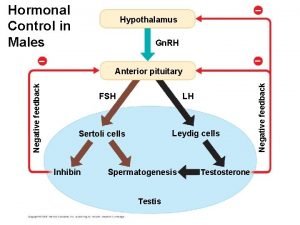
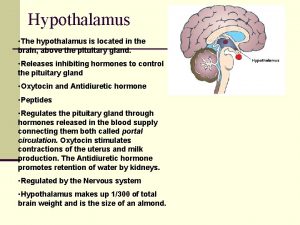
Hormonal Control in Males Hypothalamus Gn RH FSH


- Slides: 20
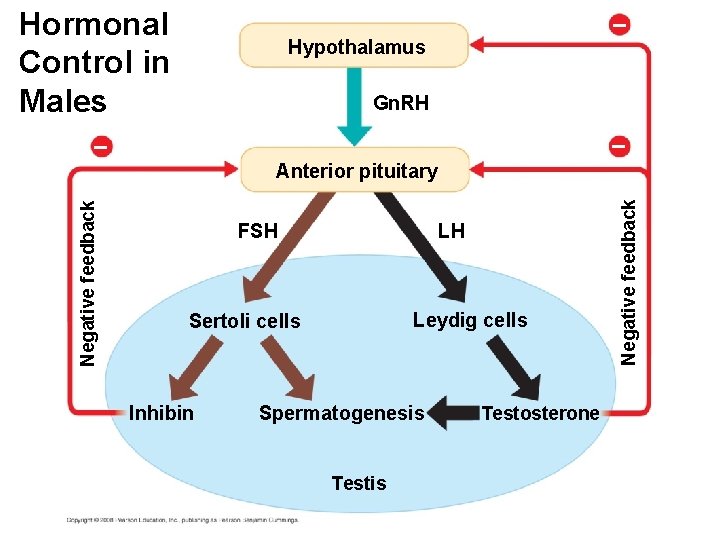
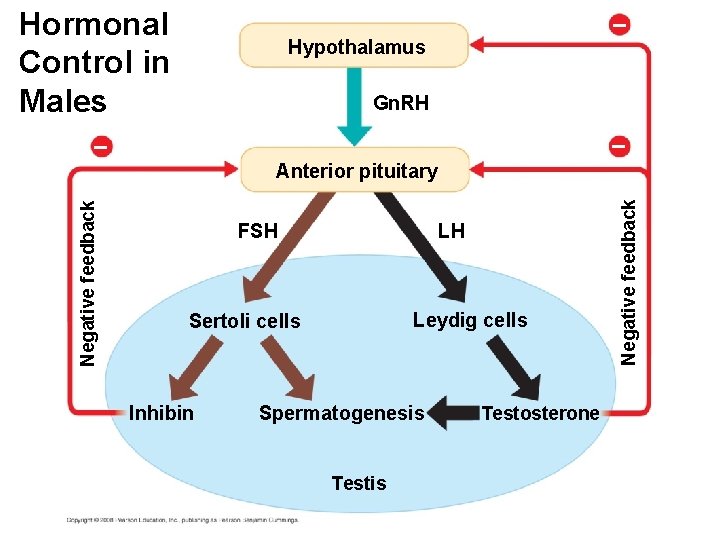
Hormonal Control in Males – Hypothalamus Gn. RH – – FSH LH Leydig cells Sertoli cells Inhibin Spermatogenesis Testosterone Negative feedback Anterior pituitary
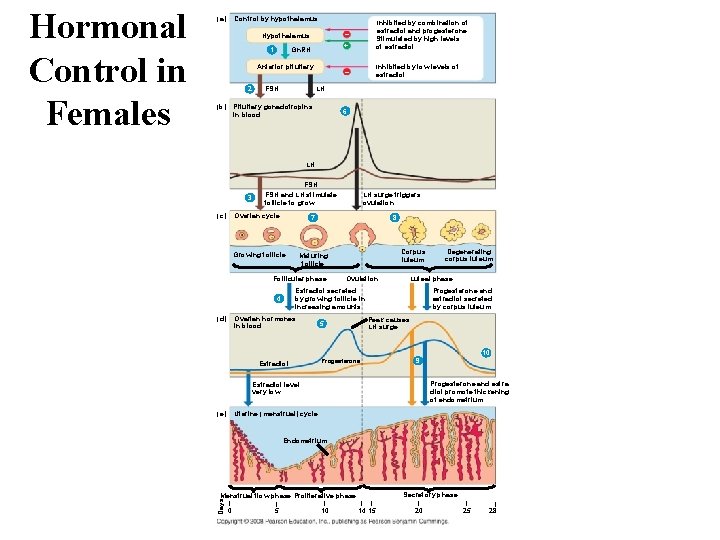
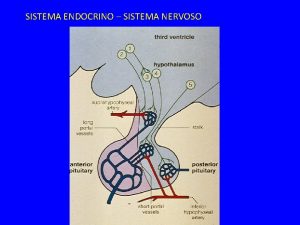
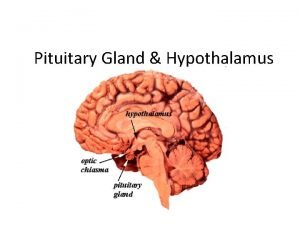
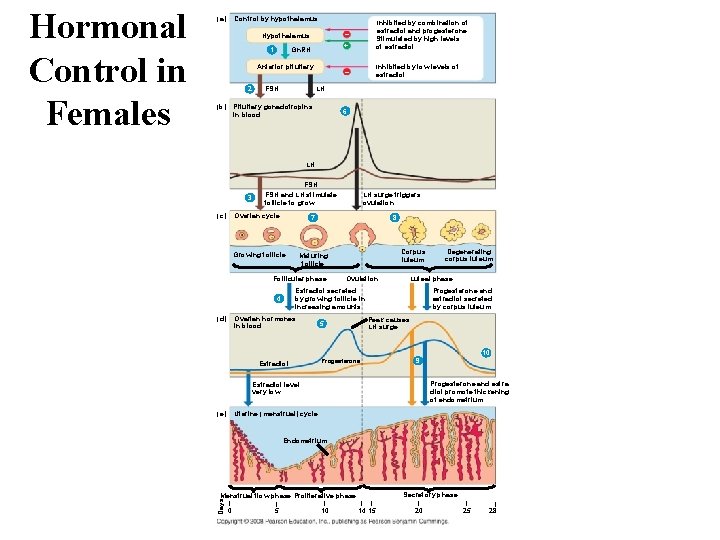
Hypothalamus – Gn. RH + Inhibited by combination of estradiol and progesterone Stimulated by high levels of estradiol – Inhibited by low levels of estradiol 1 Anterior pituitary 2 (b) FSH LH Pituitary gonadotropins in blood 6 LH FSH 3 (c) FSH and LH stimulate follicle to grow Ovarian cycle 8 Corpus luteum Maturing follicle Follicular