Chapter 17 18 Neuroendocrine System Contains the hypothalamus






- Slides: 44
Chapter 17 & 18
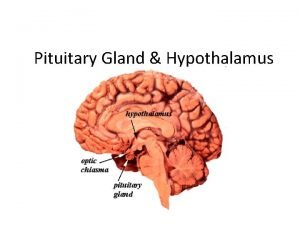
§ Neuroendocrine System § Contains the hypothalamus and Pituitary Gland § Controls thyroid, adrenal and reproductive function



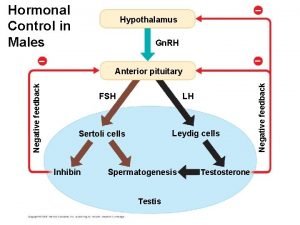
§ TROPIC HORMONES § § § MSH: secretion of melanin (melanocyte stimulating hormone) FSH: estrogen production and spermatogenesis (follicle stimulating hormone) LH: ovulation, progesterone and testosterone production (luteinizing hormone) ACTH: cortisol production and maintenance of adrenal gland (adrenocorticotropic hormone) TSH: thyroid hormone production (thyroid stimulating hormone) GH: skeletal muscle growth, regulates metabolism, necessary for stress adaptation (growth hormone) § Regulated by GHRH and Somatostatin § IGF-1 and IGF-2 (insulin-like growth factor) § Prolactin: milk production (lactation)
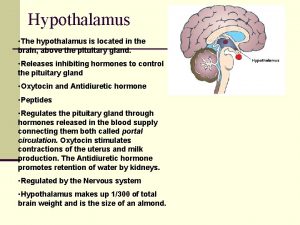
§ POLYPEPTIDE HORMONES § ADH (vasopressin): controls plasma osmolality (antidiuretic hormone) § Regulated by glutamate and GABA § Increased release with stress, trauma, decreased intravascular volume § Decreased release with decreased plasma osmolality and increased intravascular volume § Oxytocin: uterine contraction and milk ejection § Also has some antidiuretic effects

§ Adrenal Medulla § Catecholamine secretion § Epinephrine and norepinephrine
§ Adrenal Cortex § Glucocorticoids § Carbohydrate metabolism, immune suppression, anti-inflammatory effects, suppress bone formation, suppress ADH secretion, stimulate gastric acid secretion § In high levels cause: § Increased appetite, fat deposits in face, abdomen, upper back, hypocalcemia, decreased ACTH synthesis
§ Cortisol § CRH ACTH cortisol secretion § Potent naturally occurring glucocorticoid § Necessary for maintenance of life § Diurnal release of ACTH § Negative feedback loop associated with ACTH release § Increased release: low levels of circulating cortisol; stress reactions § Decreased release: high levels of circulating cortisol; synthetic glucocorticoid use
§ Mineralcorticoids § Aldosterone § Natural occurring mineralcorticoid § Promotes sodium retention and potassium excretion § Regulated by the renin-angiotensin system (primarily angiotensin II) § Sodium and water depletion § Hyperkalemia § Decreased blood volume


§ 1. Inadequate Synthesis § Precursor dysfunction § 2. Failure of Feedback Systems § Too much or too little hormone synthesis § 3. Inactive Hormones § Directly inhibited or degraded § 4. Ineffective Hormone Delivery § Decreased blood supply § Inadequate carriers § 5. Decreased Target-Cell Sensitivity § Too little receptors § Presence of antibodies on receptors
§ Increased ADH release regardless of plasma osmolality § Causes: § Neoplasms § Pulmonary disorders § CNS disorders § Medications
§ Manifestations: § HYPONATREMIA § Thirst § Dyspnea § Fatigue § Vomiting § Confusion (late) § Lethargy (late) § Convulsions (late) § Irreversible neurological damage (late)
§ Diagnostics: § Serum hypoosmolality § Serum hyponatremia § Urine hyperosmolality § Normal adrenal, thyroid, and renal function § Resistant hyponatremia § Treatment: § Fluid restriction § Hypertonic solutions § Use of demeclocycline
§ Tetracycline drug class § Has unique side effect of stimulating urine flow § Used for SIADH
§ Decreased ADH release § Causes: § Neurogenic § Insufficient secretion of ADH § Interference of ADH synthesis (brain tumors, aneurysm, infection, thrombosis) § Nephrogenic § Renal tubules do not respond appropriately to ADH § Acquired § Pyelonephritis, polycystic kidney disease, anesthetics, medications § Genetic
