Chapter 36 The Experience of Loss Death and
- Slides: 28
Chapter 36 The Experience of Loss, Death, and Grief
Scientific Knowledge Base: Types of Loss Developing a personal understanding of your own feeling about grief and death will help you better serve your patients. • Necessary Loss: A part of life. These cause us to undergo some type of change. (Job change, moving, friendships) • Maturational loss: are a type of necessary loss and include those changes that occur across the life span. (Mother’s sense of loss when child goes to kindergarten) • Situational loss: sudden and unpredictable (Physical injury, loss of function, income, dreams or life goals)
Scientific Knowledge Base: Grief • Grief = An emotional response to a loss, manifested in ways unique to an individual based on personal experiences, cultural expectations, and spiritual beliefs.
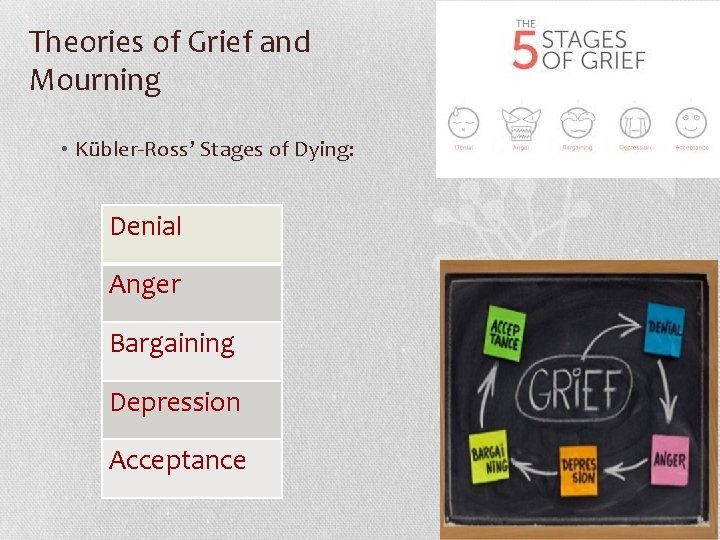
Theories of Grief and Mourning • Kübler-Ross’ Stages of Dying: Denial Anger Bargaining Depression Acceptance
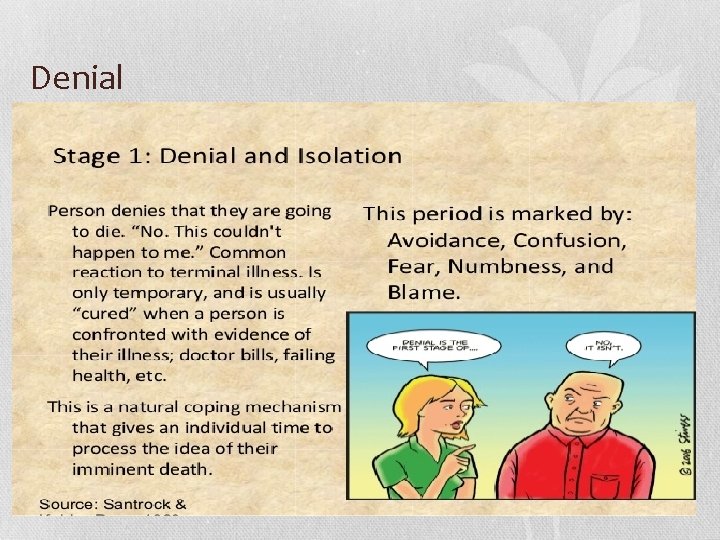
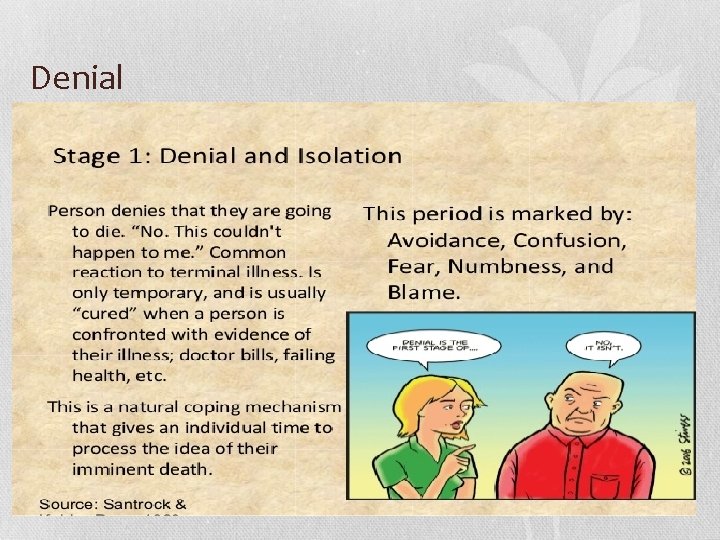
Denial
Anger
Bargaining
Depression
Acceptance
Advance Directives • Advance Directive: A document or verbal statement in which an individual states choices for medical treatment or designates who should make treatment choices if the individual should lose decision making capacity. • Durable Power Of Attorney for Health Care: An advance directive in which an individual names someone else (the "agent" or "proxy") to make health care decisions for him/her. • Living