Chapter 54 Care of Patients with Musculoskeletal Trauma









- Slides: 46
Chapter 54 Care of Patients with Musculoskeletal Trauma
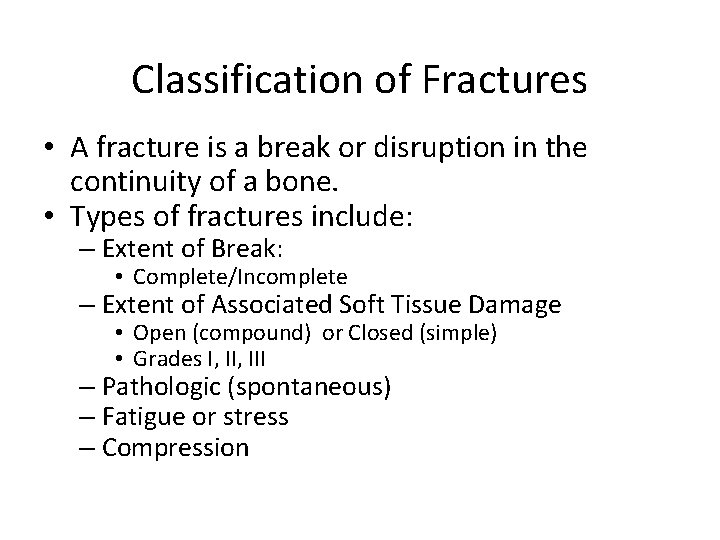
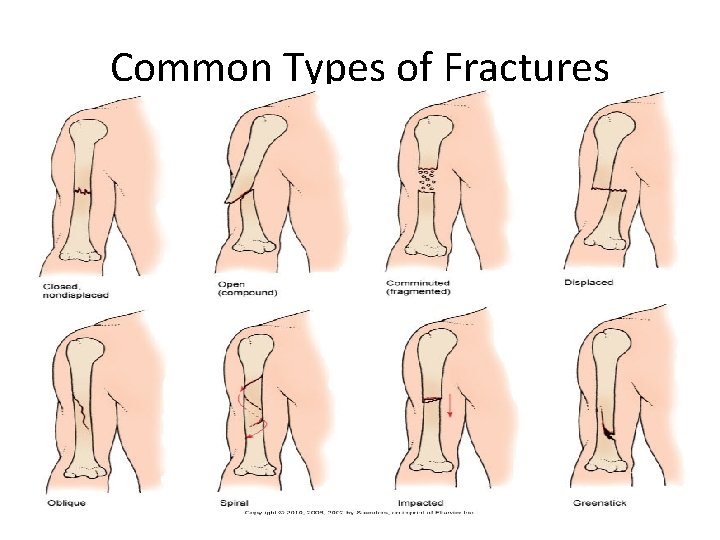
Classification of Fractures • A fracture is a break or disruption in the continuity of a bone. • Types of fractures include: – Extent of Break: • Complete/Incomplete – Extent of Associated Soft Tissue Damage • Open (compound) or Closed (simple) • Grades I, III – Pathologic (spontaneous) – Fatigue or stress – Compression
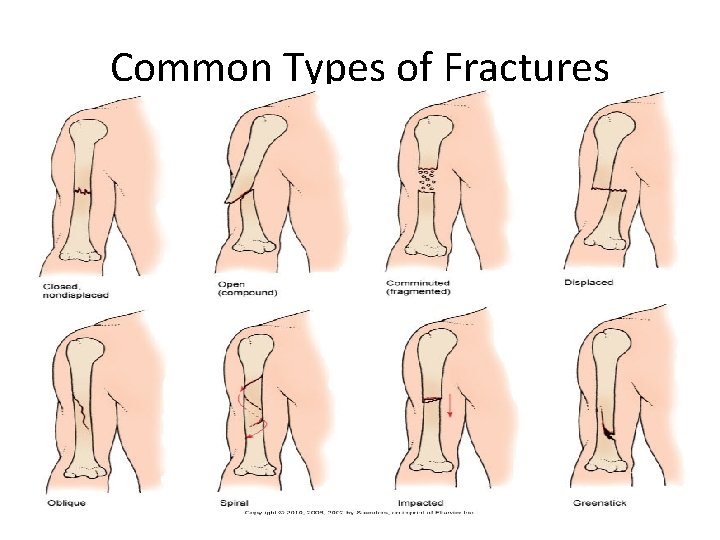
Common Types of Fractures
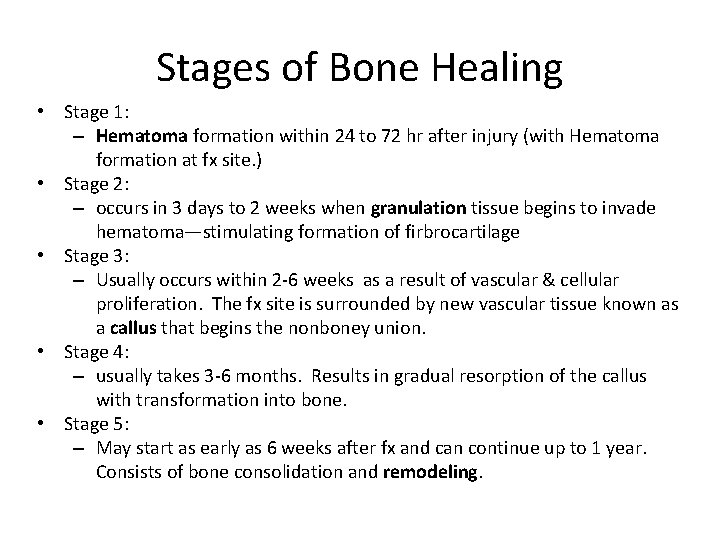
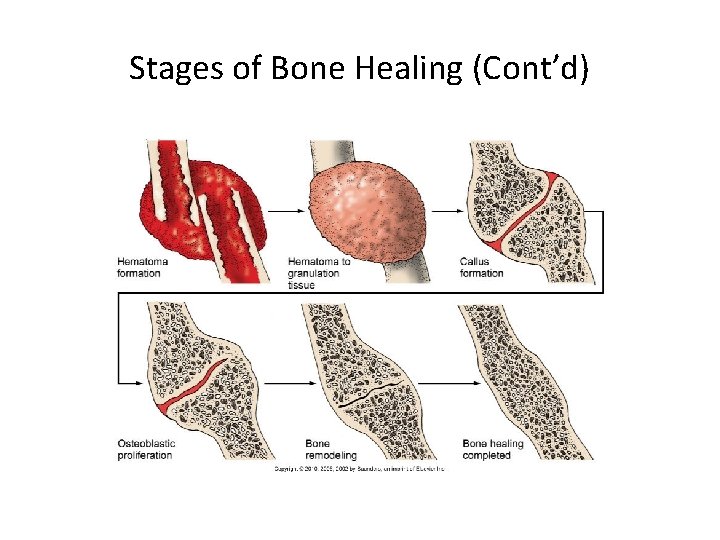
Stages of Bone Healing • Stage 1: – Hematoma formation within 24 to 72 hr after injury (with Hematoma formation at fx site. ) • Stage 2: – occurs in 3 days to 2 weeks when granulation tissue begins to invade hematoma—stimulating formation of firbrocartilage • Stage 3: – Usually occurs within 2 -6 weeks as a result of vascular & cellular proliferation. The fx site is surrounded by new vascular tissue known as a callus that begins the nonboney union. • Stage 4: – usually takes 3 -6 months. Results in gradual resorption of the callus with transformation into bone. • Stage 5: – May start as early as 6 weeks after fx and can continue up to 1 year. Consists of bone consolidation and remodeling.
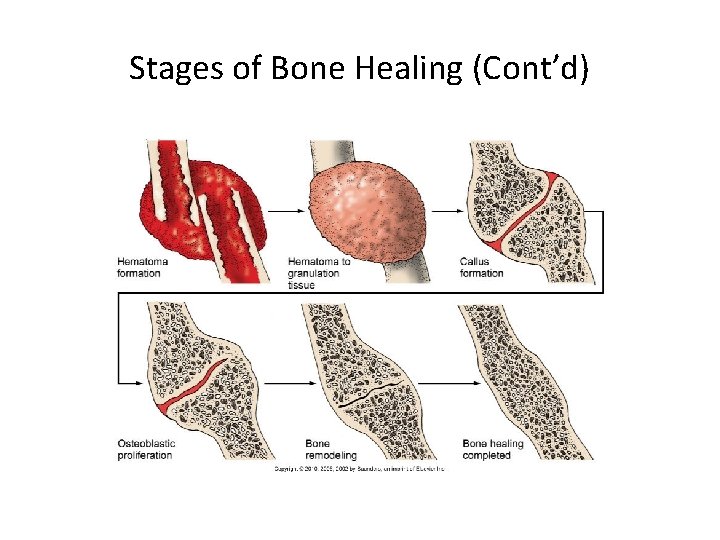
Stages of Bone Healing (Cont’d)
Acute Compartment Syndrome �Serious condition in which increased pressure within one or more compartments causes massive compromise of circulation to the area �Prevention of pressure buildup of blood or fluid accumulation �Pathophysiologic changes sometimes referred to as ischemia-edema cycle �Six Ps” including pain, pressure, paralysis, Paresthesia, pallor, and pulselessness �ACS is not common, but it creates an emergency situation when it does occur. Within 4 to 6 hours after the onset of compartment syndrome, neurovascular and muscle damage are irreversible. The limb can become useless in 24 to 48 hours. 6

Emergency Care • • Monitor compartment pressures. Fasciotomy may be performed to relieve pressure. Pack and dress the wound after fasciotomy. Goal is early recognition of s/s. – Can begin in 6 -8 hours after an injury or take up to 2 days to appear. – If suspected, implement interventions to relieve pressure: loosen dressing/bandage. If cast, know policy of who can cut it off. – notify provider immediately
Possible Results of Acute Compartment Syndrome Infection Motor weakness Volkmann’s contractures Myoglobinuric renal failure, known as rhabdomyolysis • Crush syndrome- next slide • •
Crush Syndrome �Occurs from an external crush injury that compresses one or more compartments in the leg, arm, or pelvis. It is a potentially lifethreatening, systemic complication that results from hemorrhage and edema after a severe fracture injury. (Assess pulses distal to injury) Specific causes of CS include: Twisting-type injuries Natural disasters, such as earthquakes Work-related injuries, such as being trapped under heavy equipment such as a car Drug or alcohol overdose, when one or more limbs may be compressed by body weight for a prolonged time Older adults who fall are unable to get up and lie for a prolonged time 9
Other Complications of Fractures • Shock • Fat embolism syndrome— – serious complication resulting from a fracture; fat globules are released from yellow bone marrow into bloodstream – S/S: confusion, tachypnea, restless • Intervention: Administer O 2 via NC. • Venous thromboembolism • Infection • Chronic complications— – ischemic necrosis (avascular necrosis [AVN] or osteonecrosis) – Delayed Union
Musculoskeletal Assessment Asses & Document: use standard precautions –use sterile gloves when touching areas where skin is broken. 1. Assess all major body systems first for life-threatening complications of respiratory, CV, and neurologic systems (priority) –esp head, chest, and abdomen; quick head to toe; Address life-threatening issues before fx. 2. FX Care: 1. inspect the Fracture site: a. When inspecting the site of a possible fracture, look for a change in bone alignment. b. shortening of length of bone & change in bone shape c. ROM d. Pain on ROM. If pain, stop movement immediately! e. crepitus (grating sound caused by bone fragments) f. Outward Bruising or bleeding. Ecchymosis (bruising) over fx may be present from bleeding into underlying soft tissue) 2. control bleeding 3. VS 4. place pt in supine position 5. keep pt warm 6. immobilize area of fracture by splinting (object/device that extends to the joints above & below the fx. ). esp> if grating or grinding sound heard 7. place sterile gauze loosely over open area of a compound fx 8. check neurovascular status after splinting.
Musculoskeletal Assessment (Cont’d) • Subcutaneous emphysema with bubbles under the skin • Swelling at the fracture site neurovascular assessment including : skin color (no change), skin temperature (warm-normal), movement active and passive (can move without discomfort; sensation: ask Paresthesia present; pulses –palpate pulses distal to injury (normal-strong equal); capillary refill (least reliable) Degree of soft tissue damage and amount of bleeding Muscle spasm- pain is usually due to muscle spasm or edema.
Special Assessment Considerations • For fractures of the shoulder and upper arm, assess patient in sitting or standing position. • Support the affected arm to promote comfort. • For distal areas of the arm, assess patient in a supine position. • For fracture of lower extremities and pelvis, patient is in supine position.
• Nonsurgical management typically involves closed reduction and immobilization with a bandage, splint, cast, or traction. Risk for Peripheral Neurovascular Dysfunction • Interventions include: – Emergency care— • assess for respiratory distress, bleeding, and head injury – Nonsurgical management— • closed reduction and immobilization with a bandage, splint, cast, or traction
Casts • Rigid device that immobilizes the affected body part while allowing other body parts to move • Cast materials—plaster, fiberglass, polyestercotton • Types of casts for various parts of the body— arm, leg, brace, body
Casts (Cont’d) • Cast care and patient education • Cast complications— – infection, – circulation impairment, • Teach patient to notify & see physician if the cast feel tight and fingers are puffy. – peripheral nerve damage, – complications of immobility

Immobilization Device Fiberglass Synthetic Cast
Traction • Application of a pulling force to the body to provide reduction, alignment, and rest at that site • Running or Balanced Suspension – Running-the pulling force is in one direction and the patient's body acts as countertraction – Balanced Suspension- provides the countertraction so that the pulling force of the traction is not altered when the bed or patient is moved. • Types of traction—skin, skeletal, plaster, brace, circumferential

External Fixation Device BUCKS TRACTION CRUTCHFIELD TONGS
Traction (Cont’d) • Traction care: – Maintain correct balance between traction pull and countertraction force • Weight are not removed without order • Should be freely hanging at all times (do not rest on floor) – Care of Weights – Skin inspection – Pin care • Monitor for infection (swollen, red, crusty w/dried drainage – Culture the drainage – Assessment of neurovascular status
Operative Procedures • Open reduction with internal fixation (ORIF) • External fixation – Monitor for infection at pin sites • Postoperative care—similar to that for any surgery; certain complications specific to fractures and musculoskeletal surgery include fat embolism and venous thromboembolism
Procedures for Nonunion • • Electrical bone stimulation Bone grafting Bone banking Low-intensity pulsed ultrasound (Exogen therapy)
Acute Pain • Interventions include: – Reduction and immobilization of fracture – Assessment of pain – Drug therapy—opioid and non-opioid drugs – Complementary and alternative therapies—ice, heat, elevation of body part, massage, baths, back rub, therapeutic touch, distraction, imagery, music therapy, relaxation techniques 23
Risk for Infection – Assess for pneumonia and urinary tract infection. – Administer broad-spectrum antibiotics prophylactically. • Interventions include: – Apply strict aseptic technique for dressing changes and wound irrigations. – Assess for local inflammation. – Report purulent drainage immediately to health care provider.
Impaired Physical Mobility • Interventions include: – Use of crutches to promote mobility – Use of walkers and canes to promote mobility
Imbalanced Nutrition: Less Than Body Requirements • Interventions include: – Diet high in protein, calories, and calcium; supplemental vitamins B and C • LOW FAT MILK, VIT C SUPPLEMENTS, ROAST PORT – Frequent, small feedings and supplements of highprotein liquids – Intake of foods high in iron
Upper Extremity Fractures • Fractures include those of the: – Clavicle • SPLINT OR BANDAGE FOR IMMOBILIZATION – Scapula • Immobilization until healed – Humerus • Closed reduction with arm cast or splint – Olecranon • Closed reduction with cast or splint – Radius and ulna • Closed reduction with cast – Wrist and hand • Closed reduction with cast
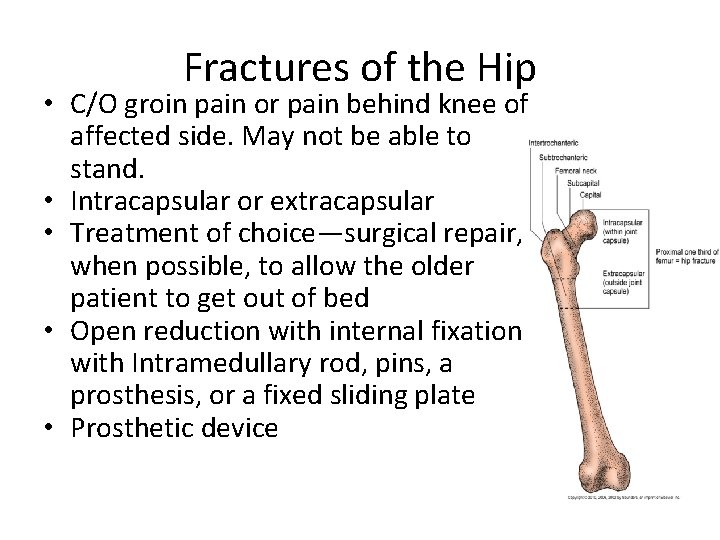
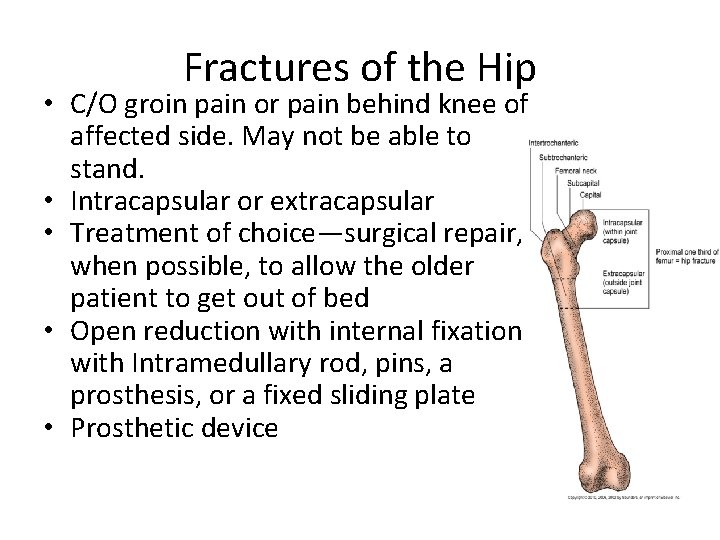
Fractures of the Hip • C/O groin pain or pain behind knee of affected side. May not be able to stand. • Intracapsular or extracapsular • Treatment of choice—surgical repair, when possible, to allow the older patient to get out of bed • Open reduction with internal fixation with Intramedullary rod, pins, a prosthesis, or a fixed sliding plate • Prosthetic device
Lower Extremity Fractures • Fractures include those of the: – Femur • ORIF – Patella – Tibia and fibula – Ankle and foot
Fractures of the Pelvis • Associated internal damage the chief concern in fracture management of pelvic fractures – Damage to blood vessels > loss of blood volume and hypovolemic shock • Monitor Blood Pressure frequently • Non–weight-bearing fracture of the pelvis • Weight-bearing fracture of the pelvis
Compression Fractures of the Spine • Most are associated with osteoporosis rather than acute spinal injury. • Multiple hairline fractures result when bone mass diminishes. • Nonsurgical management includes bedrest, analgesics, and physical therapy. • Minimally invasive surgeries are vertebroplasty and kyphoplasty, in which bone cement is injected.

Amputations • • Surgical amputation Traumatic amputation Levels of amputation Complications of amputations—hemorrhage, infection, phantom limb pain, neuroma, flexion contracture

Common Levels of Amputation

Phantom Limb Pain • Phantom limb pain is a frequent complication of amputation. • Patient complains of pain at the site of the removed body part, most often shortly after surgery. • Pain is intense burning feeling, crushing sensation, or cramping. • Some patients feel that the removed body part is in a distorted position.
Management of Pain • Phantom limb pain must be distinguished from residual limb pain because they are managed differently. • Recognize that this pain is real and interferes with the amputee’s ADLs. • Opioids are effective for residual limb pain. • IV calcitonin (Calcimar) for week after amputation effective for PLP.
Exercise After Amputation • ROM to prevent flexion contractures, particularly of the hip and knee – Priority intervention after amputation • Trapeze and overhead frame • Firm mattress • Prone position every 3 to 4 hours – To prevent hip flexion contractures • Elevation of lower-leg residual limb controversial
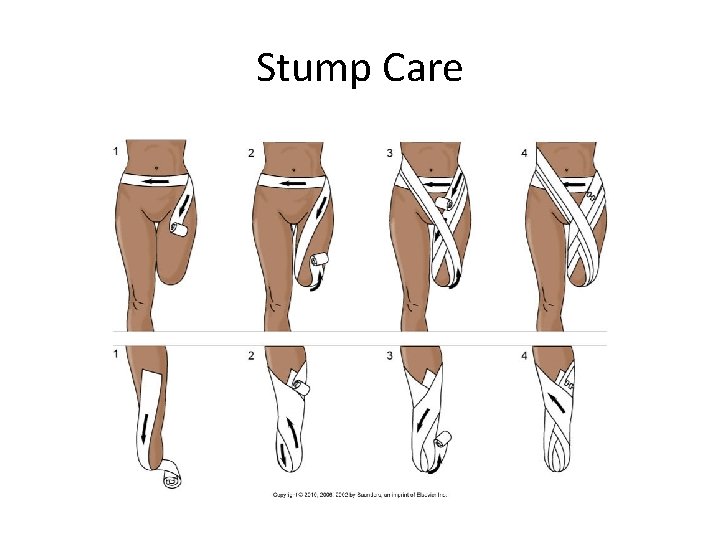
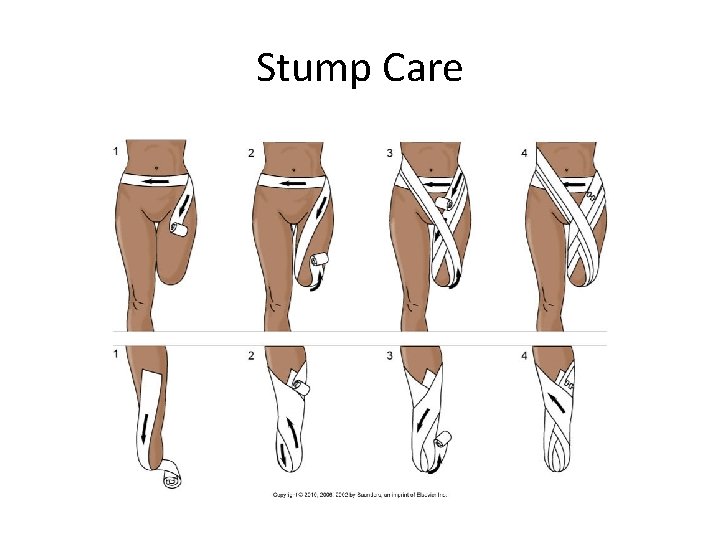
Stump Care
Prostheses • Devices to help shape and shrink the residual limb and help patient adapt • Wrapping of elastic bandages • Individual fitting of the prosthesis; special care
Knee Injuries, Meniscus • • • Mc. Murray test Meniscectomy Postoperative care Leg exercises begun immediately Knee immobilizer Elevation of the leg on one or two pillows; ice
Knee Injuries, Ligaments • When the anterior cruciate ligament is torn, a snap is felt, the knee gives way, swelling occurs, and stiffness and pain follow. • Treatment can be nonsurgical or surgical. • Complete healing of knee ligaments after surgery can take 6 to 9 months.
Tendon Ruptures • Rupture of the Achilles tendon is common in adults who participate in strenuous sports. • For severe damage, surgical repair is followed by leg immobilized in a cast for 6 to 8 weeks. • Tendon transplant may be needed.

Dislocations and Subluxations • Pain, immobility, alteration in contour of joint, deviation in length of the extremity, rotation of the extremity • Closed manipulation of the joint performed to force it back into its original position • Joint immobilized until healing occurs
Strains • Excessive stretching of a muscle or tendon when it is weak or unstable • Classified according to severity—first-, second, and third-degree strain • Management—cold and heat applications, exercise and activity limitations, antiinflammatory drugs, muscle relaxants, and possible surgery

Sprains • Excessive stretching of a ligament • Treatment of sprains: – First-degree—rest, ice for 24 to 48 hr, compression bandage, and elevation (RICE) – Second-degree—immobilization, partial weight bearing as tear heals – Third-degree—immobilization for 4 to 6 weeks, possible surgery

Rotator Cuff Injuries • Shoulder pain; cannot initiate or maintain abduction of the arm at the shoulder • Conservative treatment—NSAIDs, physical therapy, sling support, ice or heat applications during healing • Surgical repair for a complete tear
This work is licensed under a Creative Commons Attribution 4. 0 International License. Except where otherwise noted, this content by Southern Regional Technical College is licensed under the Creative Commons Attribution 4. 0 International License. To view a copy of this license, click https: //creativecommons. org/licenses/by/4. 0/ Healthcare Careers Work!(HCW) is sponsored by a $2. 3 million grant from the U. S. Department of Labor, Employment & Training Administration. TAACCCT Grant #TC- 26488 -14 -60 -A-13. Southern Regional Technical College is an equal opportunity employer and will make adaptive equipment available to persons with disabilities upon request. This workforce product was funded by a grant awarded by the U. S. Department of Labor’s Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U. S. Department of Labor. The U. S. Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.
 Chapter 40 musculoskeletal care modalities
Chapter 40 musculoskeletal care modalities Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders The musculoskeletal system chapter 21
The musculoskeletal system chapter 21 Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 15 musculoskeletal system practical
Chapter 15 musculoskeletal system practical Buck's extension traction
Buck's extension traction The factors of care that patients can expect to receive
The factors of care that patients can expect to receive Cataracts ncp
Cataracts ncp Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Sengstaken blakemore tube nursing care
Sengstaken blakemore tube nursing care Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary 4 r's trauma informed care
4 r's trauma informed care Lgbt trauma informed care
Lgbt trauma informed care 4 r's trauma informed care
4 r's trauma informed care 4 r's trauma informed care
4 r's trauma informed care 4 r's trauma informed care
4 r's trauma informed care Libby bergman
Libby bergman Sensory modulation
Sensory modulation Dshs uncompensated trauma care application
Dshs uncompensated trauma care application Early total care
Early total care Trauma-informed care cheat sheet
Trauma-informed care cheat sheet Trauma-informed care activities for staff
Trauma-informed care activities for staff Trauma informed care for foster youth
Trauma informed care for foster youth Chapter 36 patients with special challenges
Chapter 36 patients with special challenges Diamond carry ems
Diamond carry ems Which is preferred when moving equipment and patients?
Which is preferred when moving equipment and patients? Backboarding a patient
Backboarding a patient Types of joint movement
Types of joint movement Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Musculoskeletal system
Musculoskeletal system Musculoskeletal icd 10
Musculoskeletal icd 10 Kode icd 10 fraktur vertebra thorakal
Kode icd 10 fraktur vertebra thorakal Musculoskeletal fitness assessment
Musculoskeletal fitness assessment Work related musculoskeletal disorders definition
Work related musculoskeletal disorders definition Musculoskeletal pronounce
Musculoskeletal pronounce Musculoskeletal system medical terminology
Musculoskeletal system medical terminology Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Musculoskeletal system
Musculoskeletal system West coast musculoskeletal
West coast musculoskeletal ömpsq
ömpsq Musculoskeletal
Musculoskeletal Musculoskeletal integrity
Musculoskeletal integrity