Role of Decompressive Craniectomy in Head Injury Terengganu







- Slides: 34

Role of Decompressive Craniectomy in Head Injury Terengganu Neurotrauma Symposium 2019
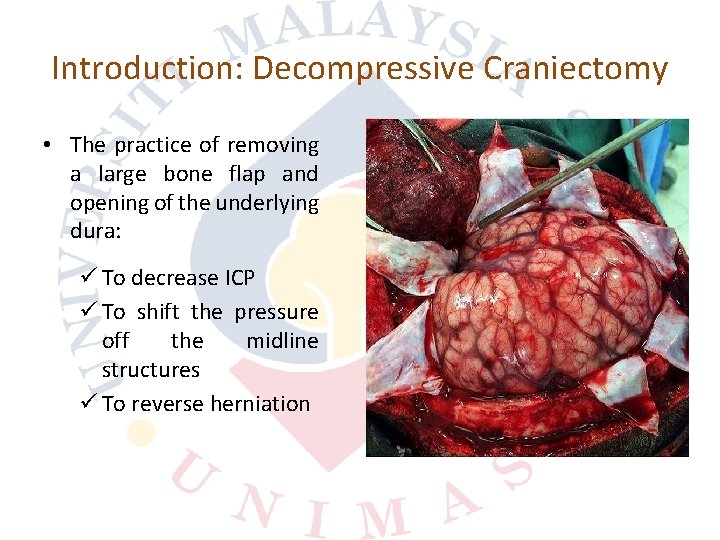
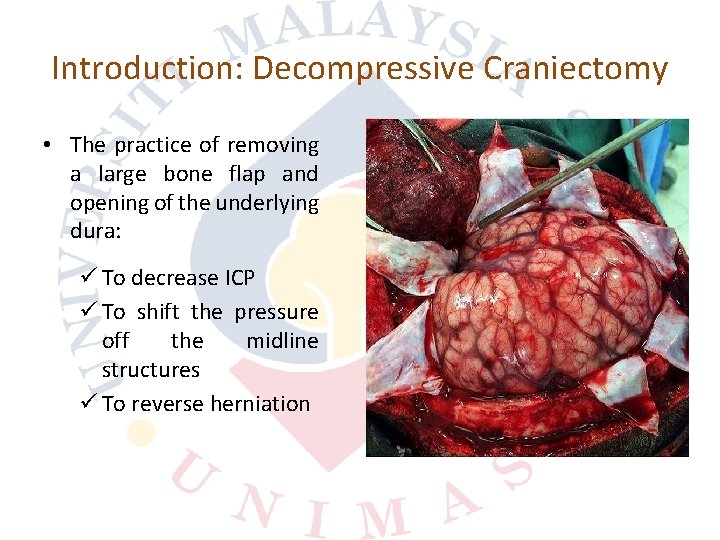
Introduction: Decompressive Craniectomy • The practice of removing a large bone flap and opening of the underlying dura: ü To decrease ICP ü To shift the pressure off the midline structures ü To reverse herniation
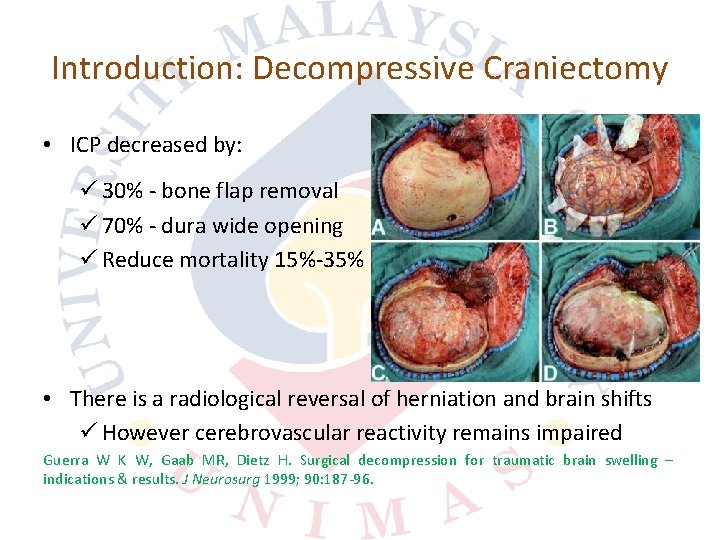
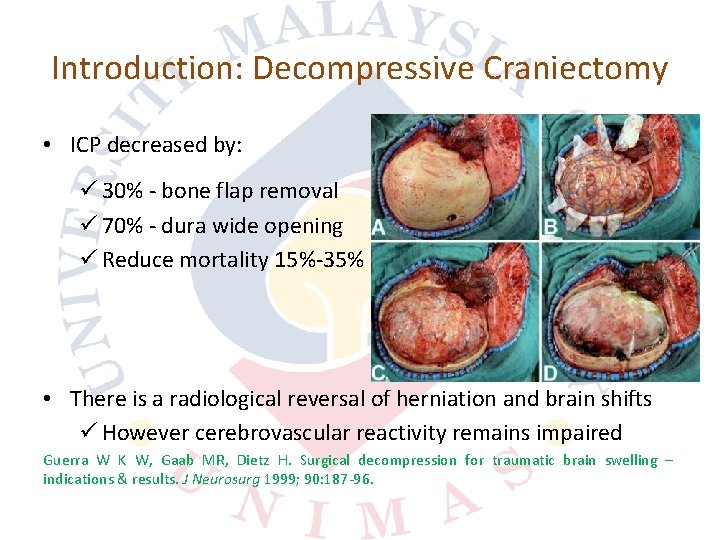
Introduction: Decompressive Craniectomy • ICP decreased by: ü 30% bone flap removal ü 70% dura wide opening ü Reduce mortality 15% 35% • There is a radiological reversal of herniation and brain shifts ü However cerebrovascular reactivity remains impaired Guerra W K W, Gaab MR, Dietz H. Surgical decompression for traumatic brain swelling – indications & results. J Neurosurg 1999; 90: 187 96.

Types of DC: Unilateral • Hemicraniectomy / frontotemporoparietal craniectomy ü Removal of a large frontotemporoparietal bone flap

Types of DC: Bifrontal • Bifrontal DC ü Removal of a bone flap extending from the floor of anterior cranial fossa to the coronal suture, and to the middle cranial fossa floor bilaterally
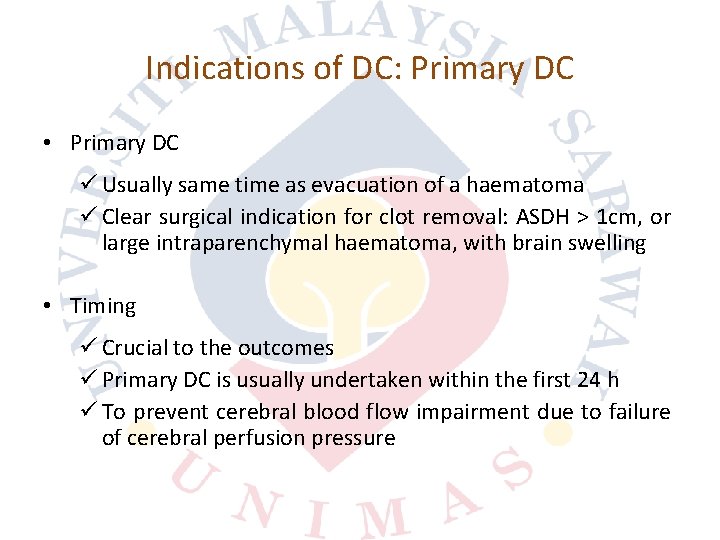
Indications of DC: Primary DC • Primary DC ü Usually same time as evacuation of a haematoma ü Clear surgical indication for clot removal: ASDH > 1 cm, or large intraparenchymal haematoma, with brain swelling • Timing ü Crucial to the outcomes ü Primary DC is usually undertaken within the first 24 h ü To prevent cerebral blood flow impairment due to failure of cerebral perfusion pressure
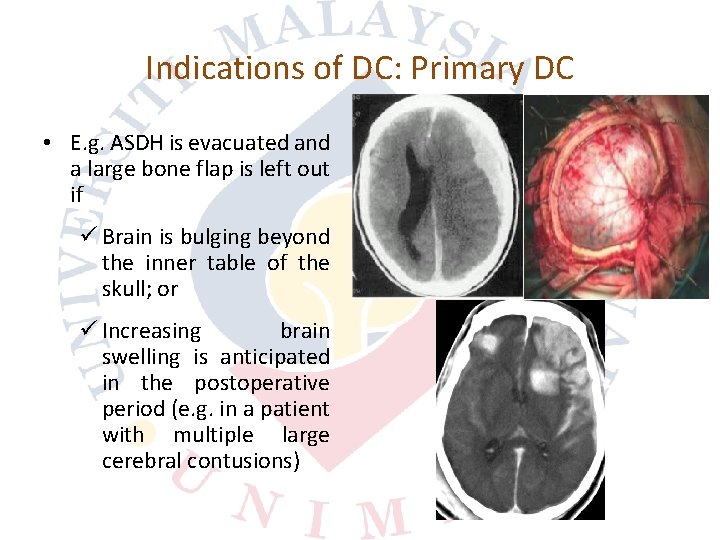
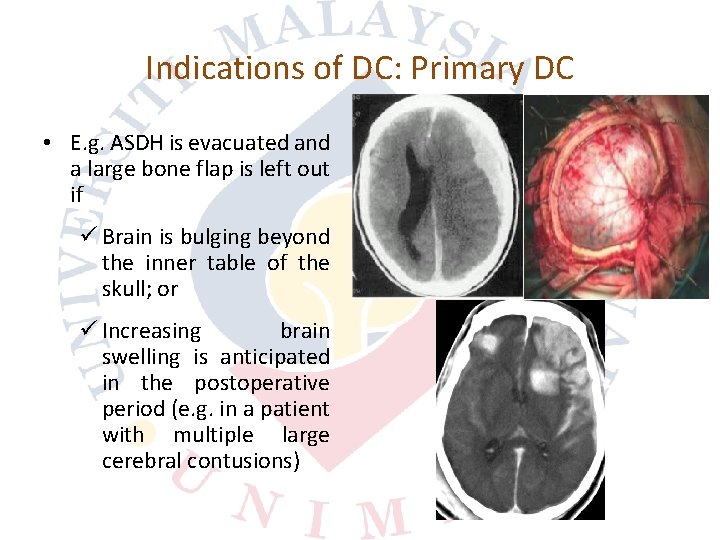
Indications of DC: Primary DC • E. g. ASDH is evacuated and a large bone flap is left out if ü Brain is bulging beyond the inner table of the skull; or ü Increasing brain swelling is anticipated in the postoperative period (e. g. in a patient with multiple large cerebral contusions)
Indications of DC: Secondary DC • Patients who initially managed with ICP monitoring; or • Patients who have had a craniotomy for evacuation of an intracranial hematoma in the early phase after injury ü To control refractory elevation of ICP, and/or ü To treat clinical or radiological deterioration
Factors Affecting Outcome: Timing • In intraparenchymal bleed, the onset of life threatening brain swelling is within 2 to 3 hours ü Due to the osmotic load (up to 390 m. Osmol) exerted by the break down debris of membrane & cytoplasmic structures • A second phase of oedema occurs from 3 to 5 days ü Due to the breakdown of RBC and resultant inflammatory cascades • The optimal timing of surgery is within 6 hours

Factors Affecting Outcome: DC Size • Small and inadequate size may cause further brain damage ü Squeezing of the brain cortex and cortical veins ü Increase the risk of contusions at the bone edge and may cause greater axonal strain
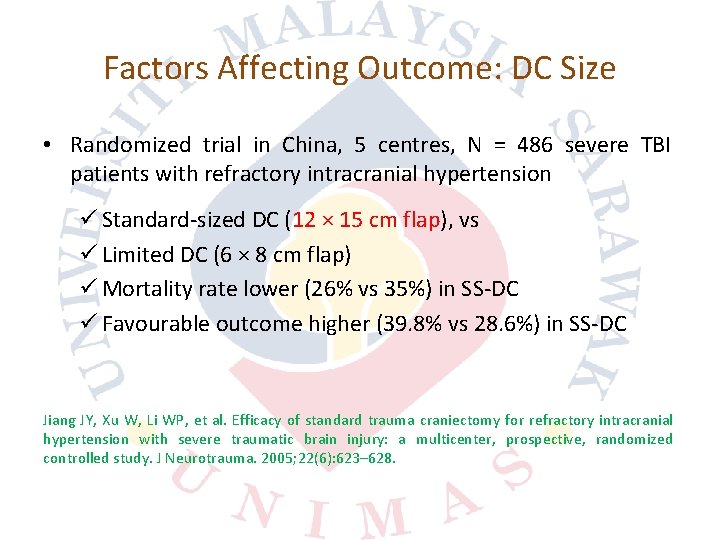
Factors Affecting Outcome: DC Size • Randomized trial in China, 5 centres, N = 486 severe TBI patients with refractory intracranial hypertension ü Standard sized DC (12 × 15 cm flap), vs ü Limited DC (6 × 8 cm flap) ü Mortality rate lower (26% vs 35%) in SS DC ü Favourable outcome higher (39. 8% vs 28. 6%) in SS DC Jiang JY, Xu W, Li WP, et al. Efficacy of standard trauma craniectomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter, prospective, randomized controlled study. J Neurotrauma. 2005; 22(6): 623– 628.
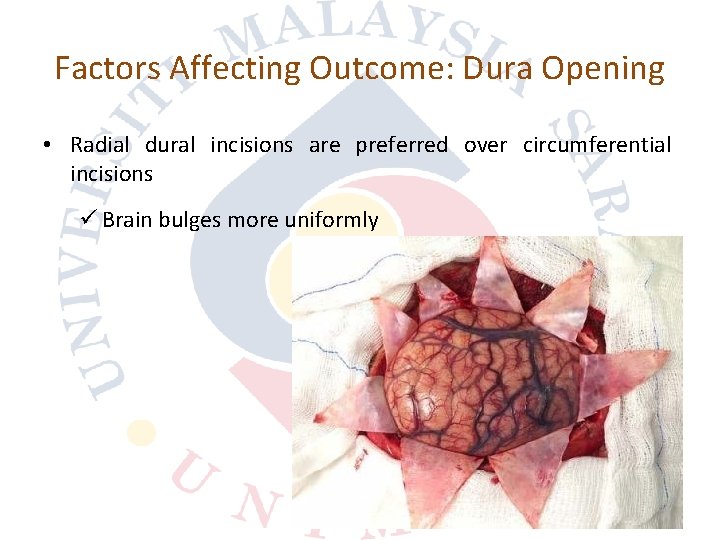
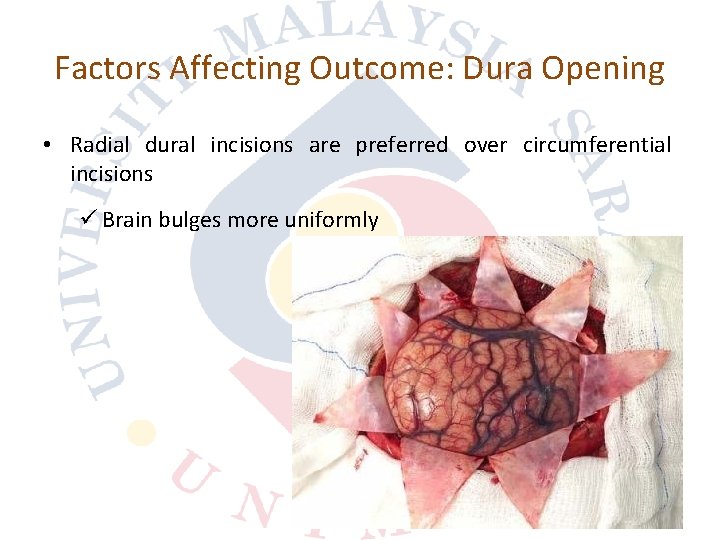
Factors Affecting Outcome: Dura Opening • Radial dural incisions are preferred over circumferential incisions ü Brain bulges more uniformly

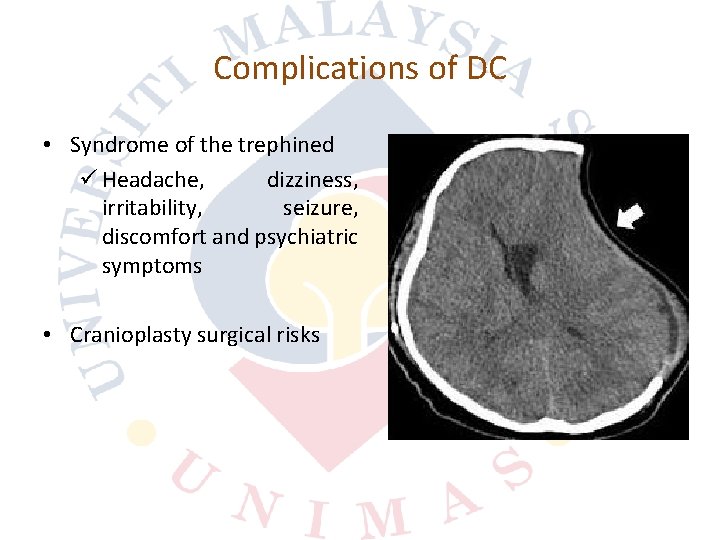
Complications of DC • Postoperative haematoma expansion • Infection • CSF absorption disorder (subdural hygroma and hydrocephalus)
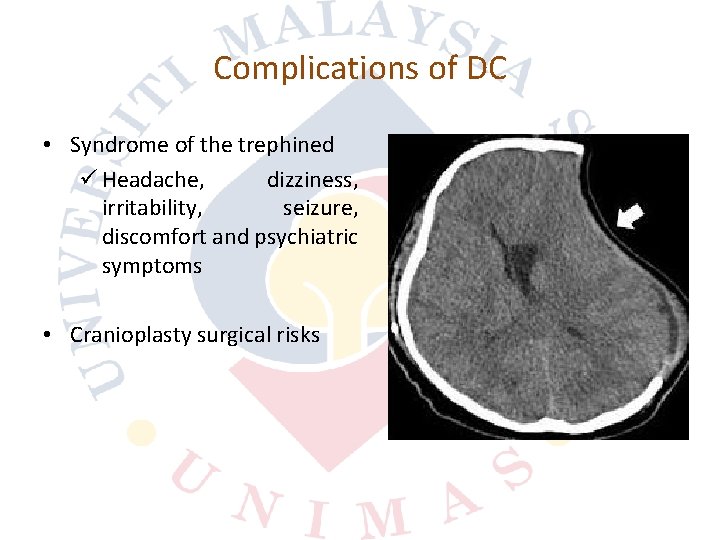
Complications of DC • Syndrome of the trephined ü Headache, dizziness, irritability, seizure, discomfort and psychiatric symptoms • Cranioplasty surgical risks
Raised ICP • Haematoma ü EDH, SDH, contusion, intraparenchymal haematoma • Brain swelling ü Cytotoxic oedema (influx of calcium and mitochondrial failure) ü Vasogenic oedema (derangement of blood brain barrier) ü Osmotic load of cellular breakdown products
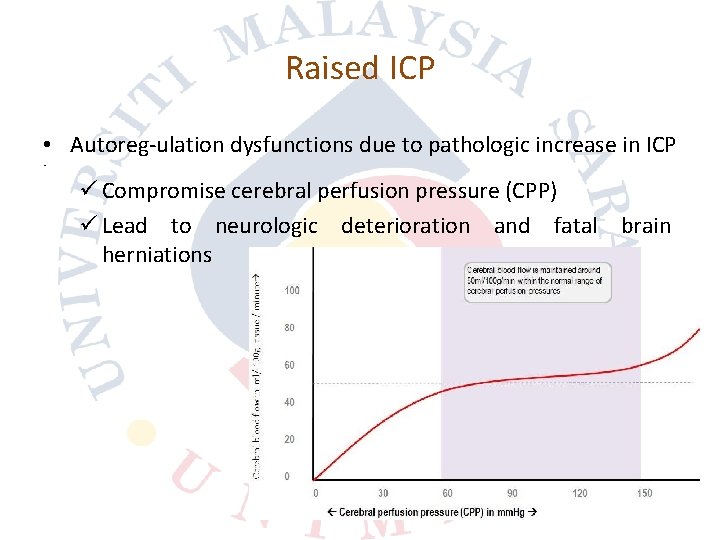
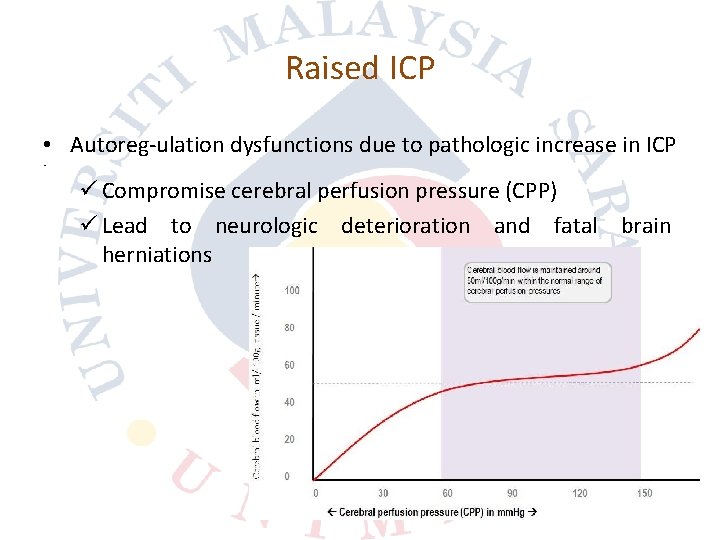
Raised ICP • Autoreg ulation dysfunctions due to pathologic increase in ICP • ü Compromise cerebral perfusion pressure (CPP) ü Lead to neurologic deterioration and fatal brain herniations
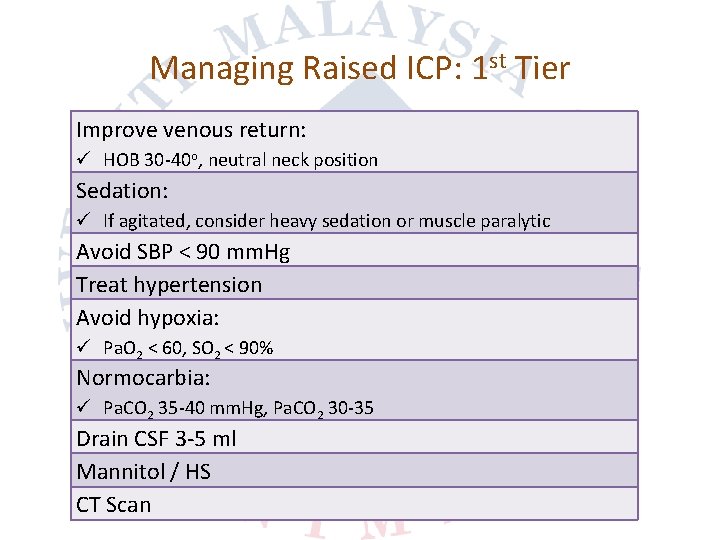
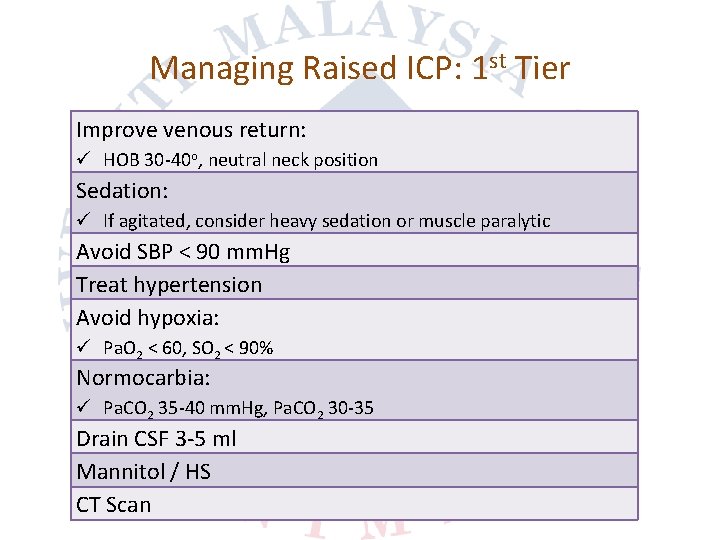
Managing Raised ICP: 1 st Tier Improve venous return: ü HOB 30 40 o, neutral neck position Sedation: ü If agitated, consider heavy sedation or muscle paralytic Avoid SBP < 90 mm. Hg Treat hypertension Avoid hypoxia: ü Pa. O 2 < 60, SO 2 < 90% Normocarbia: ü Pa. CO 2 35 40 mm. Hg, Pa. CO 2 30 35 Drain CSF 3 5 ml Mannitol / HS CT Scan
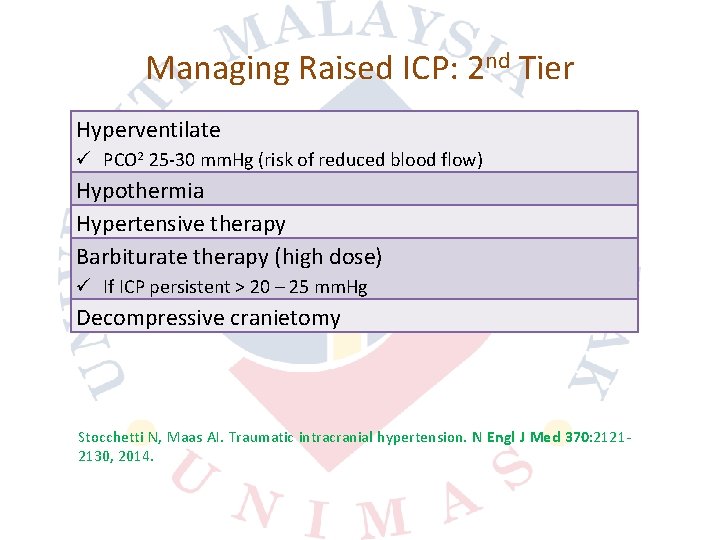
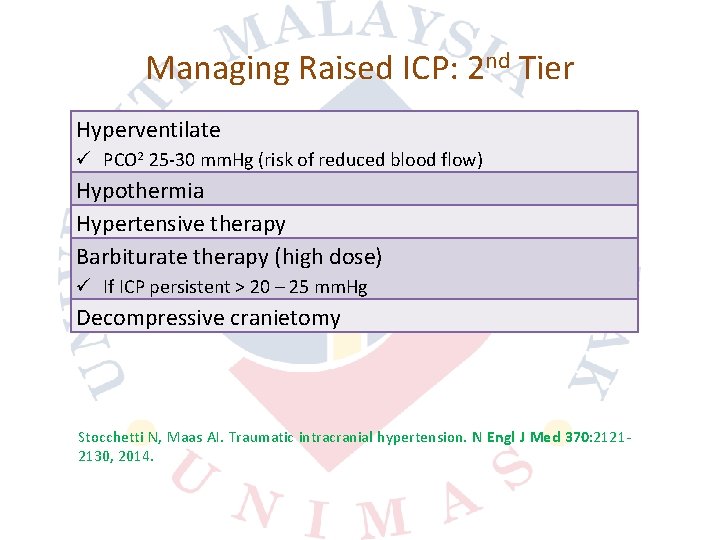
Managing Raised ICP: 2 nd Tier Hyperventilate ü PCO 2 25 30 mm. Hg (risk of reduced blood flow) Hypothermia Hypertensive therapy Barbiturate therapy (high dose) ü If ICP persistent > 20 – 25 mm. Hg Decompressive cranietomy Stocchetti N, Maas AI. Traumatic intracranial hypertension. N Engl J Med 370: 2121 2130, 2014.
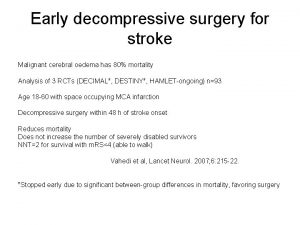
Main RCT in TBI • DECRA trial ü Examined the role of neuroprotective, secondary, and bifrontal DC for moderate intracranial hypertension • RESCUEicp trial ü Examined the role of last tier secondary DC for severe and refractory intracranial hypertension
DECRA Trial • Published in 2011 (2002 to 2010) ü Australia, New Zealand, and Saudi Arabia DECRA Trial
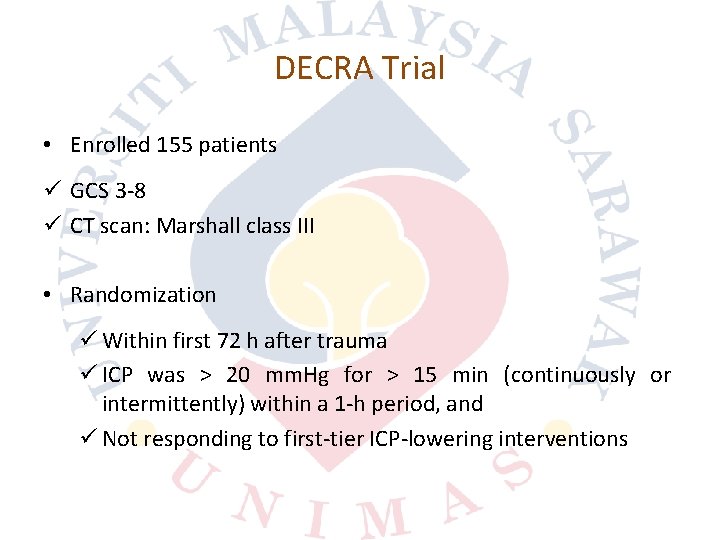
DECRA Trial • Enrolled 155 patients ü GCS 3 8 ü CT scan: Marshall class III • Randomization ü Within first 72 h after trauma ü ICP was > 20 mm. Hg for > 15 min (continuously or intermittently) within a 1 h period, and ü Not responding to first tier ICP lowering interventions
DECRA Trial • Randomisation ü Bifrontal DC (n = 72) ü Continuing medical care (n = 82) • Primary endpoint ü Extended Glasgow Outcome Scale (GOSE) score at 6 months
DECRA Trial • Mortality ü 19% vs 18% (DC vs MC) • Unfavourable GOSE ü 70% vs 51%; p = 0. 02 (DC vs MC) • Possible explanation ü Craniectomy allowed expansion of the swollen brain outside the skull and caused axonal stretch
DECRA Trial • ICP readings (DC vs MC) ü 14 ± 6. 8 vs 19 ± 8. 9 (p<0. 001) • Days of medical ventilation (DC vs MC) ü 11 vs 15 (median, p<0. 001) • Days of ICU stay (DC vs MC) ü 13 vs 18 (median, p<0. 001)

DECRA Trial • Study conclusion: ü In adults with severe diffuse traumatic brain injury and refractory intracranial hypertension, early bifrontotemporoparietal decompressive craniectomy decreased intracranial pressure and the length of stay in the ICU but was associated with more unfavorable outcomes
DECRA Trial: Limitations • Patients with non reactive pupils ü 27% in DC group ü 12% in SC group • Bifrontal DC without falx sectioning • Definition of refrac tory ICP ü Lower raised in ICP ü Short in duration ü Could not be sure it really reflect intractable increased ICP
RESCUEicp Trial • Published in 2016 (2004 to 2014) ü In 20 countries ü < 10% of the RESCUEicp patient population was enrolled in LMICs (36/408 patients from 6 countries) ü USM (3) ü UMMC (3)
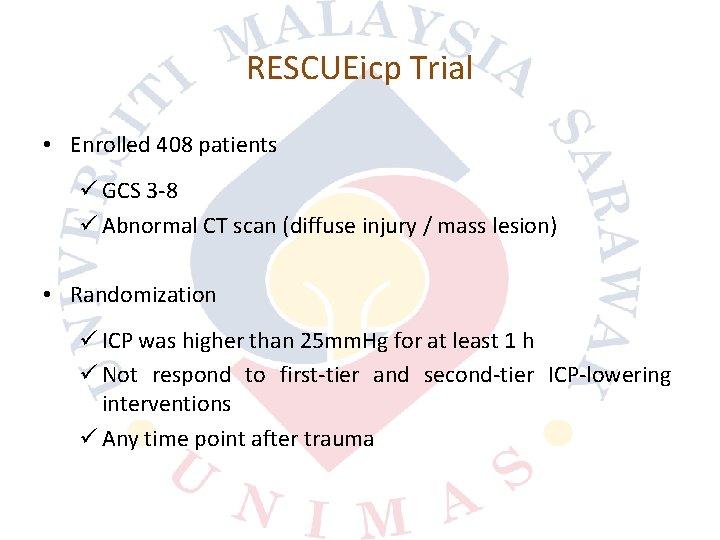
RESCUEicp Trial • Enrolled 408 patients ü GCS 3 8 ü Abnormal CT scan (diffuse injury / mass lesion) • Randomization ü ICP was higher than 25 mm. Hg for at least 1 h ü Not respond to first tier and second tier ICP lowering interventions ü Any time point after trauma
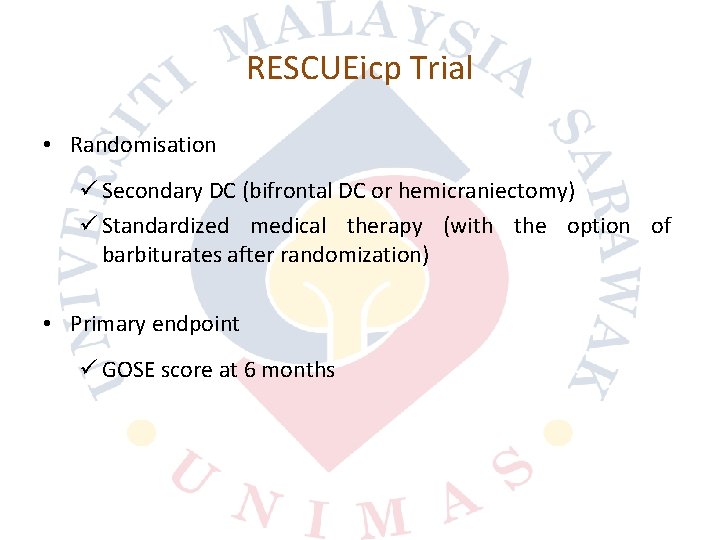
RESCUEicp Trial • Randomisation ü Secondary DC (bifrontal DC or hemicraniectomy) ü Standardized medical therapy (with the option of barbiturates after randomization) • Primary endpoint ü GOSE score at 6 months
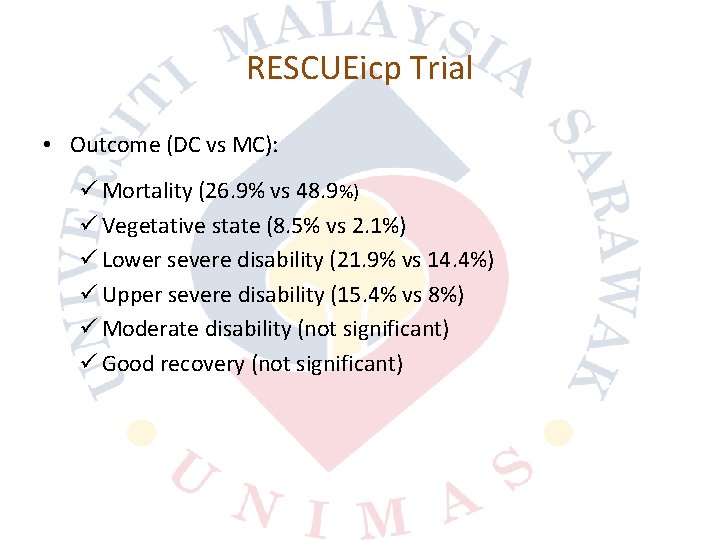
RESCUEicp Trial • Outcome (DC vs MC): ü Mortality (26. 9% vs 48. 9%) ü Vegetative state (8. 5% vs 2. 1%) ü Lower severe disability (21. 9% vs 14. 4%) ü Upper severe disability (15. 4% vs 8%) ü Moderate disability (not significant) ü Good recovery (not significant)

RESCUEicp Trial • Study conclusion: ü Secondary DC can be a life saving procedure in severe TBI patients with refractory posttraumatic intracranial hypertension ü However, increases the number of patients surviving in a vegeta tive state
RESCUE ASDH • Lacking of consensus on the indications for primary DC in ASDH • Primary DC in ASDH cases üUK/Irishneurosurgeons (29/138; 21%) üOther European countries neurosurgeons (48/110; 44%) Kolias AG, Belli A, Li LM, Timofeev I, Corteen EA, Santarius T, et al. Primary decompressive craniectomy for acute subdural haematomas: results of an international survey. Acta Neurochir. 2012; 154(9): 1563– 1565.
Practical Issues in DC • CPG in Malaysia • International Guidelines • Evidence based studies • Neuro monitoring facilities • Safe surgery • Expectation from family members
Conclusions • Role of DC in head injury ü Clear indications ü Good clinical judgment ü Clear information given to family members
 Vertebroplasty icd 10 code
Vertebroplasty icd 10 code Craniectomie décompressive avc
Craniectomie décompressive avc Example of intentional injury
Example of intentional injury Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Copyright
Copyright Patrick lynch head injury colorado
Patrick lynch head injury colorado Head injury assessment
Head injury assessment Nursing care plan for head injury slideshare
Nursing care plan for head injury slideshare Cholesteatoma
Cholesteatoma The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. Pro minent
Pro minent What is a tonic syllable
What is a tonic syllable Tagi html
Tagi html Quad innervation
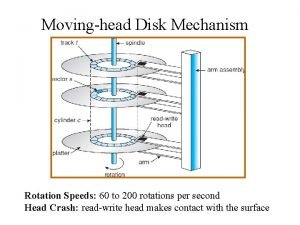
Quad innervation The head of a moving head disk
The head of a moving head disk The tone unit
The tone unit Dividing head formula
Dividing head formula Head body parts
Head body parts Moving head disk mechanism
Moving head disk mechanism Head nurse role
Head nurse role Statuses and their related roles determine the structure
Statuses and their related roles determine the structure Web role in azure
Web role in azure Krappmann schaubild
Krappmann schaubild Kepentingan pembinaan negara bangsa
Kepentingan pembinaan negara bangsa E khutbah terengganu
E khutbah terengganu Khutbah multimedia terengganu
Khutbah multimedia terengganu Enakmen jenayah syariah terengganu
Enakmen jenayah syariah terengganu Suruhanjaya perkhidmatan negeri terengganu
Suruhanjaya perkhidmatan negeri terengganu Hukum menyusahkan jiran
Hukum menyusahkan jiran Doa antara dua khutbah terengganu
Doa antara dua khutbah terengganu Khutbah multimedia terengganu
Khutbah multimedia terengganu Mukim di hulu terengganu
Mukim di hulu terengganu E khutbah terengganu
E khutbah terengganu Itik gembo gembo maksud
Itik gembo gembo maksud Sejarah kesultanan perak tingkatan 2
Sejarah kesultanan perak tingkatan 2