§ Manifestations: § Polyuria § Nocturia § Thirst § Polydipsia § Dilute urine § Urine hypoosmolality § Serum hypernatremia § Serum hyperosmolality
§ Treatment: § Desmopressin § Treatment of underlying cause
§ Vasopressin § Antidiuretic hormone § Promotes renal conservation of water, increasing permeability of renal tubules § Used for Diabetes Insipidus § Given intranasally, SQ, IV, or PO § Adverse effects: § Excessive water retention § Limited side effects
§ Causes: § Inadequate Hypothalamic Releasing Hormones § Inadequate anterior pituitary gland § Infarction § Adenoma § Damage to pituitary stalk § Meningitis § Tuberculosis § Autoimmune disorders
§ Manifestations: § Deficient ACTH : anorexia, fatigue, hypoglycemia § Deficient TSH : cold intolerance, lethargy, decreased metabolism § Deficient FSH and LH : amenorrhea, testicular atrophy, decreased libido § Deficient GH : hypopituitary dwarfism (children) Feeling of poor well-being, osteoporosis, fatigue (adult) generalized complaints Panhypopituitarism (all anterior pituitary hormones are deficient)
§ Acromegaly § Prolonged exposure to increased GH and IGF-1 § Middle aged adults § Rare § Slowly progressive § Cause: § Pituitary adenoma
§ Manifestations: § Enlarged tongue § Enlarged sweat glands § Coarse skin § Excessive body hair § Enlargement of facial bones (protrusion of forehead and jaw) § Enlargement of hands and feet
§ Treatment: § Surgical removal of GH secreting adenoma § Radiation § Octreotide § Lanreotide § Pegvisomant
§ Ocreotide § IM injection § Indicated for acromegaly § Adverse effects: § GI symptoms § gallstones § Lanreotide § Prefilled SQ syringe § Adverse effects: § Diarrhea § gallstones
§ Pegvisomant § Most effective drug option for acromegaly § SQ injection § Expensive § Adverse effects: § GI upset § Chest pain § Flu-like symptoms § Monitor hepatic function
§ Prolactinoma § Sustained, elevated release of prolactin § Manifestations: § Galactorrhea § Amenorrhea § Treatment: § Bromocriptine § Cabergoline § Causes: § Pituitary tumor
Ergot derivatives Cabergoline -PO with or without food -can be used to correct amenorrhea, infertility and galactorrhea associated with a prolactinoma -can also cause tumor regression -immediate effects of decreased prolactin secretion -should monitor prolactin monthly until normal, treatment can stop after 6 months of normal levels -adverse effects: nausea, headache, dizziness Bromocriptine Similar, except is not tolerated as well as cabergoline
§ HYPERCORTISOLISM § Cushing Syndrome § Chronic exposure to excessive cortisol § Cushing Disease § Excessive secretion of ACTH § Cushing-Like Syndrome § Administration of synthetic glucocorticoids
§ Manifestations: § Weight gain § Fat deposits in face, trunk and cervical area (moon face, buffalo hump) § Glucose intolerance (hyperglycemia) § Protein wasting (thin extremities) § Osteoporosis § Collagen loss (thin, weak skin, striae, bruising) § Increased catecholamine activity (hypertension) § Increased mineralcorticoid activity (edema, potassium loss) § Cushing Disease in Females (increased androgen levels) § Increased hair growth § Acne § amenorrhea
§ Diagnostics: § Urine cortisol § Dexamethasone suppression test § Measurement of ACTH and cortisol levels
§ Treatment: treat underlying cause tumor removal radiation therapy Ketoconazole antifungal, but also blocks glucocorticoid synthesis 600 -800 mg/day (high doses) must monitor liver enzymes at this high dose
§ HYPOCORTISOLISM § Addison’s Disease (Primary Adrenal Insufficiency) : increased ACTH, decreased cortisol and aldosterone § Secondary Adrenal Insufficiency : decreased ACTH § Causes: § Autoimmune attack of the adrenal cortex (Primary Adrenal Insufficiency) § Prolonged administration of glucocorticoids (Secondary Adrenal Insufficiency) § Pituitary tumors (Secondary Adrenal Insufficiency) § Infections (tuberculosis)
