Decompressive Hemicraniectomy and Duraplasty for Malignant Infarction of


- Slides: 23

Decompressive Hemicraniectomy and Duraplasty for Malignant Infarction of the Middle Cerebral Artery 神經內科 洪國華
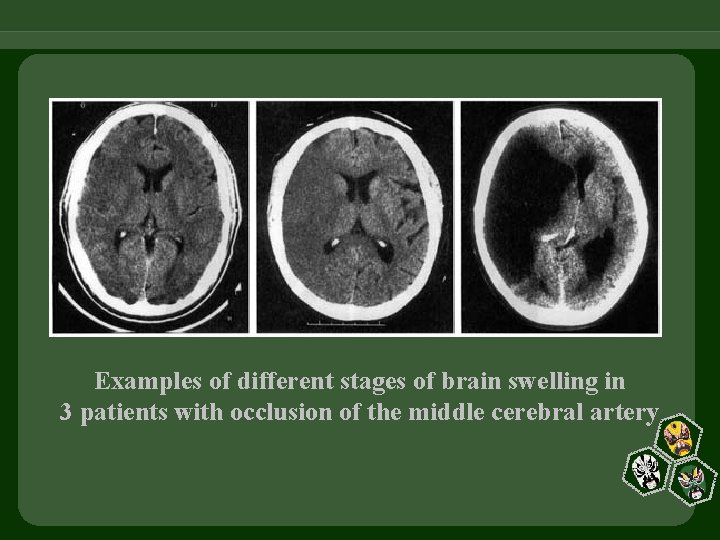
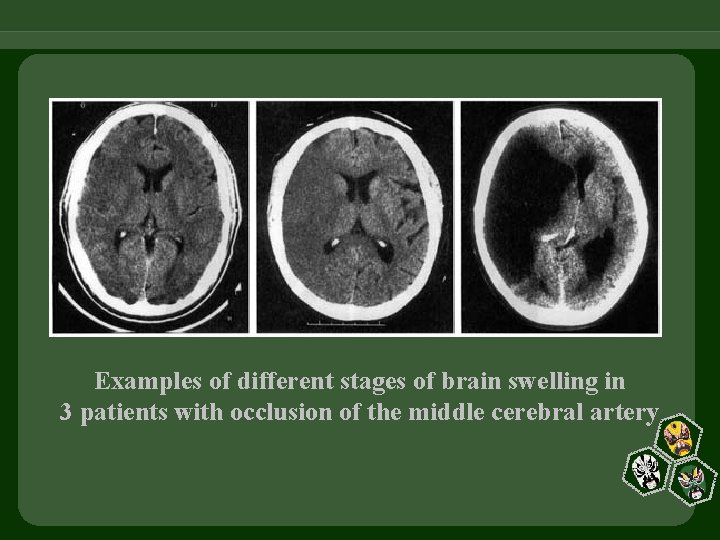
Examples of different stages of brain swelling in 3 patients with occlusion of the middle cerebral artery
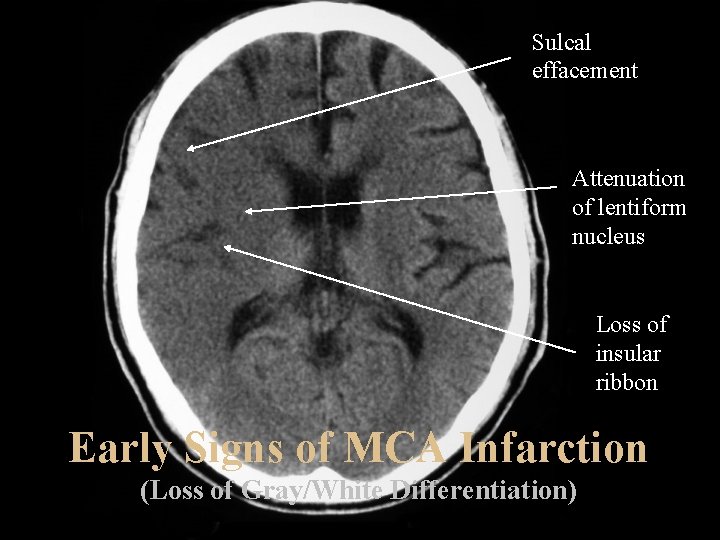
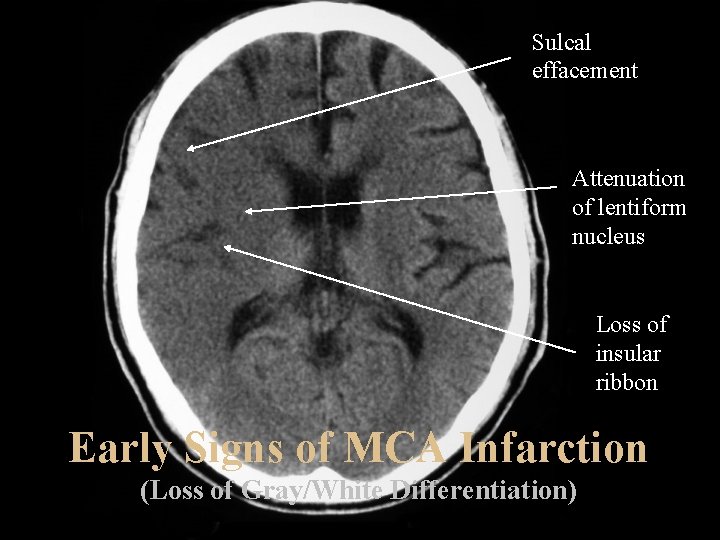
Sulcal effacement Attenuation of lentiform nucleus Loss of insular ribbon Early Signs of MCA Infarction (Loss of Gray/White Differentiation)
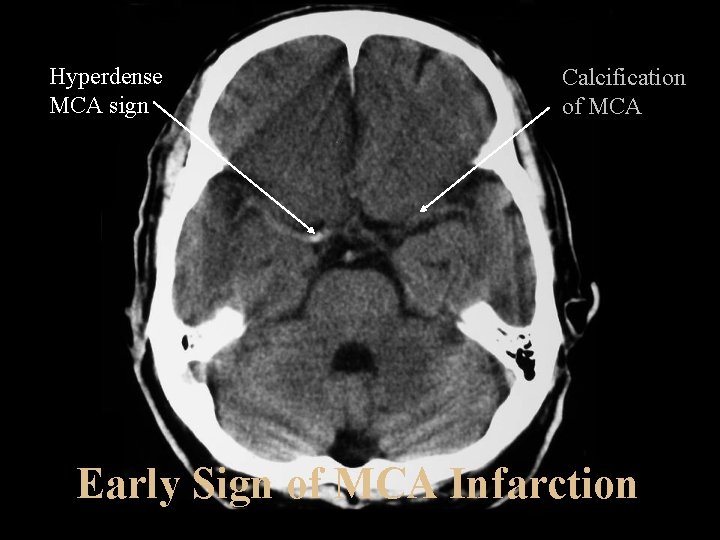
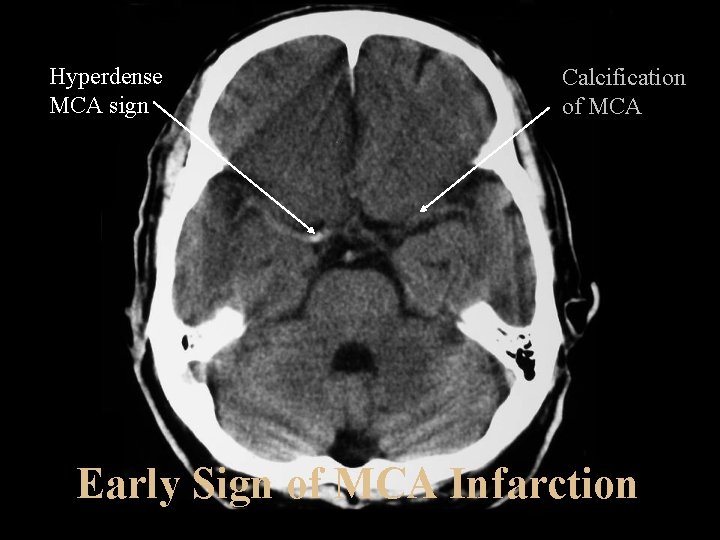
Hyperdense MCA sign Calcification of MCA Early Sign of MCA Infarction
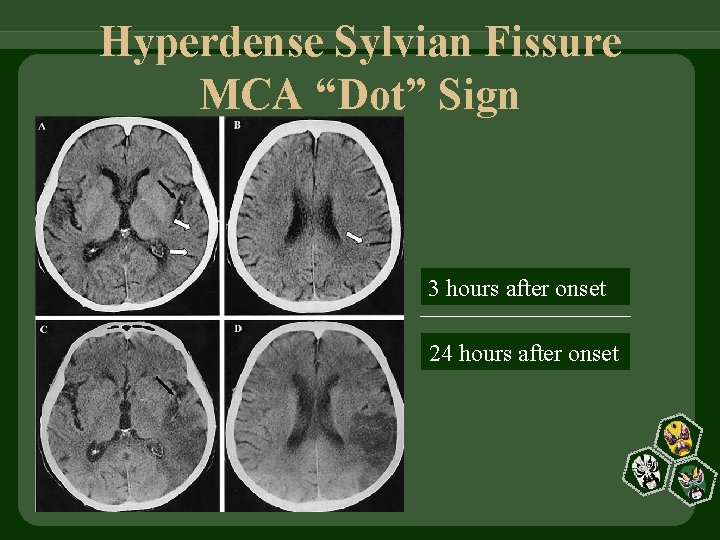
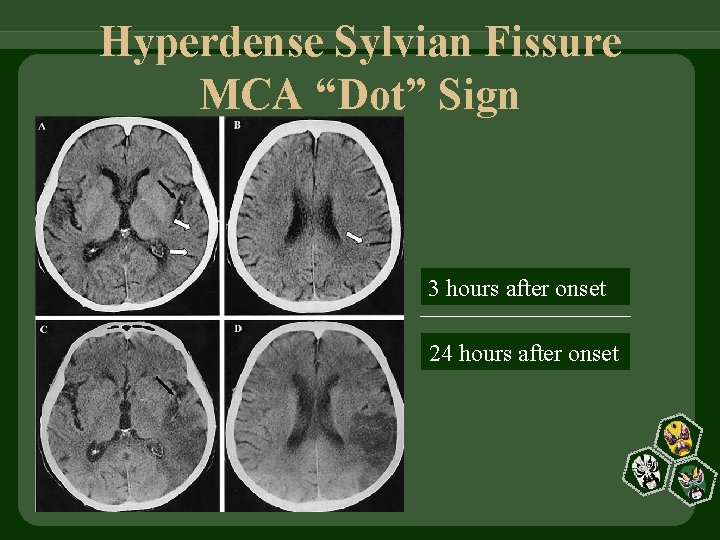
Hyperdense Sylvian Fissure MCA “Dot” Sign 3 hours after onset 24 hours after onset
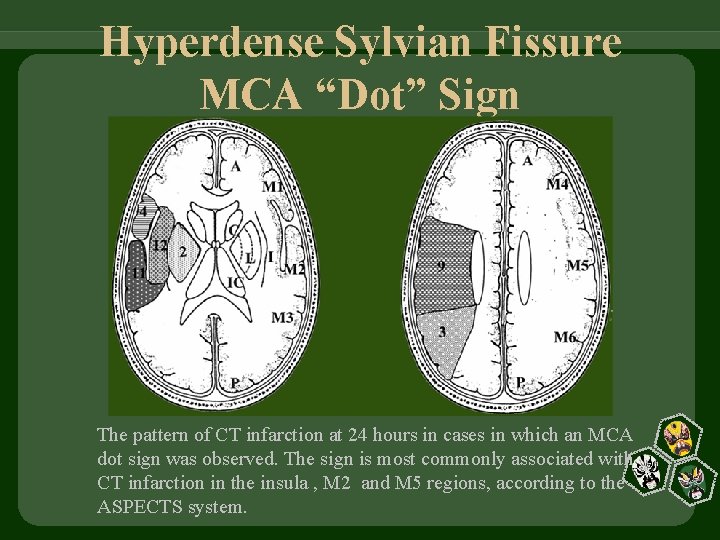
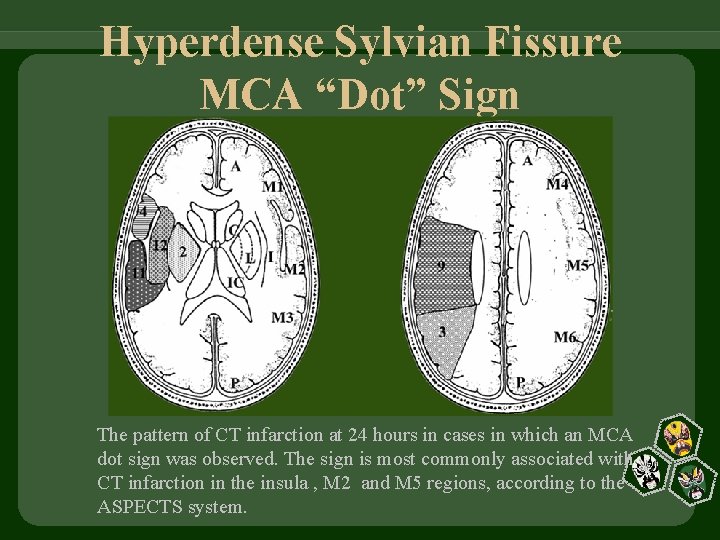
Hyperdense Sylvian Fissure MCA “Dot” Sign The pattern of CT infarction at 24 hours in cases in which an MCA dot sign was observed. The sign is most commonly associated with CT infarction in the insula , M 2 and M 5 regions, according to the ASPECTS system.
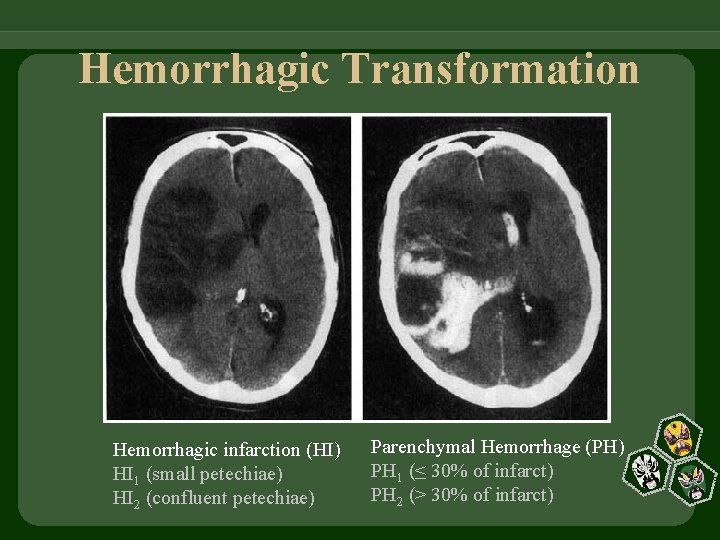
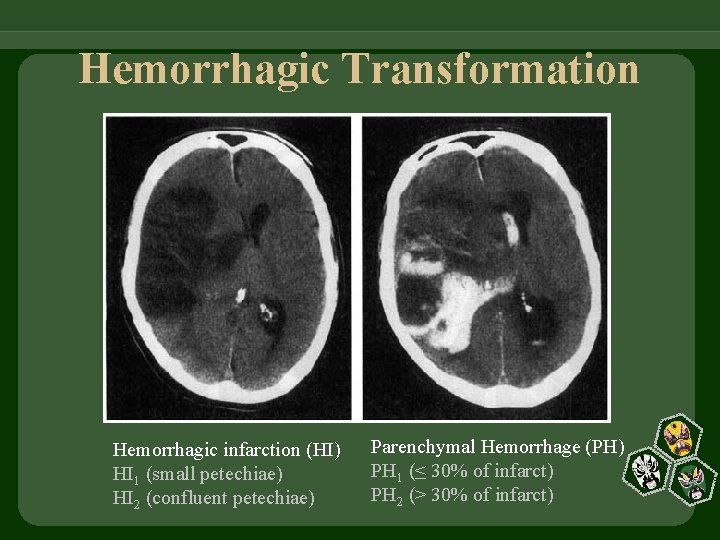
Hemorrhagic Transformation Hemorrhagic infarction (HI) HI 1 (small petechiae) HI 2 (confluent petechiae) Parenchymal Hemorrhage (PH) PH 1 (≤ 30% of infarct) PH 2 (> 30% of infarct)
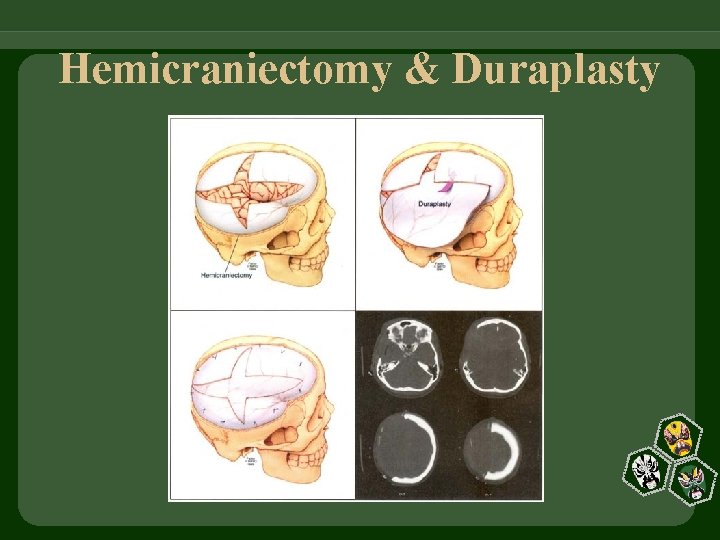
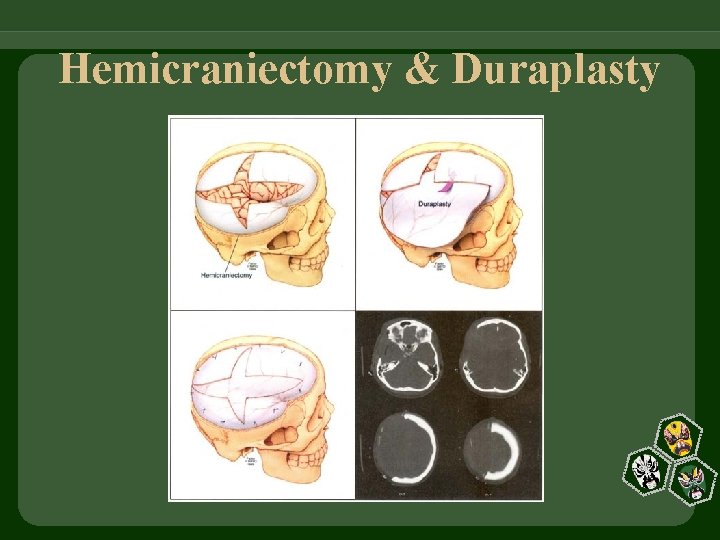
Hemicraniectomy & Duraplasty
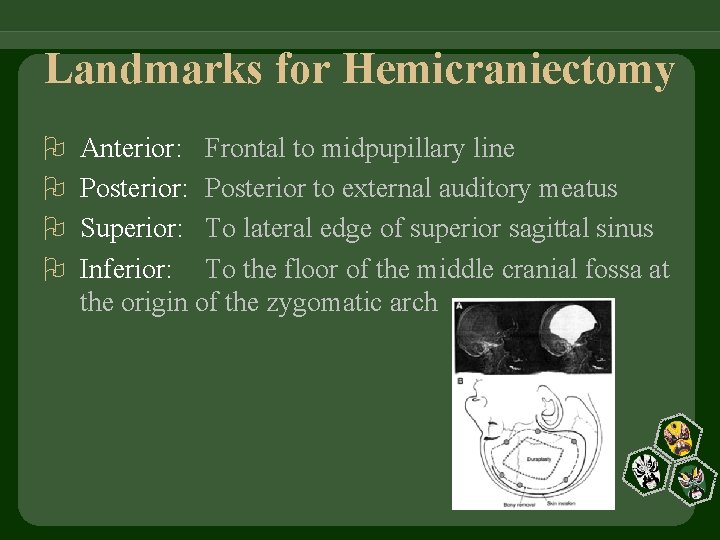
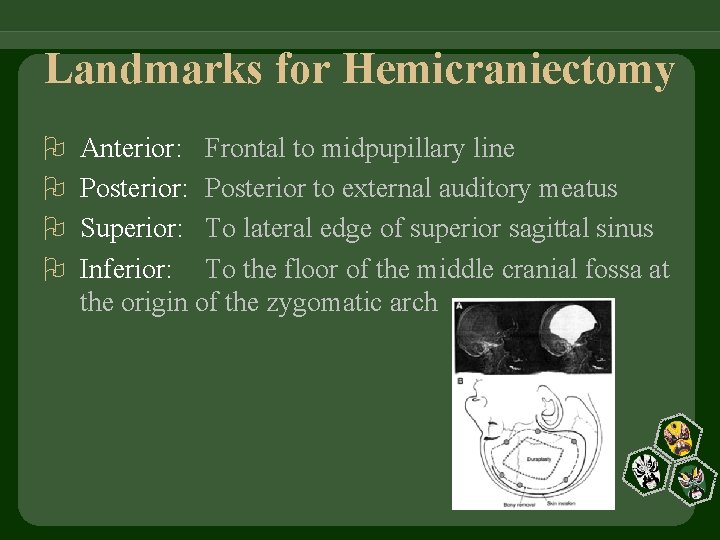
Landmarks for Hemicraniectomy Anterior: Frontal to midpupillary line Posterior: Posterior to external auditory meatus Superior: To lateral edge of superior sagittal sinus Inferior: To the floor of the middle cranial fossa at the origin of the zygomatic arch

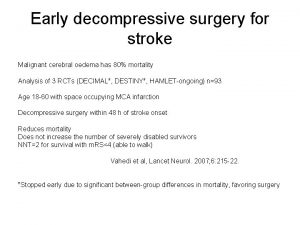
5 Randomized Trials He. ADDFIRST (US) He. MMI (Philippines) HAMLET (Netherlands) DECIMAL (France) DESTINY (Germany)
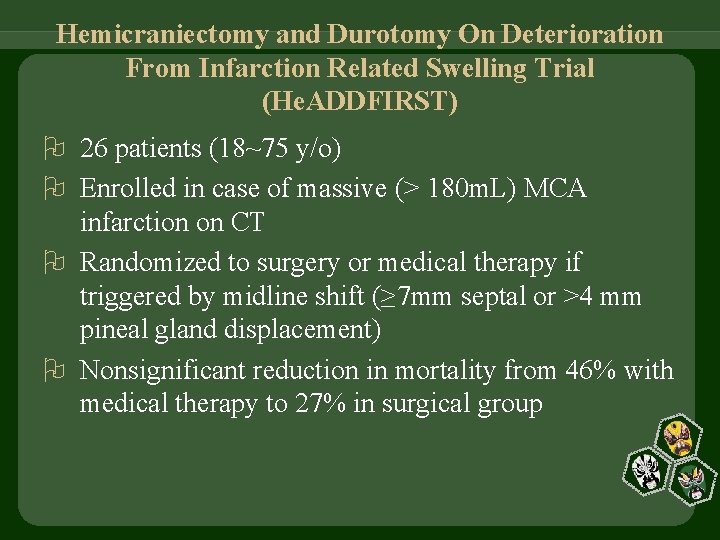
Hemicraniectomy and Durotomy On Deterioration From Infarction Related Swelling Trial (He. ADDFIRST) 26 patients (18~75 y/o) Enrolled in case of massive (> 180 m. L) MCA infarction on CT Randomized to surgery or medical therapy if triggered by midline shift (≥ 7 mm septal or >4 mm pineal gland displacement) Nonsignificant reduction in mortality from 46% with medical therapy to 27% in surgical group
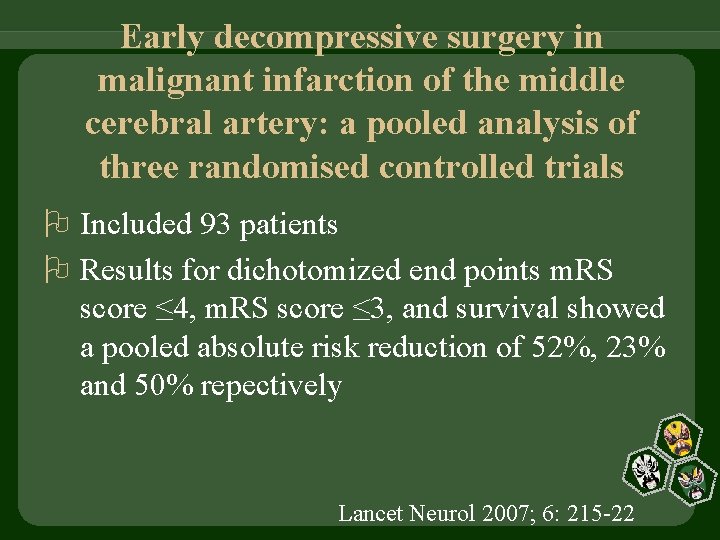
Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials Included 93 patients Results for dichotomized end points m. RS score ≤ 4, m. RS score ≤ 3, and survival showed a pooled absolute risk reduction of 52%, 23% and 50% repectively Lancet Neurol 2007; 6: 215 -22
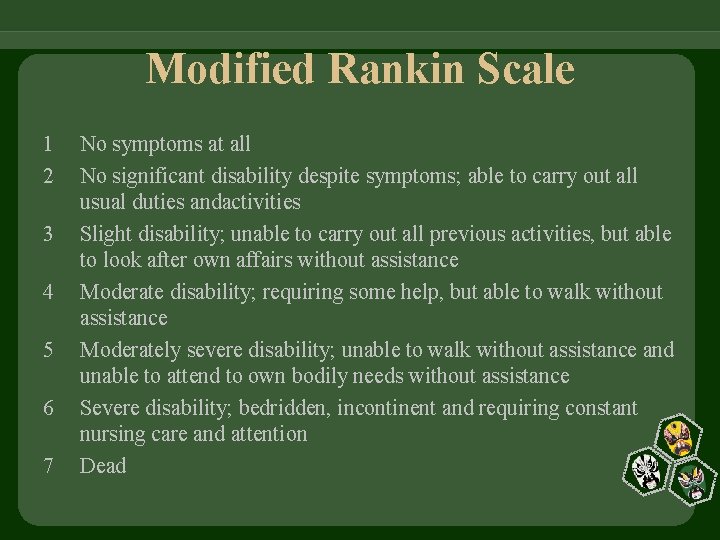
Modified Rankin Scale 1 2 3 4 5 6 7 No symptoms at all No significant disability despite symptoms; able to carry out all usual duties andactivities Slight disability; unable to carry out all previous activities, but able to look after own affairs without assistance Moderate disability; requiring some help, but able to walk without assistance Moderately severe disability; unable to walk without assistance and unable to attend to own bodily needs without assistance Severe disability; bedridden, incontinent and requiring constant nursing care and attention Dead
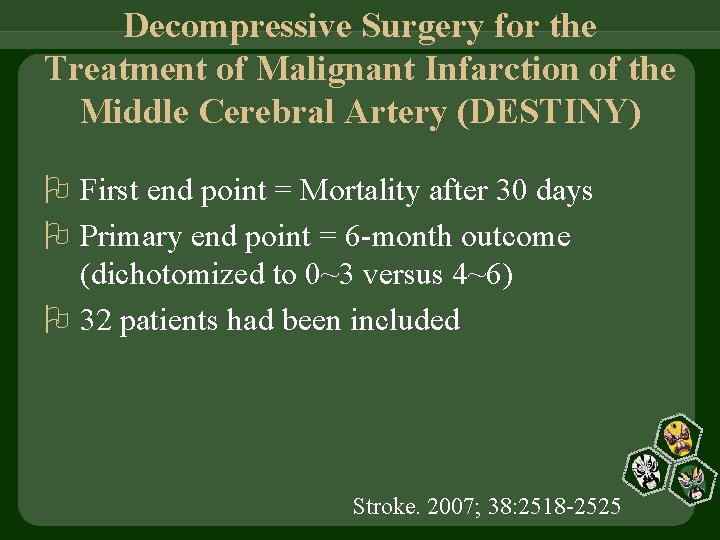
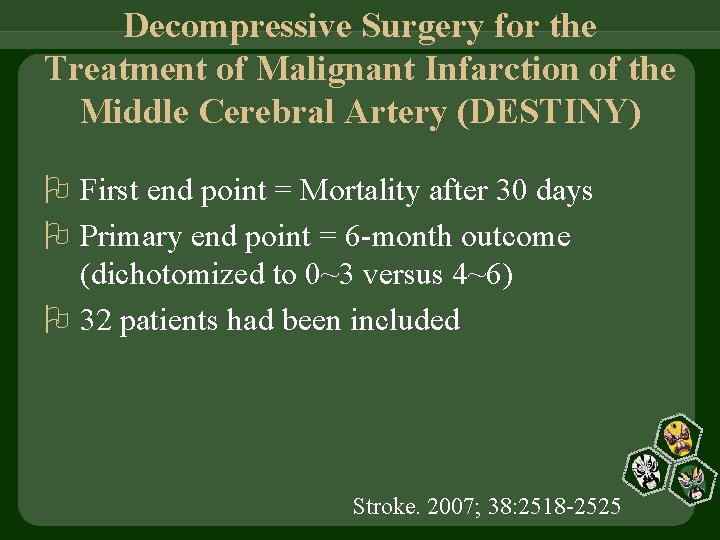
Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery (DESTINY) First end point = Mortality after 30 days Primary end point = 6 -month outcome (dichotomized to 0~3 versus 4~6) 32 patients had been included Stroke. 2007; 38: 2518 -2525
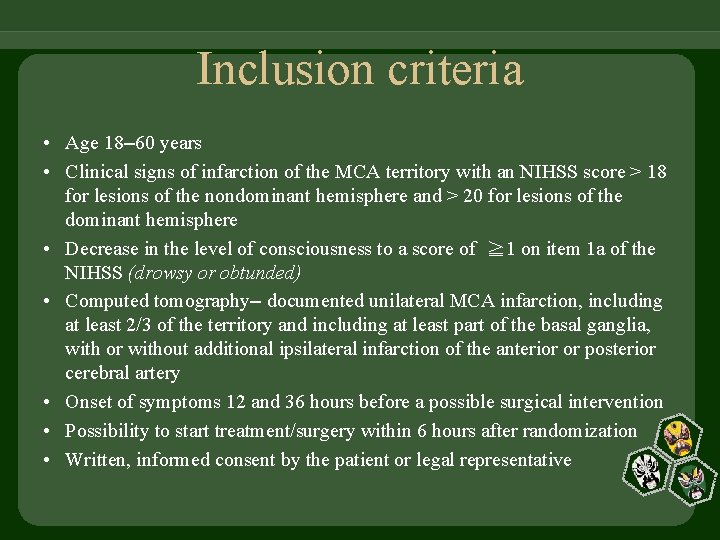
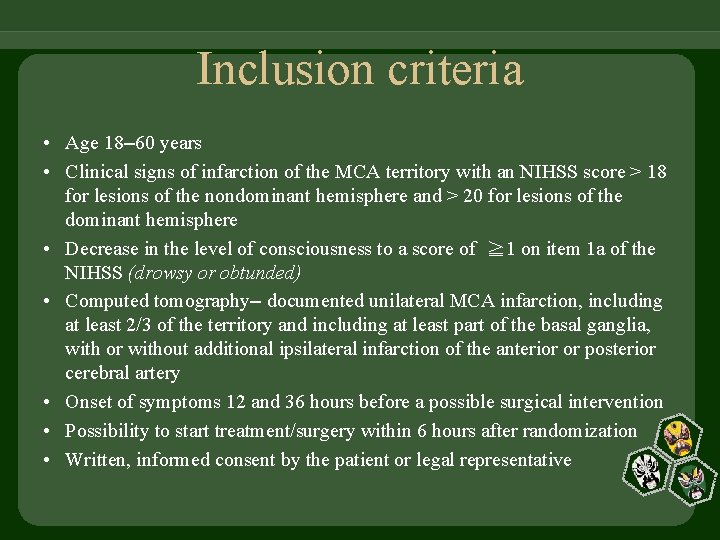
Inclusion criteria • Age 18– 60 years • Clinical signs of infarction of the MCA territory with an NIHSS score > 18 for lesions of the nondominant hemisphere and > 20 for lesions of the dominant hemisphere • Decrease in the level of consciousness to a score of ≧ 1 on item 1 a of the NIHSS (drowsy or obtunded) • Computed tomography– documented unilateral MCA infarction, including at least 2/3 of the territory and including at least part of the basal ganglia, with or without additional ipsilateral infarction of the anterior or posterior cerebral artery • Onset of symptoms 12 and 36 hours before a possible surgical intervention • Possibility to start treatment/surgery within 6 hours after randomization • Written, informed consent by the patient or legal representative
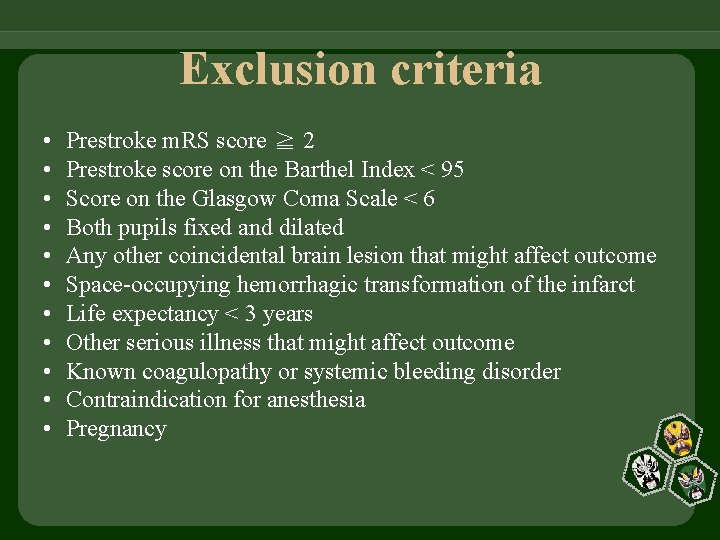
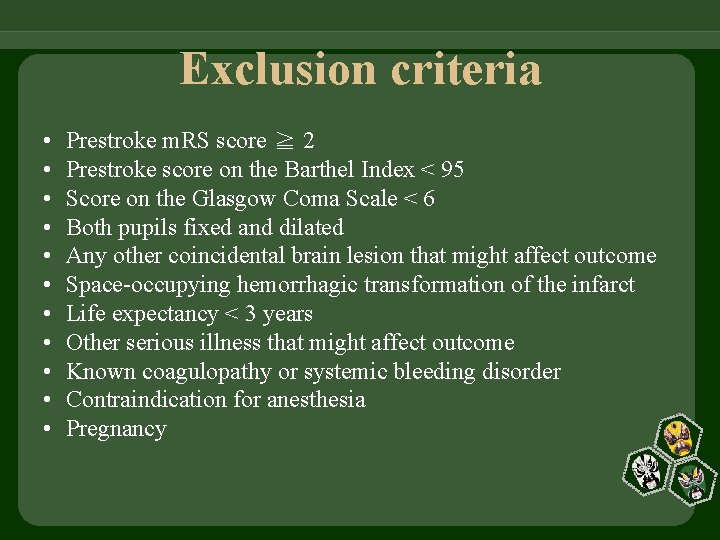
Exclusion criteria • • • Prestroke m. RS score ≧ 2 Prestroke score on the Barthel Index < 95 Score on the Glasgow Coma Scale < 6 Both pupils fixed and dilated Any other coincidental brain lesion that might affect outcome Space-occupying hemorrhagic transformation of the infarct Life expectancy < 3 years Other serious illness that might affect outcome Known coagulopathy or systemic bleeding disorder Contraindication for anesthesia Pregnancy
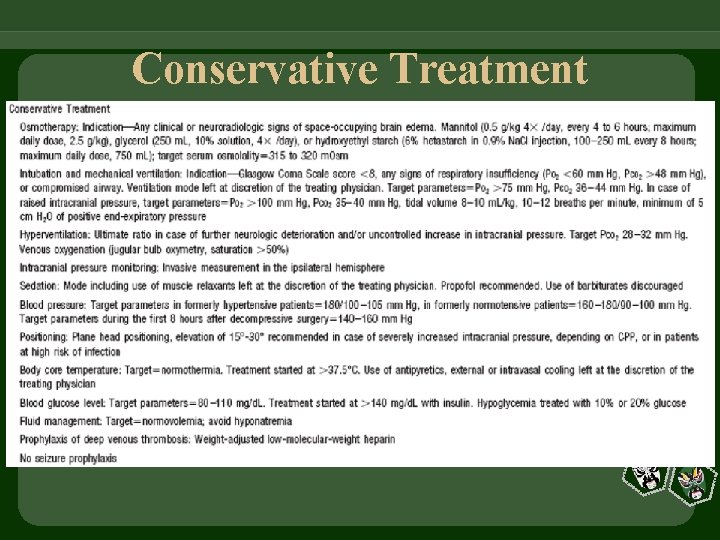
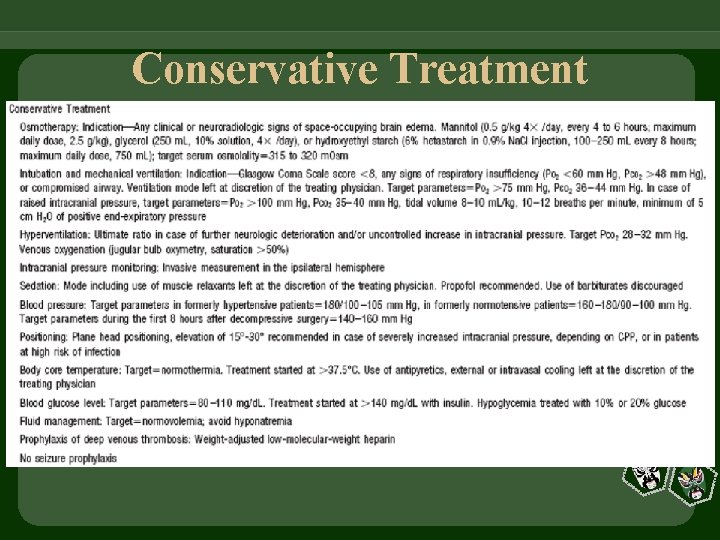
Conservative Treatment
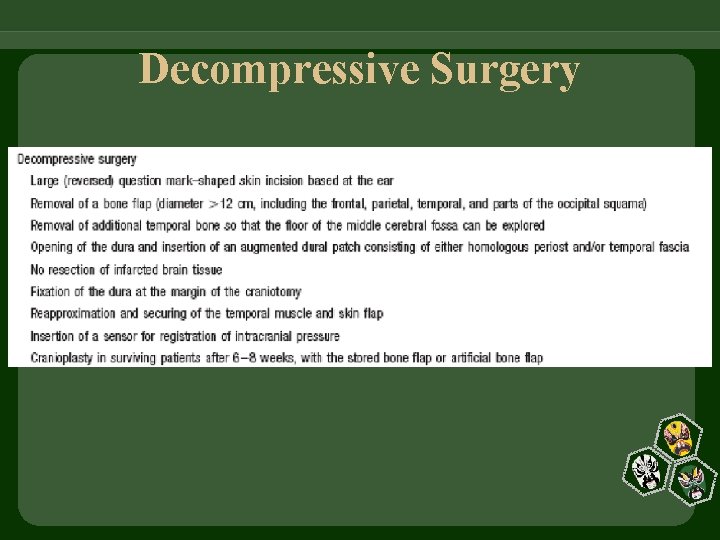
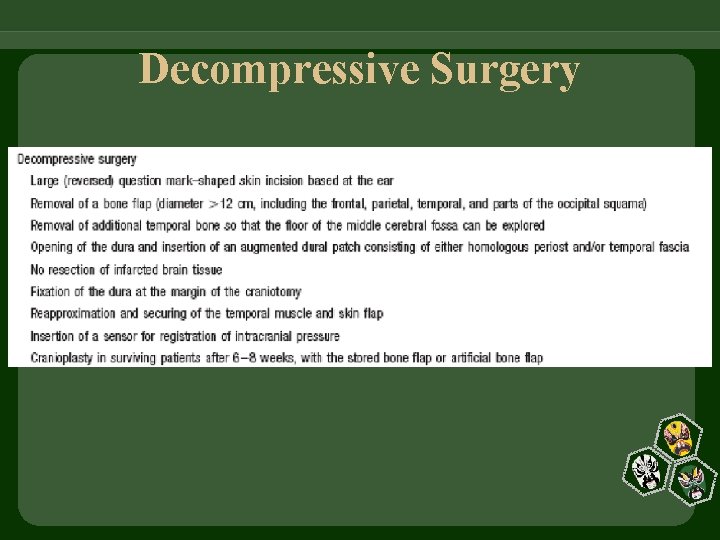
Decompressive Surgery
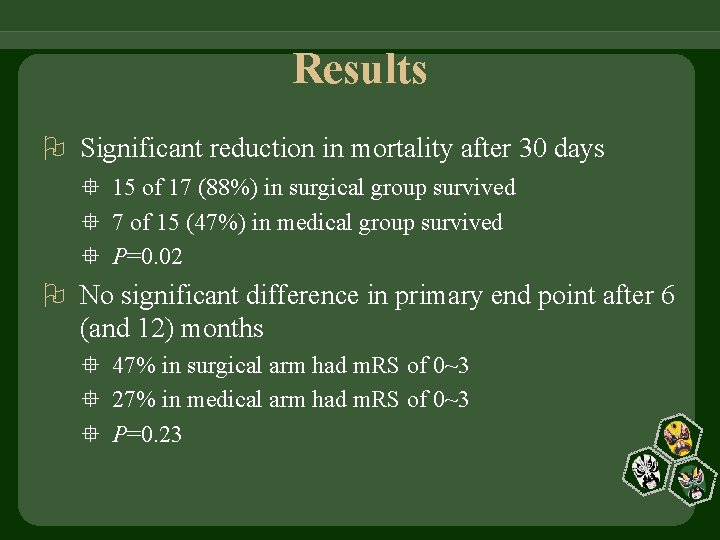
Results Significant reduction in mortality after 30 days 15 of 17 (88%) in surgical group survived 7 of 15 (47%) in medical group survived P=0. 02 No significant difference in primary end point after 6 (and 12) months 47% in surgical arm had m. RS of 0~3 27% in medical arm had m. RS of 0~3 P=0. 23
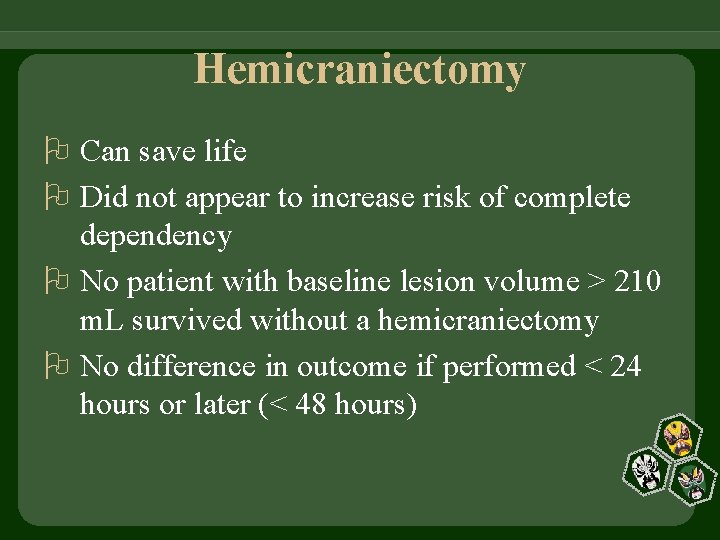
Hemicraniectomy Can save life Did not appear to increase risk of complete dependency No patient with baseline lesion volume > 210 m. L survived without a hemicraniectomy No difference in outcome if performed < 24 hours or later (< 48 hours)
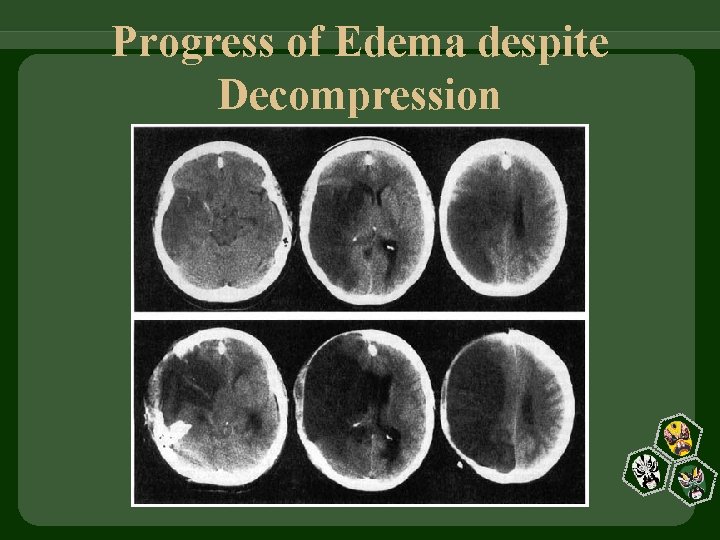
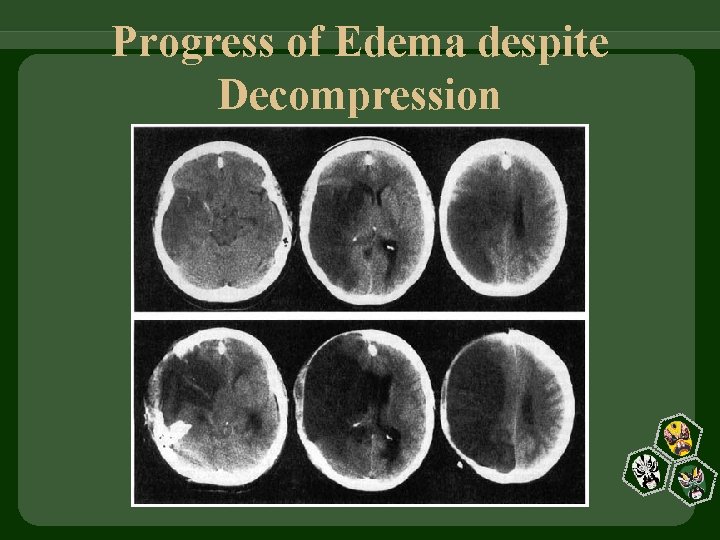
Progress of Edema despite Decompression
For Every 10 Hemicraniectomies for MCA Infarction 5 patients will escape death and at 1 year Mild disability = 1 Moderate-to-severe disability = 3 (unable to walk independently)
Hemicraniectomy + Duraplasty A second chance on life for patients with space-occupying MCA infarction
 Myelomalacia icd 10
Myelomalacia icd 10 Avc malin
Avc malin Pico question myocardial infarction
Pico question myocardial infarction Myocardinal infraction
Myocardinal infraction Jamal gross
Jamal gross Idioventricular rhythm ecg
Idioventricular rhythm ecg Anterior leads
Anterior leads Pancreas wiki
Pancreas wiki Myocardial infarction pain location
Myocardial infarction pain location Peter hino md
Peter hino md Liposarcoma
Liposarcoma Benign and malignant tumor
Benign and malignant tumor Benign vs malignant
Benign vs malignant Malignant neuroleptic syndrome
Malignant neuroleptic syndrome Nail body
Nail body Cataractectomy
Cataractectomy Kitwood's psychological needs
Kitwood's psychological needs Neuroleptic malignant syndrome
Neuroleptic malignant syndrome Hypokalemia
Hypokalemia Hypertensive urgency
Hypertensive urgency Malignant neoplasm of the blood-forming organs
Malignant neoplasm of the blood-forming organs Malignant mesothelioma
Malignant mesothelioma Malignant neoplasm of liver
Malignant neoplasm of liver Neoplasia
Neoplasia