phase Ovulation Ovarian hormones in blood Degenerating corpus luteum Luteal phase Estradiol secreted by growing follicle in increasing amounts 4 (d) LH surge triggers ovulation 7 Growing follicle Progesterone and estradiol secreted by corpus luteum Peak causes LH surge 5 10 Estradiol 9 Progesterone and estradiol promote thickening of endometrium Estradiol level very low Uterine (menstrual) cycle (e) Endometrium Secretory phase Menstrual flow phase Proliferative phase Days Hormonal Control in Females Control by hypothalamus (a) | 0 | 5 | 10 | | 14 15 | 20 | 25 | 28
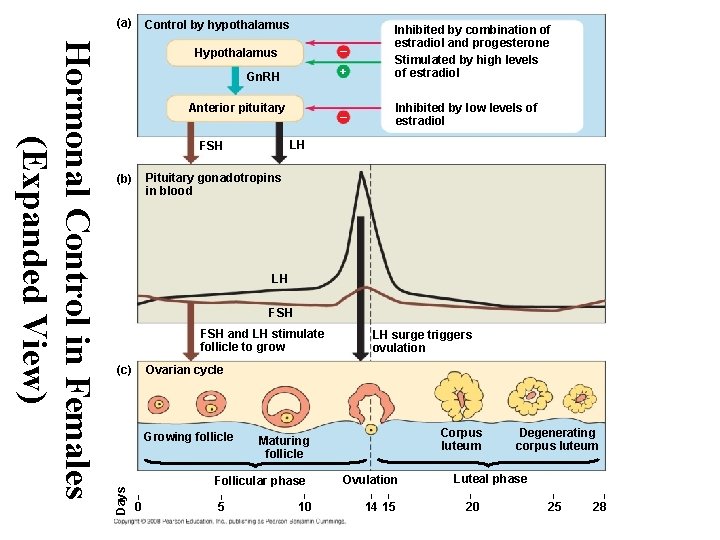
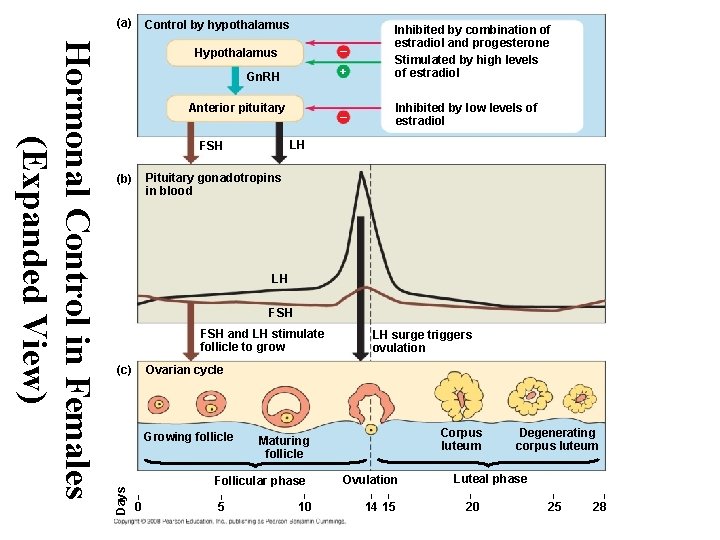
(a) Control by hypothalamus – Gn. RH + – Inhibited by low levels of estradiol Anterior pituitary LH FSH Pituitary gonadotropins in blood (b) LH FSH and LH stimulate follicle to grow LH surge triggers ovulation Ovarian cycle (c) Growing follicle Days Hormonal Control in Females (Expanded View) Hypothalamus Inhibited by combination of estradiol and progesterone Stimulated by high levels of estradiol Corpus luteum Maturing follicle Follicular phase | | | 0 5 10 Ovulation | | 14 15 Degenerating corpus luteum Luteal phase | 20 | 25 | 28
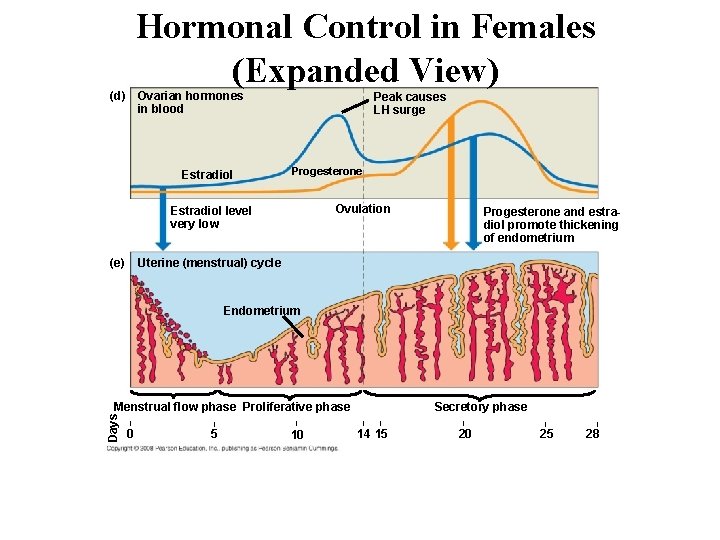
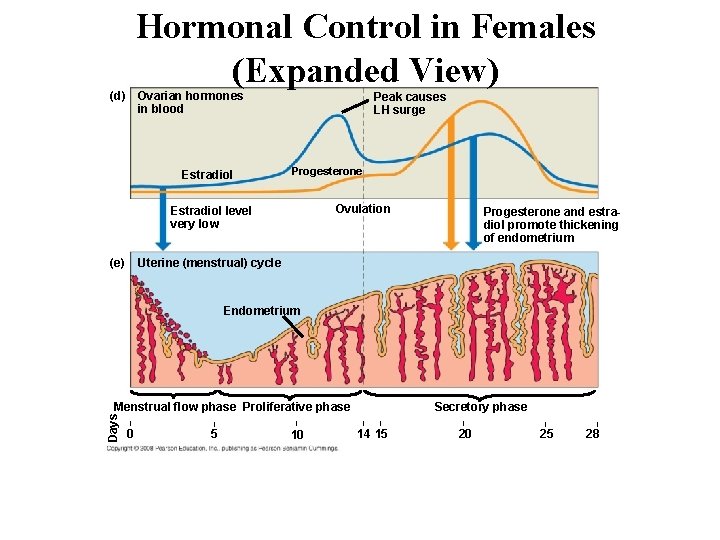
Hormonal Control in Females (Expanded View) (d) Ovarian hormones in blood Estradiol Peak causes LH surge Progesterone Ovulation Estradiol level very low (e) Progesterone and estradiol promote thickening of endometrium Uterine (menstrual) cycle Endometrium Days Menstrual flow phase Proliferative phase | 0 | | 5 10 Secretory phase | | 14 15 | 20 | 25 | 28
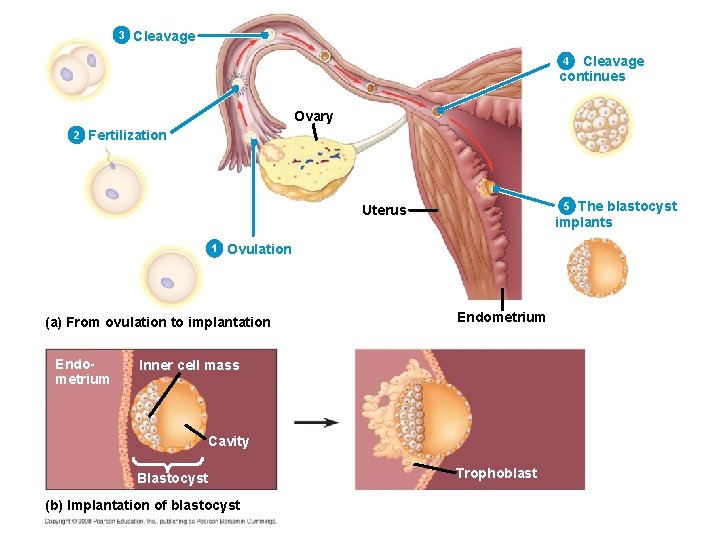
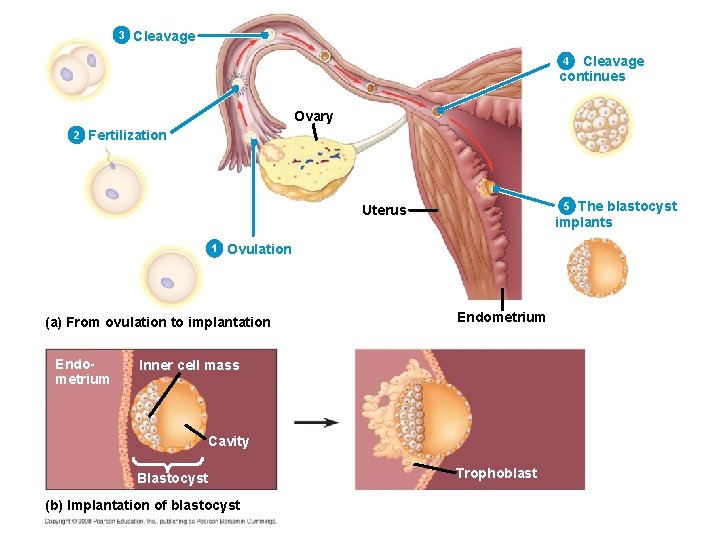
