COMPLEX REGIONAL PAIN SYNDROME Utkan Aydin MD CMKI








![Ketamine ■ Psychonautics (from the Greek ψυχή psychē ["soul", "spirit" or "mind"] and ναύτης Ketamine ■ Psychonautics (from the Greek ψυχή psychē ["soul", "spirit" or "mind"] and ναύτης](https://slidetodoc.com/presentation_image_h/049cd755f98e5d84be36fe49936cb773/image-57.jpg)

- Slides: 67
COMPLEX REGIONAL PAIN SYNDROME Utkan Aydin, MD CMKI Morning Lecture, 11/9/2015

The painful patient ■ Beware of patients being erroneously labeled by physicians ■ Patients can be looking for a disease label to justify their symptoms. ■ They may think it enhances their claim and/or may be seeking the role of sick or injured. They can be manipulating a psychosocial situation. Morton l. Kasdan, ASSH January 2011 Correspondence News
The painful patient ■ Humpty Dumpty sat on a wall, Humpty Dumpty had a great fall. All the king's horses and all the king's men Couldn't put Humpty together again Morton l. Kasdan, ASSH January 2011 Correspondence News
The painful patient ■ Know your patient and evaluate any secondary agenda. ■ Ask ourselves are we really doing this patient help or harm by labeling with RSD (CRPS) without objective bilateral imaging. ■ Evaluate whether we doing the “right thing” - giving the patient a label that is not confirmed with objective findings? ■ Always confirm a diagnosis with clear objective findings. ■ Understand there is nothing wrong with telling a patient you have pain that I cannot explain (Code 729. 5). Morton l. Kasdan, ASSH January 2011 Correspondence News
Terminology ■ Reflex Sympathetic Dystrophy ■ Causalgia ■ Neurodistrophy ■ Shoulder-hand syndrome ■ Sudeck’s atrophy ■ Sympathalgia Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Terminology ■ International Association for the Study of Pain (1994) – CRPS ■ Type I Pain syndrome without identifiable nerve lesion ■ Type II Syndrome with identifiable nerve injury or compression ■ Type III Other syndromes (e. g. fibromyalgia) Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Terminology ■ Type II is a clinical diagnosis – Supported by NCS ■ Type I and Type II can be divided into: – Sympathetically mediated pain – Sympathetically independent pain Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Terminology Pain ■ An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.
Terminology Allodynia Pain due to a stimulus that does not normally provoke pain.
Terminology Causalgia ■ A syndrome of sustained burning pain, allodynia, and hyperpathia after a traumatic nerve lesion, often combined with vasomotor and sudomotor dysfunction and later trophic changes.
Terminology Hyperalgesia ■ Increased pain from a stimulus that normally provokes pain.
Terminology Hyperesthesia ■ Increased sensitivity to stimulation, excluding the special senses.
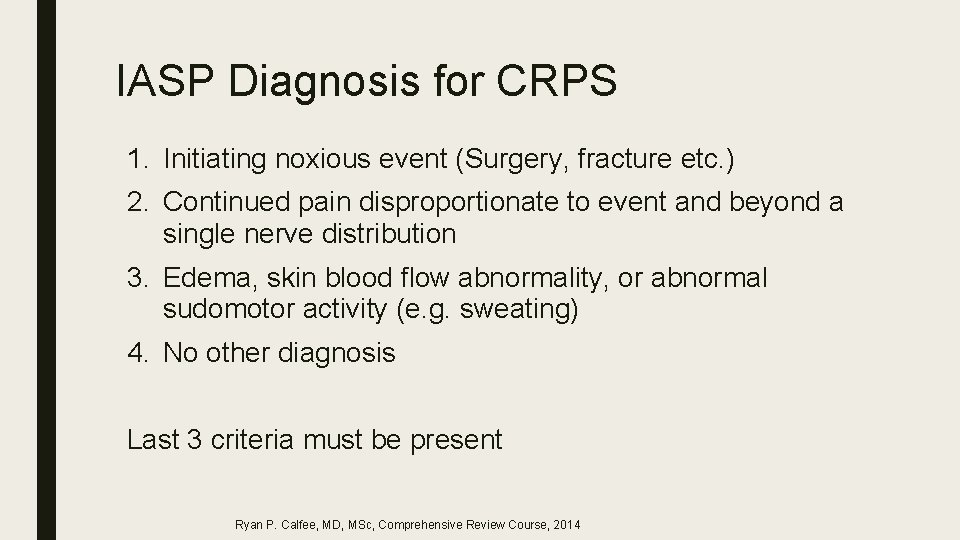
Terminology Noxious stimulus ■ A stimulus that is damaging or threatens damage to normal tissues.
IASP Diagnosis for CRPS 1. Initiating noxious event (Surgery, fracture etc. ) 2. Continued pain disproportionate to event and beyond a single nerve distribution 3. Edema, skin blood flow abnormality, or abnormal sudomotor activity (e. g. sweating) 4. No other diagnosis Last 3 criteria must be present Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Signs and Symptoms of CRPS ■ Pain starts in one limb but can present in the trunk (spine, abdomen, pelvis) ■ Constant pain, even at rest with intermittent exacerbations. Unexplained and diffuse ■ Severe pain ■ Temperature, color change. ■ Edema ■ Area of pain larger than the primary injury ■ Limited range of motion
Signs and Symptoms of CRPS ■ Allodynia ‐ pain on light touch ■ Nail growth changes (faster, distorted), hair growth changes (coarser, darker, rapid growth, hair falling), skin changes (atrophy of skin), skin lesions
Muscle symptoms in CRPS ■ Muscle spasms ■ Dystonia ■ Tremors ■ Myoclonus




Best Diagnostic tool ■ A good history and physical examination ■ A repeat examination may be done to come to a diagnosis because of the fleeting nature of some of the symptoms (color change, temperature asymmetry)
Pain physiology 1. Ascending nociceptive signals – Transmitted by Aδ and C afferent fibers – Dorsal horn of spinal cord (modulated) – Spinothalamic tract (cortical modulation) 2. Descending modulation – Periaqueductal gray matter – Nucleus raphe magnus (pons) Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Production of CRPS ■ Cutaneous – Epidermal neurite density – Afferent fiber desity ■ Sensitization of peripheral nerves secondary to excitatory mediators ■ Central sensitization – Spinal neurons ■ Altered symphathetic function – Increased nerve adrenergic receptors – Sympatho-afferent coupling ■ Upregulation of catecholamine receptors (vasoconstriction) ■ Genetic – Somatotopic maps Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
CRPS and Depression ■ CRPS causes suffering and affects mood but is NOT a psychogenic condition – 22 -78% chronic pain patients are depressed ■ Mersky, 1983 – Mood improves with pain resolution ■ Mellick et al. Arch Phys Med Reh 1997 Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Central Sensitization ■ Increase in the excitability of neurons within the central nervous system (CNS) so that normal inputs produce abnormal responses
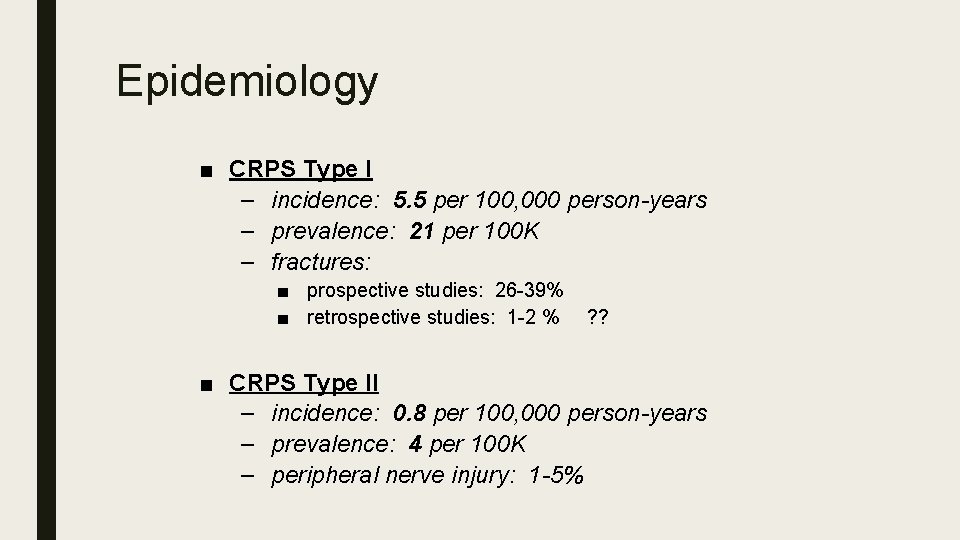
CRPS Associations ■ Anxiety prior to TKA predictive of CRPS at 1 month ■ Harden et al, Pain 2003 ■ Allergy/Hypersensitivity associated with CRPS in orthopaedic patients – 68% vs 34% in 115 CRPS vs 15 controls ■ Li et al, Orthopedics 2014 ■ Longer duration of anesthesia during limb surgery ■ Sumitani et al, Rheumatology 2013 Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Epidemiology ■ CRPS Type I – incidence: 5. 5 per 100, 000 person-years – prevalence: 21 per 100 K – fractures: ■ prospective studies: 26 -39% ■ retrospective studies: 1 -2 % ? ? ■ CRPS Type II – incidence: 0. 8 per 100, 000 person-years – prevalence: 4 per 100 K – peripheral nerve injury: 1 -5%
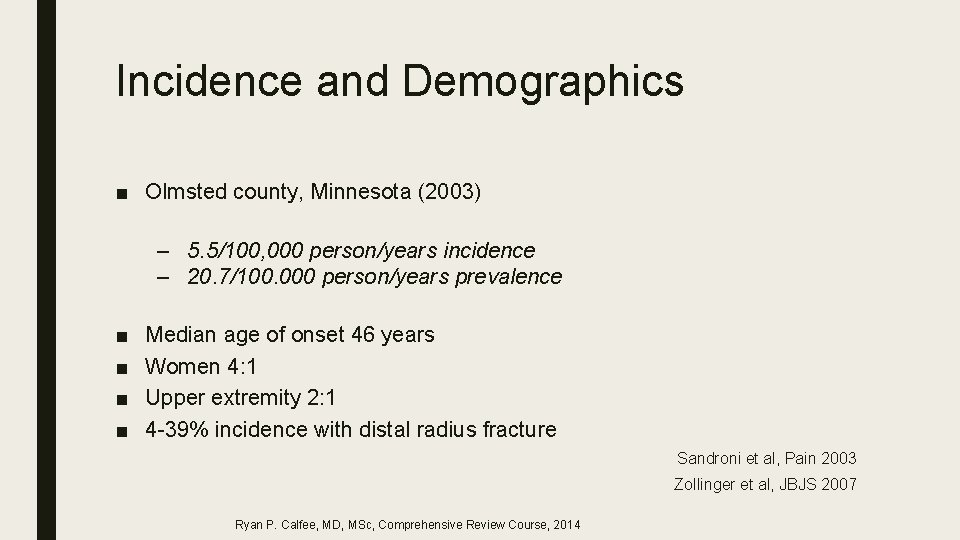
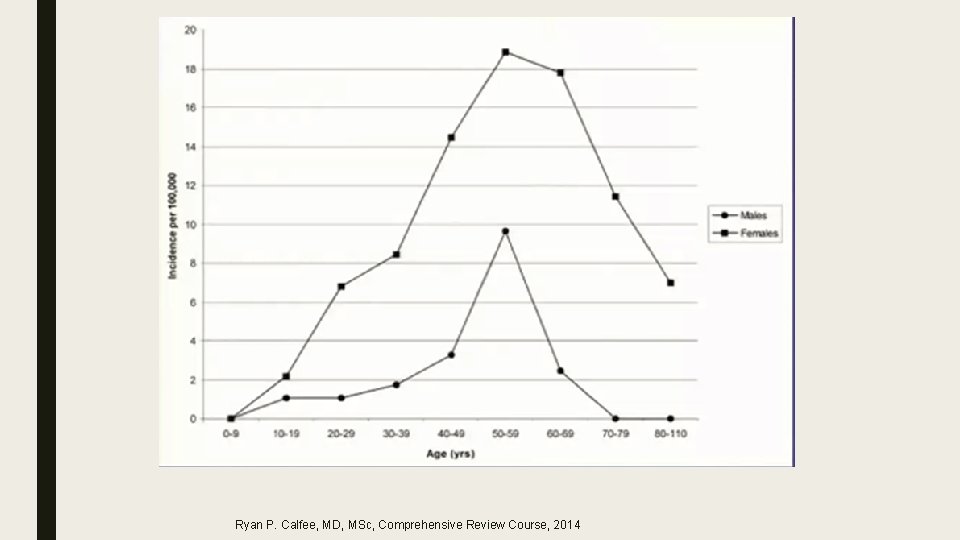
Incidence and Demographics ■ Olmsted county, Minnesota (2003) – 5. 5/100, 000 person/years incidence – 20. 7/100. 000 person/years prevalence ■ ■ Median age of onset 46 years Women 4: 1 Upper extremity 2: 1 4 -39% incidence with distal radius fracture Sandroni et al, Pain 2003 Zollinger et al, JBJS 2007 Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
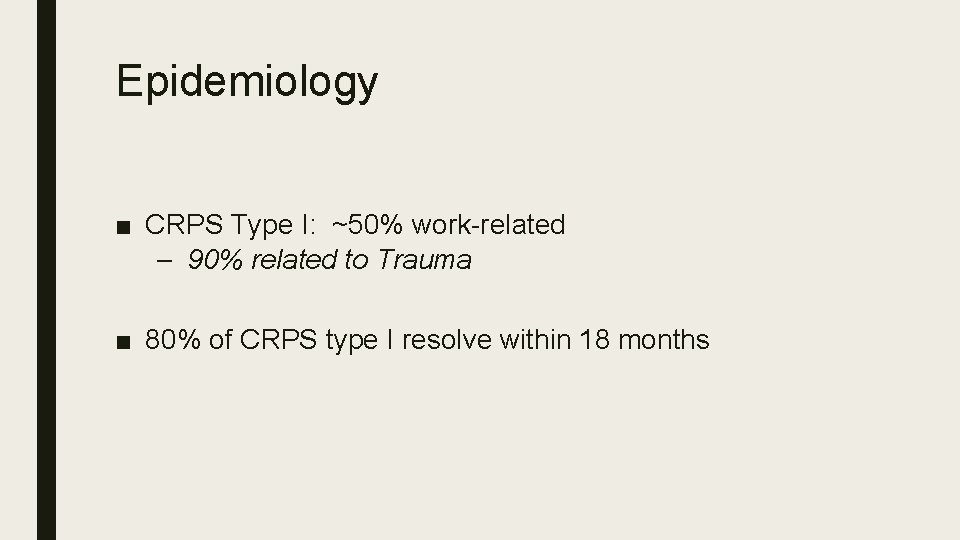
Epidemiology ■ CRPS Type I: ~50% work-related – 90% related to Trauma ■ 80% of CRPS type I resolve within 18 months
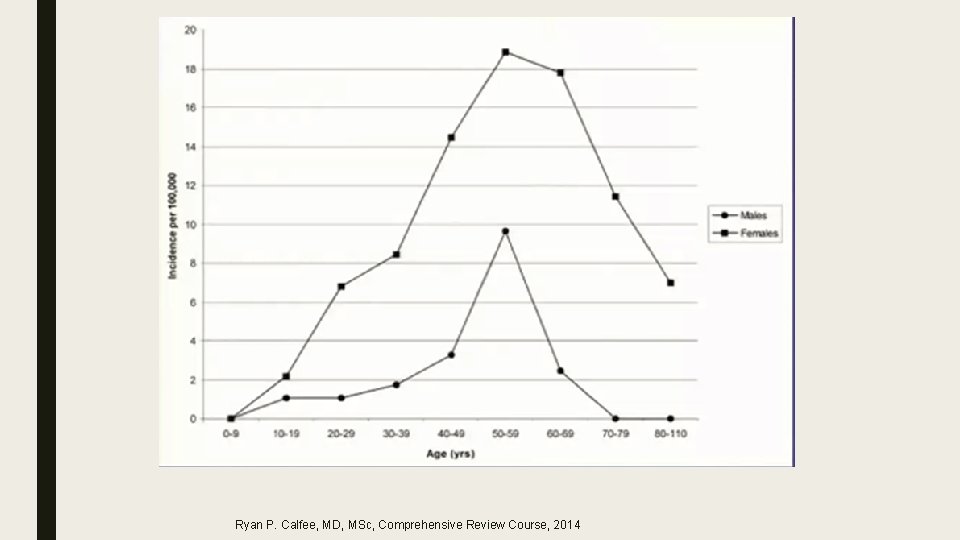
Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
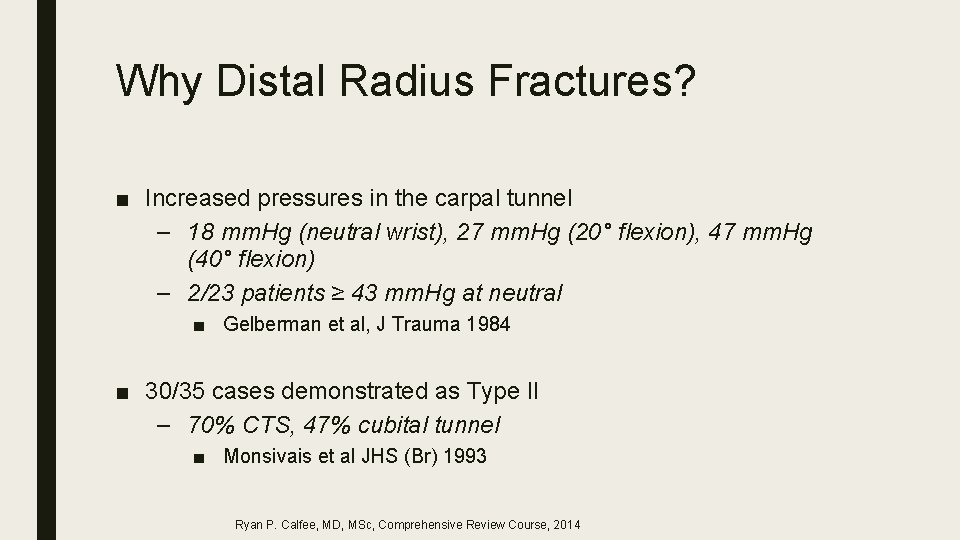
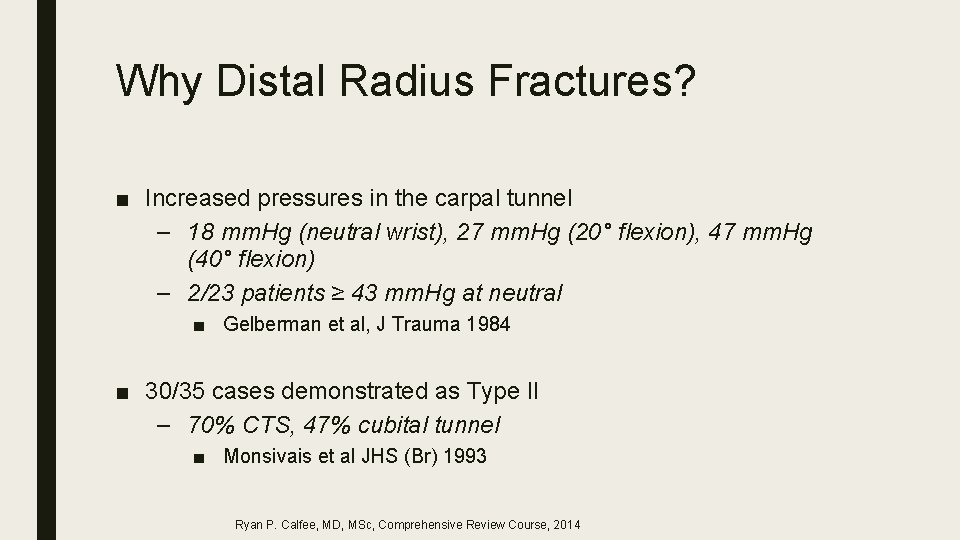
Why Distal Radius Fractures? ■ Increased pressures in the carpal tunnel – 18 mm. Hg (neutral wrist), 27 mm. Hg (20° flexion), 47 mm. Hg (40° flexion) – 2/23 patients ≥ 43 mm. Hg at neutral ■ Gelberman et al, J Trauma 1984 ■ 30/35 cases demonstrated as Type II – 70% CTS, 47% cubital tunnel ■ Monsivais et al JHS (Br) 1993 Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
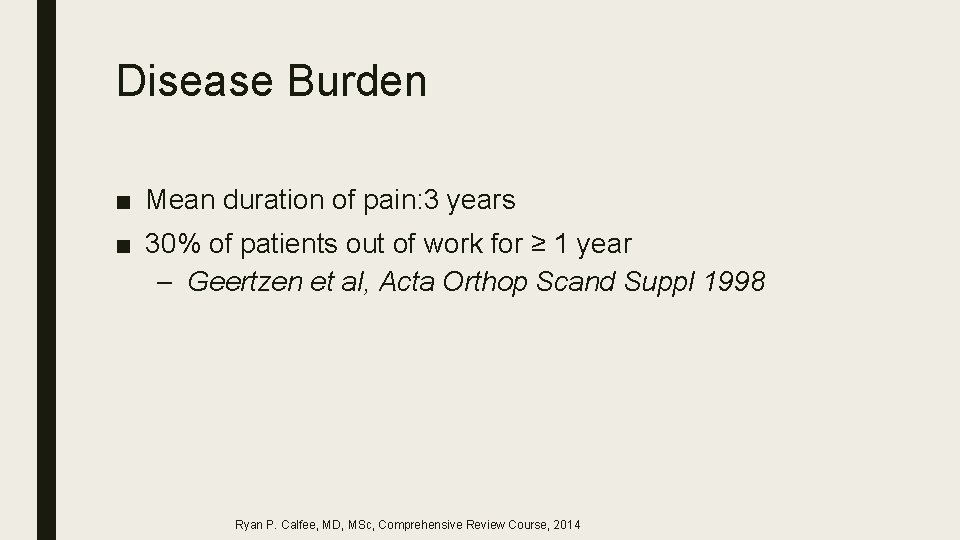
Disease Burden ■ Mean duration of pain: 3 years ■ 30% of patients out of work for ≥ 1 year – Geertzen et al, Acta Orthop Scand Suppl 1998 Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
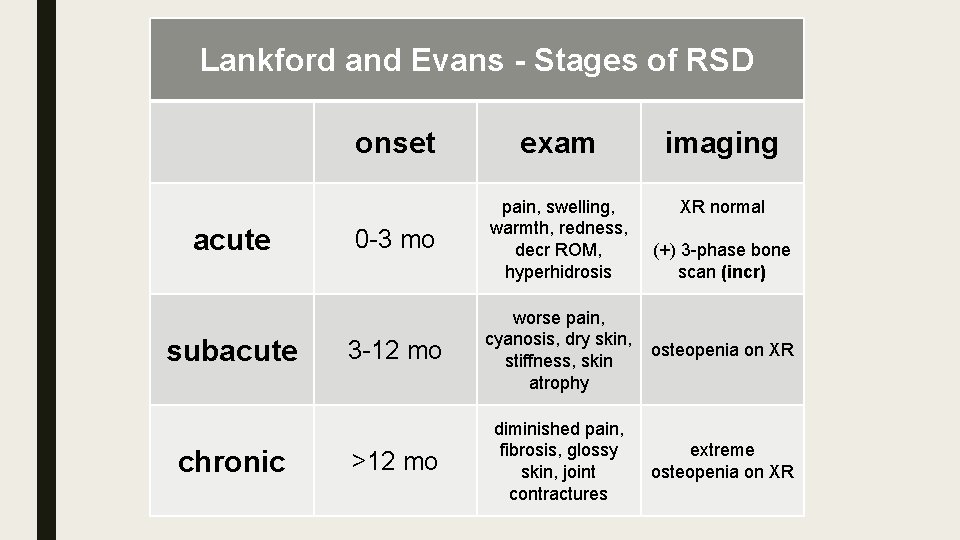
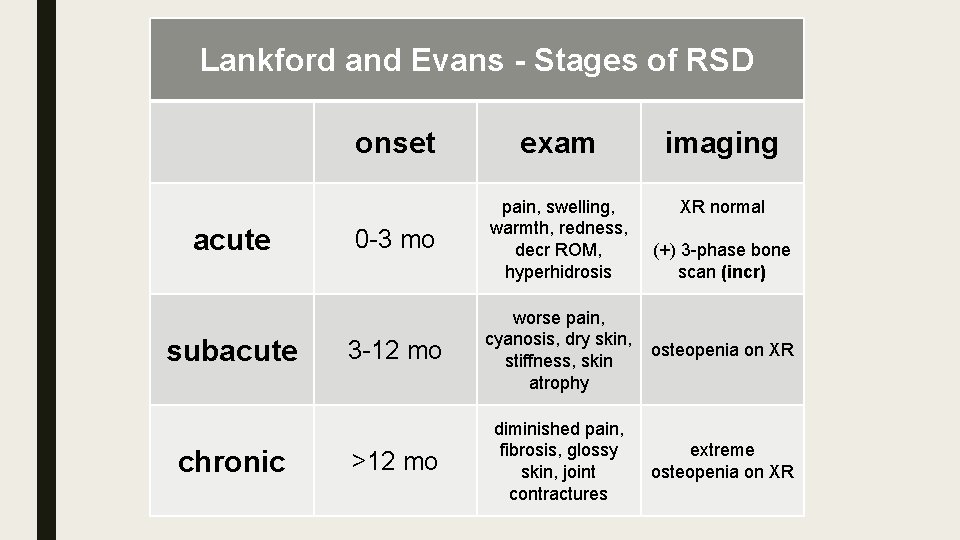
Lankford and Evans - Stages of RSD acute subacute chronic onset exam imaging XR normal 0 -3 mo pain, swelling, warmth, redness, decr ROM, hyperhidrosis 3 -12 mo worse pain, cyanosis, dry skin, stiffness, skin atrophy osteopenia on XR >12 mo diminished pain, fibrosis, glossy skin, joint contractures extreme osteopenia on XR (+) 3 -phase bone scan (incr)
Staging ■ Acute – Aching, burning, hyperemia ■ Dystrophic – Tissue thickening ■ Atrophic – Less pain, cool skin, contracture ■ No clear time-course Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Staging ■ Hot vs Cold ■ Others argue that when pain is gone there is no more CRPS – Compartment syndrome and Volkmann’s Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
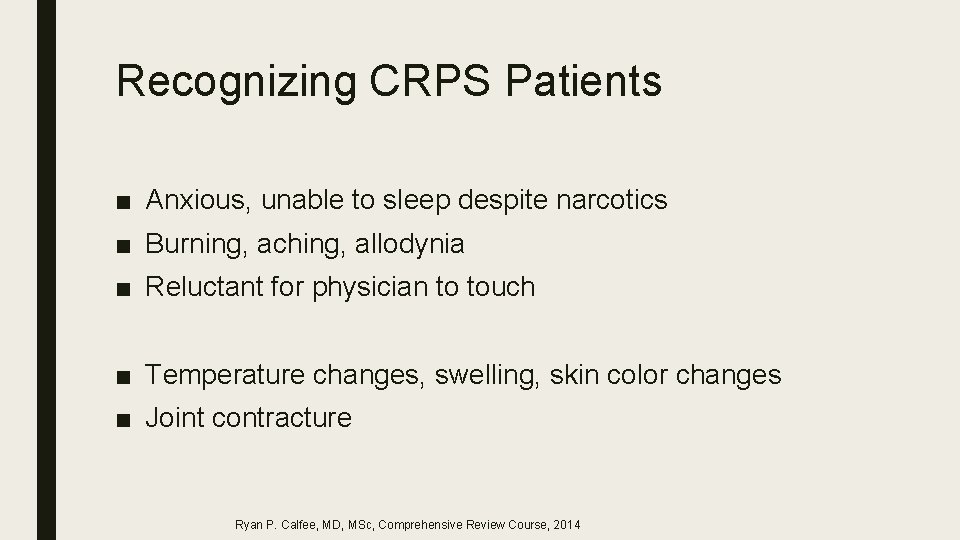
Recognizing CRPS Patients ■ Anxious, unable to sleep despite narcotics ■ Burning, aching, allodynia ■ Reluctant for physician to touch ■ Temperature changes, swelling, skin color changes ■ Joint contracture Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
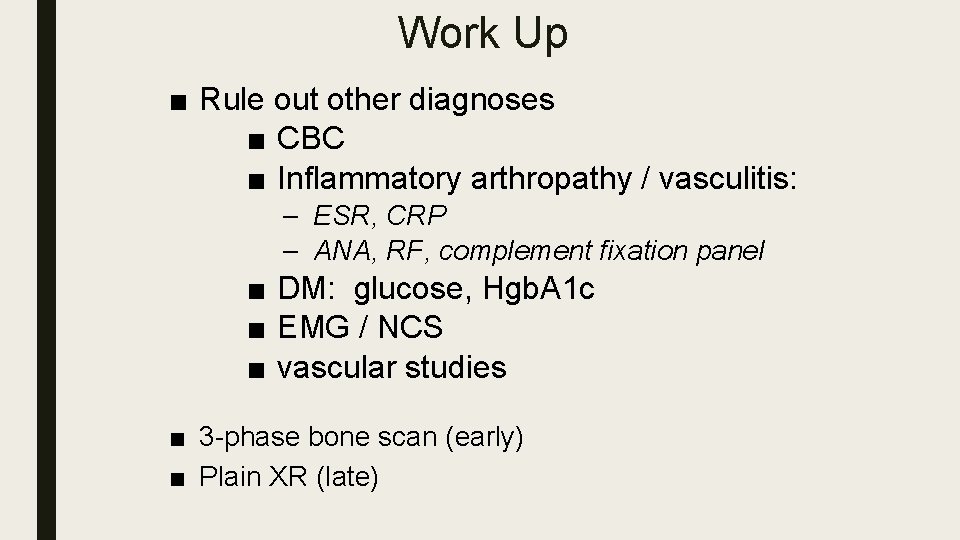
Differential Diagnosis ■ ■ diabetic, etc ■ ■ Post-traumatic ■ neuralgia ■ ■ anatomically defined territory ■ ■ CNS disorders ■ ■ Neuropathy ■ ■ stroke tumor MS trauma ■ Spinal cord ■ Radiculopathy Plexopathy Nerve entrapment Vasculitis / vascular Psychiatric Toxic Infectious ■ viral ■ fungal ■ Lyme disease ■ Iatrogenic
Work Up ■ Rule out other diagnoses ■ CBC ■ Inflammatory arthropathy / vasculitis: – ESR, CRP – ANA, RF, complement fixation panel ■ DM: glucose, Hgb. A 1 c ■ EMG / NCS ■ vascular studies ■ 3 -phase bone scan (early) ■ Plain XR (late)
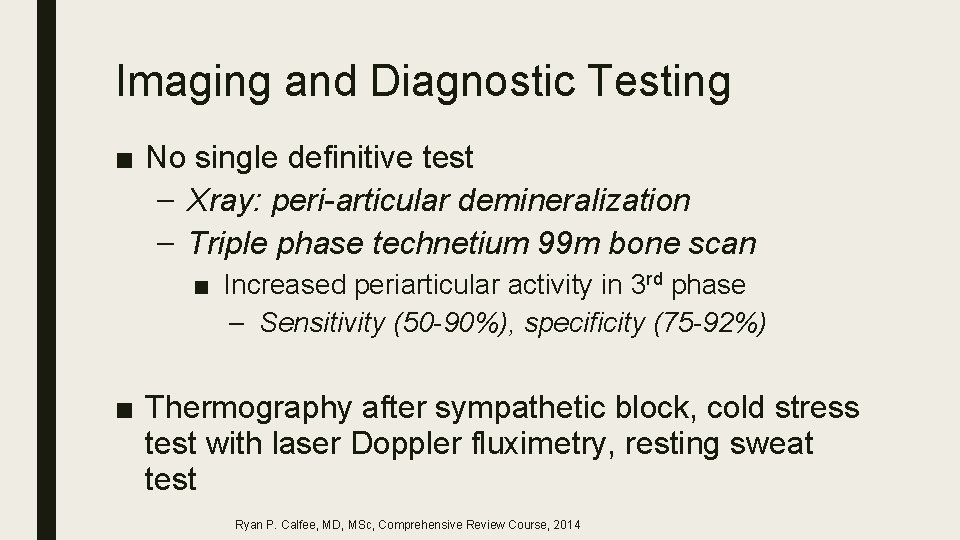
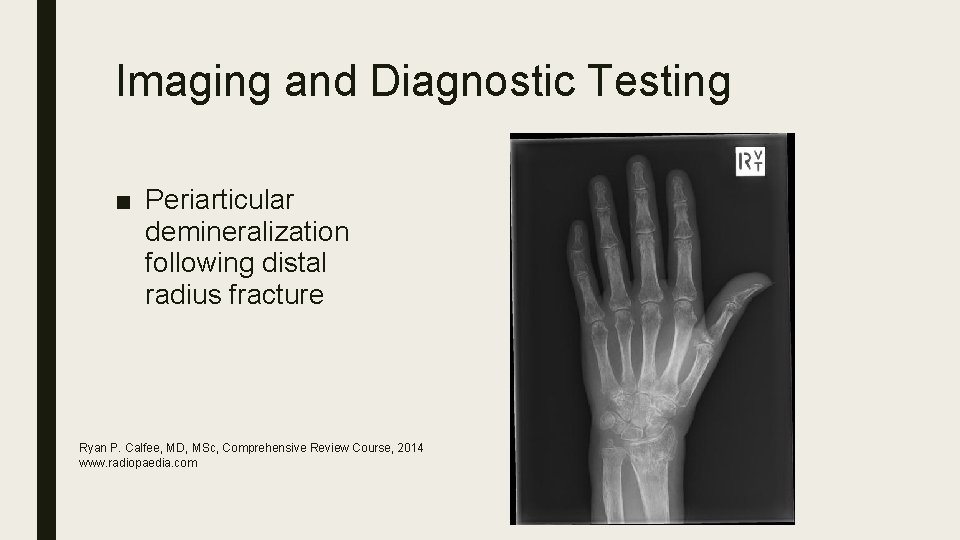
Imaging and Diagnostic Testing ■ No single definitive test – Xray: peri-articular demineralization – Triple phase technetium 99 m bone scan ■ Increased periarticular activity in 3 rd phase – Sensitivity (50 -90%), specificity (75 -92%) ■ Thermography after sympathetic block, cold stress test with laser Doppler fluximetry, resting sweat test Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
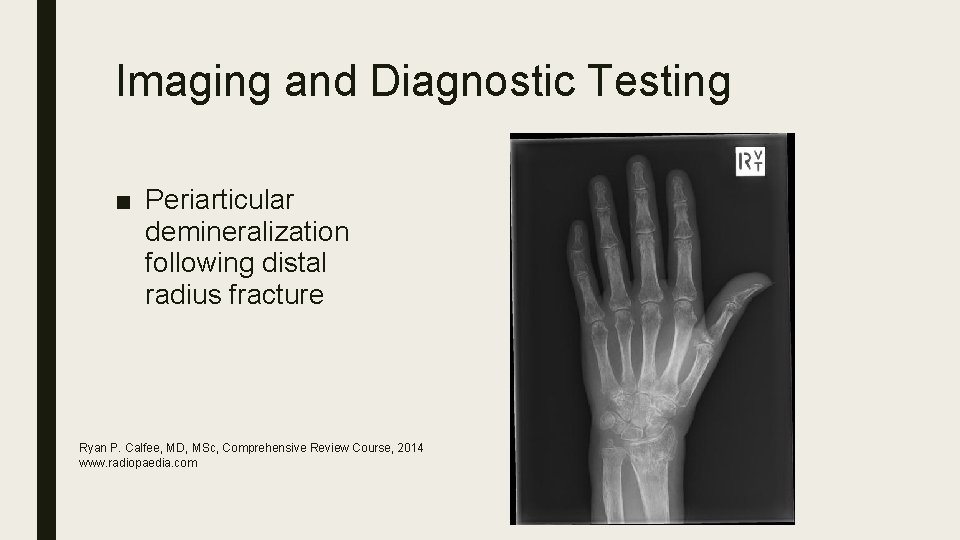
Imaging and Diagnostic Testing ■ Periarticular demineralization following distal radius fracture Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014 www. radiopaedia. com
Sympathetic Mediated? ■ Diagnostic stellate ganglion block or oral sympatholytic challenge – Blocks must produce Horner’s, increased extremity peripheral venous engorgement ■ Influence of sympathetic system in a patient may vary over time Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
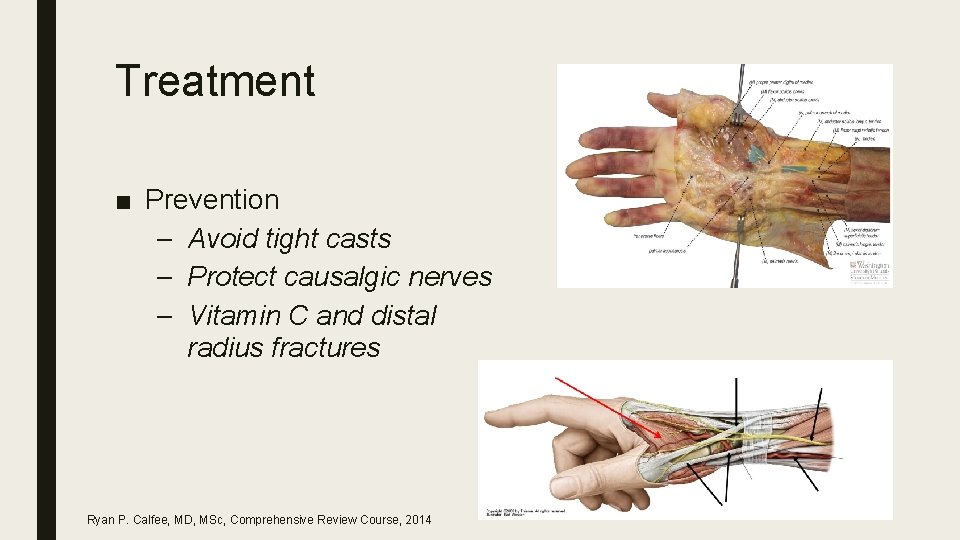
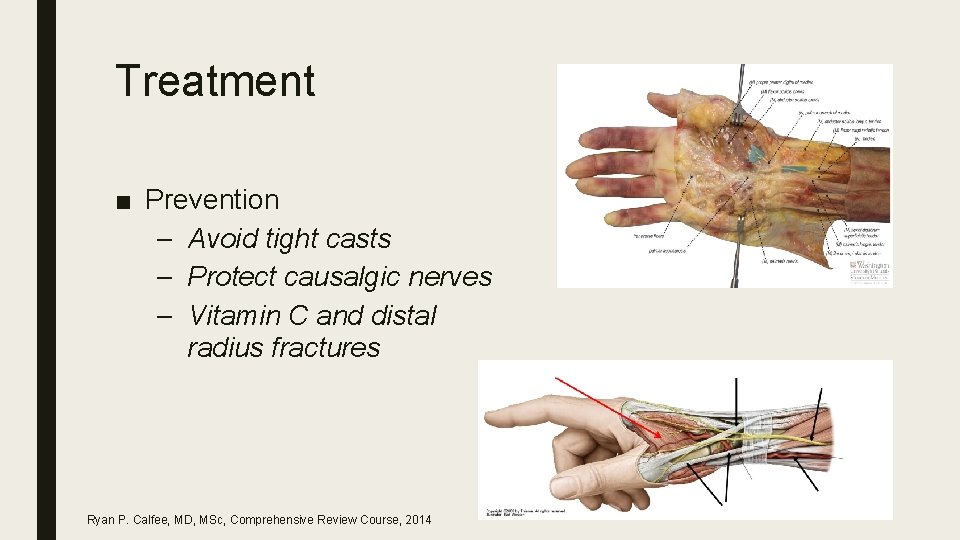
Treatment ■ Prevention – Avoid tight casts – Protect causalgic nerves – Vitamin C and distal radius fractures Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
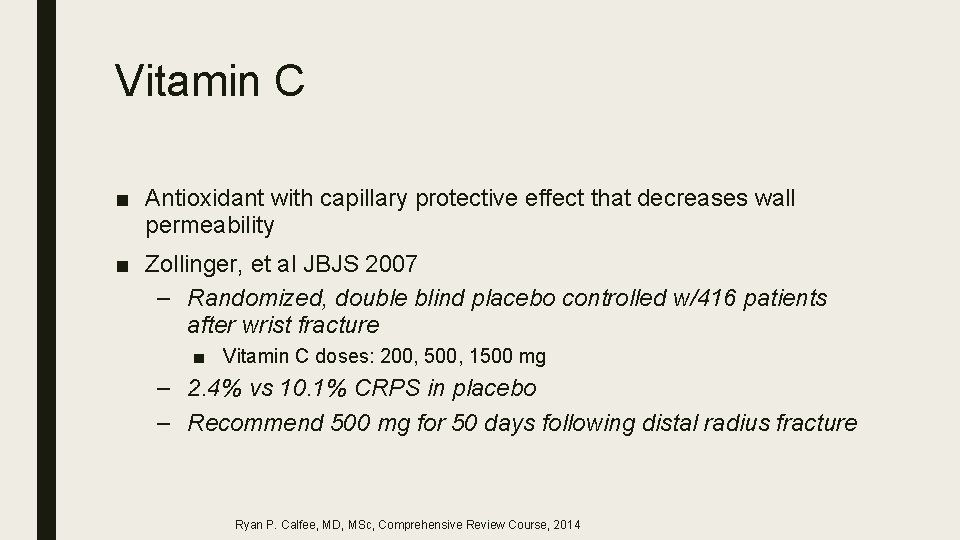
Vitamin C ■ Antioxidant with capillary protective effect that decreases wall permeability ■ Zollinger, et al JBJS 2007 – Randomized, double blind placebo controlled w/416 patients after wrist fracture ■ Vitamin C doses: 200, 500, 1500 mg – 2. 4% vs 10. 1% CRPS in placebo – Recommend 500 mg for 50 days following distal radius fracture Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Vitamin C ■ Besse, et al F&A Surg, 2009 – 2 groups (total 420 patiens) w/ and w/o Vit C ■ 1 gram post op daily for 45 days ■ 1. 7% incidence vs 9. 6 incidence CRPS ■ Is Vitamin C totally safe? Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
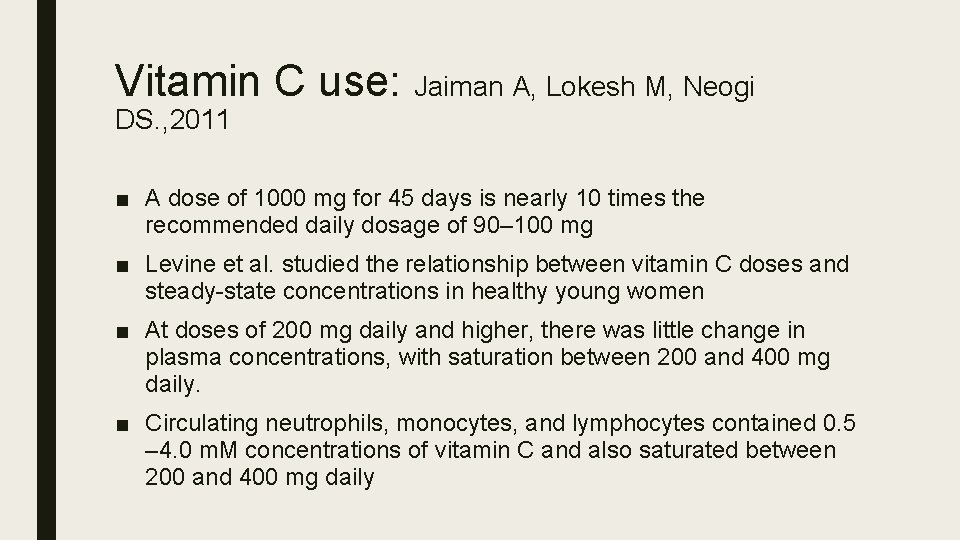
Vitamin C use: Jaiman A, Lokesh M, Neogi DS. , 2011 ■ A dose of 1000 mg for 45 days is nearly 10 times the recommended daily dosage of 90– 100 mg ■ Levine et al. studied the relationship between vitamin C doses and steady-state concentrations in healthy young women ■ At doses of 200 mg daily and higher, there was little change in plasma concentrations, with saturation between 200 and 400 mg daily. ■ Circulating neutrophils, monocytes, and lymphocytes contained 0. 5 – 4. 0 m. M concentrations of vitamin C and also saturated between 200 and 400 mg daily
Vitamin C use ■ In a study by Taylor and Curhan, participants consuming 1000 mg/day or more of vitamin C excreted 6. 8 mg/day more urinary oxalate than participants consuming <90 mg/day (P trend < 0. 001) ■ Multivariate relative risk of kidney stone formation for men consuming 1000 mg or greater of vitamin C per day was 41% higher than those consuming less than the recommended dietary allowance of 90 mg/day.
Vitamin C use: Besse JL. 2012 ■ Our study used a 1000 mg Vitamin C protocol for Foot and Ankle surgery, it is logical for us to recommend this dose. ■ For six years, our orthopaedic and traumatologic department has used this protocol for all operations. We can estimate that more than 10, 000 patients received this 1000 mg Vitamin C prevention and we never observed any adverse effects. We only checked history of (uric acid) kidney stone. ■ However I agree that in light of the last Zollinger publication [4], 500 mg of Vitamin C is probably enough.

Treatment ■ As a hand surgeon the greatest impact is to: 1. Make the diagnosis 2. Distinguish type II disease and decompress involved nerves Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014

Treatment ■ Ideally incorporates a multidisciplinary team: – Hand surgeon – Primary medical providers – Pain specialists – Therapists – Psychologists – Social workers Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Treatment 1. OT and PT – Minimize pain and edema – Maximize comfortable mobility 2. Nerve stimulation (PNS/CNS) – Gate theory ■ Geurts et al, Neuromodulation 2013 3. Nerve blocks (esp. sympathetics) 4. Medication (None FDA approved) – Antidepressants, anticonvulsants, antiadrenergic, steroids, bisphosponates Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014

Treatment Options ■ Corticosteroids ■ CCBs ■ Calcium-reg drugs ■ Beta blockers ■ Opioids ■ Oral sympatholytics ■ NSAIDs ■ Clonidine ■ TCAs / SSRIs ■ Sympathetic blocks ■ Sodium channel blockers ■ Ketamine ■ GABA agonists ■ Gabapentin ■ Spinal cord stimulator ■ PT/OT ■ Psych
Treatment ■ Bisphophonates – Class of drugs used to treat bone loss. ■ Calcium regulating drugs – in refractory cases ■ Clodronate (300 mg) daily IV for 10 days – pain, swelling, movement range in acute CRPS ■ Alendronate (7. 5 mg) once IV ‐ pain, swelling, movement range in acute CRPS ■ Pamidronate 60 mg IV Forouzanfar T, Koke AJ, Kleef M van, Weber WE. Treatment of complex regional pain syndrome type I. Eur J Pain 2002; 6(2): 105‐ 22. Adami S, Fossaluzza V, Gatti D, Fracassi E, Braga V. Bisphonate therapy of reflex sympathetic dystrophy syndrome. Ann Rheum Dis 1997; 56(3): 201‐ 4.
Treatment ■ Ketamine – CRPS ‐ activation and proliferation NMDA of receptors – Strong NMDA Receptor blocker – One of the safest anesthetic drugs – Powerful analgesic even at low doses – Poor absorption when administered orally. – Effective as IV or submucosal (Troche)
Ketamine
![Ketamine Psychonautics from the Greek ψυχή psychē soul spirit or mind and ναύτης Ketamine ■ Psychonautics (from the Greek ψυχή psychē ["soul", "spirit" or "mind"] and ναύτης](https://slidetodoc.com/presentation_image_h/049cd755f98e5d84be36fe49936cb773/image-57.jpg)
Ketamine ■ Psychonautics (from the Greek ψυχή psychē ["soul", "spirit" or "mind"] and ναύτης naútēs ["sailor" or "navigator"] — "a sailor of the soul") refers both to a methodology for describing and explaining the subjective effects of altered states of consciousness, including those induced by meditation or mind-altering substances.
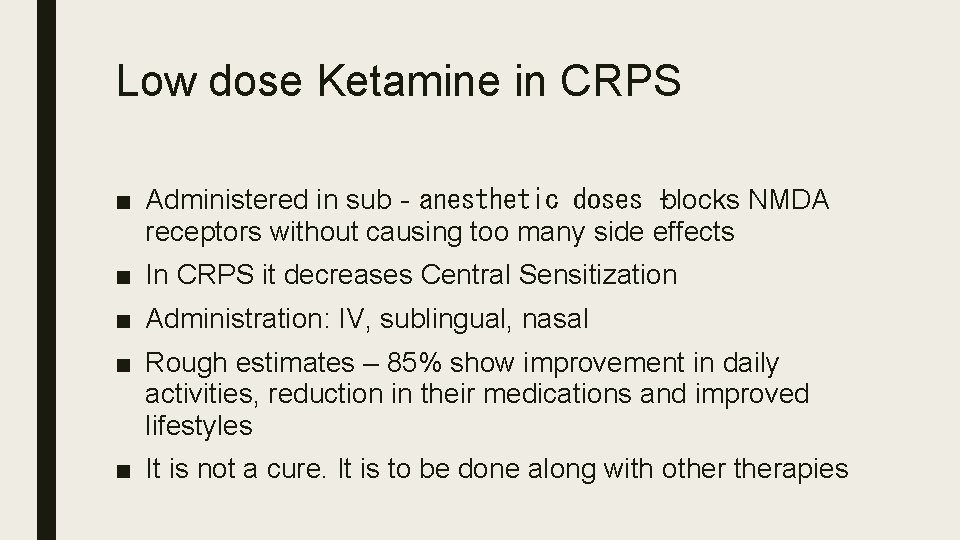
Low dose Ketamine in CRPS ■ Administered in sub‐anesthetic doses –blocks NMDA receptors without causing too many side effects ■ In CRPS it decreases Central Sensitization ■ Administration: IV, sublingual, nasal ■ Rough estimates – 85% show improvement in daily activities, reduction in their medications and improved lifestyles ■ It is not a cure. It is to be done along with otherapies
N‐ Acetyl Cysteine (NAC) ■ Useful for cold allodynia ■ N‐Acetylcysteine 600 mg three times a day for three months Perez RS, Zuurmond WW, Bezemer PD, Kuik DJ, Loenen AC van, Lange JJ de, et al. The treatment of complex regional pain syndrome type. I with free radical scavengers: a randomized controlled study. Pain 2003; 102(3): 297‐ 307
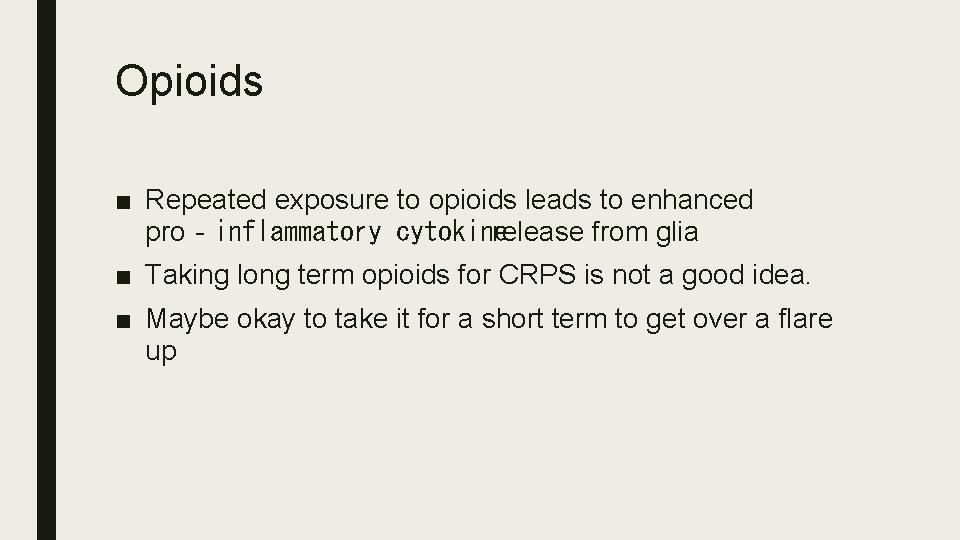
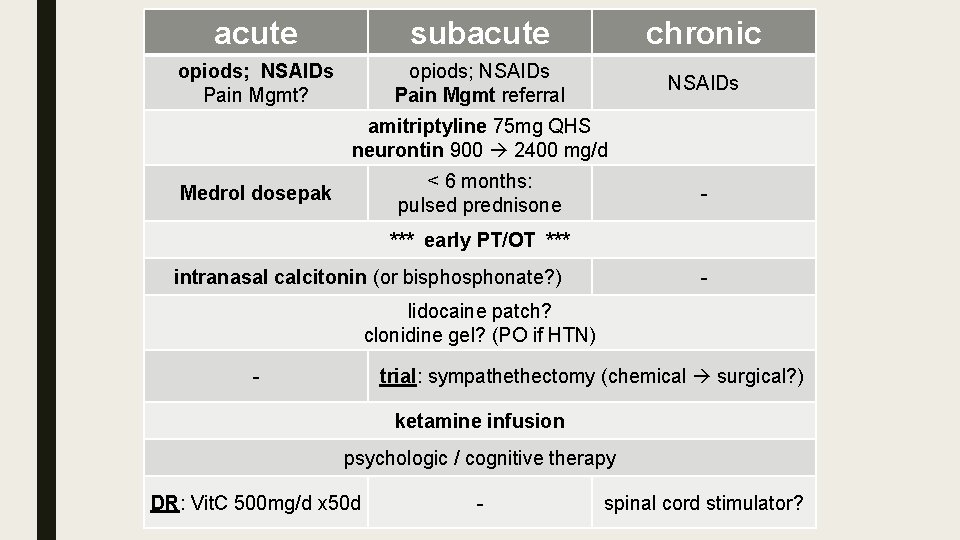
Opioids ■ Repeated exposure to opioids leads to enhanced pro‐inflammatory cytokine release from glia ■ Taking long term opioids for CRPS is not a good idea. ■ Maybe okay to take it for a short term to get over a flare up
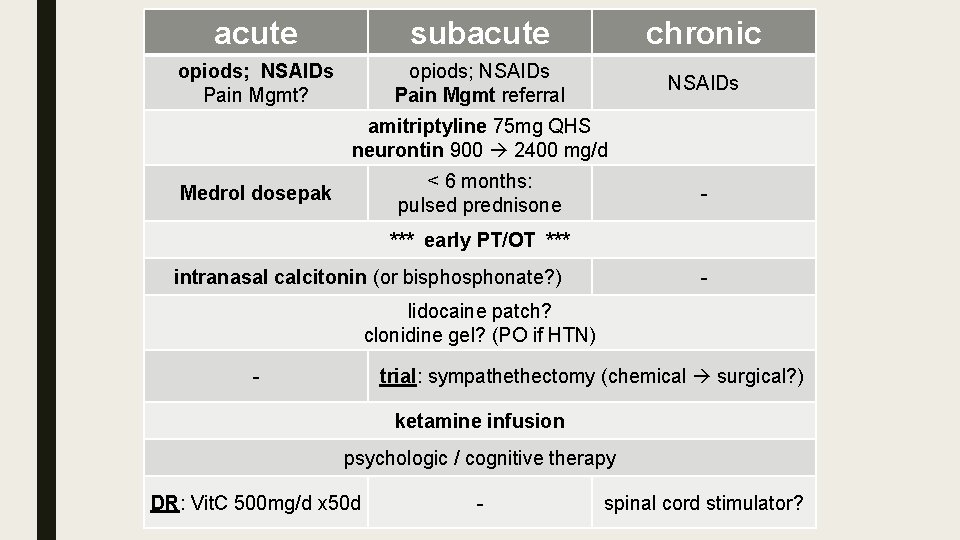
acute subacute chronic opiods; NSAIDs Pain Mgmt? opiods; NSAIDs Pain Mgmt referral NSAIDs amitriptyline 75 mg QHS neurontin 900 2400 mg/d < 6 months: pulsed prednisone Medrol dosepak - *** early PT/OT *** intranasal calcitonin (or bisphonate? ) - lidocaine patch? clonidine gel? (PO if HTN) trial: sympathethectomy (chemical surgical? ) - ketamine infusion psychologic / cognitive therapy DR: Vit. C 500 mg/d x 50 d - spinal cord stimulator?
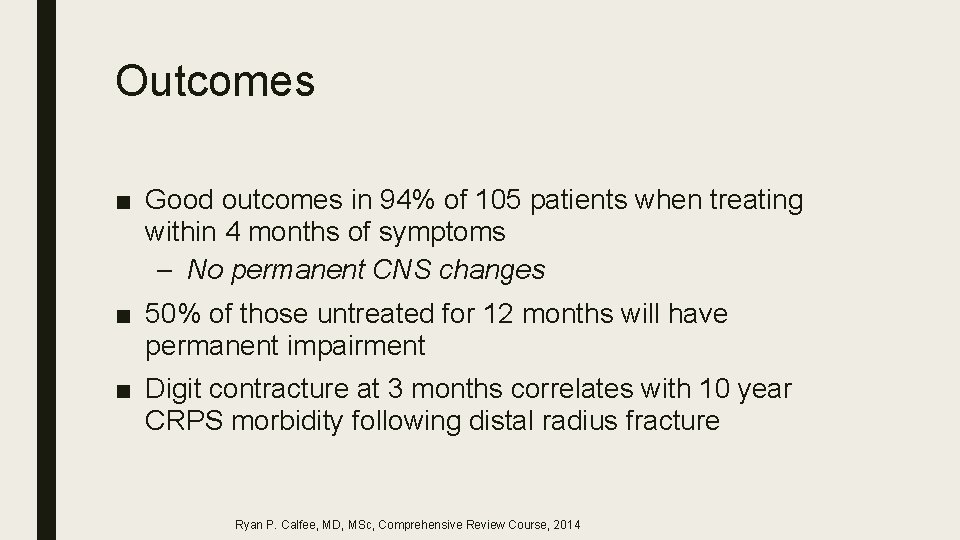
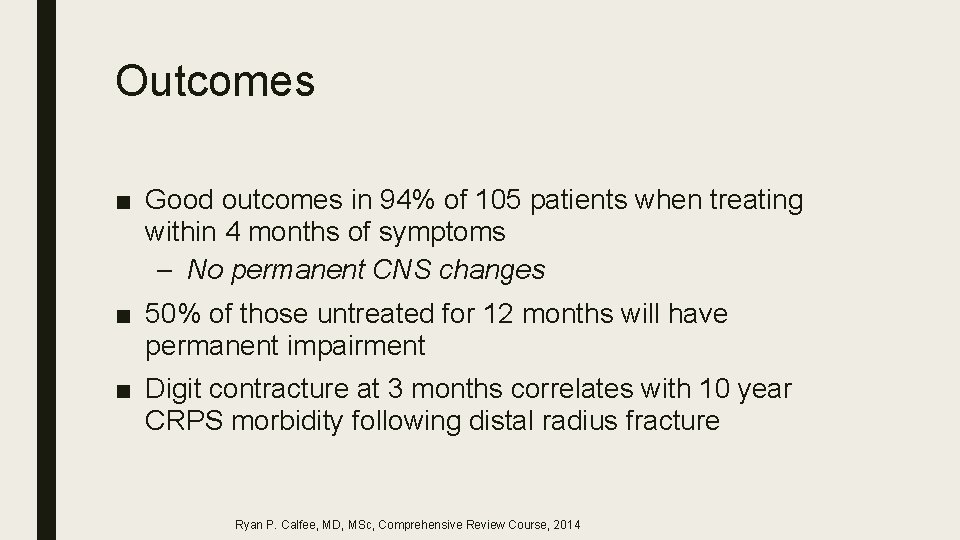
Outcomes ■ Good outcomes in 94% of 105 patients when treating within 4 months of symptoms – No permanent CNS changes ■ 50% of those untreated for 12 months will have permanent impairment ■ Digit contracture at 3 months correlates with 10 year CRPS morbidity following distal radius fracture Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
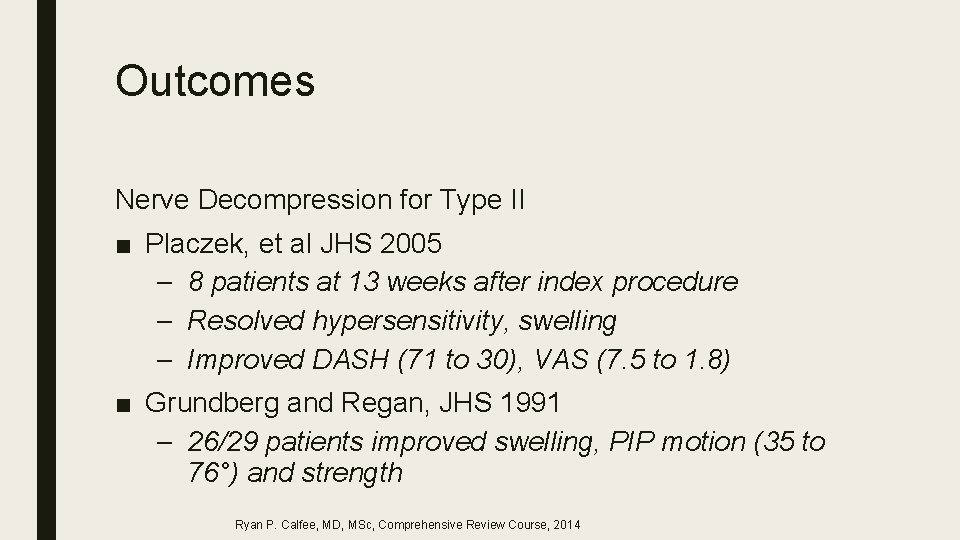
Outcomes Nerve Decompression for Type II ■ Placzek, et al JHS 2005 – 8 patients at 13 weeks after index procedure – Resolved hypersensitivity, swelling – Improved DASH (71 to 30), VAS (7. 5 to 1. 8) ■ Grundberg and Regan, JHS 1991 – 26/29 patients improved swelling, PIP motion (35 to 76°) and strength Ryan P. Calfee, MD, MSc, Comprehensive Review Course, 2014
Surgery after CRPS ■ Perioperative stellate ganglion block may reduce recurrence – Recurrence 10% vs 72% in 100 patients ■ Reuben et al, 2000
Summary ■ CRPS is likely the end result of a complex interaction of multiple inter-related nervous system changes ■ CRPS leads to marked and prolonged morbidity ■ Vitamin C is effective for prevention of CRPS associated with distal radius fracture
Summary ■ Early treatment of CRPS optimizes outcomes ■ Type II CRPS should be treated with nerve decompression

Thank you !
 Madpain
Madpain Tender nipples sign of early pregnancy
Tender nipples sign of early pregnancy Pms or pregnancy
Pms or pregnancy Package diagram
Package diagram Organization
Organization Unsent message to aydin
Unsent message to aydin Nazmi aydın
Nazmi aydın Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Aydin marine
Aydin marine Sevil aydın
Sevil aydın Aydin bal
Aydin bal Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Nizamettin aydin
Nizamettin aydin Aydın başar
Aydın başar Aydın bir türk kadınıyım
Aydın bir türk kadınıyım Aydın kekemelik merkezi
Aydın kekemelik merkezi Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Aydın kendirci
Aydın kendirci Nizamettin aydin
Nizamettin aydin Bushra hasan
Bushra hasan Sinan aydın mali müşavir
Sinan aydın mali müşavir Psychodynamic and psychoanalytic theory difference
Psychodynamic and psychoanalytic theory difference Ghon complex and ranke complex
Ghon complex and ranke complex Sublimation defense mechanism
Sublimation defense mechanism Simple compound complex rules
Simple compound complex rules Freud complexes
Freud complexes Pauline and bruno have a big argument
Pauline and bruno have a big argument Pqrstu pain assessment
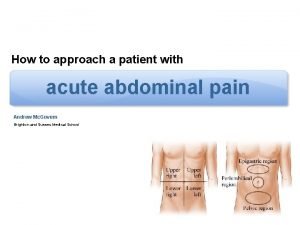
Pqrstu pain assessment Ruq
Ruq Detaching from emotional pain grounding
Detaching from emotional pain grounding Vena mediana cubiti
Vena mediana cubiti Ac pain
Ac pain Npass tool
Npass tool Total pain
Total pain Brief pain inventory
Brief pain inventory Canadian c spine rules
Canadian c spine rules Dr lascarides pain management
Dr lascarides pain management Pain management ehr
Pain management ehr Pqrst pain assessment
Pqrst pain assessment Sclerotogenous pain patterns
Sclerotogenous pain patterns Dr gilbertha st rose
Dr gilbertha st rose Afebrile vss
Afebrile vss Nips pain scale
Nips pain scale Peripheral sensitization
Peripheral sensitization Searing pain definition
Searing pain definition Au bon pain history
Au bon pain history Gallblader pain
Gallblader pain Laporan kasus low back pain
Laporan kasus low back pain Nccpc pain scale
Nccpc pain scale Blood shadow stays on the street
Blood shadow stays on the street Romeo and juliet act 1 test answer key
Romeo and juliet act 1 test answer key Referred pain
Referred pain Intertragal notch pain
Intertragal notch pain Le mone
Le mone Pain perdu histoire
Pain perdu histoire Intro to breastfeeding
Intro to breastfeeding Lodcraft history taking
Lodcraft history taking Pncreas pain
Pncreas pain Pijnmodel loeser
Pijnmodel loeser Vision gives pain a purpose
Vision gives pain a purpose Types of pain
Types of pain Apparail digestif
Apparail digestif Heel pain soccer
Heel pain soccer Iu pain management
Iu pain management Finnegan score
Finnegan score Pain reassessment
Pain reassessment D
D