Will: A written and signed declaration instructing an individual's physician to withhold or withdraw certain death delaying procedures (including artificially supplied nutrition and hydration) when the individual is in a terminal condition and unable to communicate his/her wishes. 10
DNR • Do Not Resuscitate (DNR): an explicit order that requests the withholding of any one or endotracheal intubation and initiation of ventilatory support, 2) chest compressions, 3) electrical countershock, 4) external cardiac pacing, and 5) bolus administration of inotropes, vasopressors or antiarrhythmics. A DNR order does not limit or restrict the use of any other medical treatment, diagnosis or intervention prior to cardiopulmonary or respiratory arrest. • MUST have a new order with each admission! 11
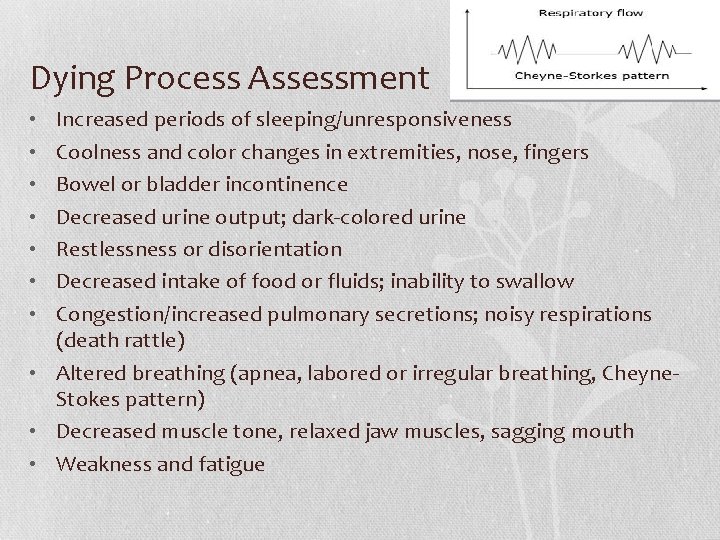
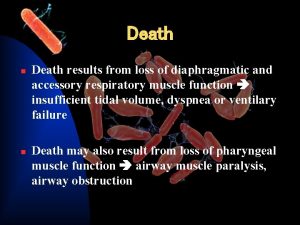
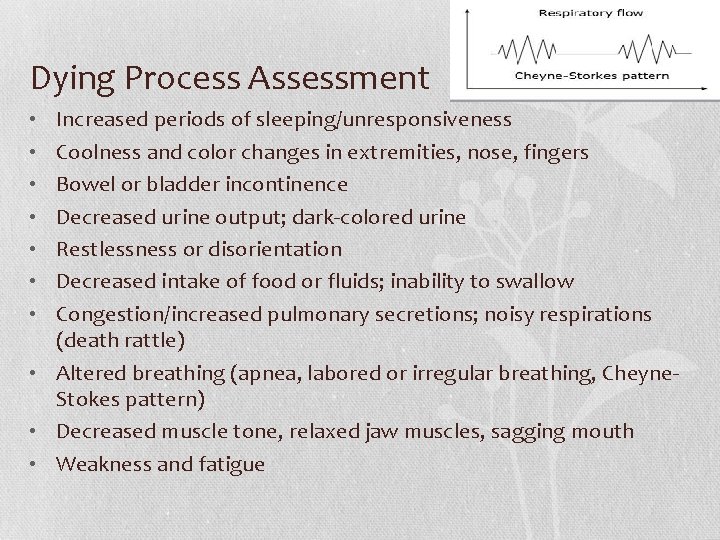
Dying Process Assessment Increased periods of sleeping/unresponsiveness Coolness and color changes in extremities, nose, fingers Bowel or bladder incontinence Decreased urine output; dark-colored urine Restlessness or disorientation Decreased intake of food or fluids; inability to swallow Congestion/increased pulmonary secretions; noisy respirations (death rattle) • Altered breathing (apnea, labored or irregular breathing, Cheyne. Stokes pattern) • Decreased muscle tone, relaxed jaw muscles, sagging mouth • Weakness and fatigue • •