3 Cleavage continues 4 Ovary 2 Fertilization The blastocyst implants 5 Uterus 1 Ovulation (a) From ovulation to implantation Endometrium Inner cell mass Cavity Blastocyst (b) Implantation of blastocyst Trophoblast
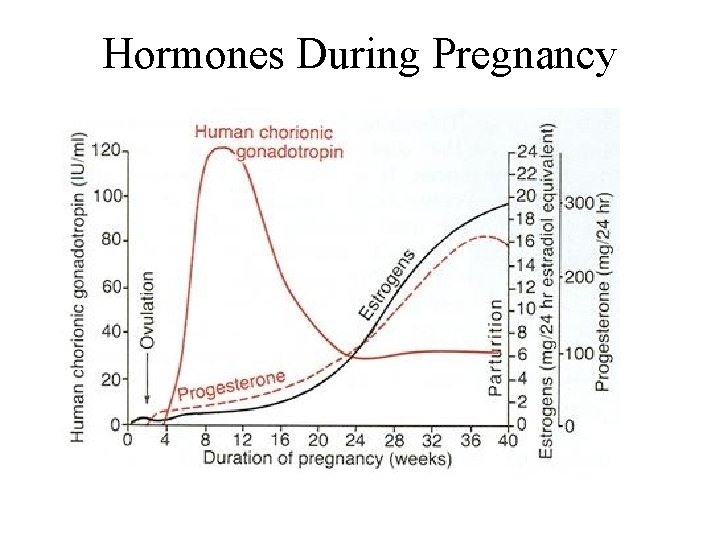
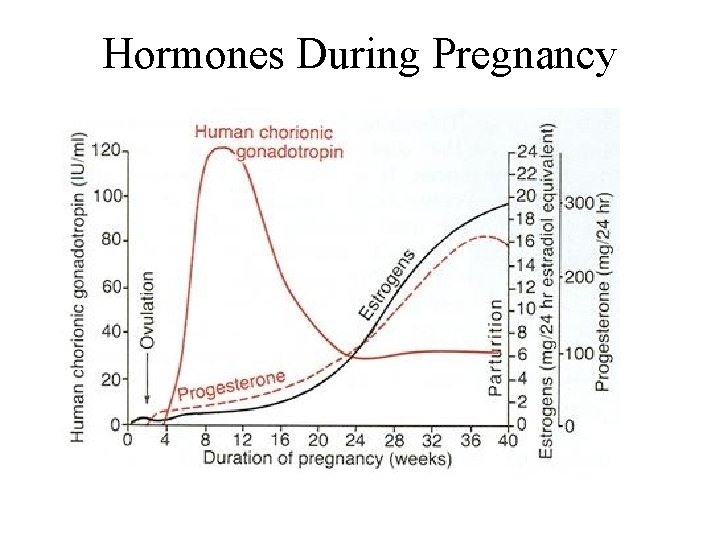
Hormones During Pregnancy

Maternal Fetal Blood Flow Maternal arteries Maternal veins Placenta Maternal portion of placenta Umbilical cord Chorionic villus, containing fetal capillaries Maternal blood pools Uterus Fetal arteriole Fetal venule Umbilical cord Fetal portion of placenta (chorion) Umbilical arteries Umbilical vein
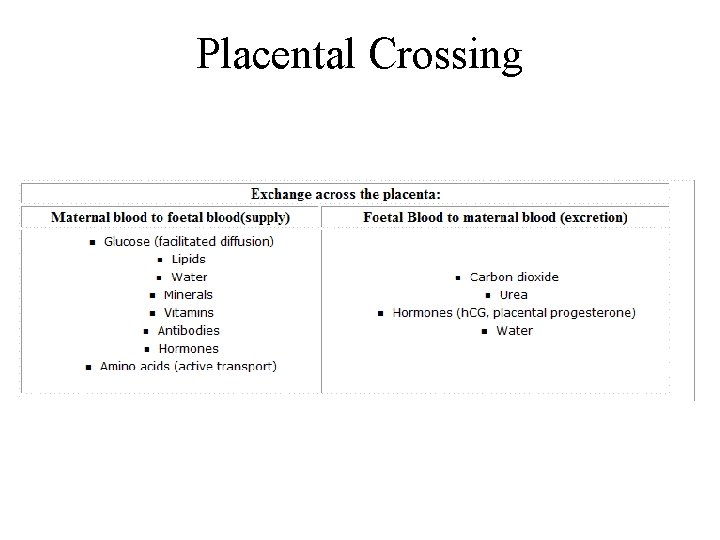
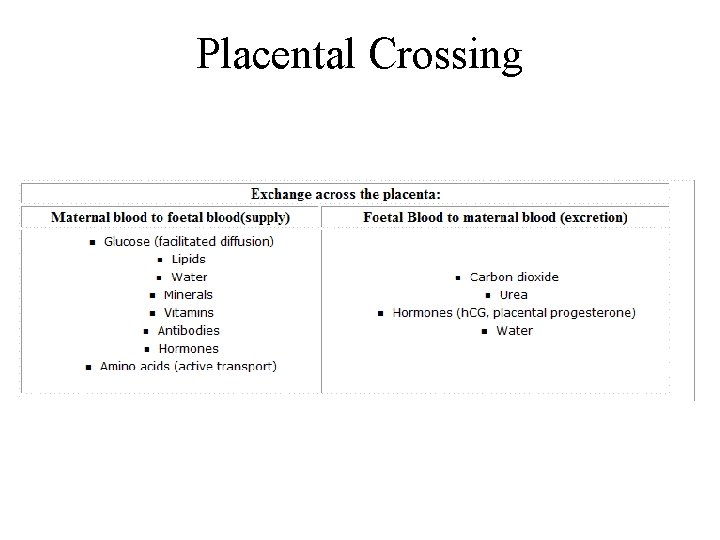
Placental Crossing
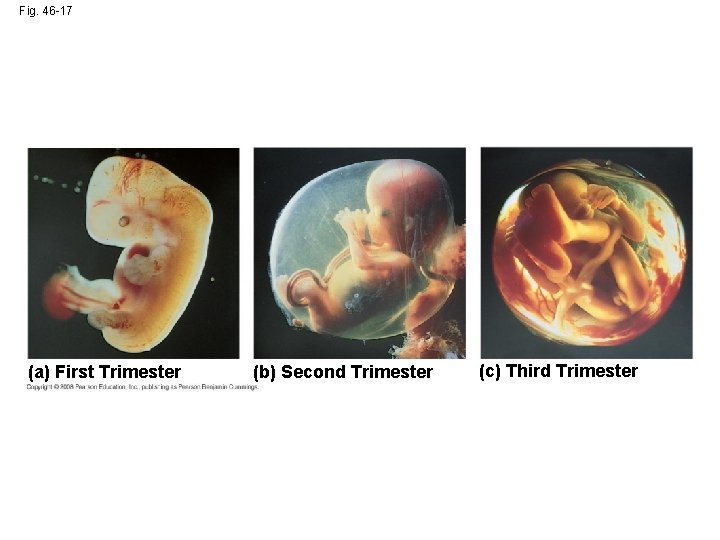
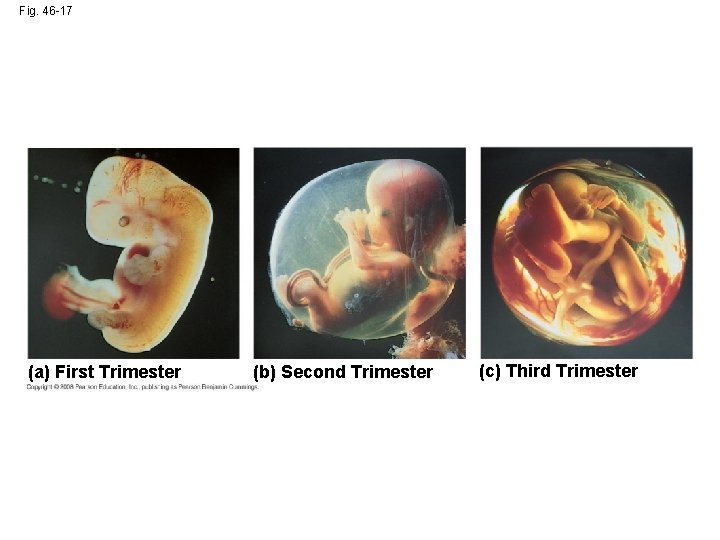
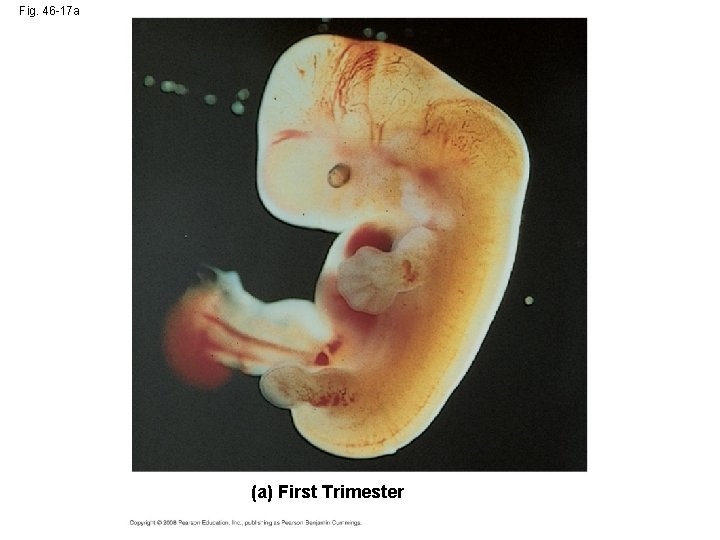
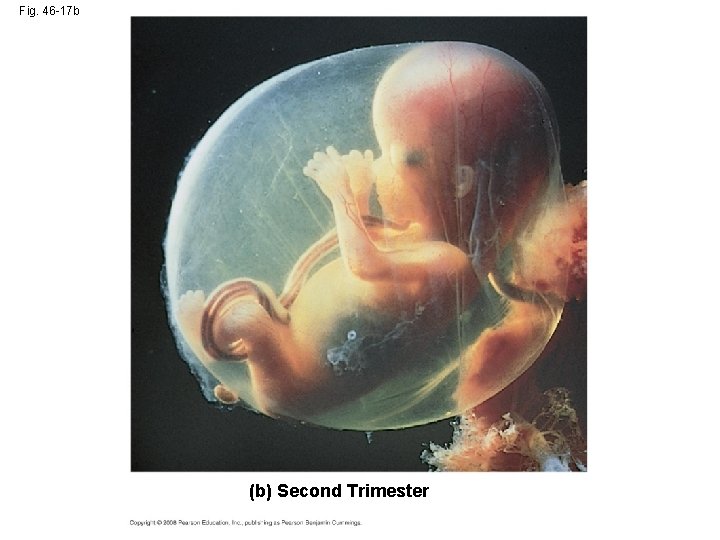
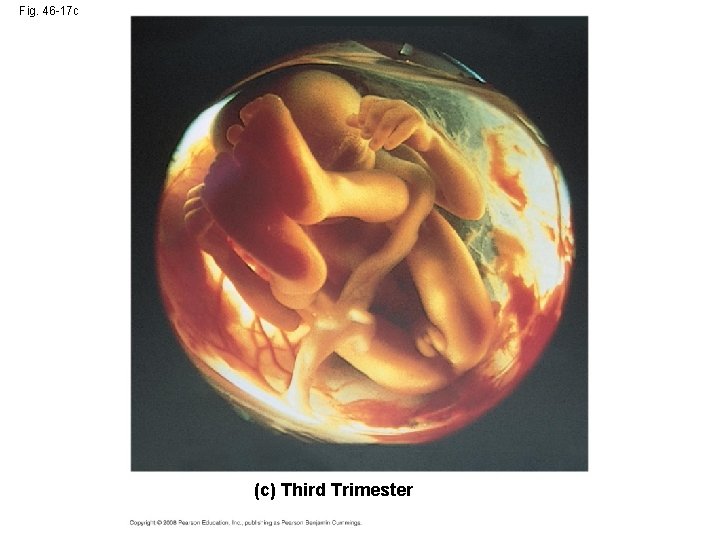
