Dental trauma in children Introduction Peak incidences are
- Slides: 37
Dental trauma in children
Introduction • Peak incidences are found at 2 -3 years of age, motor coordination is developing.
Pathogenesis • Surrounding bone is less dense and less mineralised. • A tooth can easily displaced instead of fractured. • Frontal trauma is quite frequent —> lateral luxation
Etiology • Falls • Accidents • Child abuse • Self-inflicted ora-dental
Goals Prevent the occurrence of sequelae in the permanent dentition. The ways which may damage permanent dentition 1. Direct displacement toward the permanent tooth bud 2. Infection caused by bacteria invasion to the injury site 3. Extraction, Repositioning, or Pulp treatment
History taking • Loss of consciousness ? • Tetanus innoculation • How injury occurred ? … • normal or abnormal • Who reported?
Clinical examination • Extra-oral • Intra-oral • Tooth mobility and alignment
Extra-oral examination • facial asymmetry • swelling of the lips • skin laceration • scars (previous injuries) • bleeding from nostrils • mouth opening
Intra-oral examination • Surrounding soft tissue • lips, oral mucosa, gingiva, and frenum • Submucosal haemorrhage • upper lip / under tongue • Bleeding from sulcus
Radiographic examination AAPD guideline recommends size 2 film for 1. 90° horizontal view 2. Occlusal view 3. Extra-oral lateral view
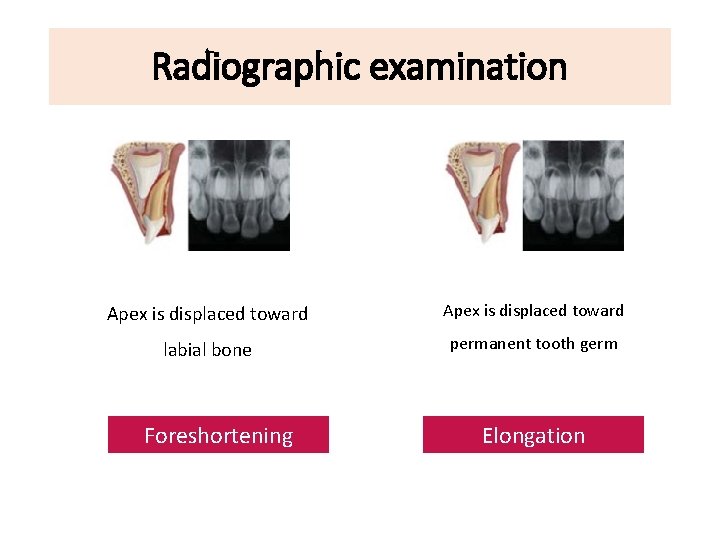
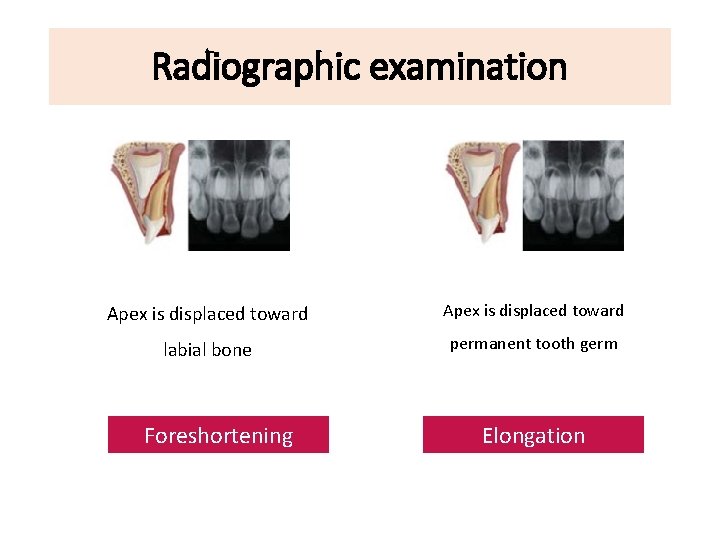
Radiographic examination Apex is displaced toward labial bone permanent tooth germ Foreshortening Elongation
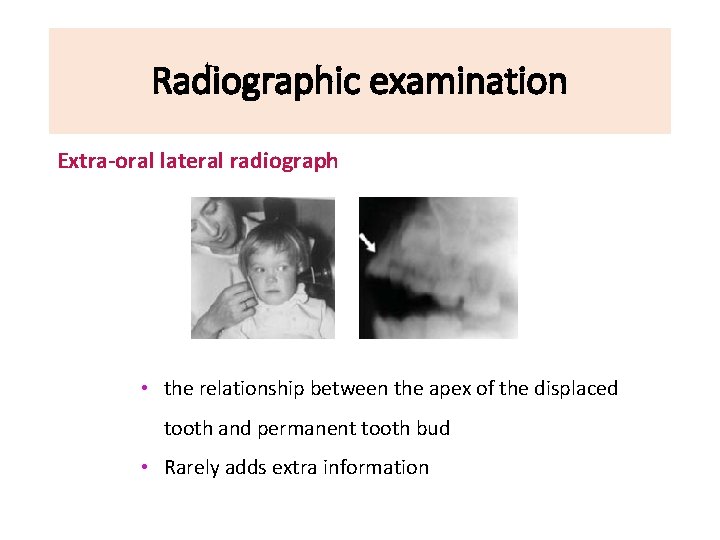
