walking around or running in place, but permitted to move their legs. Plash WB, et al. Diagnosing POTS: comparison of tilt testing compared with standing haemodynamics. Clinical Science 2013; 124: 109– 114
Head-up Tilt Testing Stage 1: head-up tilt to 70° for 45 min Stage 2 (optional): Return to supine for 10 minutes, then head-up tilt for 15 minutes with isoproterenol (1 -2 mcg/kg/min). Some use nitroglycerine after 20 min upright.
Is tilt testing necessary for individuals with recurrent syncope? In patients with … no evidence of ischemia and a structurally normal heart, the pretest probability that the diagnosis is neurocardiogenic syncope is high, so headup tilt table testing contributes little to establishing the diagnosis. AHA/ACCF Scientific Statement on the evaluation of syncope. JACC 2006; 47: 473 -84


Back to our patient …
Course 6 month F/U: With trials of increased salt and fluid, Florinef, midodrine, able to get to school more regularly.
Course 8 month F/U: Consecutive viral URIs are followed by markedly increased fatigue, disrupted sleep, and more frontal and retro-orbital HA. Unable to attend school. On return to clinic, exam notably different. Now has rotatory nystagmus, diminished gag reflex, brisk reflexes with 2 -3 beats of clonus at ankles. (Normal DTRs 8 months earlier)
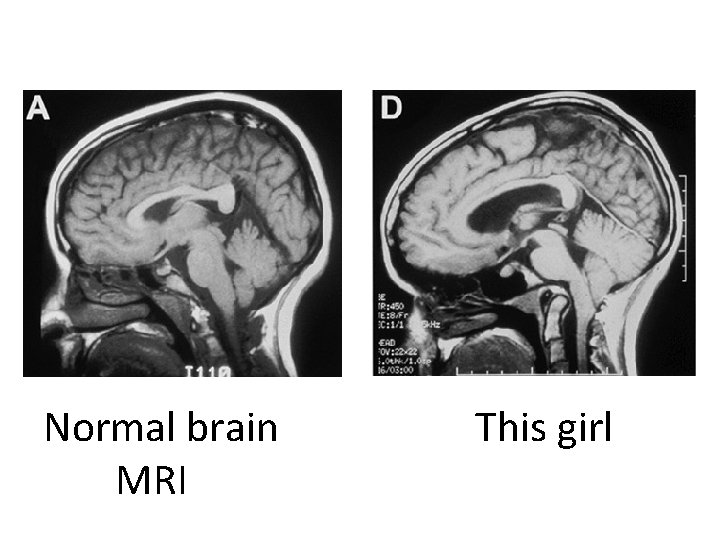
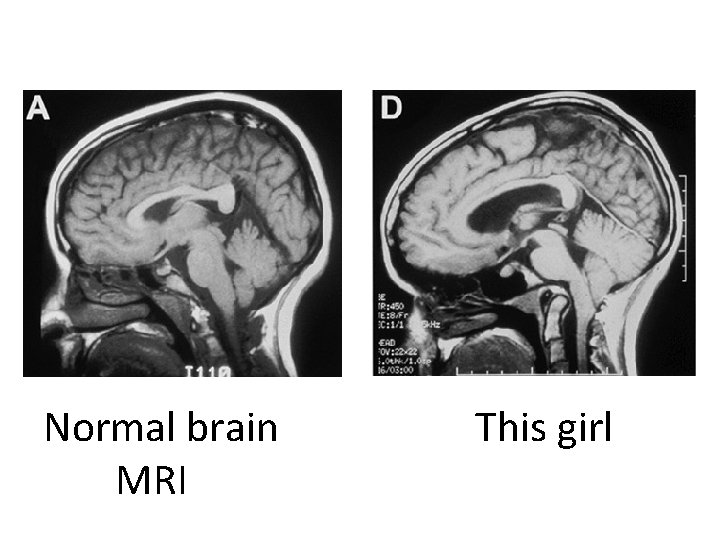
Normal brain MRI This girl
Beyond POTS ( … and OI, and CFS) “we should view the POTS diagnosis as a starting place for the discovery of the cause of the patient’s problem rather than a final answer as to what the patient actually has … as a final common pathway by which a myriad of genetic and acquired pathophysiologies may present to the physician. ” Mustafa HI, Robertson DR. J Neurol Neurosurg Psychiatry 2010; 81: 237 -8.
48
ACKNOWLEDGEMENTS • • Grants from NIAID, Do. D, CFIDS Association of America Sunshine Natural Wellbeing Foundation (endowed Chair) Volunteer RA Colleen Marden Summer students (John Fan, Alli Johns, Marissa Flaherty, Jocelyn Ray, Samantha Jasion, Erica Cranston) • Many families and patients: – Special thanks to the following: Boies, Cornell, Smith, Caldwell, Ellen, Kelly, Kiely, Mc. Ferron, Minutoli, Newbrand, Megan Lauver, Hannah Vogel 49
Appendix
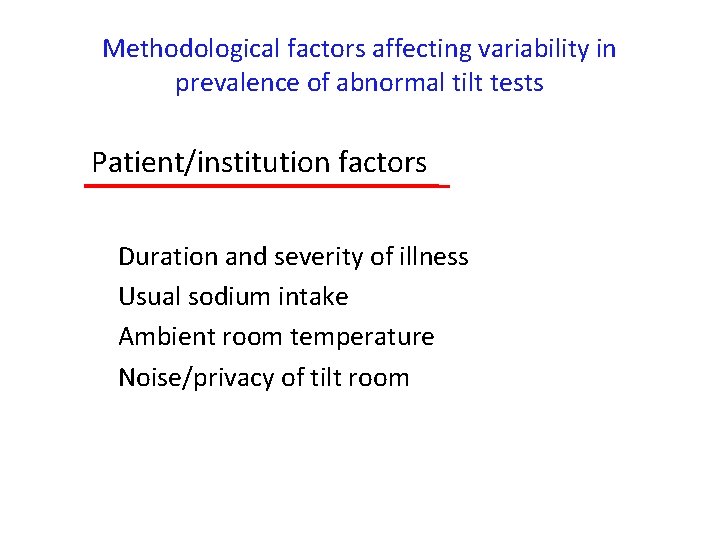
Methodological factors affecting variability in prevalence of abnormal tilt tests Patient/institution factors Duration and severity of illness Usual sodium intake Ambient room temperature Noise/privacy of tilt room
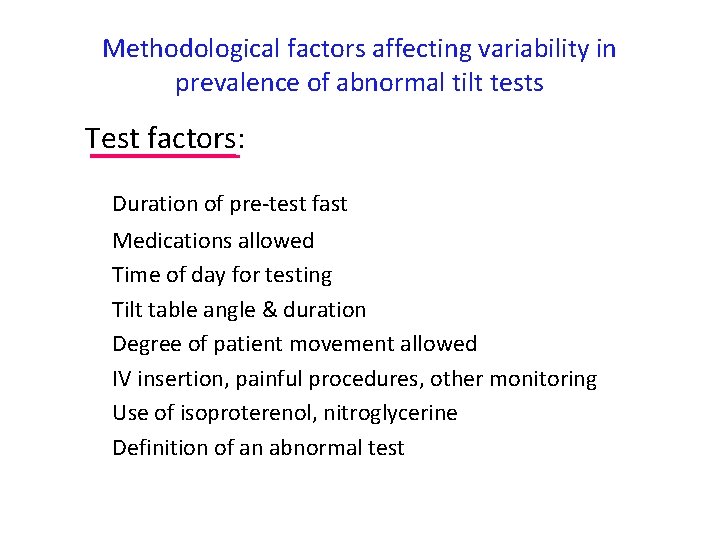
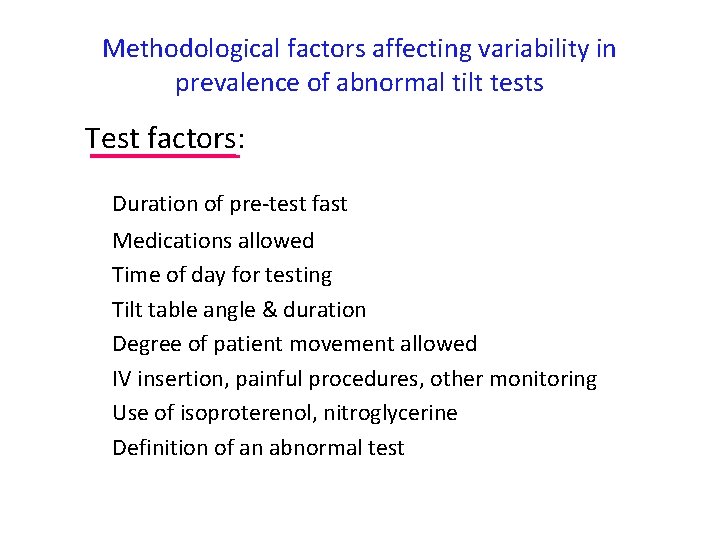
Methodological factors affecting variability in prevalence of abnormal tilt tests Test factors: Duration of pre-test fast Medications allowed Time of day for testing Tilt table angle & duration Degree of patient movement allowed IV insertion, painful procedures, other monitoring Use of isoproterenol, nitroglycerine Definition of an abnormal test
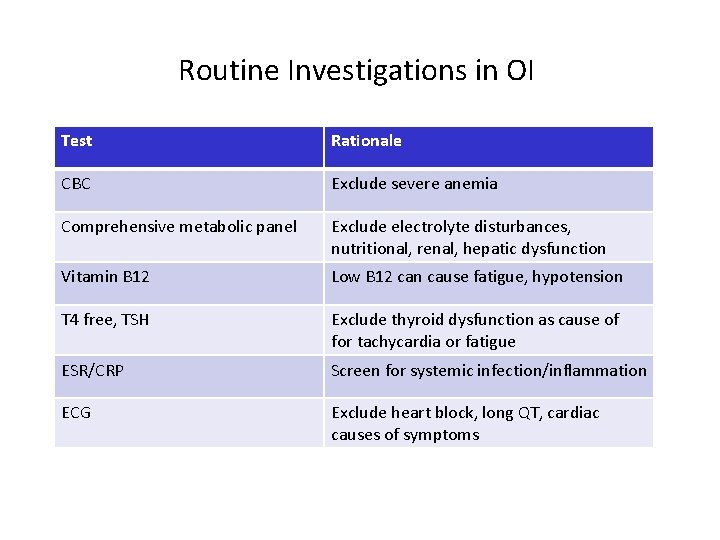
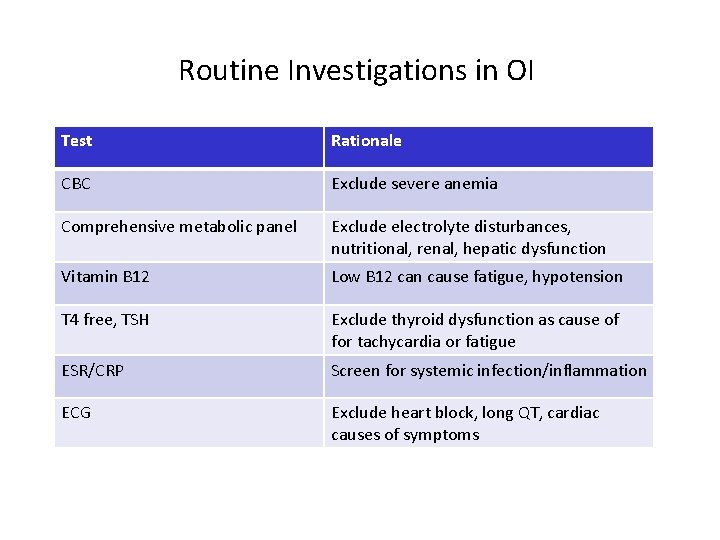
Routine Investigations in OI Test Rationale CBC Exclude severe anemia Comprehensive metabolic panel Exclude electrolyte disturbances, nutritional, renal, hepatic dysfunction Vitamin B 12 Low B 12 can cause fatigue, hypotension T 4 free, TSH Exclude thyroid dysfunction as cause of for tachycardia or fatigue ESR/CRP Screen for systemic infection/inflammation ECG Exclude heart block, long QT, cardiac causes of symptoms