Fig. 46 -17 (a) First Trimester (b) Second Trimester (c) Third Trimester
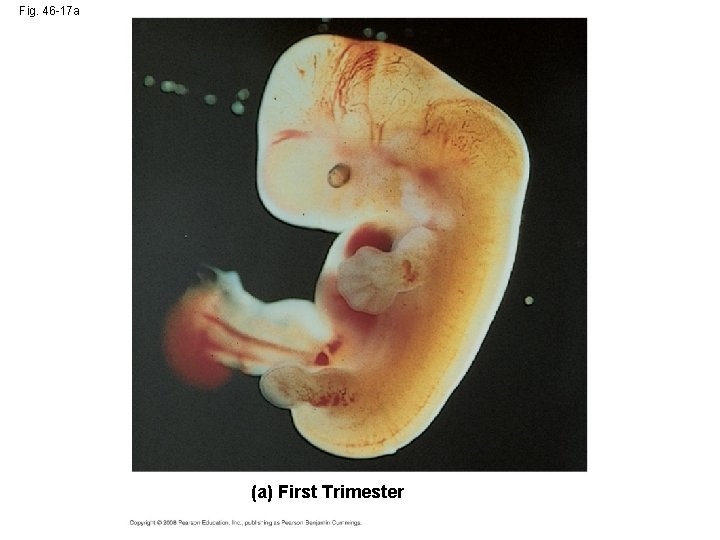
Fig. 46 -17 a (a) First Trimester
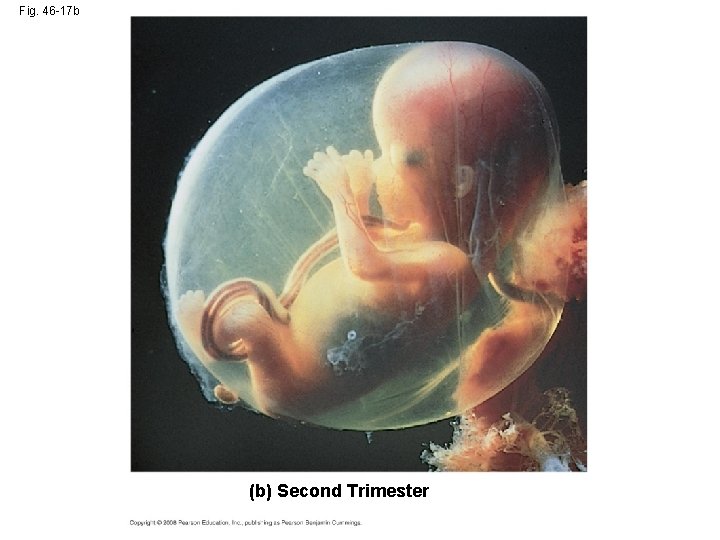
Fig. 46 -17 b (b) Second Trimester
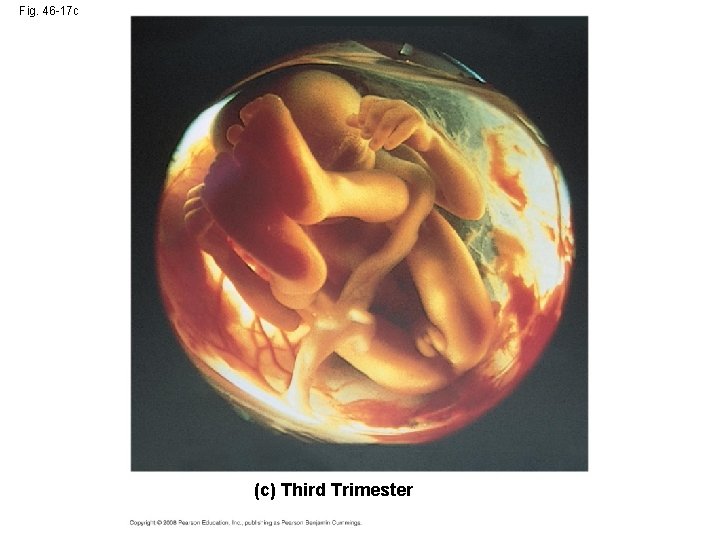
Fig. 46 -17 c (c) Third Trimester
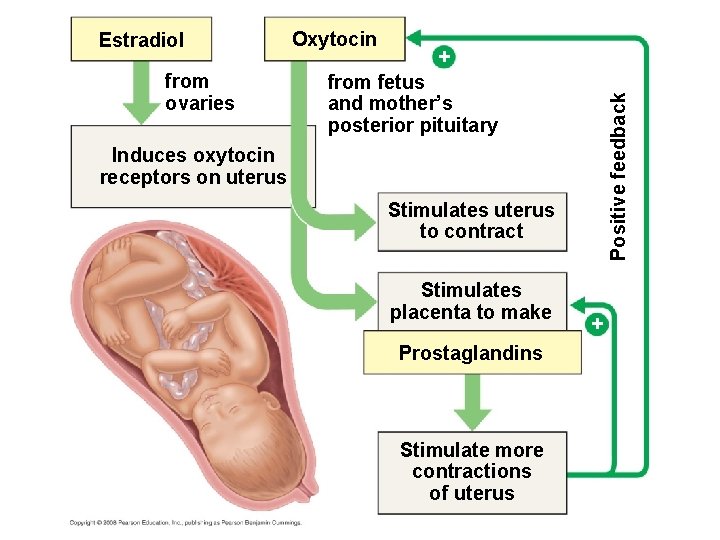
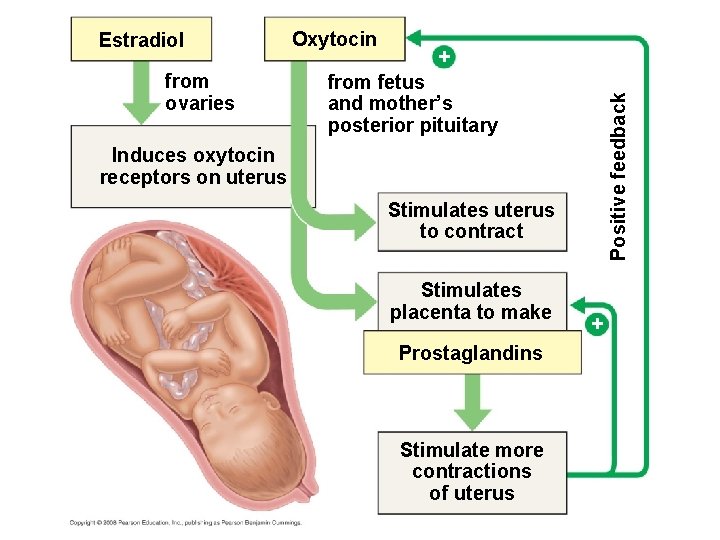
from ovaries Oxytocin + from fetus and mother’s posterior pituitary Positive feedback Estradiol Induces oxytocin receptors on uterus Stimulates uterus to contract Stimulates placenta to make Prostaglandins Stimulate more contractions of uterus +
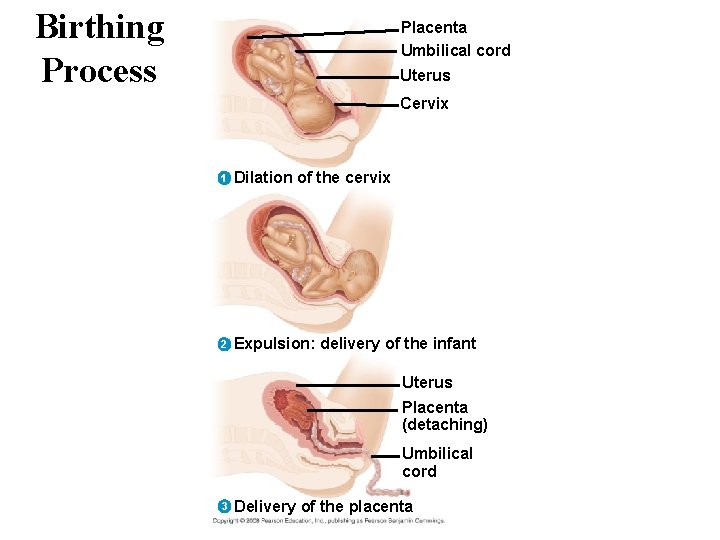
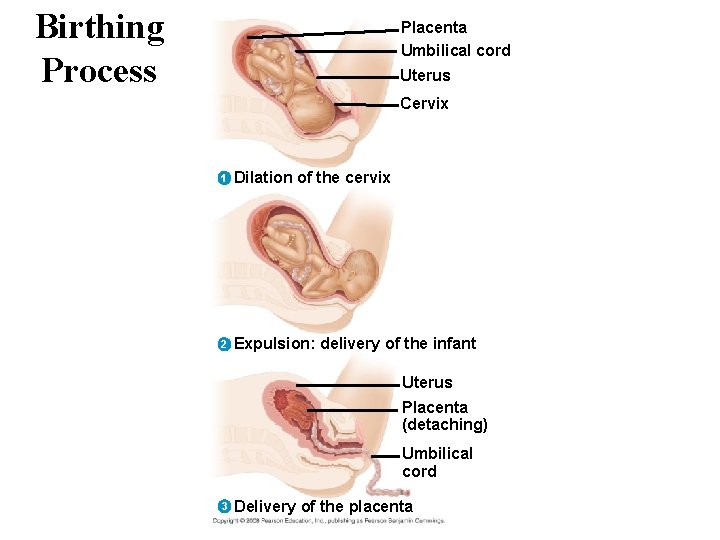
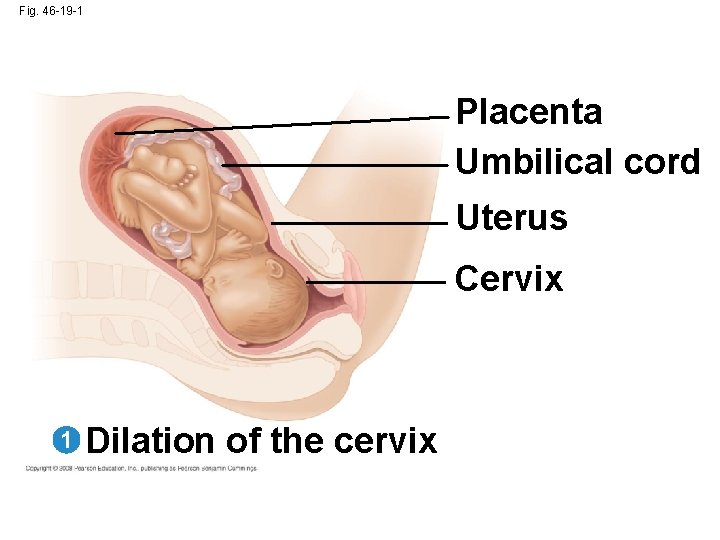
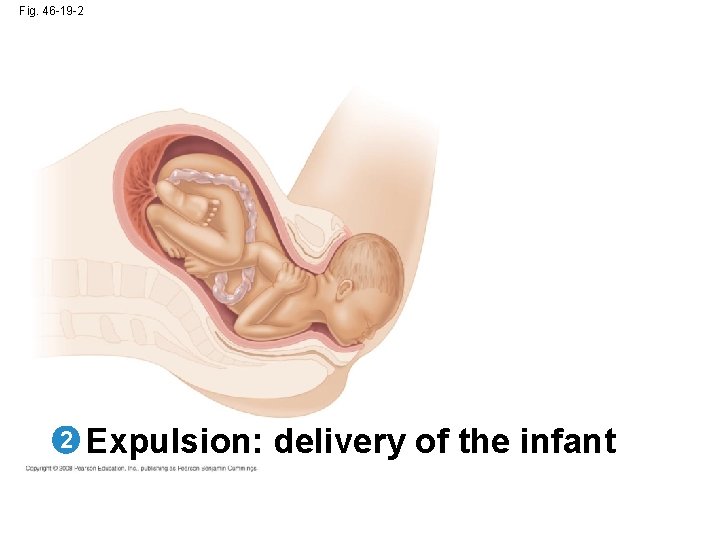
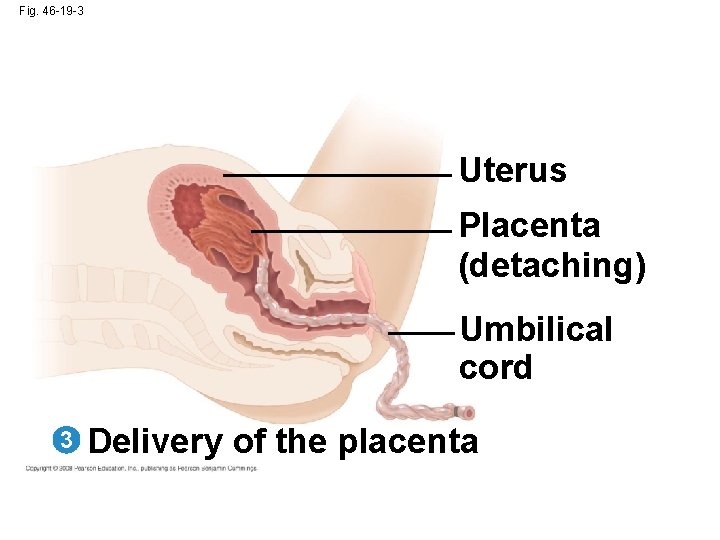