Palliative Care • Palliative care focuses on the prevention, relief, reduction, or soothing of symptoms of disease or disorders throughout the entire course of an illness, including care of the dying and bereavement follow-up for the family. • The primary goal of palliative care is to help patients and families achieve the best possible quality of life
Hospice Care • Hospice care is a philosophy and a model for the care of terminally ill patients and their families. • Patients accepted into a hospice program usually have less than 6 to 12 months to live. • Hospice services are available in home, hospital, extended care, or nursing home settings.
Hospice Care • To be eligible for home hospice services, a patient must have a family caregiver to provide care when the patient is no longer able to function alone. • Aides for hygienic needs • Nurse to coordinate and manage symptoms relief • As the patient’s death comes closer, the hospice team provide intensive support to the patient and family.
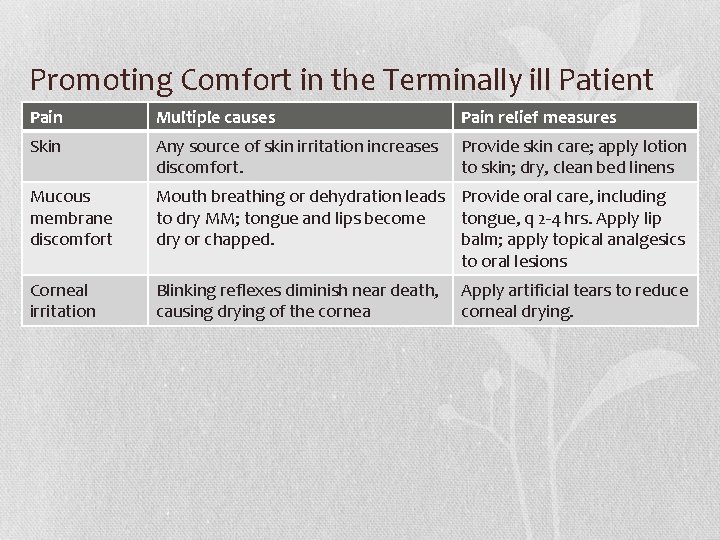
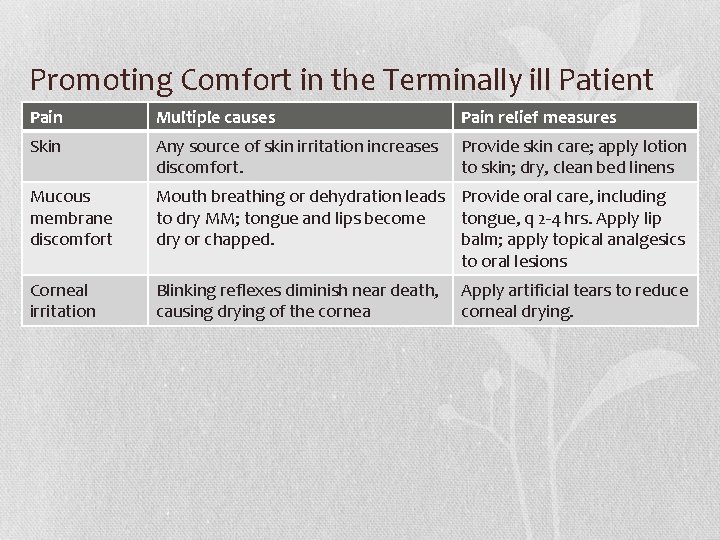
Promoting Comfort in the Terminally ill Patient Pain Multiple causes Pain relief measures Skin Any source of skin irritation increases discomfort. Provide skin care; apply lotion to skin; dry, clean bed linens Mucous membrane discomfort Mouth breathing or dehydration leads Provide oral care, including to dry MM; tongue and lips become tongue, q 2 -4 hrs. Apply lip dry or chapped. balm; apply topical analgesics to oral lesions Corneal irritation Blinking reflexes diminish near death, causing drying of the cornea Apply artificial tears to reduce corneal drying.