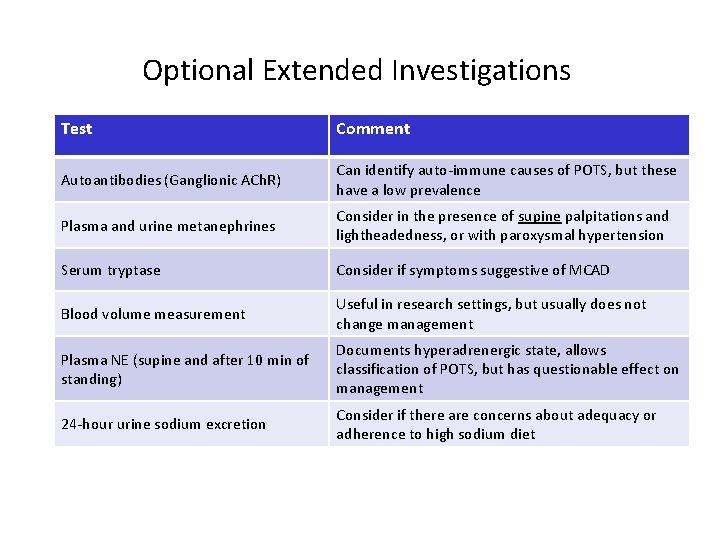
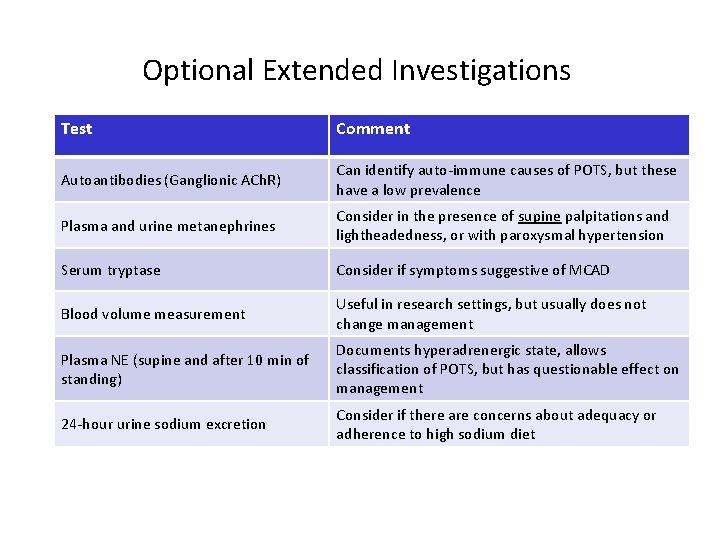
Optional Extended Investigations Test Comment Autoantibodies (Ganglionic ACh. R) Can identify auto-immune causes of POTS, but these have a low prevalence Plasma and urine metanephrines Consider in the presence of supine palpitations and lightheadedness, or with paroxysmal hypertension Serum tryptase Consider if symptoms suggestive of MCAD Blood volume measurement Useful in research settings, but usually does not change management Plasma NE (supine and after 10 min of standing) Documents hyperadrenergic state, allows classification of POTS, but has questionable effect on management 24 -hour urine sodium excretion Consider if there are concerns about adequacy or adherence to high sodium diet
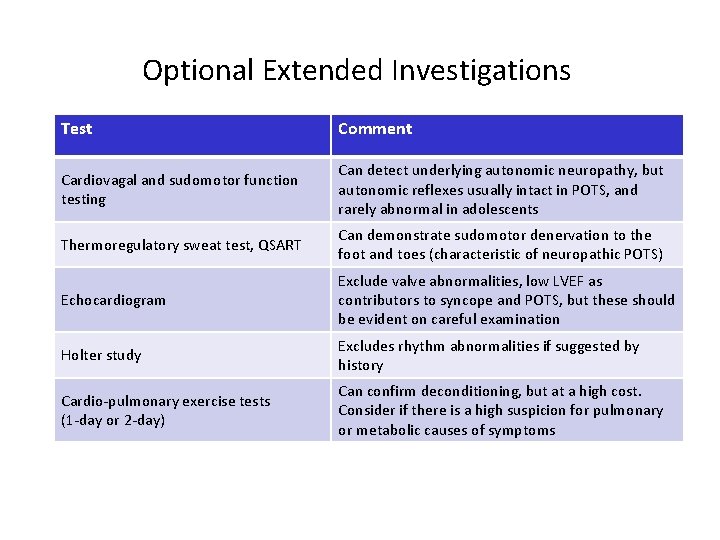
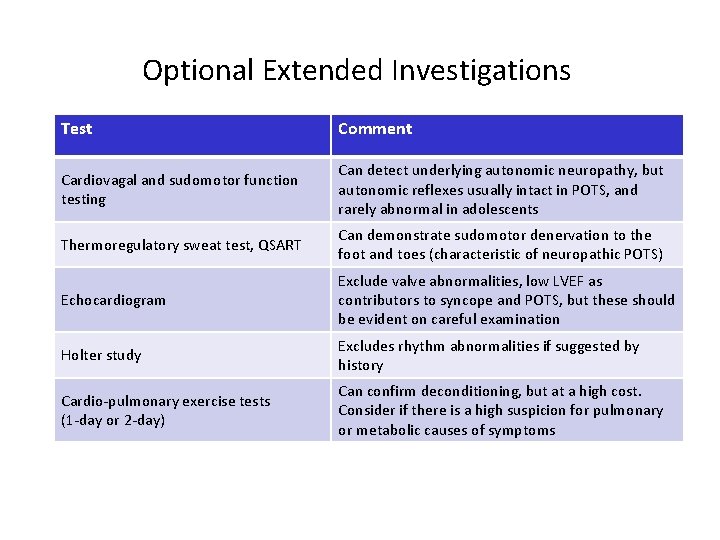
Optional Extended Investigations Test Comment Cardiovagal and sudomotor function testing Can detect underlying autonomic neuropathy, but autonomic reflexes usually intact in POTS, and rarely abnormal in adolescents Thermoregulatory sweat test, QSART Can demonstrate sudomotor denervation to the foot and toes (characteristic of neuropathic POTS) Echocardiogram Exclude valve abnormalities, low LVEF as contributors to syncope and POTS, but these should be evident on careful examination Holter study Excludes rhythm abnormalities if suggested by history Cardio-pulmonary exercise tests (1 -day or 2 -day) Can confirm deconditioning, but at a high cost. Consider if there is a high suspicion for pulmonary or metabolic causes of symptoms
 Fibromyalgia vs chronic fatigue
Fibromyalgia vs chronic fatigue Group level diagnostic model
Group level diagnostic model Classification of antianginal drugs
Classification of antianginal drugs A defective vacuum brake booster will cause a ________.
A defective vacuum brake booster will cause a ________. Diagnosing hypertension
Diagnosing hypertension Hypertensive emergency
Hypertensive emergency Yodsawalai chodpathumwan
Yodsawalai chodpathumwan Caplan syndrome
Caplan syndrome Cultural intelligence profiles
Cultural intelligence profiles Enzymes and lactose intolerance lab answers
Enzymes and lactose intolerance lab answers Positive orthostatic vital signs
Positive orthostatic vital signs Positive orthostatics
Positive orthostatics Orthostatic vital signs
Orthostatic vital signs Orthostatics definition
Orthostatics definition Vital sign normal
Vital sign normal Orthostatic vital sign
Orthostatic vital sign Orthostatic hypotension
Orthostatic hypotension Orthostatic hypotensin
Orthostatic hypotensin Intolerance theme in the crucible
Intolerance theme in the crucible Stibio intolérance
Stibio intolérance Lactose
Lactose Lactose intolerance countries
Lactose intolerance countries John proctor the crucible quotes
John proctor the crucible quotes Maltose intolerance
Maltose intolerance Lactose
Lactose Metobolic encephalopathy
Metobolic encephalopathy Lactose intolerance histology
Lactose intolerance histology Reproductive isolation
Reproductive isolation Digestion and absorption of carbohydrates biochemistry
Digestion and absorption of carbohydrates biochemistry Energy expenditure and fatigue
Energy expenditure and fatigue Age fatigue inattentiveness eyesight and footwear are
Age fatigue inattentiveness eyesight and footwear are Many fears are born of fatigue and loneliness
Many fears are born of fatigue and loneliness Fatigue and damage tolerance course
Fatigue and damage tolerance course Compassion fatigue signs
Compassion fatigue signs Fatigue management toolbox talk
Fatigue management toolbox talk Ofcfbrazil
Ofcfbrazil Fatigue assessment tool
Fatigue assessment tool Beach marks fatigue
Beach marks fatigue What is predominant energy system
What is predominant energy system Ted talk compassion fatigue
Ted talk compassion fatigue Gerber equation fatigue
Gerber equation fatigue Steinberg fatigue
Steinberg fatigue Employee fatigue training
Employee fatigue training Monitor alarm fatigue an integrative review
Monitor alarm fatigue an integrative review Tu es fatigué
Tu es fatigué 30m sprint fatigue test
30m sprint fatigue test Fatigue stress
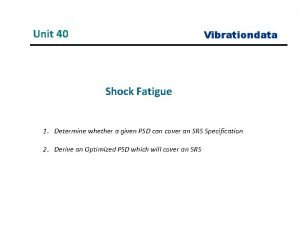
Fatigue stress System shock fatigue
System shock fatigue Fatigue toolbox talk
Fatigue toolbox talk Drivers fatigue management test
Drivers fatigue management test Composite fatigue
Composite fatigue Fatigue test
Fatigue test Muscle fatigue
Muscle fatigue Slides fatigue test
Slides fatigue test Asthénie amaigrissement anorexie
Asthénie amaigrissement anorexie Fatigue
Fatigue