Birthing Process Placenta Umbilical cord Uterus Cervix 1 Dilation of the cervix 2 Expulsion: delivery of the infant Uterus Placenta (detaching) Umbilical cord 3 Delivery of the placenta
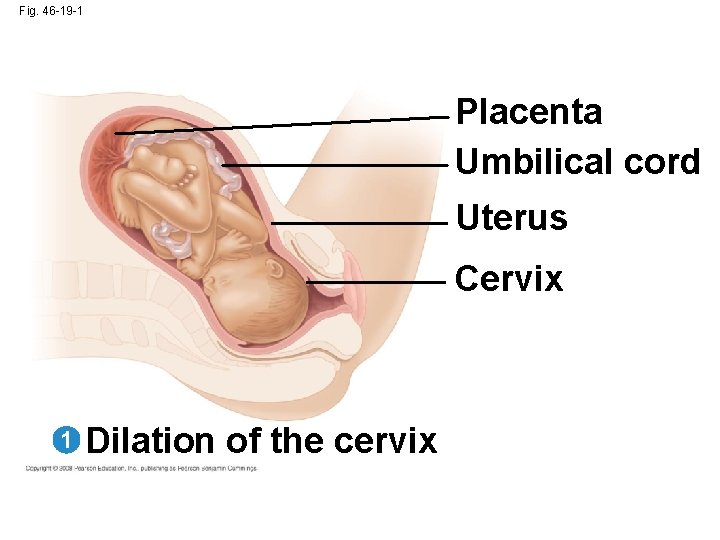
Fig. 46 -19 -1 Placenta Umbilical cord Uterus Cervix 1 Dilation of the cervix
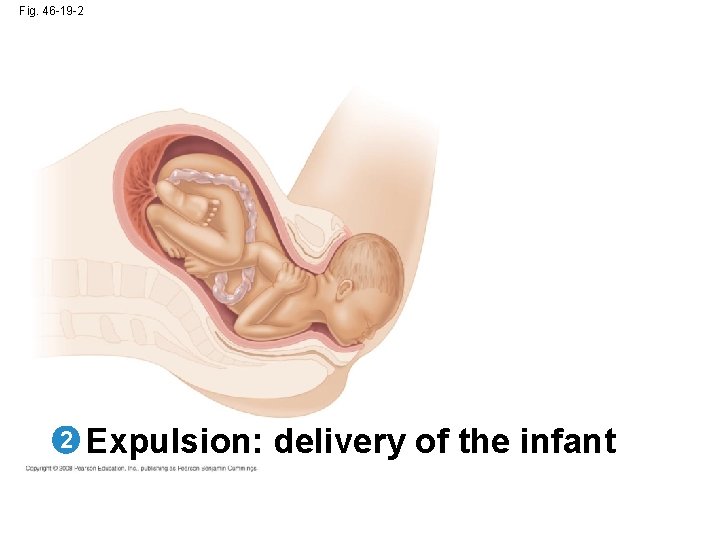
Fig. 46 -19 -2 2 Expulsion: delivery of the infant
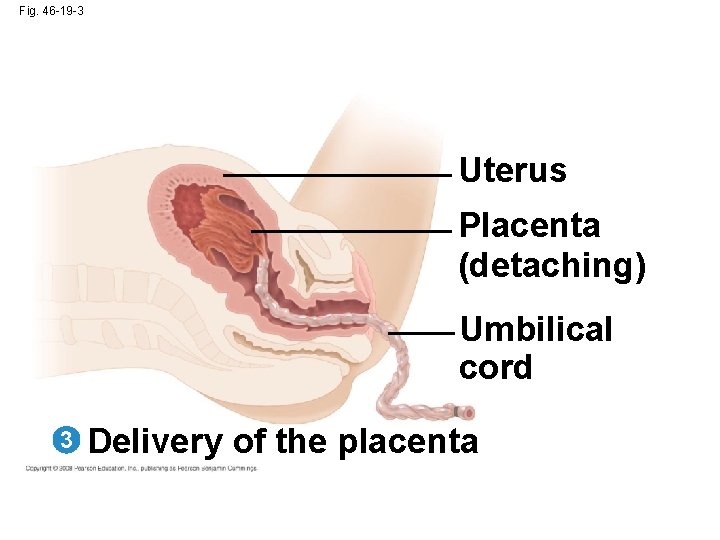
Fig. 46 -19 -3 Uterus Placenta (detaching) Umbilical cord 3 Delivery of the placenta
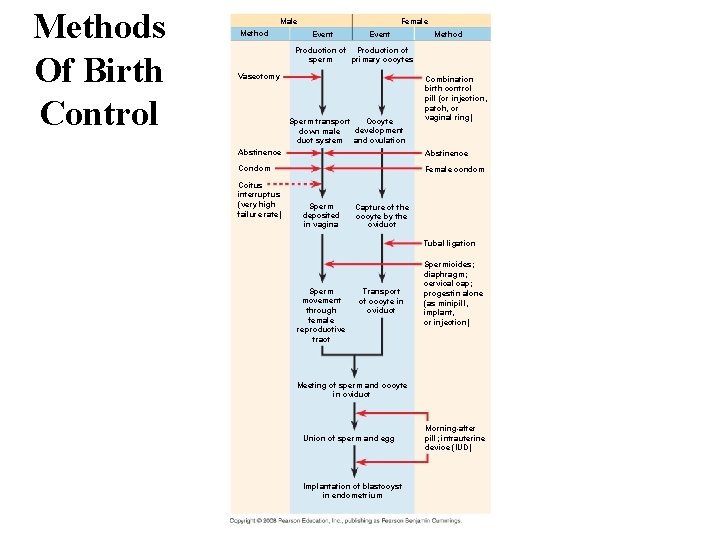
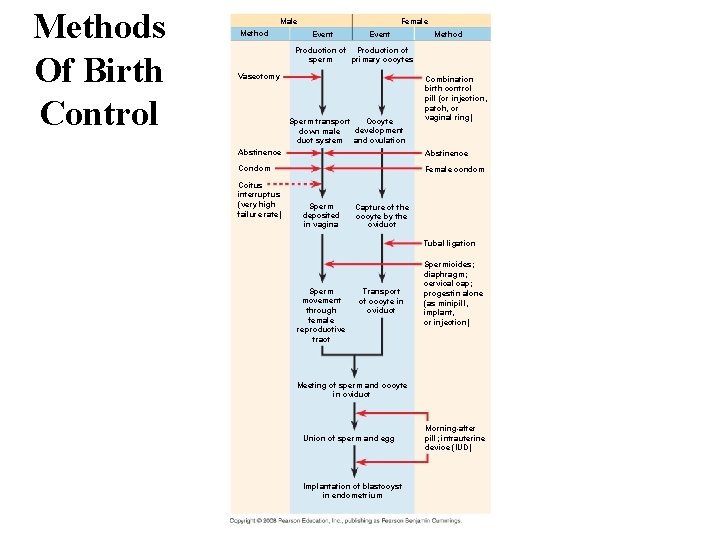
Methods Of Birth Control Male Method Female Event Method Production of sperm primary oocytes Vasectomy Oocyte Sperm transport development down male duct system and ovulation Combination birth control pill (or injection, patch, or vaginal ring) Abstinence Condom Female condom Coitus interruptus (very high failure rate) Sperm deposited in vagina Capture of the oocyte by the oviduct Tubal ligation Sperm movement through female reproductive tract Transport of oocyte in oviduct Spermicides; diaphragm; cervical cap; progestin alone (as minipill, implant, or injection) Meeting of sperm and oocyte in oviduct Union of sperm and egg Implantation of blastocyst in endometrium Morning-after pill; intrauterine device (IUD)
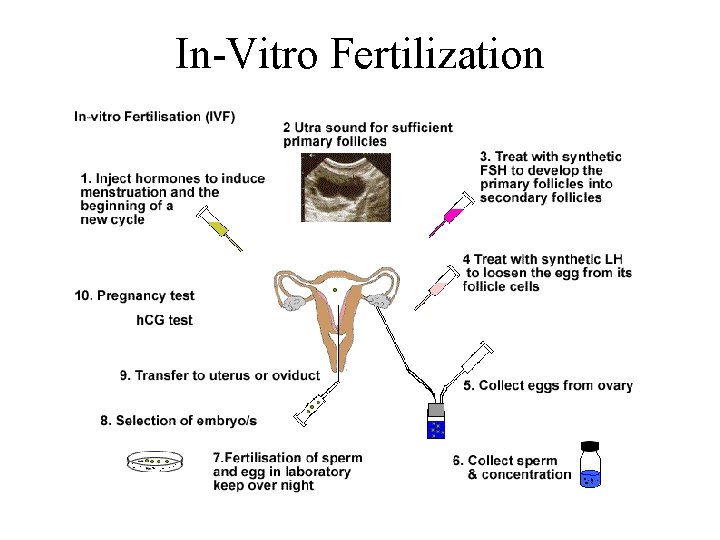
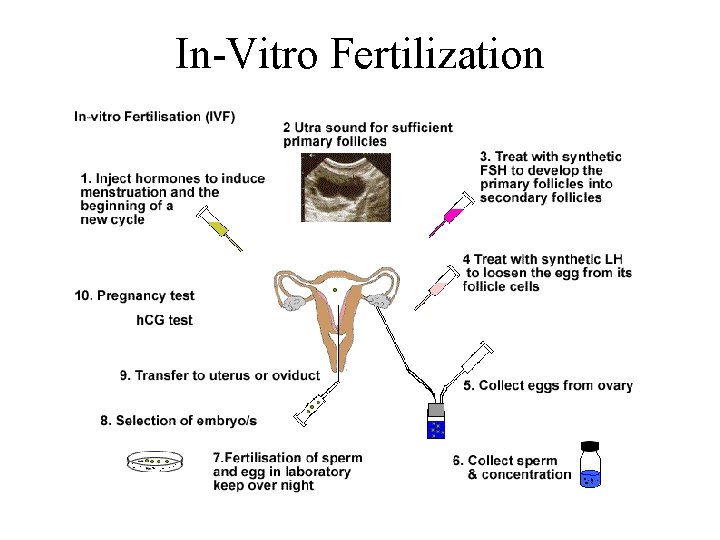
In-Vitro Fertilization

Ethics of In-Vitro Fertilization • Advantages of IVF: there as many reasons for this treatment as there are people seeking this treatment. – over comes infertility – allow families for people who must be sterilised e. g. . radiography/chemo therapy cancer patients • Disadvantages of IVF: – what happens to unwanted embryo's – what happens to orphaned embryo's – should infertility be by-passed
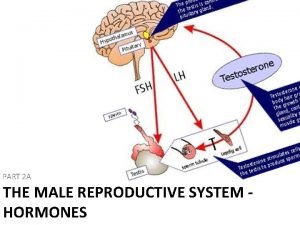
 Lh and fsh in males
Lh and fsh in males In males, fsh prods these organs to produce testosterone.
In males, fsh prods these organs to produce testosterone. Fsh and lh in female reproductive system
Fsh and lh in female reproductive system Distrofia fsh
Distrofia fsh Fsh alto
Fsh alto Fsh valori
Fsh valori Fsh valori
Fsh valori Premenopausa
Premenopausa Fsh alto
Fsh alto Prof lupoli, endocrinologo napoli
Prof lupoli, endocrinologo napoli Premenopausa sintomi seno
Premenopausa sintomi seno Fsh alto
Fsh alto Mistagmus
Mistagmus Sexualizare definitie
Sexualizare definitie Gena sry prezenta
Gena sry prezenta Funcion de las proteinas en los seres vivos
Funcion de las proteinas en los seres vivos Pearson
Pearson Fsh
Fsh What is fsh
What is fsh Recombinant fsh
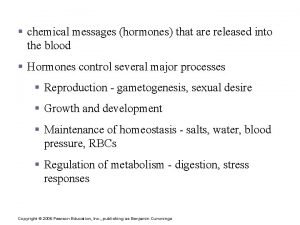
Recombinant fsh Hormonal stimulus
Hormonal stimulus