Radiographic examination Extra-oral lateral radiograph • the relationship between the apex of the displaced tooth and permanent tooth bud • Rarely adds extra information
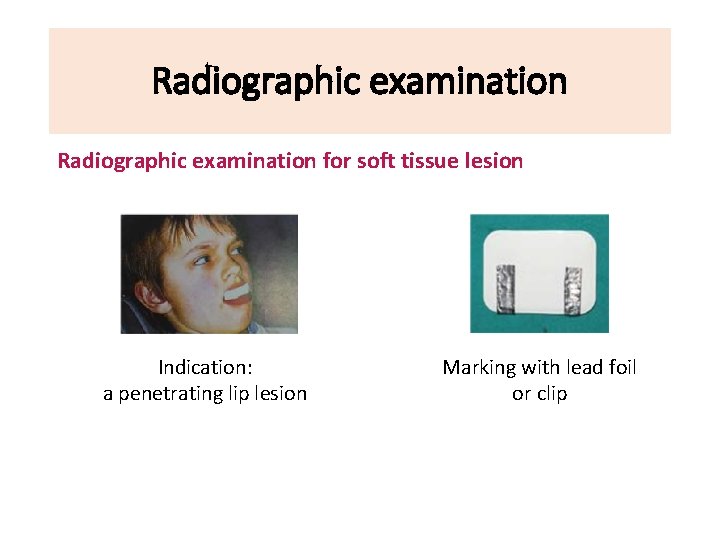
Radiographic examination for soft tissue lesion Indication: a penetrating lip lesion Marking with lead foil or clip
Treatment principle • To minimise the risk to the permanent teeth • Implies a conservative approach • Child: Behaviour management • Parents: Empathy and support their minds
Treatment principle • Traumatic injuries to primary teeth - Lack of scientific data • Factors related to treatment selection 1. Shedding time 2. A child’ maturity and compliance 3. The close proximity of the root of primary tooth to permanent tooth bud
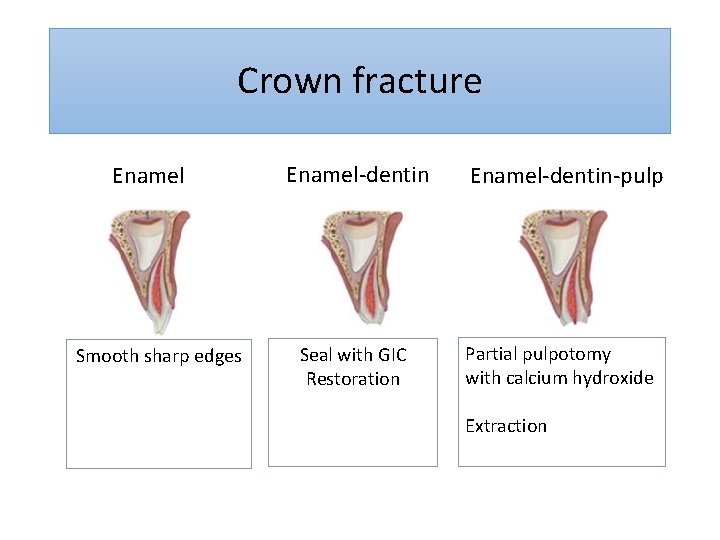
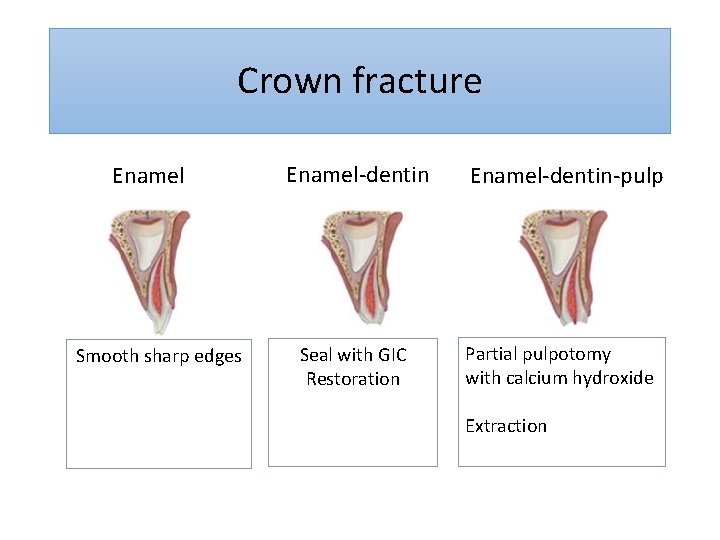
