Comparison of hypersensitivity reactions reaction Lymphocyte Effector cells


- Slides: 32
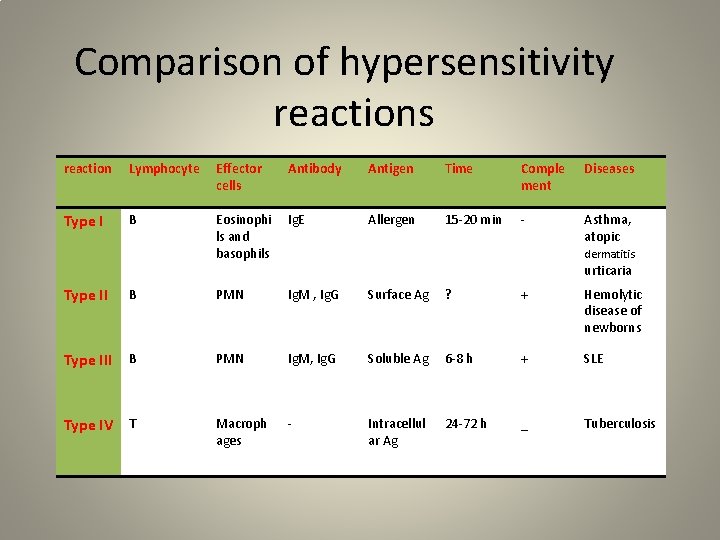
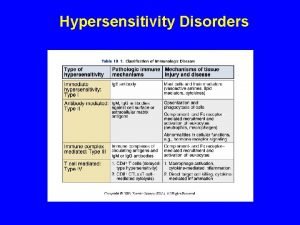
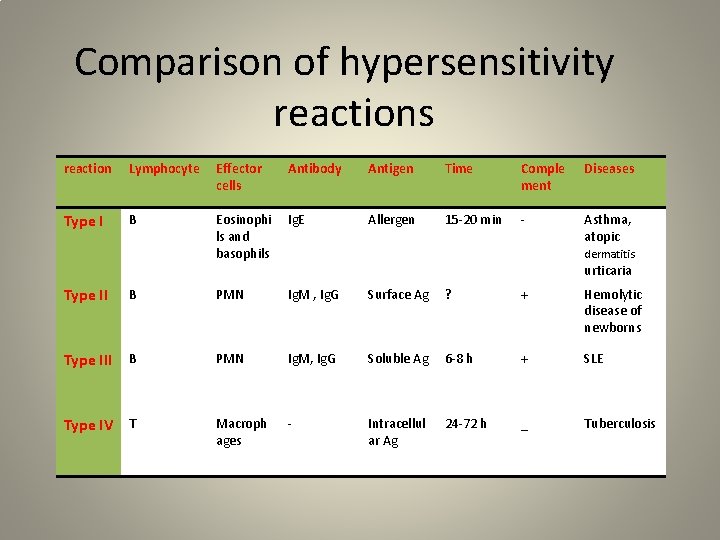
Comparison of hypersensitivity reactions reaction Lymphocyte Effector cells Antibody Antigen Time Comple ment Diseases Type I B Eosinophi ls and basophils Ig. E Allergen 15 -20 min - Asthma, atopic dermatitis urticaria Type II B PMN Ig. M , Ig. G Surface Ag ? + Hemolytic disease of newborns Type III B PMN Ig. M, Ig. G Soluble Ag 6 -8 h + SLE Type IV T Macroph ages - Intracellul ar Ag 24 -72 h _ Tuberculosis
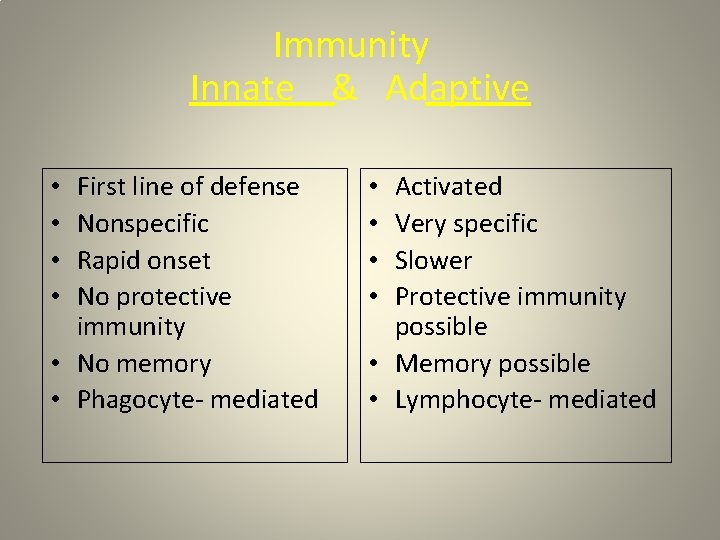
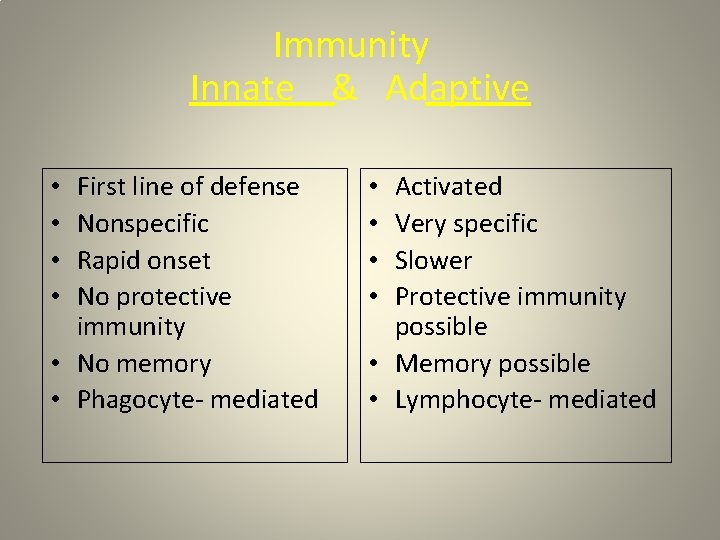
Immunity Innate & Adaptive First line of defense Nonspecific Rapid onset No protective immunity • No memory • Phagocyte- mediated • • Activated Very specific Slower Protective immunity possible • Memory possible • Lymphocyte- mediated • •
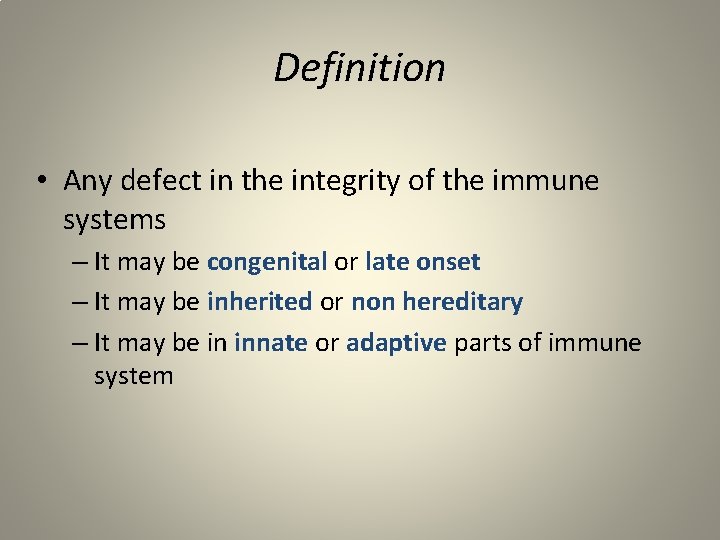
Definition • Any defect in the integrity of the immune systems – It may be congenital or late onset – It may be inherited or non hereditary – It may be in innate or adaptive parts of immune system
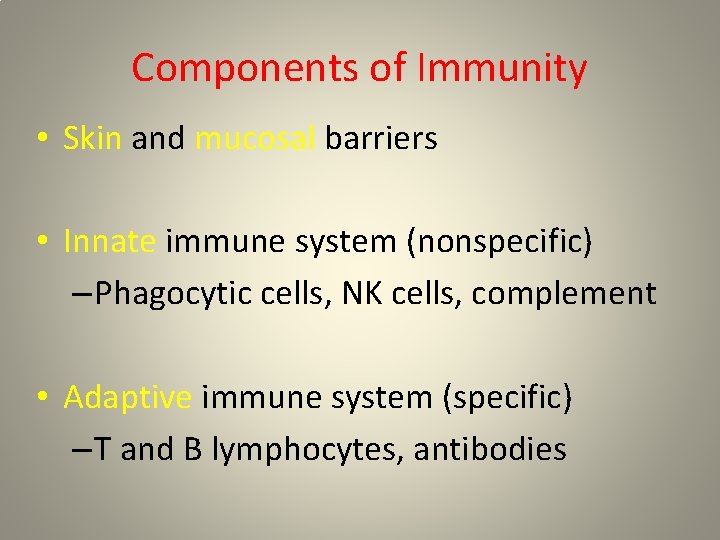
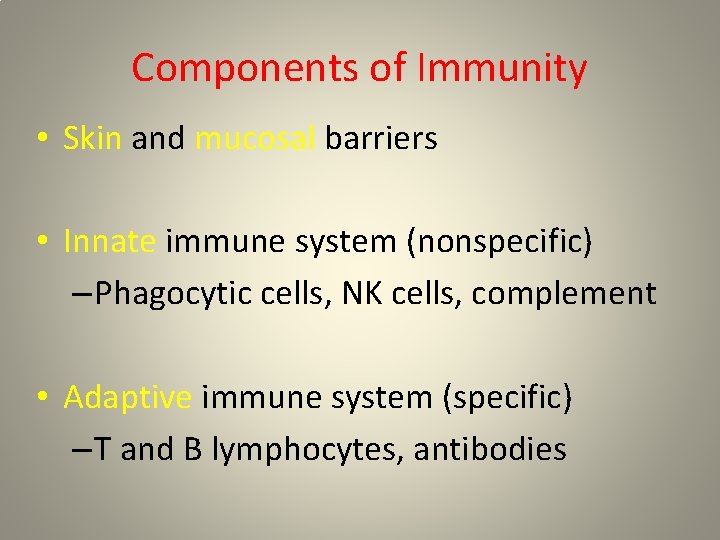
Components of Immunity • Skin and mucosal barriers • Innate immune system (nonspecific) – Phagocytic cells, NK cells, complement • Adaptive immune system (specific) – T and B lymphocytes, antibodies
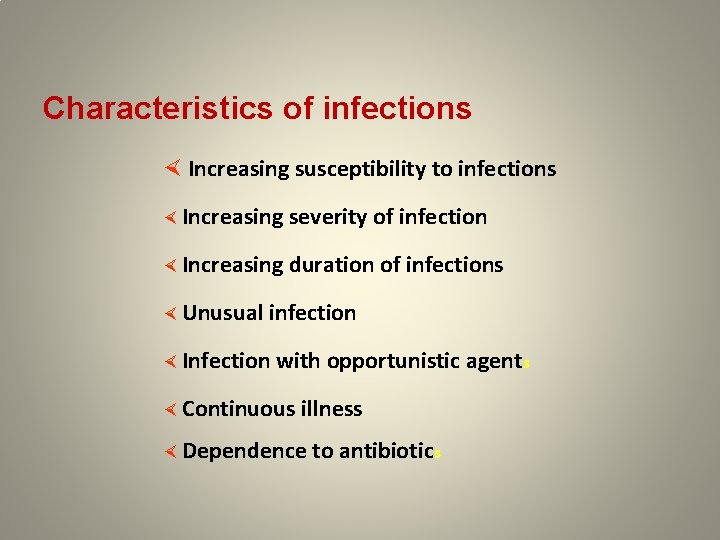
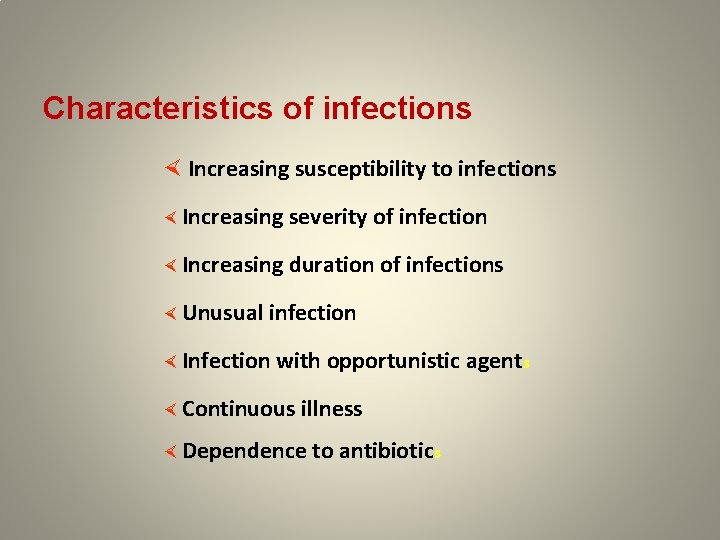
Characteristics of infections × Increasing susceptibility to infections × Increasing severity of infection × Increasing duration of infections × Unusual infection × Infection with opportunistic agents × Continuous illness × Dependence to antibiotics
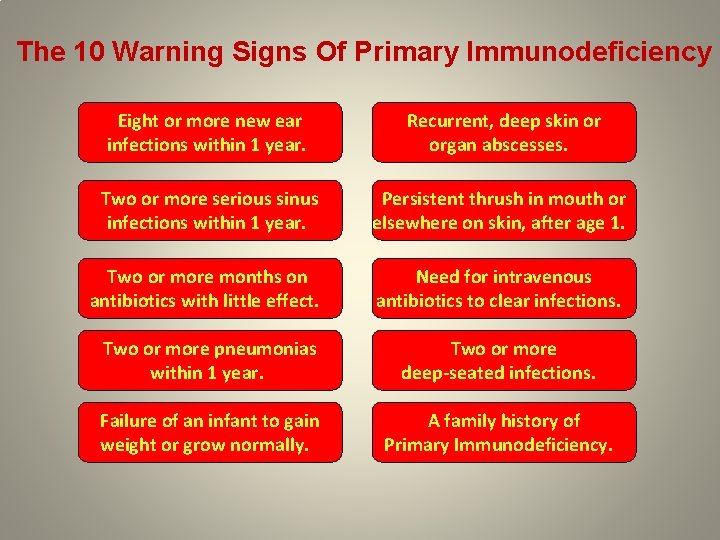
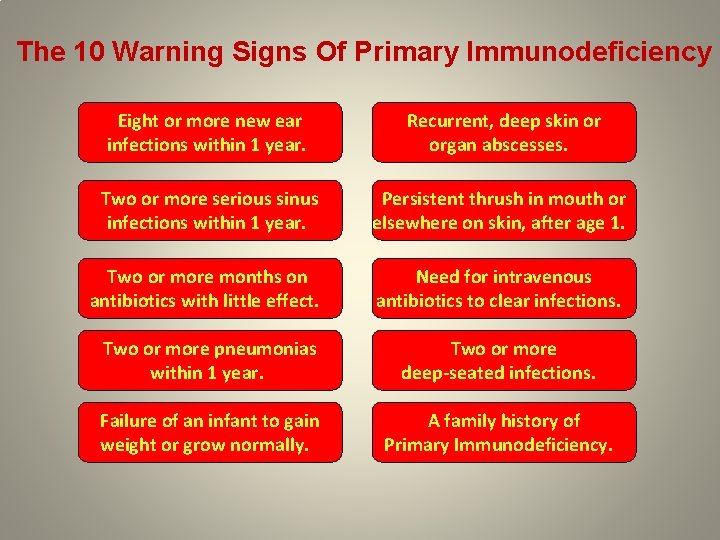
The 10 Warning Signs Of Primary Immunodeficiency Eight or more new ear infections within 1 year. Recurrent, deep skin or organ abscesses. Two or more serious sinus infections within 1 year. Persistent thrush in mouth or elsewhere on skin, after age 1. Two or more months on antibiotics with little effect. Need for intravenous antibiotics to clear infections. Two or more pneumonias within 1 year. Two or more deep-seated infections. Failure of an infant to gain weight or grow normally. A family history of Primary Immunodeficiency.
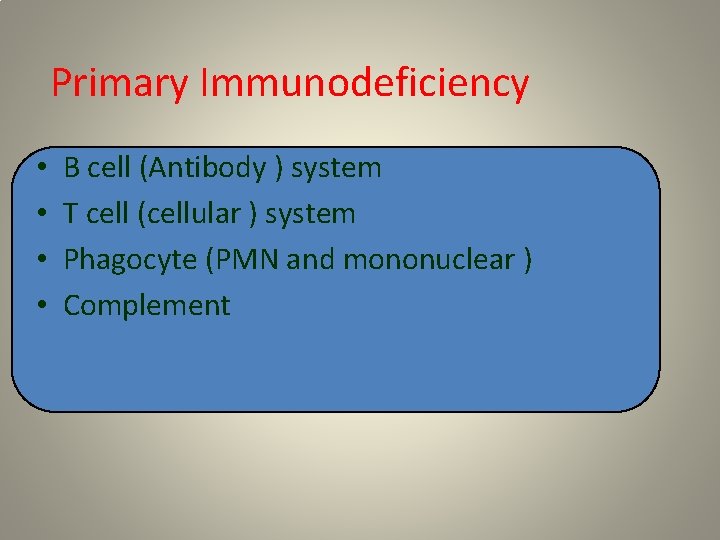
Primary Immunodeficiency • • B cell (Antibody ) system T cell (cellular ) system Phagocyte (PMN and mononuclear ) Complement
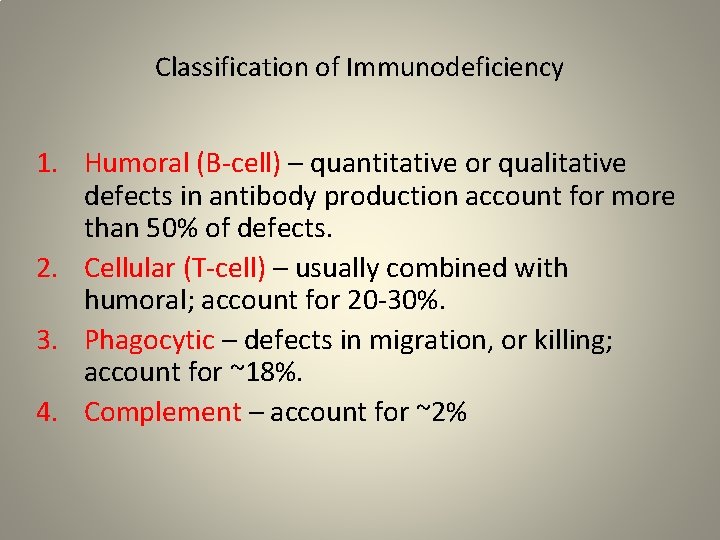
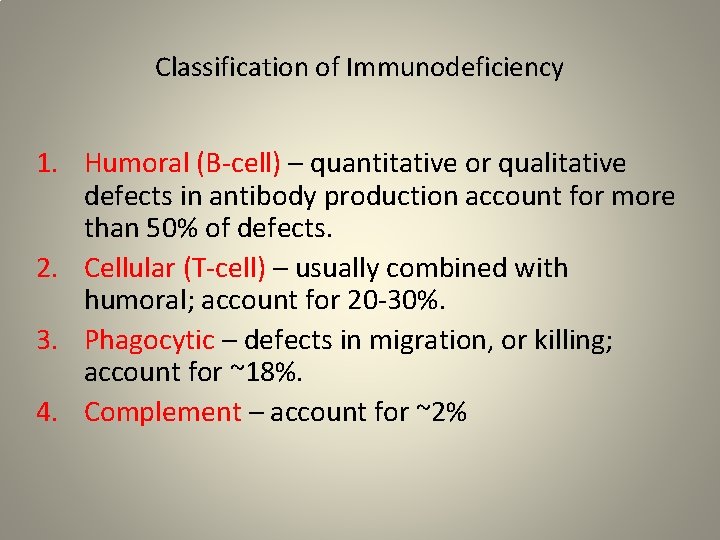
Classification of Immunodeficiency 1. Humoral (B-cell) – quantitative or qualitative defects in antibody production account for more than 50% of defects. 2. Cellular (T-cell) – usually combined with humoral; account for 20 -30%. 3. Phagocytic – defects in migration, or killing; account for ~18%. 4. Complement – account for ~2%
About %40 of cases are diagnosed in the first year Another %40 by age 5 years Another %15 by age 16 Only %5 in adulthood About %10 of registered cases are adults Late-onset Patients exhibit CVID
• Common Risk Factors for Frequent Infections – Day-care, school – Second-hand smoke – Atopy – Anatomic abnormalities including ciliary defects – Retained foreign body – Gastroesophageal reflue – Cystic fibrosis
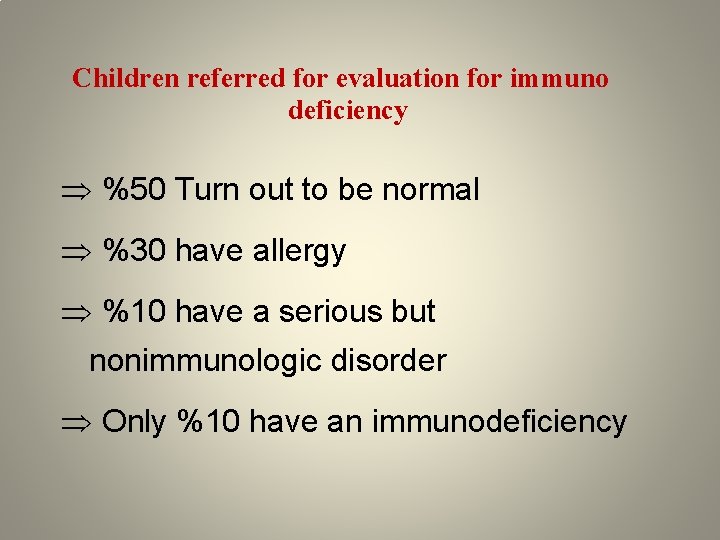
Children referred for evaluation for immuno deficiency %50 Turn out to be normal %30 have allergy %10 have a serious but nonimmunologic disorder Only %10 have an immunodeficiency
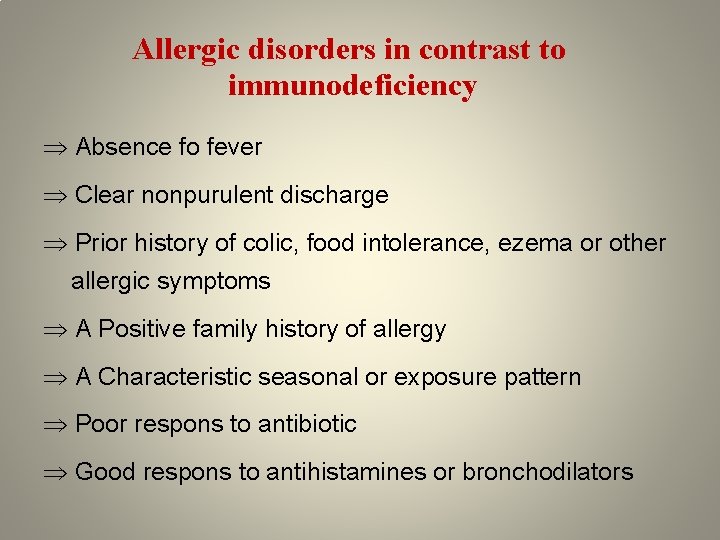
Allergic disorders in contrast to immunodeficiency Absence fo fever Clear nonpurulent discharge Prior history of colic, food intolerance, ezema or other allergic symptoms A Positive family history of allergy A Characteristic seasonal or exposure pattern Poor respons to antibiotic Good respons to antihistamines or bronchodilators
Approach for Suspected Immune Deficiency are as following:
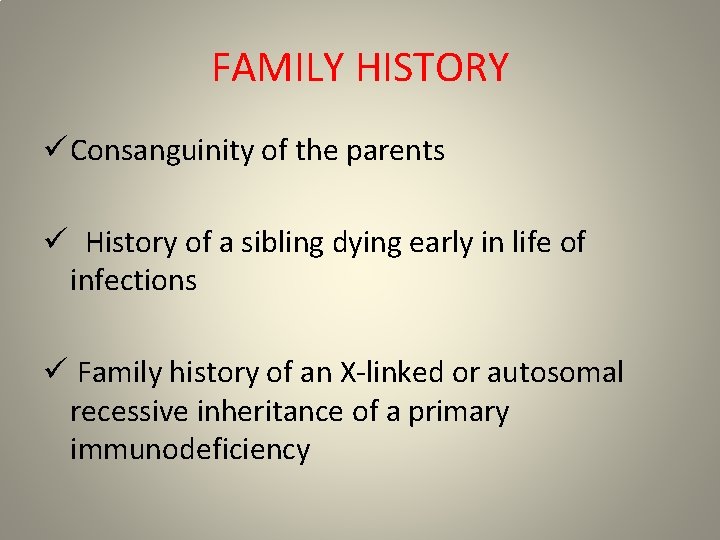
FAMILY HISTORY ü Consanguinity of the parents ü History of a sibling dying early in life of infections ü Family history of an X-linked or autosomal recessive inheritance of a primary immunodeficiency
GENERAL • Complete blood count, including hemoglobin, differential white blood cell count(ALC , ANC) and morphology, and platelet count, ESR • Radiographs to document infection in chest, sinus, mastoids, and long bones, if indicated by clinical history • Cultures, if appropriate
History Our Guide • Predominant B-Cell defects – Onset after maternal antibodies diminish, usually after 5 -7 mos, later childhood to adulthood. – Bacteria: strep, staph, H. flu; Campylobacter, enteroviruses, giardia, cryptosporidia – Recurrent sinopulmonary infections, chronic GI symptoms, malabsorption, arthritis, viral meningoencephalitis – Autoimmunity, lymphoreticular malignancy; thymoma, lymphoma
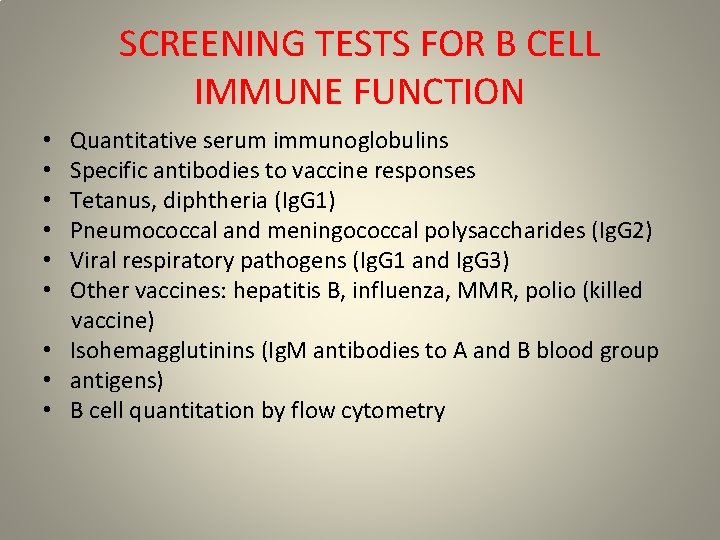
SCREENING TESTS FOR B CELL IMMUNE FUNCTION Quantitative serum immunoglobulins Specific antibodies to vaccine responses Tetanus, diphtheria (Ig. G 1) Pneumococcal and meningococcal polysaccharides (Ig. G 2) Viral respiratory pathogens (Ig. G 1 and Ig. G 3) Other vaccines: hepatitis B, influenza, MMR, polio (killed vaccine) • Isohemagglutinins (Ig. M antibodies to A and B blood group • antigens) • B cell quantitation by flow cytometry • • •
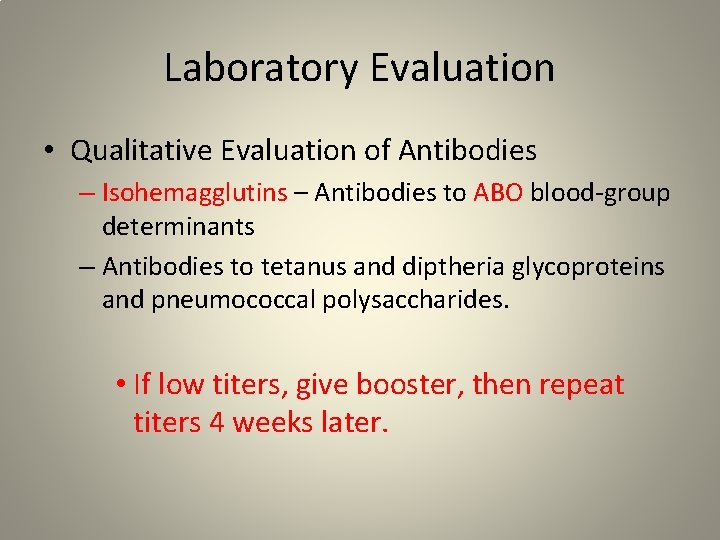
Laboratory Evaluation • Qualitative Evaluation of Antibodies – Isohemagglutins – Antibodies to ABO blood-group determinants – Antibodies to tetanus and diptheria glycoproteins and pneumococcal polysaccharides. • If low titers, give booster, then repeat titers 4 weeks later.
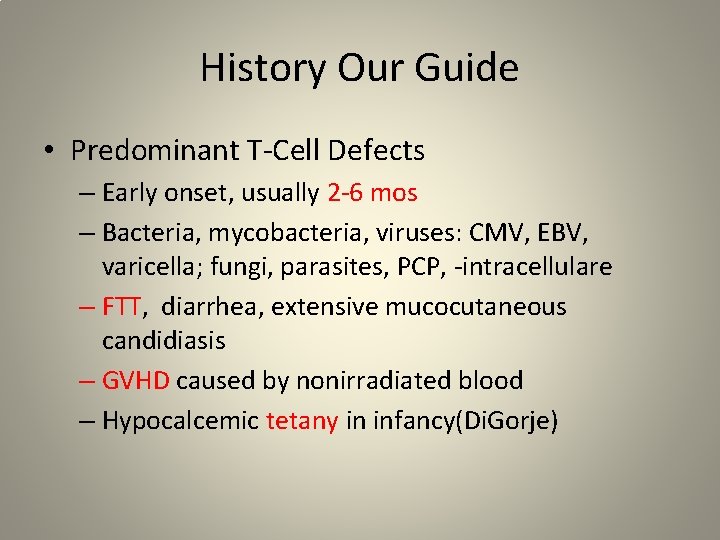
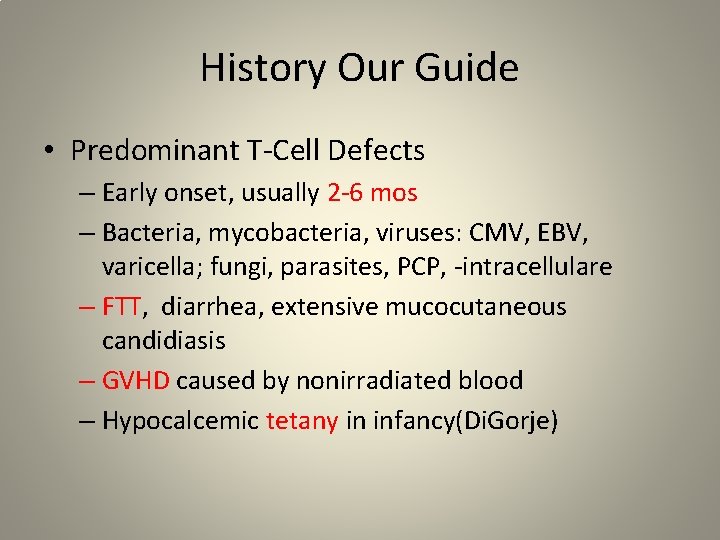
History Our Guide • Predominant T-Cell Defects – Early onset, usually 2 -6 mos – Bacteria, mycobacteria, viruses: CMV, EBV, varicella; fungi, parasites, PCP, -intracellulare – FTT, diarrhea, extensive mucocutaneous candidiasis – GVHD caused by nonirradiated blood – Hypocalcemic tetany in infancy(Di. Gorje)
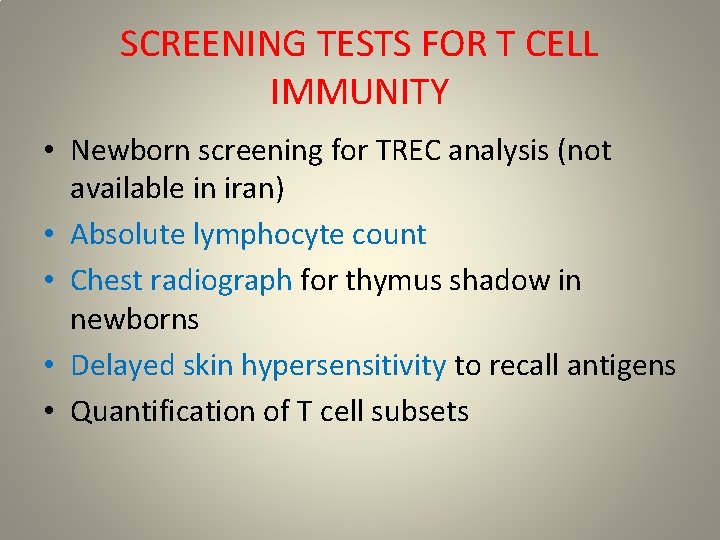
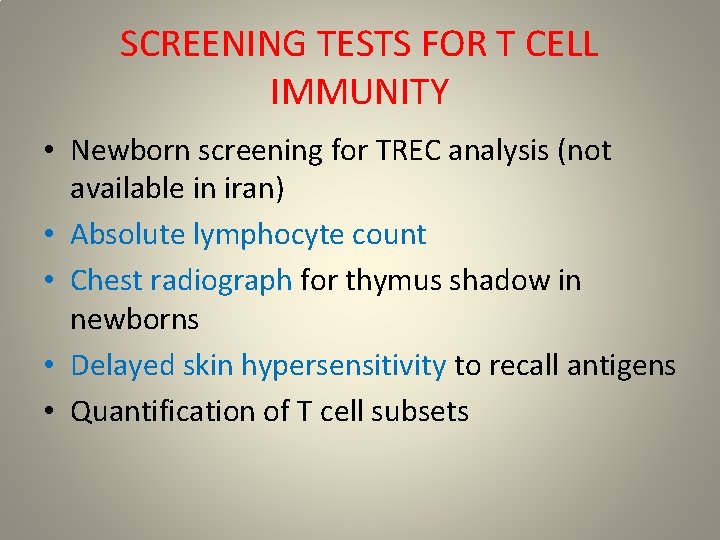
SCREENING TESTS FOR T CELL IMMUNITY • Newborn screening for TREC analysis (not available in iran) • Absolute lymphocyte count • Chest radiograph for thymus shadow in newborns • Delayed skin hypersensitivity to recall antigens • Quantification of T cell subsets
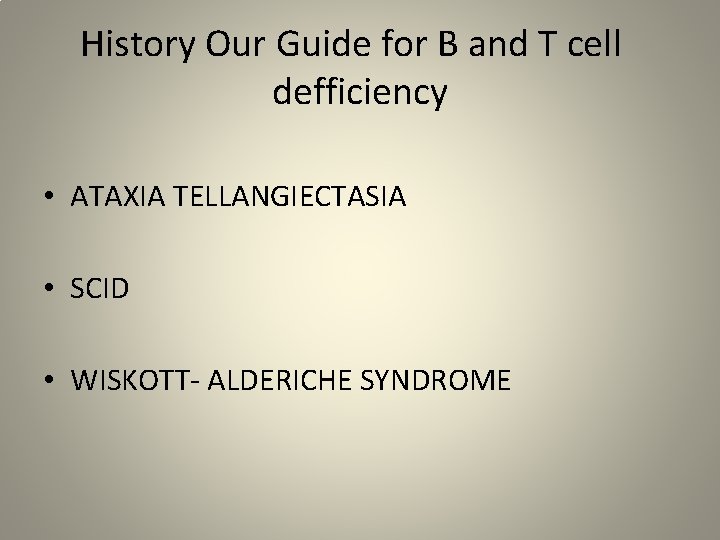
History Our Guide for B and T cell defficiency • ATAXIA TELLANGIECTASIA • SCID • WISKOTT- ALDERICHE SYNDROME
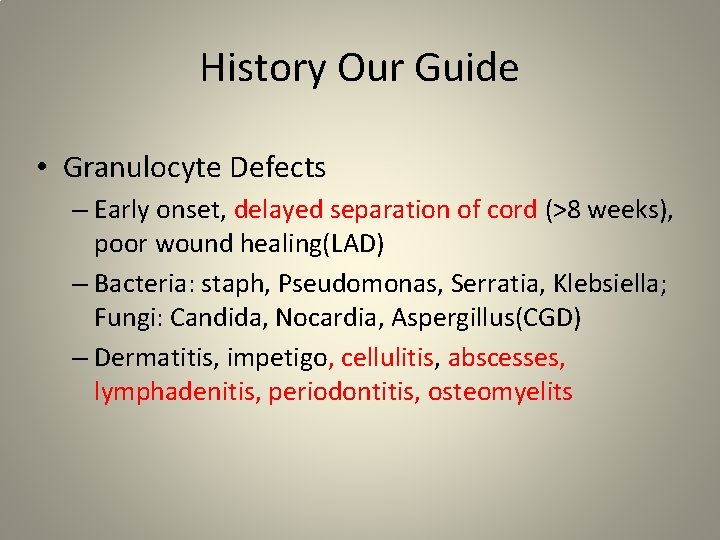
History Our Guide • Granulocyte Defects – Early onset, delayed separation of cord (>8 weeks), poor wound healing(LAD) – Bacteria: staph, Pseudomonas, Serratia, Klebsiella; Fungi: Candida, Nocardia, Aspergillus(CGD) – Dermatitis, impetigo, cellulitis, abscesses, lymphadenitis, periodontitis, osteomyelits
History Our Guide • Complement Defects – Late (C 5 -C 9) – Neisserial infections: meningitidis, septic arthritis from gonorrhoeae. – Early (C 1, C 4, and C 2) – autoimmune disease – C 3 deficiency – overwhelming sepsis, especially with gram negative organisms

SCREENING TESTS FOR INNATE DEFENSE FACTORS • Absolute granulocyte count, cell morphology • Serum total hemolytic complement for classic pathway (CH 50), alternative pathway hemolytic activity (AH 50) • Nitroblue tetrazolium (NBT) test or flow cytometry using dihydrorhodamine (DHR) « Staphylococcus aureus, Serratia marcescens, and Aspergillus” • Flow cytometry for leukocyte adhesion molecules (CD 11/CD 18 • and CD 15 a) • Ig. E (JOB )
B Cell Immunodeficiencies • Bruton’ s (X-linked) Agammaglobulinemia • • • Autosomal Recessive Hyper-Ig. M Syndrome X-linked Lymphoproliferative Syndrome Transient Hypogammaglobulinemia of Infancy Common Variable Immunodeficiency (CVID) Selective Ig. A Deficiency Ig. G Subclass Deficiency
General Management of Patients with Immunodeficiency • Avoid transfusions with blood products unless they • • are irradiated and cytomegalovirus-negative. Avoid live virus vaccines, especially in patients with severe T-cell deficiencies or agammaglobulinemia, and in household members. Use prophylaxis to Pneumocystis jiroveci (carinii) in T-cell immunodeficiency, and in X-linked hyper. Ig. M, consider antifungal prophylaxis in T-cell immunodeficiency. Follow pulmonary function in patients with recurrent pneumonia. Use chest physiotherapy and postural drainage in patients with recurrent pneumonia.
• Consider using prophylactic antibiotics because minor infections can quickly disseminate. • Examine diarrheal stools for Giardia lamblia and Clostridium difficile. • Avoid unnecessary exposure to individuals with infection. • Boil water for T-cell defects and hyper-Ig. M syndrome (Cryptosporidium risk). • Use immunoglobulin for severe antibody deficiency states (400– 600 mg/kg q 3– 4 wk IV). • BMT for T cell and Innate defect
v When Ig. G level are normal or near normal but Antibody deficiency is susceptible ØIg. G subclasses should be measured (Ig. G=70%, Ig. G 2 =20%, Ig. G 3=7%, Ig. G 4=3%) ØAntibody function should be measured v In patient with selective Ig. A deficiency Ig. G subclasses should be measured v Many Ig. A deficiency patients have Ig. G 2 subclass deficiency
v. In older children and adults , a total Ig level above 800 mg/ dl with normal screening antibody test excludes antibody deficiency v. Total Ig (Ig. G+Ig. M +Ig. A )< 400 or Ig. G level <200 mg /dl usually indicates antibody immunodeficiency

 Effector cells nervous system
Effector cells nervous system Immune effector cells
Immune effector cells Immune effector cells
Immune effector cells Refifs
Refifs Hygiene hypothesis
Hygiene hypothesis Delayed type hypersensitivity reactions
Delayed type hypersensitivity reactions Lymphocyte
Lymphocyte Aiguille de kuss
Aiguille de kuss Metarubricyte
Metarubricyte Lymphocyte
Lymphocyte Cytotoc
Cytotoc Vih
Vih Cytotoxic lymphocyte
Cytotoxic lymphocyte Lymphocyte size
Lymphocyte size Lymphoide primaire
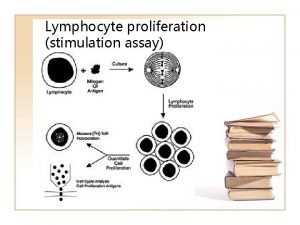
Lymphoide primaire Lymphocyte proliferation
Lymphocyte proliferation Antibody
Antibody How does a light sensor work
How does a light sensor work Effector organ
Effector organ End effector examples
End effector examples Sensor integrator effector
Sensor integrator effector Effector mechanism of humoral immunity
Effector mechanism of humoral immunity Effector function of antibody
Effector function of antibody End effector needle
End effector needle Section 2 classifying chemical reactions worksheet answers
Section 2 classifying chemical reactions worksheet answers Chemical reactions section 3 reactions in aqueous solutions
Chemical reactions section 3 reactions in aqueous solutions Section 2 classifying chemical reactions
Section 2 classifying chemical reactions Unit 5 chemical reactions answers
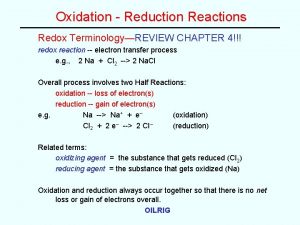
Unit 5 chemical reactions answers Redox reaction examples
Redox reaction examples Menzyme
Menzyme Sensitization hypersensitivity
Sensitization hypersensitivity Vasovagal reaction
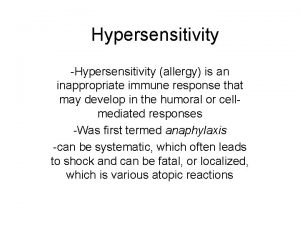
Vasovagal reaction Hypersensitivity definition
Hypersensitivity definition