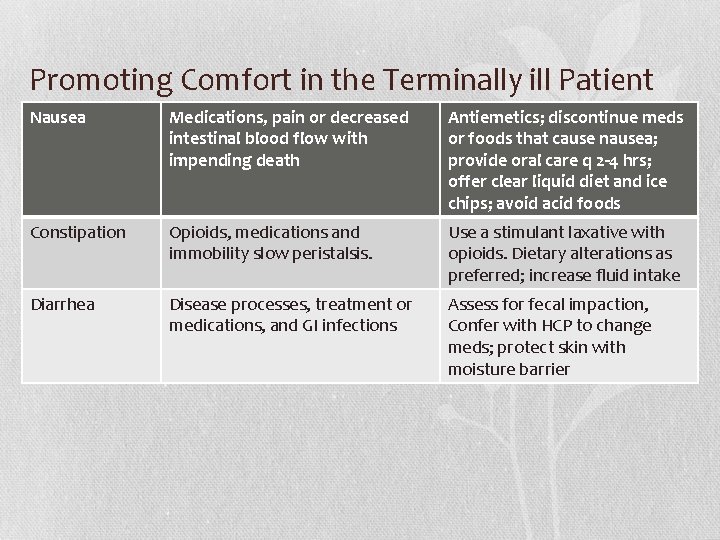
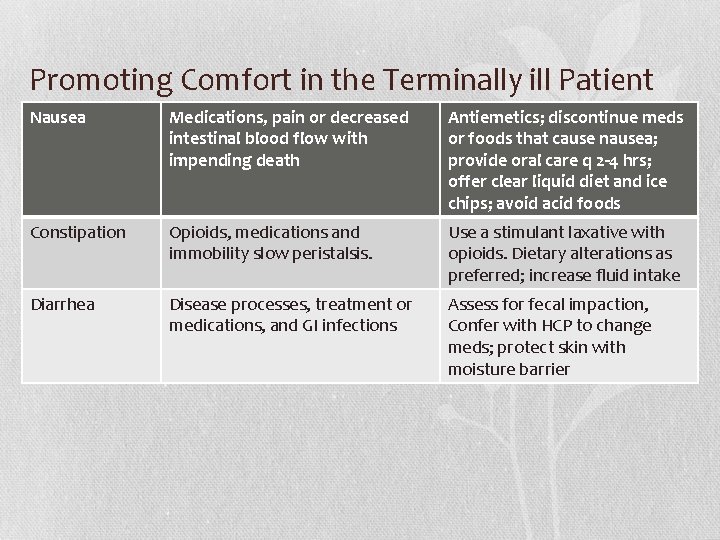
Promoting Comfort in the Terminally ill Patient Nausea Medications, pain or decreased intestinal blood flow with impending death Antiemetics; discontinue meds or foods that cause nausea; provide oral care q 2 -4 hrs; offer clear liquid diet and ice chips; avoid acid foods Constipation Opioids, medications and immobility slow peristalsis. Use a stimulant laxative with opioids. Dietary alterations as preferred; increase fluid intake Diarrhea Disease processes, treatment or medications, and GI infections Assess for fecal impaction, Confer with HCP to change meds; protect skin with moisture barrier
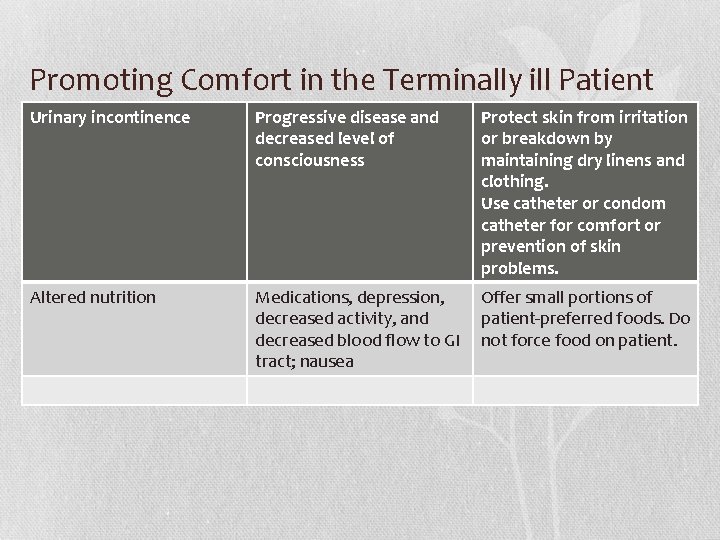
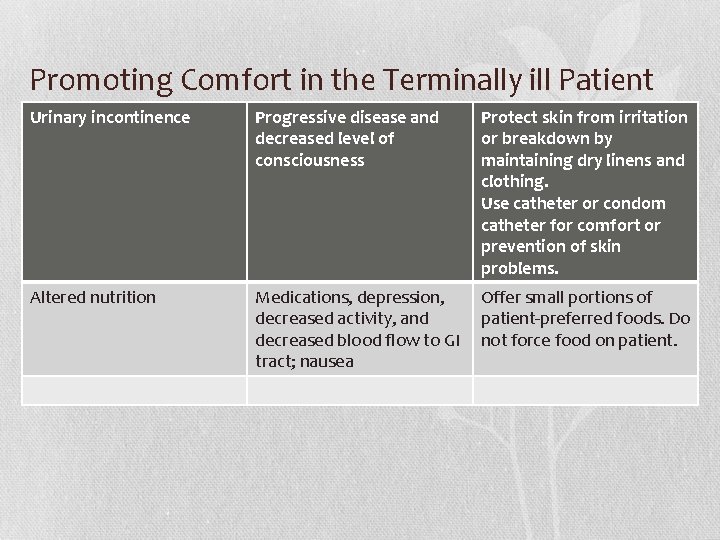
Promoting Comfort in the Terminally ill Patient Urinary incontinence Progressive disease and decreased level of consciousness Protect skin from irritation or breakdown by maintaining dry linens and clothing. Use catheter or condom catheter for comfort or prevention of skin problems. Altered nutrition Medications, depression, decreased activity, and decreased blood flow to GI tract; nausea Offer small portions of patient-preferred foods. Do not force food on patient.
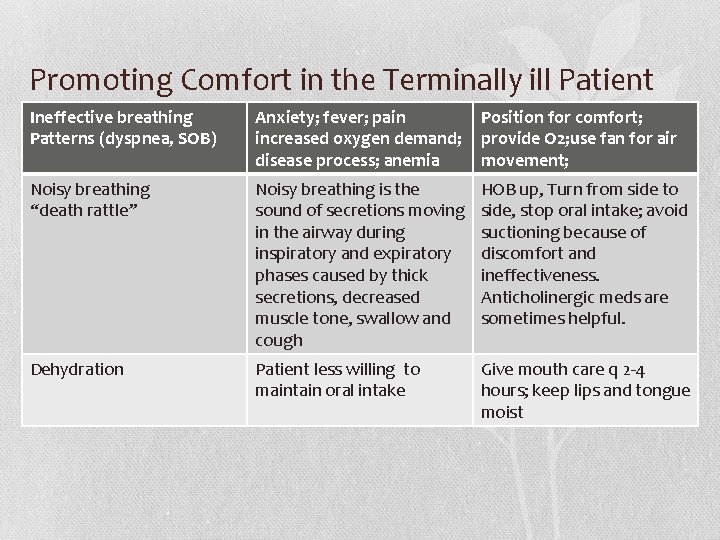
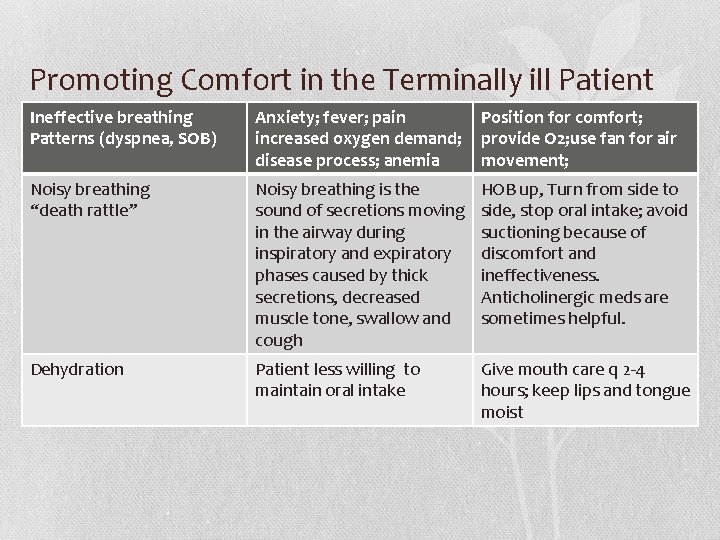
Promoting Comfort in the Terminally ill Patient Ineffective breathing Patterns (dyspnea, SOB) Anxiety; fever; pain increased oxygen demand; disease process; anemia Position for comfort; provide O 2; use fan for air movement; Noisy breathing “death rattle” Noisy breathing is the sound of secretions moving in the airway during inspiratory and expiratory phases caused by thick secretions, decreased muscle tone, swallow and cough HOB up, Turn from side to side, stop oral intake; avoid suctioning because of discomfort and ineffectiveness. Anticholinergic meds are sometimes helpful. Dehydration Patient less willing to maintain oral intake Give mouth care q 2 -4 hours; keep lips and tongue moist
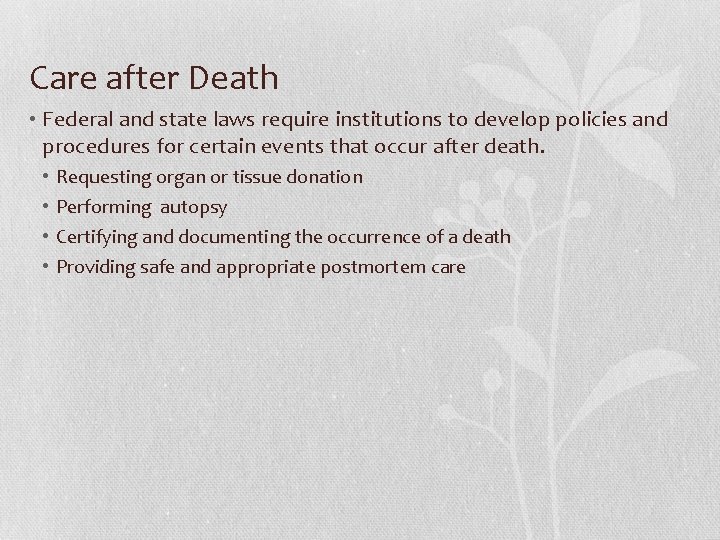
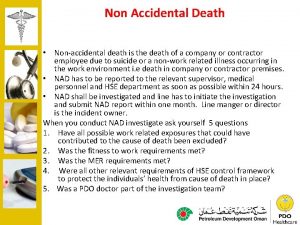
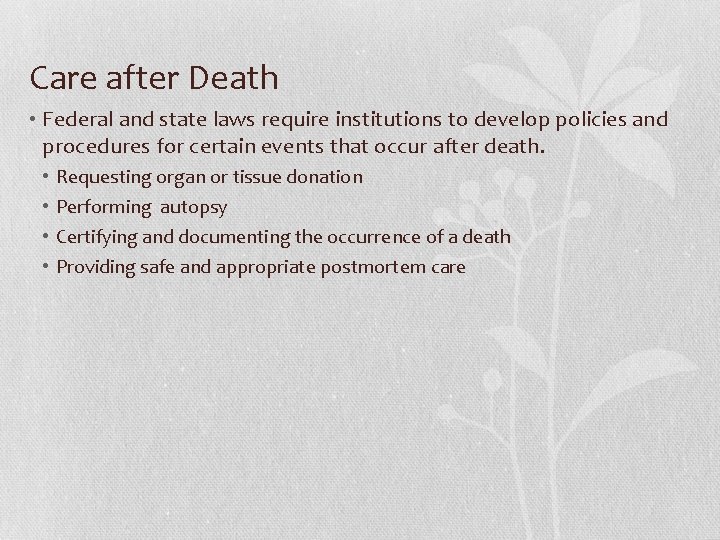
Care after Death • Federal and state laws require institutions to develop policies and procedures for certain events that occur after death. • • Requesting organ or tissue donation Performing autopsy Certifying and documenting the occurrence of a death Providing safe and appropriate postmortem care
Care of the Body after Death • In your collaborative groups read about the rituals of dying from the various cultures: • • African-American Chinese Hispanic/Latino Native American Islamic Buddhists Hindu Jewish (Hint: See table 36 -10 )
Care of the Body after Death • Identify the patient with 2 identifiers • Provide sensitive and dignified nursing care to the patient and family. • Elevate the HOB as soon as possible after death to prevent discoloration of the face • Collect ordered specimens • Ask if the family wishes to participate in preparation of the body • Remove all equipment, tubes, indwelling lines • Cleanse the body thoroughly
Care of the Body after Death • Provide sensitive and dignified nursing care to the patient and family. • Cover body with clean sheet, place head on a pillow and leave arms outside covers if possible. • Close eyes by gently holding them shut • Ensure dentures are in mouth to maintain facial shape • Cover any signs of body trauma • Prepare and clean the room, deodorize room if needed, and lower lights