Crown fracture Enamel Smooth sharp edges Enamel-dentin Seal with GIC Restoration Enamel-dentin-pulp Partial pulpotomy with calcium hydroxide Extraction
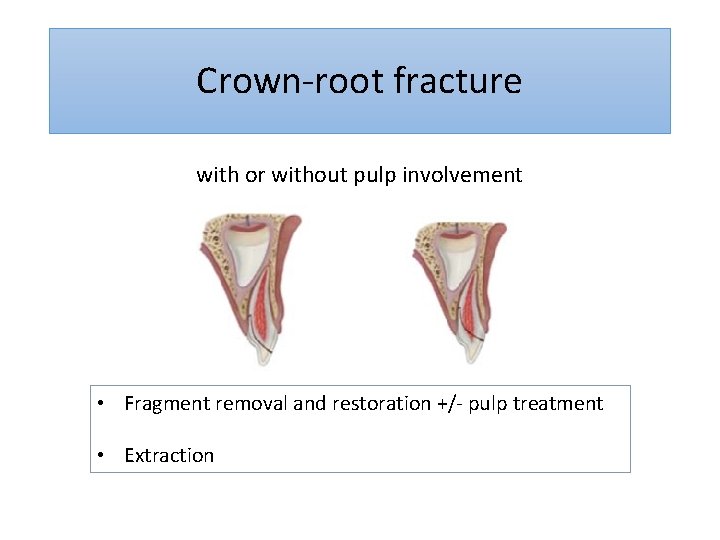
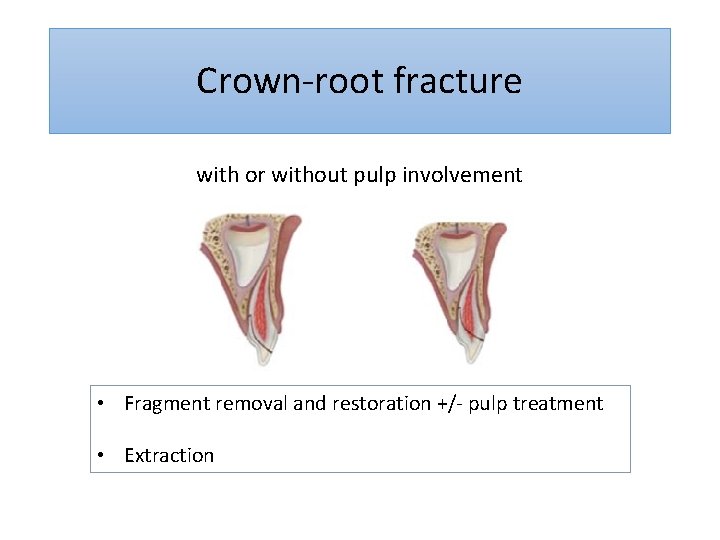
Crown-root fracture with or without pulp involvement • Fragment removal and restoration +/- pulp treatment • Extraction
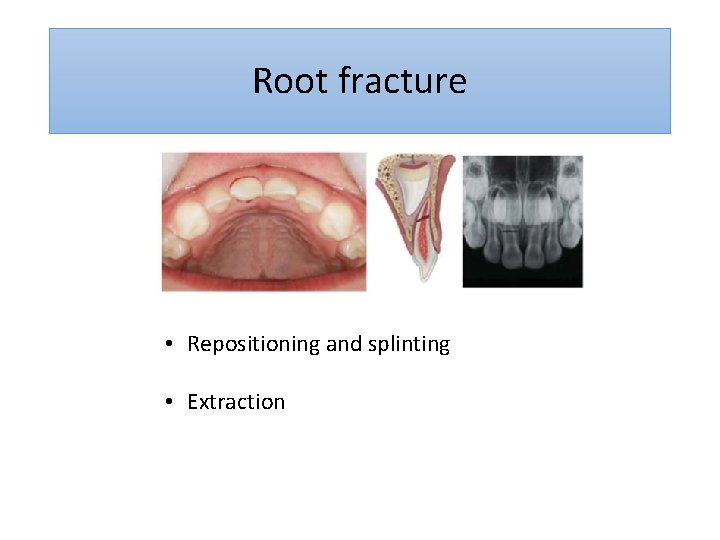
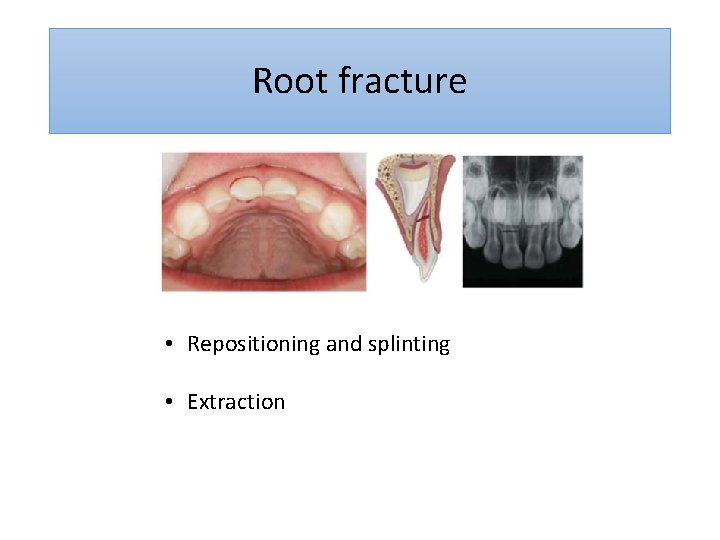
Root fracture • Repositioning and splinting • Extraction
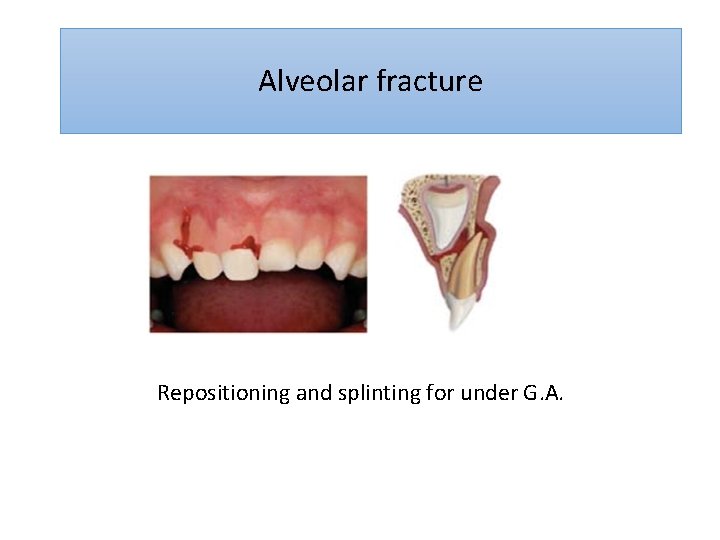
Alveolar fracture Repositioning and splinting for under G. A.
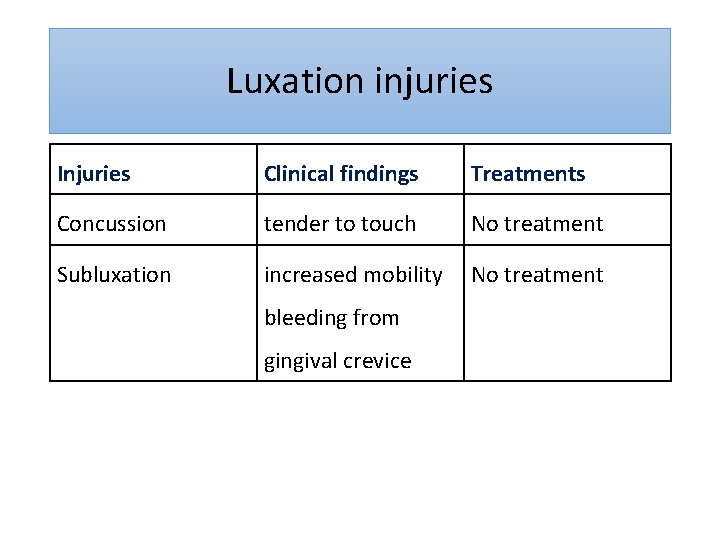
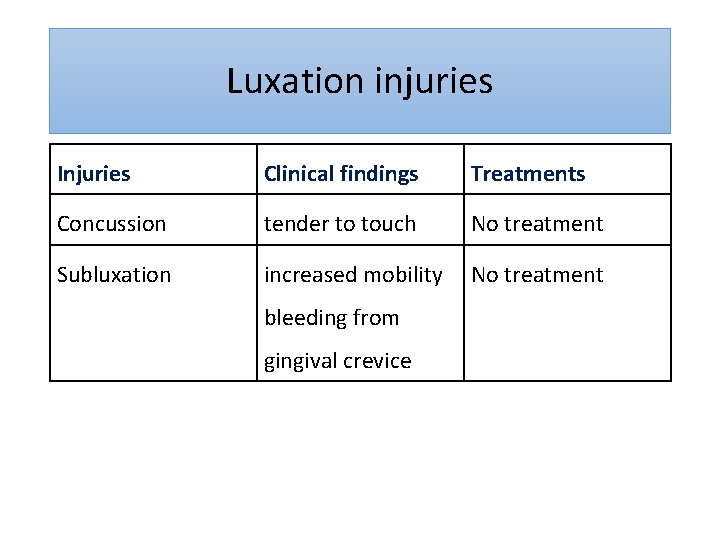
Luxation injuries Injuries Clinical findings Treatments Concussion tender to touch No treatment Subluxation increased mobility No treatment bleeding from gingival crevice
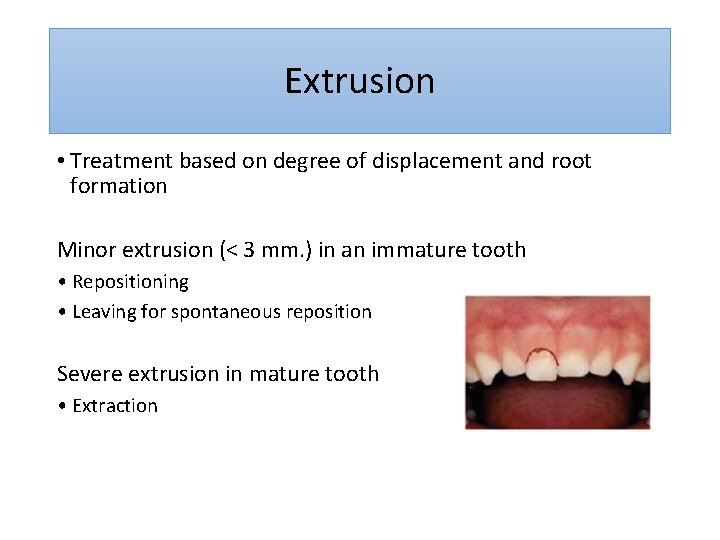
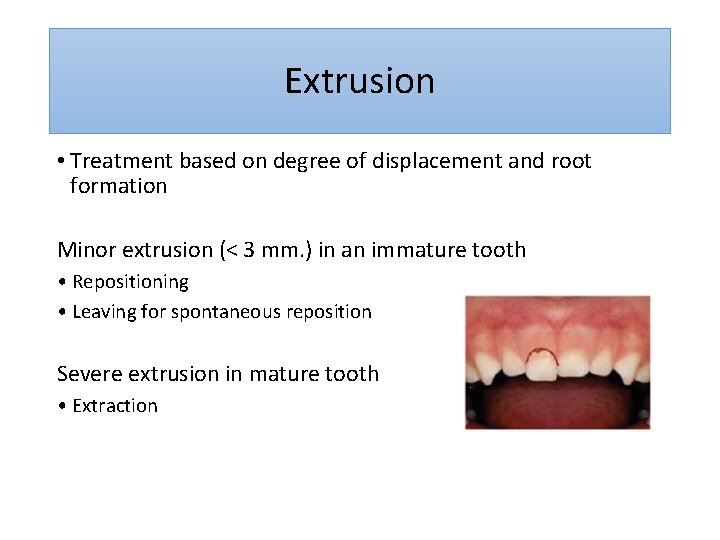
Extrusion • Treatment based on degree of displacement and root formation Minor extrusion (< 3 mm. ) in an immature tooth • Repositioning • Leaving for spontaneous reposition Severe extrusion in mature tooth • Extraction
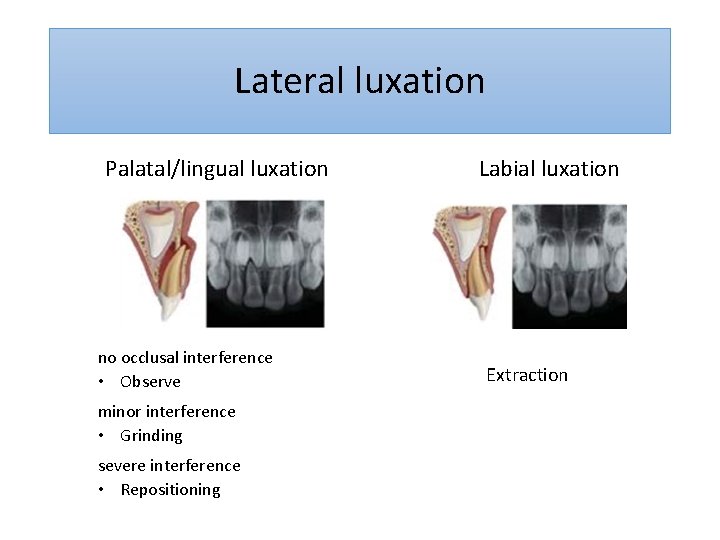
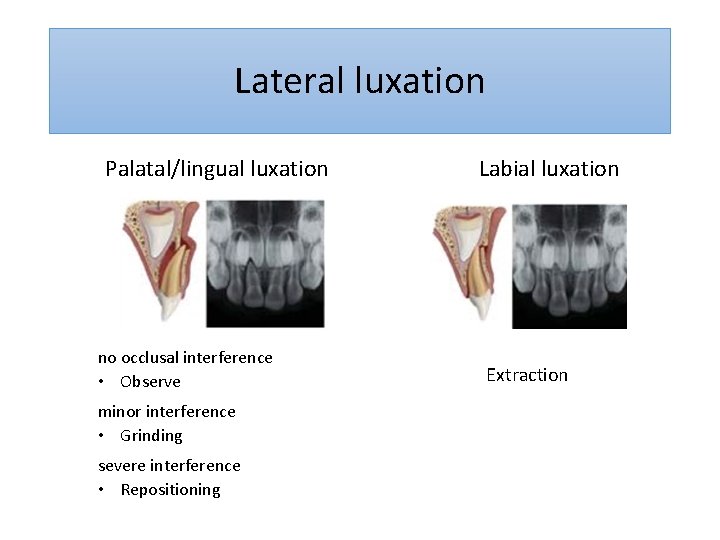
Lateral luxation Palatal/lingual luxation no occlusal interference • Observe minor interference • Grinding severe interference • Repositioning Labial luxation Extraction
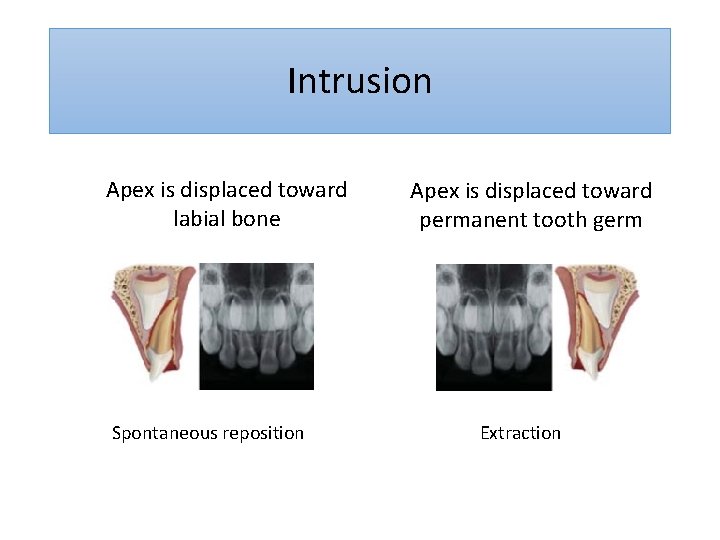
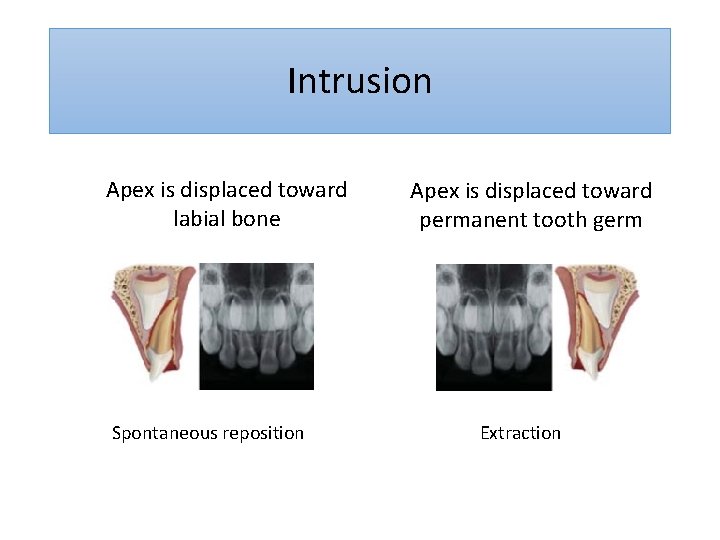
Intrusion Apex is displaced toward labial bone Spontaneous reposition Apex is displaced toward permanent tooth germ Extraction
Intrusion • Spontaneous eruption normally take place within 3 months • However some cases (25%) were not fully erupted after 1 year of trauma
Intrusion • complications during the re-eruption phase • acute inflammation around the displaced tooth • gingiva : swelling • pus from gingival crevice Immediate extraction and antibiotic therapy
Avulsion • Alternative trauma scenarios should be explored • deeply intrusion ? • Avulsed primary tooth should not be replanted • may displace a coagulum into the follicle of permanent incisor • pulp necrosis may cause mineralization disturbance
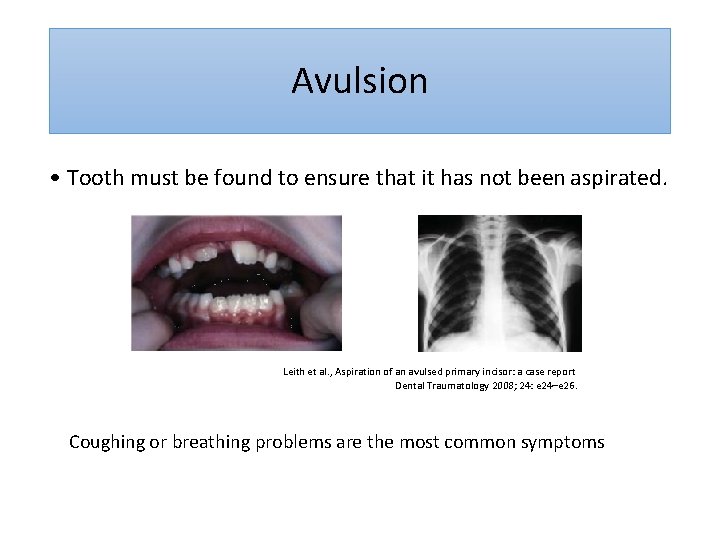
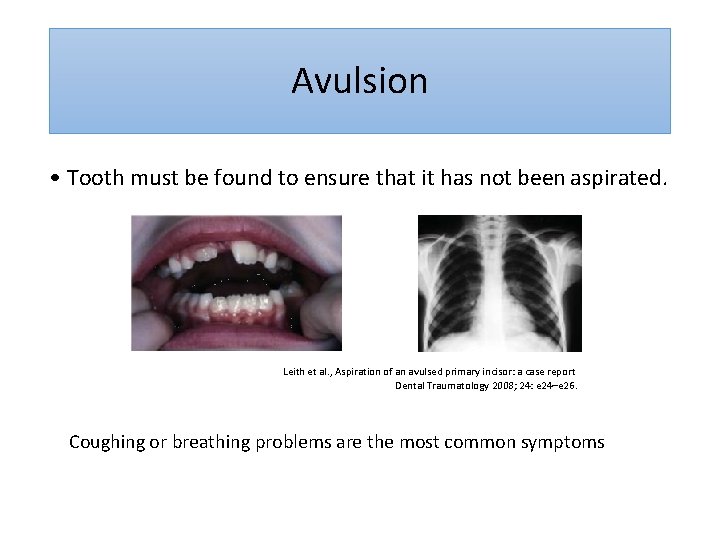
Avulsion • Tooth must be found to ensure that it has not been aspirated. Leith et al. , Aspiration of an avulsed primary incisor: a case report Dental Traumatology 2008; 24: e 24–e 26. Coughing or breathing problems are the most common symptoms
Chin trauma • Crown and crown-root fractures may occur in molar regions • Treatment depend on the severity of fracture • If extraction is the treatment of choice, space maintainer should be considered
Complications in the primary dentition How to evaluate ? • Color changes • Radiographic findings • Clinical findings : abscess
Color changes • After luxation injuries • Pink / Yellow / Gray
Color changes Gray discoloration • Transient —> Permanent yellow discoloration • Permanent —> frequently associated with pulp necrosis
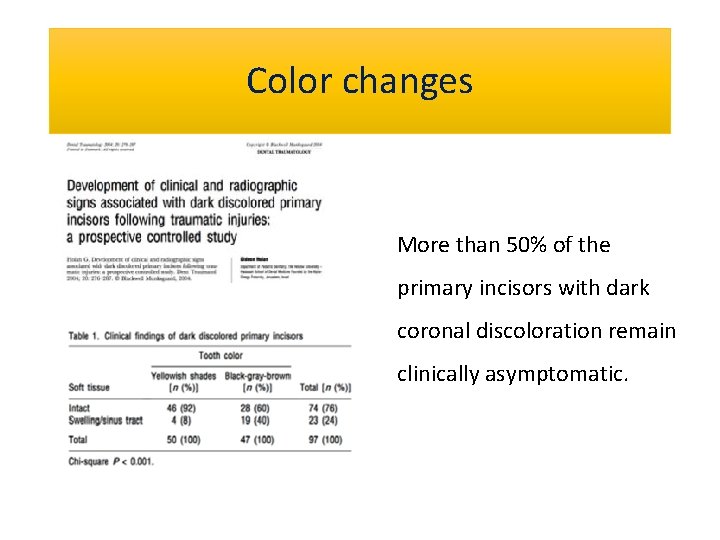
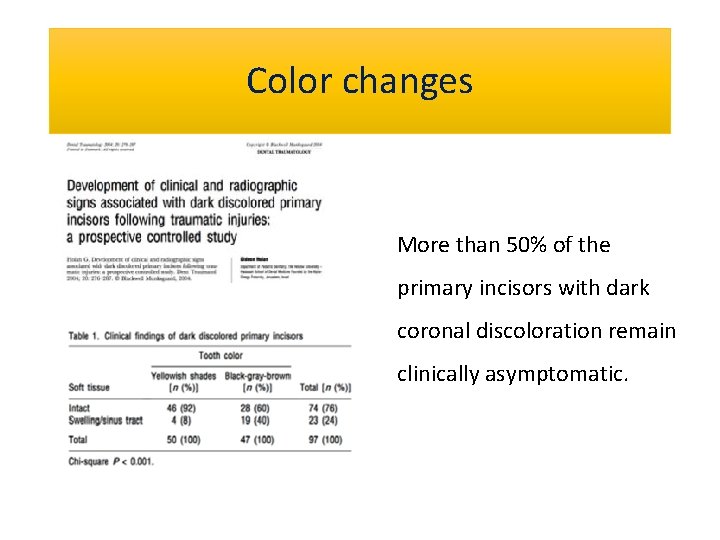
Color changes More than 50% of the primary incisors with dark coronal discoloration remain clinically asymptomatic.
Pulp necrosis • Related factors • age • degree of displacement • presence of crown fracture
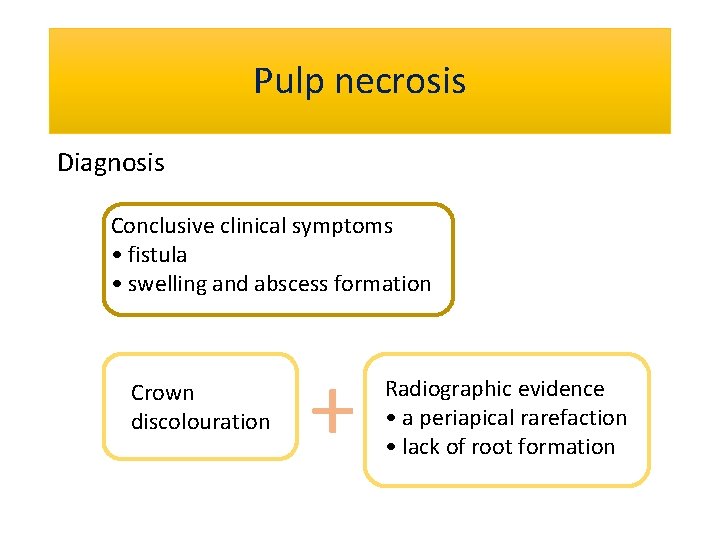
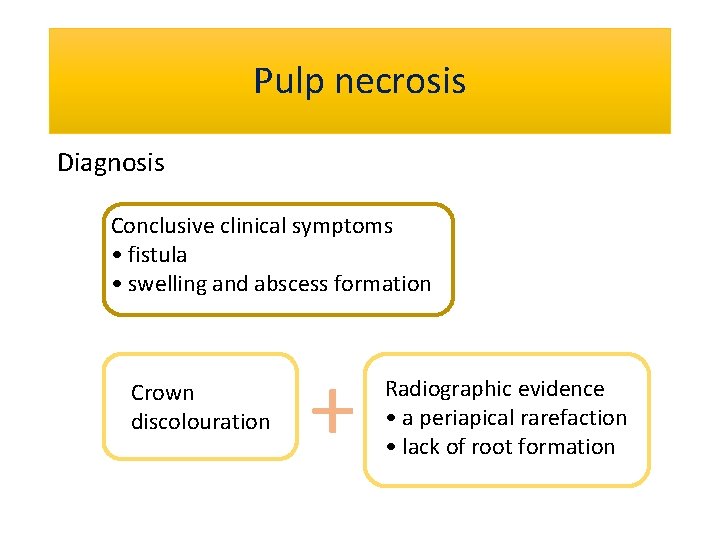
Pulp necrosis Diagnosis Conclusive clinical symptoms • fistula • swelling and abscess formation Crown discolouration + Radiographic evidence • a periapical rarefaction • lack of root formation
Instructions to parents • Keep an affected area clean • Soft toothbrush • Swab with chlorhexidine • No pacifiers and nursing bottle • โอกาสเกด trauma ซำ
Trauma ��������� ���� ? • Crown discolouration with or without enamel hypoplasia • Malformation or dilaceration of the crown • Cessation of root development • Odontoma-like formation • Disturbance in eruption
Conclusion
 Mikael ferm
Mikael ferm Peak voltage formula
Peak voltage formula Peak to peak voltage
Peak to peak voltage Widows peak phenotype
Widows peak phenotype Tscyc screening form
Tscyc screening form Tscc score sheet
Tscc score sheet Dental trauma
Dental trauma Widows peak dental
Widows peak dental Introduction of exceptional child
Introduction of exceptional child Exceptional children an introduction to special education
Exceptional children an introduction to special education Impression materials in dentistry ppt
Impression materials in dentistry ppt Introduction to dental materials
Introduction to dental materials Robert woofendale
Robert woofendale Vicarious traumatisation
Vicarious traumatisation Trauma gestig behindert
Trauma gestig behindert Trauma thorax
Trauma thorax Trauma sensitief lesgeven
Trauma sensitief lesgeven Trauma awareness and treatment center utah
Trauma awareness and treatment center utah 4 r's trauma informed care
4 r's trauma informed care Lgbt trauma informed care
Lgbt trauma informed care Dental mobility classification
Dental mobility classification Miemss trauma decision tree
Miemss trauma decision tree Examples of little t trauma
Examples of little t trauma Trauma bond
Trauma bond Trauma timeline template
Trauma timeline template Anita ravi md
Anita ravi md Golden hour of trauma
Golden hour of trauma Triune brain theory and trauma
Triune brain theory and trauma 4 r's trauma informed care
4 r's trauma informed care Nethercutt emergency center
Nethercutt emergency center Psykoedukation trauma
Psykoedukation trauma Trauma bonding cycle
Trauma bonding cycle Dermoabrasiones
Dermoabrasiones National trauma data bank annual report 2020
National trauma data bank annual report 2020 Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Descerebración y decorticación
Descerebración y decorticación Ocular trauma score
Ocular trauma score Adhd vs trauma
Adhd vs trauma