§ Manifestations: § Weakness § Fatigue § Hyperpigmentation of the skin (only in Addison’s disease) § Weight loss § Hypotension § Hypoglycemia § Syncope
§ Diagnostics: § Hyperkalemia § Hyponatremia § Hypoglycemia § Decreased serum and urine cortisol § Increased ACTH (Addison’s Disease)
§ Treatment: § Lifelong glucocorticoid supplementations (higher doses during acute stressors) § Hydrocortisone § Mineralcorticoid supplementation § Fludrocortisone
§ Hydrocortisone § For use in Addison’s Disease § Take entire dose in am or 2/3 in am and remainder in afternoon § Lifelong supplementation § Increased dose at times of stress § Excessive doses can produce symptoms of Cushing’s Syndrome
§ Fludricortisone § Mineralcorticoid replacement § 0. 1 mg PO daily § Used in combination with glucocorticoid § Adverse effects: § With high doses § Hypertension § Hypokalemia § Weight gain § Edema
§ Caused by adrenal adenomas or carcinomas § Feminization: development of female secondary sex characteristics § Gynecomastia, testicular atrophy, decreased libido, early development of sex characteristics § Virilization: development of male secondary sex characteristics § Excessive face/body hair growth, clitoral enlargement, amenorrhea, acne, breast atrophy
§ PHEOCHROMOCYTOMA § Causes continuous, excessive secretion of catecholamines § Rare and can be malignant § Manifestations: § Hypertension, tachycardia, diaphoresis, palpitations, headaches, hypermetabolism § Treatment: § Check for excessive catecholamines in blood and urine § Surgical removal of tumor § Alpha and beta blockers
 Neuroendocrine system
Neuroendocrine system N
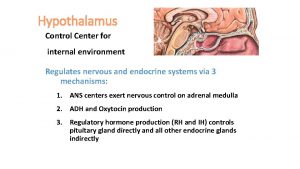
N Mechanisms of hypothalamic control over endocrine function
Mechanisms of hypothalamic control over endocrine function Neuroendocrine reflex ppt
Neuroendocrine reflex ppt Neuroendocrine syndrome in gynecology
Neuroendocrine syndrome in gynecology Hypothalamus function in sleep
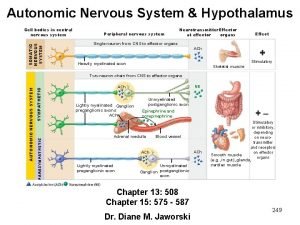
Hypothalamus function in sleep Hypothalamus ans
Hypothalamus ans Vplnt
Vplnt Papez circuit ppt
Papez circuit ppt Preoptic area hypothalamus
Preoptic area hypothalamus Hypothalamus
Hypothalamus What is the function of the hypothalamus
What is the function of the hypothalamus Myxedima
Myxedima Psychology chapter 9 motivation and emotion
Psychology chapter 9 motivation and emotion Calcitonin and pth are antagonistic hormones
Calcitonin and pth are antagonistic hormones Hypothalamus mri coronal
Hypothalamus mri coronal Where is trh produced
Where is trh produced Hypothalamus function
Hypothalamus function Hypothalamus hormones
Hypothalamus hormones Hypothalamus hormones
Hypothalamus hormones Lh and fsh in males
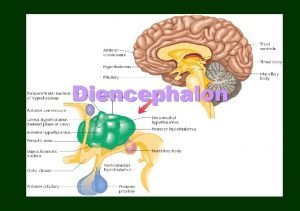
Lh and fsh in males Thalamus
Thalamus Hypothalamus hormones
Hypothalamus hormones Somatic nervous system neurotransmitters
Somatic nervous system neurotransmitters Hypothalamus epinephrine
Hypothalamus epinephrine 9 months
9 months Corticoliberin
Corticoliberin Pituitary gland
Pituitary gland Hypothalamus eating disorders
Hypothalamus eating disorders Fasciculus lenticularis
Fasciculus lenticularis Hypothalamus
Hypothalamus Eminentia mediana hypothalamus
Eminentia mediana hypothalamus Human reproductive system
Human reproductive system Secretory gland
Secretory gland Hypothalamus hormones
Hypothalamus hormones Endocrine organ histology
Endocrine organ histology Spinal cord structures
Spinal cord structures Le message hormonal
Le message hormonal Thermolyse
Thermolyse Pituitary gland
Pituitary gland Agrp hypothalamus
Agrp hypothalamus Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em