CSUALS An Innovative Approach to Cardiac Surgery ALS


![Epinephrine: AHA Circulation 2015; 132[suppl 2]: S 444–S 464. www. csu-als. org ©�CSU-ALS NA™�& Epinephrine: AHA Circulation 2015; 132[suppl 2]: S 444–S 464. www. csu-als. org ©�CSU-ALS NA™�&](https://slidetodoc.com/presentation_image_h/955912fe6f4ecc2594a24819d250c76e/image-45.jpg)



- Slides: 57
CSU-ALS: An Innovative Approach to Cardiac Surgery ALS David E. Lizotte, Jr. MPAS, PA-C, FAPACVS
Disclosures: President, CSU-ALS North America www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
The CSU-ALS Provider Course: Evidence Review Objectives www. csu-als. org 1. Discuss important literature findings regarding resuscitation of arrest after cardiac surgery 2. Contrast key differences between Advanced Cardiac Life Support (ACLS) protocols and the protocol endorsed by The Society of Thoracic Surgeons (STS) and The European Association of Cardiothoracic Surgery (EACTS) 3. Identify key roles and responsibilities in the STS/EACTS protocol for resuscitation of postoperative cardiac arrest ©�CSU-ALS NA™�& CALSs UK™�
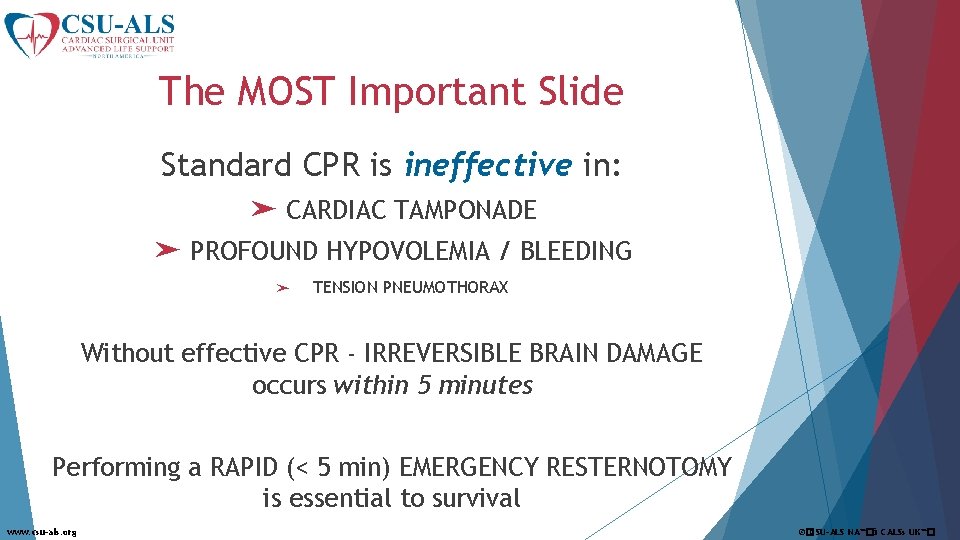
The MOST Important Slide Standard CPR is ineffective in: ➤ CARDIAC TAMPONADE ➤ PROFOUND HYPOVOLEMIA / BLEEDING ➤ TENSION PNEUMOTHORAX Without effective CPR - IRREVERSIBLE BRAIN DAMAGE occurs within 5 minutes Performing a RAPID (< 5 min) EMERGENCY RESTERNOTOMY is essential to survival www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Cardiac arrest after heart surgery is different! ➤ 326, 200 out of hospital (OHCA) cardiac arrests/year Survival to discharge in 10. 6% § Good neurologic recovery in 8. 3% ➤ 209, 000 in hospital (IHCA) cardiac arrests/year § Survival to discharge in 24% ➤ 2500 -5000 post-cardiac surgery arrests/year § High potential for reversible causes and recovery § Wide variation in survival; 40 -79% reported § Best survival in those with shockable rhythms § AHA 2015 Heart & Stroke Statistics www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Why is ACLS not recommended after heart surgery? www. csu-als. org ACLS is designed for out of hospital cardiac arrest STS Protocol is designed for CVICU ©�CSU-ALS NA™�& CALSs UK™�
Why is Cardiac Arrest After Heart Surgery Different? ➤ Patients are intubated with multi-modal monitoring ➤ Arrests are witnessed/monitored ➤ Multidisciplinary ➤ Chest team members are available compressions carry increased risk ➤ Emergency resternotomy should proceed rapidly; within 5 minutes if unstable after airway/rhythm management www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
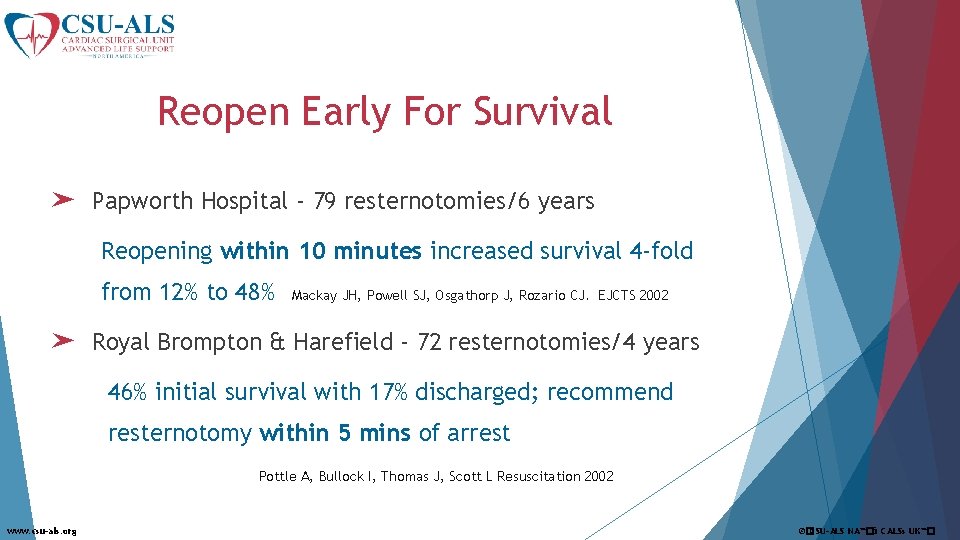
Reopen Early For Survival ➤ Papworth Hospital - 79 resternotomies/6 years Reopening within 10 minutes increased survival 4 -fold from 12% to 48% Mackay JH, Powell SJ, Osgathorp J, Rozario CJ. EJCTS 2002 ➤ Royal Brompton & Harefield - 72 resternotomies/4 years 46% initial survival with 17% discharged; recommend resternotomy within 5 mins of arrest Pottle A, Bullock I, Thomas J, Scott L Resuscitation 2002 www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
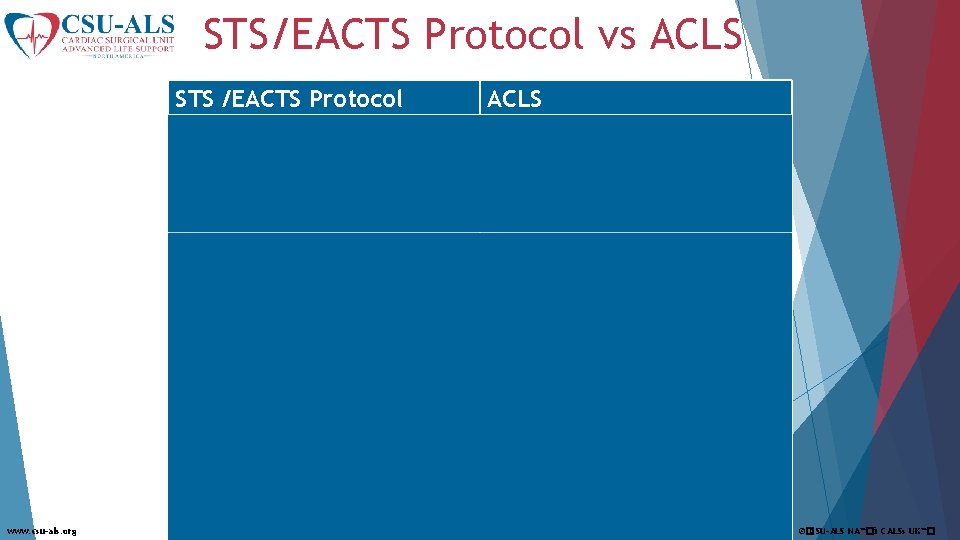
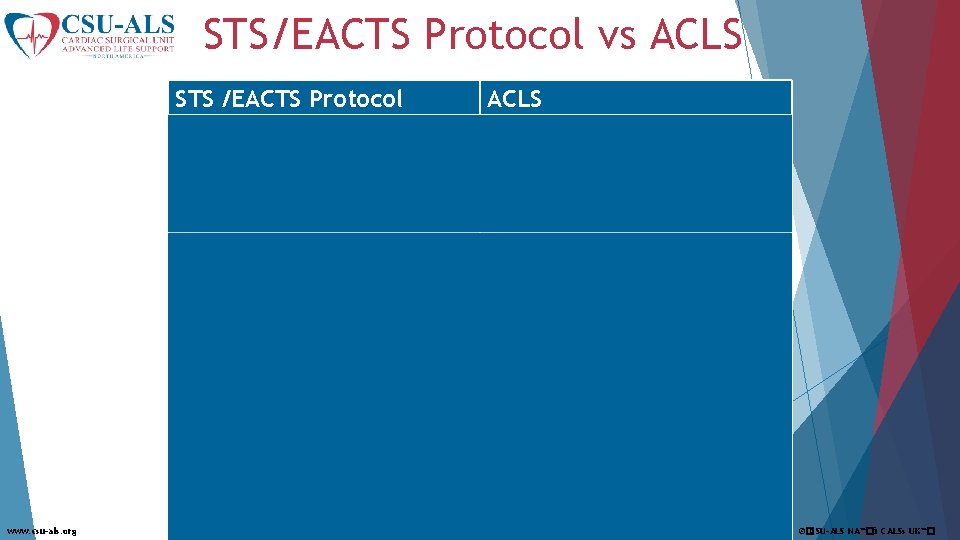