Care of the Body after Death • Provide sensitive and dignified nursing care to the patient and family. • Offer family members the options to view the body and ask if they want your or other support persons to accompany them. • Encourage grievers to say good-bye • Provide privacy and an unrushed atmosphere. • Determine which personal belongings stay with the body. Document time, date, description of the items taken and who received them.
Care of the Body after Death • Provide sensitive and dignified nursing care to the patient and family. • Apply identifying name tags and shroud before transporting the body. • Maintain privacy and dignity when transporting the body to another location; cover the body or stretcher with a clean sheet.
Nurse’s Presence
Importance of Nurses’ Self-Care • You cannot give fully engaged, compassionate care to others when you feel depleted or do not feel cared for yourself. • Frequent, intense, or prolonged exposure to grief and loss places nurses at risk for developing compassion fatigue. • Being a professional includes caring for yourself physically and emotionally. • To avoid the extremes of becoming overly involved in patients’ suffering or detaching from them, nurses develop self-care strategies to maintain balance.
Importance of Nurses’ Self-Care (cont’d)
 Scrap account
Scrap account Direct experience and indirect experience
Direct experience and indirect experience Imprinting meaning psychology
Imprinting meaning psychology Early experience vs. later experience
Early experience vs. later experience Forensic pathology definition
Forensic pathology definition Leasiest
Leasiest Lesson 3 coping with loss and grief
Lesson 3 coping with loss and grief Chapter 4 managing stress and coping with loss lesson 1
Chapter 4 managing stress and coping with loss lesson 1 Chapter 36 loss and grief
Chapter 36 loss and grief Chapter 4 lesson 2 managing stress answer key
Chapter 4 lesson 2 managing stress answer key Chapter 4 managing stress and coping with loss
Chapter 4 managing stress and coping with loss Chapter 8: race and ethnicity as lived experience
Chapter 8: race and ethnicity as lived experience Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton
Tư thế worm breton Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
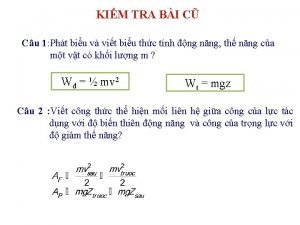
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật