Consequences of AgeAssociated Peripheral Neuropathy James W Mold

- Slides: 28
Consequences of Age-Associated Peripheral Neuropathy James W. Mold, M. D. , M. P. H. Department of Family and Preventive Medicine University of Oklahoma
Co-investigators Michelle Roberts, B. S. Frank Lawler, M. D. , M. P. H.
Background Loss of deep tendon reflexes and vibratory sensation at the ankle are so commonly seen in older people that they are generally considered to be “normal” and relatively unimportant. However, a previous cross-sectional study showed that this “age-associated peripheral neuropathy” (AAPN) can be associated with bothersome symptoms and lower quality of life. Mold JW, Vesely S. The prevalence and consequences of peripheral sensory neuropathy in older patients. JABFP 2004; 17(5): 309 -318.
Research Question Does the presence of age-associated peripheral neuropathy (AAPN) at baseline predict: 1. Earlier mortality 2. Earlier visits to Emergency Departments, 3. Earlier hospitalizations, and/or 4. Reduced health-related quality of life (HRQo. L)
Design and Setting Inception cohort of non-institutionalized, non-demented individuals >65 y. o. recruited from active patient rolls of 23 primary care physicians, all members of a statewide PBRN (N=854) Enrolled in two waves over a two-year period Followed prospectively for up to five years with annual evaluations
Other Exclusions For these analyses, we included only those participants who had no selfreported history of diabetes, autoimmune disease, (SLE, RA, scleroderma), sarcoidosis, chronic hepatitis, chronic renal failure, Crohn’s, B 12 deficiency, or hereditary neuropathy (N=604)
Methods Alerted by letter from the patient’s physician Contacted by phone by a project coordinator Enrolled and evaluated by a research nurse (R. N. ) in the participant’s primary care physician’s office Re-enrolled and re-evaluated similarly once a year at approximately the same time of year
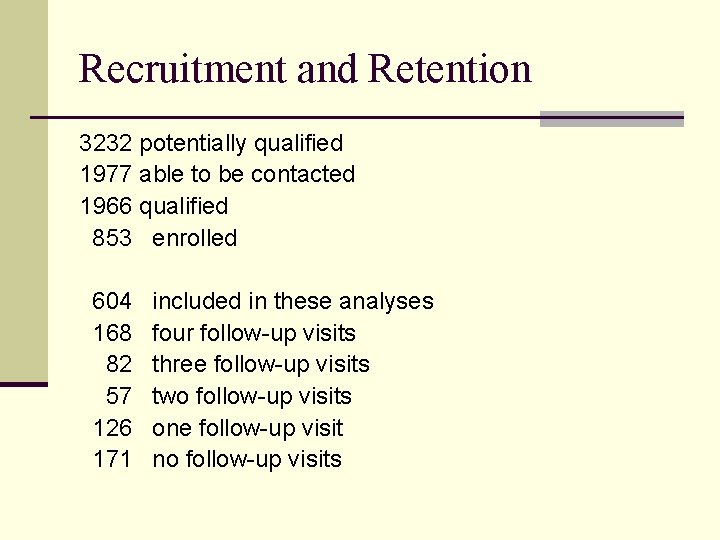
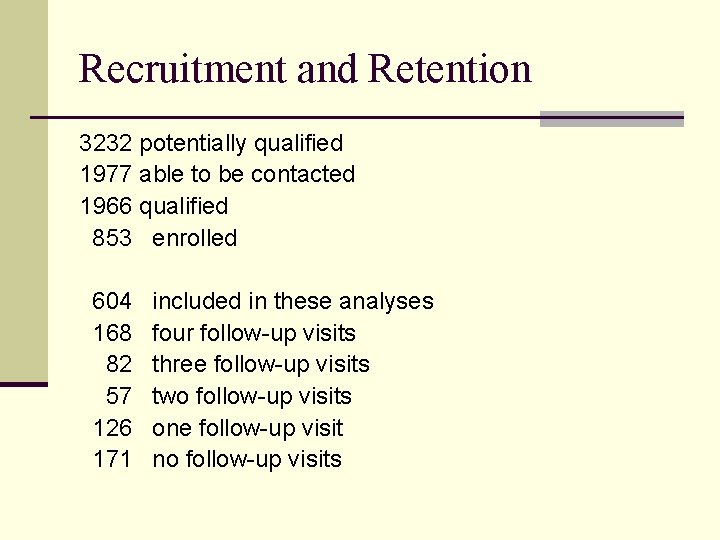
Recruitment and Retention 3232 potentially qualified 1977 able to be contacted 1966 qualified 853 enrolled 604 168 82 57 126 171 included in these analyses four follow-up visits three follow-up visits two follow-up visits one follow-up visit no follow-up visits
Recruitment and Retention Participation was associated with younger age, white race, being male, being better educated, and being in better health Retention was associated with younger age and worse cognition at baseline.
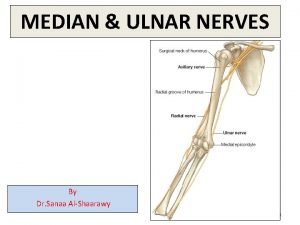
Data Collection Self-administered questionnaire, checked for completeness by research nurse Age, gender, race, use of cigarettes, military service, medical problems, functional status, self-rated health Peripheral neurological examination Deep tendon reflexes knees and ankles Vibratory sensation ankles and great toes Position sensation great toes Touch sensation soles of feet
Neurological Examination Two registered nurses trained by a neurologist to do peripheral neurological examination Each item was scored as present or absent (0, 1) Inter-rater reliability tested on volunteers and then on 25 consecutive enrollees Perfect agreement on all but DTR at ankle where they disagreed on 3/25 and were given additional training
Peripheral Neuropathy Peripheral neuropathy arbitrarily defined as bilateral absence of one or more of the following four sensory functions: DTR at ankles Vibration at ankles Position at great toes Touch on soles of feet
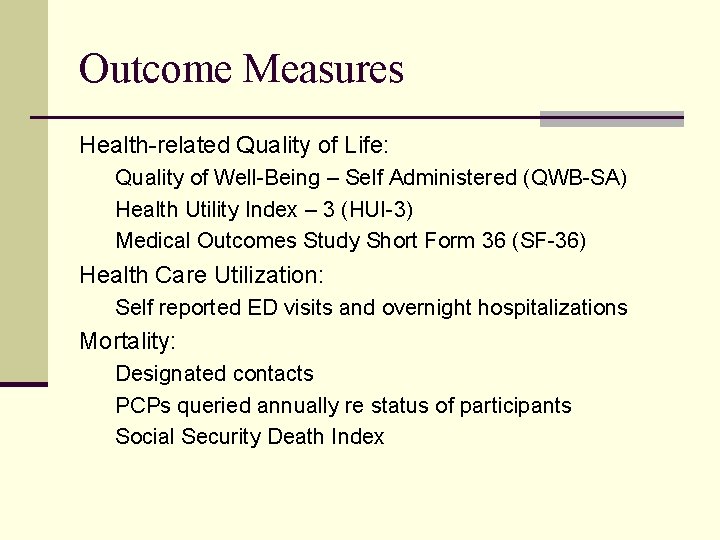
Outcome Measures Health-related Quality of Life: Quality of Well-Being – Self Administered (QWB-SA) Health Utility Index – 3 (HUI-3) Medical Outcomes Study Short Form 36 (SF-36) Health Care Utilization: Self reported ED visits and overnight hospitalizations Mortality: Designated contacts PCPs queried annually re status of participants Social Security Death Index
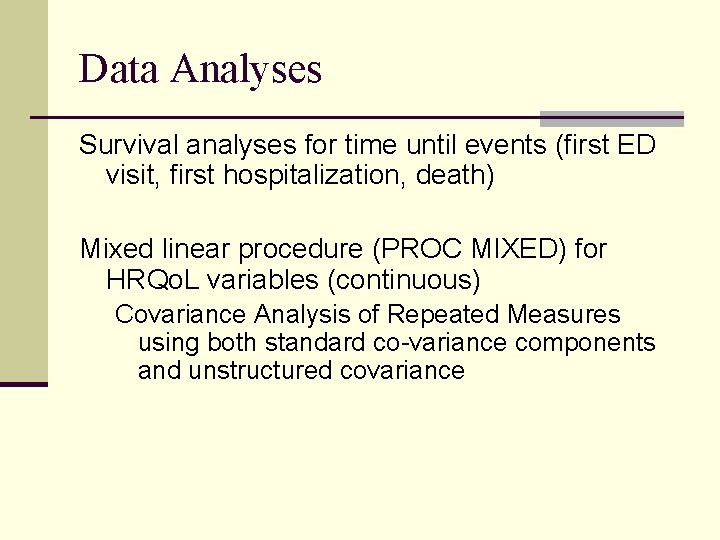
Data Analyses Survival analyses for time until events (first ED visit, first hospitalization, death) Mixed linear procedure (PROC MIXED) for HRQo. L variables (continuous) Covariance Analysis of Repeated Measures using both standard co-variance components and unstructured covariance
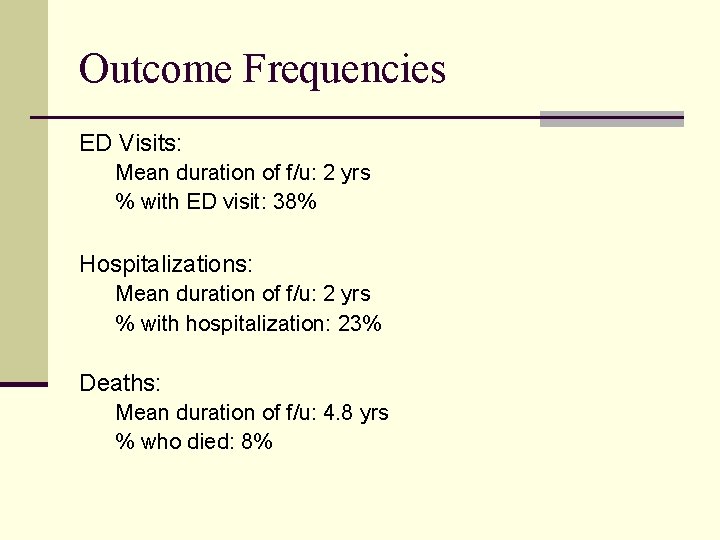
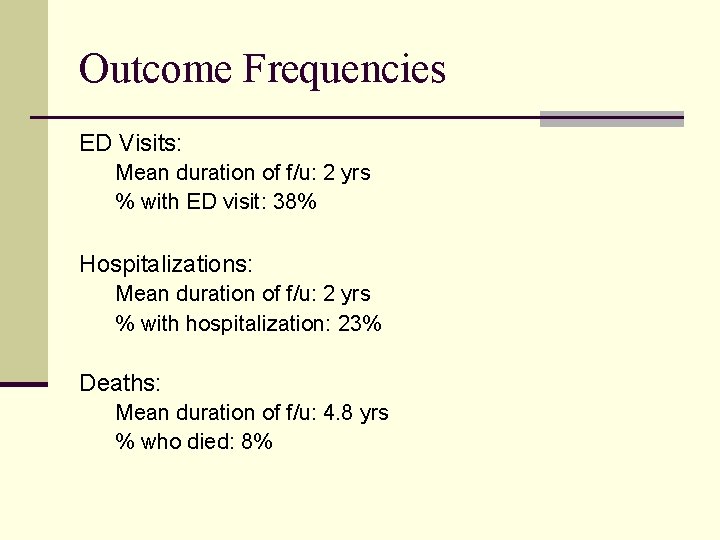
Outcome Frequencies ED Visits: Mean duration of f/u: 2 yrs % with ED visit: 38% Hospitalizations: Mean duration of f/u: 2 yrs % with hospitalization: 23% Deaths: Mean duration of f/u: 4. 8 yrs % who died: 8%
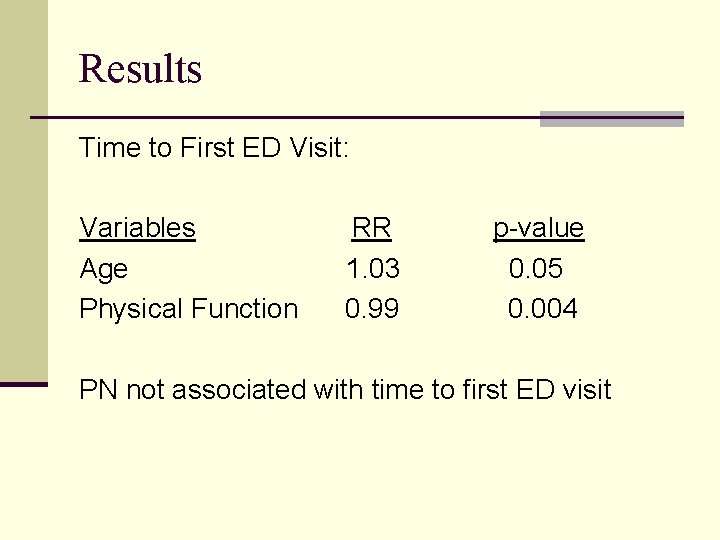
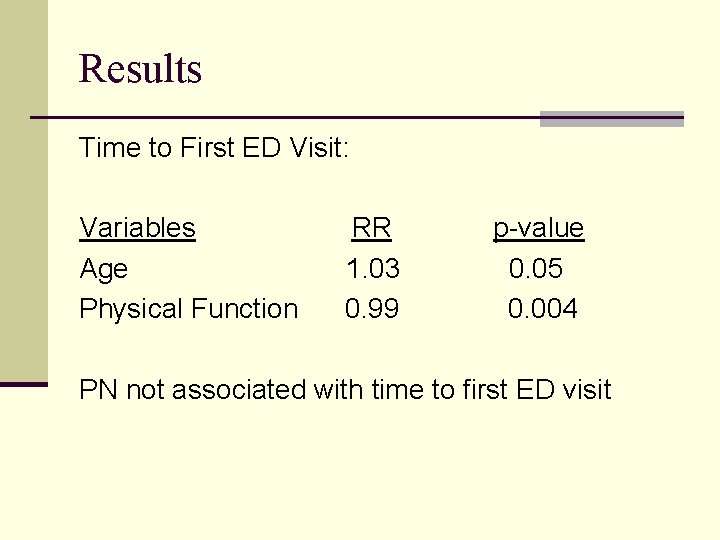
Results Time to First ED Visit: Variables Age Physical Function RR 1. 03 0. 99 p-value 0. 05 0. 004 PN not associated with time to first ED visit
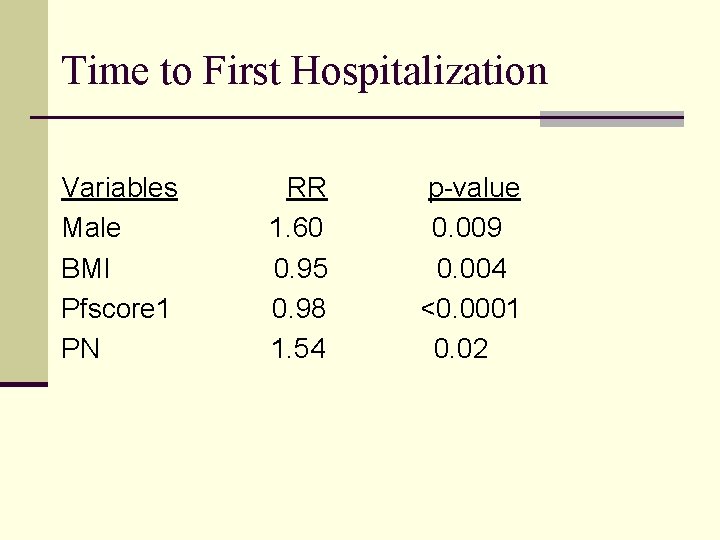
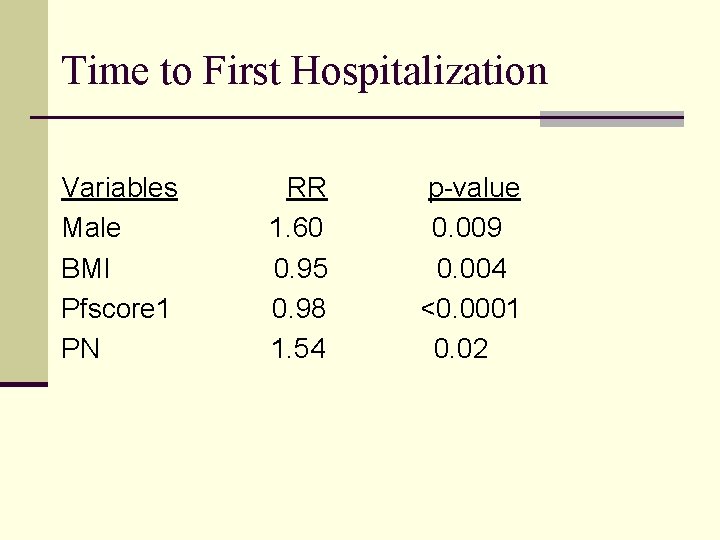
Time to First Hospitalization Variables Male BMI Pfscore 1 PN RR 1. 60 0. 95 0. 98 1. 54 p-value 0. 009 0. 004 <0. 0001 0. 02
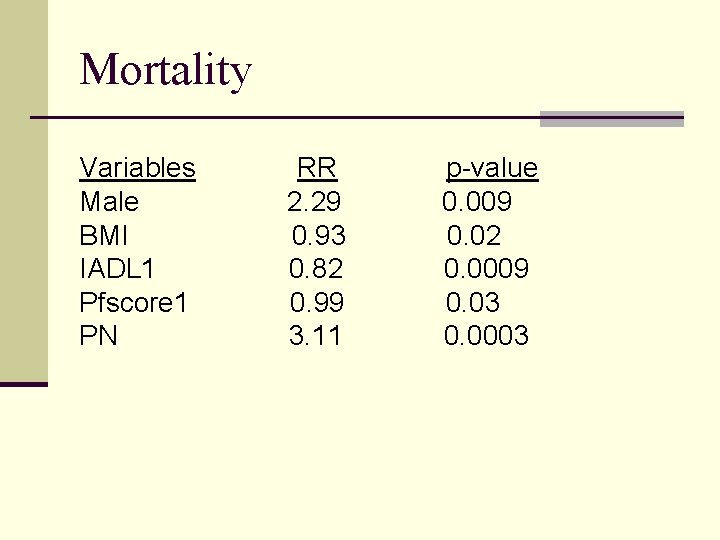
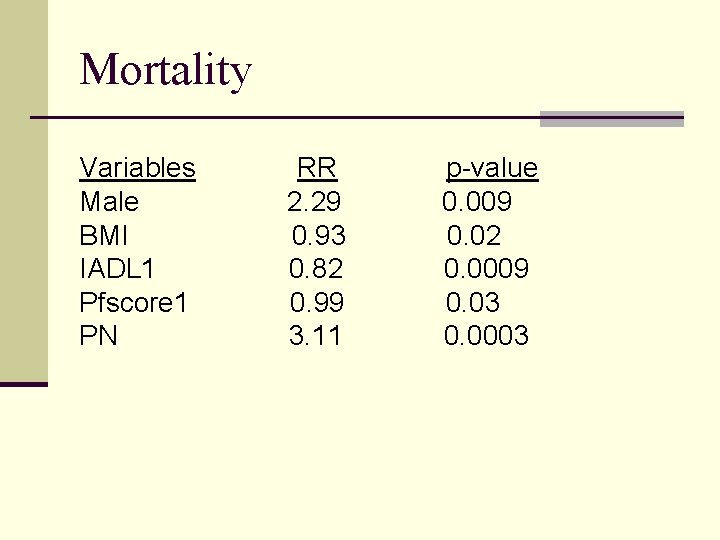
Mortality Variables Male BMI IADL 1 Pfscore 1 PN RR 2. 29 0. 93 0. 82 0. 99 3. 11 p-value 0. 009 0. 02 0. 0009 0. 03 0. 0003

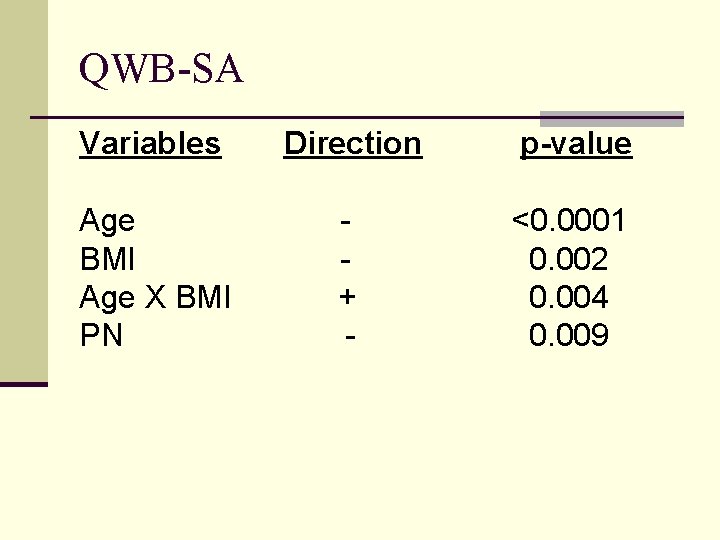
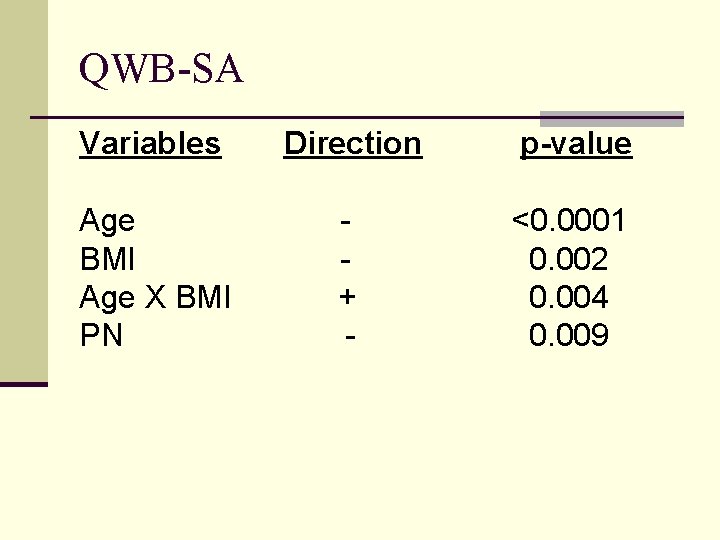
QWB-SA Variables Direction p-value Age BMI Age X BMI PN + - <0. 0001 0. 002 0. 004 0. 009
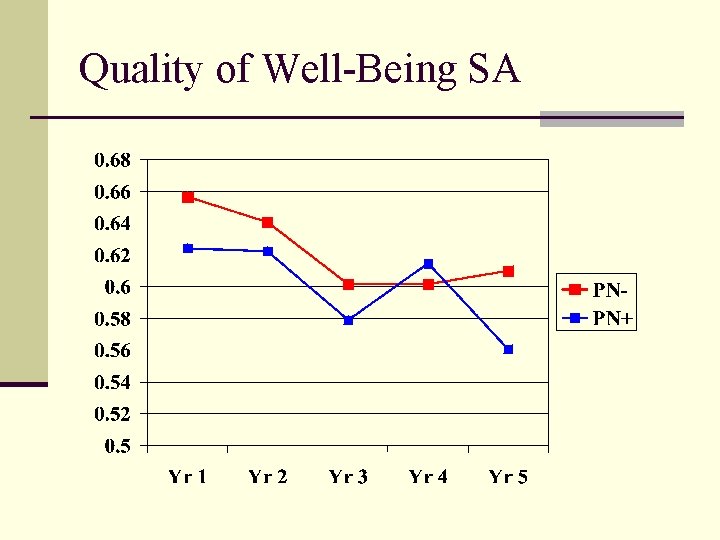
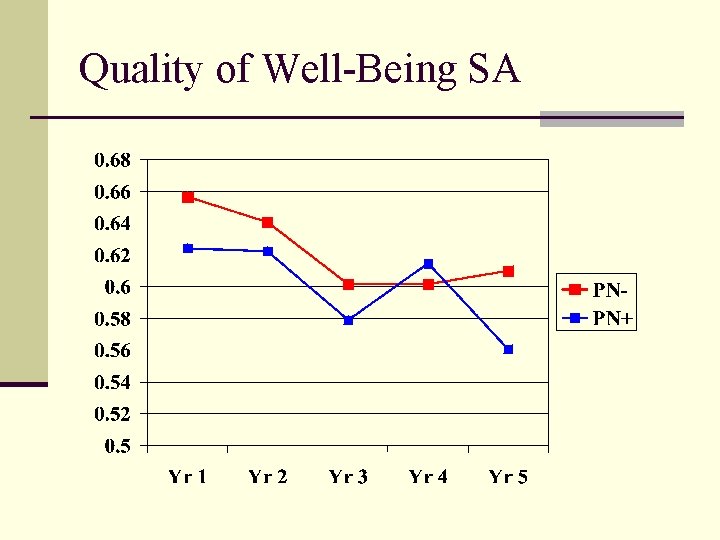
Quality of Well-Being SA
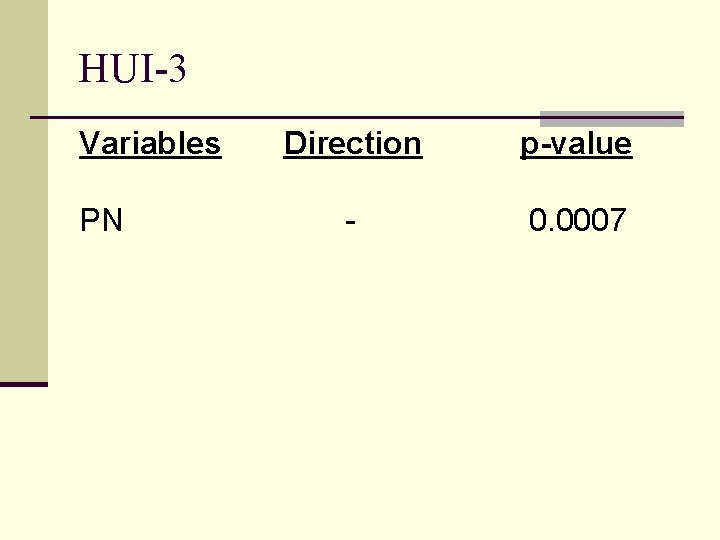
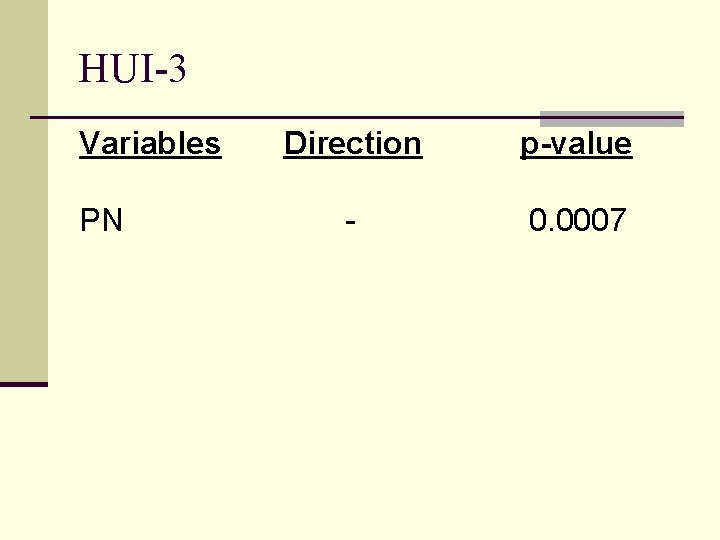
HUI-3 Variables PN Direction p-value - 0. 0007
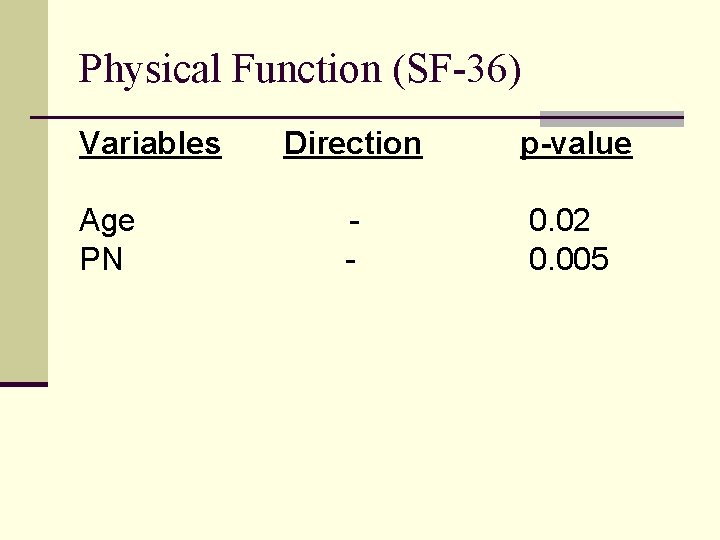
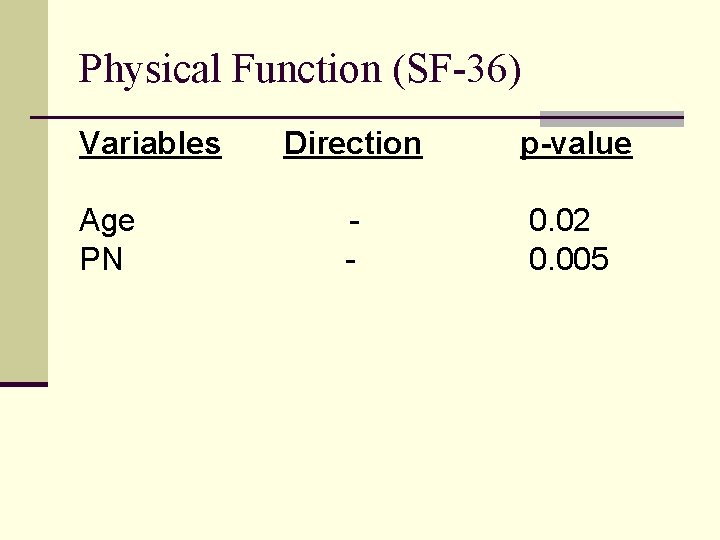
Physical Function (SF-36) Variables Age PN Direction p-value - 0. 02 0. 005
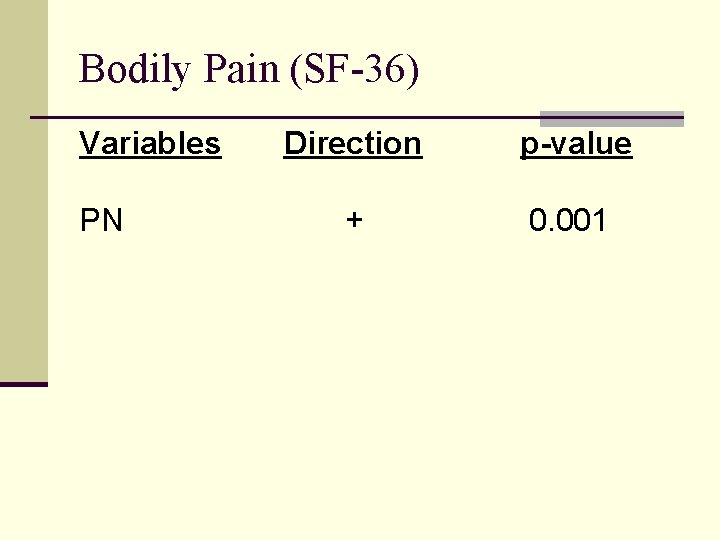
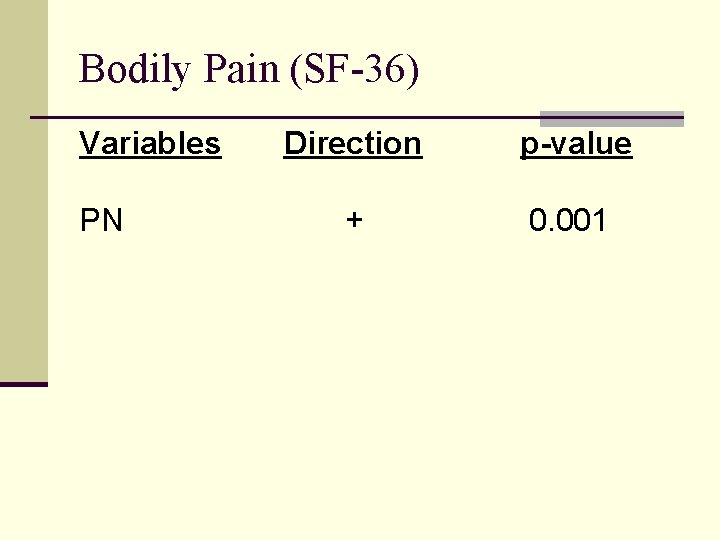
Bodily Pain (SF-36) Variables PN Direction p-value + 0. 001
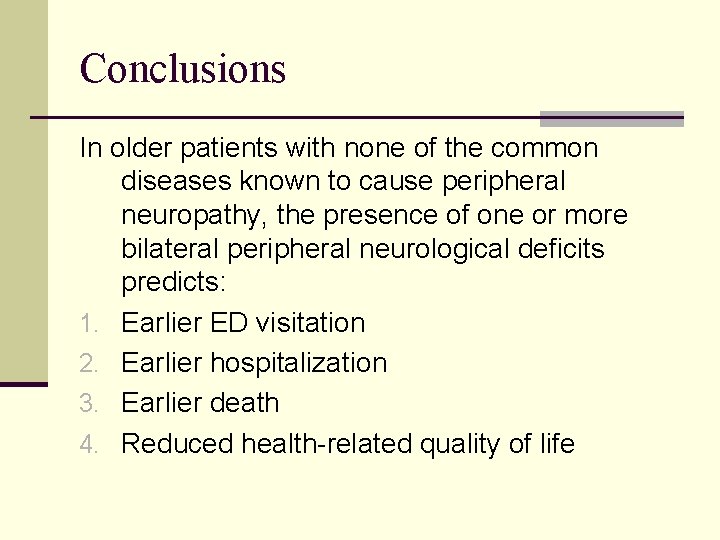
Conclusions In older patients with none of the common diseases known to cause peripheral neuropathy, the presence of one or more bilateral peripheral neurological deficits predicts: 1. Earlier ED visitation 2. Earlier hospitalization 3. Earlier death 4. Reduced health-related quality of life
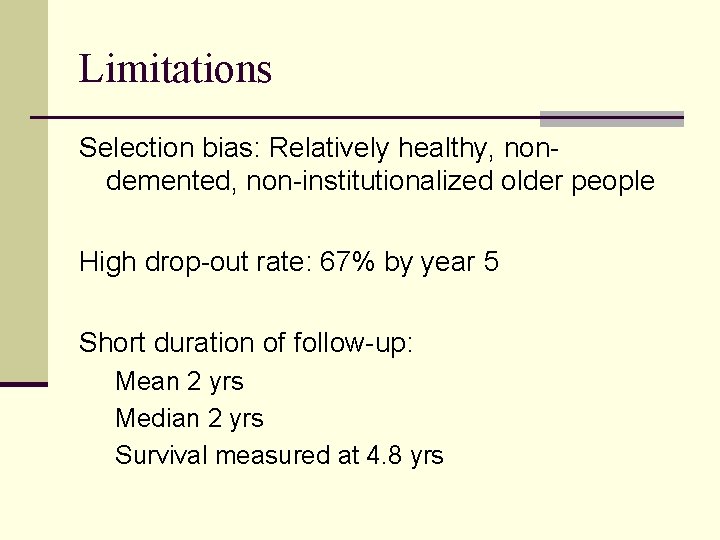
Limitations Selection bias: Relatively healthy, nondemented, non-institutionalized older people High drop-out rate: 67% by year 5 Short duration of follow-up: Mean 2 yrs Median 2 yrs Survival measured at 4. 8 yrs
Limitations Peripheral neuropathy was determined by physical examination Blanket exclusion of patients with most common known causes rather than actual diagnostic evaluation Medical problems and utilization were by selfreport (no medical record validation)
Questions
 Causes of peripheral neuropathy abcde
Causes of peripheral neuropathy abcde Ideopathic peripheral neuropathy
Ideopathic peripheral neuropathy Diabetes neuropathy
Diabetes neuropathy Pot type mold & plunger type mold are the classification of
Pot type mold & plunger type mold are the classification of Protista unicellular or multicellular
Protista unicellular or multicellular Pot type transfer moulding diagram
Pot type transfer moulding diagram Chiropractic neuropathy marketing
Chiropractic neuropathy marketing Diabetic neuropathy schaumburg
Diabetic neuropathy schaumburg Muscles supply by median nerve
Muscles supply by median nerve Albuminocytologic dissociation
Albuminocytologic dissociation Myotonia congenita
Myotonia congenita Large fibre neuropathy
Large fibre neuropathy Norma compression stockings
Norma compression stockings Description of pain
Description of pain Diabetic autonomic neuropathy
Diabetic autonomic neuropathy Giant cell arteritis
Giant cell arteritis Neuropathy test
Neuropathy test Scsi unit fbi
Scsi unit fbi James clayton lawson
James clayton lawson Cascading consequences
Cascading consequences Consequences of enolization
Consequences of enolization Air pollution consequences
Air pollution consequences Cause and effect examples
Cause and effect examples Romeo and juliet act 4 scene 2 questions
Romeo and juliet act 4 scene 2 questions Adhd and borderline personality disorder
Adhd and borderline personality disorder Consequences of variation
Consequences of variation Linking words adding
Linking words adding Berlin blockade consequences
Berlin blockade consequences Ideas have consequences bad ideas have victims
Ideas have consequences bad ideas have victims