STS/EACTS Protocol vs ACLS STS /EACTS Protocol ACLS For VF/p. VT Defibrillation takes priority; may CPR should be performed defer CPR for up to 1 minute immediately on all patients 3 successive shocks before CPR 1 shock CPR For Asystole Dual chamber pacing, max output CPR and EPI For VF/p. VT, Asystole, Pulseless Electrical Activity No epi unless by senior clinician; Epinephrine 1000 mcg every 3 -5 If used pre-arrest reduce dose minutes www. csu-als. org Use 6 key roles in arrest; 2 sterile providers gown & glove Similar roles and responsibilities Rapid resternotomy (<5 min) if no response to pacing or defibrillation N/A ©�CSU-ALS NA™�& CALSs UK™�
The STS/EACTS Resuscitation Protocol History 2003: Two UK surgeons initiate project: J Dunning, A Levine 2004: First UK course in Manchester 2009: EACTS Guidelines for Resuscitation After Cardiac Surgery Dunning J, et al. Eur J Cardiothorac Surg 2009; 36: 3 -28 2009: First US course in San Francisco 2010: International Liaison Committee on Resuscitation & European Resuscitation Council guidelines Nolan JP, et al. Resuscitation 2010; 81: 1219 -1276 2015 CSU-ALS North America Developed for National Standardization and Organization of Protocol 2015: STS Resuscitation Task Force initiated 2017: Publication of STS Consensus Statement www. csu-als. org Dunning J, et al. Ann Thorac Surg, Feb 2017 ©�CSU-ALS NA™�& CALSs UK™�
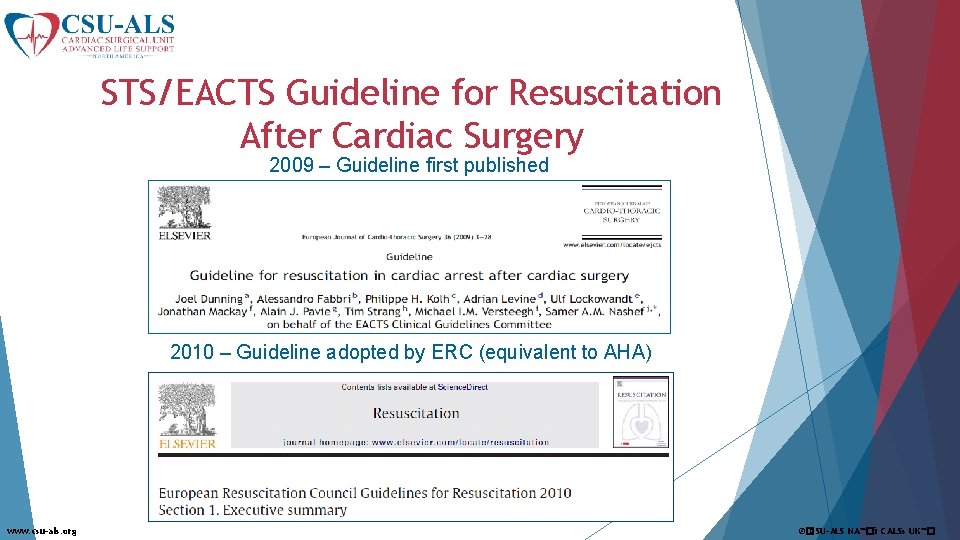
STS/EACTS Guideline for Resuscitation After Cardiac Surgery 2009 – Guideline first published 2010 – Guideline adopted by ERC (equivalent to AHA) www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
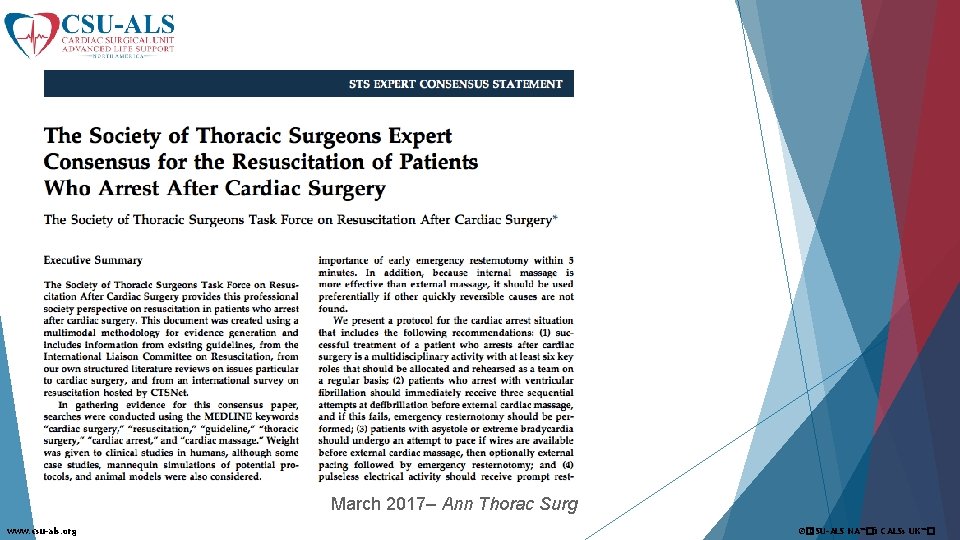
March 2017– Ann Thorac Surg www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
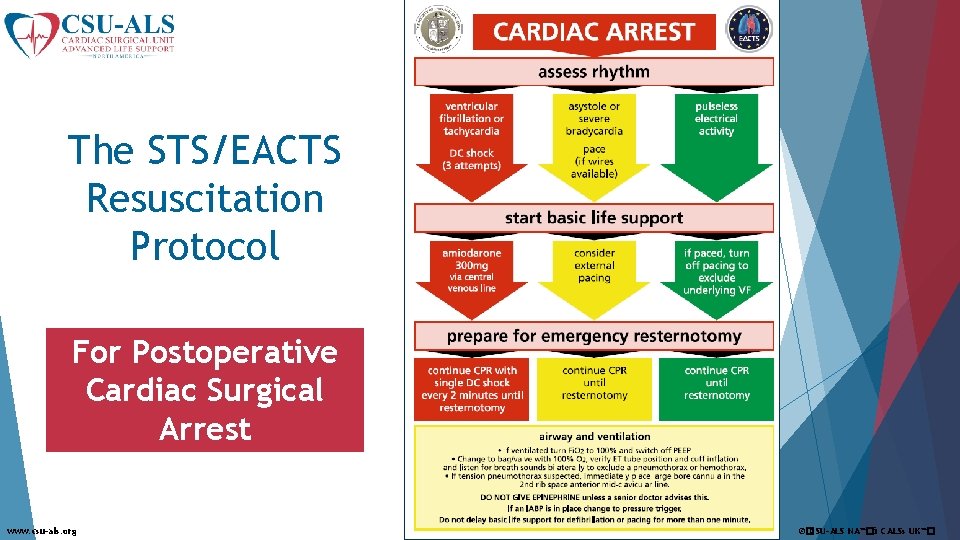
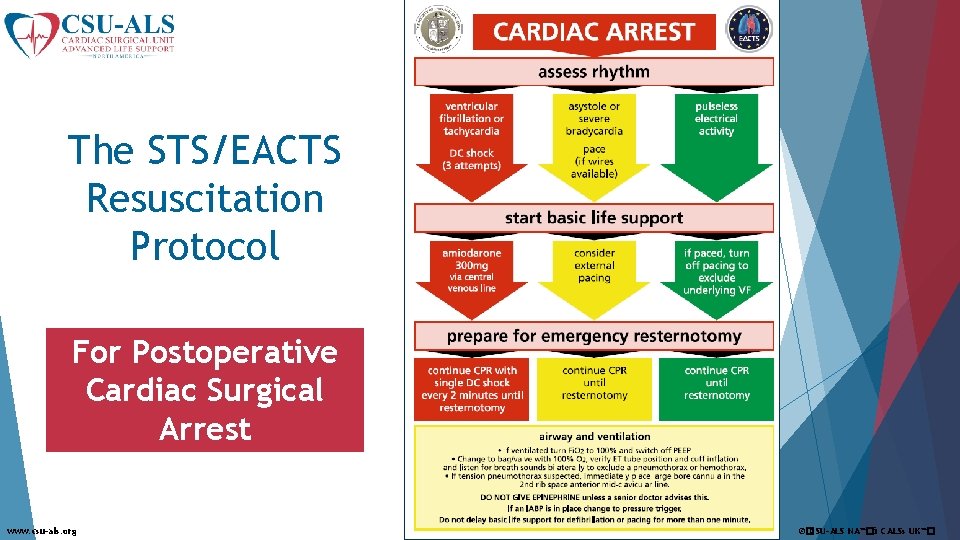
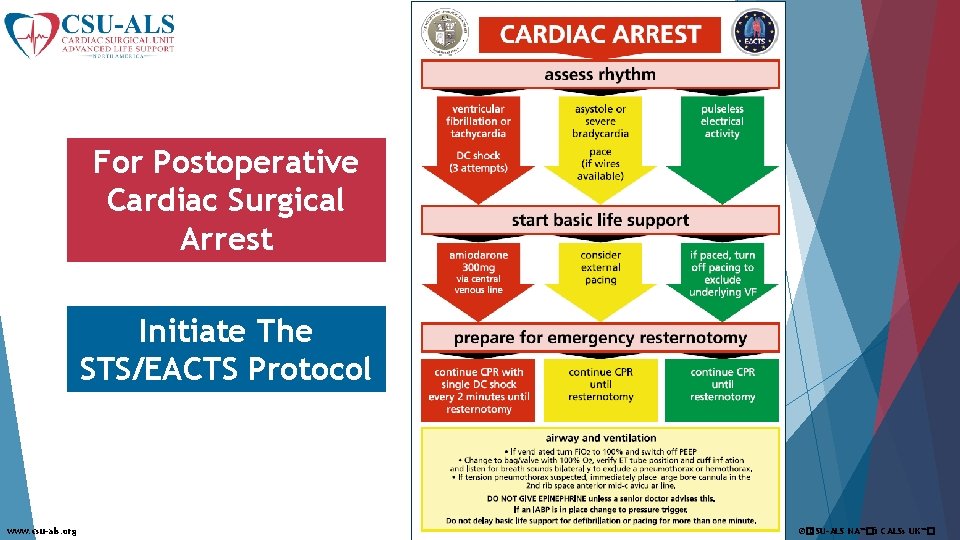
The STS/EACTS Resuscitation Protocol For Postoperative Cardiac Surgical Arrest www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
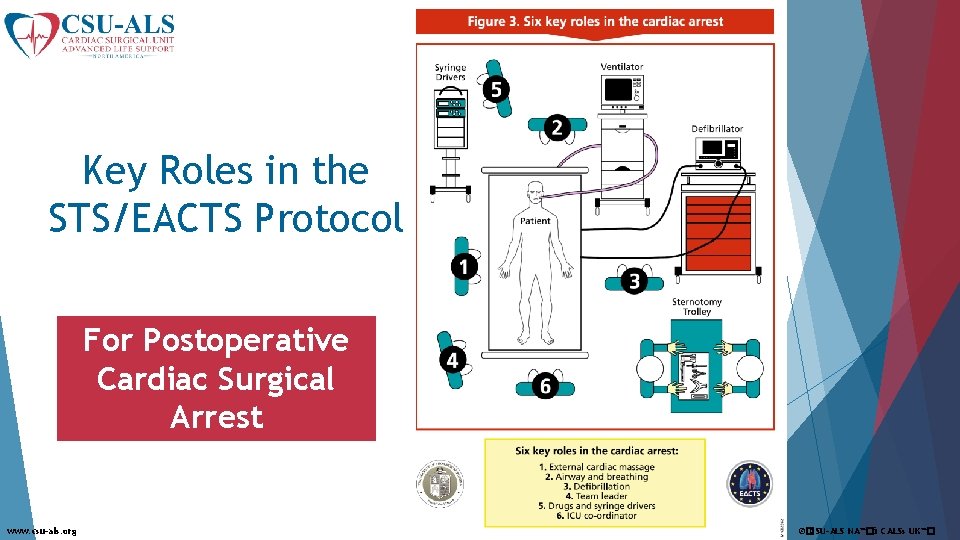
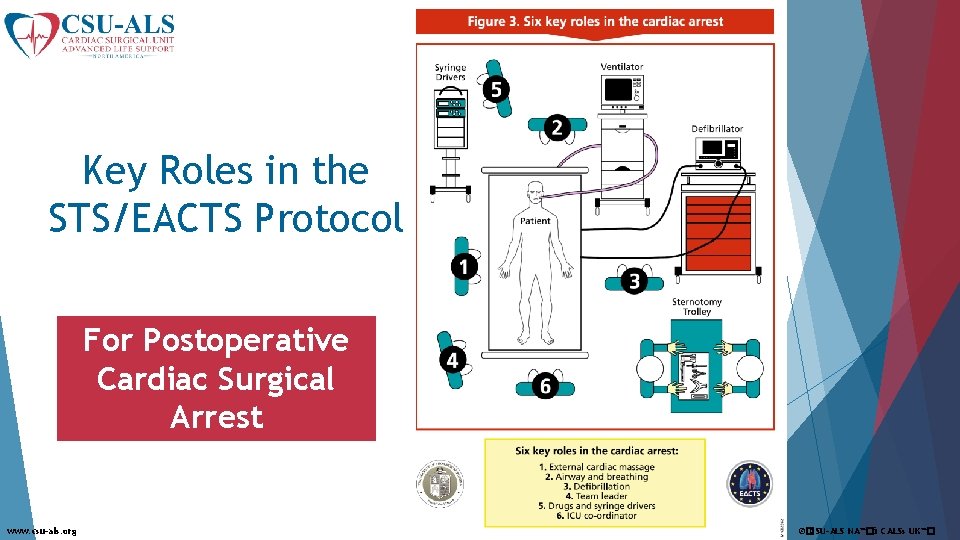
Key Roles in the STS/EACTS Protocol For Postoperative Cardiac Surgical Arrest www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
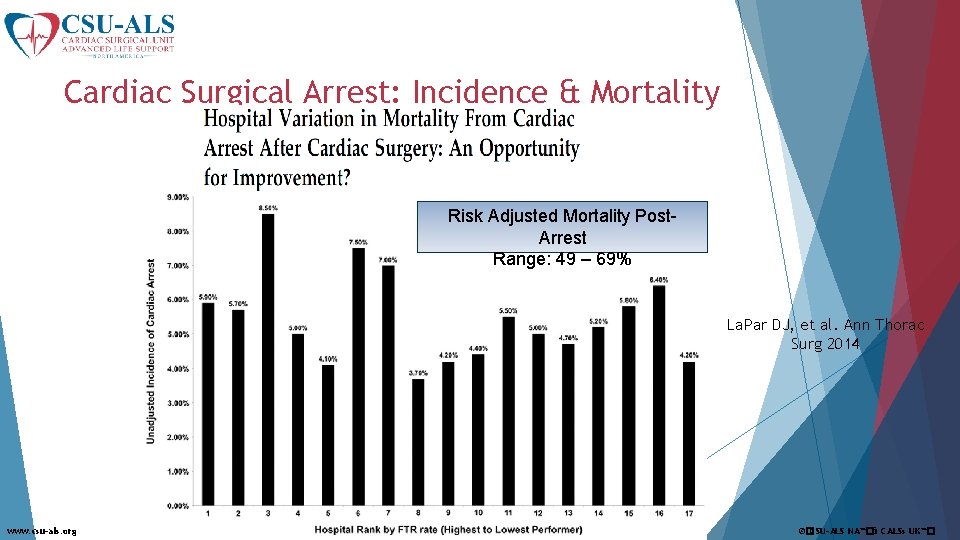
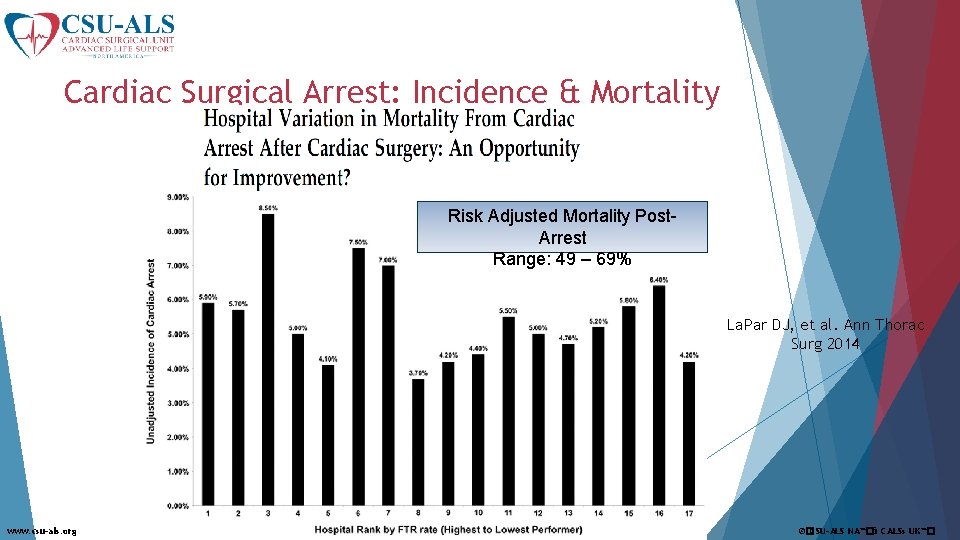
Cardiac Surgical Arrest: Incidence & Mortality Risk Adjusted Mortality Post. Arrest Range: 49 – 69% La. Par DJ, et al. Ann Thorac Surg 2014 www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
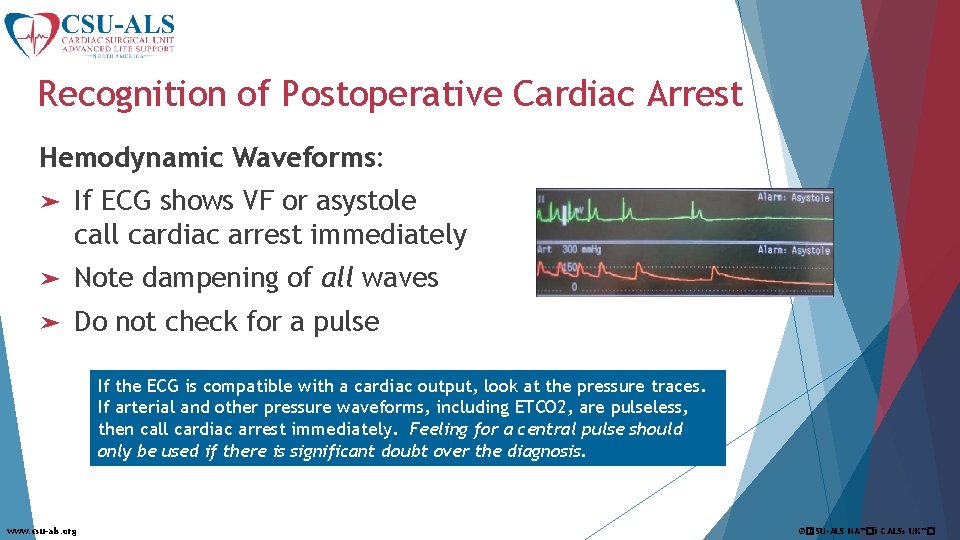
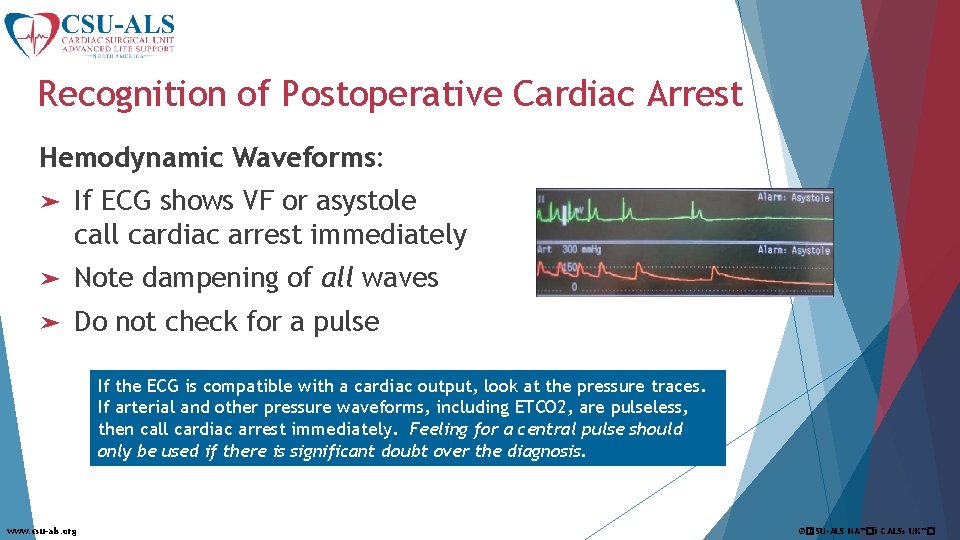
Recognition of Postoperative Cardiac Arrest Hemodynamic Waveforms: ➤ If ECG shows VF or asystole call cardiac arrest immediately ➤ Note dampening of all waves ➤ Do not check for a pulse If the ECG is compatible with a cardiac output, look at the pressure traces. If arterial and other pressure waveforms, including ETCO 2, are pulseless, then call cardiac arrest immediately. Feeling for a central pulse should only be used if there is significant doubt over the diagnosis. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
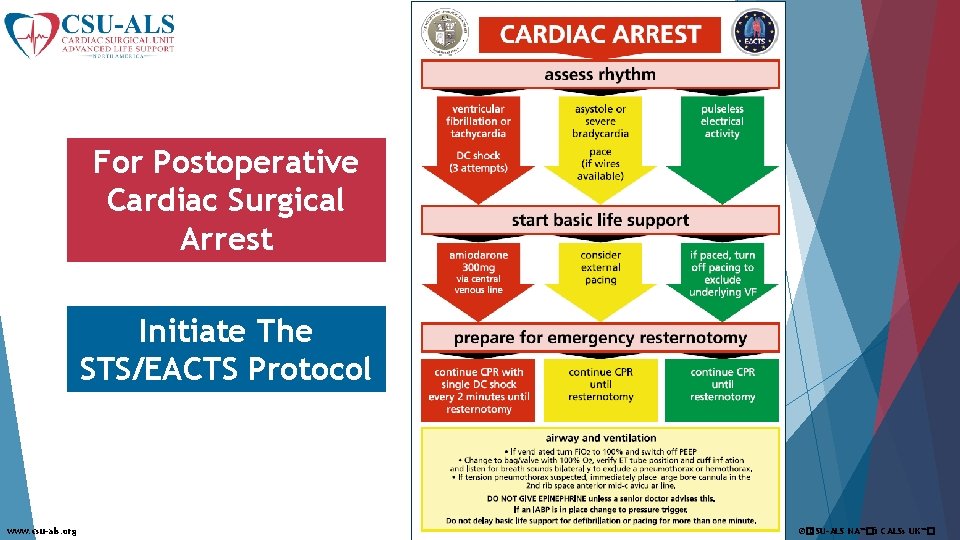
For Postoperative Cardiac Surgical Arrest Initiate The STS/EACTS Protocol www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
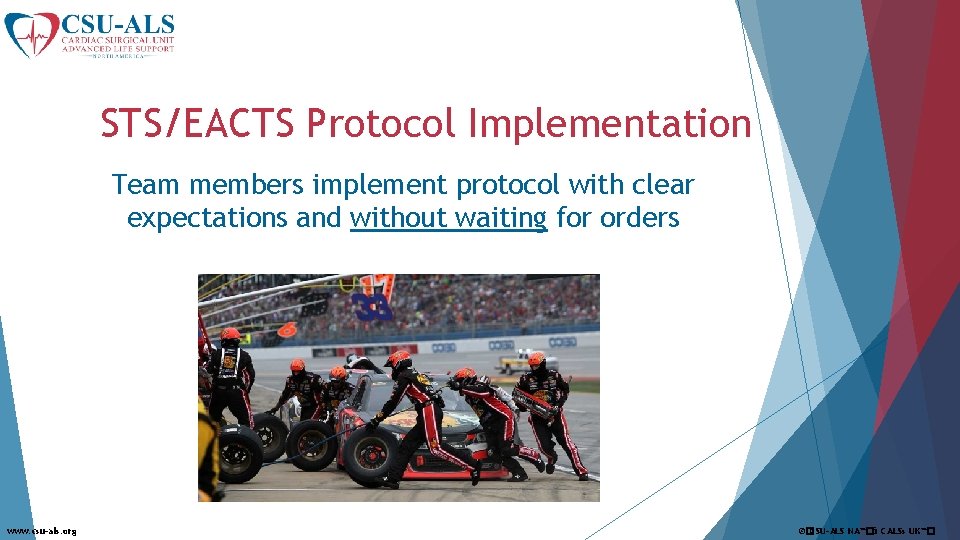
STS/EACTS Protocol Implementation Team members implement protocol with clear expectations and without waiting for orders www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
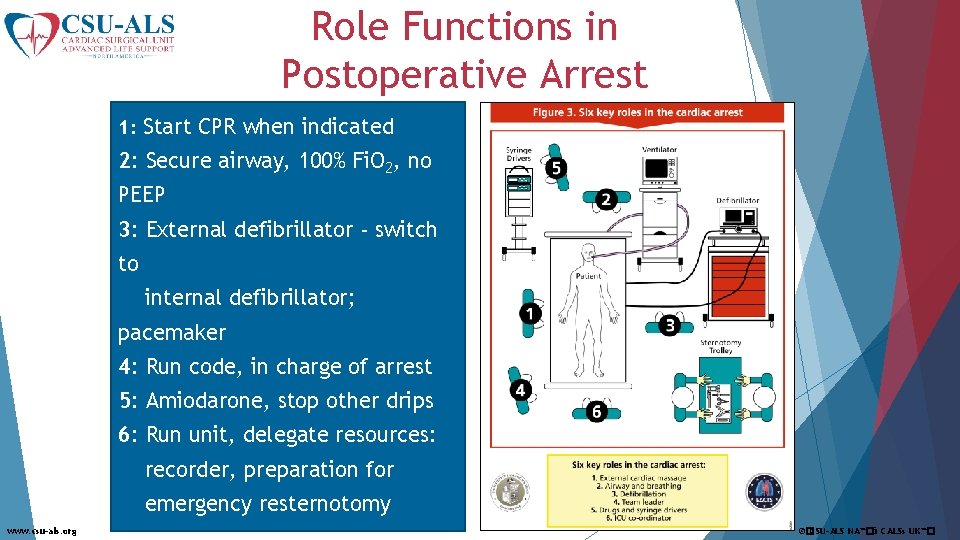
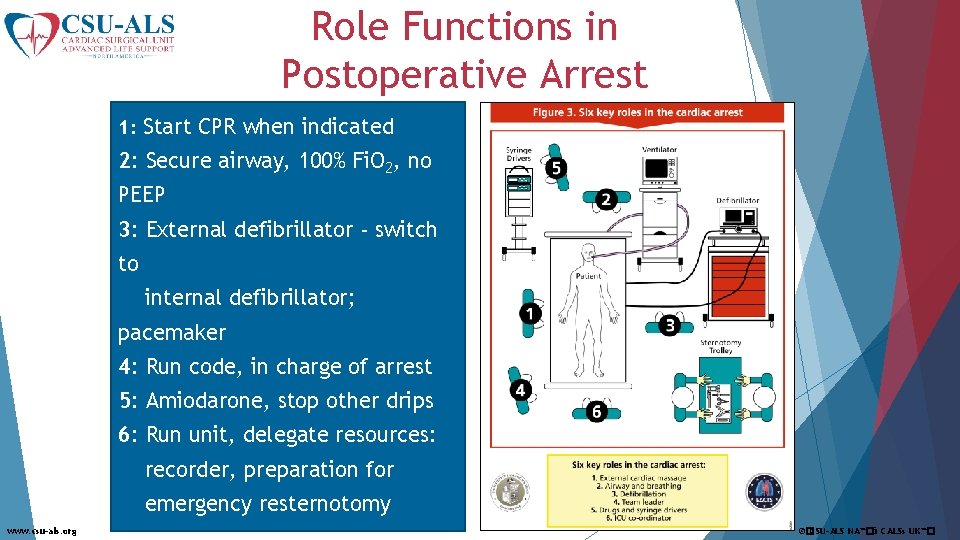
Role Functions in Postoperative Arrest 1: Start CPR when indicated 2: Secure airway, 100% Fi. O 2, no PEEP 3: External defibrillator - switch to internal defibrillator; pacemaker 4: Run code, in charge of arrest 5: Amiodarone, stop other drips 6: Run unit, delegate resources: recorder, preparation for emergency resternotomy www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
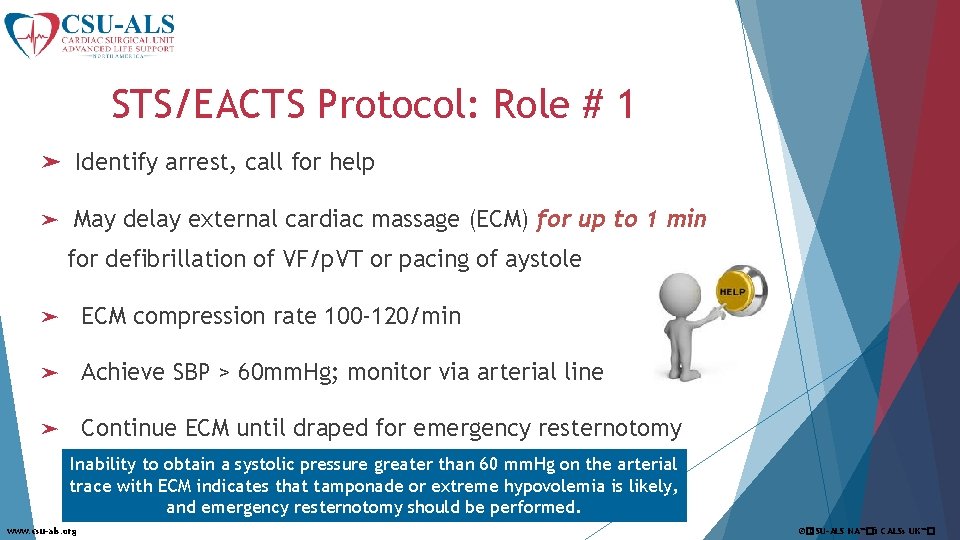
STS/EACTS Protocol: Role # 1 ➤ Identify arrest, call for help ➤ May delay external cardiac massage (ECM) for up to 1 min for defibrillation of VF/p. VT or pacing of aystole ➤ ECM compression rate 100 -120/min ➤ Achieve SBP > 60 mm. Hg; monitor via arterial line ➤ Continue ECM until draped for emergency resternotomy Inability to obtain a systolic pressure greater than 60 mm. Hg on the arterial trace with ECM indicates that tamponade or extreme hypovolemia is likely, and emergency resternotomy should be performed. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
STS/EACTS Protocol: Role # 2 - Airway Increase Fi. O 2 to 100% Disconnect from ventilator & use bag/valve § Look/listen for equal movement § Confirm presence of ETCO 2 § Treat tension pneumo with lg-bore needle, 2 nd anterior intercostal space. ➤ Once adequate airway/breathing confirmed, reconnect to ventilator, remove PEEP ➤ ➤ If inflating the lungs with the bag-valve device is not possible, and a suction catheter will not pass down the ETT, then tube occlusion or mal-positioning should be suspected. The ETT should be immediately removed and a bag-valve-mask with airway adjuncts used. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
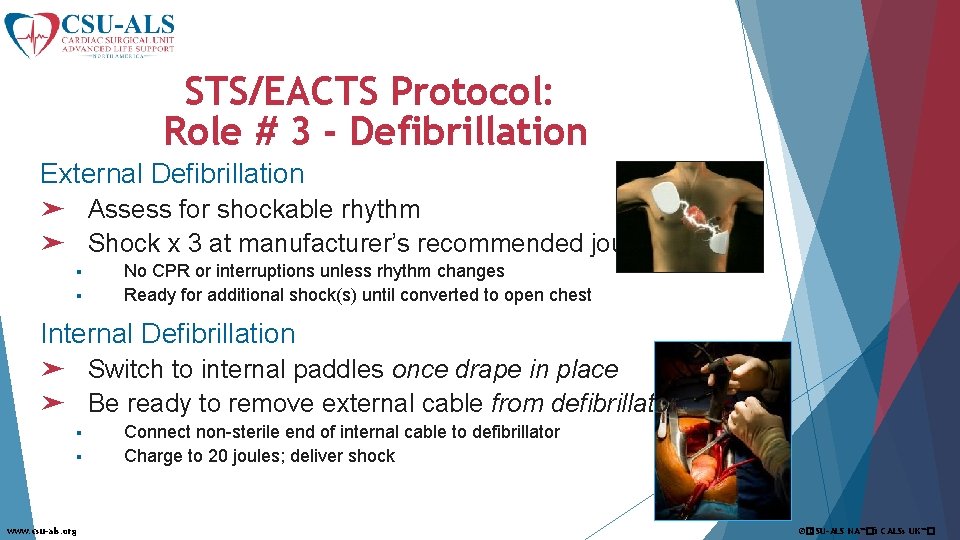
STS/EACTS Protocol: Role # 3 - Defibrillation External Defibrillation ➤ Assess for shockable rhythm ➤ Shock x 3 at manufacturer’s recommended joules § § No CPR or interruptions unless rhythm changes Ready for additional shock(s) until converted to open chest Internal Defibrillation ➤ Switch to internal paddles once drape in place ➤ Be ready to remove external cable from defibrillator § § www. csu-als. org Connect non-sterile end of internal cable to defibrillator Charge to 20 joules; deliver shock ©�CSU-ALS NA™�& CALSs UK™�
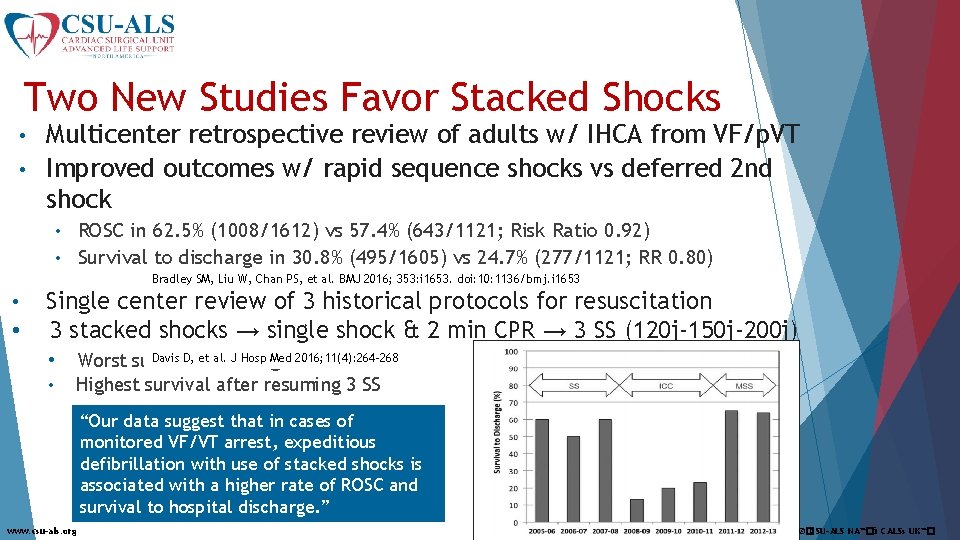
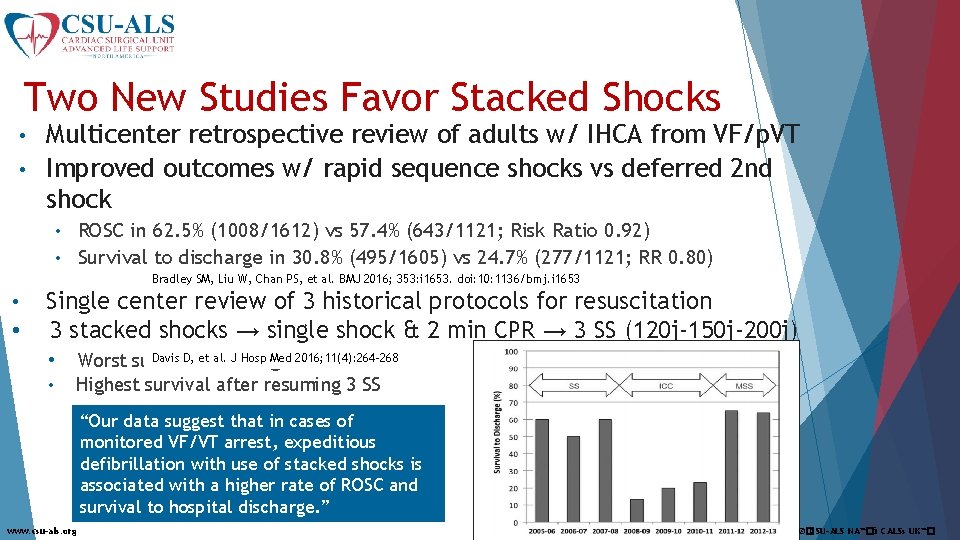
Two New Studies Favor Stacked Shocks Multicenter retrospective review of adults w/ IHCA from VF/p. VT • Improved outcomes w/ rapid sequence shocks vs deferred 2 nd shock • ROSC in 62. 5% (1008/1612) vs 57. 4% (643/1121; Risk Ratio 0. 92) • Survival to discharge in 30. 8% (495/1605) vs 24. 7% (277/1121; RR 0. 80) • Bradley SM, Liu W, Chan PS, et al. BMJ 2016; 353: i 1653. doi: 10: 1136/bmj. i 1653 • • Single center review of 3 historical protocols for resuscitation 3 stacked shocks → single shock & 2 min CPR → 3 SS (120 j-150 j-200 j) • • Davis D, et al. J Hosp Med 2016; 11(4): 264 -268 Worst survival with single shock Highest survival after resuming 3 SS “Our data suggest that in cases of monitored VF/VT arrest, expeditious defibrillation with use of stacked shocks is associated with a higher rate of ROSC and survival to hospital discharge. ” www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
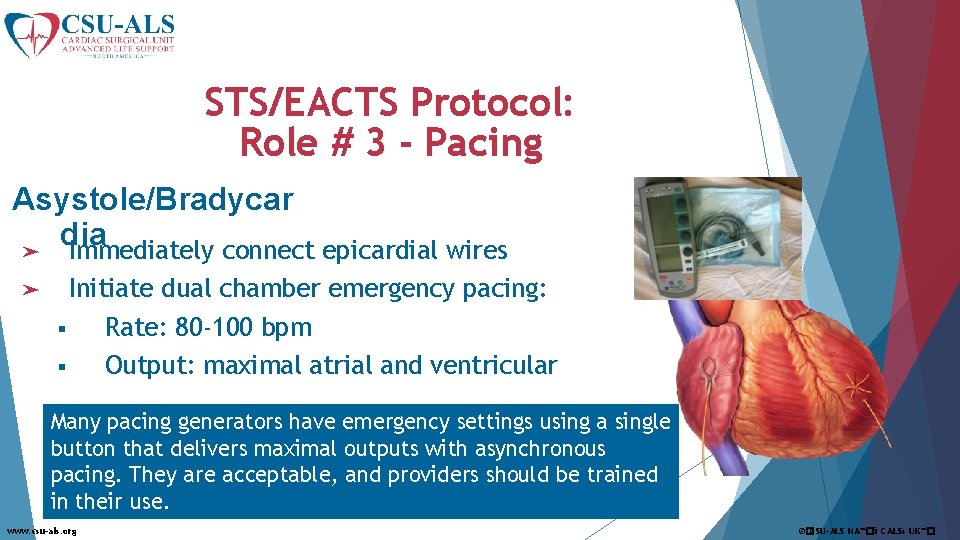
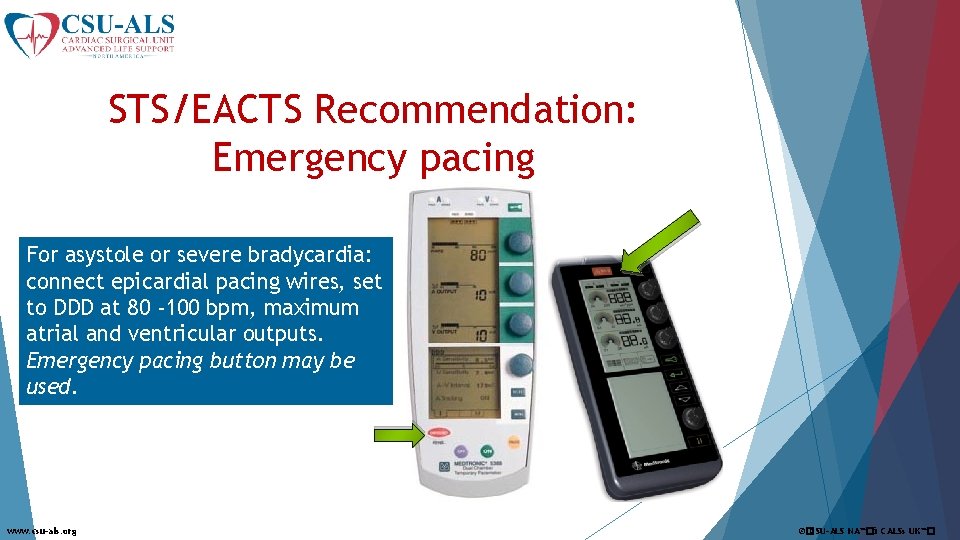
STS/EACTS Protocol: Role # 3 - Pacing Asystole/Bradycar dia ➤ Immediately connect epicardial wires ➤ Initiate dual chamber emergency pacing: § Rate: 80 -100 bpm § Output: maximal atrial and ventricular Many pacing generators have emergency settings using a single button that delivers maximal outputs with asynchronous pacing. They are acceptable, and providers should be trained in their use. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
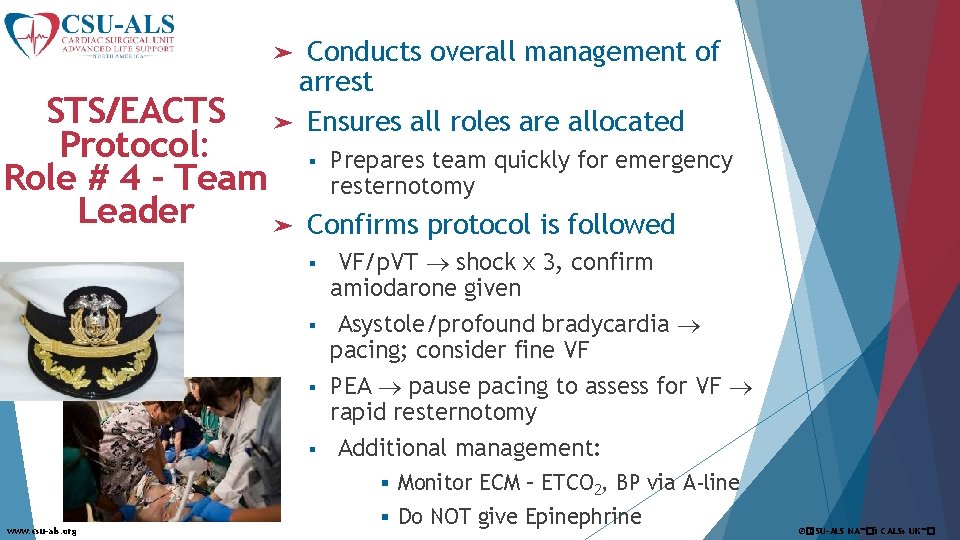
Conducts overall management of arrest ➤ Ensures all roles are allocated ➤ STS/EACTS Protocol: Role # 4 - Team Leader ➤ § Prepares team quickly for emergency resternotomy Confirms protocol is followed § § VF/p. VT shock x 3, confirm amiodarone given Asystole/profound bradycardia pacing; consider fine VF PEA pause pacing to assess for VF rapid resternotomy Additional management: § Monitor ECM – ETCO 2, BP via A-line www. csu-als. org § Do NOT give Epinephrine ©�CSU-ALS NA™�& CALSs UK™�
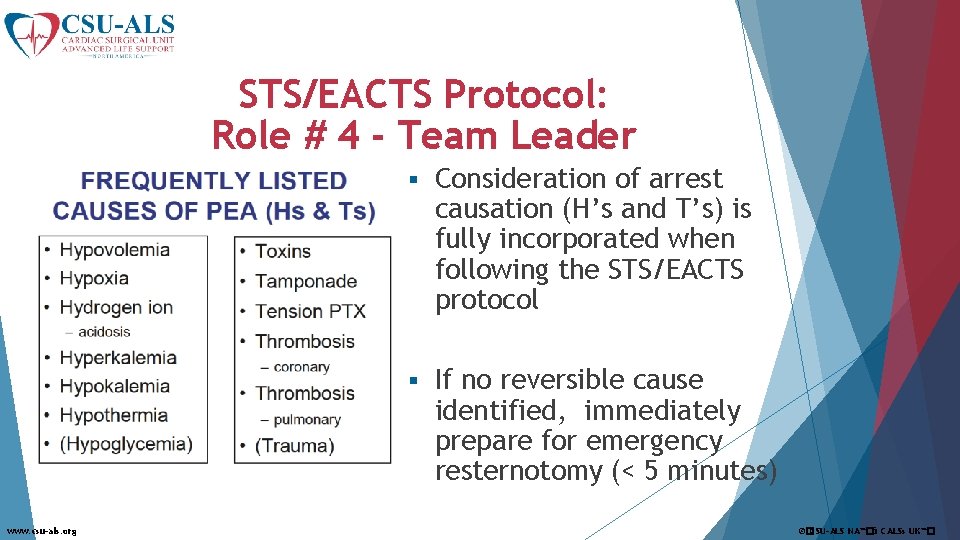
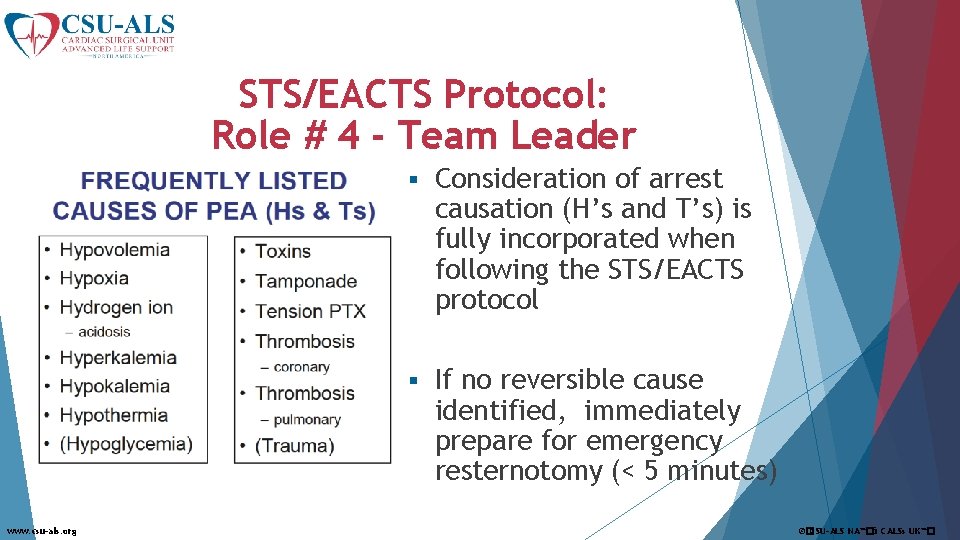
STS/EACTS Protocol: Role # 4 - Team Leader www. csu-als. org § Consideration of arrest causation (H’s and T’s) is fully incorporated when following the STS/EACTS protocol § If no reversible cause identified, immediately prepare for emergency resternotomy (< 5 minutes) ©�CSU-ALS NA™�& CALSs UK™�
STS/EACTS Protocol: Role # 5 - Medications ➤ For established arrest after initial resuscitation fails: ➤ Stop all infusions (potential toxins) ➤ Manage medications § Amiodarone for shockable rhythm § Do NOT give epinephrine www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
STS/EACTS Protocol: Role # 6 – ICU Coordinator ➤ Senior person to coordinate activity peripheral to bedside ➤ Prepares for resternotomy as soon as arrest is called § § § Calls for expert assistance Continually reports to team leader Directs available personnel § § § www. csu-als. org 2 -3 persons gowned/gloved for resternotomy One person assigned to hand off sterile supplies Equipment: carts, lighting, suction, POC lab sampling Transport: blood, labs, OR equipment Environment – remove clutter, control personnel/traffic ©�CSU-ALS NA™�& CALSs UK™�
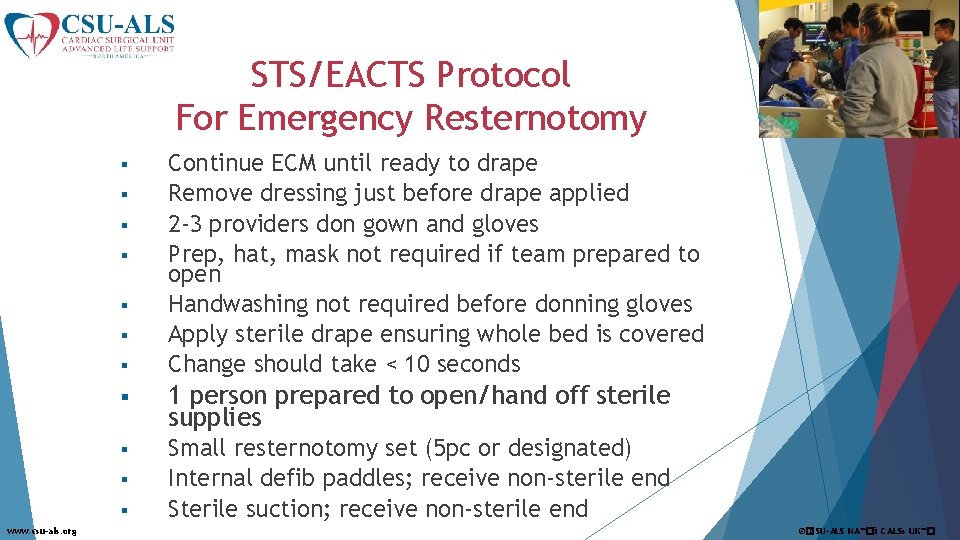
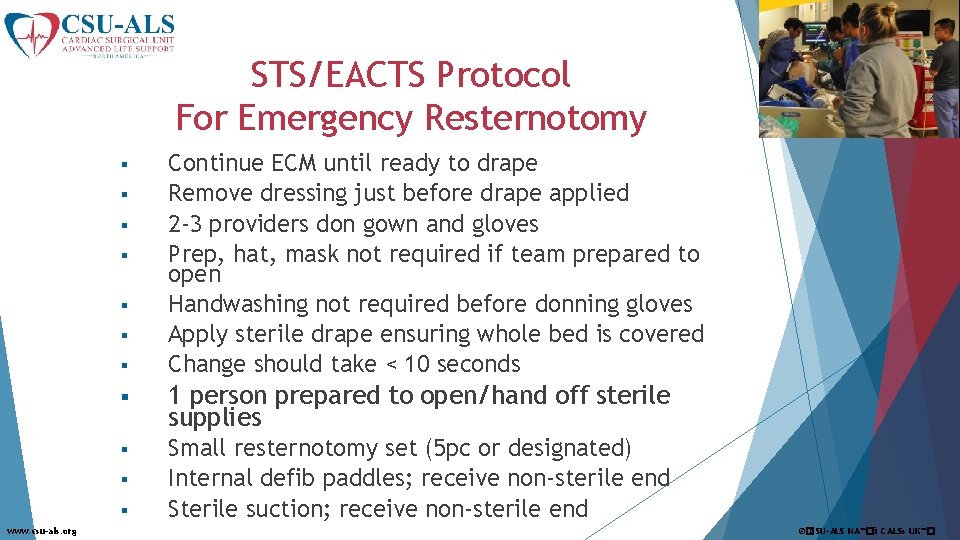
STS/EACTS Protocol For Emergency Resternotomy § § § § 1 person prepared to open/hand off sterile supplies § Small resternotomy set (5 pc or designated) Internal defib paddles; receive non-sterile end Sterile suction; receive non-sterile end § § www. csu-als. org Continue ECM until ready to drape Remove dressing just before drape applied 2 -3 providers don gown and gloves Prep, hat, mask not required if team prepared to open Handwashing not required before donning gloves Apply sterile drape ensuring whole bed is covered Change should take < 10 seconds ©�CSU-ALS NA™�& CALSs UK™�
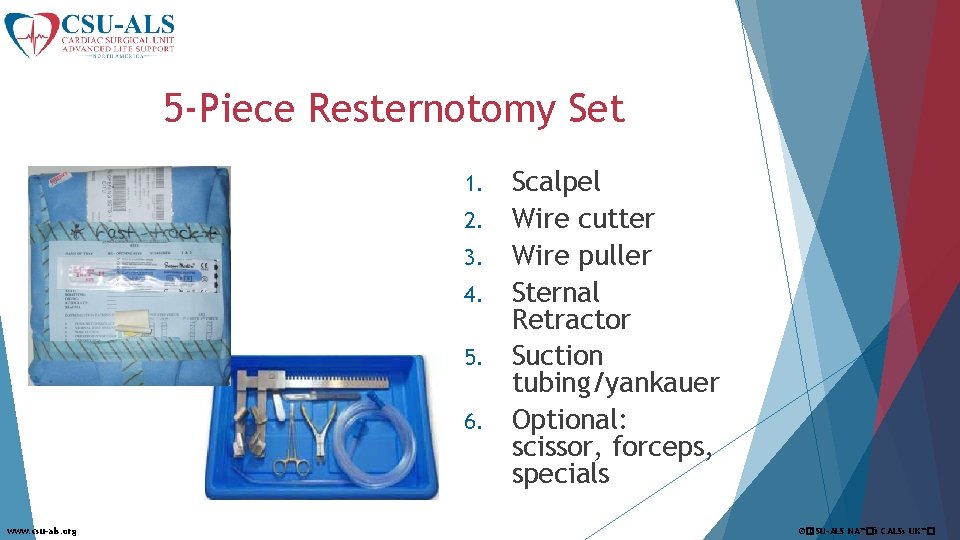
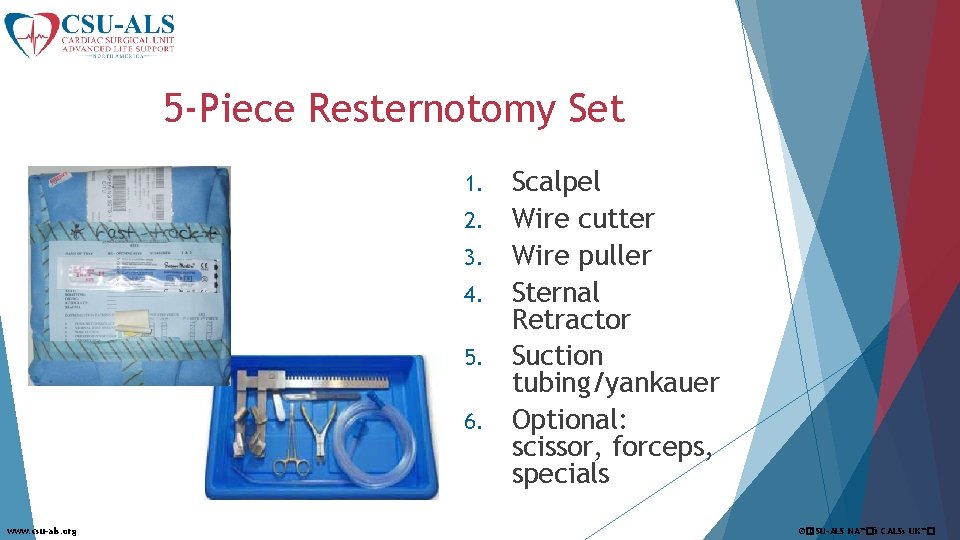
5 -Piece Resternotomy Set 1. 2. 3. 4. 5. 6. www. csu-als. org Scalpel Wire cutter Wire puller Sternal Retractor Suction tubing/yankauer Optional: scissor, forceps, specials ©�CSU-ALS NA™�& CALSs UK™�

Protocol for Resternotomy 1. Sterile providers § § 2. 3. Scalpel used deeply along prior incision, down to wires Cut all wires with wire cutters, pull out with heavy needle holder; ideally one person cuts while the other pulls § § 4. Sternal edges will separate – tamponade may be relieved Be prepared with sterile suction Insert chest retractor underneath sternum; open widely § § § www. csu-als. org Receive 5 pc instrument set onto sterile field Receive internal defibrillator paddles onto field Assess for bleeding – maintain sterile suction Identify grafts before starting 2 -handed internal massage Internal defibrillator paddles 20 j x 3 ©�CSU-ALS NA™�& CALSs UK™�
Resuscitation Protocol Outside ICU ➤ Emergency resternotomy should form an integral part of the cardiac arrest protocol until postoperative day 10 ➤ In mixed wards outside of ICU, it may not be appropriate to follow this guideline ➤ However, STS/EACTS recommendations for immediate defibrillation or pacing, and epinephrine dosing, are preferred in lieu of the 2015 AHA guidelines www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�

Evidence Behind the Protocol www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
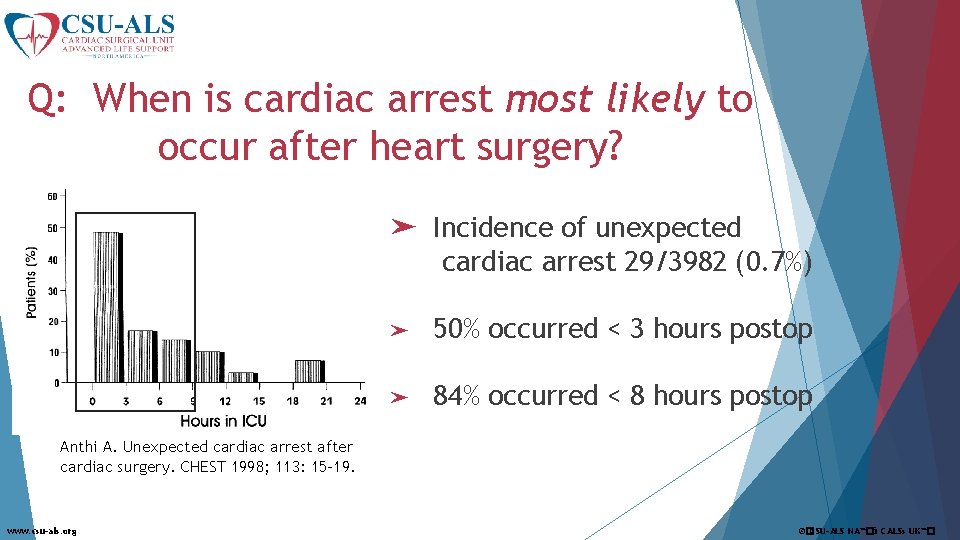
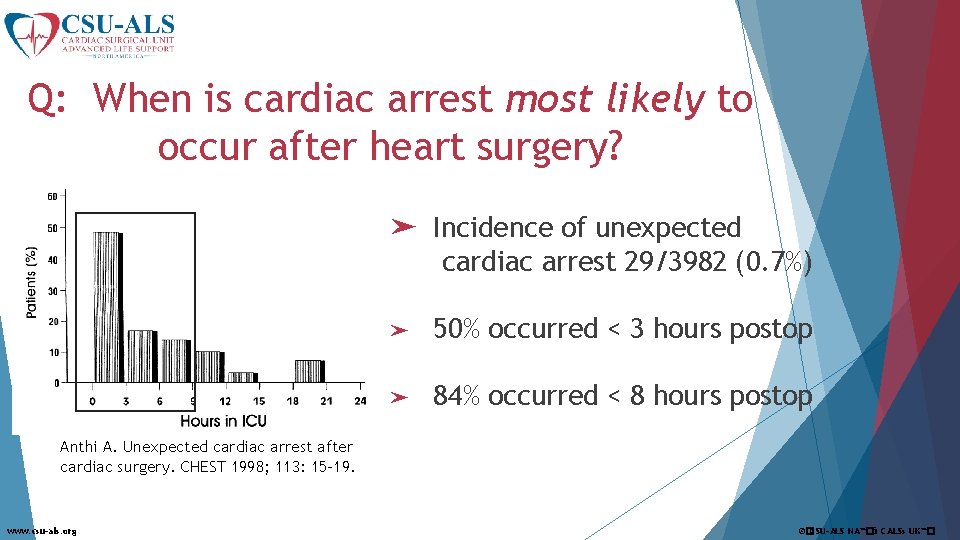
Q: When is cardiac arrest most likely to occur after heart surgery? ➤ Incidence of unexpected cardiac arrest 29/3982 (0. 7%) ➤ 50% occurred < 3 hours postop ➤ 84% occurred < 8 hours postop Anthi A. Unexpected cardiac arrest after cardiac surgery. CHEST 1998; 113: 15 -19. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
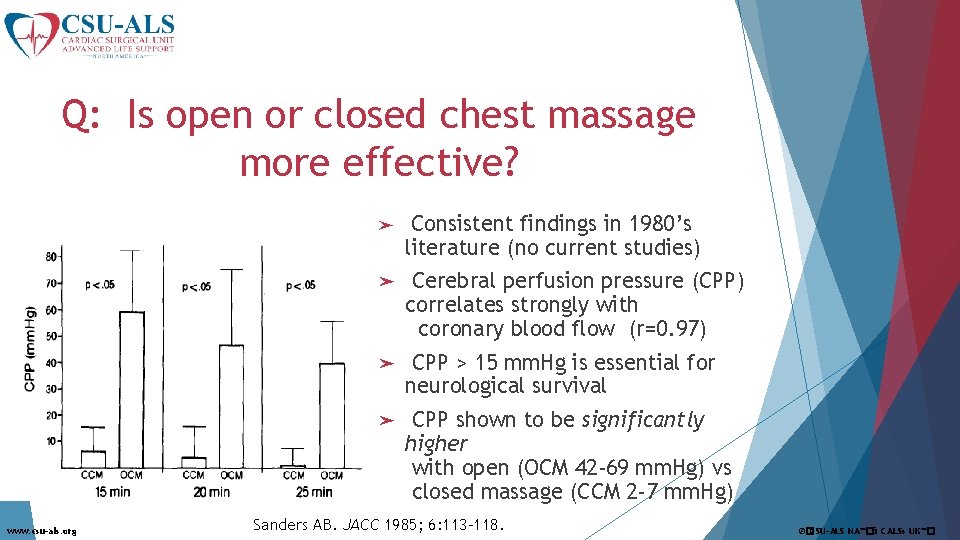
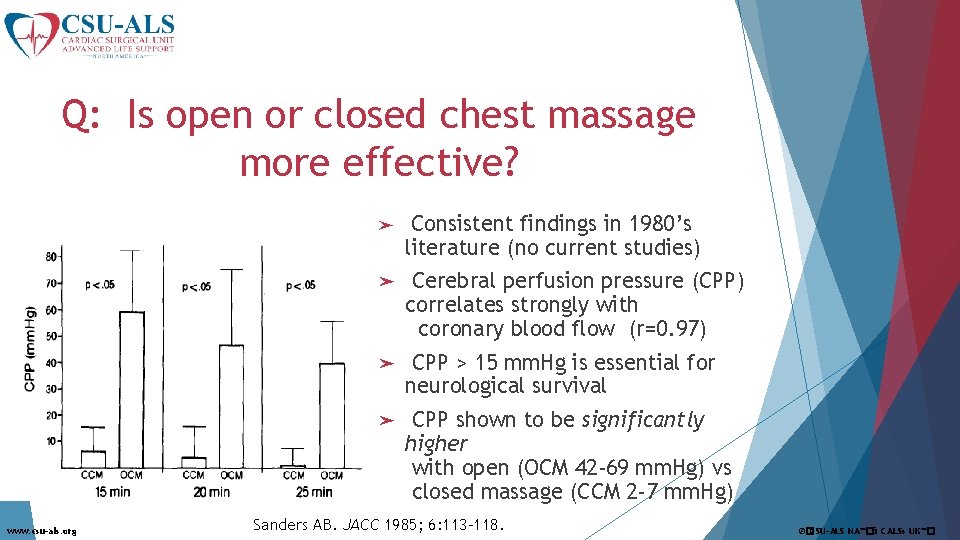
Q: Is open or closed chest massage more effective? www. csu-als. org ➤ Consistent findings in 1980’s literature (no current studies) ➤ Cerebral perfusion pressure (CPP) correlates strongly with coronary blood flow (r=0. 97) ➤ CPP > 15 mm. Hg is essential for neurological survival ➤ CPP shown to be significantly higher with open (OCM 42 -69 mm. Hg) vs closed massage (CCM 2 -7 mm. Hg) Sanders AB. JACC 1985; 6: 113 -118. ©�CSU-ALS NA™�& CALSs UK™�
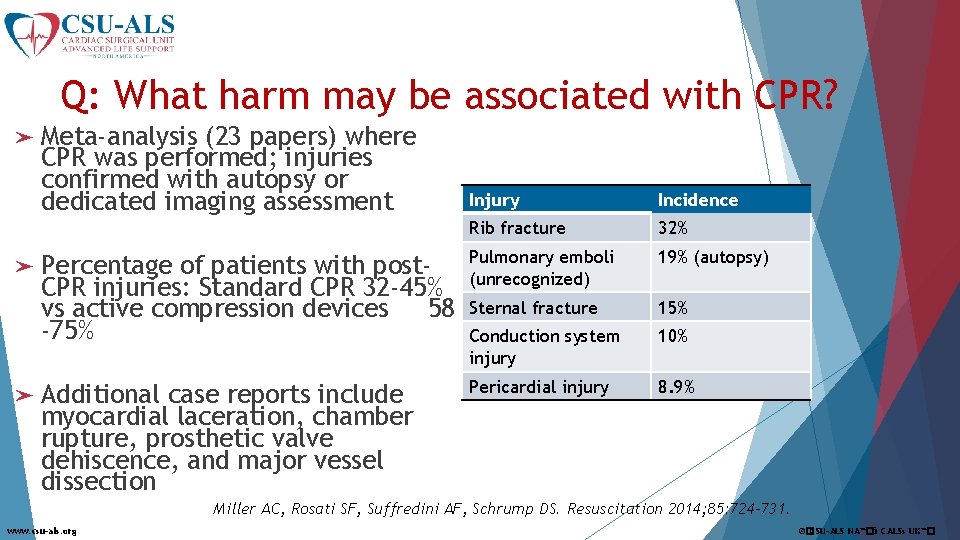
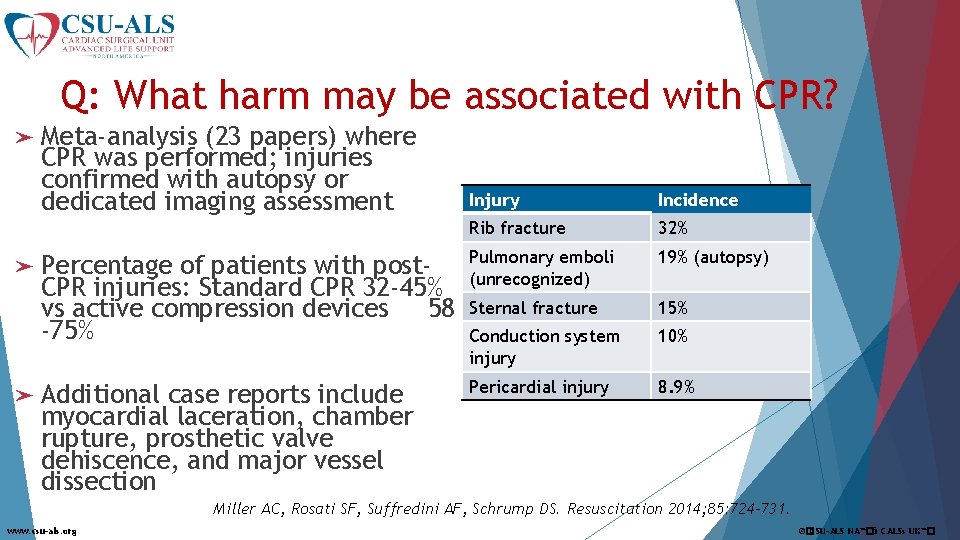
Q: What harm may be associated with CPR? ➤ Meta-analysis (23 papers) where CPR was performed; injuries confirmed with autopsy or dedicated imaging assessment ➤ Percentage of patients with post. CPR injuries: Standard CPR 32 -45% vs active compression devices 58 -75% ➤ Additional case reports include myocardial laceration, chamber rupture, prosthetic valve dehiscence, and major vessel dissection Injury Incidence Rib fracture 32% Pulmonary emboli (unrecognized) 19% (autopsy) Sternal fracture 15% Conduction system injury 10% Pericardial injury 8. 9% Miller AC, Rosati SF, Suffredini AF, Schrump DS. Resuscitation 2014; 85: 724 -731. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
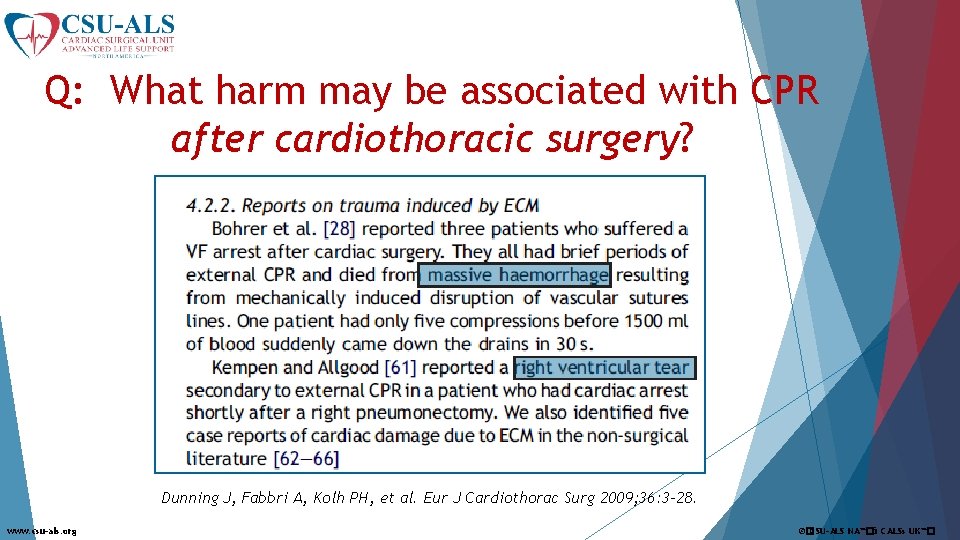
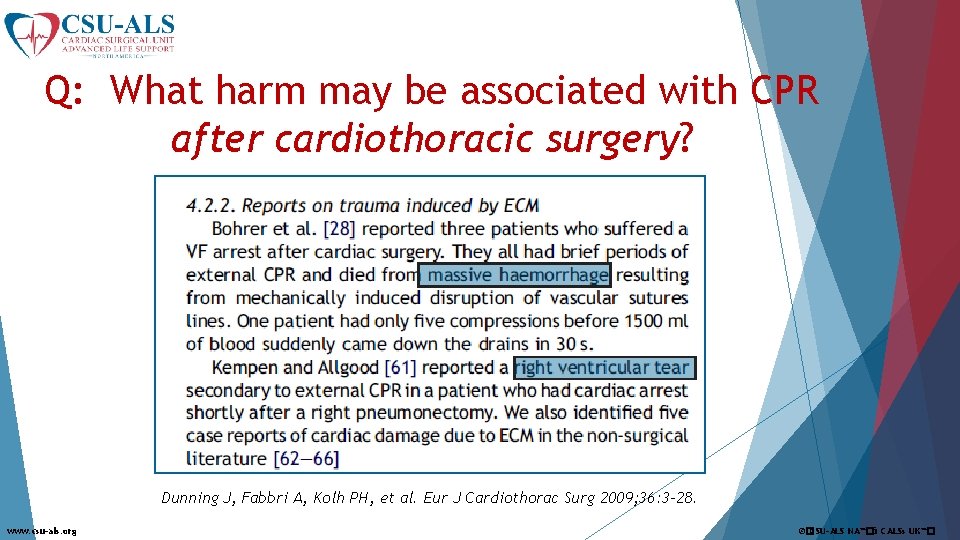
Q: What harm may be associated with CPR after cardiothoracic surgery? Dunning J, Fabbri A, Kolh PH, et al. Eur J Cardiothorac Surg 2009; 36: 3 -28. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
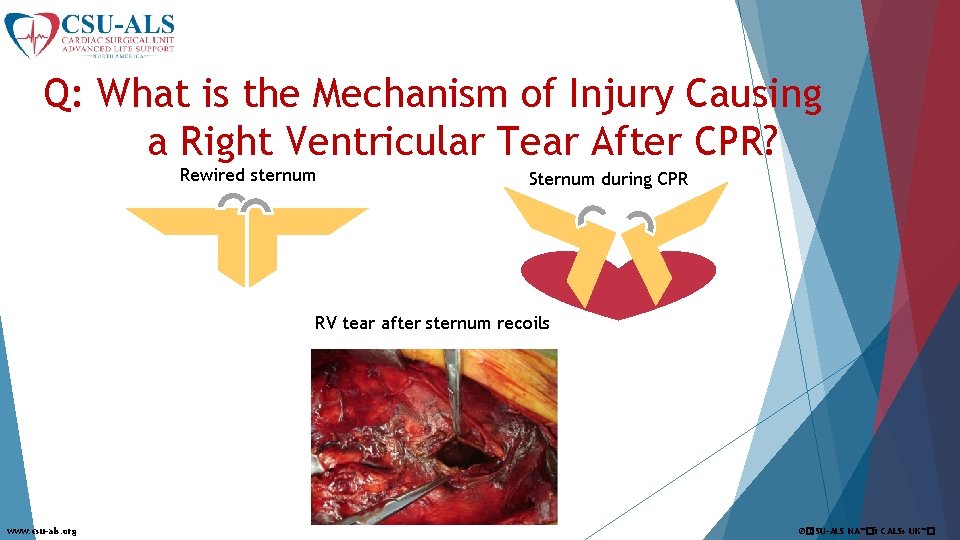
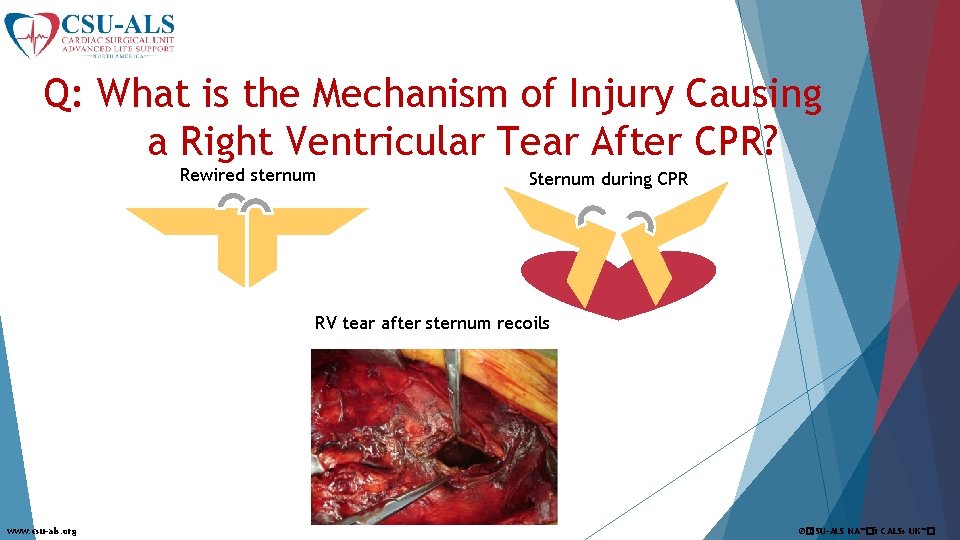
Q: What is the Mechanism of Injury Causing a Right Ventricular Tear After CPR? Rewired sternum Sternum during CPR RV tear after sternum recoils www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
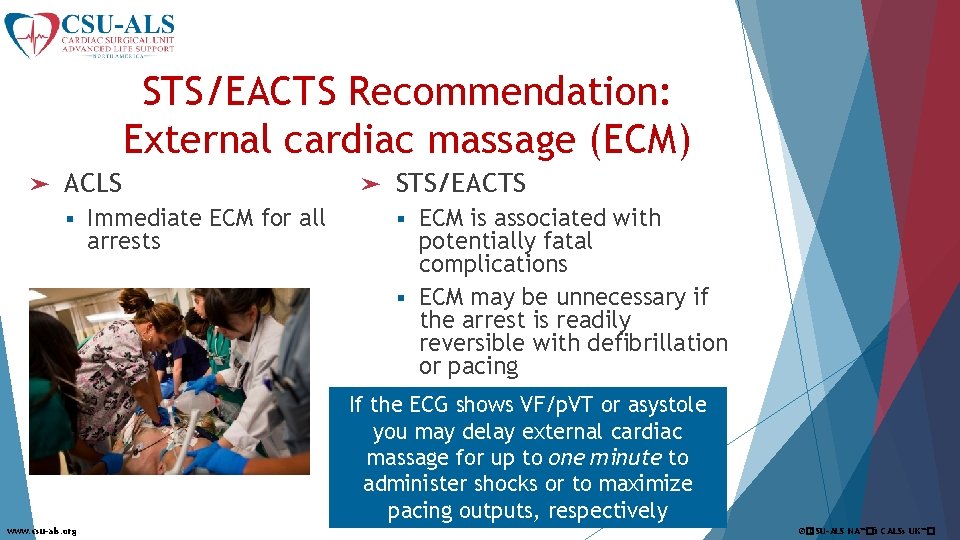
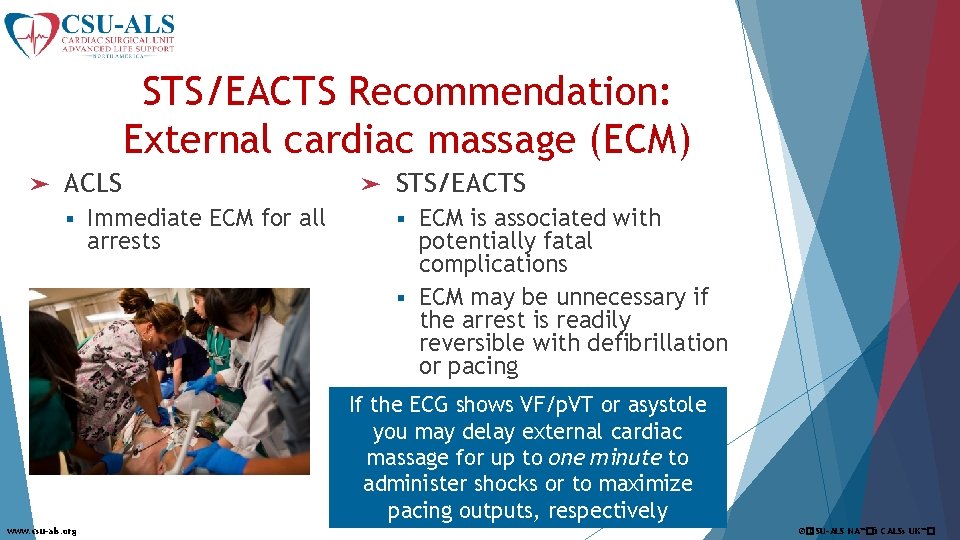
STS/EACTS Recommendation: External cardiac massage (ECM) ➤ ACLS § Immediate ECM for all arrests ➤ STS/EACTS ECM is associated with potentially fatal complications § ECM may be unnecessary if the arrest is readily reversible with defibrillation or pacing § If the ECG shows VF/p. VT or asystole you may delay external cardiac massage for up to one minute to administer shocks or to maximize pacing outputs, respectively www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
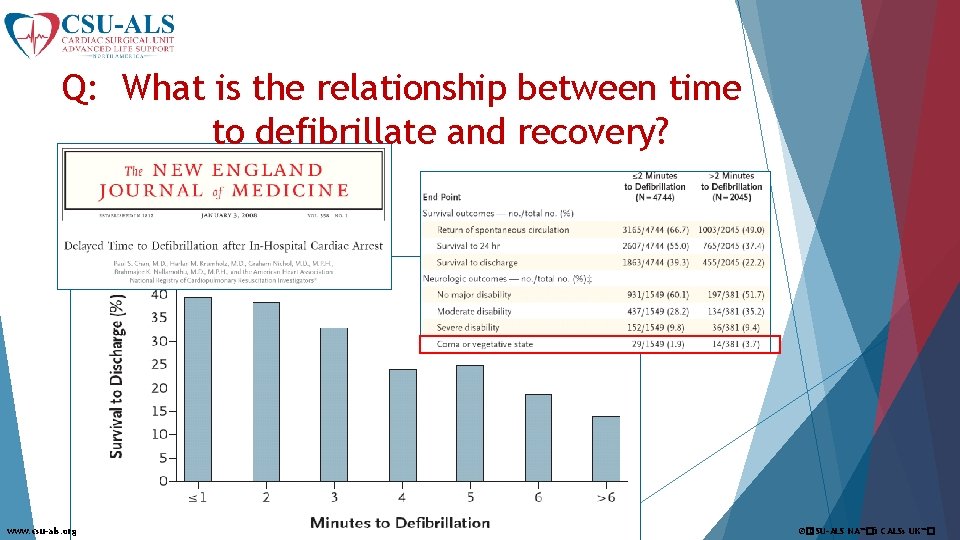
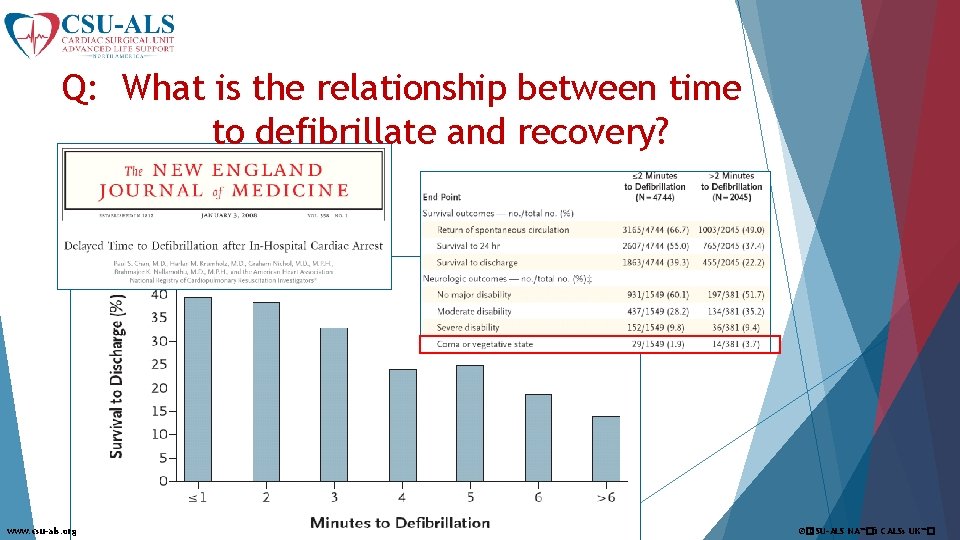
Q: What is the relationship between time to defibrillate and recovery? www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
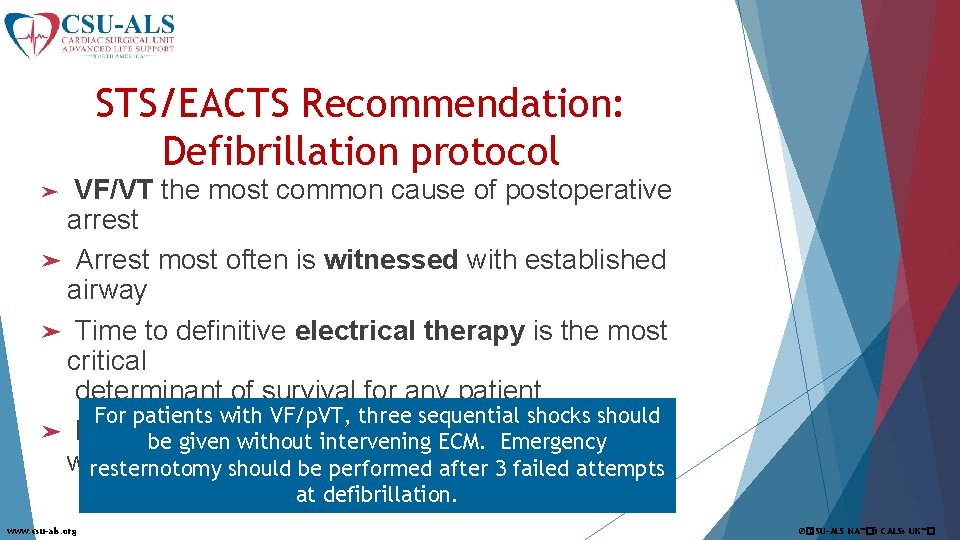
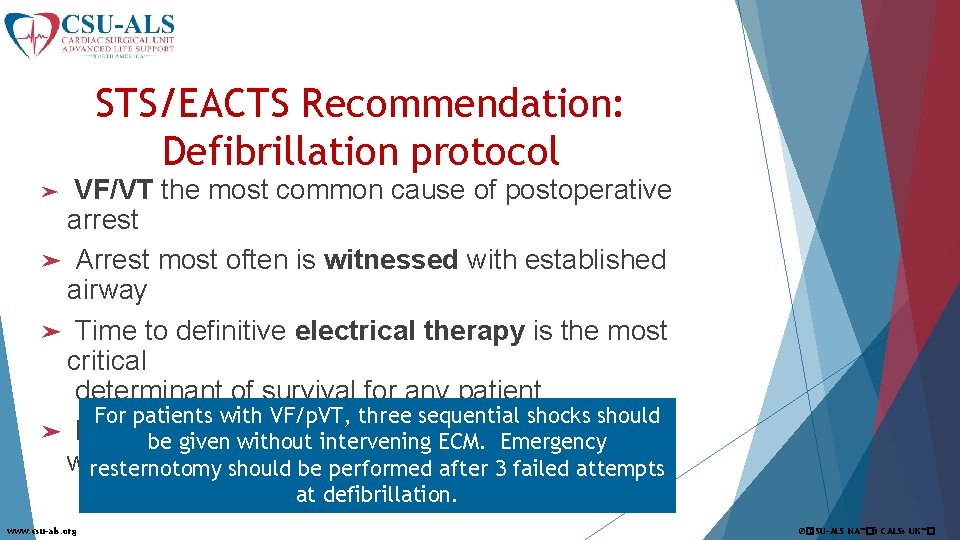
STS/EACTS Recommendation: Defibrillation protocol VF/VT the most common cause of postoperative arrest ➤ Arrest most often is witnessed with established airway ➤ Time to definitive electrical therapy is the most critical determinant of survival for any patient For patients with VF/p. VT, three sequential shocks should ➤ Data now support sequential shocks in be given without 3 intervening ECM. Emergency witnessed arresternotomy should be performed after 3 failed attempts ➤ at defibrillation. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
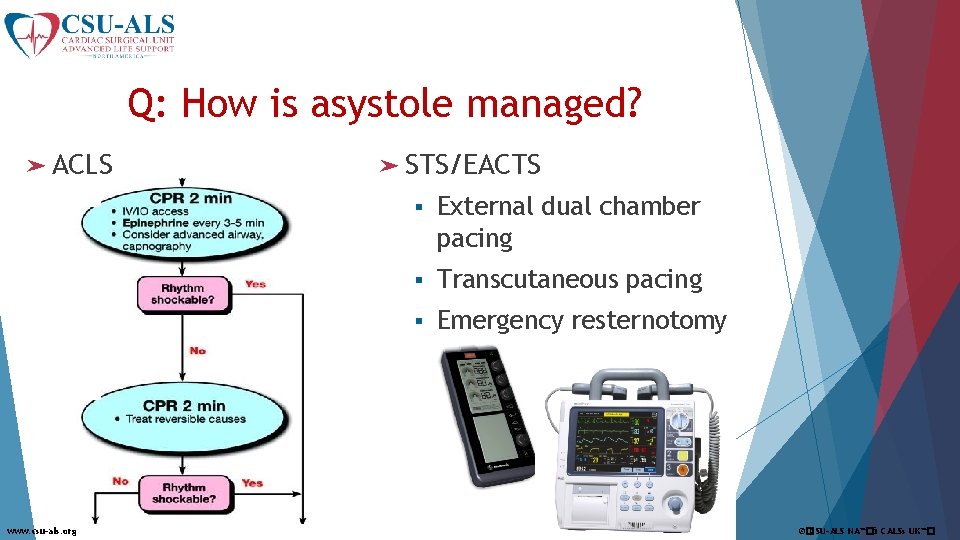
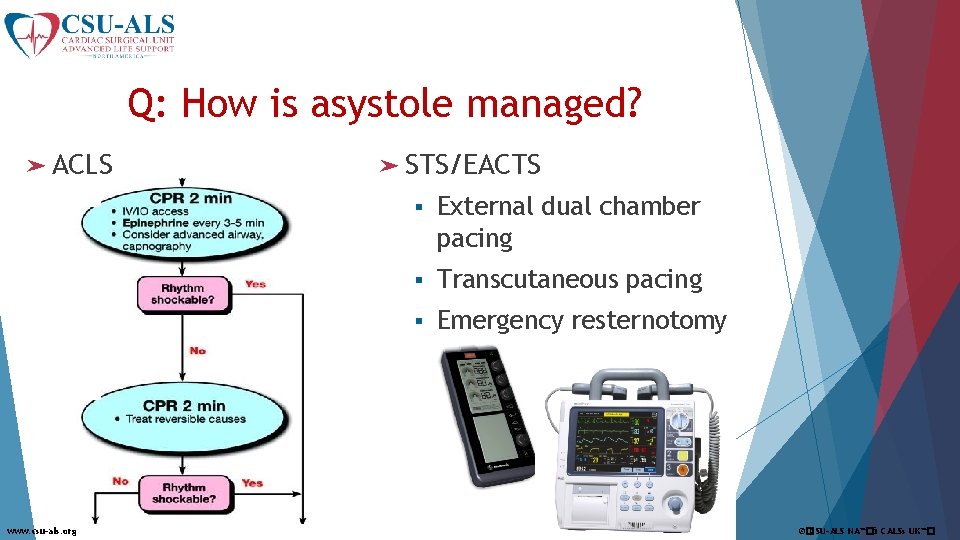
Q: How is asystole managed? ➤ ACLS www. csu-als. org ➤ STS/EACTS § External dual chamber pacing § Transcutaneous pacing § Emergency resternotomy ©�CSU-ALS NA™�& CALSs UK™�
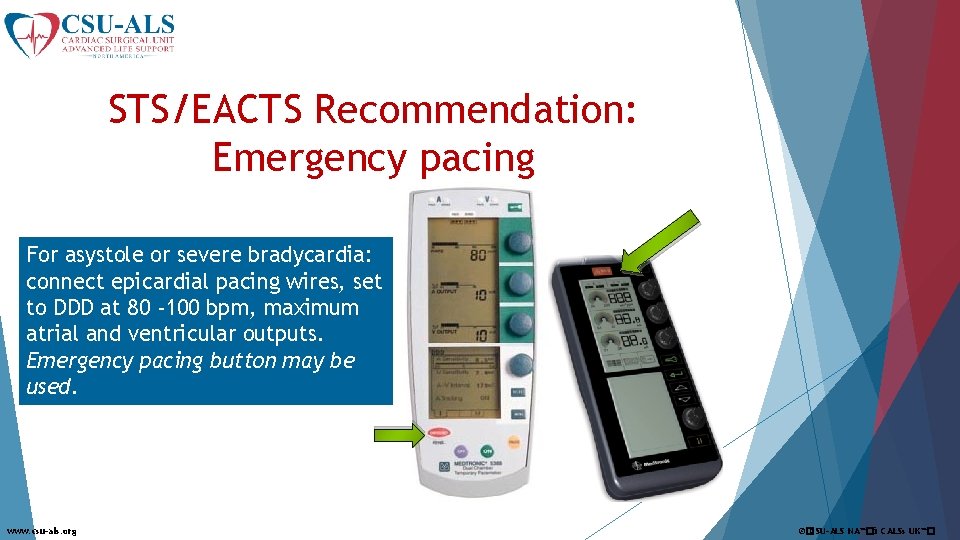
STS/EACTS Recommendation: Emergency pacing For asystole or severe bradycardia: connect epicardial pacing wires, set to DDD at 80 -100 bpm, maximum atrial and ventricular outputs. Emergency pacing button may be used. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
STS/EACTS Recommendation: PEA An ECG showing QRS complexes without pulsatile waveforms or ETCO 2 should be considered a PEA cardiac arrest If the rhythm is pulseless electrical activity and a pacemaker is connected and functioning, briefly turn off the pacemaker to exclude underlying ventricular fibrillation. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
![Epinephrine AHA Circulation 2015 132suppl 2 S 444S 464 www csuals org CSUALS NA Epinephrine: AHA Circulation 2015; 132[suppl 2]: S 444–S 464. www. csu-als. org ©�CSU-ALS NA™�&](https://slidetodoc.com/presentation_image_h/955912fe6f4ecc2594a24819d250c76e/image-45.jpg)
Epinephrine: AHA Circulation 2015; 132[suppl 2]: S 444–S 464. www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
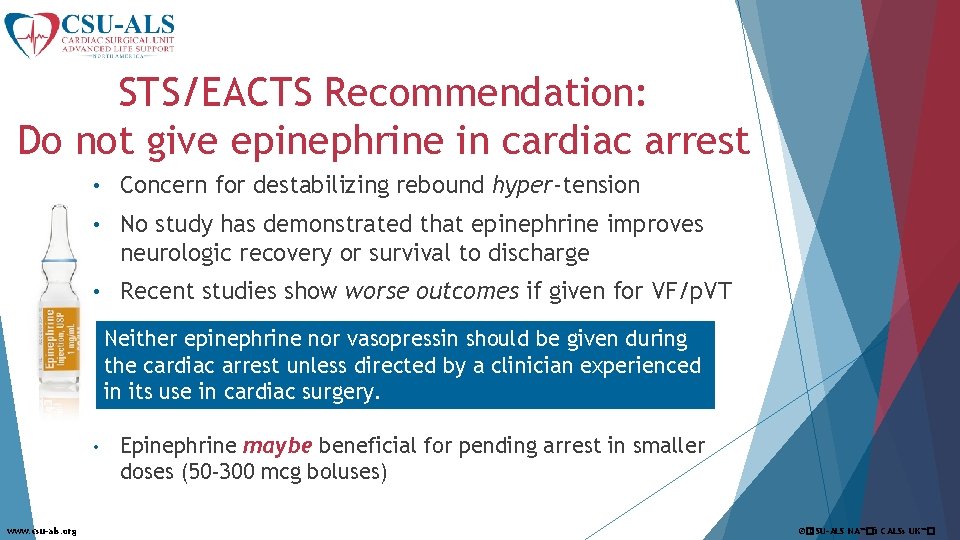
STS/EACTS Recommendation: Do not give epinephrine in cardiac arrest • Concern for destabilizing rebound hyper-tension • No study has demonstrated that epinephrine improves neurologic recovery or survival to discharge • Recent studies show worse outcomes if given for VF/p. VT Neither epinephrine nor vasopressin should be given during the cardiac arrest unless directed by a clinician experienced in its use in cardiac surgery. • www. csu-als. org Epinephrine maybe beneficial for pending arrest in smaller doses (50 -300 mcg boluses) ©�CSU-ALS NA™�& CALSs UK™�
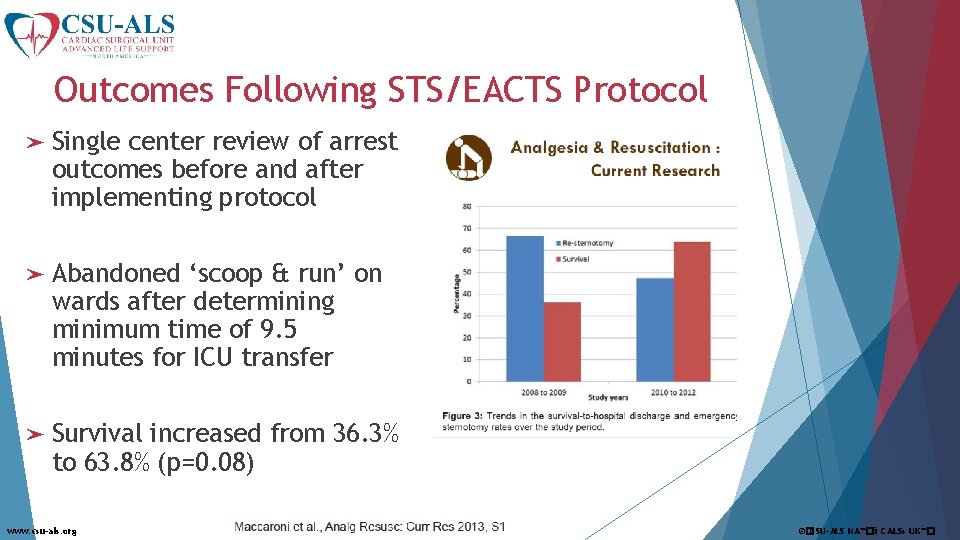
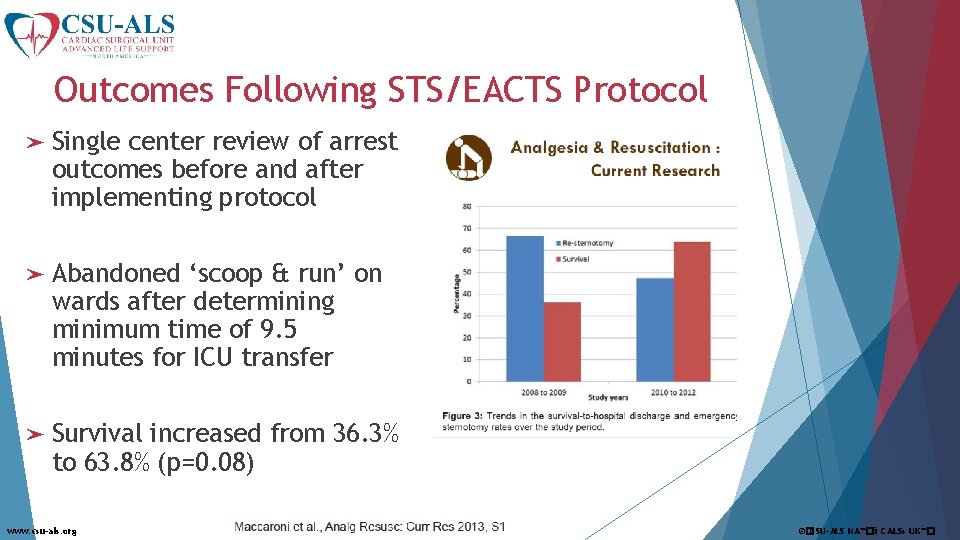
Outcomes Following STS/EACTS Protocol ➤ Single center review of arrest outcomes before and after implementing protocol ➤ Abandoned ‘scoop & run’ on wards after determining minimum time of 9. 5 minutes for ICU transfer ➤ Survival increased from 36. 3% to 63. 8% (p=0. 08) www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
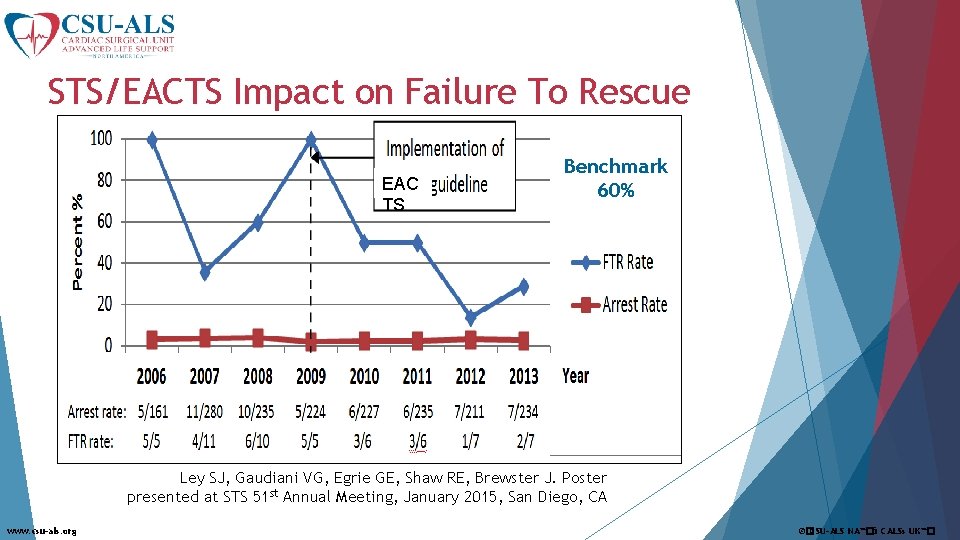
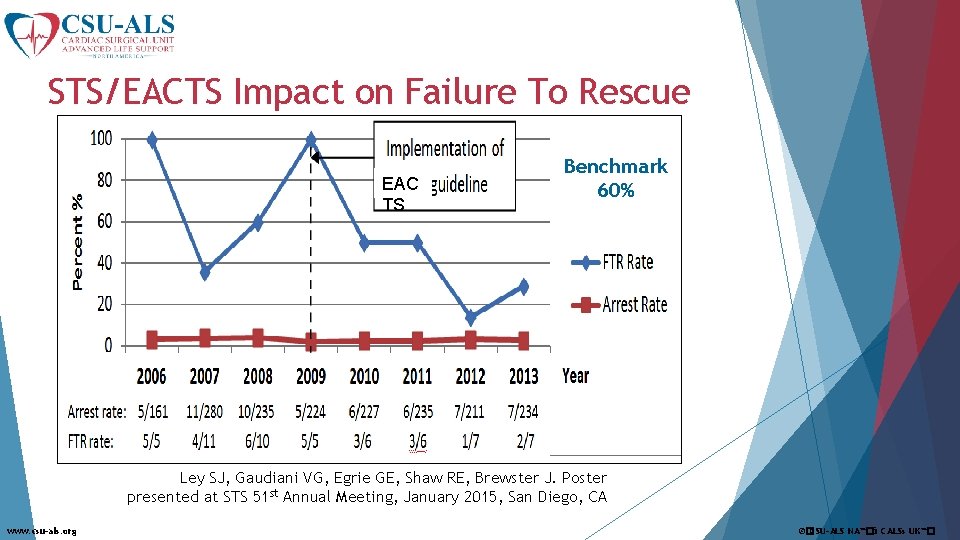
STS/EACTS Impact on Failure To Rescue EAC TS Benchmark 60% Ley SJ, Gaudiani VG, Egrie GE, Shaw RE, Brewster J. Poster presented at STS 51 st Annual Meeting, January 2015, San Diego, CA www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�

Leadership ➤ 25 Members Multidisciplinary Advisory Board for North America ➤Program Administration Manual/ Standardized Course ➤E-Learning Pre-Course/ Maintenance of Certification ➤ 2 year Recertification Cycle ➤Course Manual ➤Provider Model for Certification/ Recertification ➤Trainer Course/ Model for Trainer Certification/ Recertification www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Certification/ Recertification Provider ➤Live Course Every 2 Years – taught at your institution ➤E-Learning Maintenance of Certification at 1 year ➤Access to E-Learning during 2 Year Certification Period ➤Encourage re-sternotomy practice quarterly on units www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Certification/ Recertification Trainer ➤Live Course Every 2 Years – taught nationally ➤Proctoring x 2 ➤E-Learning Maintenance of Certification at 1 year ➤Access to E-Learning during 2 Year Certification Period ➤Encourage re-sternotomy practice quarterly on units www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Implementation Strategies ➤Review Current Practices – Gap Analysis vs. STS Protocol ➤Work with your Code Blue Committee ➤Physician Champion ➤Update Protocols/ Policies and Procedures/ Standing Orders ➤Clarify Scope of Practice Concerns www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�

Obstacles to Implementation ➤Culture ➤Cost ➤Confusion
CSU-ALS North America ➤ 501(c) 3 Non-Profit ➤All Volunteer Board ➤More than 50 sites using the Protocol ➤Accredited Centers/ Centers of Excellence ➤www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
Summary Management of Arrest after Cardiac Surgery ➤ Arrest management in ICU is an anticipated problem that requires teamwork and preparation ➤ A modified approach is warranted based on the environment and population – superior outcomes are demonstrated with: § § § www. csu-als. org Immediate arrhythmia management – prior to ECM Knowledge of protocol and key roles fostering timely emergency resternotomy Removal of epinephrine from arrest algorithm ©�CSU-ALS NA™�& CALSs UK™�
Summary Management of Arrest after Cardiac Surgery ➤ A collaborative approach is required for this training to be successfully implemented ➤ We have lived in an ACLS culture for decades that must be overcome for successful implementation ➤ You know have an international body as a resources and partner in implementing this education.

Questions? www. csu-als. org ©�CSU-ALS NA™�& CALSs UK™�
 Csu-als
Csu-als Cardiac surgery
Cardiac surgery Alsf lighting system
Alsf lighting system Multiple approach-avoidance
Multiple approach-avoidance Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Differentiate between virtual circuit and datagram network
Differentiate between virtual circuit and datagram network Bandura's reciprocal determinism
Bandura's reciprocal determinism Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Research approach definition
Research approach definition Waterfall approach marketing example
Waterfall approach marketing example Traditional development approach
Traditional development approach Microsoft innovative educator trainer academy
Microsoft innovative educator trainer academy Functional vs innovative products
Functional vs innovative products Innovative ideas to grow business
Innovative ideas to grow business Innovative metal products
Innovative metal products Regression taschenrechner
Regression taschenrechner Innovative analytical solutions
Innovative analytical solutions Innovative business communication
Innovative business communication Innovative integration
Innovative integration Innovative finance
Innovative finance Innovative routines international
Innovative routines international Inventive and innovative
Inventive and innovative Innovative management for a changing world
Innovative management for a changing world Revenue generating ideas for museums
Revenue generating ideas for museums Classroom
Classroom Innovative train technology
Innovative train technology Innovative technology in science inquiry
Innovative technology in science inquiry Explain the innovative features of scripting languages.
Explain the innovative features of scripting languages. Functional vs innovative supply chain
Functional vs innovative supply chain A&a innovative solutions pvt ltd
A&a innovative solutions pvt ltd Innovative english school
Innovative english school Innovative training techniques
Innovative training techniques Innovative management for turbulent times
Innovative management for turbulent times Innovative library services
Innovative library services Innovative communication tools
Innovative communication tools Innovative features of scripting languages
Innovative features of scripting languages Adjunct employee management system
Adjunct employee management system Organizational innovation definition
Organizational innovation definition Innovative features of scripting language
Innovative features of scripting language Creative wheel
Creative wheel Milstat
Milstat These are entrepreneurs who are to follow the path shown by
These are entrepreneurs who are to follow the path shown by Innovative business models in agriculture
Innovative business models in agriculture Inclusive assessment examples
Inclusive assessment examples Innovative healthcare business solutions
Innovative healthcare business solutions Double splice tape
Double splice tape Pengertian karya inovatif
Pengertian karya inovatif Innovative university of eurasia
Innovative university of eurasia Dependent position legs
Dependent position legs Precordium
Precordium Mediastinum
Mediastinum Aschoff bodies diagram
Aschoff bodies diagram Properties of cardiac muscle
Properties of cardiac muscle Cardiac stimulants and depressants
Cardiac stimulants and depressants Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Reasons for cardiac arrest
Reasons for cardiac arrest Heart physiology
Heart physiology Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle